Abstract
This research tested the prediction that reading a preventive brochure leads people to watch a preventive video, and that watching this video in turn leads to an increase in the likelihood of participating in a preventive counseling session. A sample of men and women from a southeastern community in the United States was recruited for a general health survey with the objective of examining participation in HIV-prevention interventions. Unobtrusive measures of exposure to HIV-prevention brochures, an HIV-prevention video, and an HIV-prevention counseling session were obtained. Findings indicated that reading the brochures increased watching the video and that watching the video increased participation in the counseling session. The association between exposure to the video and exposure to the counseling was mediated by expectations that the counseling would be useful. Findings are discussed in terms of the need to ensure exposure to interventions to achieve intervention effectiveness.
Keywords: HIV prevention, Selective exposure, Participation in health promotion programs
HIV-prevention interventions are normally tested under conditions that allow researchers to detect behavior change while removing biases in participant selection into the intervention (Erhardt et al. 2002; Rabinowitz 2002; Raj et al. 2001; Tobias et al. 2006). Despite this valuable dominant approach, in real-world conditions, people choose to enroll in preventive interventions (Catania et al. 1990; Lauby et al. 1996; DiFrancesco et al. 1998; Hennessy et al. 2002; Veach et al. 2000). Moreover, some of the audiences most vulnerable to HIV choose not to enroll in HIV-prevention interventions (Noguchi et al. (in press); Yancey et al. 2006), requiring research on the conditions that increase participation in HIV-prevention interventions.
The present research concerned associations among exposure to HIV-prevention brochures, HIV-prevention videos, and HIV-prevention counseling as presented to high-HIV-risk clients of health facilities. Of these strategies, Albarracín et al. (2003) showed that brochures are less effective than either videos and face to face communications, and Albarracín et al. (2005) found that face to face interventions are more effective than non-face to face interventions. In fact, the amount of change in condom use is d = 0.11 for brochures and posters, d = 0.31 for videos, television, and radio, and d = 0.26 for face-to-face interventions (all significantly different from d = 0.08 in control groups; reanalysis of Albarracín et al. (2005)).
In the present research, we hypothesized that, although brochures alone may not trigger changes in risky behavior (see Albarracín et al. 2005), they may augment exposure to a more effective video available shortly after the brochures. Similarly, a video with modest behavioral effects may yield agreement to partake in an HIV-prevention counseling session. As client-tailored counseling has proven efficacious for a variety of populations (Albarracín et al. 2005), any tool that increases exposure to it is of value for curbing infection with HIV. Using unobtrusive observations of exposure to brochures, videos, and counseling, the present research examined these hypothetical associations and their potential cognitive mediators.
From Brochures to Videos to Counseling
The hypothesis guiding this paper was that exposure to HIV-prevention programs may increase as a function of exposure to other HIV-prevention programs. In particular, participation in a relatively simple and brief strategy (e.g., reading a brochure) may facilitate later exposure to a more complex and likely effective strategy (e.g., watching a video or participating in a counseling session). For example, attitudes toward HIV-prevention programs may become more favorable as one is exposed to these programs. In fact, such tendencies have been documented by research on mere exposure, which denotes the ability of exposure to an object to automatically increase liking for the object (Zajonc 1968). For example, compared to people who do not read an HIV-prevention brochure, those who do may expect a subsequent HIV-prevention video to be more useful or favorable (i.e., the audience may have a more positive attitude about preventive programs). Hence, the expectation that the video is useful may mediate the greater exposure to the video following exposure to the brochure.
A different reason to expect that initial exposure to HIV-prevention materials will increase later exposure is that the initial material may decrease perceived threats to recipients' attitudes and behavioral practices (Brehm 1966; see also Albarracín and Mitchell 2004; McGuire 1964; Schlenker et al. 1994). People who normally worry that counseling might limit their freedom, for example, may be reassured by commonly used, unimposing HIV-prevention videos. In turn, this decreased threat may increase exposure to future programs designed to produce a change to condom use (Albarracín and Mitchell 2004). For example, the foot-in-the-door principle (Freedman and Fraser 1966) has been used to increase compliance with a request to become an organ donor, complete a long dietary survey via the internet, and take a taxi while under the influence of alcohol (Girandola 2002; Gueguen 2002; Taylor and Booth-Butterfield 1993). Although a meta-analysis of studies revealed that the foot-in-the-door effect was at best weak (Dillard et al. 1984), the effect could be present in exposure to HIV-prevention interventions. Such an effect may be mediated by expectations that given little imposition in the initial requests, subsequent ones will not be threatening.
Yet another reason to expect associations among exposure to different HIV-prevention programs is that early exposure may increase fear of HIV. If, as hypothesized in various theoretical models (see Breckler 1984; Fisher and Fisher 1992, 2000), fear of HIV motivates people to engage in protective behavior, an increase in fear could influence exposure to later programs that promote risk reduction. In this situation, fear of HIV may mediate the positive influence of exposure to an earlier program on participation in subsequent programs. Alternatively, fear can also trigger defensive cognitive processes, including avoidance of thoughts about the source of the fear (e.g., HIV) (Rogers 1975). If this is the case, initial programs that increase fear may ultimately reduce exposure to subsequent programs.
Present Research
To examine exposure to different HIV-prevention programs over the course of a visit to a health facility, a high-risk sample of sexually active participants from Gainesville (FL) was recruited for a health interview. Halfway through the interview, the interviewer paused the administration, announcing a break. At that point, an observer/counselor entered the room to do work unrelated to the interview, and unobtrusively recorded the participant's exposure behavior (Webb et al. 1966). Specifically, participants had the opportunity to (a) read HIV-prevention brochures, (b) watch a video on HIV prevention, and (c) participate in a brief HIV-risk-reduction counseling session. Thus, the behavior of the participant was observed and could be recorded with respect to the brochures, the video, and the counseling. Analyses were conducted to study associations among the three exposure measures, followed by tests of mediation.
Method
Participants
Participants were 400 community members (295 females and 105 males) who were paid $5 for the eligibility screening and $40 for participation in the main study if eligible. Non-eligible participants were paid a total of $5, and completers were paid a total of $45. Eighty percent of the participants were recruited through flyers placed in the community, and the remaining 20% from referral from the Alachua County Health Department clinics. Seventy-four percent of the participants were female, the M age was 33.73 (SD = 10.41), and the sample was ethnically diverse (59% African-American, 34% European-American, 4% Latino-American, 1% American Indian, 1% Asian-American, 3% of other ethnicities). Fifty-four percent of the sample had an income of less than $10,000 a year, and 78% graduated from high school, with an average of 12.77 (SD = 2.45) years of school. Ninety-five percent of the sample reported having a main partner, and participants had a M of 0.19 (SD = 0.50) STIs in the previous year. In terms of condom use, 46% of the participants never used condoms in the previous six months, 36% used condoms sometimes, and 19% almost never.
Research Team
The staff of the study consisted of an interviewer and an observer/counselor. The interviewer administered the questionnaire and offered the materials to the participant. During the interviewer's absence, the observer/counselor recorded the participant's behavior in relation to HIV-prevention brochures, a video, and a counseling program, and also facilitated the HIV-risk-reduction counseling session if the participant accepted.
Procedure
Recruitment
Patients were either recruited by flyers placed in the Health Department, in the surrounding community, or through referral from members of the community or the clinics of the Health Department. To prevent contamination and reduce self-selection, the study was described in the flyer and instructions for referrals as a “general health study;” there was no mention of HIV or condom use in either the flyer or the referral instructions.
To make an appointment, participants called a designated number. During this phone call, a brief eligibility pre-screening was conducted. Participants had to be 18–50 years old, sexually active, not be pregnant or have a partner who was pregnant, and report using condoms “never,” “almost never,” or “sometimes” during the last six months. People younger than 18 years old or older than 50 years old, sexually inactive participants, pregnant participants or those with a pregnant partner, and consistent condom users were excluded. These recruitment restrictions, including age, were in place to make sure that the sample was truly at highest risk for infection with HIV (Centers for Disease Control 2005).
Interview Protocol
When participants arrived for their interview, they checked in at the front desk of the Alachua County Health Department and waited to be seen. When the interviewer was ready, the participant was taken to the interview room where s/he was re-screened for eligibility using the brief phone questionnaire. If the participant was still eligible, the interview began. The interviewer recorded gender, age, past condom use, presence of a main sexual partner, years of education, income, and ethnicity. There were also general health questions (e.g., “Do you feel tightness in your chest? YES/NO,” “On average, how many cigarettes do you smoke per day?”), including number of past STIs (“In the past year, how many times have you had a sexually transmitted disease such as Syphilis, Gonorrhea, Herpes, and Chlamydia?”), and questions about condom use (e.g., “Of the times you have had sex in the last month, how many times did you use a condom?”). The main objective of the questionnaire was to facilitate the unobtrusive observation of exposure to HIV-prevention programs in the context of a general health study.
After 30 min elapsed, while the first part of the interview was being conducted, the observer/counselor knocked on the door of the interview room and requested to use the space to do work. The interviewer responded that they were in the middle of the interview but would call the counselor during the break. Subsequently, when the first half of the questionnaire was completed, the interviewer called the counselor and excused her/himself from the room.
While the counselor was in the room, the participant had 10 min to peruse the six brochures placed on the table. (These six brochures were prescreened and selected by health care professionals and community members on the basis of educational value and attractiveness to the target population). After 10 minutes elapsed, the interviewer knocked on the door and offered the participant a 10-minute video about HIV. The client could either accept or decline to watch the video. Next, the interviewer returned and offered the participant the option of participating in a HIV-risk-reduction counseling session. If the participant previously accepted the video, the interviewer waited 10 min before returning to offer the counseling. In contrast, if the participant declined to watch the video, the interviewer would only wait 5 min before returning to the room and offering the counseling to the participant. After the interviewer offered the counseling, if the participant accepted, the counselor was asked to counsel the participant. If the participant declined, however, the interviewer exited the room and returned 5 minutes later to administer the post-test questionnaire.
Materials
Brochures
Six brochures were used in this study. The titles were as follows and the color of each brochure is in parentheses: “Women & HIV: Think about It” (pink), “Men & HIV: Think about It” (blue), “Safer Sex Self-Test” (purple), “Condoms: Think about It,” (green), “HIV: Think about It,” (red), and “101 Ways to Avoid HIV” (multi-colored). The content was similar across the “Women & HIV: Think about It”, “Men & HIV: Think about It,” and “HIV: Think about It,” brochures, with information items such as: “You can have HIV and not know it,” “You can look fine and still pass HIV to others,” “You can't tell by looking at someone if they have HIV,” “If you (or a woman) get(s) HIV you (or she) can pass it to your (her) baby in the womb,” “Always carry condoms in your wallet (or purse),” “Talk about sex before you have sex,” “The best way to protect yourself is not to have sex,” “Never share needles or works.” The “Safer Sex Self-Test” and “Condoms: Think about It” brochures had recommendations more specific to when and how to use condoms (e.g., “Always make sure a condom is put on as soon as the penis is erect”) and facts concerning risky behaviors (e.g., “I know that getting drunk or using drugs can affect my judgment and make me more likely to take risks.”) The “101 Ways” brochure was a series of recommendations and some of the facts of the aforementioned brochures with items such as: “Anyone can get HIV,” “If you choose to be abstinent, avoid sexy situations.” Of note, the results of analyses with the continuous number of brochures were the same in direction and effect size as the results of chi-square tests with a dichotomous measure of brochure reading (1 = yes, 2 = no). For comparability with the other exposure measures, which were discrete, analyses are based on this dichotomous measure of brochure exposure.
Video
The video, a segment from “Just Like Me” (AIDS Risk Reduction Project 1997), contained informational and motivational arguments. It comprised a series of vignettes featuring people describing how they contracted HIV or what living with HIV entails. The video is quite emotional in tone.
Counseling
The counseling session included teachings of behavioral control or skills, including condom use behavioral skills, condom use negotiation skills, and self-management skills (specific techniques to promote control over the decision to use condoms). The counseling session also served to correct misconceptions about HIV and HIV transmission, as well as to foster positive attitudes toward condom use. The session was adapted from Project Respect (Centers for Disease Control 1997).1
Exposure Measures
The key dependent measures in the study were exposure to materials as reported by the observer. There were records of the number of brochures read, whether the participant accepted or declined the video, and whether the participant accepted or declined the counseling. Reports from both the participant and the observer were recorded to ensure reliability of these behavioral measures. Reliability between participant and observer reports of exposure was high, ranging from r (400) = .78, p < .01 to r (400) = 1.00, p < .01.
Measures of Potential Mediators
At the end of the session, participants were asked to retrospectively report their thoughts at the time they decided whether to watch the video and participate in the counseling session. They indicated whether they thought that the video and the counseling would (a) make it easier for them to use condoms, (b) be necessary for them, (c) not make them change their point of view, (d) force them to do things they did not like, (e) challenge their beliefs, (f) make them feel scared, and (g) make them worry about HIV and STIs. Participants responded to these items on a four-point scale with anchors 1 = not at all, 2 = a little, 3 = quite a bit, and 4 = a lot). We then combined these measures into three indices of expectations suggested by our predictions about potential mediators of exposure decisions and confirmed with factor analysis, χ2 (11) = 11.19, p > .43, CFI = 1.00, NNFI = 1.00, SRMR = 0.02. A factor of expectations of usefulness included the statements that participation “would make it easier for me to use condoms” and “is necessary for me” (α = .73 and .77 for the video and the counseling, respectively). A factor of expectations of threat to one's attitudes/behavior included the statements that participation “would not make me change my point of view [reverse scored],” “force me to do things I do not like,” and “would challenge my beliefs” (α = .67 and .61 for the video and the counseling, respectively). A factor of expectations of fear included the statements that participation “would make me feel scared” and “would make me worry about HIV and STD” (α = .67 and .72 for the video and the counseling, respectively).
Results
Preliminary Analyses
Preliminary analyses were conducted to describe the distributions of our measures and determine if they were suitable for the proposed analyses. Table 1 presents descriptive statistics for the exposure and expectation measures. As shown, the video was the most popular strategy, followed by brochures and counseling. These analyses also suggested that all measures had sufficient variance for conducting analyses.
Table 1.
Descriptive statistics
| M or % | SD | |
|---|---|---|
| Number of brochures | 1.76 | 1.85 |
| Read brochures | 62% | - |
| Accepted video | 84% | - |
| Accepted counseling | 52% | - |
| Expected threat to attitudes/behavior posed by video | 1.48 | 0.75 |
| Expected threat to attitudes/behavior posed by counseling | 1.40 | .643 |
| Expected video usefulness | 2.48 | 1.07 |
| Expected counseling usefulness | 2.36 | 1.11 |
| Expected fear posed by video | 1.99 | 0.95 |
| Expected fear posed by counseling | 1.81 | 0.91 |
-: Not applicable. All expectations were measured on the following scale: 1 = not at all, 2 = a little, 3 = quite a bit, and 4 = a lot
Test of Hypotheses
Associations among Exposure Measures
We first analyzed exposure to the brochures, the video, and the counseling to test associations between earlier and later exposure using chi-square tests. Findings revealed that exposure to the brochure correlated positively with exposure to the video, χ2 (1) = 14.98, p < .001, OR = 3, and exposure to the video correlated positively with exposure to the counseling, χ2(1) = 15.88, p < .001, OR = 3.22. Both of these effects were statistically significant and large in size. Exposure to the video was respectively 90 and 75% with and without prior exposure to the brochures. Likewise, exposure to the counseling was respectively 57 and 29% with and without prior exposure to the video. In contrast, exposure to the brochures had no significant association with exposure to the counseling, χ2 (1) = 0.01, ns. Exposure to the counseling was respectively 52 and 48% with and without prior exposure to the brochures.
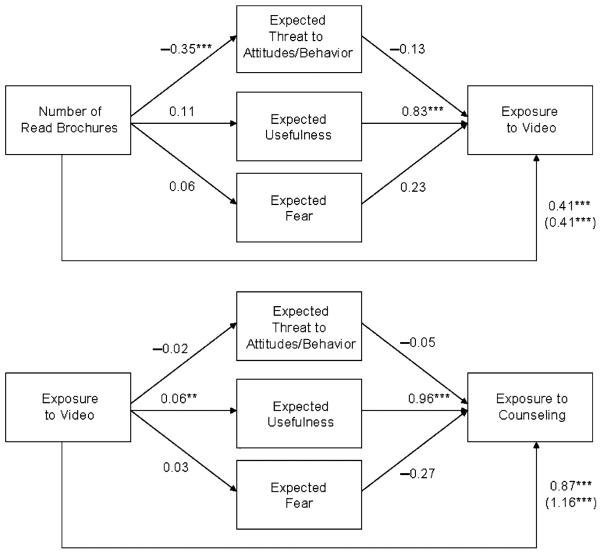
Mediation Analyses
We also conducted mediation analyses to examine whether the associations of exposure to the brochures and the video and of exposure to the video and the counseling were mediated by expectations of usefulness, threat to recipients attitudes/behavior, and fear. As described by Baron and Kenny (1986), mediation is likely to take place if exposure to the brochure or video is associated with a given set of expectations (first regressions), exposure to the brochure or video is associated with exposure to the video or counseling (second regression), and if expectations are associated with exposure to the video or counseling even when controlling for exposure to brochure/video (third regression). In addition, the association between exposure to the brochure or video and exposure to the video or counseling must be weaker when the expectation measures are included in the equation.
The relevant mediational models appear in Fig. 1. As shown, the conditions for mediation were met only for expectations of usefulness in the model predicting exposure to the counseling. Consistent with the possibility of mediation, inclusion of expected usefulness reduced the direct effect of exposure to the video on exposure to the counseling from B = 1.16 (Wald Test = 14.82, p < .001) to B = 0.87 (Wald Test = 6.98, p < .001). Thus, this finding suggested that exposure to the video increased exposure to the counseling by making the counseling appeared more useful to participants.
Fig. 1.
Mediation analyses. Numbers next to each path are regression coefficients. Parenthetical numbers represent direct effects (rs) when potential mediators were not included. **: p < .01, ***: p < .001
Discussion
Our study revealed a cascading effect by which exposure to simple, inexpensive HIV-prevention messages is a gateway to subsequent programs. In particular, our findings suggest that ensuring exposure to HIV-prevention brochures increases exposure to HIV-prevention videos, which in turn increases exposure to one-on-one HIV-prevention counseling. Hence, when the clients of a particular health facility are at high risk for HIV, placing HIV-prevention brochures where clients will notice them may increase exposure to available HIV-prevention videos. Moreover, HIV-prevention videos, which were highly sought by our sample (see Table 1), may improve exposure to one-on-one HIV-prevention counseling, and potentially, HIV testing.
In addition to establishing associations among exposure to HIV-prevention brochures, videos, and counseling, our study examined the cognitive mediators of these associations (see Figure 3). In this regard, there was no support for the hypothesis that the video increased exposure to the counseling by decreasing the threat to recipients' attitudes and behaviors expected for HIV-prevention programs. Instead, the link between exposure to the video and the counseling was mediated by expectations that the counseling would be useful (see Fig. 1). Apparently, mere exposure to an HIV-prevention video increased judgments of the usefulness of HIV-prevention counseling, perhaps independently of the content of the video.
Furthermore, the mediation analyses provided no support for fear of HIV as a potential mediator of the association between video and counseling exposure. This finding is important for two reasons. First, it is unlikely that the video persuaded people that HIV was a personal concern, leading to greater exposure to subsequent programs for that reason. Hence, mere exposure remains the most plausible explanation for our findings. Second, past research has demonstrated that the use of fear is not an efficacious tool for decreasing HIV risk behavior (Albarracín et al. 2005; Earl and Albarracín 2007). Similarly, in the context of enrollment in programs, altering an audience's fear level may not increase people's participation.
Interestingly, we could not find a significant mediator for the association between exposure to the brochures and exposure to the video. It would be plausible to attribute this lack of significant mediation to the overwhelming acceptance of exposure to the video by 84% of our participants. Given this aspect, future research in which the videos are less sought out may provide a better test for mediational mechanisms of exposure to the video. Nonetheless, several correlations with exposure to the video were significant, suggesting that ceiling effects are less likely to be involved.
Another explanation for the lack of mediation of the link between exposure to the brochures and the video concerns how the materials were offered. Whereas the brochures were simply placed on a table next to the participant, the video was explicitly offered by the interviewer. Thus, accepting or declining the video implied a public commitment that could have made expectations more salient and predictive of future exposure (Deutsch and Gerard 1955; Schlenker 1980). In contrast, if exposure to the brochures did not make expectations salient, its effects on exposure to the video might have been more automatic. From this perspective, the effects on the video may not be detectable unless researchers use more implicit measures of attitudes toward or expectations about the video (for a review, see Krosnick et al. 2005). Future research should investigate mediation by these types of cognitions.
Furthermore, it is important to note that exposure to the brochures and videos were quasi-experimental factors. On the one hand, the lack of a significant correlation between exposure to the brochures and the counseling speaks against the possibility of a third variable underlying exposure in general. On the other hand, future work should experimentally assign participants to viewing HIV-prevention brochures or videos and then measure effects on subsequent acceptance. Moreover, it would be important to systematically alter the order in which HIV-prevention brochures, videos, and counseling are offered to clients. Such research may identify the most effective ways of gaining acceptance when HIV-prevention programs are launched in the real world.
An important question for future research is to investigate the effect of past risky behavior on exposure to HIV prevention programs. To maintain confidentiality, data regarding sexual behavior are usually obtained by self-report. However, various factors influence the accuracy of self-reports, such as the length of the time interval or the social context of the evaluation (Schroeder et al. 2003), as well as the order in which participants answer questions (Schwarz et al. 1998). Although past research suggests that self-reports are reliable sources of information on issues such as STI infections, or use of drugs, alcohol or tobacco (Upchurch and Mason 2002; Bauman et al. 1982), future studies might include objective behavioral measures and follow up of the participants. Tracking new STI infections and using frequent HIV tests may be ways in which the influence of behavior to effectively investigate the effects of behavior on exposure to preventive programs.
A limitation of this research was our retrospective questionnaire to measure the clients' expectations about the video and counseling. Even when these retrospective responses could be influenced by rationalizations, the use of a retrospective questionnaire permitted a relatively unbiased observation of exposure to the different aspects of the program. Future work in this area, however, may be conducted by counterbalancing the order of these measures to observe if these cognitions were salient when participants were making decisions about the program.
Issues of sampling are also relevant when considering the applicability of our findings to other populations. Clearly, the need for increasing participation seems key to our low-income, high-risk community sample, but may be less pronounced in groups that are de facto exposed to HIV-prevention programs. For example, prison inmates and students in academic settings may have less opportunity to select out of programs, even when selective attention to the programs is likely to remain a critical factor. Moreover, the need to observe participation in the context of a research study necessarily imposed some selection to our study sample. Future work may be conducted in waiting rooms without the observed individuals being recruited into a study.
In closing, an impressive number of studies have demonstrated the efficacy of interventions to persuade and train people to use condoms (see Cottler et al. 1998; Fogarty et al. 2001; Healton and Messeri 1993; Kalichman et al. 1996; Kegeles et al. 1996; Kelly et al. 1991, 1992, 1997; Lauby et al. 2000; MacLachlan et al. 1997; McCusker et al. 1996; National Institute of Mental Health [NIMH] Multisite HIV Prevention Trial Group, 1998; O'Leary et al. 1998; Rotheram-Borus et al. 2001; CDC AIDS Community Demonstration Projects Research Group, 1999). However, these studies have never considered the actual reach of these interventions. In this context, identifying ways of using simple tools to increase exposure to HIV-prevention programs should advance the technology available to curb infections with HIV.
Footnotes
This study included four different conditions consisting of scripted introductions to the program. These results have been reported in another paper.
References
- AIDS Risk Reduction Project . Just like me: Talking about AIDS (Videotape) University of Connecticut; Storrs, CT: 1997. [Google Scholar]
- Albarracín D, Gillette J, Earl A, Glasman LR, Durantini MR, Ho MH. A test of major assumptions about behavior change: A comprehensive look at HIV prevention interventions since the beginning of the epidemic. Psychological Bulletin. 2005;131:856–897. doi: 10.1037/0033-2909.131.6.856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albarracín D, McNatt PS, Klein C, Ho R, Mitchell A, Kumkale GT. Persuasive communications to change actions: An analysis of behavioral and cognitive impact in HIV prevention. Health Psychology. 2003;22:166–17. doi: 10.1037//0278-6133.22.2.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albarracín D, Mitchell AL. The role of defensive confidence in preference for proatttitudinal information: How believing that one is strong can be a weakness. Personality and Social Psychology Bulletin. 2004;30:1565–1584. doi: 10.1177/0146167204271180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bauman KE, Koch GG, Bryan ES. Validity of self-reports of adolescent cigarette smoking. International Journal of the Addictions. 1982;17:1131–1136. doi: 10.3109/10826088209056345. [DOI] [PubMed] [Google Scholar]
- Breckler SJ. Empirical validation of affect, behavior, and cognition as distinct components of attitude. Journal of Personality and Social Psychology. 1984;47:1191–1205. doi: 10.1037//0022-3514.47.6.1191. [DOI] [PubMed] [Google Scholar]
- Brehm JW. A theory of psychological reactance. Academic Press; New York: 1966. [Google Scholar]
- Catania JA, Gibson DR, Chitwood DD, Coates TJ. Methodological problems in AIDS behavioral research: Influences on measurement error and participation bias in studies of sexual behavior. Psychological Bulletin. 1990;108:339–362. doi: 10.1037/0033-2909.108.3.339. [DOI] [PubMed] [Google Scholar]
- CDC AIDS Community Demonstration Projects Research Group Community-level HIV intervention in 5 cities: Final outcome data from the CDC AIDS Community Demonstration Projects. American Journal of Public Health. 1999;89:1–10. doi: 10.2105/ajph.89.3.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control Cases of HIV infection and AIDS in the United States and Dependent Areas, 2005. HIV/AIDS Surveillance Report. 2005;17:1–54. [Google Scholar]
- Centers for Disease Control . Project RESPECT: Preliminary outcome study. Project RESPECT Group; Atlanta, GA: 1997. [Google Scholar]
- Cottler LB, Compton WM, Ben Abdallah A, Cunningham-Williams R, Abram F, Fichtenbaum C, Dotson W. Peer-delivered interventions reduce HIV risk behaviors among out-of-treatment drug abusers. Public Health Reports. 1998;113:31–41. [PMC free article] [PubMed] [Google Scholar]
- Deutsch M, Gerard HG. A study of normative and informational social influences upon individual judgment. Journal of Abnormal and Social Psychology. 1955;51:629–636. doi: 10.1037/h0046408. [DOI] [PubMed] [Google Scholar]
- DiFrancesco W, Kelly JA, Sikkema KJ, Somlai AM, Murphy DA, Stevenson LY. Differences between completers and early dropouts from two HIV intervention trials: A health belief approach to understanding prevention program attrition. American Journal of Public Health. 1998;88:1068–1073. doi: 10.2105/ajph.88.7.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillard J, Hunter J, Burgoon M. Sequential-request persuasive strategies: Meta-analysis of foot-in-the-door and door-in-the-face. Human Communication Research. 1984;10:461–488. [Google Scholar]
- Earl A, Albarracín D. Nature, decay, and spiraling of the effects of fear-inducing arguments and HIV counseling and testing: A meta-analysis of the short- and long-term outcomes of HIV-prevention interventions. Health Psychology. 2007;26:496–506. doi: 10.1037/0278-6133.26.4.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehrhardt AA, Exner TM, Hoffman S, Silberman I, Lew CS, Miller S, Levin B. A gender-specific HIV/STD risk reduction intervention for women in a health care setting: Short-and long-term results of a randomized clinical trial. AIDS Care. 2002;14:147–161. doi: 10.1080/09540120220104677. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA. Changing AIDS risk behavior. Psychological Bulletin. 1992;111:455–474. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA. Theoretical approaches to individual-level change in HIV risk behavior. In: Peterson JL, DiClemente RJ, editors. Handbook of HIV Prevention: AIDS Prevention and Mental Health. Kluwer Academic Publishers; New York, NY: 2000. pp. 3–55. [Google Scholar]
- Fogarty LA, Heiling C, Armstrong K, Cabral R, Galavotti C, Gielen AC, Green BM. Long term effectiveness of a peer-based intervention promoting condom and contraceptive use among HIV-positive and at-risk women. Public Health Reports. 2001;116:103–119. doi: 10.1093/phr/116.S1.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman JL, Fraser SC. Compliance without pressure: The foot-in-the-door technique. Journal of Personality and Social Psychology. 1966;4:195–202. doi: 10.1037/h0023552. [DOI] [PubMed] [Google Scholar]
- Girandola F. Sequential requests and organ donation. Journal of Social Psychology. 2002;142:171–178. doi: 10.1080/00224540209603893. [DOI] [PubMed] [Google Scholar]
- Gueguen N. Foot-in-the-door technique and computer-mediated communication. Computers in Human Behavior. 2002;18:11–15. [Google Scholar]
- Healton CG, Messeri P. The effect of video interventions on improving knowledge and treatment compliance in the sexually transmitted disease clinic setting: Lesson for HIV health education. Sexually Transmitted Disease. 1993;20:70–76. doi: 10.1097/00007435-199303000-00003. [DOI] [PubMed] [Google Scholar]
- Hennessy M, Mercier M, Williams SP, Arno JN. Client preferences for STD/HIV prevention programs. Evaluation and Program Planning. 2002;25:117–124. [Google Scholar]
- Kalichman SC, Carey MP, Johnson BT. Prevention of sexually transmitted HIV infection: A meta-analytic review of the behavioral outcome literature. Annals of Behavioral Medicine. 1996;18:6–15. doi: 10.1007/BF02903934. [DOI] [PubMed] [Google Scholar]
- Kegeles SM, Hays RB, Coates TJ. The Mpowerment Project: A community-level HIV Prevention Intervention for Young Gay Men. American Journal of Public Health. 1996;86:1129–1136. doi: 10.2105/ajph.86.8_pt_1.1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JA, Murphy DA, Sikkema KJ, McAuliffe TL, Roffman RA, Solomon LJ, et al. Randomised, controlled, community level HIV-prevention intervention for sexual-risk behavior among homosexual men in US cities. Lancet. 1997;350:1500–1505. doi: 10.1016/s0140-6736(97)07439-4. [DOI] [PubMed] [Google Scholar]
- Kelly JA, St., Lawrence JS, Diaz YE, Stevenson LY, Hauth AC, Brasfield TL, et al. HIV risk behavior reduction following intervention with key opinion leaders of population: An experimental analysis. American Journal of Public Health. 1991;81:168–171. doi: 10.2105/ajph.81.2.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JA, St., Lawrence JS, Stevenson LY, Hauth AC, Kalichman SC, Diaz YE, et al. Community AIDS/HIV risk reduction: The effects of endorsements by popular people in three cities. American Journal of Public Health. 1992;82:1483–1489. doi: 10.2105/ajph.82.11.1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krosnick JA, Judd CM, Wittenbrink B. The measurement of attitudes. In: Albarracín D, Johnson BT, Zanna MP, editors. The handbook of attitudes. Erlbaum Associates; Mahwah, NJ: 2005. pp. 21–76. [Google Scholar]
- Lauby J, Kotranski L, Feighan K, Collier K, Semaan S, Halbert J. Effects of intervention attrition and research attrition on the evaluation of an HIV prevention program. Journal of Drug Issues. 1996;26:1–16. [Google Scholar]
- Lauby JL, Smith PJ, Stark M, Person B, Adams J. A community-level HIV prevention intervention for inner-city women: Results of the Women and Infants Demonstration Projects. American Journal of Public Health. 2000;90:216–222. doi: 10.2105/ajph.90.2.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacLachlan M, Chimombo M, Mpeba N. AIDS education for youth through active learning: A school-based approach from Malawi. International Journal of Educational Development. 1997;17:41–50. [Google Scholar]
- McCusker J, Stoddard AM, Hindin RN, Garfield FB, Frost R. Changes in HIV risk behavior following alternative residential programs of drug abuse treatment and AIDS education. Annals of Epidemiology. 1996;6:119–125. doi: 10.1016/1047-2797(95)00128-x. [DOI] [PubMed] [Google Scholar]
- McGuire WJ. Inducing resistance to persuasion: Some contemporary approaches. In: Berkowitz L, editor. Advances in experimental social psychology. Vol. 1. Academic Press; New York: 1964. pp. 191–229. [Google Scholar]
- National Institute of Mental Health Multisite HIV Prevention Trial Group The NIMH Multisite HIV prevention trial: Reducing HIV sexual risk behavior. Science. 1998;280:1889–1894. doi: 10.1126/science.280.5371.1889. [DOI] [PubMed] [Google Scholar]
- Noguchi K, Albarracín D, Durantini MR, Glasman LR. Who is exposed to health promotion programs and when? A meta-analysis of motivations underlying participation in HIV prevention interventions. Psychological Bulletin. doi: 10.1037/0033-2909.133.6.955. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Leary A, Ambrose TK, Raffaelli M, Mailbach E, Jemmott LS, Jemmott JB, III, et al. Effects of an HIV risk reduction project on sexual risk behavior of low-income STD patients. AIDS Education and Prevention. 1998;10:483–492. [PubMed] [Google Scholar]
- Rabinowitz DC. Predictors of attrition in a predominantly Caucasian middle-class clinic-based weight loss program. Dissertation Abstracts International, Section B. 2002;62:5796. [Google Scholar]
- Raj A, Amaro H, Cranston K, Martin B, Cabral H, Navarro A, Conron K. Is a general women's health promotion program as effective as an HIV-intensive prevention program in reducing HIV risk among Hispanic women? Public Health Reports. 2001;116:599–607. doi: 10.1093/phr/116.6.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers RW. A protection motivation theory of fear appeals and attitude change. Journal of Psychology. 1975;91(5):93–114. doi: 10.1080/00223980.1975.9915803. [DOI] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Lee MB, Murphy DA, Futterman D, Duan N, Birnbaum JM, et al. Efficacy of a preventive intervention for youth living with HIV. American Journal of Public Health. 2001;91:400–405. doi: 10.2105/ajph.91.3.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlenker BR. Impression management: The self-concept, social identity, and interpersonal relations. Brooks/Cole; Monterey, CA: 1980. [Google Scholar]
- Schlenker B, Dlugolecki DW, Doherty K. The impact of self-presentations, on self-appraisal and behavior: The power of public commitment. Personality and Social Psychology Bulletin. 1994;20:20–33. [Google Scholar]
- Schroder KEE, Carey MP, Vanable PA. Methodological challenges in research on sexual risk behavior: II. Accuracy of self-reports. Annals of Behavioral Medicine. 2003;26:104–123. doi: 10.1207/s15324796abm2602_03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarz N, Groves RM, Schuman H. Survey methods. In: Gilbert DT, Fiske ST, Lindzey G, editors. The handbook of social psychology. 4th edition Vol. 1. Boston, Massachusetts; McGraw-Hill: 1998. pp. 143–179. [Google Scholar]
- Taylor T, Booth-Butterfield S. Getting a foot-in-the-door with drinking and driving: A field study of healthy influence. Communication Research Reports. 1993;10:95–101. [Google Scholar]
- Tobias C, Drainoni M, Wood S. An analysis of HRSA-funded services for HIV-positive substance users: A study of Ryan White CARE Act Title III, Title IV, and SPNS providers. AIDS Patient Care STDs. 2006;18:604–613. doi: 10.1089/apc.2004.18.604. [DOI] [PubMed] [Google Scholar]
- Upchurch DM, Mason WM. Validity of self-reports of incidents of sexually transmitted diseases. Paper presented at the Annual Meeting of the Population Association of America; Atlanta, GA. May, 2002. [Google Scholar]
- Veach LJ, Ramley TP, Kippers SM, Sorg JD. Retention predictors related to intensive outpatients programs for substance use disorders. American Journal of Drug and Alcohol Abuse. 2000;26:417–428. doi: 10.1081/ada-100100253. [DOI] [PubMed] [Google Scholar]
- Webb EJ, Campbell DT, Schwartz RD, Sechrest LB. Unobtrusive measures: Nonreactive research in the social sciences. Rand McNally; Chicago: 1966. [Google Scholar]
- Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annual Review of Public Health. 2006;27:1–28. doi: 10.1146/annurev.publhealth.27.021405.102113. [DOI] [PubMed] [Google Scholar]
- Zajonc RB. Attitudinal effects of mere exposure. Journal of Personality and Social Psychology, Monograph Supplement. 1968;9:1–27. [Google Scholar]