Abstract
HIV-prevention intervention effectiveness depends on understanding whether clients with highest need for HIV-prevention counseling accept it. With this objective, a field study with a high-risk community sample from the southeastern United States (N = 350) investigated whether initial knowledge about HIV, motivation to use condoms, condom-use-relevant behavioral skills, and prior condom use correlate with subsequent acceptance of an HIV-prevention counseling session. Ironically, participants with high (vs. low) motivation to use condoms, high (vs. low) condom-use-relevant behavioral skills, and high (vs. low) prior condom use were more likely to accept the HIV-prevention counseling. Moreover, the influence of motivation to use condoms, condom-use-relevant behavioral skills, and prior condom use on acceptance of the counseling was mediated by expectations that the counseling session would be useful. Methods to reduce barriers to recruitment of clients for counseling programs are discussed.
Keywords: counseling acceptance, selective exposure, intervention, HIV, condom use
HIV-prevention counseling sessions are often designed to reduce the spread of HIV by increasing knowledge about HIV, motivation to use condoms, condom-use-relevant behavioral skills, and condom use (Albarracín et al., 2003, 2005). One primary assumption of this work is that the people who most need the programs (i.e., those who are not currently using condoms or who do not have the knowledge, motivation, or skills to initiate condom use) will accept HIV-prevention counseling when it is offered. Unfortunately, however, individuals who are already engaging in protective behaviors may accept counseling to a greater extent than those who are not already engaging in protective behaviors. For instance, recent meta-analytic data suggest that participants with consistent condom use are more likely to accept HIV-prevention counseling than those with less consistent condom use (Noguchi, Albarracín, Durantini, & Glasman, 2007). This situation is troubling because preventive efforts must reach people who are not currently engaging in HIV-protective behaviors. As a result, understanding who accepts HIV-prevention counseling is critical to understanding how to maximize intervention effectiveness.
A related question concerns why people may be more or less likely to accept counseling. For instance, prior to accepting an HIV-prevention counseling session, participants may develop expectations about what acceptance of the counseling will entail (Ajzen & Fishbein, 1980, 2005; Fishbein & Ajzen, 1975). These expectations are likely antecedents of the decision of whether to accept the counseling session (Ajzen & Fishbein, 1980, 2005; Fishbein & Ajzen, 1975; Zillmann, Chen, Knobloch, & Callison, 2004). Participants may think that the program will be successful at increasing condom use (“expected usefulness” Albarracín, Durantini, Earl, Gunnoe, & Leeper, 2008; Albarracín, Leeper, Earl, & Durantini, 2008). However, participants may also expect that the counseling program will try to change attitudes or behaviors they refuse to change (“expected threat” Albarracín, Durantini, et al., 2008; Albarracín, Leeper, et al., 2008; Albarracín & Mitchell, 2004). Acceptance is likely to be higher when participants expect the program to be useful but lower when participants feel that it will threaten their current practices. However, neither of these possibilities has been examined in relation to people’s HIV-relevant knowledge, motivation, behavioral skills, or prior condom use.
Clearly, it is necessary to understand the potential disconnect between those who need HIV-prevention counseling and those who actually receive this counseling and how expectations about the content of the counseling session may contribute to this situation. With this objective, we observed whether participants accepted an invitation to partake in HIV-prevention counseling when a session was offered to them in a health setting. In combination with the use of questionnaire measures, this observation allowed us to examine whether HIV-relevant knowledge, motivation to use condoms, condom-use-relevant behavioral skills, and prior condom use correlate with acceptance of HIV-prevention counseling. Furthermore, we examined whether participants’ expectations about the content of the counseling were intervening factors in the relations of HIV-relevant knowledge, motivation, behavioral skills, and prior condom use with acceptance of the counseling.
Predictors of Acceptance of HIV-Prevention Counseling
The decision of whether to accept HIV-prevention counseling is likely based on psychological factors, such as attitudes and beliefs (Albarracín et al., 2005; Durantini, Albarracín, Mitchell, Earl, & Gillette, 2006; Earl & Albarracín, 2007; Noguchi et al., 2007). When confronted with a counseling session designed to promote behavior change, prior knowledge, motivation, behavioral skills, and actual behavior are likely to influence acceptance of the program (Ajzen & Fishbein, 1980, 2005; Bandura, 1997; Fishbein & Ajzen, 1975; Fisher & Fisher, 1992, 2000; Noguchi et al., 2007). In the case of HIV-prevention counseling, knowledge about HIV, motivation to use condoms (including attitudes, beliefs, intentions, and norms), condom-use-relevant behavioral skills (including perceived behavioral control and negotiation skills), and prior condom use are likely to predict counseling acceptance.
Past research has linked knowledge, motivation, behavioral skills, and prior behavior to acceptance of information in multiple domains. In the political domain, Nixon voters with more knowledge about the U.S. Senate Watergate hearings were more likely to attend to new information about the hearings than were voters with less knowledge about the hearings (Sweeney & Gruber, 1984). In the domain of health and body image, women with lower appearance anxiety were more likely to view media that sexually objectifies women than women with higher appearance anxiety (Aubrey, 2006). In the area of alcohol drinking, heavy alcohol drinkers tend to watch more advertisements for alcohol than do light drinkers and nondrinkers (Perrissol, Boscher, Cerclé, & Somat, 2005). Similar to these past findings, acceptance of HIV-prevention counseling may depend on HIV-relevant psychological factors, such as knowledge about HIV, motivation to use condoms, condom-use-relevant behavioral skills, and prior condom use.
The question concerning the associations linking counseling acceptance with knowledge, motivation, behavioral skills, and prior behavior is an empirical one. These associations may depend, in part, on how these factors influence specific expectations about the content of the counseling session (Ajzen & Fishbein, 1980, 2005; Fishbein & Ajzen, 1975; Zillmann et al., 2004). Expectations that a counseling program is useful and nonthreatening may be associated with increased acceptance, whereas expectations that a counseling program is useless and threatening may be associated with decreased acceptance. Yet, participants may be more likely to view information, even if it contradicts their current practices, if they feel that the information is useful for them (i.e., the information has high expected usefulness; Canon, 1964; Edeani, 1979; Festinger, 1957; Freedman & Sears, 1965; Innes, 1978). In the case of HIV prevention, individuals may be more likely to accept counseling when they expect that the session will be useful, personally relevant, or conducive to condom use than when participants do not have these expectations (i.e., high expected usefulness of the counseling session to increase condom use; Albarracín, Durantini, et al., 2008; Albarracín, Leeper, et al., 2008; Noguchi et al., 2007).
In contrast, threats to past attitudes and behaviors may play important roles. According to reactance theory, acceptance of information is unlikely when people feel that the information threatens their freedom to do what they want (Brehm, 1966, 1972; Silvia, 2006). As a result, participants may be less likely to view information if they feel that the information will force them to change their attitudes or behaviors when they do not want to (i.e., the information has high expected threat; Brehm, 1972; Hart et al., 2008; McFarland & Warren, 1992; Noguchi et al., 2007). In the case of HIV prevention, people who expect that the counseling will not force a point of view, or that they can successfully defend cherished attitudes and practices, may accept the counseling more than those for whom the counseling overtly threatens these attitudes and practices (i.e., low expected threat of the counseling session to participants’ current attitudes or behavior; Albarracín, Durantini, et al., 2008; Albarracín, Leeper, et al., 2008; Albarracín & Mitchell, 2004; Noguchi et al, 2007).
There is past evidence and theorizing in support of an association between HIV-relevant knowledge and expectations about, and subsequent acceptance of, HIV-prevention counseling. In particular, people with high knowledge about HIV may want to confirm or increase their knowledge, resulting in greater acceptance of HIV-prevention counseling (Knobloch-Westerwick, Dillman Carpentier, Blumhoff, & Nickel, 2005). Another possibility is that participants with high knowledge about HIV may have learned about HIV through previous participation in HIV-prevention counseling. Meta-analytic data suggest that participation in HIV-prevention counseling can successfully increase knowledge about HIV both immediately and longitudinally (Albarracín et al., 2003, 2005; Earl & Albarracín, 2007). As a result of past involvement in counseling, high-knowledge individuals, in comparison with low-knowledge individuals, may feel that counseling programs will be more useful for them. This increase in perceived usefulness may subsequently enhance acceptance of HIV-prevention counseling (Albarracín, Durantini, et al., 2008; Albarracín, Leeper, et al., 2008; Knobloch-Westerwick et al., 2005).
The motivation to use condoms is also likely associated with expectations and counseling acceptance. As predicted for knowledge, people who are favorably motivated to use condoms may be more likely to view a counseling session as more useful than people who are not motivated to use condoms. That is, compared with unmotivated people, highly motivated people already see value in condom use and other HIV-prevention practices and should therefore perceive an HIV-prevention counseling session as more useful and consider participation worthwhile (Albarracín, Durantini, et al., 2008; Albarracín, Leeper, et al., 2008; Noguchi et al., 2007). Correspondingly, people with low motivation to use condoms may view the counseling session as less useful and, as a result, may be less willing to accept it. In addition to expectations of usefulness, expectations of the counseling as a personal threat could yield similar associations. For instance, people with low motivation to use condoms may expect that the counseling will challenge their beliefs and force new practices to a greater extent than people with high motivation to use condoms (Lundgren & Prislin, 1998; McFarland & Warren, 1992; Sweeney & Gruber, 1984). In this case, participants with low motivation to use condoms may be less likely to accept an HIV-prevention counseling session than participants with high motivation to use condoms (Albarracín, Durantini, et al., 2008; Noguchi et al., 2007).
Similarly to those participants high in motivation to use condoms, participants high in condom-use-relevant behavioral skills may also accept the HIV-prevention counseling session on the basis of perceived utility. People with high behavioral skills may be more likely to accept HIV-prevention counseling if they feel that the counseling could reinforce their current skills (Baum, 1994; Canon, 1964; Festinger, 1957; Freedman & Sears, 1965; Innes, 1978; Knobloch-Westerwick et al., 2005). In contrast, participants with low behavioral skills may feel that the HIV-prevention counseling session will force them to practice skills they do not want to practice (Albarracín, Durantini, et al., 2008; Albarracín, Leeper, et al., 2008). Therefore, participants with low behavioral skills may not accept the counseling if they feel unable or unprepared to use condoms or practice their skills (Albarracín, Durantini, et al., 2008; Albarracín, Leeper, et al., 2008; Albarracín & Mitchell, 2004).
Finally, prior condom use may influence the decision of whether to accept an HIV-prevention counseling session. For instance, participants with high condom use may feel that accepting an HIV-prevention counseling session may be an opportunity to reinforce their current behaviors. In this case, accepting an HIV-prevention counseling session may be perceived as more useful for those who are currently using condoms than for those who are not currently using condoms (Albarracín, Leeper, et al., 2008). In contrast, participants with low prior condom use may feel that accepting HIV-prevention counseling would challenge their current practices (Albarracín & Mitchell, 2004). As such, participants with low prior condom use may be less likely to accept HIV-prevention counseling than participants with high prior condom use.
The Present Study
Acceptance of prevention programs is a critical first step to changing behavior. With this in mind, the present study examined factors relevant to the decision of whether to accept an HIV-prevention counseling session. Specifically, we examined whether HIV-relevant knowledge, motivation to use condoms, condom use-relevant behavioral skills, or prior condom use predicted acceptance of an HIV-prevention counseling session. In addition, we examined whether HIV-relevant knowledge, motivation to use condoms, condom-use-relevant behavioral skills, and prior condom use influenced expectations about the content of the counseling session. These expectations are likely to be the immediate precursors of the decision of whether to accept the counseling. As such, we tested whether two indexes of expectations (expected usefulness and expected threat) mediated the hypothesized relations of (a) HIV-relevant knowledge, motivation to use condoms, condom-use-relevant behavioral skills, and prior condom use with (b) acceptance of the counseling session. Finally, to check generalizbility of our findings, we examined whether other characteristics of the participants (e.g., demographic variables, past participation in HIV or sexually transmitted infection [STI] counseling and testing, and number of sexual partners) moderated the associations between counseling acceptance and our variables of interest (i.e., HIV-relevant knowledge, motivation, behavioral skills, and prior condom use).
Method
Overview and Design
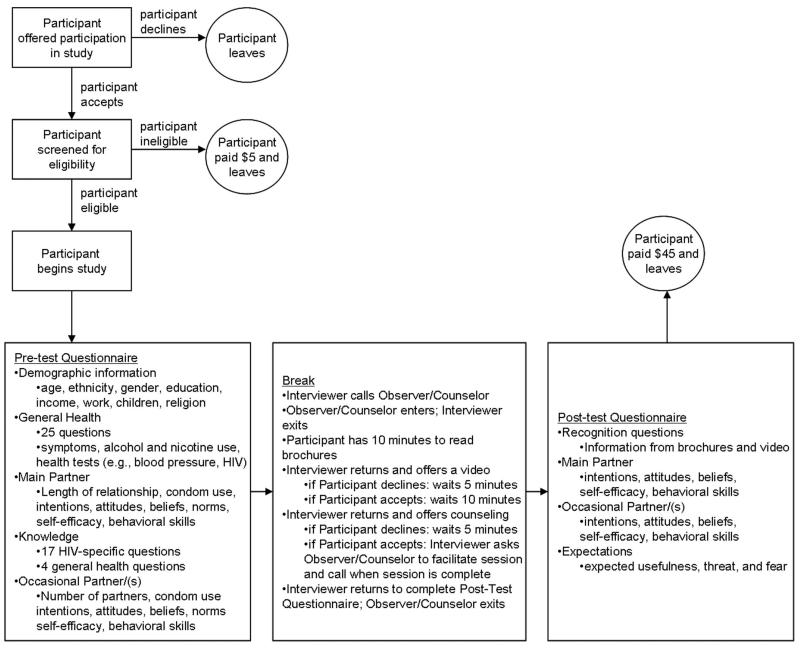
Participants were 350 community members recruited through flyers or direct referrals from community members. Reference was made to what was described as a “health survey,” and prospective participants who called were asked various questions about health, including questions pertaining to sexual activity. Only participants who were sexually active in the prior 6 months and not currently pregnant were considered eligible and scheduled to come in for an interview at a subsequent time. At the time of this interview, after signing the informed consent, the participant responded to a questionnaire administered by a member of the research team (see Figure 1 for an overview of study protocol). Critical to this study, halfway through the interview, the interviewer interrupted the administration, announcing a 30-min break. At that point, an observer/counselor entered the room, pretending to do work unrelated to the interview and unobtrusively recorded whether the participant accepted the offer of a brief HIV-prevention counseling session. Following this ostensible break, the interviewer returned and administered measures of expectations about the content of the counseling session. On completion of the interview, participants were fully and carefully debriefed in a discussion of the purpose of the investigation as a study of condom use and counseling acceptance, which included an explanation of the role of the observer/counselor.
Figure 1.
Flow chart of study events.
Participants
Participants were 350 community members (260 women and 90 men), who were paid $5 for the eligibility screening and $40 for participation in the main study if eligible. Ineligible participants were paid $5, and completers were paid a total of $45. Table 1 contains a description of the sample.
Table 1. Descriptive Statistics.
| Variable | Value |
|---|---|
| Demographic variables | |
| Women | 74% |
| Age in years | 32.12 (9.75) |
| Ethnic descent | |
| African American | 65% |
| European American | 28% |
| Latino/Latina American | 3% |
| American Indian/Alaska Native | 2% |
| Asian American | 1% |
| Other | 1% |
| Income | |
| $0–9,999 | 61% |
| $10,000–19,999 | 23% |
| $20,000–29,999 | 11% |
| $30,000–39,999 | 2% |
| $40,000–49,999 | 1% |
| $50,000–59,999 | 1% |
| $60,000 or above | 1% |
| Hours per week worked outside of the home | 17.32 (20.12) |
| Number of children | 1.81 (1.68) |
| Religious preference | |
| Christian, non-Catholic | 56% |
| Other | 32% |
| Catholic | 7% |
| Nonbeliever | 3% |
| Jew | 1% |
| Muslim | 1% |
| Substance use | |
| Smoke tobacco | 55% |
| Number of cigarettes smoked per day | 6.23 (8.17) |
| Drink alcohol | 51% |
| Number of alcoholic beverages drunk per week | 3.54 (8.06) |
| Have a main partner | 87% |
| Duration of relationship in months | 55.55 (59.23) |
| Had an STI in the past year | 13% |
| Had an HIV test | 91% |
| Today | 1% |
| Within a week | 2% |
| Within a month | 10% |
| Within three months | 13% |
| Within six months | 14% |
| Within a year | 18% |
| Over a year ago | 33% |
| Never | 9% |
| Accept HIV-prevention counseling | 28% |
|
| |
| Measures of HIV-relevant knowledge, motivation, behavioral skills, and prior condom use | |
| Knowledge (range = 0–100%) | 77.08% (0.15) |
| Motivation index | |
| Attitudes (range = 1–7) | 5.25 (1.31) |
| Beliefs (range = 1–5) | 3.63 (0.53) |
| Intentions (range = 1–7) | 5.12(1.55) |
| Norms (range = 1–5) | 2.95 (1.18) |
| Behavioral skills index | |
| Self-efficacy (range = 0–10) | 6.59 (2.31) |
| Negotiation skills (range = 1–5) | 4.22 (1.62) |
| Condom use (range = 0–100%) | 36.09% (0.41) |
| With main partner in last month (range = 0–100%) | 29.32% (0.41) |
| With main partner in last three months (range = 0–100%) | 30.97% (0.41) |
| With main partner in last six months (range = 0–100%) | 30.90% (0.41) |
| With casual/occasional partner in last month (range = 0–100%) | 74.69% (0.39) |
| With casual/occasional partner in last three months (range = 0–100%) | 70.47% (0.41) |
| With casual/occasional partner in last six months (range = 0–100%) | 73.53% (0.37) |
| Measures of expectations about counseling | |
| Expected usefulness | |
| Useful for me (range = 1–4) | 2.33 (1.23) |
| Would make it easier for me to use condoms (range = 1–4) | 2.14(1.19) |
| Necessary for me (range = 1–4) | 2.14(1.23) |
| Expected threat to attitudes/behavior | |
| Would not make me change my point of view (range = 1–4) | 1.88 (1.10) |
| Force me to do things I do not like (range = 1–4) | 1.34(0.74) |
| Would challenge my beliefs (range = 1–4) | 1.57 (1.00) |
Note. Numerical entries are either percentages (designated as such) or means with standard deviations in parentheses. STI = sexually transmitted infection.
Research Team
The staff of the study included an interviewer and an observer/counselor. The interviewer administered the questionnaire. The observer/counselor served as a recorder of the participant’s behavior in relation to the counseling session and also facilitated the HIV-prevention counseling session if the participant accepted.
Procedure
Recruitment
Participants were not actively recruited by the study staff. Instead, they were recruited by viewing a flyer advertising the study, which was placed extensively in the community and the Alachua County Health Department, or through a personal referral from health department staff or members of the community. Both of these recruitment strategies are common practice in public health research (Bender et al., 2007; Stice, Marti, Spoor, Presnell, & Shaw, 2008; Woolsey et al., 1954). To prevent contamination and reduce self-selection, recruiters and flyers described the study as a “general health study” without any mention of study specifics, such as a focus on HIV prevention and condom use, the offer of materials, or the presence of the observer/counselor. Participants were primarily drawn from the health department. Specifically, 42% of participants reported seeing the flyer in the health department, and 27% were recruited directly from health department clinics. An additional 31% were community members who reported not attending the health department regularly for services. Participants called a prespecified phone number to make an appointment, at which time they were screened for eligibility. Participants had to be over 18 years of age and sexually active and could not be pregnant or trying to become pregnant. Participants were also considered ineligible if they mentioned information about the study that was not included on the flyer (e.g., calling for the “sex study” or the “condom study” mentioning anything about the materials or the confederate).
Unobtrusive observation
We used unobtrusive observation to measure acceptance of the counseling. This approach has the advantage of measuring acceptance of counseling without the participant being influenced by knowledge that this was the main measure of the study (Webb, Campbell, Schwartz, & Sechrest, 1966). In addition, unobtrusive observation closely resembles conditions under which referral to a counseling program is normally made (e.g., in a health setting by a health professional to health counseling).1
Interview protocol
An overview of interview protocol is provided in Figure 1. When participants arrived for their interview, they checked in at the front desk of the health department and waited to be seen. When the interviewer was ready, the participant was taken to the interview room where she or he was re-screened for eligibility. If the participant was still eligible, the face-to-face interview began.2 The first part of the interview consisted of general health questions, such as “Do you feel tightness in your chest?” followed by the response alternatives yes and no, and “On average, how many cigarettes do you smoke per day?” The next section of the questionnaire addressed the decisions to use or not use condoms with a main sexual partner and included measures of motivation to use condoms, condom-use-relevant behavioral skills, and prior condom use. Subsequently, participants’ HIV-relevant knowledge was assessed, along with motivation to use condoms, condom-use-relevant behavioral skills, and prior condom use with occasional sexual partners.
After 30 min had elapsed, and while the first part of the interview was being completed, the observer/counselor knocked on the door of the interview room and requested to use the space to conduct some office work. The interviewer responded that he or she was in the middle of the interview but that the observer/counselor would be called in during the break. Subsequently, when the first half of the questionnaire was completed, the interviewer called the observer/counselor and told her or him that the room was available during the study break. The interviewer then excused herself or himself from the interview, indicating that she or he had to enter the participant’s data before finishing the interview.
After the observer/counselor entered the room, the interviewer exited. Later, the interviewer returned and offered the participant the option of accepting an HIV-prevention counseling session by asking the participant “While you are waiting, would you be interested in taking part in an HIV-risk reduction counseling session?”3 If the participant accepted, the observer/counselor was asked to counsel the participant. When the observer/counselor had completed the counseling session, she or he called the interviewer to continue the study. If the participant declined, however, the interviewer exited the room and returned 5 min later to administer the posttest questionnaire. When the interviewer returned, the observer/counselor left and the posttest commenced. Altogether, the interview and counseling took approximately 90–120 minutes to complete. This study was approved by the Institutional Review Boards (IRBs) of the University of Florida (IRB-1) and the State of Florida’s Department of Health. Written informed consent was provided to participate in a study described as examining health behavior, to include answering questions about current health practices, but that did not involve anything not normally done while at the health department. For instance, participants were instructed that they would be asked questions about their current health and health practices and that they may be offered participation in health-promotion programs. In addition, participants were reassured that their confidentiality would be carefully guarded and that participation was entirely voluntary.
Measures of HIV-Relevant Knowledge, Motivation, Behavioral Skills, and Prior Condom Use
The questionnaire measured HIV-relevant knowledge, motivation to use condoms, condom-use-relevant behavioral skills, and prior condom use. It also assessed many demographic and behavioral variables, including education, ethnicity, gender, age, past participation in HIV or STI counseling and testing, and number of sexual partners. All measures of HIV-relevant knowledge, motivation, behavioral skills, and prior condom use were collected before participants had the option of accepting the HIV-prevention counseling.
Knowledge
Knowledge measures tapped information about HIV and condom use with 17 statements that participants evaluated as true or false (e.g., “It is possible to get HIV when a person gets a tattoo” “A natural or lamb skin condom is good at preventing HIV” “Some drugs have been made for curing AIDS” “Using Vaseline or baby oil with condoms lowers the risk of getting HIV” Kamb et al., 1998). Knowledge scores were calculated by summing the number of questions each participant answered correctly (α = .72).
Motivation
Measurement of motivation to use condoms integrated attitudes and beliefs about condom use, intentions to use condoms in the future, and subjective norms about condom use (Ajzen & Fishbein, 1980, 2005; Fishbein & Ajzen, 1975). Measures of motivation included attitudes about condom use (e.g., “If you were to use a condom every time you have vaginal sex with your main partner in the next six months, would it be very unpleasant or very pleasant?” “If you were to use a condom every time you have vaginal sex with your occasional partner(s) in the next six months, would it be very bad or very good?”), beliefs about condom use (e.g., “If you were to use a condom every time you had sex with your main partner, it would protect you from HIV” “If you were to use a condom every time you had sex with your occasional partner(s), it would break the mood [reverse scored]”), normative influence over condom use (e.g., “Does your main partner think that you should or should not use a condom every time you have vaginal sex with him/her?” “Does your mother think that you should or should not use a condom every time you have vaginal sex with your occasional partner(s)?”), and intentions to use condoms (e.g., “How strong are your intentions to use condoms with your main partner in the next six months?”). These measures were adapted from previous studies (Albarracín et al., 2000). Participants reported attitudes using 14 items on a 7-point scale ranging from 1 (negative attitude), for example, “very unpleasant,” “very bad”) to 7 (positive attitude), for example, “very pleasant,” “very good”. Participants responded to 30 beliefs about condom use using a 5-point scale ranging from 1 (strongly disagree) to 5 (strongly agree). Sixteen normative influences were reported on a 5-point scale ranging from 1 (feels strongly I SHOULD NOT use a condom) to 5 (feels strongly I SHOULD use a condom). Four intentions were reported on a 7-point scale ranging from 1 (very weak) to 7 (very strong). All measures were converted to z-scores to create an overall index of motivation to use condoms (α = .86).
Behavioral skills
Condom-use-relevant behavioral skills measures captured perceptions of control over using condoms and condom use negotiation skills (Ajzen & Fishbein, 1980, 2005; Bandura, 1997). Measures of behavioral skills included perceptions of control over condom use (e.g., “How sure are you that you could use a condom every time you have vaginal sex with you main partner when you have been drinking or doing drugs?” “How sure are you that you could use a condom every time you have vaginal sex with your occasional partner(s) when you have to interrupt or delay sex to purchase condoms?”) and skills for negotiating condom use with a partner (e.g., “Assume you wanted to use a condom with your main partner, but you’re not sure how s/he will react. How would you convince him/her to go along with your plan? What would s/he say in response? If that strategy didn’t work, what else might you use?” “Assume you wanted to avoid using a condom with your occasional partner, but you’re not sure how s/he will react. How would you convince him/her to go along with your plan? What would s/he say in response? If that strategy didn’t work, what else might you use?”). The measures of perceptions of control were adapted from Project RESPECT (Kamb et al., 1998), whereas the negotiation skills were coded on the basis of work by DeBro, Campbell, and Peplau (1994). Participants responded to questions about perceptions of control in 18 situations using an 11-point scale ranging from 0 (absolutely sure I could not use a condom in this situation) to 10 (absolutely sure I could use a condom in this situation). They reported on their negotiation skills using free response. Two independent coders then coded each answer for the viability of each strategy on a 5-point scale ranging from 1 (completely unviable strategy), for example, “I wouldn’t even try to convince him. It would be a question of trust” and “I don’t even know what to say” to 5 (completely viable strategy), for example, “I’ll tell him I’m gonna start practicing safe sex. If you wanna be my partner than you will have to practice safe sex. He’ll go along with it, and if he don’t, I’ll get the condom and just put it on him” “I would tell her it was in the best interest for both of us for our health and safety. If she wouldn’t go along with it, then we wouldn’t have sex”) Interrater reliability for coded free responses was r(350) = .90, p < .01; κ(350) = .91, p < .01. All measures were converted to z scores and then combined into an overall index of behavioral skills (α= .89).
Prior condom use
Condom use measures included reports of the percentage and number of times participants used condoms over a period of time. Participants were asked to report the frequency of sexual intercourse over the previous month, the previous 3 and 6 months, and the number of times of sexual intercourse for which condoms were used with both main and occasional partners. An overall percentage of condom use across both types of partners (main and occasional) was then derived from this information by dividing the number of times participants used a condom by the total number of times participants reported sexual intercourse and aggregating across time periods. As such, the index is composed of reports of condom use with all partners over several time periods (α= .90).
Measure of Acceptance of the Counseling
The dependent measure in the study was acceptance of an HIV-prevention counseling session. For this measure, reports from both the participant and the confederate were recorded to ensure the reliability of the observation. Reliability between the participant and confederate reports of counseling acceptance was high, r(350) = 1.00, p < .01; κ(350) = 1.00, p < .01.
Measures of Expectations as Hypothetical Mediators
To measure potential mediators of counseling acceptance, we asked participants to report their thoughts at the time of deciding whether to participate in the counseling session. Specifically, we asked participants if they thought that the counseling would (a) be useful for them, (b) make it easier for them to use condoms, (c) be necessary for them, (d) not make them change their point of view, (d) force them to do things they did not like, or (f) challenge their beliefs. Participants responded on a 4-point scale indicating their agreement or disagreement with each statement (i.e., 1= not at all, 2 = a little, 3 = quite a bit, or 4 = a lot). These measures were then combined into two indexes suggested by theory and confirmed with factor analysis, χ2(4) = 11.19, p > .43, comparative fit index = 1.00, non-normed fit index = 1.00, standardized root mean square residual = 0.02. A first index of expected usefulness included the statements that participation “would be useful for me,” “would make it easier for me to use condoms,” and “is necessary for me” (α= .81). A second index of expected threat to one’s attitudes or behavior included the statements that participation “would not make me change my point of view” [reversescored], “force me to do things I do not like,” and “would challenge my beliefs” (α= .74). These expectations about the content of the counseling were measured after participants had the option of accepting the HIV-prevention counseling.
Results
We tested for positive and negative linear associations of HIV-relevant knowledge, motivation to use condoms, condom-use-relevant behavioral skills, and prior condom use with acceptance of the counseling. In addition, we conducted mediation analyses to examine whether expectations about the content of the counseling session mediated the relations between HIV-relevant knowledge, motivation, behavioral skills, and prior condom use with acceptance of the counseling session. Finally, generalizability analyses tested whether these associations were contingent on participant characteristics, including demographic variables, past participation in HIV or STI counseling and testing, and number of sexual partners on acceptance of the HIV-prevention counseling.
Associations With Acceptance of Counseling
We used logistic regression, with acceptance of the counseling as the dependent measure and HIV-relevant knowledge, motivation, behavioral skills, and prior condom use as predictors in separate models. The first set of regressions examined the linear contribution of the predictors to counseling acceptance. There were several important linear associations, which appear in Table 2. Consistent with the positive linear prediction, we found positive linear relations for motivation, behavioral skills, and past condom use: for motivation, B = 0.17, Wald = 11.28, p < .01, OR = 1.18; for behavioral skills, B = 0.23, Wald = 8.47, p < .01, OR = 1.26; and for past condom use, B = 0.27, Wald = 5.25, p < .05, OR = 1.31. In contrast, the relation between HIV-relevant knowledge and acceptance of the counseling session, albeit identical in direction, was not statistically significant (B = 0.15, Wald = 1.39, p > .23, OR = 1.16).
Table 2. Simple Logistic Regression Analyses Predicting Acceptance of the HIV-Prevention Counseling Session.
| Percentage of acceptance |
||||||
|---|---|---|---|---|---|---|
| Predictor | B | SE | Wald test | Odds ratio (95% CI) | High | Low |
| Knowledge | .15 | .13 | 1.39 | 1.16(0.91, 1.49) | 44 | 33 |
| Motivation index | .17 | .05 | 11.28** | 1.18 (1.07, 1.31) | 43 | 31 |
| Behavioral skills index | .23 | .08 | 8.47** | 1.26(1.08, 1.47) | 46 | 29 |
| Condom use | .27 | .12 | 5.25* | 1.31 (1.04, 1.66) | 49 | 28 |
Note. Entries are coefficients from simple regressions. B = unstandardized regression coefficient; SE = standardized error estimate of the regression coefficients; CI = confidence interval. Wald tests are tests of significance, distributed as chi-squares with 1 degree of freedom. Odds ratios are related to the probability of participating in the counseling for participants with high HIV-relevant knowledge, motivation, behavioral skills, or prior condom use relative to participants with low HIV-relevant knowledge, motivation, behavioral skills, or prior condom use. The percentage of acceptance is a function of the regression equations computed for each variable; percentages are listed for participants who are high (one standard deviation above the mean) versus low (one standard deviation below the mean) for each measure. STI = sexually transmitted infection.
p < .05.
p < .01.
Mediation Analyses
We also examined whether expectations about the counseling’s expected usefulness or expected threat to one’s attitudes or behavior mediated the influence of HIV-relevant motivation, behavioral skills, and prior condom use on acceptance of the counseling session. As described by Baron and Kenny (1986), mediation is likely to take place if HIV-relevant motivation, behavioral skills, or prior condom use is associated with a given index of expectations (first regressions); if acceptance of the counseling is associated with the expectation index (second regression); and if acceptance of the counseling is associated with HIV-relevant motivation, behavioral skills, and prior condom use (third regression). In addition, the association of HIV-relevant motivation, behavioral skills, and prior condom use with acceptance of the counseling must be weaker when the expectation measures are included in the equation.
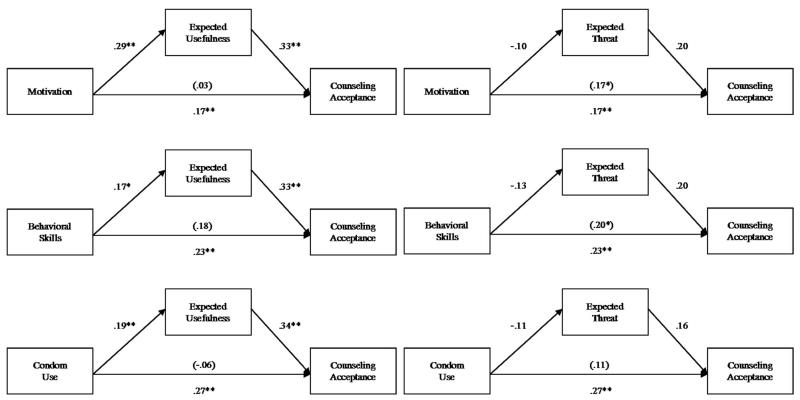
The relevant mediation models appear in Figure 2. The first regressions were estimated with linear procedures, whereas the second and third applied logistic procedures. As shown, the expected usefulness of the counseling (“would be useful for me,” “would make it easy for me to use condoms,” and “necessary for me”) emerged as a mediator of the influence of motivation, behavioral skills, and prior condom use and acceptance of the counseling session and was confirmed with Sobel tests: (for motivation, t = 3.03, p < .01; for behavioral skills, t = 1.98, p < .05; for prior condom use, t = 2.16, p < .05).4 That is, participants with higher (vs. lower) motivation to use condoms, higher (vs. lower) condom-use-relevant behavioral skills, and frequent (vs. infrequent) prior condom use expected the counseling to be more useful and were more likely to accept it as a result. In contrast, expected threat to one’s attitudes or behavior did not play a mediating role: for motivation, t =−0.20, p > .90; for behavioral skills, t =−1.17, p > .90; and for prior condom use, t =−0.22, p > .90.
Figure 2.
Analyses of the influence of motivation to use condoms, condom-use-relevant behavioral skills, and prior condom use on acceptance of HIV-prevention counseling with expected usefulness and expected threat as mediators. Coefficients are standardized regression coefficients. Coefficients in parentheses represent the regression coefficient for counseling acceptance on motivation, behavioral skills, or prior condom use, controlling for the mediator.
Generalizability Analyses
We were also interested in examining the generalizability of our findings by testing whether participants’ characteristics predicted acceptance of the counseling session or expectations about the content of the counseling session beyond HIV-relevant knowledge, motivation, behavioral skills, and prior condom use. Thus, we conducted a set of regression analyses that examined the effects of demographic variables (e.g., age, ethnicity, gender, level of education, and level of income), past participation in HIV or STI counseling and testing, and number of sexual partners on acceptance of the counseling. First, no demographic variable systematically predicted acceptance of the counseling session or either of the expectations indexes (all Bs < 0.18, ps > 0.10). In addition, past HIV and STI testing did not significantly predict either acceptance of the counseling program or the expectations indexes (all Bs < 0.13, ps > 0.17). In contrast, number of partners significantly positively predicted condom use (B = .17, p < .01) but significantly negatively predicted behavioral skills (B =−.13, p < .05). However, number of partners was not significantly correlated with knowledge, motivation, the expectations indexes, or acceptance of the counseling session (all Bs < .09, ps > .23).
Better information about the generalizability of our results, however, comes from confirming that the identified associations hold across groups. For this purpose, a last set of regressions included the predictors (e.g., HIV-relevant knowledge, motivation, behavioral skills, or prior condom use) as well as a moderator (e.g., level of education, ethnicity, gender, age, past participation in HIV or STI counseling and testing, or number of sexual partners) and the interaction between the predictor and the moderator. However, the analyses showed no significant interactions.5
Discussion
Although much work has been dedicated to designing efficacious intervention programs, the potential of these programs to change behavior can be curtailed if the audiences who need them do not accept them. Given this situation, we investigated hypotheses about the influence of HIV-relevant knowledge, motivation to use condoms, condom-use-relevant behavioral skills, and prior condom use on acceptance of an HIV-prevention counseling session. Of these hypotheses, only the hypothesized positive linear relation received support, suggesting that participants with high HIV-relevant motivation, behavioral skills, and prior condom use were most likely to participate in further prevention efforts.
In addition to testing the influences of aspects such as prior attitudes and behaviors on exposure decisions, we investigated whether expectations about the content of the counseling session mediated these influences. Thus, we examined two indexes of expectations about the counseling session: (a) expected usefulness of the counseling session to increase condom use, and (b) expected threat of the counseling session to participants’ current attitudes or behavior. Findings indicated that only expected usefulness mediated the influence of HIV-relevant motivation, behavioral skills, and prior condom use on counseling acceptance. Specifically, participants with high motivation, behavioral skills, and prior condom use expected the counseling to be more useful for them and therefore were more likely to accept.
Implications for Theory
Our findings about the association of motivation to use condoms, condom-use-relevant behavioral skills, and prior condom use with acceptance of the HIV-prevention counseling session have implications for three prior models of behavior change. First, the findings suggest that Fisher and Fisher’s (1992, 2000) classification of the factors involved in behavior change is also useful to study participation decisions. Specifically, although knowledge appeared to play no role, motivation (attitudes, beliefs, norms, and intentions), behavioral skills (negotiation skills and perceived behavioral control), and past behavior (prior condom use) predicted acceptance of HIV-prevention counseling.
Second, our findings suggest that, in line with dissonance theory, people prefer consonant, or behavior-consistent, information, rather than dissonant, or behavior-inconsistent, information (Festinger, 1957). Specifically, participants who already had high motivation to use condoms, good condom-use-relevant behavioral skills, and frequent prior condom use were the most likely to accept counseling designed to increase condom use. This result is ironic given that those who could most benefit from an HIV-prevention counseling session are the ones who are not already engaging in the recommended risk-reduction behaviors. Sadly though, those at highest risk for HIV infection are least likely to accept preventive efforts.
Third, our findings suggest that people are not motivated to avoid information that tries to force them to change. Specifically, expected threat did not mediate the relation of HIV-relevant knowledge, motivation, behavioral skills, and prior condom use with acceptance of the counseling session. Given the decades of evidence supporting reactance theory, it seems unlikely that expected threat to one’s position should play no role in the decision of whether to accept counseling. One possibility is that participants may expect the threat but do not want to self-report that they are expecting the counseling to change their attitudes or behavior. For instance, if participants admit that the counseling would be a threat to their current practices and subsequently participate in the counseling session, they may feel that the counseling will force a change that they do not want. However, if participants admit that the counseling would be a threat to their current practices and subsequently do not participate in the counseling session, they may be stuck in a self-presentational quandary, wherein they appear weak and unable to defend their current practices. Another possibility is that participants may not be aware of experiencing reactance (Albarracín & Vargas, in press). As such, perhaps it is not surprising that self-reported expected threat did not mediate the effects of HIV-relevant motivation, behavioral skills, and prior condom use with acceptance of the counseling. Further work may examine the implications of expected threat for counseling acceptance.
Implications for Counseling Practices
The results of this study have several important implications for practice. First, these data suggest that further efforts must be directed toward recruiting and enrolling target audiences. Contrary to the assumption that those who are at highest risk for HIV are the ones who seek out and accept HIV-prevention counseling, these findings suggest that those who already protect themselves from HIV are the most likely to accept. Second, these data provide a potential intervention point to increase acceptance of disease-prevention interventions. Specifically, in this study, the expected usefulness of the program was associated with increased acceptance. If program designers are able to increase participants’ perceptions that the programs may be worth their while, practitioners may be better able to attract reluctant audiences.
One potentially fruitful strategy to increase acceptance may be to carefully structure the offer of counseling programs. For example, individuals with low (vs. high) motivation to use condoms, low (vs. high) condom-use-relevant behavioral skills, and low (vs. high) condom use have different expectations about the content of the counseling session. As a result, different groups may need specific scripted introductions to the program or different methods of referral to counseling. Participants with low motivation, behavioral skills, or condom use may require introductions that suggest that the counseling will be useful to them. However, to avoid reactance, such suggestions may need to be combined with statements that the recipients will be in charge of the decision of whether to use condoms. For instance, recent work by Albarracín, Durantini, et al. (2008) suggests that simply changing the way a counseling program is offered by altering the description of the content of the counseling session can boost enrollment in the counseling. For instance, Albarracín, Durantini, et al.’s (2008) experimental meta-intervention condition described the counseling as providing useful information about HIV and HIV prevention without forcing change in reluctant participants. Participants in the study with low intentions to use condoms were 15% more likely to enroll in the counseling following exposure to the experimental rather than the control condition (60% vs. 45%). Future research should investigate different methods for effectively enrolling high-risk populations.
Limitations and Future Directions
Although the results of the mediation analyses suggested that expected usefulness was implicated in the observed biases, there are two important considerations. First, the measures of the mediators were obtained at the end of the study, thus requiring retrospective reports from the participants. As is well known, people are often unable to report on the reasons for their decisions (Nisbett & Wilson, 1977). In addition, we did not experimentally manipulate HIV-relevant knowledge, motivation, behavioral skills, prior condom use, or expectations about the counseling session. Thus, future research should go beyond our correlational design to experimental replication of our findings.
A second potential concern might be that the sample may bias the relations of motivation, behavioral skills, and prior condom use with acceptance of an HIV-prevention counseling session. For instance, a large proportion of the sample was female (74%) and African American (56%), with low incomes (61% earned less than $10,000 per year). However, moderation analyses examining the effects of ethnicity, gender, and level of income showed no effect of any of these variables on acceptance of the counseling session. Another possibility is that prior enrollment in a program might be used as a basis to rationalize that it is useful (i.e., “I enrolled; therefore, it must be useful”). However, past participation in HIV or STI counseling and testing did not predict either counseling acceptance or expectations about the counseling session. A final alternative is that people at highest risk for HIV infection (e.g., those who have more sexual partners) may more frequently use condoms than people at lower risk for infection (e.g., those who have fewer sexual partners). Our data, however, speak against this alternative. Specifically, number of sexual partners did not predict acceptance of the counseling program or either of the indexes of expectations.
In our study, the obtained effect sizes were small, suggesting limited biases introduced by motivation to use condoms, condom-use-relevant behavioral skills, and prior condom use. Nonetheless, these effects are not trivial. For example, acceptance of the counseling was 31% and 43% for participants with low and high motivation, respectively. Similarly, acceptance was 29% and 46%, respectively, for participants with low and high behavioral skills and 28% and 49%, respectively, for participants with relatively low and high prior condom use. These differences suggest that there are meaningful differences in the probability of accepting an HIV-prevention counseling session on the basis of prior motivation, behavioral skills, and condom use. Moreover, detecting these small findings suggests that the methods used in this research are sensitive and that other determinants of acceptance could be analyzed with similar techniques.
Another aspect that future research might address is the retention of participants within a prevention program after the program has commenced. Perhaps the factors influencing initial acceptance also influence retention. If so, higher risk audiences may drop out more than lower risk audiences. Recently, a meta-analysis by Noguchi et al. (2007) suggested that this is the case. One further possibility for examining retention in preventive programs may be to use the same indexes of expectations presented in this study. For instance, expected usefulness may increase acceptance and may also decrease participant dropout. This hypothesis could be tested by having participants fill out expectation indexes at several points in the process of deciding to enroll in the program and deciding to remain in the program once it is initiated. Future research should investigate these options, and also find other ways of measuring the mediators of exposure. For instance, if self-report measures are subject to self-presentational concerns, perhaps using measures that are not subject to these flaws (e.g., psychophysiological measures, such as galvanic skin response or eyeblink) may provide additional insights.
Final Note
To conclude, we note that although researchers have examined myriad factors relevant to health-intervention design, these efforts are incomplete without understanding who accepts the programs. By examining factors relevant to acceptance decisions, we now have a clearer picture not only of who accepts but also of why participants may or may not accept relevant counseling programs. By understanding these factors, researchers may be better able to solicit acceptance from target populations and prepare interventions to attract at-risk populations. Ironically, participants with low motivation to use condoms, low condom-use-relevant behavioral skills, and low prior condom use are the least likely to accept the HIV-prevention counseling designed for them. This finding is alarming because these participants are the ones who have the most to gain from acceptance. Thus, future research should investigate how to increase acceptance by high-risk audiences.
Acknowledgments
This research was supported by Grant R01 NR08325-01 from the National Institutes of Health. We thank Laura Glasman for her invaluable assistance in designing this project’s questionnaire. We also thank the project assistants during the years 2003–2005 and James A. Shepperd and Jesse Dallery for detailed comments on an earlier version of the article. Earlier versions of some of the analyses described here were presented as a thesis by the Allison Earl, conducted under the direction of Dolores Albarracín.
Footnotes
One concern is that the presence of the observer/counselor may have influenced participants’ willingness to accept the counseling. However, the presence of the observer/counselor was necessary to measure participants’ acceptance of the counseling. In addition, the observer/counselor was present in the room for approximately 20 min before the offer to participate in the counseling. During this time, participants also had the option to read brochures and watch a video. As such, steps were taken to minimize the invasiveness of the observer/counselor’s presence when the counseling was offered. Furthermore, although such influence is a possibility, it is unlikely given prior data on this problem. Specifically, a meta-analysis by Noguchi et al. (2007) suggested that the acceptance rates for counseling programs are similar across type of offer (e.g., in person, by computer).
Although there are other methodologies that also yield accurate, sensitive measures (e.g., computer-aided or paper-and-pencil measures), a face-to-face interview was more adequate for the paradigm to work successfully. This face-to-face interview allowed us to include a break during which the observation of acceptance took place.
Before the offer to participate in the counseling session, and while the counselor was in the room, the participant had 10 min to peruse six brochures sitting on the table. After 10 min had elapsed, the interviewer knocked on the door, apologized for a delay, and offered the participant a 10-min video about HIV. The client could either accept or decline to have the video played. If the participant previously accepted the video, the interviewer waited 10 min before returning to offer the counseling. In contrast, if the participant declined to watch the video, the interviewer would wait only 5 min before returning to the room and offering the counseling to the participant. Analyses of the effects on and of brochures and videos are presented in other reports.
Sobel tests are not designed for logistic regression analyses but are offered for descriptive purposes.
These data are available at http://www.psych.uiuc.edu/~dalbarra/sal/.
Contributor Information
Allison Earl, Department of Psychology, University of Florida.
Dolores Albarracín, Department of Psychology, University of Florida.
Marta R. Durantini, Department of Psychology, University of Florida
Joann B. Gunnoe, Alachua County Health Department, Gainesville, Florida
Josh Leeper, Department of Psychology, University of Florida.
Justin H. Levitt, Department of Psychology, University of Florida
References
- Ajzen I, Fishbein M. Understanding and predicting social behavior. Prentice Hall; Englewood Cliffs, NJ: 1980. [Google Scholar]
- Ajzen I, Fishbein M. The influence of attitudes on behavior. In: Albarracín D, Johnson BT, Zanna MP, editors. The handbook of attitudes. Erlbaum; Mahwah, NJ: 2005. pp. 173–221. [Google Scholar]
- Albarracín D, Durantini MR, Earl A, Gunnoe JB, Leeper J. Beyond the most willing audiences: A meta-intervention to increase exposure to HIV prevention interventions by vulnerable populations. Health Psychology. 2008;27:638–644. doi: 10.1037/0278-6133.27.5.638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albarracín D, Gillette J, Earl AN, Glasman LR, Durantini MR, Ho MH. A test of major assumptions about behavior change: A comprehensive look at the effects of passive and active HIV-prevention interventions since the beginning of the epidemic. Psychological Bulletin. 2005;131:856–897. doi: 10.1037/0033-2909.131.6.856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albarracín D, Ho R, McNatt PS, Williams WR, Rhodes F, Malotte CK, Hoxworth T, Bolan G, Zenilman J, Iatesta M, The Project RESPECT Study Group The structure of beliefs about condom use. Health Psychology. 2000;19:458–468. doi: 10.1037//0278-6133.19.5.458. [DOI] [PubMed] [Google Scholar]
- Albarracín D, Leeper J, Earl A, Durantini MR. From brochures to videos to counseling: Exposure to HIV-prevention programs. AIDS and Behavior. 2008;12:354–362. doi: 10.1007/s10461-007-9320-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albarracín D, McNatt PS, Klein C, Ho R, Mitchell A, Kumkale GT. Persuasive communications to change actions: An analysis of behavioral and cognitive impact in HIV prevention. Health Psychology. 2003;22:167–177. doi: 10.1037//0278-6133.22.2.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albarracín D, Mitchell A. The role of defensive confidence in preference for proattitudinal information: How believing that one is strong can be a weakness. Personality and Social Psychology Bulletin. 2004;30:1565–1584. doi: 10.1177/0146167204271180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albarracín D, Vargas P. Attitudes and persuasion: From biology to social responses to persuasive intent. In: Fiske S, Gilbert D, editors. Handbook of social psychology. Oxford University Press; New York: in press. [Google Scholar]
- Aubrey JS. Exposure to sexually objectifying media and body self-perceptions among college women: An examination of the selective exposure hypothesis and the role of moderating variables. Sex Roles. 2006;55:159–172. [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. Freeman; New York: 1997. [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Baum WM. Understanding behaviorism: Science, behavior, and culture. Allyn & Bacon; Boston: 1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bender DS, Skodoll AE, Dyck IR, Markowitz JC, Shea MT, Yen S, et al. Ethnicity and mental health treatment utilization by patients with personality disorders. Journal of Consulting and Clinical Psychology. 2007;75:992–999. doi: 10.1037/0022-006X.75.6.992. [DOI] [PubMed] [Google Scholar]
- Brehm JW. A theory of psychological reactance. Academic Press; New York: 1966. [Google Scholar]
- Brehm JW. Responses to loss of freedom: A theory of psychological reactance. General Learning Corporation; 1972. [Google Scholar]
- Canon LK. Self-confidence and selective exposure to information. In: Festinger L, editor. Conflict, decision, and dissonance. Stanford University Press; Stanford, CA: 1964. pp. 83–95. [Google Scholar]
- DeBro SC, Campbell SM, Peplau LA. Influencing a partner to use a condom: A college student perspective. Psychology of Women Quarterly. 1994;18:165–182. doi: 10.1111/j.1471-6402.1994.tb00449.x. [DOI] [PubMed] [Google Scholar]
- Durantini MR, Albarracín D, Mitchell AL, Earl AN, Gillette JC. Conceptualizing the influence of social agents of behavior change: A meta-analysis of the effectiveness of HIV-prevention interventionists for different groups. Psychological Bulletin. 2006;132:212–248. doi: 10.1037/0033-2909.132.2.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earl A, Albarracín D. Nature, decay, and spiraling of the effects of fear-inducing arguments and HIV counseling and testing: A meta-analysis of the short- and long-term outcomes of HIV-prevention interventions. Health Psychology. 2007;26:496–506. doi: 10.1037/0278-6133.26.4.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edeani DO. Field study of selective exposure and selective recall as functions of locus of control and information utility. Dissertation Abstracts International. 1979;40:2960. [Google Scholar]
- Festinger L. A theory of cognitive dissonance. Stanford University Press; Stanford, CA: 1957. [Google Scholar]
- Fishbein M, Ajzen I. Belief, attitude, intention, and behavior: An introduction to theory and research. Addison Wesley; Reading, MA: 1975. [Google Scholar]
- Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychological Bulletin. 1992;111:455–474. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA. Theoretical approaches to individuallevel change in HIV risk behavior. In: Peterson JL, DiClemente RJ, editors. Handbook of HIV prevention. Plenum; New York: 2000. pp. 3–55. [Google Scholar]
- Freedman JL, Sears DO. Warning, distraction, and resistance to influence. Journal of Personality and Social Psychology. 1965;1:262–266. doi: 10.1037/h0021872. [DOI] [PubMed] [Google Scholar]
- Hart WP, Albarracín D, Lindberg M, Brechen I, Merrill L, Lee KH, Eagly AH. A meta-analysis of selective exposure to information. 2008. Feeling validated versus being correct? Manuscript in preparation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Innes JM. Selective exposure as a function of dogmatism and incentive. Journal of Social Psychology. 1978;106:261–265. doi: 10.1080/00224545.1978.9924177. [DOI] [PubMed] [Google Scholar]
- Kamb ML, Fishbein M, Douglas JM, Rhodes F, Rogers J, Bolan G, Zenilman, Hoxworth T, Malotte CK, Iatesta M, Kent C, Lentz A, Graziano S, Byers, Peterman TA. Efficacy of risk-reduction counseling to prevent human immunodeficiency virus and sexually transmitted diseases: A randomized controlled trial. Project RESPECT Study Group. Journal of the American Medical Association. 1998;280:1161–1167. doi: 10.1001/jama.280.13.1161. [DOI] [PubMed] [Google Scholar]
- Knobloch-Westerwick S, Dillman Carpentier F, Blumhoff A, Nickel N. Informational utility effects on selective exposure to good and bad news: A cross-cultural investigation. Journalism and Mass Communication Quarterly. 2005;82:181–195. [Google Scholar]
- Lundgren SR, Prislin R. Motivated cognitive processing and attitude change. Personality and Social Psychology Bulletin. 1998;24:715–726. [Google Scholar]
- McFarland SG, Warren JC. Religious orientations and selective exposure among fundamentalist Christians. Journal for the Scientific Study of Religion. 1992;31:163–174. [Google Scholar]
- Nisbett RE, Wilson TD. Telling more than we can know: Verbal reports on mental processes. Psychological Review. 1977;84:231–259. [Google Scholar]
- Noguchi K, Albarracín D, Durantini MR, Glasman LR. Who participates in which health promotion programs? A meta-analysis of motivations underlying enrollment and retention in HIV-prevention interventions. Psychological Bulletin. 2007;133:955–975. doi: 10.1037/0033-2909.133.6.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perrissol S, Boscher G, Cerclé A, Somat A. Alcohol drinking, self-efficacy and selective exposure to alcohol adverts. European Review of Applied Psychology. 2005;55:235–243. [Google Scholar]
- Silvia PJ. Reactance and the dynamics of disagreement: Multiple paths from threatened freedom to resistance to persuasion. European Journal of Social Psychology. 2006;36:673–685. [Google Scholar]
- Stice E, Marti CN, Spoor S, Presnell K, Shaw H. Dissonance and health weight eating disorder prevention programs: Long-term effects from a randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2008;76:329–340. doi: 10.1037/0022-006X.76.2.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweeney PD, Gruber KL. Selective exposure: Voter information preferences and the Watergate affair. Journal of Personality and Social Psychology. 1984;46:1208–1221. [Google Scholar]
- Webb EJ, Campbell DT, Schwartz RD, Sechrest L. Unobtrusive measures: Nonreactive research in the social sciences. Rand McNally; Chicago, Illinois: 1966. [Google Scholar]
- Woolsey TD, Cochran WG, Mainland D, Martin MP, Moore FE, Jr., Patton RE. On the use of sampling in the field of public health. American Journal of Public Health National Health. 1954;44:719–740. doi: 10.2105/ajph.44.6.719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zillmann D, Chen L, Knobloch S, Callison C. Effects of lead framing on selective exposure to internet news reports. Communication Research. 2004;31:58–81. [Google Scholar]