Abstract
Background
Health care officials and legislators need accurate data on prevalence and numbers of individuals with bleeding disorders in order to plan and allot their budgets; the manufacturers of coagulation factors also need these data to estimate the amount of factors required to prevent scarcity of these products.
Materials and methods
We surveyed the prevalence of haemophilia A, haemophilia B, von Willebrand's disease and rare bleeding disorders in North-Eastern Iran. The survey was done in the period from September 2009 to March 2011. Information was collected from the medical records in three major hospitals and a haemophilia centre; the patients' updated data were obtained by telephone.
Results
Overall in the current survey 552 patients with inherited coagulation disorders were identified and their medical records obtained. Of these, 429 (77.5%) had common bleeding disorders (haemophilia A, haemophilia B, von Willebrand's disease), 85 (15.6%) had rare bleeding disorders (deficiency of coagulation factors V, VII, X, XIII, I, XI, combined factor V and VIII deficiency) and 38 (6.9%) had platelet disorders.
The commonest bleeding disorders were haemophilia A (n=287, 51.9%), haemophilia B (n=92, 16.6%), von Willebrand's disease (n=50, 9%), factor V deficiency (n=21, 3.8%), factor VII deficiency (n=19, 3.4%), factor X deficiency (n=2, 0.36%), combined factor V and VIII deficiency (n=28, 5.8%), factor XIII deficiency (n=11, 1.99%), factor XI deficiency (n=2, 0.4%), afibrinogenaemia (n=2, 0.36%) and platelet disorders (n=38, 6.9%).
Discussion
There is notable population of individuals with bleeding disorders in North-Eastern Iran.
Keywords: haemophilia A and B, von Willebrand's disease, platelet disorders, rare bleeding disorders, North-Eastern Iran
Introduction
The prevalences of haemophilia A (HA) and haemophilia B (HB) have been estimated as 10.5 and 2.8/100,000 male births, respectively. The prevalence of HA per 100,000 males in developed countries is 12.8±6.0 (mean±SD) while it is 6.6±4.8 in developing countries1,2. The prevalence of haemophilia in developing countries is less than that in both developed countries and the average international incidence3. Literature reviews imply that the incidence of HA and HB is the same in all racial and population groups and has been estimated to be 20 per 100,000 male births1,4.
The prevalence of HA has been reported for only three of ten countries in Asia and ranges from 2.9–3.6 per 100,000 males4.
The possible reasons for under-diagnosed bleeding disorders in developing countries may be lack of diagnostic capabilities and insufficient public awareness of abnormal bleeding5. In developing countries in which governmental resources are restricted, health legislators tend to pay more attention to public health concerns that affect larger proportions of the community1,6. Nevertheless, health care officials need accurate data on the prevalence and numbers of individuals with bleeding disorders in order to plan and allot their budgets. Furthermore, the manufacturers of coagulation factors also need these data to estimate the amount of factors required to prevent scarcity of these products7,8.
There are 18 cities and towns in North-Eastern Iran. There is a lack of information on the prevalence of common and rare bleeding disorders in this area. The aim of this study was to document the prevalence, demographic and epidemiological features and bleeding manifestations of common and rare bleeding disorders in this area of Iran.
Materials and methods
This survey was done during the period from September 2009 to March 2011. The medical records of three major referral hospitals (Ghaem Hospital, Imam Reza Hospital and Dr. Sheikh Paediatric Hospital) were examined and all diagnosed cases with bleeding disorders were extracted. The medical records were related to all individuals with bleeding disorders who had been referred to these hospitals in the last 15 years (1997 and after). The medical records of patients after 1997 are accessible by a computerised system. Ghaem Hospital and Imam Reza Hospital were the main centres for the treatment of bleeding disorders until January 2004 when a special paediatric hospital was established and patients with bleeding disorders were referred to it. In order to avoid missing any bleeders we integrated the medical records from the above described three hospitals with records from Mashhad Haemophilia Centre. All the data required were extracted from the medical records and, as a complement, all the individuals were telephoned to obtain updated information. The data collected comprised age, sex, family history of a bleeding disorder, home injection ability, history of orthopaedic surgery, last time of plasma or cryoprecipitate usage, bleeding symptoms and use of orthopaedic devices. The criteria for regarding haemorrhagic symptoms as positive are described fully in reference 9.
Results
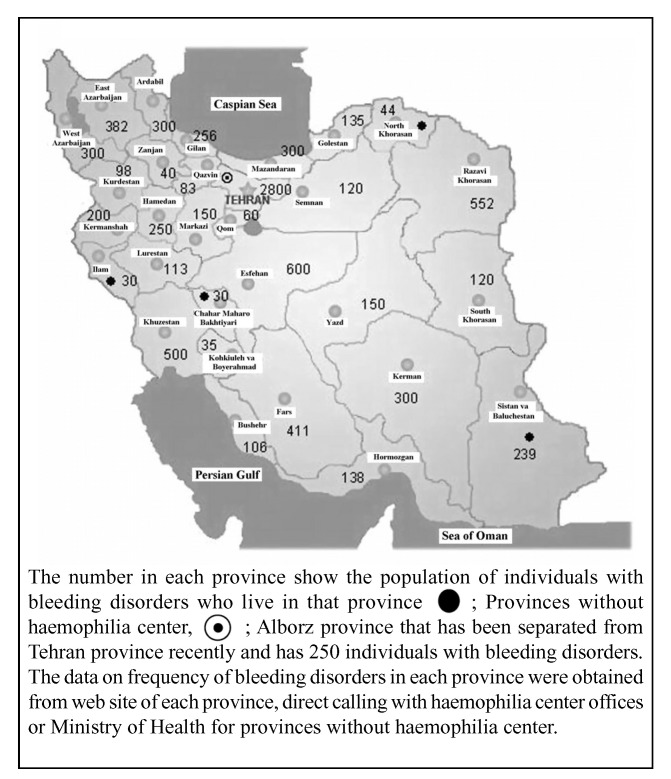
Khorasan Razavi is one of the three provinces that make up greater Khorasan. The total population of the province in 2009 was about 5,493,690, of whom 2,787,620 were male. The province's capital, Mashhad, had a population of 3,140,838, of whom 1,591,066 were male (Figure 1).
Figure 1.
The Khorasan Razavi province location in NorthEastern Iran and distribution numbers of bleeding disorders in various provinces of the country.
There are limited genetic facilities in our hospitals and those available are used for the diagnosis of patients with leukaemia. There are also shortages of experienced staff and equipment, so genetic evaluation of bleeding patients is not routinely performed in our province at present. As regards haemostatic evaluation, all patients with a history of a bleeding tendency were referred to the country's capital, Tehran, for coagulation studies and the determination of both the type of bleeding disorder and its severity until 2006 when a coagulometer was set up in the Sarvar clinic for assays of both coagulation factors and thrombophilia. About 80% of the coagulation studies in the patients described in this survey were carried out in Tehran.
The full significance of each bleeding manifestations is explained in reference 9. Petechiae and purpura are not reported among haemorrhagic symptoms, because some patients deny such mild symptoms and patients' reports are not fully reliable. Foot surgery was regarded positive when the patient had a history of any orthopaedic operation for a fracture, joint replacement, or joint fixation. Patients were considered to be sensitive to blood products if they experienced itching or developed skin rashes during or after injection of a blood product.
Overview
Overall 552 cases with inherited bleeding disorders were identified and evaluated. Of these, 429 (77.5%) had common bleeding disorders (HA, HB, von Willebrand's disease [vWD]), 85 (15.6%) had rare bleeding disorders (deficiency of coagulation factors V, VII, X, XIII, I, XI, combined factor V and VIII deficiency) and 38 (6.9%) had platelet disorders. A rough estimated frequency of bleeding disorders in the province was 10.05, while the frequency of HA and HB was 6.90, the frequency of rare bleeding disorders was 1.55, the frequency of vWD was 0.91 and the frequency of platelet disorders was 0.69 in 100,000 males.
Of the 552 cases, 463 were male (83.8%) and 89 were female (16.2%). The youngest affected individual was a 45-day old neonate with factor V deficiency and oldest one was a 91-year old male with mild HA. The mean age (±SD) of the patients was 25.86±14.61 years. The commonest bleeding disorders were HA (n =287, 51.9%), HB (n =92, 16.6%), vWD (n =50, 9%), factor V deficiency (n =21, 3.8%), factor VII deficiency (n =19, 3.4%), factor X deficiency (n =2, 0.36%), combined factor V and VIII deficiency (n =28, 5.8%), factor XIII deficiency (n =11, 1.99%), factor XI deficiency (n =2, 0.4%), afibrinogenaemia (n =2, 0.36%) and platelet disorders (n =38, 6.9%).
Two hundred and six (40%) of the subjects could inject coagulation concentrate, while 308 (60%) were dependent on medical services for their injections.
Haemophilia A
There were 287 cases with HA. The rough estimated prevalence of HA was 10.29 per 100,000 males. As regards phenotype, 143 (49.8%) had severe HA, 59 (20.6%) had moderate HA and 85 (29.6%) had mild HA. The youngest individual was a 3-year old child with a severe phenotype and the oldest was a 91-year old man with mild HA. The mean age (±SD) was 27.25±15.77 years, while the median was 25 years.
Of the patients with HA, 212 (73.9%) were adults, while 75 (26.1%) were children. Two hundred and thirty-one patients (82.9%) had a positive history of bleeding in the family while 49 (17.1%) were sporadic cases. One hundred and fifty patients (52.4%) had learnt to self-infuse, whereas 136 (47.6%) were dependent on health agencies for their infusions. Among 143 individuals with severe HA, 104 (72.7%) had learnt to inject factor VIII concentrate, whereas 27 (46.5%) of the 58 individuals with moderate HA and 19 (22.3%) of the 85 with mild HA had learnt to do so. The Mann-Whitney test revealed that learning to self-inject coagulation factor was correlated with the severity of HA (P =0.000). In our region in situations in which HA patients do not have access to factor VIII concentrate, they inject cryoprecipitate. The mean (±SD) time since last usage of cryoprecipitate among these individuals was 14.36±10.63 months. Three HA individuals (1%) were sensitised to cryoprecipitate infusion.
Overall, 21 (7.7%) haemophiliacs had undergone orthopaedic surgery, with the most common operations being those to the feet (16 cases, 76.1%).
With regards to blood-borne viral infections, the frequencies were as follow; hepatitis B surface antigen (Hbs Ag) positivity, 5 cases (1.8%), anti-hepatitis C virus (HCV) positivity, 70 cases (24.6%), anti-human immunodeficiency virus (HIV), 1 case (0.4%) and anti-human T-lymphotropic virus (HTLV-I), 0 cases.
Overall, 49 (15.6%) subjects had a history of having undergone surgery: the most common causes were post trauma (11 cases, 24.4%), appendectomy (10 cases, 22.2%) and hernia (6 cases, 13.3%). Of these 49 cases, 23 subjects had experienced bleeding during or after surgery (46.9%), while 26 cases (53.1%) had not had notable bleeding.
The frequencies of bleeding manifestations were as follows: haemarthrosis 207 (72.6%), epistaxis 160 (55.9%), vast ecchymosis 203 (71%), haematuria 92 (32.3%), umbilical cord bleeding 5 (1.8%), central nervous system bleeding 7 (2.4%), post-dental extraction bleeding 105 (89%), gastro-intestinal tract bleeding 60 (21%), haematoma 12 (4.2%) and gum haemorrhage 15 (5.3%).
Overall, 75 (26.13%) had a history of using orthopaedic aids: walking stick 64 (22.4%), crutch 10 (3.5%) and wheel chair 1 (0.3%).
Factor VIII inhibitor status and its relation with concentrate treatment have already been described by Modaresi et al. and Mansouritorghabeh et al.10,11.
Haemophilia B
There were 92 cases with HB. The rough estimated prevalence of HB was 3.30 per 100,000 males. The phenotype was severe in 43 (46.7%) patients, moderate in 33 (35.9%) and mild in 16 (17.4%). The youngest patients were two children who were 2 years old and had a severe phenotype, while the oldest patient with HB was a 62-year old man with a mild phenotype. The mean age (±SD) of the patients was 25.14±12.17 years and the median was 24 years. Sixty-six patients (71.7%) were adult and 26 (28.3%) were children. Eighty-one patients (88%) had a positive history in the family and 11 (12%) were sporadic cases. Among the patients with HB, 44 (47.8%) had learnt to infuse coagulation factor by themselves, while 48 (52.2%) were dependent on health agencies for their infusions. An analysis of the findings showed that independence from medical services for injections differed according to the severity of disorder: severe 25 (56.8%), moderate 14 (31.8%), mild 5 (11.4%). The Mann-Whitney test revealed that learning to self-inject was correlated with the severity of HB (P =0.047). In our region, in circumstances in which patients with HB do not have access to factor IX concentrate, they usually inject fresh-frozen plasma (FFP). The mean time since last use of FFP was 11.72±10.28 months. One case (1.1%) was sensitised to FFP injection. Ten haemophiliacs (11.2%) had experienced orthopaedic surgery, including operations to the hands (1 case, 10%), feet (8 cases, 80%) and pelvis (1 case, 10%). Fifteen cases (15.7%) had undergone various types of surgery (excluding orthopaedic surgery) and of these, 10 cases (66.6%) had had bleeding during or after their operations. The most common surgeries were haemorrhoid surgery (2 cases, 14.3%) and lumbar vertebrae surgery (2 cases, 14.3%).
The frequencies of blood-borne viral infections were as follows: HBs Ag positivity, 2 cases (2.2%); anti- HCV positivity, 33 cases (35.9%); anti- HIV, 0 cases; and anti- HTLV-I, 1 case (1.1%).
The frequencies of bleeding manifestations were as follows: haemarthrosis 64 (69.9%), epistaxis 51 (55.4%), vast ecchymosis 53 (57.6%), haematuria 31 (33.7%), umbilical cord bleeding 5 (5.4%), central nervous system bleeding 7 (7.6%), post-dental extraction bleeding 37 (97.4%), gastro-intestinal tract bleeding 22 (23.9%) and gum haemorrhage 3 (3.3%).
Overall, 36 (39.1%) patients with HB had a history of using orthopaedic aids: walking stick 31 (33.7%), crutches 3 (3.3%) and wheel chair 2 (2.2%).
The data on factor IX inhibitor status and relation with types of treatment have already been described12,13.
von Willebrand's disease
There were 50 cases with vWD. The rough estimated prevalence of vWD was 1.79 per 100,000 population. Subclasses of vWD were not determined because of the lack of diagnostic facilities in our province. The youngest patient diagnosed with vWD in our survey was a 6-year old child, while the oldest was a 67-year old woman. The median age of the patients with vWD was 24 years: 36 cases (72%) were adults, while 14 cases (28%) were children. Thirty-one (62%) patients had one or more relative diagnosed with vWD, whereas the other 19 (38%) cases were sporadic. Seven of the patients (14%) had learnt to infuse coagulation factor concentrate at home by themselves, while 41 (82%) were dependent on health agencies for their infusions. In our province, in situations in which vWD patients do not have access to semi-pure factor VIII concentrate, they inject cryoprecipitate. The mean time since last use of cryoprecipitate was 8.09±7.54 months. One patient (2%) was sensitive to cryoprecipitate injections. None of the patients with vWD had undergone orthopaedic surgery.
None of the patients was positive for HBs Ag, HIV or HTLV-I, while 7 (14%) were positive for HCV. Overall 17 had undergone various types of surgery. Among them 15 (88.23%) had bleeding during or after surgery, with bleeding episodes being most common after delivery (4 cases, 26.6%), appendectomy (3 cases, 20%) and caesarean section (3 cases, 20%).
The frequencies of bleeding manifestations were as follows: haemarthrosis 19 (38%), epistaxis 43 (86%), vast ecchymosis 38 (76%), haematuria 8 (16%), menorrhagia 14 (63.3% of those at risk), umbilical cord bleeding 2 (4%), central nervous system bleeding 0, post-dental extraction bleeding 11 (84.6% of those at risk), gastro-intestinal tract bleeding 12 (24%), post-operative bleeding 11 episodes in 17 cases (64.7%) and gum haemorrhage 16 (32%).
Overall, 3 (6%) patients with vWD used orthopaedic aids (including a walking stick).
Factor V deficiency
There were 21 cases with factor V deficiency. The haemorrhagic manifestations of 16 of these cases were reported in 201014. The demographic and haemostatic characteristics of the five new cases are described below. The youngest patient was a 2-month old neonate and the oldest was a woman of 63 years. The mean age was 34±0.26 years and the median was 27 years. Three patients (60%) had a family history of factor V deficiency and two cases (40%) were sporadic. Two cases (40%) came from two families with first degree consanguineous marriages. The patients' haemorrhagic and demographic characteristics are presented in Table I. Three of these patients (cases 3, 4 and 5) have undergone periodontal surgery, caesarean section and hernia repair. In all cases, bleeding was successfully controlled through the use of FFP. None of new cases had a history of blood-borne viral infections.
Table I.
The demographic and haemostatic findings in five individuals with factor V deficiency.
| Case | Age (years) | Sex | Factor V level (%) | Epistaxis | Ecchymoses | Post circumcision bleeding | Post dental extraction bleeding | Haematoma |
|---|---|---|---|---|---|---|---|---|
| 1 | 1 Mo | F | 14 | − | + | + | ||
| 2 | 45 | M | 3 | + | − | + | + | |
| 3 | 36 | M | 1 | + | + | + | + | − |
| 4 | 27 | F | 1 | − | + | − | ||
| 5 | 63 | F | 10.5 | + | + | − | ||
| Total | 3 (60%) | 4 (80%) | 2 (100%)* | 1 (100%)* | 2 (40%) |
Legend Mo: month; F: female; M: male;
Percentages calculated on the basis of the number of patients who could have this bleeding complication.
Factor VII deficiency
There were 19 cases with factor VII deficiency. The haemorrhagic manifestations of 12 of these cases were reported in 200815. There are now seven new cases, whose haemostatic and demographic characteristics are presented in Table II. The youngest was a 6-year old male and the oldest a 33-year old woman. Their mean age was 15.42 years and their median age was 20 years. Two patients (28.5%) had a positive family history for factor VII deficiency, whereas five cases (71.5%) were sporadic. Four (57%) came from four first degree consanguineous marriages, whereas in the other three cases (43%) the patients' parents were not related. The commonest bleeding manifestations were ecchymosis 5 (71%), epistaxis 4 (57%), post-dental extraction bleeding 4 (80%) and gastrointestinal tract bleeding 3 (43%) (Table II). None had blood-borne viral infections.
Table II.
The demographic and haemostatic findings in seven individuals with factor VII deficiency.
| Case | Age | Sex | F VII level (%) | Consanguineous | Epistaxis | Ecchymoses | Post dental extraction bleeding | GI bleeding | Menorrhagia | Post circumcision bleeding |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 74 | M | 5.8 | − | + | + | − | + | + | |
| 2 | 10 | M | 1 | − | + | + | + | − | − | |
| 3 | 13 | M | 1 | + | + | + | + | + | ||
| 4 | 10 | M | 1 | + | + | + | + | − | ||
| 5 | 33 | F | 35 | − | − | − | − | + | ||
| 6 | 23 | M | 1 | + | − | − | + | − | − | |
| 7 | 6 | M | 1 | + | − | + | −wf | + | +wf | |
| Total | 4 (57%) | 4 (57%) | 5 (71%) | 4 (80%)* | 3 (43%) | 1 (100%) |
Legend M: male; F: female; wf: with recombinant factor VII; GI: gastro-intestinal;
Percentage calculated on the basis of the number of patients who could have this bleeding complication.
Platelet disorders
There were 38 cases with platelet disorders. The youngest was a 3-year old child and the oldest was a 47-year old man. Their median age was 16 years old. Eighteen (47.4%) were adults and 20 (52.6%) were children. Twenty-five (65.8%) patients had a positive family history and 13 (34.2%) were sporadic cases. The mean time since the last use of platelets was 7±8.07 months. No individuals had undergone orthopaedic surgery. Four patients had been subjected to some type of surgery and three of these (75%) had bled during or after their operations. None of them had a history of blood-borne viral infections. The frequencies of bleeding manifestations were as follows: haemarthrosis 1 (2.6%), epistaxis 32 (84.2%), vast ecchymosis 36 (94.7%), haematuria 4 (10.5%), post-operative bleeding 3 (7.9%), menorrhagia 10 (26.3%), umbilical cord bleeding 3 (7.9%), 2 (5.4%) central nervous system bleeding, post-dental extraction bleeding 10 (90%), gastro-intestinal tract bleeding 4 (10.5%) and gum haemorrhage 17 (45.9%). None used orthopaedic aids.
Factor XIII deficiency
There were 11 cases with factor XIII deficiency: the youngest was a 7-year old male and the oldest were two 42-year old women. The median of age of patients with factor XIII deficiency was 20 years. Six patients (54.5%) had a positive family history, while five cases (45.5%) were sporadic. Eight (72.7%) came from consanguineous marriages, whereas the parents of the other three cases (27.3%) were not related. The mean time since last use of cryoprecipitate was 8.4 months. Two of the 11 patients with factor XIII deficiency had undergone surgery (Table III): case 1 had had a caesarean section and appendectomy, while case 10 underwent surgical removal of an ovarian cyst. In both cases cryoprecipitate was used and the patients did not have abnormal bleeding. Two women had had abortions (cases 4 and 5) which had been followed by severe bleeding subsequently controlled by cryoprecipitate infusion. Other demographic and haemostatic data are presented in Table III. None had blood-borne viral infections.
Table III.
The demographic and haemostatic findings in 11 individuals with factor XIII deficiency.
| Case | Age (year) | Sex | Family | Ecchymoses | Cord blood bleeding | Epistaxis | Post dental extraction bleeding | Haemarthrosis | CNS bleeding | Haematuria | Menorrhagia |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 28 | F | 1 | + | − | − | − | + | − | − | − |
| 2 | 17 | M | 1 | + | + | − | + | − | − | ||
| 3 | 42 | F | 2 | + | − | + | − | − | + | + | + |
| 4 | 29 | F | 3 | + | + | − | + | − | + | − | + |
| 5 | 28 | F | 4 | + | − | − | + | − | − | − | + |
| 6 | 15 | F | 5 | + | + | − | + | − | − | − | |
| 7 | 7 | M | 6 | − | + | + | + | − | − | − | |
| 8 | 9 | M | 6 | + | + | − | − | + | − | ||
| 9 | 42 | F | 7 | + | + | − | − | − | − | − | − |
| 10 | 21 | F | 7 | − | + | + | − | − | − | − | − |
| 11 | 9 | M | 8 | + | + | − | − | + | − | − | |
| Total | 9 (82%) | 8 (73%) | 3 (27%) | 3 (27%) | 4 (36%) | 3 (27%)* | 1 (9%) | 3 (43%)* |
Legend F: female; M: male; CNS: central nervous system;
Percentages calculated on the basis of the number of patients who could have this bleeding complication.
Factor XI deficiency
There were two patients with factor XI deficiency. These two patients were brothers who were 12 and 9 years old. The factor XI level was 2% in the elder boy and 11% in the younger one. The discrepancy between factor XI plasma concentrations in the two brothers seems to be due to inadequate laboratory assessment. The parents of these boys were not consanguineous. The elder boy had a history of spontaneous gastrointestinal tract bleeding and haemorrhage after tooth extraction, while the younger one had had epistaxis. The elder boy had undergone circumcision using FFP without bleeding while the younger boy was circumcised without FFP and without bleeding. Neither had blood-borne viral infections.
Afibrinogenaemia
There were two cases with afibrinogenaemia. The younger was a 17-year old female and the elder was a 30-year old man. Neither had a positive family history and neither came from a consanguineous marriage. Both of them had used cryoprecipitate within the preceding month. The female had a history of ecchymoses, menorrhagia and bleeding after tooth extraction, while the male had a history of ecchymoses and haemarthrosis. He was using a walking stick because of his joint bleeds. Neither had a history of infection by blood-borne viruses.
Combined factor V and VIII deficiency
Overall, there were 28 individuals in our region with combined factor V and VIII deficiency. We have already reported the clinical characteristics of 22 of these cases in 2004 and 20069,16. The newly diagnosed cases comprise three females from one family and three males from three other unrelated families. Four cases (66.6%) were born of consanguineous marriages. The youngest new case was a 7-year old girl, while the oldest one was a 51-year old male. The mean age of the new cases was 24.33 years, while the median age was 26.5 years. Overall, 26 patients (81.2%) were adults, while six (18.8%) were children. The mean plasma levels of factor V and VIII were 7.6% and 13.4%, respectively. The commonest bleeding episodes were epistaxis (n=4, 66.6%), ecchymosis (n=4, 66.6%), bleeding after dental extractions (n=4, 66.6% but in 100% of patients in whom teeth were removed) and menorrhagia (n=2, 33.3%, but in both, i.e. 100%, of the adult women) (Table IV). One 27-year old female (case 3) had two caesarean sections. She had bleeding 50 days after the first caesarean, which was controlled successfully using factor VIII concentrate and FFP. She experienced severe bleeding 2 days after the second caesarean section, which required a total hysterectomy; the bleeding was controlled with FFP and factor VIII concentrate. Two bags of whole blood were used to correct the patient's anaemia and hypovolaemia. None of the patients had a history of infection with blood-borne viruses.
Table IV.
The demographic and haemostatic findings in five individuals with combined factor V and VIII deficiency.
| Case | Age | Family | Sex | Consang. marriage | FV level (%) | FVIII level (%) | Ecchymosis | Epistaxis | Menorrhagia | Haematoma | Haematuria | Post dental extraction bleeding | Post-operative bleeding | Haemarthrosis | Post trauma bleeding |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 7 | 1 | F | − | 5 | 5 | − | + | − | − | − | + | |||
| 2 | 26 | 1 | F | + | 4.6 | 5.5 | + | − | + | − | − | + | − | ||
| 3 | 27 | 1 | F | + | 6 | 5 | + | + | + | + | − | + | + | ||
| 4 | 12 | 2 | M | + | 3 | 40 | + | + | + | − | + | + | + | ||
| 5 | 23 | 3 | M | + | 17 | 13 | − | + | − | + | + | − | |||
| 6 | 51 | 4 | M | − | 10 | 12 | + | − | − | − | + | + | + | ||
| Total | 4 | 4 (66.6%) | 4 (66.6%) | 4 (66.6%) | 2 (100%)* | 2 (33.3%) | 1 (16.6%) | 4 (100%)* | 2 (100%)* | 3 (50%) | 2 (100)* |
Legend FV: factor V level, FVIII: factor VIII level, F: female, M: male, consang. marriage: consanguineous marriage.
Percentage calculated on the basis of the number of patients who could have this bleeding complication.
Factor X deficiency
There were two cases with factor X deficiency. Both were males. One was 9 years old, the other 56 years old. Their factor X levels were <1%. They were both offspring of first degree consanguineous marriages. The 9-year old boy had a history of umbilical cord bleeding and two episodes of central nervous system bleeding at the age of 26 days and 3 months. He had survived them without any sequelae using infusions of factor X concentrate. The 56-year old male had experienced ecchymoses, haematuria, haemarthrosis, haemorrhage after tooth extraction and gastrointestinal tract bleeding. Neither of these patients had infections with blood-borne viruses.
Discussion
About 84% of the population on the earth live in countries with low or middle income and have 93% of the world's illnesses, while they access 18% of the total income and 11% of global health expenditure3. Bleeding disorders account for a notable part of the various diseases in developing countries, in which the rate of consanguineous marriages is high. Indeed, the prevalence of rare bleeding disorders is 10-fold higher in these countries than in developed countries17.
With the improvement of medical facilities, the number of individuals with haemophilia who survive to parenthood (over 19 years old) has increased5,18. The annual reports of the World Federation of Haemophilia (WFH) give an idea about the rising prevalence of haemophilia over time in 80% of countries1. Identification and quantification of affected individuals are essential in order to plan and deliver care services for patients with bleeding disorders19,20.
Health care providers in developing countries may need to remember that care expenses are greater in haemophiliacs who receive insufficient treatment because of the sequelae of undertreatment which include severe pain, muscle and/or joint bleeds potentially leading to permanent disability and loss of function, or even death in childhood or early adulthood.
According to our census of Haemophilia centres, about 8,000 individuals with bleeding disorders are registered in Iran. The provinces of Tehran, Khorasan and Isfahan are those with the greatest numbers of affected individuals (Figure 1).
We evaluated a total of 552 cases with inherited bleeding disorders in our survey. We certainly believe that this is not the real number of bleeders in our area. We expect that there are more than 1,000 cases in greater Khorasan. The lack of haemostatic facilities (in terms of both equipment and experienced staff) may be a major handicap to their identification. It is estimated that 90% of individuals with haemophilia are diagnosed in developed countries, while in some developing countries only 5% of affected cases have been identified and there is no national registry system3. The Ministry of Health in Iran recently established a national registry of bleeding disorders. Although it is in the early stage of completing the registration of affected individuals by various centres, in the future it will fill many gaps in the knowledge about various inherited bleeding disorders.
As far as regards phenotypic subtypes of HA, it is estimated that 43–70% of patients have the severe form, 15–26% have moderate disease and that 15–31% have a mild phenotype. Our findings were consistent with this, with the phenotype of our patients being severe in 143 (49.8%), moderate in 59 (20.6%) and mild in 65 (29.6%) of the individuals with HA and severe (46.7%), moderate (35.9%) and mild (17.4%) in those with HB. About 82.9% of affected subjects with HA had a positive family history. This shows that there is a lack of premarital genetic consultation for members of haemophiliacs' families. It is evident that the detection of carriers and antenatal diagnosis in early pregnancy could reduce the incidence of haemophiliacs and is an accessible solution. Self-infusion of concentrates by haemophiliacs is a potential skill that should be promoted and followed up by haemophilia centres. It enables more effective treatment of bleeding episodes, saves the use of coagulation factors and reduces the time spent in hospital. In the series discussed here, 52.4% of patients with HA and 47.8% of those with HB were independent of medical services for injection of the relevant coagulation concentrates. The patients with severe haemophilia were more likely than those with a moderate or mild form of the disease to have acquired this skill. This reflects the fact that patients with severe haemophilia require more infusions.
The commonest inherited bleeding disorder, in terms of prevalence, would be vWD21,22. However, in our series, vWD ranked third, affecting 50 patients. As the commonest phenotype of vWD is mild, many affected patients do not investigate their bleeding manifestations to make a diagnosis. Also we cannot determine subtypes of vWD in the current cases with vWD, this confirm our claim on lack of haemostasis facilities in our geographic area. The lack of subtyping in vWD may lead to inappropriate treatment and a waste of coagulation products. A review of the local literature revealed that the reported frequency of vWD was lower in central and west Iran. Most reports came from capital cities and there are no reports from towns23,24.
The commonest rare bleeding disorders were deficiencies of factor V, factor VII and combined factor V and VIII. This finding is not compatible with a report from the centre of Iran but is compatible to some extent with reports from the west of Iran24,25.
Acknowledgements
This study was done with the help of a grant from the Vice-Chancellor of Research in Mashhad University of Medical Sciences and with the permission of the local Ethics Committee. The authors would like to thank all individuals with bleeding disorders who participated in this survey.
Footnotes
The Authors declare no conflicts of interest.
References
- 1.Stonebraker JS, Bolton-Maggs PHB, Soucie J, et al. A study of variations in the reported haemophilia A prevalence around the word. Haemophilia. 2010;16:20–32. doi: 10.1111/j.1365-2516.2009.02127.x. [DOI] [PubMed] [Google Scholar]
- 2.El-Bostany EA, Omer N, Salama EE, et al. The spectrum of inherited bleeding disorders in pediatrics. Blood Coagul Fibrinolysis. 2008;19:771–5. doi: 10.1097/MBC.0b013e32830f1b99. [DOI] [PubMed] [Google Scholar]
- 3.Pinto MT, Ortiz Z. Haemophilia in developing world: success, frustrations and opportunities. Haemophilia. 2004;10:14–9. doi: 10.1111/j.1365-2516.2004.00986.x. [DOI] [PubMed] [Google Scholar]
- 4.Nathwani AC, Tuddenham EGD. Epidemiology of coagulation disorders. Bailliere's Clin Haematol. 1992;5:383–49. doi: 10.1016/s0950-3536(11)80025-9. [DOI] [PubMed] [Google Scholar]
- 5.O' Mahony B, Black C. Expanding hemophilia care in developing countries. Semin Thromb Hemost. 2005;31:561–8. doi: 10.1055/s-2005-922228. [DOI] [PubMed] [Google Scholar]
- 6.Skinner MW. WFH - the cornerstone of global development: 45 years of progress. Haemophilia. 2008;14:1–9. doi: 10.1111/j.1365-2516.2008.01707.x. [DOI] [PubMed] [Google Scholar]
- 7.Skinner MW. Building our global family-achieving treatment for all. Haemophilia. 2010;16(Suppl 5):1–10. doi: 10.1111/j.1365-2516.2010.02285.x. [DOI] [PubMed] [Google Scholar]
- 8.O' Mahony B. WFH: back to the future. Haemophilia. 2004;10:1–8. doi: 10.1111/j.1365-2516.2004.00981.x. [DOI] [PubMed] [Google Scholar]
- 9.Mansouritorghabeh H, Rezaieyazdi Z, Pourfathollah AA, et al. Haemorrhagic symptoms in patients with combined factors V and VIII deficiency in north-eastern Iran. Haemophilia. 2004;10:271–5. doi: 10.1111/j.1365-2516.2004.00890.x. [DOI] [PubMed] [Google Scholar]
- 10.Modaresi AR, Torghabeh MH, Pourfathollah AA, et al. Pattern of factor VIII inhibitor in patient with haemophilia A in the north east of Iran. Hematology. 2006;11:215–7. doi: 10.1080/10245330600667526. [DOI] [PubMed] [Google Scholar]
- 11.Mansouritorghabeh H, Pourfathollah AA, Rezaieyazdi Z. Coagulation therapy in hemophilia A and its relation with factor VIII inhibitor in northeastern Iran. Iranian J Med Sci. 2004;29:199. [Google Scholar]
- 12.Mansouritorghabeh H, Pourfathollah AA, Mahmoodian Shooshtari M, Rezaieyazdi Z. First survey of factor IX inhibitor in northeastern Iran. Med J Islamic Rep Iran. 2005;19:91–2. [Google Scholar]
- 13.Mansouritorghabeh H, Pourfathollah AA, Shooshtari M. Evaluation of the relationship between factor IX inhibitor in hemophilia B patients and different types of therapy in the north-eastern part of Iran. Iranian J Blood Cancer. 2009;1:83–6. [Google Scholar]
- 14.Mansouritorghabeh H, Manavifar L, Mobalegh A, Shirdel A. Haemorrhagic manifestations and prevalence of factor V deficiency in north-eastern Iran. Haemophilia. 2010;16:367–80. doi: 10.1111/j.1365-2516.2009.02139.x. [DOI] [PubMed] [Google Scholar]
- 15.Mansouritorghabeh H, Badiei Z, Noori F. Clinical pictures and prevalence of factor VII deficiency in Northeastern of Iran. Haemophilia. 2008;14:157–9. doi: 10.1111/j.1365-2516.2007.01568.x. [DOI] [PubMed] [Google Scholar]
- 16.Mansouritorghabeh H, Rezaieyazdi Z, Pourfathollah AA. Combined factor V and VIII deficiency: a new family and their haemorrhagic manifestation. Haemophilia. 2006;12:169–71. doi: 10.1111/j.1365-2516.2006.01177.x. [DOI] [PubMed] [Google Scholar]
- 17.Peyvandi F, Duga S, Akhavan S, Mannucci PM. Rare coagulation deficiencies. Haemophilia. 2002;8:308–21. doi: 10.1046/j.1365-2516.2002.00633.x. [DOI] [PubMed] [Google Scholar]
- 18.Karimi M, Rahmani S, Ardeshiri R, Pasalar M. Health status in Iranian haemophilia patients. Haemophilia. 2008;14:615–7. doi: 10.1111/j.1365-2516.2008.01696.x. [DOI] [PubMed] [Google Scholar]
- 19.Stonebraker JS, Brooker M, Amans RE, et al. A study of reported factor VIII use around the word. Haemophilia. 2010;16:33–46. doi: 10.1111/j.1365-2516.2009.02131.x. [DOI] [PubMed] [Google Scholar]
- 20.Daliri AA, Haghparast H, Mamikhani J. Cost-effectiveness of prophylaxis against on demand treatment in boys with severe hemophilia A in Iran. Int J Technol Assess Health Care. 2009;25:584–7. doi: 10.1017/S0266462309990420. [DOI] [PubMed] [Google Scholar]
- 21.Sirvastava A, Rodeghiero F. Epidemiology of von Willebrand disease in developing countries. Semin Thromb Hemost. 2005;31:569–76. doi: 10.1055/s-2005-922229. [DOI] [PubMed] [Google Scholar]
- 22.Rodeghiero F, Castaman G, Dini E. Epidemiological investigation of the prevalence of von Willebrand,s disease. Blood. 1987;69:545–9. [PubMed] [Google Scholar]
- 23.Karimi M, Yarmohammadi HI, Ardeshiri R, Yarmohammadi HO. Inherited coagulation disorders in southern Iran. Haemophilia. 2002;8:740–4. doi: 10.1046/j.1365-2516.2002.00699.x. [DOI] [PubMed] [Google Scholar]
- 24.Ziaei JE, Dolatkhah R, Dastgiri S, et al. Inherited coagulation disorders in the northwestern region of Iran. Haemophilia. 2005;11:424–6. doi: 10.1111/j.1365-2516.2005.01118.x. [DOI] [PubMed] [Google Scholar]
- 25.Mehdizadeh M, Kardoost M, Baghaeepour MR, et al. Occurrence of haemophilia in Iran. Haemophilia. 2009;15:348–51. doi: 10.1111/j.1365-2516.2008.01874.x. [DOI] [PubMed] [Google Scholar]