Abstract
High levels of antiretroviral therapy (ART) adherence are required to achieve optimal viral suppression. To better understand mechanisms associated with ART adherence, this study characterized demographic and social-cognitive correlates of ART adherence among HIV-infected individuals from a medium-sized, Northeastern U.S. city (n = 116; 42% female; 43% African-American). Participants completed an ACASI survey assessing demographics, social-cognitive constructs, and ART adherence; participants’ most recent viral load was obtained from their medical charts. Suboptimal ART adherence (taking less than 95% of prescribed medications during the past month) was reported by 39% of participants and was associated with being female, being a minority, and having a detectable viral load. In a hierarchical logistic regression analysis, greater than 95% ART adherence was associated with higher levels of adherence self-efficacy (AOR = 1.1; p = .015), higher perceived normative beliefs about the importance of ART adherence (AOR = 1.3; p = .03), and lower concern about missing ART doses (AOR = .63; p = .002). Adherence did not differ based on ART outcome expectancies, ART attitudes, or the perceived necessity of ART. In fact, most participants endorsed positive attitudes and expectancies regarding the need for and effectiveness of ART. Taken together, results indicate that sub-optimal adherence remains high among HIV-infected minority women, a sub-population that experiences particularly high rates of chronic stress due to both illness specific stressors and broader environmental stressors. Consistent with Social-Cognitive Theory, adherence problems in our sample were linked with deficits in self-efficacy as well as perceived norms and behavioral intentions that do not support a goal of 100% adherence. We suggest that interventions to improve adherence informed by Social-Cognitive theory to a) target patients who are at risk for adherence problems, b) provide a supportive environment that promotes high-rates of adherence, and c) address inaccurate beliefs regarding optimal adherence levels.
Keywords: Social-Cognitive Theory, antiretroviral medication adherence, antiretroviral medication adherence self-efficacy, antiretroviral medication adherence outcome expectancies
Despite increased HIV prevention efforts, rates of new infections remain relatively stable, with approximately 50,000 new HIV infections diagnosed in the United States (US) annually (Prejean et al., 2011) and more than 1 million individuals living with HIV in the US (CDC, 2010). Antiretroviral therapy (ART) has improved the longevity of HIV-infected individuals and markedly decreased HIV-related mortality (Palella et al., 1998; Schackman et al., 2006). However, ART medications require high levels of adherence to maintain viral suppression and prevent the development of drug-resistant HIV strains (Balfour et al., 2006; Clavel & Hance, 2004; Paterson et al., 2000). While optimal ART adherence rates vary by drug type (Bangsberg, 2006; Bangsberg, Kroetz, & Deeks, 2007), an adherence level of 95% or greater is consistently associated with optimal viral suppression across ART drug types (Krakovska & Wahl, 2007; Low-Beer, Yip, O’Shaughnessy, Hogg, & Montaner, 2000; Paterson, et al., 2000).
Since suboptimal ART adherence increases the risk for negative health outcomes, efforts to identify factors associated with adherence are urgently needed. Diverse correlates of ART adherence have been examined, including demographic characteristics (Barclay et al., 2007; Kamau, Olson, Zipp, & Clark, 2011), mental health or substance use difficulties (Murphy, Greenwell, & Hoffman, 2002; Reynolds et al., 2004), psychosocial functioning (e.g., social support; Finocchario-Kessler et al., 2011; Simoni, Frick, Lockhart, & Liebovitz, 2002), and other health conditions (e.g., co-morbid pain; Berg, Cooperman, Newville, & Arnsten, 2009). Prominent theoretical frameworks to explain ART adherence include the Information-Motivation-Behavior model (Fisher, Fisher, Amico, & Harman, 2006), Social Problem Solving framework (Johnson, Elliott, Neilands, Morin, & Chesney, 2006), and the Stress and Coping model (Johnson, Heckman, Hansen, Kochman, & Sikkema, 2009). Additionally, there is a growing literature examining the extent to which core constructs from Social-Cognitive Theory (Bandura, 1977; Bandura, 2004) are associated with ART adherence.
Social-Cognitive Theory (SCT) postulates that personal characteristics, social interactions, and behavioral factors interactively determine health behavior engagement (Bandura, 2004). Central to SCT is self-efficacy, or one’s confidence in his/her ability to engage in a particular behavior under various circumstances (Bandura, 1977). Self-efficacy has been studied as a correlate of ART adherence, with greater self-efficacy levels to consistently take ART medications associated with better ART adherence (Barclay, et al., 2007; Catz, Kelly, Bogart, Benotsch, & McAuliffe, 2000; Fumaz et al., 2008; Gifford et al., 2000; Godin, Cote, Naccache, Lambert, & Trottier, 2005; Murphy, et al., 2002; Rudy, Murphy, Harris, Muenz, & Ellen, 2010; Simoni, Frick, & Huang, 2006). Outcome expectancies, defined as an individual’s appraisal of potential consequences for a behavior, influence whether a behavior is performed or not (Bandura, 2004). Expectancies for negative ART outcomes (e.g., medication side effects) have been linked to poor adherence (Catz, et al., 2000; Murphy, et al., 2002; Rudy, et al., 2010). SCT suggests that individuals with greater self-efficacy and positive outcome expectancies will influence one’s beliefs and attitudes towards a behavior (Bandura, 2004). For instance, positive medication attitudes have been associated with improved ART adherence (Godin, et al., 2005). Moreover, more permissive attitudes about the importance of ART adherence may be indicative of a higher vulnerability for suboptimal adherence (Malcolm, Ng, Rosen, & Stone, 2003).
While a number of studies have examined individual SCT constructs (e.g., self-efficacy) as correlates of ART adherence, there is a dearth of empirical research examining the application of a broader set of SCT constructs to ART adherence. To our knowledge, only a single study has evaluated the utility of a comprehensive SCT model of ART adherence (DiIorio et al., 2009). In addition to modeling the relationship between self-efficacy and outcome expectancies to ART adherence, DiIorio and colleagues examined the role of depression levels and related psychosocial constructs (e.g., stigma). Self-efficacy and depression were directly related to ART adherence; related constructs (i.e., stigma, patient satisfaction, social support) were indirectly linked to ART adherence via self-efficacy or depression (DiIorio, et al., 2009). While this study highlights the role of depression and other psychosocial factors in relationship to ART adherence, there is a need to further examine the extent to which core SCT constructs (i.e., self-efficacy, outcome expectancies) and related attitudes, beliefs, and norms are associated with ART adherence.
Thus, to better understand mechanisms associated with ART adherence, this study examined social-cognitive factors associated with ART adherence among HIV-infected individuals. Consistent with SCT, we predicted that greater ART adherence self-efficacy and positive outcome expectancies would be associated with higher ART adherence levels. This study also examined demographic differences in ART adherence and the association between ART adherence and participants’ health status.
Methods
Procedures
Participant recruitment
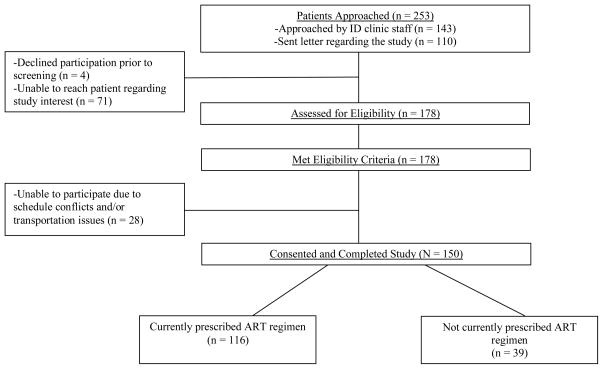
Patients were recruited during outpatient medical visits at a University-based Infectious Disease (ID) Clinic in Syracuse, New York, a mid-sized Northeastern city, or via letter for patients who participated in prior studies and agreed to be re-contacted. Figure 1 provides a CONSORT diagram of participant recruitment and enrollment. Patients were informed that participation involved completing a computerized survey of HIV-related health practices. Eligibility requirements for this study were: (a) receiving outpatient care at the ID clinic; (b) 18 years or older; (c) English-speaking; and (d) medically and cognitively capable of participation. For this study, analyses were limited to participants reporting current ART use (N = 116). All participants provided written informed consent and were compensated $20 for their time and travel. All study procedures were approved by the Institutional Review Boards of the participating institutions.
Figure 1.
CONSORT Diagram for participant recruitment and study completion.
Survey administration
The questionnaire battery was administered using audio computer-assisted self-interviewing (ACASI) in a private assessment room. The survey took approximately one hour to complete (range: 45 minutes-2 hours).
Measures
Demographic characteristics
Participants reported their gender, ethnicity, age, current employment status, annual income, and the number of years since receiving their HIV diagnosis.
Medical chart data
Medical chart data collected included: (a) current ART regimen medications; (b) number of ART pills prescribed; (c) most recent viral load (undetectable: < 50 copies RNA/mL or detectable: > 50 copies RNA/mL); and (d) medical providers’ notation of any ART-associated adherence problems (yes/no).
ART adherence
The measure of ART adherence was informed by a review of self-report ART adherence measurement (Simoni et al., 2006). Participants reported their level of ART adherence during the past month by completing a visual analog scale (0 to 100%) in which they rated how much of their HIV medications they took. Responses were dichotomized to reflect optimal (i.e., taking 95–100% of ART doses; coded as 1) versus suboptimal (i.e., taking less than 95% of ART doses; coded as 0) adherence levels.
ART adherence self-efficacy
ART adherence self-efficacy was measured by a 12-item scale (Johnson et al., 2007). Participants rated their confidence to maintain ART adherence in different situations (e.g., “Stick to your treatment schedule even when your daily routine is disrupted”) from 1 (not confident at all) to 4 (completely confident I can do it). A total score across items was calculated, with higher scores indicating greater levels of ART adherence self-efficacy (α = 1.0).
ART outcome expectancies
Six items were developed for the present study to assess outcome expectancies for ART on long-term health outcomes. A sample item includes, “If you did not take your HIV medications as they are prescribed to you, how likely is it that your immune system would get weaker?” Participants rated their outcome expectancies from 1 (not at all likely) to 4 (very likely) with scores summed across items. Higher scores were indicative of more negative outcome expectancies for ART non-adherence (α = .73).
Attitudes towards ART non-adherence
Eleven items assessed participants’ attitudes and beliefs about ART adherence. Items measured beliefs reflecting permissive attitudes toward adherence and the perceived risks of non-adherence (e.g., “Some people make a big deal about taking HIV medications “perfectly,” but it really isn’t that important.”) For each item, participants indicated the extent to which they agreed or disagreed using a 6-point Likert scale with response options ranging from “Strongly Agree” to “Strongly Disagree.” Higher scores on this measure were indicative of greater perceived risks of non-adherence (α = .64).
Perceived necessity of ART
Participants’ beliefs regarding the perceived necessity of ART were measured with an 8-item scale (Horne et al., 2004; Horne, Cooper, Gellaitry, Date, & Fisher, 2007). A sample item includes, “My health in the future depends on HIV medications.” Participants rated their agreement with each statement from 1 (strongly disagree) to 6 (strongly agree). A total score was calculated, with higher scores indicating greater perceived ART necessity (α = .80).
ART adherence normative beliefs
Two items assessed perceived norms surrounding optimal ART adherence levels. First, participants identified what they believe is an optimal rate of adherence (i.e., “Based on what you personally believe, not just what your doctor tells you, what is a good rate of adherence?”); participants provided a rating from 0 to 100%. Second, participants reported on the number missed ART doses that would be of concern out of 10 possible future doses; participants provided a number between 0 and 10 for their response (Graham, Bennett, Holmes, & Gross, 2007).
Data Analyses
Descriptive statistics were calculated to describe social-cognitive factors, current ART adherence levels, and related health status variables. Next, bivariate analyses compared participants who endorsed optimal ART adherence levels (i.e., taking 95–100% of prescribed ART doses in the past month) and those who endorsed suboptimal adherence levels (i.e., taking less than 95% of prescribed doses in the past month) on demographic characteristics and health status variables. Bivariate analyses then examined differences in social-cognitive constructs between the optimal and suboptimal adherence groups. Independent samples t-tests examined differences between groups for continuous variables and chi-square analyses examined differences between groups for categorical outcomes. Social-cognitive factors significantly associated with adherence levels at the bivariate level (p < .10) were then entered into a multivariate, logistic regression analysis, controlling for significant demographic differences and ART regimen characteristics between groups.
Results
Participant Characteristics
HIV-infected individuals (N = 116; 40% female, 58% male, 2% transgender) participated in the study, with 43% self-identifying as African-American, 47% Caucasian, 4% American Indian or Alaskan Native, 2% Native Hawaiian or Other Pacific Islander, and 4% as Multiracial. 10% of participants identified as Hispanic. Participants’ ages ranged between 21 and 64 (M age = 45.3, SD = 8.6). Sixty-two percent were unemployed, and 63% reported a yearly income of less than $10,000. The average number of years since being diagnosed with HIV was 12.3 years (SD = 6.2).
Descriptive Statistics
Sixty-one percent had taken ART for more than 7 years and 7% for less than one year. Medical chart data reflected that participants were prescribed an average of 2.6 ART pills per day (SD = .96, range = 1–5). According to participants’ medical charts, 72% had an undetectable viral load and 28% had a detectable viral load at their last medical visit. Medical providers noted ART adherence problems in the medical charts of 48% of participants. Participants reported taking an average of 89.7% of their prescribed ART medications during the past month (SD = 18.3; range = 0–100). Suboptimal ART adherence (i.e., taking less than 95% of prescribed medications during the past month) was reported by 39% of participants. Table 1 provides descriptive statistics for SCT constructs. On average, participants reported the perception that, regardless of what their doctor tells them, an optimal rate of adherence is 94%, (range = 50–100; SD=13.6). Of a possible 10 doses, participants indicated that 2.2 missed ART doses (range = 0–10; SD = 2.7) would be of concern.
Table 1.
Descriptive Statistics for Social-Cognitive Constructs (N = 116)
| M (SD) | Median | IQRa | Rangeb | Possible Rangec | |
|---|---|---|---|---|---|
| ART adherence self-efficacy | 40.9 (7.8) | 44.0 | 11.0 | 12–48 | 12–48 |
| ART outcome expectancies | 20.8 (3.7) | 22.5 | 6.0 | 10–24 | 6–24 |
| Attitudes towards ART non-adherence | 46.1 (8.2) | 46.5 | 9.75 | 21–66 | 11–66 |
| Perceived necessity of ART | 42.9 (5.6) | 44.6 | 8.0 | 13.7–48 | 8–48 |
| ART adherence normative beliefs | |||||
| Optimal rate of ART adherence | 94.0 (13.6) | 100.0 | 4.5 | 50–100 | 0–100 |
| Number of missed ART doses | 2.2 (2.7) | 1.0 | 3.0 | 0–10 | 0–10 |
Note:
Interquartile range;
Range of obtained scores;
Range of possible scores for each measure.
Differences in Adherence Levels by Sociodemographic Characteristics and Health Status Variables
First, bivariate analyses examined potential differences in adherence levels by demographic characteristics and health status variables (see Table 2). Women and racial minorities were more likely to endorse suboptimal ART adherence than men and Caucasian individuals. There were no differences in adherence by age, current employment status, or monthly income. Participants reporting optimal adherence levels were more likely to have an undetectable viral load at their last medical appointment, were more likely to report being on ART for fewer years, and were taking fewer ART pills than individuals with lower adherence levels.
Table 2.
ART Adherence Levels by Demographic Characteristics and Health Status Variables (N = 116)
| Suboptimal ART Adherencea (n = 45) | Optimal ART Adherenceb (n = 71) | Test Statistic | |
|---|---|---|---|
| Demographic characteristics | |||
| Age | 45.6 (8.1) | 45.2 (8.9) | t (114) = .29, p = .77 |
| Female gender | 26 (57.8%) | 23 (32.4%) | χ2 = 7.3, p = .02 |
| Racial minority | 31 (68.9%) | 31 (43.7%) | χ2 = 7.0, p = .01 |
| Currently employed | 15 (33.3%) | 29 (40.8%) | χ2 = .66, p = .44 |
| Monthly income less than $850 | 28 (62.2%) | 37 (52.1%) | χ2 = 1.34, p = .25 |
| Health status variables | |||
| Detectable viral load at last medical visit | 19 (42.2%) | 13 (18.3%) | χ2 = 7.9, p = .006 |
| Years on ART medication | 7.0 (1.8) | 5.9 (2.6) | t (114) = 2.5, p = .015 |
| Number of daily ART pills | 2.9 (.81) | 2.4 (1.0) | t (112) = 3.0, p = .003 |
Note: Means (standard deviations) are presented for continuous variables. Frequencies (corresponding percentage) are presented for dichotomous outcomes. Independent samples t-tests were used to assess differences between continuous variables. χ2 analyses were used to assess differences in dichotomous outcomes.
Suboptimal ART adherence is defined as taking less 95% of prescribed ART medications during the past month.
Optimal ART adherence is defined as 95% or greater percent of prescribed ART medications during the past month.
Social-Cognitive Correlates of ART Adherence
Bivariate analyses
First, bivariate analyses examined differences in social-cognitive constructs between individuals with suboptimal ART adherence and those with optimal ART adherence levels (see Table 3). Participants with optimal adherence levels endorsed: (a) greater ART adherence self-efficacy; (b) more negative outcome expectancies for ART non-adherence; (c) greater perceived risk of ART non-adherence; (d) greater perceived need for ART; (e) higher levels of optimal ART adherence; and (f) fewer number of missed ART doses that would be of concern.
Table 3.
ART Adherence Status as a function of Social-Cognitive Constructs (N = 116): Bivariate Results
| Suboptimal ART Adherencea (n = 45) | Optimal ART Adherenceb (n = 71) | Test Statistic | |
|---|---|---|---|
| ART adherence self-efficacy | 35.9 (9.0) | 43.9 (5.1) | t (112) = −6.1, p < .001 |
| ART outcome expectancies | 19.4 (4.0) | 21.7 (3.2) | t (114) = −3.4, p = .001 |
| Attitudes towards ART non-adherence | 44.1 (7.3) | 47.4 (8.5) | t (114) = −2.1, p = .039 |
| Perceived necessity of ART | 41.3 (6.9) | 43.9 (4.4) | t (114) = −2.1, p = .014 |
| ART adherence normative beliefs | |||
| Optimal rate of ART adherence | 86.2 (19.3) | 99.1 (2.3) | t (114) = −5.6, p < .001 |
| Number of missed ART doses | 3.3 (3.1) | 1.5 (2.1) | t (114) = 3.7, p < .001 |
Note: Means (standard deviations) are presented for continuous variables. Independent samples t-tests were used to assess differences between continuous variables.
Suboptimal ART adherence is defined as taking less 95% of prescribed ART medications during the past month.
Optimal ART adherence is defined as 95% or greater percent of prescribed ART medications during the past month.
Multivariate analyses
Table 3 displays results from a hierarchical logistic regression analysis controlling for participant gender, ethnicity, years on ART, and number of daily ART pills. Greater than 95% ART adherence was associated with higher levels of adherence self-efficacy (AOR = 1.1, 95% CI = 1.02–1.2), higher perceived normative beliefs about the importance of ART adherence (AOR = 1.3, 95% CI = 1.02–1.5), and fewer acceptable missed ART doses (AOR = .63, 95% CI = .47-.85). Adherence level did not differ based on ART outcome expectancies, ART attitudes, or the perceived necessity of ART. The overall model (χ2 = 75.70; p < .001) indicated a high goodness-of-fit with the data.
Discussion
Findings reflect elevated rates of suboptimal adherence among an outpatient sample of HIV-infected individuals. More than one-third of participants endorsed suboptimal ART adherence during the past month, which may not maintain adequate viral suppression (Paterson, et al., 2000). Indeed, lower adherence levels were associated with having a detectable viral load at the last medical appointment. Suboptimal ART adherence increases the risk for adverse health outcomes and accelerated disease progression, underscoring the need to better understand mechanisms that may underlie poor adherence.
Suboptimal adherence was more common among women, a finding consistent with a recent review indicating lower ART adherence rates among HIV-infected women relative to men (Puskas et al., 2011). However, the relationship between gender and ART adherence has been inconsistent with other studies finding no difference in ART adherence levels by gender (Ammassari et al., 2002). Additionally, HIV-infected minority individuals also endorsed lower levels of adherence. This finding is consistent with the broader literature suggesting disparities in HIV treatment and health outcomes among racial minorities (Cargill, Stone, & Robinson, 2004). Poor adherence among women and minority individuals living with HIV is an important and long-standing problem. Efforts to achieve and sustain optimal adherence in these vulnerable groups indicate that intervention approaches must be comprehensive and intensive (Holstad, DiIorio, Kelley, Resnicow, & Sharma, 2011; Simoni, Pantalone, Plummer, & Huang, 2007).
An examination of SCT correlates indicated that ART adherence was associated with higher levels of adherence self-efficacy. Greater confidence in one’s ability to maintain consistent ART adherence has been linked to higher ART adherence across a number of studies (Barclay, et al., 2007; Catz, et al., 2000; DiIorio, et al., 2009; Fumaz, et al., 2008), highlighting the importance of self-efficacy as a predictor of consistent adherence. This finding underscores the need to assess ART adherence self-efficacy within ongoing HIV care and provide intervention approaches to improve patients’ ability and confidence to maintain optimal levels of ART adherence. Patients who expressed the personal belief for lower levels of optimal ART adherence were more likely to report suboptimal adherence. Similarly, participants who reported lower levels of concern with a greater number of missed ART doses were also more likely to report poor adherence. Collectively, these two findings are of importance for patient-provider interactions. Care providers should understand that patients may develop their own personal beliefs about optimal adherence rates that differ from those provided by care providers. This suggests that providers should take time to assess patients’ personal beliefs about ART adherence and address inaccurate beliefs regarding optimal ART adherence levels.
Contrary to expectations, adherence levels did not vary as a function of ART outcome expectancies and a measure of broader attitudes toward ART. Prior studies of ART outcome expectancies have produced mixed results. Several studies showed an association between positive outcome expectancies and better ART adherence (Catz, et al., 2000; Murphy, et al., 2002; Rudy, et al., 2010) and one suggests that outcome expectancies were not directly related to adherence (DiIorio, et al., 2009). Differences in assessment measures and ceiling effects may account for some of the inconsistency in the relationship between outcome expectancies and adherence behavior.
Limitations
This study is limited by its cross-sectional design. Thus, we could not examine the longitudinal impact of social-cognitive constructs on ART adherence and overall health functioning. Additionally, our measure of ART adherence relied upon self-report data, which has inherent limitations (Simoni, Kurth, et al., 2006), and focused on a single adherence level (i.e., 95% or greater adherence levels) over the course of the past month, which may not be representative of ART adherence patterns. Lower required levels of adherence to achieve viral suppression for specific regimen classes have been reported (Bangsberg, 2006; Bangsberg, et al., 2007) and thus our cut-off adherence level may have been overly conservative for some prescribed regimens. Additionally, measures of CD4 and viral load were collected from chart reviews of the last medical visit and thus were not collected at the same time as the self-reported adherence measure for all participants. Lastly, this sample consisted of HIV-infected individuals recruited from a medium-sized, Northeastern city. Therefore, results may not generalize to the broader HIV-infected population.
Conclusions
Consistent with SCT, adherence problems in our sample were linked with deficits in self-efficacy as well as beliefs that do not support a goal of 100% adherence. SCT provides a framework for identifying patients at high risk for adherence problems and designing comprehensive behavioral interventions to increase ART adherence among HIV-infected individuals. According to SCT, the link between health-related cognitions (i.e., beliefs and intentions) and actual behavior are self-regulatory processes and skills (Bandura, 2005). Thus, future SCT-informed interventions should target maladaptive adherence-related cognitions, address skills to maintain consistent adherence, enhance self-efficacy, and improve self-regulation skills that facilitate the translation of positive intentions into sustained behavior. Additionally, promotion of positive provider interactions surrounding adherence may bolster adherence self-efficacy (Johnson et al., 2006).
Table 4.
Social-Cognitive Correlates of ART Adherence Level (N = 116): Logistic Regression Results
| Predictor | Odds Ratio (SE) | 95% CI | p-value |
|---|---|---|---|
| Demographic characteristics | |||
| Female gender | .28 (.69) | .07, 1.1 | .06 |
| Caucasian | 3.2 (.67) | .86, 12.1 | .08 |
| ART regimen | |||
| Years on ART medication | .78 (.18) | .55, 1.1 | .17 |
| Number of daily ART pills | .48 (.37) | .23, .99 | .05 |
| Social-cognitive constructs | |||
| ART adherence self-efficacy | 1.1 (.05) | 1.02, 1.2 | .015 |
| ART outcome expectancies | 1.1 (.09) | .89, 1.3 | .35 |
| Attitudes towards ART non-adherence | .95 (.04) | .88, 1.0 | .19 |
| Perceived necessity of ART | 1.0 (.05) | .95, 1.2 | .33 |
| ART adherence normative beliefs | |||
| Optimal rate of ART adherence | 1.3 (.10) | 1.02, 1.5 | .03 |
| Number of missed ART doses | .63 (.15) | .47, .85 | .002 |
Notes: CI: Confidence Interval
References
- Ammassari A, Trotta MP, Murri R, Castelli F, Narciso P, Noto P, Antinori A. Correlates and predictors of adherence to highly active antiretroviral therapy: overview of published literature. Journal Of Acquired Immune Deficiency Syndromes. 2002;31(Suppl 3):S123–S127. doi: 10.1097/00126334-200212153-00007. [DOI] [PubMed] [Google Scholar]
- Balfour L, Kowal J, Silverman A, Tasca GA, Angel JB, Macpherson PA, Cameron DW. A randomized controlled psycho-education intervention trial: Improving psychological readiness for successful HIV medication adherence and reducing depression before initiating HAART. AIDS Care. 2006;18(7):830–838. doi: 10.1080/09540120500466820. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. URL http // www.apa.org/journals/rev.html. [DOI] [PubMed] [Google Scholar]
- Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- Bandura A. The primacy of self-regulation in health promotion. Applied Psychology: An International Review. 2005;54(2):245–254. [Google Scholar]
- Bangsberg DR. Less than 95% adherence to nonnucleoside reverse-transcriptase inhibitor therapy can lead to viral suppression. Clinical Infectious Diseases: An Official Publication Of The Infectious Diseases Society Of America. 2006;43(7):939–941. doi: 10.1086/507526. [DOI] [PubMed] [Google Scholar]
- Bangsberg DR, Kroetz DL, Deeks SG. Adherence-resistance relationships to combination HIV antiretroviral therapy. Curr HIV/AIDS Rep. 2007;4(2):65–72. doi: 10.1007/s11904-007-0010-0. [DOI] [PubMed] [Google Scholar]
- Barclay TR, Hinkin CH, Castellon SA, Mason KI, Reinhard MJ, Marion SD, Durvasula RS. Age-associated predictors of medication adherence in HIV-positive adults: Health beliefs, self-efficacy, and neurocognitive status. Health Psychology. 2007;26(1):40–49. doi: 10.1037/0278-6133.26.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg KM, Cooperman NA, Newville H, Arnsten JH. Self-efficacy and depression as mediators of the relationship between pain and antiretroviral adherence. AIDS Care. 2009;21(2):244–248. doi: 10.1080/09540120802001697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cargill VA, Stone VE, Robinson MR. HIV treatment in African Americans: Challenges and opportunities. Journal of Black Psychology. 2004;30(1):24–39. doi: 10.1177/0095798403259243. [DOI] [Google Scholar]
- Catz SL, Kelly JA, Bogart LM, Benotsch EG, McAuliffe TL. Patterns, correlates, and barriers to medication adherence among persons prescribed new treatments for HIV disease. Health Psychology: Official Journal Of The Division Of Health Psychology, American Psychological Association. 2000;19(2):124–133. [PubMed] [Google Scholar]
- CDC. HIV Surveillance Report, 2008. 2010 Retrieved August 16, 2010, from http://www.cdc.gov/hiv/topics/surveillance/resources/reports/
- Clavel F, Hance AJ. HIV drug resistance. The New England Journal Of Medicine. 2004;350(10):1023–1035. doi: 10.1056/NEJMra025195. [DOI] [PubMed] [Google Scholar]
- DiIorio C, McCarty F, Depadilla L, Resnicow K, Holstad MM, Yeager K, Lundberg B. Adherence to antiretroviral medication regimens: a test of a psychosocial model. AIDS and Behavior. 2009;13(1):10–22. doi: 10.1007/s10461-007-9318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finocchario-Kessler S, Catley D, Berkley-Patton J, Gerkovich M, Williams K, Banderas J, Goggin K. Baseline predictors of ninety percent or higher antiretroviral therapy adherence in a diverse urban sample: the role of patient autonomy and fatalistic religious beliefs. AIDS Patient Care and STDs. 2011;25(2):103–111. doi: 10.1089/apc.2010.0319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA, Amico KR, Harman JJ. An information-motivation-behavioral skills model of adherence to antiretroviral therapy. Health Psychology. 2006;25(4):462–473. doi: 10.1037/0278-6133.25.4.462. [DOI] [PubMed] [Google Scholar]
- Fumaz CR, Munoz-Moreno JA, Molto J, Ferrer MJ, Lopez-Blazquez R, Negredo E, Clotet B. Sustained antiretroviral treatment adherence in survivors of the pre-HAART era: attitudes and beliefs. AIDS Care. 2008;20(7):796–805. doi: 10.1080/09540120701694022. [DOI] [PubMed] [Google Scholar]
- Gifford AL, Bormann JE, Shively MJ, Wright BC, Richman DD, Bozzette SA. Predictors of self-reported adherence and plasma HIV concentrations in patients on multidrug antiretroviral regimens. Journal Of Acquired Immune Deficiency Syndromes. 2000;23(5):386–395. doi: 10.1097/00126334-200004150-00005. [DOI] [PubMed] [Google Scholar]
- Godin G, Cote J, Naccache H, Lambert LD, Trottier S. Prediction of adherence to antiretroviral therapy: A one-year longitudinal study. AIDS Care. 2005;17(4):493–504. doi: 10.1080/09540120412331291715. [DOI] [PubMed] [Google Scholar]
- Graham J, Bennett IM, Holmes WC, Gross R. Medication beliefs as mediators of the health literacy-antiretroviral adherence relationship in HIV-infected individuals. AIDS and Behavior. 2007;11(3):385–392. doi: 10.1007/s10461-006-9164-9. [DOI] [PubMed] [Google Scholar]
- Holstad MM, DiIorio C, Kelley ME, Resnicow K, Sharma S. Group motivational interviewing to promote adherence to antiretroviral medications and risk reduction behaviors in HIV infected women. AIDS and Behavior. 2011;15(5):885–896. doi: 10.1007/s10461-010-9865-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horne R, Buick D, Fisher M, Leake H, Cooper V, Weinman J. Doubts about necessity and concerns about adverse effects: identifying the types of beliefs that are associated with non-adherence to HAART. International Journal of STD & AIDS. 2004;15(1):38–44. doi: 10.1258/095646204322637245. [DOI] [PubMed] [Google Scholar]
- Horne R, Cooper V, Gellaitry G, Date HL, Fisher M. Patients’ perceptions of highly active antiretroviral therapy in relation to treatment uptake and adherence: the utility of the necessity-concerns framework. Journal Of Acquired Immune Deficiency Syndromes. 2007;45(3):334–341. doi: 10.1097/QAI.0b013e31806910e3. [DOI] [PubMed] [Google Scholar]
- Johnson CJ, Heckman TG, Hansen NB, Kochman A, Sikkema KJ. Adherence to antiretroviral medication in older adults living with HIV/AIDS: a comparison of alternative models. AIDS Care. 2009;21(5):541–551. doi: 10.1080/09540120802385611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MO, Chesney MA, Goldstein RB, Remien RH, Catz S, Gore-Felton C, Morin SF. Positive provider interactions, adherence self-efficacy, and adherence to antiretroviral medications among HIV-infected adults: A mediation model. AIDS Patient Care and STDs. 2006;20(4):258–268. doi: 10.1089/apc.2006.20.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MO, Elliott TR, Neilands TB, Morin SF, Chesney MA. A Social Problem-Solving Model of Adherence to HIV Medications. Health Psychology. 2006;25(3):355–363. doi: 10.1037/0278-6133.25.3.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MO, Neilands TB, Dilworth SE, Morin SF, Remien RH, Chesney MA. The Role of Self-Efficacy in HIV Treatment Adherence: Validation of the HIV Treatment Adherence Self-Efficacy Scale (HIV-ASES) Journal of Behavioral Medicine. 2007;30(5):359–370. doi: 10.1007/s10865-007-9118-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamau TM, Olson VG, Zipp GP, Clark M. Coping self-efficacy as a predictor of adherence to antiretroviral therapy in men and women living with HIV in Kenya. AIDS Patient Care and STDs. 2011;25(9):557–561. doi: 10.1089/apc.2011.0125. [DOI] [PubMed] [Google Scholar]
- Krakovska O, Wahl LM. Optimal drug treatment regimens for HIV depend on adherence. Journal Of Theoretical Biology. 2007;246(3):499–509. doi: 10.1016/j.jtbi.2006.12.038. [DOI] [PubMed] [Google Scholar]
- Low-Beer S, Yip B, O’Shaughnessy MV, Hogg RS, Montaner JS. Adherence to triple therapy and viral load response. Journal Of Acquired Immune Deficiency Syndromes. 2000;23(4):360–361. doi: 10.1097/00126334-200004010-00016. [DOI] [PubMed] [Google Scholar]
- Malcolm SE, Ng JJ, Rosen RK, Stone VE. An examination of HIV/AIDS patients who have excellent adherence to HAART. AIDS Care. 2003;15(2):251–261. doi: 10.1080/0954012031000068399. [DOI] [PubMed] [Google Scholar]
- Murphy DA, Greenwell L, Hoffman D. Factors associated with antiretroviral adherence among HIV-infected women with children. Women & Health. 2002;36(1):97–111. doi: 10.1300/J013v36n01_07. [DOI] [PubMed] [Google Scholar]
- Palella FJ, Jr, Delaney KM, Moorman AC, Loveless MO, Fuhrer J, Satten GA, Holmberg SD. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. The New England Journal Of Medicine. 1998;338(13):853–860. doi: 10.1056/NEJM199803263381301. [DOI] [PubMed] [Google Scholar]
- Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, Singh N. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Annals of Internal Medicine. 2000;133(1):21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]
- Prejean J, Song R, Hernandez A, Ziebell R, Green T, Walker F, Group HIS. Estimated HIV Incidence in the United States, 2006–2009. PLoS ONE. 2011;6(8):e17502. doi: 10.1371/journal.pone.0017502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puskas CM, Forrest JI, Parashar S, Salters KA, Cescon AM, Kaida A, Hogg RS. Women and Vulnerability to HAART Non-Adherence: A Literature Review of Treatment Adherence by Gender from 2000 to 2011. Curr HIV/AIDS Rep. 2011;8(4):277–287. doi: 10.1007/s11904-011-0098-0. [DOI] [PubMed] [Google Scholar]
- Reynolds NR, Testa MA, Marc LG, Chesney MA, Neidig JL, Smith SR, Robbins GK. Factors influencing medication adherence beliefs and self-efficacy in persons naive to antiretroviral therapy: a multicenter, cross-sectional study. AIDS and Behavior. 2004;8(2):141–150. doi: 10.1023/B:AIBE.0000030245.52406.bb. [DOI] [PubMed] [Google Scholar]
- Rudy BJ, Murphy DA, Harris DR, Muenz L, Ellen J. Prevalence and Interactions of Patient-Related Risks for Nonadherence to Antiretroviral Therapy Among Perinatally Infected Youth in the United States. AIDS Patient Care & STDs. 2010;24(2):97–104. doi: 10.1089/apc.2009.0198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schackman BR, Gebo KA, Walensky RP, Losina E, Muccio T, Sax PE, Freedberg KA. The lifetime cost of current human immunodeficiency virus care in the United States. Med Care. 2006;44(11):990–997. doi: 10.1097/01.mlr.0000228021.89490.2a. [DOI] [PubMed] [Google Scholar]
- Simoni JM, Frick PA, Huang B. A longitudinal evaluation of a social support model of medication adherence among HIV-positive men and women on antiretroviral therapy. Health Psychology. 2006;25(1):74–81. doi: 10.1037/0278-6133.25.1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simoni JM, Frick PA, Lockhart D, Liebovitz D. Mediators of social support and antiretroviral adherence among an indigent population in New York City. AIDS Patient Care and STDs. 2002;16(9):431–439. doi: 10.1089/108729102760330272. [DOI] [PubMed] [Google Scholar]
- Simoni JM, Kurth AE, Pearson CR, Pantalone DW, Merrill JO, Frick PA. Self-report measures of antiretroviral therapy adherence: A review with recommendations for HIV research and clinical management. AIDS and Behavior. 2006;10(3):227–245. doi: 10.1007/s10461-006-9078-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simoni JM, Pantalone DW, Plummer MD, Huang B. A randomized controlled trial of a peer support intervention targeting antiretroviral medication adherence and depressive symptomatology in HIV-positive men and women. Health Psychology. 2007;26(4):488–495. doi: 10.1037/0278-6133.26.4.488. [DOI] [PMC free article] [PubMed] [Google Scholar]