Abstract
BACKGROUND
Efforts to expand the donor pool by recruiting younger donors have resulted in higher numbers of initial donations, but retention of young donors continues to be a problem.
STUDY DESIGN AND METHODS
Path analysis was used to examine the simultaneous relationships among syncopal reactions, donation anxiety, needle pain, donor satisfaction, and donation intention in the prediction of repeat donation. Participants included 421 first- and second-time donors recruited for a study comparing the effects of pre-donation water loading with and without the use of applied muscle tension during donation (52% female, 60.8% first-time donor, mean age 20.3 years). For this longitudinal follow-up study, donor database records were accessed two years after the index donation to determine whether a repeat donation had been attempted.
RESULTS
Results of a series of path analyses demonstrated the influential role of donor anxiety in shaping donor retention (final model Χ2=35.75, RMSEA=0.03, CFI=0.98, WRMR=0.74). First, anxiety exerted a direct negative influence on donation intention, the proximal and sole direct predictor of repeat donation. Second, anxiety increased the likelihood of donor-reported needle pain, adversely affecting donation satisfaction and, subsequently, donation intention. Finally, anxiety was associated with donor ratings of syncopal reactions through its impact on needle pain, which also contributed to decreased donation intention.
CONCLUSION
These results provide novel evidence that donation anxiety plays a central role in shaping future donation behavior; hence, individual differences in anxiety must be considered when developing and testing strategies to enhance blood donor retention.
Keywords: Blood donor, syncopal reactions, anxiety, pain, donor satisfaction
INTRODUCTION
Recent efforts to expand the donor pool by recruiting younger donors have resulted in higher numbers of initial donations;1 however, retention of young donors has been a significant problem. The majority of these donors do not return to provide a repeat donation, and only a small proportion goes on to become committed blood donors.2–4 As a result, the current blood supply is highly reliant on first-time donors,5 but these new donors must constantly be replaced because they typically fail to return.
Although a number of factors shape individual decisions to donate, both retrospective and prospective studies demonstrate that the experience of syncopal reactions (i.e., full faint as well as presyncopal symptoms such as faintness, dizziness, and lightheadedness that can progress to a full faint) is a particularly important barrier to blood donor retention.6–17 For example, in a one-year prospective study of nearly 90,000 blood donors, we demonstrated a return rate of 64% for those who did not react versus 40% for those who did.18 We later confirmed this effect in a new sample of nearly 45,000 male donors — non-reactors returned at a rate of 67.3% as compared to 42.1% for reactors.15 Not surprisingly, in both of our studies the return rate was lowest for those who reacted while donating for the first time. Similar deterrent effects have been reported by other investigators, with minor reactions leading to 14–23% reductions in return rates the following year and major reactions leading to 25–49% losses.4,17,19
In an effort to reduce the likelihood of syncopal reactions, and thereby increase donor willingness to return, a number of approaches have been proposed including applied muscle tension, pre-donation hydration, and distraction. Each of these approaches has been supported by randomized controlled trials that have demonstrated significant reductions in syncopal reactions, albeit with varying outcomes across studies and donor groups.20–27 Further, recent large-scale observational studies have reported significant reductions in syncopal reactions following implementation of a combination of screening for estimated blood volume and application of muscle tension and pre-donation hydration interventions.28,29
Despite the apparent success that the various interventions have had on attenuating syncopal reactions, few studies have examined the extent to which this effect translates into enhanced donor retention. In one exception, Ditto and colleagues30 demonstrated an enhanced likelihood of return within two years among women, but not men, who had been taught to use applied muscle tension during blood donation as compared to a no-treatment control condition. Interestingly, a reduction in reported syncopal symptoms during the index donation did not account for the subsequent return behavior, suggesting that the other non-physiological mechanisms may have been responsible for the effect of the intervention on return behavior. These findings indicate that additional effort is required to look at the relationship between interventions designed to reduce syncopal reactions, donor return behavior, and potential variables that may help to explain the relationship between intervention and retention.
In line with this goal, the present report analyzes two-year donor return behavior among novice blood donors who engaged in pre-donation water consumption with and without leg muscle activation during donation as compared to those assigned to a control condition. Initial findings from this randomized controlled trial demonstrated that the interventions produced significant reductions in presyncopal reactions, as indexed by both donor self-report and phlebotomist ratings.24 In the present report we use path analysis to examine the complex simultaneous relationships among syncopal reactions, donation anxiety, needle pain, donor satisfaction, and donation intention in the prediction of donor return behavior.
MATERIALS AND METHODS
Participants
Participants were originally recruited for an intervention study examining the effect of pre-donation hydration and applied muscle tension on presyncopal reactions in response to blood donation.24 At that time, participants gave their consent to be tracked by their donor number for subsequent blood donation attempts in the next two years.
All participants were donors at American Red Cross blood collection sites in central and southeast Ohio, with the majority of the testing sites located on college campuses. Donors who met the original study’s inclusion criteria (i.e., first- or second-time blood donor, eligible to donate, at least 18 years of age) were invited to participate. The final sample for these analyses included 421 adults (219 women, 202 men) with a mean age of 20.3 years (SD = 5.2); 60.8% were first-time donors and 39.2% were donating blood for the second time. The majority of participants in the sample self-identified as Caucasian (76.5%). Demographic variables as well as the other measures included in the path analysis are summarized in Table 1. There were no significant differences between first- and second-time donors on any of the demographic variables.
Table 1.
Participant characteristics, expressed as Mean (Standard Deviation) for continuous variables and as N (%) for categorical variables.
| Variable | Units | No Treatment (n=209) | Treatment (n=212) |
|---|---|---|---|
| Age | years | 20.3 (5.7) | 20.3 (4.7) |
| Female | 108 (51.7%) | 111 (52.4%) | |
| BMI | kg/m2 | 24.5 (4.5) | 24.2 (4.3) |
| First time donor | 133 (63.6%) | 123 (58.0%) | |
| Anxiety | score (20–80) | 33.1 (8.4) | 32.1 (9.3) |
| BDRI-4* | score (0–20) | 4.4 (5.4) | 3.2 (4.7) |
| Phlebotomist rating of reaction* | None | 161 (77.0) | 187 (88.2) |
| Slight (pre-faint) | 37 (17.7) | 21 (9.9) | |
| Moderate/Severe (e.g., faint, hematoma) | 11 (5.3) | 4 (1.9) | |
| Needle Pain | score (0–5) | 1.7 (1.1) | 1.7 (1.2) |
| Donation Satisfaction | score (0–100) | 92.4 (16.7) | 94.4 (12.3) |
| Repeat Donation Intention | score (0–100) | 81.2 (25.4) | 83.7 (24.7) |
| Repeat Donation Attempt | 72 (34.4%) | 74 (34.9%) |
p<.05
Materials
Demographic Survey
Participants provided a range of personal data including their gender, history of previous donations, and race/ethnicity.
State Anxiety Inventory
Anxiety related to the impending blood donation was assessed using a version of the State Anxiety Inventory (STAI-Y),31 a 20-item scale designed to allow for self-report of state anxiety levels with total scores ranging from 20 to 80. An example item, rated from 1 (not at all) to 4 (very much), is “I am tense.” In the present study this measure had excellent internal consistency (Cronbach’s α = 0.91), which is consistent with psychometric data from previous blood donation studies.32–34
Blood Donation Reactions Inventory-4
The Blood Donation Reactions Inventory-4 asks the donor to provide subjective ratings of four syncopal symptoms associated with blood donation on a 0 (not at all) to 5 (to an extreme degree) scale, with total scores ranging from 0 to 20.35 The four items include 1) faintness, 2) dizziness, 3) weakness, and 4) lightheadedness. Previous research supports the reliability and validity of this measure,35 and in the present study the internal consistency reliability was high (Cronbach’s α = 0.94).
Additional Post-Donation Items
Donors also completed individual post-donation measures of pain during insertion of the donation needle (range 0=not at all painful to 5=extremely painful), overall satisfaction with the donation experience (rated from 0%=not at all satisfied to 100%=completely satisfied), and estimated likelihood of providing another donation in the following year (rated from 0% to 100% likely).
Donor Database Records
To provide a more objective measure of syncopal symptoms, phlebotomist classifications of donor reactions36 were obtained from the donor record. In addition, these records were consulted to determine whether each participant made a subsequent donation attempt during the two year period following enrollment in the study (i.e., both deferrals and successful donations were counted as a repeat donation).
Study Design
Participants included donors who were recruited for an intervention study comparing the effects of pre-donation water loading with and without the use of applied muscle tension techniques during donation (see 24 for a more complete description). Briefly, eligible participants completed informed consent procedures and were randomly assigned to one of four groups, including two control conditions (standard donation or placebo control) and two treatment conditions (pre-donation water or pre-donation water combined with leg exercise). Next, participants were given an anonymous identification code, provided study directions specific to their group assignment, and completed the pre-donation questionnaires (demographics and anxiety). All participants donated according to standard American Red Cross procedures and their group assignment, and then proceeded to a post-donation canteen area where they completed post-donation measures. American Red Cross donor database records were subsequently consulted to obtain information on donor reactions during the index donation.
For this follow-up study examining factors relating to repeat donation behavior, donor database records were accessed again for each of the original participants two years after the index donation in order to determine whether a repeat donation had been attempted in the intervening period.
The study protocol was approved by the Institutional Review Boards of Ohio University and the American Red Cross, and was pre-registered with www.clinicaltrials.gov (#NCT00302900).
Statistical analysis
Structural equation modeling was conducted with Mplus Version 6.12 computer software. Chi-square difference tests were used to compare models. In a step-wise fashion non-significant paths were removed from the model and individual paths suggested by high modification indices were added, and at each step the model was evaluated to see whether fit was improved. Because the main variable of interest, repeat donation, is a binary variable, the models were estimated with a weighed least square parameter estimates. A number of goodness-of-fit indices were examined for each of the models tested. The chi-square statistic provides a test of the null hypothesis that the covariance matrix conforms to the particular model being tested. Since the goal is to develop a model that fits the data, a non-significant chi-square value is desirable. Because the chi-square statistic is dependent on sample size, however, even trivial differences can lead to a significant chi-square result in large samples. Therefore, in structural equation modeling, the pattern of results across a number of goodness-of-fit tests is considered to assess how well a model fits the data. As recommended in the literature, a test from each category of fit indices (comparative fit, parsimony correction, and absolute fit) was included: comparative fit index (CFI) ranges from 0.00–1.00, with values >0.95 considered acceptable; root mean square error of approximation (RMSEA) has a lower limit of 0.00, with values <0.06 considered acceptable; and weighted root mean square residual (WRMR) ranges from 0.00 to infinity, with values <0.90 considered acceptable.37
RESULTS
To account for the interventions that were part of the clinical trial, the sample was divided into treatment and control conditions. Consistent with our original report,24 Table 1 shows that donors in the treatment condition had fewer syncopal reactions than donors in the control condition (based on both subjective ratings and phlebotomist reports); however, donors in the two conditions did not differ on any of the other characteristics that were measured.
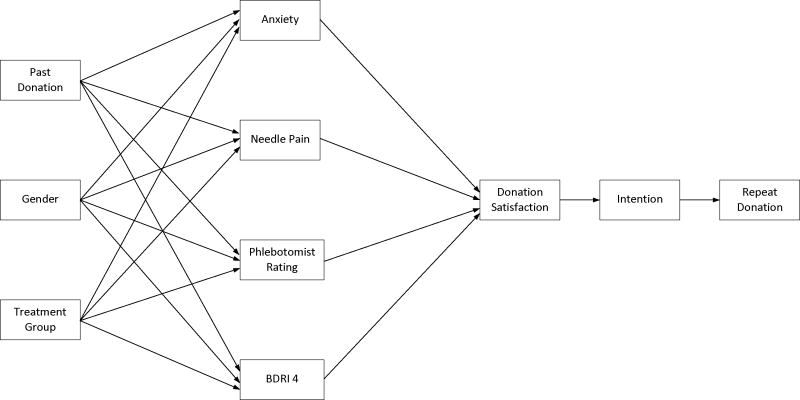
Our initial model was based on the hypothesis that attenuation of syncopal reactions would be associated with increased donor satisfaction, in turn leading to greater intentions to provide a repeat donation, and ultimately a greater likelihood of donor retention. As illustrated in Figure 1, needle pain and anxiety were expected to have a negative direct influence on donor satisfaction. Finally, prior donation history, donor sex, and treatment group assignment were included in the model based on previous evidence of their association with syncopal reactions.28,29,38,39 As can be seen in the path analysis results presented in Table 2, the goodness-of-fit tests indicated that this initial model was not a good fit to the data. Therefore, to determine if a good model fit could be achieved, a methodical approach was taken to revise the model paths. First, all non-significant paths from the original model were removed. In addition, because BDRI-4 and phlebotomist ratings both represent the same syncopal reactions from different perspectives, rather than specify a directional path these two variables were allowed to correlate. Next, in a series of sequential steps, modification indices from the path analysis were examined to determine whether additional changes improved the overall model based on the results of chi-square difference tests.
Figure 1.
Initial hypothesized model of donor return behavior.
Table 2.
Goodness-of-fit test results for the three models.
| Model | Χ2 (df), pa | CFIb | RMSEAc | WRMRd |
|---|---|---|---|---|
| 1 (Original) | 259.27 (24), <0.001 | 0.51 | 0.15 | 2.11 |
| 2 (Revised) | 43.38 (27), <0.05 | 0.97 | 0.04 | 0.83 |
| 3 (Final) | 35.75 (26), 0.10 | 0.98 | 0.03 | 0.74 |
A non-significant Χ2 is desirable;
Range 0.00–1.00, >0.95 acceptable;
Lower limit 0.00, <0.06 acceptable;
Range 0.00–infinity, <0.90 acceptable.
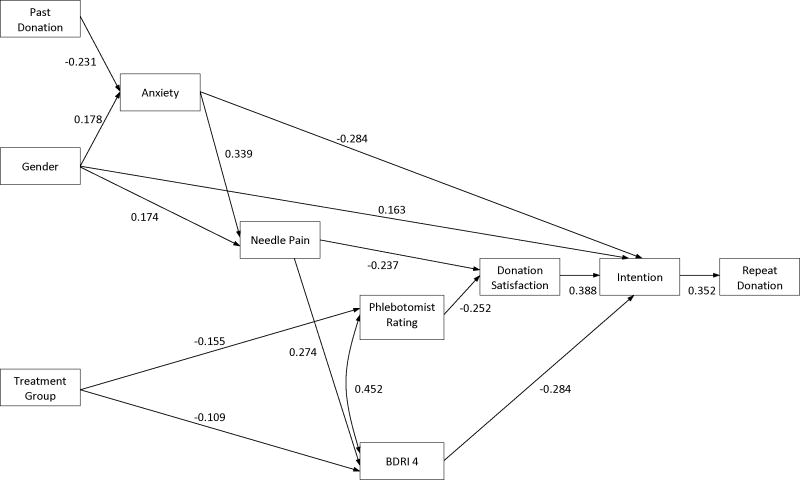
As a result of this sequential process a revised model was specified. As illustrated in Figure 2, the only direct predictor of repeat donation behavior was intention. However, multiple factors had an indirect influence on repeat donation behavior via their impact on intention. Specifically, higher levels of donation intention were reported by women and among those with less anxiety, greater donation satisfaction, and lower subjective syncopal reaction scores. In addition, donors with lower anxiety levels reported less needle pain, which in turn was related to lower subjective syncopal reaction scores. Absence of phlebotomist reports of syncopal symptoms and lower needle pain ratings were also associated with greater donation satisfaction. Finally, previous donation experience was related to lower anxiety, males reported less anxiety and needle pain, and assignment to a treatment condition was associated with attenuation of syncopal reactions relative to controls. As shown in Table 2, this revised model showed a good fit to the data, surpassing standards on all three fit indices (i.e., CFI =0.97, RMSEA=0.04, WRMR=0.83).
Figure 2.
Revised model of donor return behavior showing standardized path coefficients. For figure simplicity, residual variances for the dependent variables are not indicated.
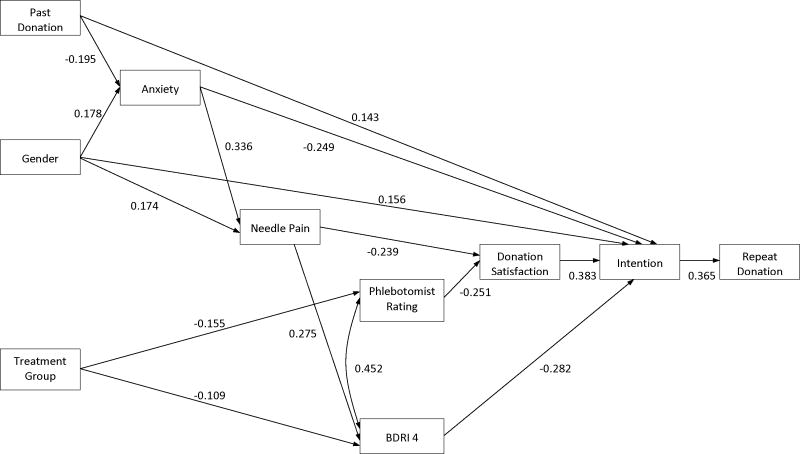
Although the revised model was a strong fit to the data, examination of the modification indices suggested that it could be improved by adding a direct path from past donation to intention (see Figure 3). Addition of this pathway yielded a significant chi-square difference test relative to the revised model, and as shown in Table 2 further improved each of the fit indices compared to both of the previous models. Thus the data best supported this final model of return donation behavior.
Figure 3.
Final model of donor return behavior showing standardized path coefficients. For figure simplicity, residual variances for the dependent variables are not indicated.
DISCUSSION
Based on previous evidence of the importance of donor satisfaction in shaping repeat donation intentions and behavior,13,40–42 we proposed that satisfaction with the donation process would be a key determinant of intention to provide a repeat donation among novice donors exposed to an intervention designed to reduce syncopal reactions. Further, we posited that donor satisfaction could be negatively influenced by the experience of anxiety, pain, and syncopal symptoms. Notably, given the scarcity of studies examining actual behavior, we ascertained repeat donation attempts by consulting donor database records for a two-year period. Results of a series of path analyses confirmed that donation intention was the sole direct influence on repeat donation behavior. As predicted, satisfaction was a direct predictor of donation intention, and higher levels of needle pain and phlebotomist reports of syncopal reactions were associated with reduced satisfaction. However, our analyses also revealed that anxiety and subjective syncopal reactions exerted a direct effect on donation intention, rather than an indirect effect via satisfaction. Specifically, greater anxiety and higher levels of self-reported syncopal symptoms were associated with a reduced intention of providing a repeat donation. Finally, those with a previous experience of blood donation reported both lower anxiety and a higher intention of repeat donation.
Many of the interrelationships supported by our path analyses substantiate prior findings in the area of blood donation research. For instance, previous studies have noted the importance of both subjectively and objectively measured syncopal symptoms in the prediction of donor retention.14,15,18,43 In the present study both donor and phlebotomist ratings of syncopal reactions were retained in the final model, suggesting that the subjective perception of syncopal symptoms accounts for unique variance in predicting donation intentions beyond the influence of syncopal symptoms per se. This result is similar to a previous study in which Blood Donations Reactions Inventory scores remained a significant predictor of donation return behavior even after controlling for donation chair reclining performed by the phlebotomist.14 Together these findings indicate that individual differences in donors’ psychological response to their symptoms may be important in shaping their future donation intentions and behavior (e.g., mild symptoms of faintness or dizziness may appear similar to an external observer, but donors may differ substantially in the extent to which they view their symptoms with alarm or possibly as an indication that they are not well-suited to future donation).
In addition to affirming the importance of syncopal reactions, our data strongly support the influential role of anxiety in the re-donation decision process. First, anxiety exerted a direct negative influence on donation intention. Second, in line with prior pain studies,44,45 anxiety increased the likelihood of the donor reporting needle pain, which adversely affected donation satisfaction. Finally, the present findings confirm results from numerous studies that higher anxiety levels are associated with increased syncopal reactions among both novice and experienced blood donors,46–49 and that these anxiety-related reactions may be associated with decreased donor return.43 While this study did not find an influence of treatment group on anxiety, there is recent evidence that muscle tensing interventions aimed at reducing syncopal reactions are most likely to help donors with elevated levels of anxiety,27,50 possibly by increasing confidence in their own ability to cope with the donation process. Accordingly, identifying and addressing elevated levels of donor anxiety may be a particularly efficient method of enhancing intentions and repeat donations among novice blood donors. Although we did not measure post-donation anxiety, it is reasonable to speculate that anxiety levels experienced after the completion of the donation process may also exert an independent effect on donation intention. This raises the possibility that interventions that address concerns that may arise after the donation (e.g., bruising, post-donation weakness, delayed syncopal symptoms) could be used to further strengthen donor retention. Consistent with this notion, Sinclair and colleagues51 demonstrated that a post-donation motivational interview designed to address individual donor concerns was associated with lower anxiety reports and an increased likelihood of repeat donation in the following year.
Although our model emphasizes that anxiety should be an important focus for intervention efforts, it also indicates that there are additional viable targets. For example, physiological interventions that can reduce the risk of syncopal reactions, such as pre-donation hydration20,21,24,52 or applied muscle tension,22,30,53,54 should increase donation intention independent of any effect that they may have on donor anxiety. Similarly, efforts to reduce the experience of needle pain (e.g. using an analgesic cream) would be expected to enhance donation satisfaction and donation intention. Finally, creative ways of promoting donation satisfaction may further enhance repeat donation intention among all donors, and may be particularly useful in offsetting the influence of minor discomfort related to needle pain or mild syncopal reactions.
The current study had a number of important strengths, including the use of a longitudinal design with assessment of repeat donation behavior, assessment of both subjective and objective measures of syncopal reactions, and use of path analysis to examine the joint influence of multiple predictors on donation intention and behavior. However, a few limitations are also worth noting. First, the present sample was restricted to relatively novice, college-aged donors and hence the findings may not generalize directly to other donor populations. Second, our effort to model future donation behavior was necessarily limited by the variables which were included in the original intervention study. Because other important predictors of donation intention and behavior have been identified in augmented Theory of Planned Behavior models of blood donation (e.g., self-efficacy, attitude, anticipated regret),42,55–60 future studies should consider inclusion of these additional predictors to help build potential stronger models.
In sum, the results of the present study provide novel and important evidence that donor anxiety, pain, syncopal reactions, and overall satisfaction each play important roles in shaping future donation behavior. Although additional research is needed to confirm these findings and to identify other potential predictors, the current findings may help guide the development of new strategies to enhance retention of novice blood donors.
Acknowledgments
Funding: We are most grateful for the cooperation and collaboration of the American Red Cross Blood Services, Central Ohio Region, and particularly for the efforts of Deborah Carvalho, Lori Gaitten, and Mary Schumacher. We are also grateful for the efforts of the research assistants who helped with data collection and entry (Tanya Cornett, Kelsey Fazenbaker, Erin Matson, Sarah McGlone, Rita Murphy, Kadian Sinclair, Zina Trost). Finally, a special note of appreciation is due to all of the donors who participated in this project.
Funding: Funding for this study was provided by a grant from the National Heart, Lung, and Blood Institute (HL077438).
Footnotes
Conflict of interest statement: The authors certify that they have no conflicts of interest or financial involvement with this manuscript.
References
- 1.Zou S, Musavi F, Notari EPt, Fang CT. Changing age distribution of the blood donor population in the United States. Transfusion. 2008;48:251–7. doi: 10.1111/j.1537-2995.2007.01517.x. [DOI] [PubMed] [Google Scholar]
- 2.Schreiber GB, Sanchez AM, Glynn SA, Wright DJ. Increasing blood availability by changing donation patterns. Transfusion. 2003;43:591–7. doi: 10.1046/j.1537-2995.2003.00388.x. [DOI] [PubMed] [Google Scholar]
- 3.Schreiber GB, Sharma UK, Wright DJ, Glynn SA, Ownby HE, Tu Y, Garratty G, Piliavin J, Zuck T, Gilcher R. First year donation patterns predict long-term commitment for first-time donors. Vox Sang. 2005;88:114–21. doi: 10.1111/j.1423-0410.2005.00593.x. [DOI] [PubMed] [Google Scholar]
- 4.Eder AF, Notari EPt, Dodd RY. Do reactions after whole blood donation predict syncope on return donation? Transfusion. 2012 doi: 10.1111/j.1537-2995.2012.03666.x. [DOI] [PubMed] [Google Scholar]
- 5.Whitaker BL, Green J, King MR, Leibeg LL, Mathew SM, Schlumpf KS, Schreiber GB. The 2007 National Blood Collection and Utilization Survey Report. Washington, D.C: 2007. [Google Scholar]
- 6.Trouern-Trend JJ, Cable RG, Badon SJ, Newman BH, Popovsky MA. A case-controlled multicenter study of vasovagal reactions in blood donors: influence of sex, age, donation status, weight, blood pressure, and pulse. Transfusion. 1999;39:316–20. doi: 10.1046/j.1537-2995.1999.39399219291.x. [DOI] [PubMed] [Google Scholar]
- 7.Piliavin JA, Callero PL. Giving Blood: The Development of an Altruistic Identity. Baltimore: Johns Hopkins; 1991. [Google Scholar]
- 8.Piliavin JA. Why do they give the gift of life? A review of research on blood donors since 1977. Transfusion. 1990;30:444–59. doi: 10.1046/j.1537-2995.1990.30590296381.x. [DOI] [PubMed] [Google Scholar]
- 9.Kaloupek DG, Stoupakis T. Coping with a stressful medical procedure: further investigation with volunteer blood donors. J Behav Med. 1985;8:131–48. doi: 10.1007/BF00845517. [DOI] [PubMed] [Google Scholar]
- 10.Ogata H, Iinuma N, Nagashima K, Akabane T. Vasovagal reactions in blood donors. Transfusion. 1980;20:679–83. doi: 10.1046/j.1537-2995.1980.20681057157.x. [DOI] [PubMed] [Google Scholar]
- 11.Sauer LA, France CR. Caffeine attenuates vasovagal reactions in female first-time blood donors. Health Psychol. 1999;18:403–9. doi: 10.1037//0278-6133.18.4.403. [DOI] [PubMed] [Google Scholar]
- 12.Staallekker LA, Stammeijer RN, Dudok de Wit C. A Dutch blood bank and its donors. Transfusion. 1980;20:66–70. doi: 10.1046/j.1537-2995.1980.20180125042.x. [DOI] [PubMed] [Google Scholar]
- 13.Thomson RA, Bethel J, Lo AY, Ownby HE, Nass CC, Williams AE. Retention of “safe” blood donors. The Retrovirus Epidemiology Donor Study. Transfusion. 1998;38:359–67. doi: 10.1046/j.1537-2995.1998.38498257374.x. [DOI] [PubMed] [Google Scholar]
- 14.France CR, France JL, Roussos M, Ditto B. Mild reactions to blood donation predict a decreased likelihood of donor return. Transfusion and Apheresis Science. 2004;30:17–22. doi: 10.1016/j.transci.2003.08.014. [DOI] [PubMed] [Google Scholar]
- 15.Rader AW, France CR, Carlson B. Donor retention as a function of donor reactions to whole-blood and automated double red cell collections. Transfusion. 2007;47:995–1001. doi: 10.1111/j.1537-2995.2007.01223.x. [DOI] [PubMed] [Google Scholar]
- 16.Newman BH, Newman DT, Ahmad R, Roth AJ. The effect of whole-blood donor adverse events on blood donor return rates. Transfusion. 2006;46:1374–9. doi: 10.1111/j.1537-2995.2006.00905.x. [DOI] [PubMed] [Google Scholar]
- 17.Eder AF, Hillyer CD, Dy BA, Notari EPt, Benjamin RJ. Adverse reactions to allogeneic whole blood donation by 16- and 17-year-olds. JAMA. 2008;299:2279–86. doi: 10.1001/jama.299.19.2279. [DOI] [PubMed] [Google Scholar]
- 18.France CR, Rader A, Carlson B. Donors who react may not come back: analysis of repeat donation as a function of phlebotomist ratings of vasovagal reactions. Transfus Apher Sci. 2005;33:99–106. doi: 10.1016/j.transci.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 19.Gorlin JB, Petersen J. Reactions in first-time high school blood donors. Transfusion. 2004;44:463. doi: 10.1111/j.0041-1132.2004.371_1.x. [DOI] [PubMed] [Google Scholar]
- 20.Hanson SA, France CR. Predonation water ingestion attenuates negative reactions to blood donation. Transfusion. 2004;44:924–8. doi: 10.1111/j.1537-2995.2004.03426.x. [DOI] [PubMed] [Google Scholar]
- 21.Newman B, Tommolino E, Andreozzi C, Joychan S, Pocedic J, Heringhausen J. The effect of a 473-mL (16-oz) water drink on vasovagal donor reaction rates in high-school students. Transfusion. 2007;47:1524–33. doi: 10.1111/j.1537-2995.2007.01293.x. [DOI] [PubMed] [Google Scholar]
- 22.Ditto B, France CR, Lavoie P, Roussos M, Adler PS. Reducing reactions to blood donation with applied muscle tension: a randomized controlled trial. Transfusion. 2003;43:1269–75. doi: 10.1046/j.1537-2995.2003.00488.x. [DOI] [PubMed] [Google Scholar]
- 23.Ditto B, France CR, Albert M, Byrne N. Dismantling applied tension: mechanisms of a treatment to reduce blood donation-related symptoms. Transfusion. 2007;47:2217–22. doi: 10.1111/j.1537-2995.2007.01449.x. [DOI] [PubMed] [Google Scholar]
- 24.France CR, Ditto B, Wissel ME, France JL, Dickert T, Rader A, Sinclair K, McGlone S, Trost Z, Matson E. Predonation hydration and applied muscle tension combine to reduce presyncopal reactions to blood donation. Transfusion. 2010;50:1257–64. doi: 10.1111/j.1537-2995.2009.02574.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bonk VA, France CR, Taylor BK. Distraction reduces self-reported physiological reactions to blood donation in novice donors with a blunting coping style. Psychosom Med. 2001;63:447–52. doi: 10.1097/00006842-200105000-00014. [DOI] [PubMed] [Google Scholar]
- 26.Ditto B, France CR. The effects of applied tension on symptoms in French-speaking blood donors: a randomized trial. Health Psychol. 2006;25:433–7. doi: 10.1037/0278-6133.25.3.433. [DOI] [PubMed] [Google Scholar]
- 27.Ditto B, France CR, Holly C. Applied tension may help retain donors who are ambivalent about needles. Vox Sang. 2010;98:e225–30. doi: 10.1111/j.1423-0410.2009.01273.x. [DOI] [PubMed] [Google Scholar]
- 28.Eder AF, Dy BA, Kennedy JM, Perez J, Demaris P, Procaccio A, Benjamin RJ. Improved safety for young whole blood donors with new selection criteria for total estimated blood volume. Transfusion. 2011;51:1522–31. doi: 10.1111/j.1537-2995.2011.03143.x. [DOI] [PubMed] [Google Scholar]
- 29.Tomasulo P, Kamel H, Bravo M, James RC, Custer B. Interventions to reduce the vasovagal reaction rate in young whole blood donors. Transfusion. 2011;51:1511–21. doi: 10.1111/j.1537-2995.2011.03074.x. [DOI] [PubMed] [Google Scholar]
- 30.Ditto B, France CR, Albert M, Byrne N, Smyth-Laporte J. Effects of applied muscle tension on the likelihood of blood donor return. Transfusion. 2009;49:858–62. doi: 10.1111/j.1537-2995.2008.02067.x. [DOI] [PubMed] [Google Scholar]
- 31.Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory (Form Y) Palo Alto, Ca: Consulting Psychologists Press; 1983. [Google Scholar]
- 32.France CR, France JL, Kowalsky JM, Cornett TL. Education in donation coping strategies encourages individuals to give blood: further evaluation of a donor recruitment brochure. Transfusion. 2010;50:85–91. doi: 10.1111/j.1537-2995.2009.02381.x. [DOI] [PubMed] [Google Scholar]
- 33.France CR, France JL, Wissel ME, Kowalsky JM, Bolinger EM, Huckins JL. Enhancing blood donation intentions using multimedia donor education materials. Transfusion. 2011;51:1796–801. doi: 10.1111/j.1537-2995.2010.03033.x. [DOI] [PubMed] [Google Scholar]
- 34.France CR, France JL, Kowalsky JM, Copley DM, Lewis KN, Ellis GD, McGlone ST, Sinclair KS. A Web-based approach to blood donor preparation. Transfusion. 2012 doi: 10.1111/j.1537-2995.2012.03737.x. [DOI] [PubMed] [Google Scholar]
- 35.France CR, Ditto B, France JL, Himawan LK. Psychometric properties of the Blood Donation Reactions Inventory: a subjective measure of presyncopal reactions to blood donation. Transfusion. 2008;48:1820–6. doi: 10.1111/j.1537-2995.2008.01831.x. [DOI] [PubMed] [Google Scholar]
- 36.Eder AF, Dy BA, Kennedy JM, Notari EP, IV, Strupp A, Wissel ME, Reddy R, Gibble J, Haimowitz MD, Newman BH, Chambers LA, Hillyer CD, Benjamin RJ. The American Red Cross donor hemovigilance program: complications of blood donation reported in 2006. Transfusion. 2008;48:1809–19. doi: 10.1111/j.1537-2995.2008.01811.x. [DOI] [PubMed] [Google Scholar]
- 37.Schreiber JB, Stage FK, King J, Nora A, Barlow EA. Reporting structural equation modeling and confirmatory factor analysis results: A review. The Journal of Educational Research. 2006;99:323–37. [Google Scholar]
- 38.Wiltbank TB, Giordano GF, Kamel H, Tomasulo P, Custer B. Faint and prefaint reactions in whole-blood donors: an analysis of predonation measurements and their predictive value. Transfusion. 2008;48:1799–808. doi: 10.1111/j.1537-2995.2008.01745.x. [DOI] [PubMed] [Google Scholar]
- 39.Kamel H, Tomasulo P, Bravo M, Wiltbank T, Cusick R, James RC, Custer B. Delayed adverse reactions to blood donation. Transfusion. 2010;50:556–65. doi: 10.1111/j.1537-2995.2009.02397.x. [DOI] [PubMed] [Google Scholar]
- 40.Schlumpf KS, Glynn SA, Schreiber GB, Wright DJ, Randolph Steele W, Tu Y, Hermansen S, Higgins MJ, Garratty G, Murphy EL. Factors influencing donor return. Transfusion. 2008;48:264–72. doi: 10.1111/j.1537-2995.2007.01519.x. [DOI] [PubMed] [Google Scholar]
- 41.Gillespie TW, Hillyer CD. Blood donors and factors impacting the blood donation decision. Transfus Med Rev. 2002;16:115–30. doi: 10.1053/tmrv.2002.31461. [DOI] [PubMed] [Google Scholar]
- 42.France JL, France CR, Himawan LK. A path analysis of intention to redonate among experienced blood donors: an extension of the theory of planned behavior. Transfusion. 2007;47:1006–13. doi: 10.1111/j.1537-2995.2007.01236.x. [DOI] [PubMed] [Google Scholar]
- 43.Ditto B, France CR. Vasovagal symptoms mediate the relationship between predonation anxiety and subsequent blood donation in female volunteers. Transfusion. 2006;46:1006–10. doi: 10.1111/j.1537-2995.2006.00835.x. [DOI] [PubMed] [Google Scholar]
- 44.Rhudy JL, Meagher MW. Fear and anxiety: divergent effects on human pain thresholds. Pain. 2000;84:65–75. doi: 10.1016/S0304-3959(99)00183-9. [DOI] [PubMed] [Google Scholar]
- 45.Lumley MA, Cohen JL, Borszcz GS, Cano A, Radcliffe AM, Porter LS, Schubiner H, Keefe FJ. Pain and emotion: a biopsychosocial review of recent research. Journal of Clinical Psychology. 2011;67:942–68. doi: 10.1002/jclp.20816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.France CR, France JL, Himawan LK, Stephens KY, Frame-Brown TA, Venable GA, Menitove JE. How afraid are you of having blood drawn from your arm? A simple fear question predicts vasovagal reactions without causing them among high school donors. Transfusion. 2012 doi: 10.1111/j.1537-2995.2012.03726.x. [DOI] [PubMed] [Google Scholar]
- 47.France CR, France JL, Kowalsky JM, Ellis GD, Copley DM, Geneser A, Frame-Brown T, Venable G, Graham D, Shipley P, Menitove JE. Assessment of donor fear enhances prediction of presyncopal symptoms among volunteer blood donors. Transfusion. 2012;52:375–80. doi: 10.1111/j.1537-2995.2011.03294.x. [DOI] [PubMed] [Google Scholar]
- 48.Meade MA, France CR, Peterson LM. Predicting vasovagal reactions in volunteer blood donors. J Psychosom Res. 1996;40:495–501. doi: 10.1016/0022-3999(95)00639-7. [DOI] [PubMed] [Google Scholar]
- 49.Labus JS, France CR, Taylor BK. Vasovagal reactions in volunteer blood donors: Analyzing the predictive power of the medical fears survey. Int J Behav Med. 2000;7:62–72. [Google Scholar]
- 50.Holly CD, Balegh S, Ditto B. Applied tension and blood donation symptoms: the importance of anxiety reduction. Health Psychol. 2011;30:320–5. doi: 10.1037/a0022998. [DOI] [PubMed] [Google Scholar]
- 51.Sinclair KS, Campbell TS, Carey PM, Langevin E, Bowser B, France CR. An adapted postdonation motivational interview enhances blood donor retention. Transfusion. 2010;50:1778–86. doi: 10.1111/j.1537-2995.2010.02618.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ando SI, Kawamura N, Matsumoto M, Dan E, Takeshita A, Murakami K, Kashiwagi S, Kiyokawa H. Simple standing test predicts and water ingestion prevents vasovagal reaction in the high-risk blood donors. Transfusion. 2009;49:1630–6. doi: 10.1111/j.1537-2995.2009.02189.x. [DOI] [PubMed] [Google Scholar]
- 53.Ditto B, Wilkins JA, France CR, Lavoie P, Adler PS. On-site training in applied muscle tension to reduce vasovagal reactions to blood donation. J Behav Med. 2003;26:53–65. doi: 10.1023/a:1021795022380. [DOI] [PubMed] [Google Scholar]
- 54.Kowalsky JM, France JL, Wissel ME, France CR. Effect of applied muscle tension on cerebral oxygenation in female blood donors. Transfusion. 2011;51:1802–8. doi: 10.1111/j.1537-2995.2011.03075.x. [DOI] [PubMed] [Google Scholar]
- 55.Masser BM, White KM, Hyde MK, Terry DJ, Robinson NG. Predicting blood donation intentions and behavior among Australian blood donors: testing an extended theory of planned behavior model. Transfusion. 2009;49:320–9. doi: 10.1111/j.1537-2995.2008.01981.x. [DOI] [PubMed] [Google Scholar]
- 56.Giles M, McClenahan C, Cairns E, Mallet J. An application of the Theory of Planned Behaviour to blood donation: the importance of self-efficacy. Health Educ Res. 2004;19:380–91. doi: 10.1093/her/cyg063. [DOI] [PubMed] [Google Scholar]
- 57.Masser BM, Bednall TC, White KM, Terry D. Predicting the retention of first-time donors using an extended Theory of Planned Behavior. Transfusion. 2012;52:1303–10. doi: 10.1111/j.1537-2995.2011.03479.x. [DOI] [PubMed] [Google Scholar]
- 58.France JL, France CR, Himawan LK. Re-donation intentions among experienced blood donors: does gender make a difference? Transfus Apher Sci. 2008;38:159–66. doi: 10.1016/j.transci.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 59.Veldhuizen I, Ferguson E, de Kort W, Donders R, Atsma F. Exploring the dynamics of the theory of planned behavior in the context of blood donation: does donation experience make a difference? Transfusion. 2011;51:2425–37. doi: 10.1111/j.1537-2995.2011.03165.x. [DOI] [PubMed] [Google Scholar]
- 60.Robinson NG, Masser BM, White KM, Hyde MK, Terry DJ. Predicting intentions to donate blood among nondonors in Australia: an extended theory of planned behavior. Transfusion. 2008;48:2559–67. doi: 10.1111/j.1537-2995.2008.01904.x. [DOI] [PubMed] [Google Scholar]