Abstract
Introduction
Single incision transumbilical laparoscopic procedures are the next step in development of minimally invasive surgery. Recent studies prove that the new technique can be a safe alternative to multiport laparoscopy; therefore it is becoming more and more popular.
Aim
We present our preliminary experience with single incision laparoscopy of the spleen.
Material and methods
We analyse a group of 9 patients (7 women and 2 men) in whom we attempted single incision laparoscopic surgery of the spleen.
Results
Single incision laparoscopy was successful in all patients – in 7 of them we performed splenectomy and in 2 unroofing of the splenic cyst. Additionally, in 3 patients we performed concomitant cholecystectomy. The operative technique was identical to multiport procedures. One patient required reoperation due to intra-abdominal bleeding from the wound on the first postoperative day. In one patient due to superficial injury of the stomach wall continuous suture was used to prevent perforation. In our opinion these complications are not the result of the new technique.
Conclusions
The described technique can become a safe alternative to multiport laparoscopy. It is a reasonable alternative in young patients to whom an excellent cosmetic effect is particularly important because until now it is the only documented advantage of this surgical technique.
Keywords: splenectomy, minimally invasive surgery, single access
Introduction
Laparoscopy has several indisputable advantages over open surgery regarding shorter hospital stay, faster recovery time, decreased intraoperative blood loss, wound infection rate and postoperative adhesion formation. Additionally, an improved cosmetic effect is becoming nowadays a more and more important factor for evaluation of the operation [1–3]. This approach has led surgeons to search for a technique which would allow one to perform an operation that leaves no scar in the abdomen. In 1997 Navarra described single incision transumbilical cholecystectomy, which from a practical point of view fulfilled the criteria of scar-less surgery [4]. Nowadays we can observe development of the very controversial and still very futuristic idea of natural orifice transluminal endoscopic surgery (NOTES). Despite the fact that the only documented advantage of single incision laparoscopic surgery is its better cosmetic effect, the popularity of this procedure is gradually increasing. It seems that the major reason for this fact is patients’ expectations. The number of centres which offer the new operative technique is rapidly growing. Furthermore, the number of studies concerning the use of this approach is increasing.
Laparoscopic splenectomy has been considered the “gold standard” for the elective surgical management of a variety of splenic disorders [5–9]. Until now, only a few case series studies describing single incision laparoscopic surgery of the spleen have been published. The first splenectomy which used the new technique in Poland was performed in 2009 in the Institute of Haematology in Warsaw.
Aim
The aim of our study was to evaluate the preliminary experience with single incision laparoscopic transumbilical surgery in patients with splenic disorder.
Material and methods
In our clinic we have performed more than 400 laparoscopic procedures of the spleen to date. Between March 2010 and October 2011, we attempted single incision laparoscopic surgery of the spleen in 9 patients: 7 men and 2 women with a median age of 22.3 years (range: 19-34 years) and body mass index of 23.3 kg/m2 (range: 20.4-26.6 kg/m2).
Single incision surgery was successful in all cases: in 7 of them we performed splenectomy and in 2 patients unroofing of the splenic cyst. The indications for splenectomy included haematological disorders: microspherocytosis (4 patients), idiopathic thrombocytopenic purpura (ITP) (2 patients), autoimmune haemolytic anaemia (1 patient). In 3 patients concomitant cholecystectomy (due to symptomatic cholelithiasis) with splenectomy was performed and utilized the same single transumbilical incision. In a further 2 patients we performed unroofing of the single splenic cyst (diameter 7 and 5 cm respectively) after exclusion of parasitic aetiology of the cyst (Table I).
Table I.
Demographic features of the study group
| No. | Gender | Age [years] | BMI [kg/m2] | Indication for operation | Longitudinal size of the spleen [cm] |
|---|---|---|---|---|---|
| 1 | F | 34 | 24.6 | ITP | 12 |
| 2 | F | 23 | 22.6 | ITP | 12 |
| 3 | F | 22 | 23.7 | Microspherocytosis/cholelithiasis | 16 |
| 4 | F | 21 | 22.4 | Microspherocytosis/cholelithiasis | 17 |
| 5 | F | 20 | 20.4 | Microspherocytosis/cholelithiasis | 14 (accessory spleen diameter 1 cm) |
| 6 | M | 20 | 26.7 | Microspherocytosis | 20 |
| 7 | F | 20 | 23.6 | Autoimmune haemolytic anaemia | 17 |
| 8 | M | 19 | 24.1 | Splenic cyst (diameter 7 cm) | 11 |
| 9 | F | 22 | 22.0 | Splenic cyst (diameter 5 cm) | 14 |
Preoperative management of all patients was identical to those undergoing multiport laparoscopic splenectomy in our department. In all of them the preoperative thrombocyte count was greater than 50 × 103/µl.
Operative technique
Generally the surgical technique was designed as a direct replication of standard multiport laparoscopic operations.
Patients were operated on in the right lateral decubitus position as during the equivalent, standard laparoscopic procedure (Photo 1). The access to the peritoneal cavity was achieved under direct visual control through a 2.5-3 cm incision and either a SILS port® (Covidien) or a TriPort® (Olympus) was introduced and pneumoperitoneum was established. After visual inspection of abdominal organs using a standard 10 mm 30° laparoscope, working instruments were inserted. For the first operation we used flexible instruments and the remaining eight were performed with standard straight instruments. The next steps of the operations were equivalent to multiport laparoscopic procedures. Opening the lesser sac and dissection of gastro-splenic ligament including short gastric vessels was performed with a harmonic scalpel (Photo 2). Later the splenic artery and vein were exposed and ligated with a clip (Photos 3, 4). The splenic hilum was then transected with Ligasure® (Photo 5). Patients in whom concomitant cholecystectomy was performed as a single-step procedure were then placed in a supine position and transabdominal Prolene® suture was used for better gallbladder retraction. Unroofing of the splenic cyst was performed with a harmonic scalpel. The inner lining of the cyst was cauterized with argon plasma. The incision in the abdominal wall was finally sutured with subcutaneous absorbable suture (Photo 6). We routinely do not use drains after single incision laparoscopic surgery.
Photo 1.
Patient and operating team position
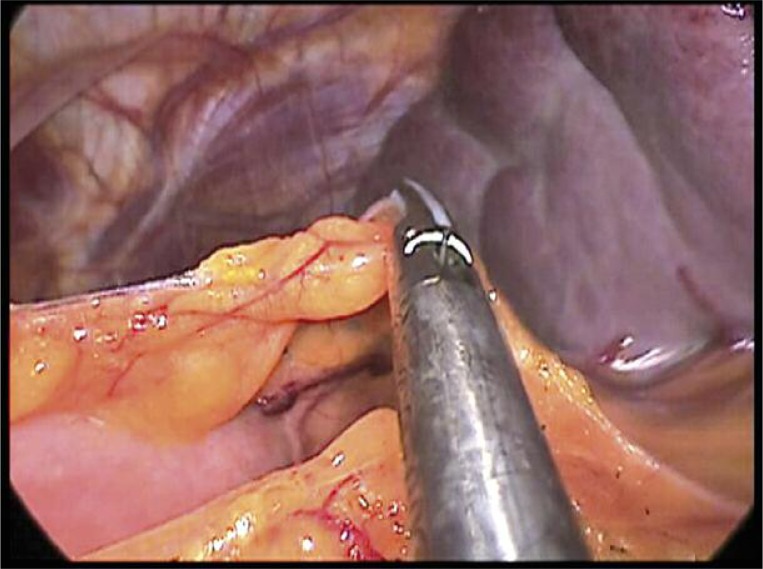
Photo 2.
Dissection of short gastric vessels
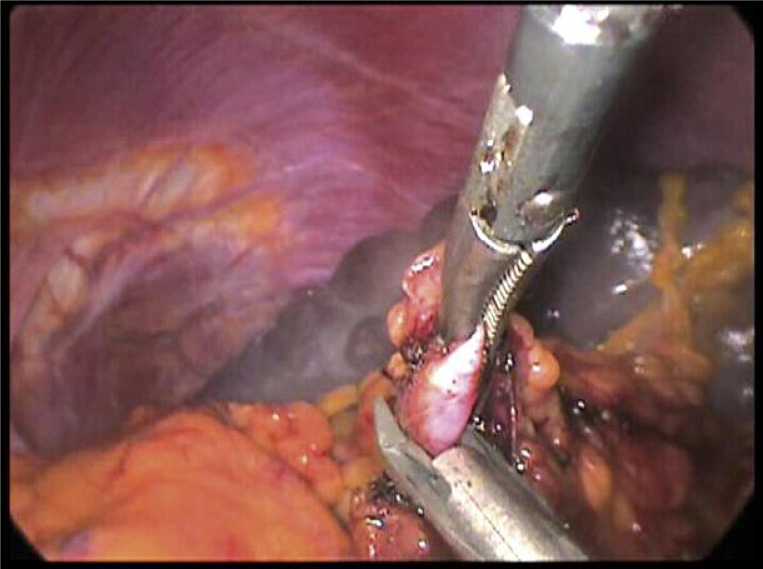
Photo 3.
Clipping of splenic artery
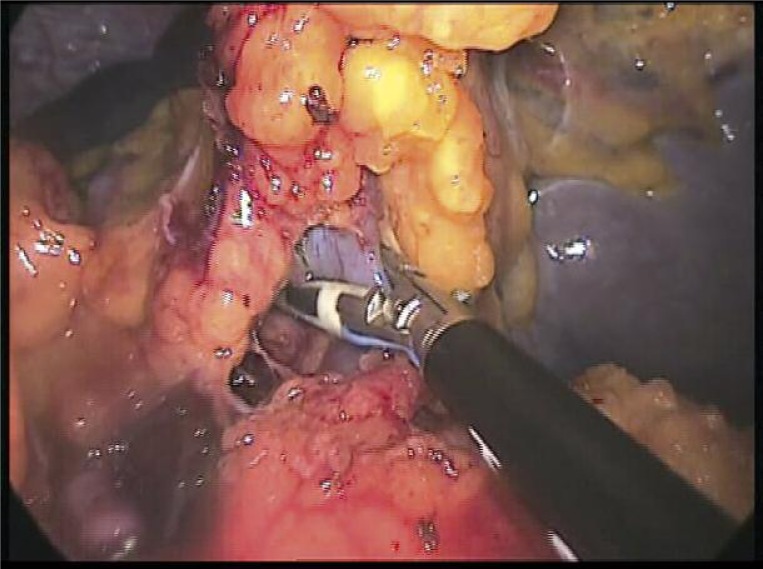
Photo 4.
Sealing splenic vein with Ligasure before application of clips from 5 mm applier
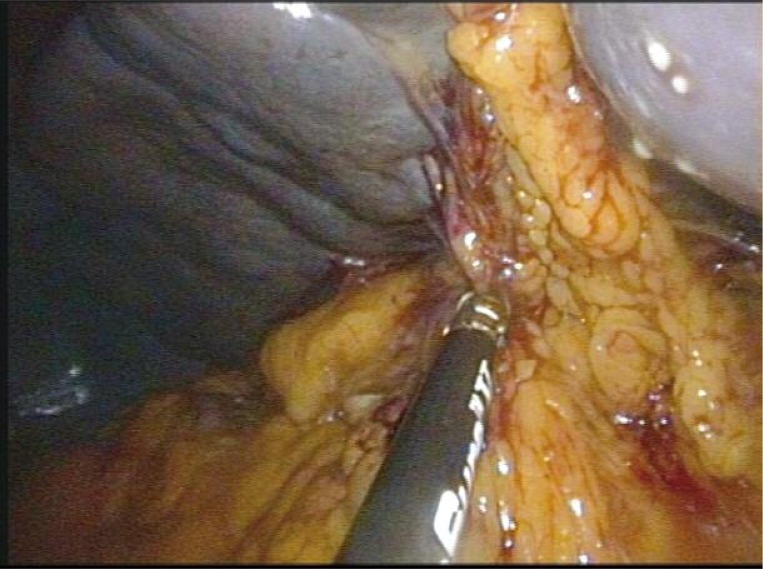
Photo 5.
Dissection of splenic hilum
Photo 6.
Umbilical wound directly after the operation
Results
All procedures were successfully performed without the need to introduce additional trocars. Median splenectomy time (excluding cholecystectomy time) was 125 min (range: 80-240 min), and splenic cyst unroofing 75 min (50 min and 100 min). Estimated blood loss was 35 ml in splenectomy cases and minimal in patients undergoing splenic cyst unroofing. In 1 patient after minor superficial thermal injury of the stomach wall continuous suture was used to strengthen the injured area and prevent perforation. One patient required reoperation on the first day after surgery because of minor intra-abdominal bleeding from the wound. Explorative intervention in this patient was also performed using the single incision technique and in this case drainage was placed through an additional incision.
Discussion
Nowadays, the cosmetic effect has become one of the major factors for evaluation of the operation. Expectations of patients, especially those well educated thanks to wide access to medical knowledge and the Internet, are rapidly growing. Moreover, their preferences have become an important element of the decision making process before the treatment strategy has even started. On the other hand, the recently invented NOTES technique (natural orifice transluminal endoscopic surgery), leaving no scar after the procedure, is not as attractive as it previously seemed. For some authors it is rather a dead end in development of minimally invasive surgery [10–12]. Therefore, as regards the cosmetic result, single incision laparoscopic transumbilical surgery is widely accepted to be a safe alternative to multiport laparoscopy. After the first report of Navarra many similar studies proving feasibility of the new technique were published [13–15]. Meanwhile the first results of successful adrenalectomy, nephrectomy, hernioplasty, as well as colon resection and bariatric procedures were released. There are also several case series of elective single incision laparoscopic splenectomy due to haematological disorders [16–21].
The first use of laparoscopic splenectomy in our institution dates back to 1998. To date we have performed more than 400 laparoscopic procedures of the spleen – elective and emergency splenectomy, partial splenectomy, splenic cyst removal and splenic artery aneurysm management. Long-lasting experience in these operations induced us to evaluate the possible use of the single incision laparoscopic technique. Due to better cosmetic results associated with the newer technique, we included in our study young patients for whom this aspect of treatment was particularly important.
Articulating laparoscopic instruments were used only during the first operation of a very tall patient. For all remaining procedures we used straight instruments and did not find any difficulties with dissecting surrounding tissues. Generally we believe that the single incision procedure undoubtedly requires the specialized instrumentation with a flexible tip; nonetheless, it is essential only during the initial phase of learning of this technique, and an experienced surgeon will probably not need it. However, these instruments may be useful during more complex procedures.
Three patients who underwent splenectomy and cholecystectomy as a one-step procedure benefited especially from the new technique. One port placed in the umbilicus allowed for both splenectomy and cholecystectomy, thus significantly reducing the number of postoperative wounds. We believe that despite the necessity of changing the patient's position during the operation, single incision surgery is a very convenient technique in this group of patients.
In our opinion complications that resulted in our patients were not associated with the new technique and could occur in a standard multiport laparoscopy study group as well. It is worth mentioning that the reoperation in the patient with postoperative bleeding was also carried out using single incision transumbilical access. No conversions to multiport laparoscopy or open procedure is most likely a result of the highly selected group of patients with normal body weight and no prior surgery. However, in any case of conversion, additional trocar placement is possible so that the operation is feasible as atypical multiport laparoscopy.
Undoubtedly, single incision laparoscopic procedures require more experience in minimally invasive surgery of the spleen. Specific instrument placement running in parallel to each other and the camera requires not only excellent coordination but also full cooperation with the assistant. Therefore this technique should preferably be performed by a more experienced surgical team.
Conclusions
Single incision surgical procedures are the next step in the development of minimally invasive surgery. For an experienced surgeon this technique may become a safe alternative to classical multiport laparoscopy. It may be considered in patients for whom an excellent cosmetic effect is extremely important. Additionally, by reducing the number of wounds, it can be very convenient in patients undergoing splenectomy and cholecystectomy as a one-step operation. However, due to the small number of case reports published worldwide with relatively short observation time, the better cosmetic result is currently the only documented advantage of this surgical procedure.
References
- 1.Carroll B, Phillips E, Semel C, et al. Laparoscopic splenectomy. Surg Endosc. 1992;6:183–5. doi: 10.1007/BF02210877. [DOI] [PubMed] [Google Scholar]
- 2.Katkhouda N, Hurwitz M, Rivera R, et al. Laparoscopic splenectomy: outcome and efficacy in 103 consecutive patients. Ann Surg. 1998;228:568–78. doi: 10.1097/00000658-199810000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Strzałka M, Bobrzyński A, Budzyński A, et al. Open or laparoscopic appendectomy? Videosurgery Miniinv. 2009;4:110–4. [Google Scholar]
- 4.Navarra G, Pozza A, Occhionorelli S, et al. One-wound laparoscopic cholecystectomy. Br J Surg. 1997;84:695. [PubMed] [Google Scholar]
- 5.Habermalz B, Sauerland S, Decker G, et al. Laparoscopic splenectomy: the clinical practice guidelines of the European Association for Endoscopic Surgery (EAES) Surg Endosc. 2008;22:821–48. doi: 10.1007/s00464-007-9735-5. [DOI] [PubMed] [Google Scholar]
- 6.Caprotti R, Porta G, Franciosi C, et al. Laparoscopic splenectomy for hematological disorders: our experience in adult and pediatric patients. Int Surg. 1998;83:303–7. [PubMed] [Google Scholar]
- 7.Glasgow R, Yee L, Mulvihill S. Laparoscopic splenectomy: the emerging standard. Surg Endosc. 1997;11:108–12. doi: 10.1007/s004649900308. [DOI] [PubMed] [Google Scholar]
- 8.Bagdasarian R, Bolton J, Bowen J, et al. Steep learning curve of laparoscopic splenectomy. J Laparoendosc Adv Surg Tech. 2000;10:319–23. doi: 10.1089/lap.2000.10.319. [DOI] [PubMed] [Google Scholar]
- 9.Delaitre B, Champault G, Barrat C, et al. Laparoscopic splenectomy for hematologic disease: study of 275 cases. French Society of Laparoscopic Surgery. Ann Chir. 2000;125:522–9. doi: 10.1016/s0003-3944(00)00236-4. [DOI] [PubMed] [Google Scholar]
- 10.Ciesielczyk B, Cwaliński J, Janusz P. Robotic surgery and NOTES – Natural Orifice Translumenal Endoscopic Surgery in treatment of cholelithiasis: revolution or failed conception. Pol Merkur Lekarski. 2008;25:380–5. [PubMed] [Google Scholar]
- 11.Jähne J. NOTES: quo vadis? Chirurg. 2010;81:405–6. doi: 10.1007/s00104-009-1826-5. [DOI] [PubMed] [Google Scholar]
- 12.Pearl J, Ponsky J. Natural orifice translumenal endoscopic surgery: a critical review. J Gastrointest Surg. 2008;12:1293–300. doi: 10.1007/s11605-007-0424-4. [DOI] [PubMed] [Google Scholar]
- 13.Prashanth P, Pradeep P, Sonali B. Single-incision laparoscopic surgery – current status and controversies. J Minim Access Surg. 2011;7:6–16. doi: 10.4103/0972-9941.72360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Phillips M, Marks J, Roberts K, et al. Intermediate results of a prospective randomized controlled trial of traditional four-port laparoscopic cholecystectomy versus single-incision laparoscopic cholecystectomy. Surg Endosc. 2012;26:1296–303. doi: 10.1007/s00464-011-2028-z. [DOI] [PubMed] [Google Scholar]
- 15.Lai E, Yang G, Tang C, et al. Prospective randomized comparative study of single incision laparoscopic cholecystectomy versus conventional four-port laparoscopic cholecystectomy. Am J Surg. 2011;202:254–8. doi: 10.1016/j.amjsurg.2010.12.009. [DOI] [PubMed] [Google Scholar]
- 16.Colon M, Telem D, Chan E, et al. Laparoendoscopic single site (LESS) splenectomy with a conventional laparoscope and instruments. JSLS. 2011;15:384–6. doi: 10.4293/108680811X13125733356918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Champagne B, Papaconstantinou H, Parmar S, et al. Single-incision versus standard multiport laparoscopic colectomy: a multicenter, case-controlled comparison. Ann Surg. 2012;255:66–9. doi: 10.1097/SLA.0b013e3182378442. [DOI] [PubMed] [Google Scholar]
- 18.Budzyński A, Matłok M, Pędziwiatr M, et al. SILS (single incision laparoscopic surgery) – new surgical approach to peritoneal cavity. Adv Med Sci. 2011;56:18–24. doi: 10.2478/v10039-011-0007-1. [DOI] [PubMed] [Google Scholar]
- 19.Huang C. Single-incision laparoscopic bariatric surgery. J Minim Access Surg. 2011;7:99–103. doi: 10.4103/0972-9941.72397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bobowicz M, Michalik M, Orłowski M, et al. Bariatric single incision laparoscopic surgery – review of initial experience. Videosurgery Miniinv. 2011;6:48–52. [Google Scholar]
- 21.Budzyński A, Pędziwiatr M, Matłok M, et al. Preliminary experience with transperitoneal single incision laparoscopic surgery adrenalectomy. Videosurgery Miniinv. 2010;5:87–92. [Google Scholar]