Abstract
Introduction
Laparoscopic adjustable gastric banding (LAGB) is effective for weight reduction in severely obese patients. However, the data about its effect on metabolic syndrome (MS) are limited.
Aim
To assess weight loss and changes of metabolic parameters 1 year after LAGB in a prospective, nonrandomized single center cohort study in morbidly obese subjects.
Material and methods
Physical examination, body weight (BW) parameters and metabolic profile were assessed at baseline and 1 year after LAGB in morbidly obese subjects. The incidence of MS was evaluated according to National Cholesterol Education Program Adult Treatment Panel III criteria.
Results
One year after the operation data from 90 patients out of 103 were available. Mean excess weight (EW) loss of 33.1% was associated with a significant improvement in all metabolic parameters: decrease of hypertension by 15.8%, hypertriglyceridemia by 42.6%, and hyperglycemia by 46.3%; and increase in high density lipoprotein cholesterol by 48.3%. This resulted in the resolution of MS in 44.2% of subjects. The significant change in the distribution of MS components was observed with the highest frequency of 4 components before and 2 components after surgery. Patients with MS at baseline lost 29.9% of EW compared to 44.3% in those without MS (p = 0.009).
Conclusions
The LAGB resulted in effective reduction of BW parameters in morbidly obese subjects 1 year after the operation. Along with the weight loss, resolution of MS and a significant shift towards decrease in the number of MS components was observed. Patients with MS were more resistant to the weight loss.
Keywords: obesity, metabolic syndrome, bariatric surgery, laparoscopic adjustable gastric banding
Introduction
Obesity has become a global epidemic. Currently, an estimated 1.1 billion people worldwide are overweight or obese and at least 2.8 million are dying each year as a result of it [1]. Obesity dramatically increases the risk of other comorbidities such as cardiovascular disease (CVD), type 2 diabetes (T2DM), dyslipidemia, joint disease, obstructive sleep apnea, polycystic ovary syndrome, different types of cancer (breast, colon, prostate, endometrial, ovarian, kidney and gall bladder), non-alcoholic steatohepatitis and others [2]. Some of the comorbidities are closely interrelated and are described as the metabolic syndrome (MS), the prevalence of which is about 50-60% [3–5] in obese subjects.
The treatment of MS remains challenging, as the pharmacological approach addresses the individual components of MS – arterial hypertension (AH), dyslipidemia, high plasma glucose – while obesity, as a key component, remains untargeted. As obesity management with oral medications is limited, bariatric surgery remains the method of choice for sustained weight loss. Different studies have shown that the incidence of concomitant diseases and the long-term mortality can be reduced by up to 62-77% and 40% respectively as a consequence of weight reduction [6, 7].
According to the National Institute of Health guidelines established in 1991 and updated by the American Association of Clinical Endocrinologists, The Obesity Society and the American Society for Metabolic and Bariatric Surgery (AACE/TOS/ASMBS) in 2008, patients are eligible for bariatric surgery if they have failed nonsurgical treatments and have a body mass index (BMI) over 40 kg/m2 or over 35 kg/m2 with comorbidities [8]. The American Diabetes Association also included bariatric surgery in the diabetes treatment algorithm for subjects with BMI > 35 kg/m2 and concomitant diseases [9].
The anatomical changes created with different types of procedures lead to variable degrees of weight loss and modification of metabolic parameters. Many studies show a positive influence of Roux-en-Y gastric bypass (RYGB) operation on the components of MS [10–13] but data on the effect of laparoscopic adjustable gastric banding (LAGB) are controversial. Some authors describe favorable weight loss and resolution of comorbidities [14–18], while others observe insufficient weight loss and a progressive decline in effectiveness over the years [19–21]. Also, there are limited data on the influence of metabolic surgery on MS as a whole rather than on separate components.
Aim
The aim of our prospective, nonrandomized single center cohort study was to assess the effect of LAGB on body weight and changes of metabolic parameters from baseline to 1 year after the procedure in morbidly obese subjects.
Material and methods
The study protocol was approved by the Lithuanian Bioethics Committee on November 6, 2008.
Subjects recruitment
All subjects included in our study were recruited from Vilnius University Hospital Santariskiu Klinikos Outpatient Clinic, where they had been referred for obesity surgery. Men and women aged 18-70 years with a BMI more than 40 kg/m2 and with BMI between 35 kg/m2 and 40 kg/m2 with associated comorbidities were considered eligible for surgical treatment. Exclusion criteria were contraindications for laparoscopy, previous bariatric surgery, pregnancy and patient's refusal. Signed informed consent was obtained from all patients. Patients were randomly assigned to groups by choosing from two identical sealed envelopes with a different band name inside. The Swedish Adjustable Gastric Band (SAGB) was used in 49 patients and the MiniMizer Extra in 54 patients.
Subjects assessment
Extensive preoperative evaluation was done by a multidisciplinary team, consisting of an endocrinologist, gastroenterologist, dietician, cardiologist and bariatric surgeon. Physical examination, anthropometric and blood pressure measurements, blood tests, 12-lead electrocardiogram (ECG), upper gastrointestinal tract endoscopy, and abdominal sonoscopy were performed in all included patients according to the study protocol. Body weight (BW) was measured and body composition analysis (hand-to-foot bioelectrical impedance analysis) for body fat mass (FM) and percent of fat mass (%FM) evaluation was performed. Fat mass evaluation was possible only if %FM did not exceed 50% (technical limitation of the bioelectrical impedance analysis device); thus all patients with %FM more than 50% were involved in statistical analysis as if they had 50% of %FM. Excess body weight (EW) was calculated using the formula: EW = (body weight) – (upper limit of normal body weight).
Upper limit of normal body weight is body weight if patients’ BMI was 25 kg/m2 and is calculated by the following formula: upper limit of normal body weight = (height in meters)2 × 25.
Excess body mass index (EBMI) was calculated by subtracting 25 kg/m2 from BMI.
Blood samples for laboratory analyses were collected after 12 h fasting. Laboratory tests included assessment of serum lipids (total cholesterol (Chol), triglycerides (TG), high density lipoprotein cholesterol (HDL), low density lipoprotein cholesterol (LDL)), plasma glucose (Glu) and glycosylated hemoglobin (HbA1c) and were performed at Vilnius University Hospital Santariškių Klinikos, Centre of Laboratory Diagnostics, using standard laboratory methods.
Patients were diagnosed with metabolic syndrome if they fulfilled three or more of the revised National Cholesterol Education Program Adult Treatment Panel III (NCEP ATPIII) criteria:
waist circumference ≥ 102 cm in males, ≥ 88 cm in females,
TG ≥ 1.7 mmol/l,
HDL < 1.03 mmol/l in males and < 1.29 mmol/l in females,
blood pressure ≥ 130/85 mm Hg,
During the course of data analysis all subjects were divided into 2 groups, with metabolic syndrome (MS group) and without MS (nonMS group), according to these criteria.
Surgical procedures
All patients underwent LAGB. Pars flaccida technique was used for both bands: the Swedish Adjustable Gastric Band and the MiniMizer Extra [24]. Surgical techniques have been described in more detail previously [25].
Patients with normal condition were discharged from the hospital on the second postoperative day with written diet instructions provided.
Follow-up assessment
The band adjustment rate was not influenced by the study protocol and was performed according to the accepted standards of the clinic. The patients were asked to arrive for band adjustment in the case of ceasing to lose weight for more than 2 weeks, but not earlier than 4 weeks after the operation. All other adjustments were also performed in case of ceasing to lose weight for more than 2 weeks, but not earlier than 4 weeks after previous adjustment.
Patients were instructed to return for a follow-up visit one year after the operation for extensive assessment by the same multidisciplinary team. The same laboratory blood tests, upper gastrointestinal tract endoscopy, ECG, and body composition analysis were repeated. The main endpoints were changes in body weight and metabolic parameters in the whole group and comparison between subjects with and without MS, irrespectively of which surgical method was used for LAGB. Patients whose band had to be removed were excluded from further weight loss analysis.
Statistical analysis
All descriptive data are shown as a percentage or as the mean with the standard deviation, and the numbers of male and female patients are shown as a ratio. Differences in age, height, body weight, BMI, fat mass, absolute and percentage of excess body weight, excess BMI, waist circumference and biochemical parameters in patients at baseline and 1 year after were evaluated with Mann-Whitney-Wilcoxon nonparametric test. Gender and MS components distribution between groups of patients at baseline and 1 year after was compared using Fisher's exact test. Comparison of changes in obesity measures in MS and nonMS patients at baseline and 1 year after the surgical procedure was assessed with Fisher's exact test. Statistical analysis was carried out with SPSS (SPSS Inc., Chicago, Illinois 60606, USA) and SAS software (SAS Institute Inc., Cary, NC 27513 USA). The α risk was set as 5% for all tests and a ρ value of < 0.05 was considered statistically significant.
Results
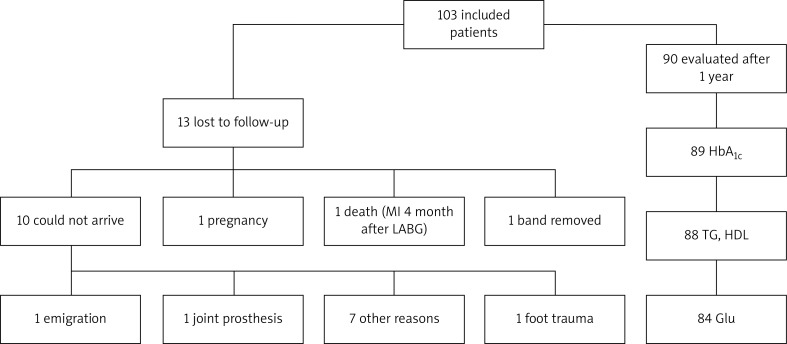
There were 103 laparoscopic gastric bandings performed by a single surgeon in morbidly obese subjects between the 1st of January 2009 and the 31st of January 2010. The group was unequal with respect to gender: there were more women than men. Thirteen patients were lost to follow up after 1 year: 8 women and 5 men. Three of them were excluded from further weight loss analysis: 1 patient was excluded because of an early band penetration and removal; 1 died from an acute myocardial infarction (MI) 4 months after LAGB operation and 1 woman became pregnant. The other ten who could not arrive were contacted by phone and data about weight loss and blood-pressure were registered. Also, there were some missing data for patients who arrived after one year. A follow-up flow diagram is presented in Figure 1.
Figure 1.
Study population follow-up flow diagram
Patients’ bands were adjusted an average of 2.5 times during the first year after the operation: 2.7 ±2.2 times (range: 0-10) in the SAGB group and 2.4 ±1.2 times (range: 0-5) in the MiniMizer Extra group (p = 0.514).
The main characteristics of the patients at baseline and 1 year after the operation are presented in Table I. One hundred and three patients had baseline age 45.9 ±11.7 years, BMI 47.5 ±7.4 kg/m2 and EW 46.11%. Significant reduction in body weight was evident in almost all subjects after 1 year. There were only 2 patients who failed to lose weight: one remained at the same weight and the other gained 4.3 kg in 1 year. The mean weight loss was 20.4 ±11.9 kg, which corresponded to 14.4% weight loss and 33.1% excess weight loss as well as excess BMI loss (EBMIL). Along with weight reduction we observed an improvement of all evaluated metabolic parameters. Modification of weight parameters and metabolic profile 1 year after the operation is shown in Table I.
Table I.
Main characteristics of the group at baseline and 1 year after the operation
| Variables | Baseline (n = 103) | One year after (n = 90) | Value of p | Absolute difference |
|---|---|---|---|---|
| Gender, males/females | 34/69 | 29/61 | NS | N/A |
| Age [years] | 45.9 ±11.7 | 46.1 ±11.2 | NS | N/A |
| Height [cm] | 170.2 ±10.0 | 170.1 ±10.0 | NS | N/A |
| Body weight [kg] | 137.7 ±24.4 | 117.3 ±24.9 | < 0.0001 | 20.4 ±11.95 |
| BMI [kg/m2] | 47.5 ±7.4 | 40.9 ±8.4 | < 0.0001 | 6.6 ±3.96 |
| Fat mass [kg] | 60.4 ±12.9 | 47.6 ±13.4 | < 0.0001 | 12.8 ±7.57 |
| Excess body weight [kg] | 65.0 ±21.2 | 46.0 ±23.9 | < 0.0001 | 19 ±15.3 |
| Excess body weight [%] | 46.11 ±8.2 | 36.35 ±13.1 | < 0.0001 | 9.76 ±7.57 |
| Excess BMI [kg/m2] | 22.5 ±7.4 | 15.9 ±8.4 | < 0.0001 | 6.6 ±5.13 |
| Waist circumference [cm] | 136.0 ±18.0 | 119 ±18.5 | < 0.0001 | 17 ±9.82 |
| TG [mmol/l] | 2.30 ±1.73 | 1.68 ±1.27 | < 0.0001 | 0.62 ±0.80 |
| HDL [mmol/l] | 1.18 ±0.34 | 1.34 ±0.34 | < 0.0001 | –0.16 ±0.24 |
| Glu [mmol/l] | 6.36 ±2.28 | 5.48 ±1.0 | 0.003 | 0.88 ±1.35 |
| HbA1c [%] | 6.18 ±1.19 | 5.57 ±0.58 | < 0.0001 | 0.61 ±0.85 |
BMI – body mass index, TG – triglycerides, HDL – high density lipoprotein cholesterol, Glu – fasting plasma glucose, HbA1c – glycosylated hemoglobin
Although all subjects were morbidly obese, not everybody had all criteria to be diagnosed with the metabolic syndrome at baseline. Increased waist circumference was the only one feature characteristic for all subjects. All other criteria of MS varied in frequency, resulting in 77 (out of 103) and 43 (out of 90) subjects with metabolic syndrome before and 1 year after the operation, respectively, as shown in Table II. After 1 year a 44.2% decrease in prevalence of MS was observed. The decrease of separate components of MS was also evident and significant, ranging from 15.8% for hypertension to 48.3% for HDL cholesterol (Table II).
Table II.
Frequency of MS and MS diagnostic criteria at baseline and 1 year after the operation
| Variables | Baseline (n = 103) | Decrease (n = 90) | Decrease [%] |
|---|---|---|---|
| MS, n | 77 | 43 | 44.2 |
| Valid% | 76.2 | 51.8 | |
| Waist circumference, n | 103 | 77 | 25.2 |
| Valid% | 100 | 92.8 | |
| Hypertension, n | 82 | 69 | 15.8 |
| Valid% | 79.6 | 67.6 | |
| TG, n | 54 | 31 | 42.6 |
| Valid% | 52.4 | 35.2 | |
| HDL, n | 58 | 30 | 48.3 |
| Valid% | 56.3 | 34.1 | |
| Glu, n | 54 | 29 | 46.3 |
| Valid% | 52.4 | 34.5 |
MS – metabolic syndrome, TG – triglycerides, HDL – high density lipoprotein cholesterol, Glu – fasting plasma glucose
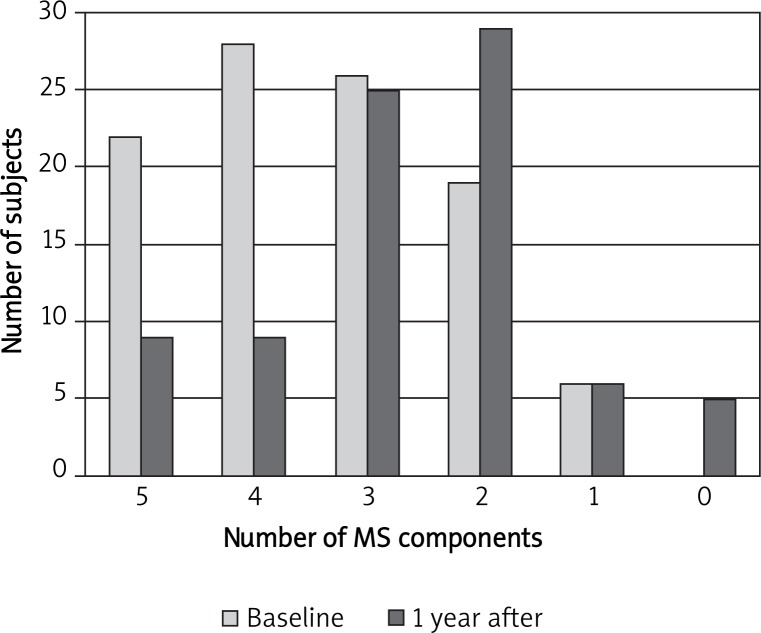
Analysis of the number of MS components in each patient revealed that there was no subject at baseline without at least one component of MS. Most subjects – 66 out of 103 – had from 3 to 5 components, with the highest frequency of 4 components in 28 patients. One year after the operation there was a significant shift towards fewer MS components for each subject, with the highest frequency of 2 in 29 patients. Of note, 5 patients had no components of MS 1 year after, as presented in Figure 2.
Figure 2.
Comparison of the distribution of me - tabolic syndrome components in all subjects at baseline and 1 year after the operation (p < 0.0001)
To assess the possible effect of the presence of MS on weight loss, we compared data between two groups: patients with MS (MS group) and patients without MS (nonMS group). At baseline there were 77 subjects in the MS group and 24 in the nonMS group. One year after the operation only 43 remained in the MS group and 21 in the nonMS group. All obesity measures were significantly higher in the MS group compared to the nonMS group at baseline, as follows: body weight 142.4 kg vs. 124.2 kg (p = 0.001), excess body weight 69.2 kg vs. 52.7 kg (p = 0.001), BMI 48.8 kg/m2 vs. 43.7 kg/m2 (p = 0.003), EBMI 23.8 kg/m2 vs. 18.7 kg/m2 (p = 0.003) respectively. The absolute change in obesity parameters was the same in both groups 1 year after operation, but the percentage change was significantly higher in the nonMS group (Table III), indicating that patients without MS lost more weight, compared to those with MS.
Table III.
Comparison of changes in obesity measures in MS and nonMS subject groups at baseline and 1 year after the operation
| Parameter | MS | nonMS | Value of p | ||||
|---|---|---|---|---|---|---|---|
| Baseline (n = 77) | 1 year after (n = 43) | Change [%] | Baseline (n = 24) | 1 year after (n = 21) | Change [%] | ||
| BW [kg] | 142.4 ±24.3 | 120.7 ±24.4 | 13.5 ±8.3 | 124.2 ±19.3 | 103.2 ±18.6 | 17.74 ±8.0 | 0.016 |
| EW [kg] | 69.2 ±21.8 | 48.9 ±23.1 | 29.9 ±19.8 | 53.6 ±13.3 | 31.4 ±17.14 | 44.3 ±25.1 | 0.009 |
| FM [kg] | 61.3 ±13.0 | 49.5 ±13.8 | 19.4 ±12.3 | 55.4 ±9.2 | 41.4 ±10.4 | 25.7 ±12.9 | 0.026 |
| BMI [kg/m2] | 48.8 ±7.6 | 42.2 ±8.5 | 13.5 ±8.3 | 44.0 ±5.2 | 36.3 ±6.5 | 17.7 ±8.0 | 0.016 |
| EBMI [kg/m2] | 23.8 ±7.6 | 17.2 ±8.5 | 29.9 ±19.8 | 19.0 ±5.2 | 11.3 ±6.5 | 44.4 ±25.1 | 0.009 |
Value of p – to compare % of change between MS and nonMS groups. BW – body weight, EW – excess weight, FM – fat mass, BMI – body mass index, EBMI – excess body mass index
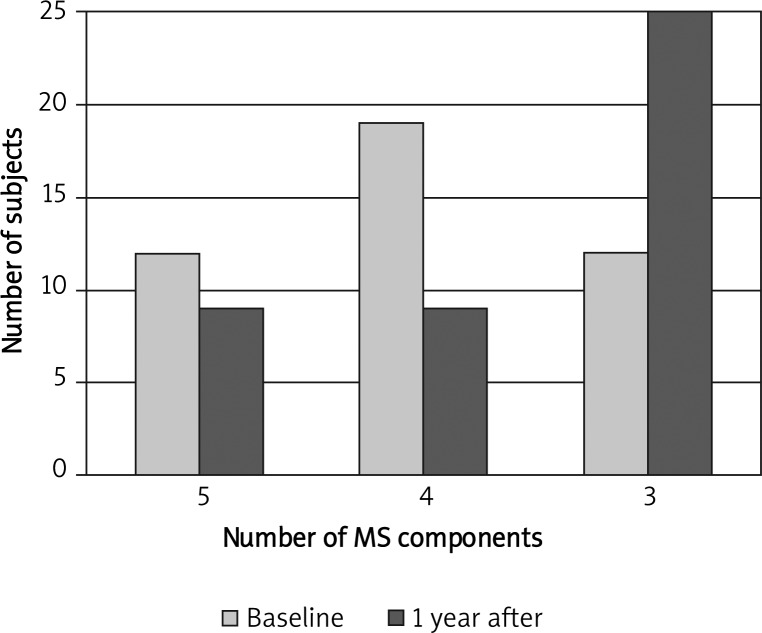
Although the operation had an obvious positive metabolic effect – 34 patients (44%) out of 77 recovered from MS – there were still 43 left with MS after 1 year. However, there was a significant shift towards a decrease in the number of metabolic syndrome components for each subject even in this group, as presented in Figure 3. These data, where the highest frequency of 4 components (in 19 patients out of 43) was observed at baseline and 3 components (in 25 patients out of 43) 1 year after operation, mimic the tendency observed in the whole group (Figure 2).
Figure 3.
Changes in the components of metabolic syndrome in 43 patients who remained with metabolic syndrome 1 year after surgery (p = 0.016)
To assess the possible relation of weight loss and components of MS, we performed correlation analysis. However, no relation between TG, HDL cholesterol or fasting plasma glucose and weight loss parameters was found. Waist circumference was the only MS component that significantly correlated with all weight loss parameters: percentage of weight loss (%WL) and percentage of BMI loss (%BMIL) (r = 0.764, p < 0.0001), percentage of excess weight loss (%EWL) and percentage of excess BMI loss (%EBMIL) (r = 0.630, p < 0.0001), and percentage of fat mass loss (%FML) (r = 0.658, p < 0.0001).
Discussion
Weight loss and resolution of comorbidities should be a major endpoint in the studies of metabolic surgery. Although it is widely accepted that it reduces morbidity and mortality in general, there is still a discussion about the effect of such surgery on MS.
Our study aimed to assess the effect of LAGB on MS and its components, as well as body weight parameters, at baseline and 1 year after the procedure in morbidly obese subjects. We found that obesity treatment in morbidly obese subjects with and without metabolic syndrome using laparoscopic adjustable gastric banding effectively reduces body weight and significantly improves metabolic parameters. It is known from previous studies that 10% BW loss can lead to resolution of a number of adiposity-related comorbidities [26]. In our study, following surgery subjects lost on average 20 kg, which corresponded to 14.4% of BW, which is an even larger weight loss, reached in a relatively short period of time. The average excess weight loss (EWL) of 33.1% and the reduction of BMI by 6.6 kg/m2 in our study was consistent with the results of others, but of smaller magnitude. According to different authors, %EWL after LAGB varies from 26% to 60% in 1 year after the operation [20, 27–34]. The median %EWL of 33.1 reached in our study is 7% above the lowest level of published data. Interpreting this result we have considered several possible limitations of the study. Although all patients were instructed to arrive in case of ceasing to lose weight, we did not apply a protocol for scheduled visits for further band adjustments after the operation. Regular professional evaluation of effectiveness of weight loss would have possibly increased weight loss success. Also, although all subjects were educated regarding their diet after the procedure, the lack of preoperative education, face-to-face dietitian consultation and the assessment of eating habits and their life style needs to be admitted. It is proved that education, tight supervision and support for life-style changes after LAGB are crucially important for a sufficient and long standing effect of weight loss. This was shown by Steffen et al., who observed significantly better results in weight loss and resolution of comorbidities in a 7-year prospective study where multi-intervention treatment and intensive follow-up support was applied [14]. Finally, the senior population in our study, compared to the others, could also explain the lower %EWL, as it becomes more difficult to reduce body weight with increasing age [35–38].
Despite relatively moderate weight loss, we observed a significant improvement in metabolic parameters. The average decrease in fasting plasma glucose was 0.88 mmol/l, decrease in TG was 0.62 mmol/l, and increase in HDL was 0.16 mmol/l, compared to 0.69-0.8 mmol/l, 0.5-0.75 mmol/l and 0.1-0.14 mmol/l respectively in other studies that have also investigated the effect of LAGB in obese patients [39–41].
We observed a reduction of all components of MS, with the best results for HDL and the poorest for hypertension. To our best knowledge the most extensive meta-analysis of similar studies is reported by Buchwald et al. [6], where weigh loss parameters and the resolution of comorbidities are described. The authors reported an average recovery from AH after LAGB of 38%, while in our study only 16% of the patients reached a resolution of AH. However, in this meta-analysis the data are presented after 2 years of follow-up after LAGB and the shorter period of observation in our study could explain the difference.
Resolution of hyperglycemia, hypertriglyceridemia and HDL cholesterol dyslipidemia was the same for all variables in our study and varied from 40% to 50%. These changes resulted in a significant reduction of the incidence of MS: there were 76% of subjects with MS before and only 52% 1 year after the operation. Moreover, an evident redistribution downstream of the number of MS components was observed, resulting in a general health improvement. Significant reduction of the incidence of MS (according to ATP III criteria) was also demonstrated by Gasteyger et al., who reported the change from initial 58% to 25% 1 year after the operation [3]. Even more dramatic reduction of MS was reported by Lee et al., who applied another restrictive procedure – vertical banded gastroplasty. The author observed resolution of MS in 95% of subjects 1 year after the operation [4].
However, although the decrease of the incidence of metabolic syndrome in our study was consistent with the others, the main difference should be admitted: the prevalence of MS in our study before the operation was significantly higher (76%) than that reported in the studies mentioned previously (50-60%). The prevalence of separate MS components was more than twice as high as in the meta-analysis of Buchwald et al.: hypertension 80% vs. 35%, hypertriglyceridemia 53% vs. 24%, impaired glucose tolerance or type 2 diabetes 41% vs. 52% of elevated fasting plasma glucose respectively. The average means of MS parameters in our patients were also greater than those reported in most studies [39–41]. Thus, we could speculate that more pronounced dysmetabolic status could have an influence on the resolution of MS and the susceptibility to lose weight.
To better assess this hypothesis we compared patients with and without MS. A significant difference was observed between the MS and nonMS group in all weight loss parameters 1 year after the operation: %WL – 13.5% vs. 17.7%; %EWL – 29.9% vs. 44.3; %FML – 19.4% vs. 25.7; %BMIL – 13.5% vs. 17.7; %EBMIL – 29.9% vs. 44.4 respectively. Results from the very few studies comparing the difference in weight loss between MS and nonMS groups after conventional treatment are controversial. Evangelou et al. revealed that obese or overweight women with MS treated with diet and, if necessary, medical therapy (orlistat or sibutramine) lose weight more effectively than those without MS [42]. In contrast, Pinkston et al. observed no difference in weight loss between MS and nonMS women groups treated with orlistat [43]. Our data indicated significantly higher body weight decrease in the group without MS at baseline, compared to those with MS; however, further investigations are needed, as to our best knowledge, this is the first study analyzing weight loss in MS and nonMS groups after LAGB in adults. Changes in the secretion of adipokines and gut hormones regulating metabolism and appetite in MS could have an influence on success in losing weight, and this has to be addressed in further research.
No significant correlations were found between weight loss parameters (%WL, %EWL, %FML, %BMIL, %EBMIL) and components of MS, except for waist circumference, showing that improvement in the metabolic profile appeared to be independent of the degree of weight loss. These results are consistent with some other studies in obese premenopausal women [41], adolescents [44] and diabetics [45] after LAGB. We could hypothesize that possibly there are other factors that serve as a link between weight change and MS components and are specific only for those having metabolic syndrome.
This study is limited by the lack of a control group undergoing conventional diet and exercise. The shortness of the study creates a limitation for making conclusions about the long-term impact of LAGB on the metabolic parameters; however, long-term follow up is ongoing, with a goal of a total of 5 years of postsurgical follow-up. Also, resolution was the only dimension by which comorbidities in our study were assessed. Reporting the improvement could be useful for short follow-up studies, where the short duration of the study may be insufficient for resolution.
Conclusions
Laparoscopic gastric banding resulted in effective reduction in body weight in morbidly obese patients 1 year after the operation. Along with the weight loss, resolution of MS and a significant shift towards decrease in the number of metabolic syndrome components was observed. Although no correlation was established between weight loss and the change in metabolic parameters, patients with MS were more resistant to weight loss. These findings indicate that LAGB could be a useful tool to reduce cardiovascular risk in severely obese adults, but further follow-up data are needed to assess whether the observed differences remain and contribute to the improvement of long-term prognosis. Our study adds to the limited literature documenting the effectiveness of LAGB in achieving not only weight loss, but also resolution of comorbidities, particularly MS in morbidly obese adults.
References
- 1.Dixon JB, Murphy DK, Segel JE, et al. Impact of laparoscopic adjustable gastric banding on type 2 diabetes. Obes Rev. 2012;13:57–67. doi: 10.1111/j.1467-789X.2011.00928.x. [DOI] [PubMed] [Google Scholar]
- 2.Runkel N, Colombo-Benkmann M, Hüttl TP, et al. Bariatric surgery. Dtsch Arztebl Int. 2011;108:341–6. doi: 10.3238/arztebl.2011.0341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gasteyger C, Suter M, Calmes JM, et al. Changes in body composition, metabolic profile and nutritional status 24 months after gastric banding. Obes Surg. 2006;16:243–50. doi: 10.1381/096089206776116381. [DOI] [PubMed] [Google Scholar]
- 4.Lee WJ, Huang MT, Wang W, et al. Effects of obesity surgery on the metabolic syndrome. Arch Surg. 2004;139:1088–92. doi: 10.1001/archsurg.139.10.1088. [DOI] [PubMed] [Google Scholar]
- 5.Kwiatkowski A, Paśnik K, Stanowski E, Badyda A. Regression of metabolic syndrome depending on type of bariatric surgery. Videosurgery Miniinv. 2009;4:53–8. [Google Scholar]
- 6.Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37. doi: 10.1001/jama.292.14.1724. [DOI] [PubMed] [Google Scholar]
- 7.Sjöström L, Narbro K, Sjöström D, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741–52. doi: 10.1056/NEJMoa066254. [DOI] [PubMed] [Google Scholar]
- 8.Mechanick JI, Kushner RF, Sugerman HJ, et al. American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery Medical Guidelines for Clinical Practice for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient. Surg Obes Rel Dis. 2008;44:S109–84. doi: 10.1016/j.soard.2008.08.009. [DOI] [PubMed] [Google Scholar]
- 9.Executive Summary: Standards of Medical Care in Diabetes - 2009. Diabetes Care. 2009;32:S6–12. doi: 10.2337/dc09-S006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Proczko-Markuszewska M, Kaska Ł, Stefaniak T, et al. Surgical treatment of a non-obese patient with type 2 diabetes – primary experience – a case report. Videosurgery Miniinv. 2011;6:99–102. [Google Scholar]
- 11.Ashrafian H, Athanasiou T, Li JV, et al. Diabetes resolution and hyperinsulinaemia after metabolic Roux-en-Y gastric bypass. Obes Rev. 2011;12:257–72. doi: 10.1111/j.1467-789X.2010.00802.x. [DOI] [PubMed] [Google Scholar]
- 12.Hofsø D, Nordstrand N, Johnson LK, et al. Obesity-related cardiovascular risk factors after weight loss: a clinical trial comparing gastric bypass surgery and intensive lifestyle intervention. Eur J Endocrinol. 2010;163:735–45. doi: 10.1530/EJE-10-0514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ali MR, Fuller WD, Rasmussen J. Detailed description of early response of metabolic syndrome after laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2009;5:346–51. doi: 10.1016/j.soard.2008.10.014. [DOI] [PubMed] [Google Scholar]
- 14.Steffen R, Potoczna N, Bieri N, Horber FF. Successful multi-intervention treatment of severe obesity: a 7-year prospective study with 96% follow-up. Obes Surg. 2009;19:3–12. doi: 10.1007/s11695-008-9675-8. [DOI] [PubMed] [Google Scholar]
- 15.O'Brien PE, McPhail T, Chaston TB, Dixon JB. Systematic review of medium-term weight loss after bariatric operations. Obes Surg. 2006;16:1032–40. doi: 10.1381/096089206778026316. [DOI] [PubMed] [Google Scholar]
- 16.Schouten R, Wiryasaputra DC, van Dielen FM, et al. Long-term results of bariatric restrictive procedures: a prospective study. Obes Surg. 2010;20:1617–26. doi: 10.1007/s11695-010-0211-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Biagini J, Karam L. Ten years experience with laparoscopic adjustable gastric banding. Obes Surg. 2008;18:573–7. doi: 10.1007/s11695-008-9470-6. [DOI] [PubMed] [Google Scholar]
- 18.O'Brien PE, Dixon JB, Brown W, et al. The laparoscopic adjustable gastric band (Lap-Band): a prospective study of medium-term effects on weight, health and quality of life. Obes Surg. 2002;12:652–60. doi: 10.1381/096089202321019639. [DOI] [PubMed] [Google Scholar]
- 19.Van Nieuwenhove Y, Ceelen W, Stockman A, et al. Long-term results of a prospective study on laparoscopic adjustable gastric banding for morbid obesity. Obes Surg. 2011;21:582–7. doi: 10.1007/s11695-010-0341-6. [DOI] [PubMed] [Google Scholar]
- 20.Kasza J, Brody F, Vaziri K, et al. Analysis of poor outcomes after laparoscopic adjustable gastric banding. Surg Endosc. 2011;1:41–7. doi: 10.1007/s00464-010-1126-7. [DOI] [PubMed] [Google Scholar]
- 21.Suter M, Calmes JM, Paroz A, et al. A 10-year experience with laparoscopic gastric banding for morbid obesity: high long-term complication and failure rates. Obes Surg. 2006;16:829–35. doi: 10.1381/096089206777822359. [DOI] [PubMed] [Google Scholar]
- 22.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 23.Genuth S, Alberti KG, Bennett P, et al. Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care. 2003;26:3160–7. doi: 10.2337/diacare.26.11.3160. [DOI] [PubMed] [Google Scholar]
- 24.Di Lorenzo N, Furbetta F, Favretti F, et al. Laparoscopic adjustable gastric banding via pars flaccida versus perigastric positioning: technique, complications, and results in 2,549 patients. Surg Endosc. 2010;24:1519–23. doi: 10.1007/s00464-009-0669-y. [DOI] [PubMed] [Google Scholar]
- 25.Abalikšta T, Brimas G, Strupas K. Laparoscopic adjustable gastric banding. A prospective randomized study comparing the Swedish Adjustable Gastric Band and the MiniMizer Extra: one-year results. Videosurgery Miniinv. 2011;6:207–16. doi: 10.5114/wiitm.2011.26254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.NHLBI Obesity Education Initiative Expert Panel on the Identification, Evaluation, and Treatment of Obesity in Adults (US) Bethesda, USA: Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults NIH Publication; 1998. [Google Scholar]
- 27.Favretti F, Ashton D, Busetto L, et al. The gastric band: first-choice procedure for obesity surgery. World J Surg. 2009;33:2039–48. doi: 10.1007/s00268-009-0091-6. [DOI] [PubMed] [Google Scholar]
- 28.Pilone V, Mozzi E, Schettino AM, et al. Improvement in health-related quality of life in first year after laparoscopic adjustable gastric banding. Surg Obes Relat Dis. 2012;8:260–8. doi: 10.1016/j.soard.2011.12.012. [DOI] [PubMed] [Google Scholar]
- 29.Sarker S, Myers J, Serot J, et al. Three-year follow-up weight loss results for patients undergoing laparoscopic adjustable gastric banding at a major university medical center: does the weight loss persist? Am J Surg. 2006;191:372–6. doi: 10.1016/j.amjsurg.2005.10.040. [DOI] [PubMed] [Google Scholar]
- 30.Parikh MS, Fielding GA, Ren CJ. U.S. experience with 749 laparoscopic adjustable gastric bands: intermediate outcomes. Surg Endosc. 2005;19:1631–5. doi: 10.1007/s00464-005-0302-7. [DOI] [PubMed] [Google Scholar]
- 31.Ahroni JH, Montgomery KF, Watkins BM. Laparoscopic adjustable gastric banding: weight loss, comorbidities, medication usage and quality of life at one year. Obes Surg. 2005;15:641–7. doi: 10.1381/0960892053923716. [DOI] [PubMed] [Google Scholar]
- 32.Mittermair RP, Aigner F, Obermüller S. Results and complications after Swedish adjustable gastric banding in older patients. Obes Surg. 2008;18:1558–62. doi: 10.1007/s11695-008-9709-2. [DOI] [PubMed] [Google Scholar]
- 33.Spivak H, Hewitt MF, Onn A, et al. Weight loss and improvement of obesity-related illness in 500 U.S. patients following laparoscopic adjustable gastric banding procedure. Am J Surg. 2005;189:27–32. doi: 10.1016/j.amjsurg.2004.06.038. [DOI] [PubMed] [Google Scholar]
- 34.Boza C, Gamboa C, Perez G, et al. Laparoscopic adjustable gastric banding (LAGB): surgical results and 5-year follow-up. Surg Endosc. 2011;25:292–7. doi: 10.1007/s00464-010-1176-x. [DOI] [PubMed] [Google Scholar]
- 35.Dixon JB, O'Brien PE. Selecting the optimal patient for LAP-BAND placement. Am J Surg. 2002;184:S17–20. doi: 10.1016/s0002-9610(02)01174-1. [DOI] [PubMed] [Google Scholar]
- 36.Wölnerhanssen BK, Peters T, Kern B, et al. Predictors of outcome in treatment of morbid obesity by laparoscopic adjustable gastric banding: results of a prospective study of 380 patients. Surg Obes Relat Dis. 2008;4:500–6. doi: 10.1016/j.soard.2008.03.252. [DOI] [PubMed] [Google Scholar]
- 37.Busetto L, Angrisani L, Basso N, et al. Safety and efficacy of laparoscopic adjustable gastric banding in the elderly. Obesity. 2008;16:334–8. doi: 10.1038/oby.2007.85. [DOI] [PubMed] [Google Scholar]
- 38.Dixon JB, Dixon ME, O'Brien PE. Pre-operative predictors of weight loss at 1-year after Lap-Band surgery. Obes Surg. 2001;11:200–7. doi: 10.1381/096089201321577884. [DOI] [PubMed] [Google Scholar]
- 39.Giusti V, Suter M, Héraïef E, et al. Effects of laparoscopic gastric banding on body composition, metabolic profile and nutritional status of obese women: 12-months follow-up. Obes Surg. 2004;14:239–45. doi: 10.1381/096089204322857636. [DOI] [PubMed] [Google Scholar]
- 40.Pontiroli AE, Pizzocri P, Librenti MC, et al. Laparoscopic adjustable gastric banding for the treatment of morbid (grade 3) obesity and its metabolic complications: a three-year study. J Clin Endocrinol Metab. 2002;87:3555–61. doi: 10.1210/jcem.87.8.8708. [DOI] [PubMed] [Google Scholar]
- 41.Gasteyger C, Suter M, Calmes JM, et al. Changes in body composition, metabolic profile and nutritional status 24 months after gastric banding. Obes Surg. 2006;16:243–50. doi: 10.1381/096089206776116381. [DOI] [PubMed] [Google Scholar]
- 42.Evangelou P, Tzotzas T, Christou G, et al. Does the presence of metabolic syndome influence weight loss in obese and overweight women? Metab Syndr Relat Disord. 2010;8:173–8. doi: 10.1089/met.2009.0066. [DOI] [PubMed] [Google Scholar]
- 43.Pinkston MM, Poston WS, Reeves RS, et al. Does metabolic syndrome mitigate weight loss in overweight Mexican American women treated for 1-year with orlistat and lifestyle modification? Eat Weight Disord. 2006;11:35–41. doi: 10.1007/BF03327751. [DOI] [PubMed] [Google Scholar]
- 44.Conroy R, Lee EJ, Jean A, et al. Effect of laparoscopic adjustable gastric banding on metabolic syndrome and its risk factors in morbidly obese adolescents. J Obes. 2011;2011:906384. doi: 10.1155/2011/906384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Singhal R, Kitchen M, Bridgwater S, Super P. Metabolic outcomes of obese diabetic patients following laparoscopic adjustable gastric banding. Obes Surg. 2008;18:1400–5. doi: 10.1007/s11695-008-9500-4. [DOI] [PubMed] [Google Scholar]