Abstract
Background
Urethral stricture is a narrowing of the urethra due to scar tissue, which leads to obstructive voiding dysfunction with potentially serious consequences for the entire urinary tract. Its prevalence among men in industrial countries is estimated at 0.9%. It produces obstructive and irritative urinary symptoms and can ultimately impair renal function. Urethral strictures can be caused by diagnostic or therapeutic urological procedures. These procedures are being performed ever more commonly, because the population is aging; thus, urethral strictures will probably become more common as well.
Methods
We selectively reviewed pertinent original articles and meta-analyses (1995–2012) on the causes, diagnostic evaluation, and treatment of urethral strictures, which were retrieved by a search in the PubMed database.
Results
Most of the relevant publications are reports of retrospective studies from single centers. Only a few prospective randomized trials and structured reviews are available. The overall level of the scientific evidence is low. 45% of urethral strictures are iatrogenic, 30% idiopathic, and 20% due to bacterial urethritis. Strictures are diagnosed with a flow test and a retrograde urethrogram. Short bulbar strictures can be treated endoscopically. For recurrent and complex strictures, only open urethral surgery can reliably and permanently remove the infravesical obstruction.
Conclusion
Urethral strictures must be recognized and treated so that their most serious long-term complication, impaired renal function, can be prevented. The clinical utility of urethrotomy is limited by a high recurrence rate.
A urethral stricture is a narrowing of the urethra caused by scarring, which functionally has the effect of obstructing the lower urinary tract. The consequences of this obstruction can enormously impair the patient’s quality of life by causing micturition disturbances; they can also damage the entire urinary tract, resulting in loss of renal function. It is therefore essential that urethral strictures, which can occur at any age and in either men or women (though they are much rarer in women), are recognized early and appropriately treated. The prevalence in industrial countries is estimated at around 0.9% (1).
Morphologically, the stricture is an alteration of the urethra by scarring (2). In men, the corpus spongiosum—in which the urethra is embedded—is also involved in the scarring. This spongiofibrosis is a reaction to various extrinsic irritants and can lead to complete replacement of the spongy tissue by scar tissue.
This disease entity can be a clinically relevant problem in patients with a urological medical history, since the development of urethral stricture may be related to endourological diagnostic procedures and treatments (3).
Etiology
Almost all strictures for which a cause can be identified are acquired (3, 4). The largest group (45%) are iatrogenic and result from urethral manipulations (traumatic indwelling catheter, transurethral interventions, correction of hypospadias, prostatectomy, brachytherapy) (3, 4). Thus, for example, the incidence of urethral stricture after transurethral prostate resection (the most common prostate intervention) is 3% to 5% (5, 6). Another cause of urethral stricture is traumatic urethral rupture associated with pelvic fracture. Bacterial urethritis can also lead to stricture (around 20% of cases); classically, these are cases of untreated gonorrhea. Another inflammatory disease associated with (distal) urethral stricture is balanitis xerotica obliterans, a chronic inflammatory disease whose exact etiology is unknown (7).
Around 30% of urethral strictures are idiopathic (3). In these cases the most likely trigger is considered to be some forgotten minor trauma that occurred a long time in the past (e.g., perineal injury while riding a bicycle) (8).
Patient age is also relevant in deciding on the cause of a stricture: In patients younger than 45 years, hypospadias correction and pelvic trauma are most commonly defined as the cause, while transurethral interventions are most common in those aged over 45 (3).
The urethra is divided into different segments that are involved in stricture with varying frequency (Figure 1). The segments passing through the prostate (prostatic urethra) and pelvic floor musculature (membranous urethra) are referred to collectively as the posterior urethra, while the anterior urethra is made up of the segment fixed to the pelvic floor (bulbar urethra) and the segment passing through the pendulous portion and glans penis (penile and glandular urethra).
Figure 1.
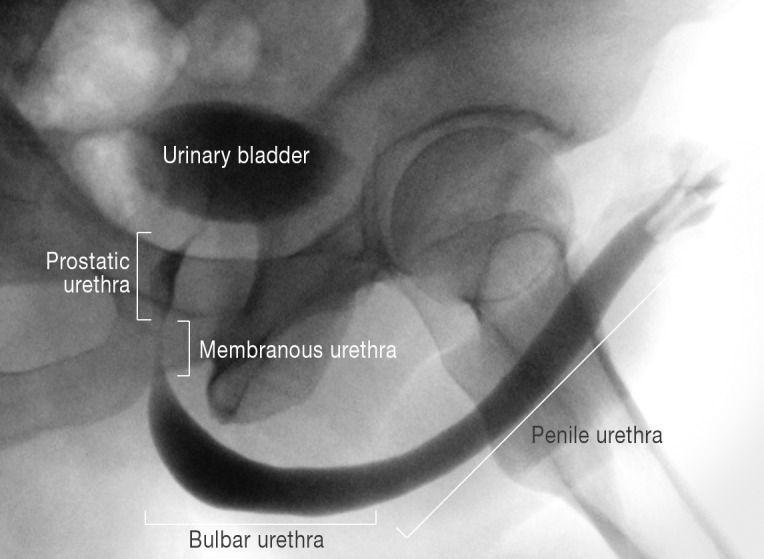
Cystourethrogram of a normal urethra, showing the anatomical segments
Bulbar strictures are most common (around 50%), followed by penile strictures (around 30%) and strictures of the navicular fossa (around 20%) (4, 9). Strictures in the posterior urethra are rare and result either from traumatic urethral rupture or from radiotherapy for prostate cancer (8, 10).
Symptoms
The main symptoms of urethral stricture are those of obstructed and irritated micturition, with increased urination time and a feeling of incomplete bladder emptying, combined with increased micturition frequency and urgency (4). Particularly in patients who have previously undergone transurethral interventions or had a long-term indwelling catheter during treatment for another disease, these symptoms should suggest the possibility of stricture (Table 1).
Table 1. Causes of urethral stricture.
| Causes | Incidence | |
| Iatrogenic | Transurethral prostate resection | 45% |
| Radical prostatectomy | ||
| Hypospadias correction | ||
| Indwelling cather | ||
| Cystoscopy | ||
| Bacterial urethritis | 20% | |
| Lichen sclerosus et atrophicus | 5% | |
| Idiopathic | 30% | |
Presenting symptoms may also be those of typical sequelae such as prostatitis or epididymitis (4). Some patients do not present until they have acute urinary retention, since early on during stricture formation, the urinary bladder can compensate for the raised infravesical resistance by detrusor hypertrophy. This leads to a rise in intravesical pressure during urination, and may be noticed on ultrasonography as a thickening of the bladder wall. Later, decompensation of the voiding function and incomplete voiding will occur, which may develop into complete urinary retention. In the end, these changes can lead to secondary urinary tract obstruction or high-pressure reflux, either of which may lead to loss of kidney function (11).
Diagnosis
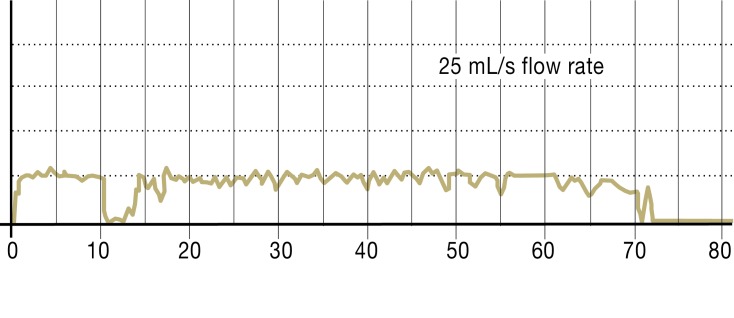
In addition to the typical history, urethral stricture can be diagnosed on the basis of its typical profile on uroflowmetry (11). This investigation records the urine stream (measured as volume per unit of time) and the overall urination time. The graph from a patient with a urethral stricture will show an extended urination time with a low-level plateau (Figure 2). The shape of this curve is pathognomonic of urethral stricture, although the investigation says nothing about the length of the stricture or where it is located. Both these need to be known before treatment can be planned, however, and for this the investigation of choice is retrograde cystourethrography (Figure 3), combined, if appropriate, with voiding cystourethrography.
Figure 2.
Typical uroflowmetry in urethral stricture, showing extended urination time and low, plateauing maximum flow
Figure 3.
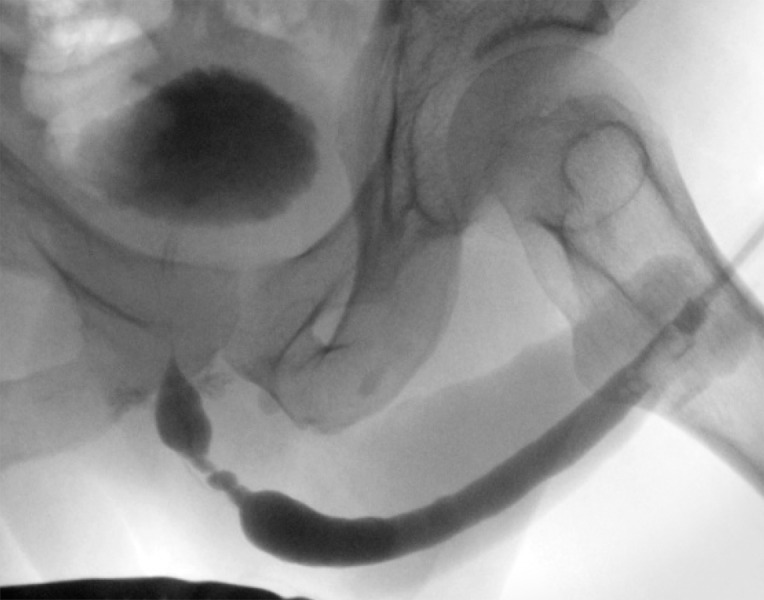
Cystourethrogram of a bulbar urethral stricture about 3 cm in length
Urethroscopy can show where the stricture is located, but if the stricture cannot be passed by the cystoscope, no information can be obtained about the length of the lesion or about any additional, more proximal strictures that may be present. For this reason, urethroscopy does not have a major role in the diagnostic work-up of urethral stricture (11).
Other primary diagnostic procedures required are ultrasonography to determine any urinary retention and ultrasound examination of the upper urinary tract to rule out hydronephrosis. Urine sediment is examined to rule out acute infection.
Treatment
When the patient first presents, the primary question is whether urinary retention or upper tract obstruction is present, which would necessitate urinary diversion and treatment of any accompanying urinary tract infection.
In patients with urinary retention or large amounts of residual urine, blind transurethral bougienage of the urethra with an indwelling catheter must absolutely be avoided, as the tissue trauma would make the condition of the urethra worse. These patients should be given a suprapubic bladder fistula. Any existing urinary tract infection must be treated according to test results.
Once the acute situation has been dealt with, definitive treatment of the stricture must be carried out. The basic choice is between endoscopic (minimally invasive) and open surgical procedures (Table 2).
Table 2. Treatment options for urethral stricture.
| Endoscopic | Open surgical |
|
|
Whichever treatment is chosen, it must be borne in mind that strictures tend to recur. The more extensive the stricture, the further distal its location, and the more often it has already been treated, the poorer are the long-term results (12, 13).
A general point to emphasize is that the scientific literature on the treatment of urethral stricture is sparse. Most of it consists of single-center retrospective analyses of usually small and often heterogeneous patient groups. Because so many different open surgical procedures are available, there are no clear data as to which procedure is best in which situation.
Endourological procedures
Bougienage of the urethral stricture is the oldest form of treatment and was used even in the pre-Christian era. In this procedure, the spongiofibrosis is stretched, thus producing innumerable microlesions in the scar tissue, leading to further scarring. For this reason, bougienage can only ever have a temporary effect on the obstruction, and as a rule the stricture may be expected to recur after 4 to 6 weeks (13). This procedure should therefore be employed only in patients who refuse surgical treatment or who are unsuited for surgery for other (e.g., anesthesiological) reasons.
In internal urethrotomy, the stricture scar is incised with a knife endoscopically, resulting in widening of the lumen. Since the resulting wound margins expand, healing is by secondary intention. This in turn leads to scar formation, explaining the high recurrence rate. Recurrence must be expected in at least 50% to 60% of cases (14, 15); some authors report long-term success rates of only 20% (13). The recurrence rate depends on the length of the stricture; better results may be expected only for short (<1.5 cm), first-time strictures of the bulbar urethra (up to 75% success [14]). A prospective randomized study showed that internal urethrotomy produces no better results than bougienage (13).
In this procedure, however, healthy tissue proximal and distal to the stricture is necessarily incised, thus making the lesion longer. The result is that a recurrent stricture is always longer than the original one. Moreover, once recurrence has occurred, with increased stricture length, permanent healing can no longer be hoped for from this procedure. It is in fact known that the number of urethrotomies performed is a negative predictive factor for failure of a subsequent urethroplasty (12).
The upshot is that urethrotomy is of only limited value. It should only be used to treat short (<1.5 cm), first-time bulbar strictures. There have been many attempts to minimize the recurrence rate by using lasers instead of cold steel, but none of these has been shown to be superior (16).
Hence, for complex or recurrent strictures, an open reconstructive procedure should be used.
Open reconstructive procedures
Good results have been achieved in short (<2.5 cm) strictures of the bulbar urethra by means of stricture resection and end-to-end anastomosis. For this, the urethra is dissected free via a perineal approach, the stricture is completely excised, and after sufficient mobilization and further spatulation of the ends, a tension-free end-to-end anastomosis of the urethra is carried out. In correctly selected patients, this procedure achieves long-term success rates of around 90% (17, 18). In young patients, a problem can be the loss of urethral length, which can lead to ventral penile curvature during erection, i.e., a downward bend of the entire penis. Particularly with strictures of the penile urethra, adequate mobilization of the urethra for a tension-free end-to-end anastomosis without ventral curvature of the penis is not possible, so alternative procedures must be employed. It must also be remembered that in this procedure the blood supply running the length of the corpus spongiosum is completely interrupted. In rare cases this can lead to a significant perfusion problem, which manifests as a lack of glans tumescence during erection (17). These complications must be avoided, especially in young patients. The procedure is also contraindicated in patients who have previously undergone correction of hypospadias, because with their altered anatomy, lacking vascular anastomoses to the corpus cavernosum, perfusion of the penile urethra after complete transection of the bulbar urethra cannot be ensured.
As a treatment for long bulbar strictures and all penile strictures, graft urethroplasty has recently come into use (19). In this procedure, the urethra is completely mobilized in the stricture region and dissected free from the corpora cavernosa. The urethra is then opened lengthways along the entire length of the stricture and a free graft sutured into the defect thus created, to widen the stricture (Figures 4, 5a+b).
Figure 4.
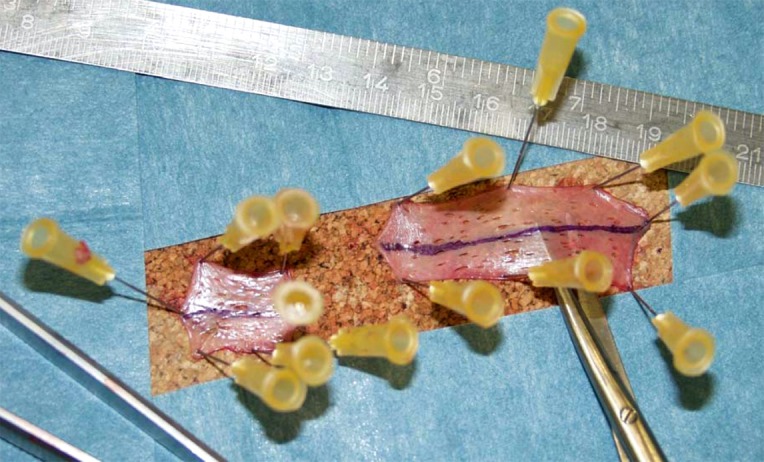
Prepared foreskin graft
Figure 5a+b.
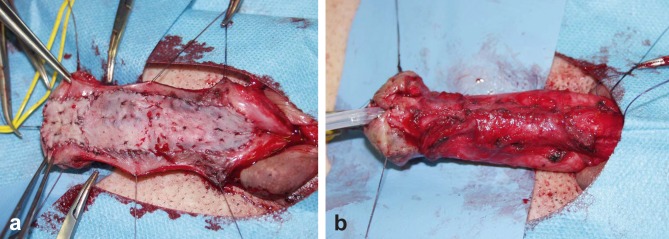
Foreskin graft after suturing into the ventrally opened urethra and after re-closure (tubularization) of the urethra
Suitable skin grafts may be taken from the foreskin or oral mucosa, or they may, exceptionally, be taken with the dermatome from the upper thigh or lower abdomen (18– 22). Numerous other materials have also been utilized (including bladder mucosa and colonic mucosa), but for various reasons have not come into widespread use. The question of which material makes the best graft has not been sufficiently investigated. This is because the scientific literature on this subject consists almost exclusively of single-center retrospective case series, which have studied different materials in heterogeneous patients groups. Few prospective investigations have been performed, and prospective randomized studies are rare.
Most studies in the past 10 years investigated oral mucosa as graft material. The largest retrospective study of bulbar strictures to date found it to be superior to foreskin grafts, with success rates after 53 months of about 60% for foreskin grafts versus about 80% for oral mucosa (18). However, comparable success rates cannot be achieved with oral mucosa for penile or distal strictures, and in this location, skin from the shaft of the penis is as good as oral mucosa (about 70% after 52 months (23, 24]). For reconstruction of distal urethras after failed hypospadias correction, penile skin has proved to be as good as oral mucosa (25). In addition to functional results, the focus in recent years has also been on possible complications at the graft donor site. No relevant complications have been described for the foreskin as donor site, but significant intraoral morbidity has been observed after the removal of oral mucosa (pain, numbness, scar contractures) (26, 27). Because of this, and because they are easier to access, the foreskin and upper thigh have the edge as graft donor sites, and an intraoral procedure can be avoided.
In operative techniques using pedicled skin flaps, the urethra is similarly opened up along the entire length of the stricture, and the resulting defect filled with an island pedicled flap of penis shaft skin prepared on the underlying fascia (dartos fascia) and swivelled onto the open urethra. Various techniques exist, but these flaps always receive their blood supply from the subdermal connective tissue. These flap techniques represent extensive procedures, and although prospective randomized studies have shown comparable success rates to those of the grafting techniques, they require a long operative time and are associated with increased complication rates (skin necrosis in about 15%, fistula formation in about 5%) (Box 1) (28, 29), and are therefore reserved for exceptional cases such as complex recurrence in the penile urethra or patients who have undergone radiotherapy.
Box. Possible complications of open reconstruction*.
Penile curvature, 5% to 20%
Impaired ejaculation, 25%
Impaired glans sensitivity, 15% (end-to-end anastomosis)
Fistula formation, 5% (flap urethroplasty)
Skin necrosis, 15% (flap urethroplasty)
A palliative procedure for patients with complex recurrent strictures who do not wish to undergo further extensive reconstructive surgery, or would not tolerate it because of co-morbidities, is perineal urethrostomy (Boutonnière), a simple and effective procedure in which the bulbar urethra is sutured directly into the perineal skin beneath the scrotum. This makes the distal urethra functionally superfluous, and preserves continence with urination in the seated position. Although some studies showed a repeat intervention to be necessary in around 30% of cases, subjective satisfaction with this procedure is over 90% (30).
For strictures running the entire length of the urethra, a two-part procedure can be worthwhile. In this, the entire urethra is first opened ventrally and the edges sutured to the surrounding skin. The resulting “urethral plate” is then, in a second session about 6 months later, re-excised and formed into a tube (“tubularized”) (31).
Urethral closure after urethral rupture is a special case. Urethral rupture occurs only in association with pelvic fractures in patients with multiple trauma. The urethra is torn off either directly above or directly below the urogenital diaphragm (supradiaphragmatic vs. infradiaphragmatic urethral rupture) (32). This leads to scarring of the defect, with complete obstruction of the urethral lumen (Figure 6). Treatment in these cases consists of complete excision of the scar tissue and anastomosis between the bulbar urethra and the prostate apex (33, 34). Something to watch out for is that in patients with supradiaphragmatic rupture (around 30%), the continence mechanism may be damaged, as it may be excised with the dense scar tissue.
Figure 6.
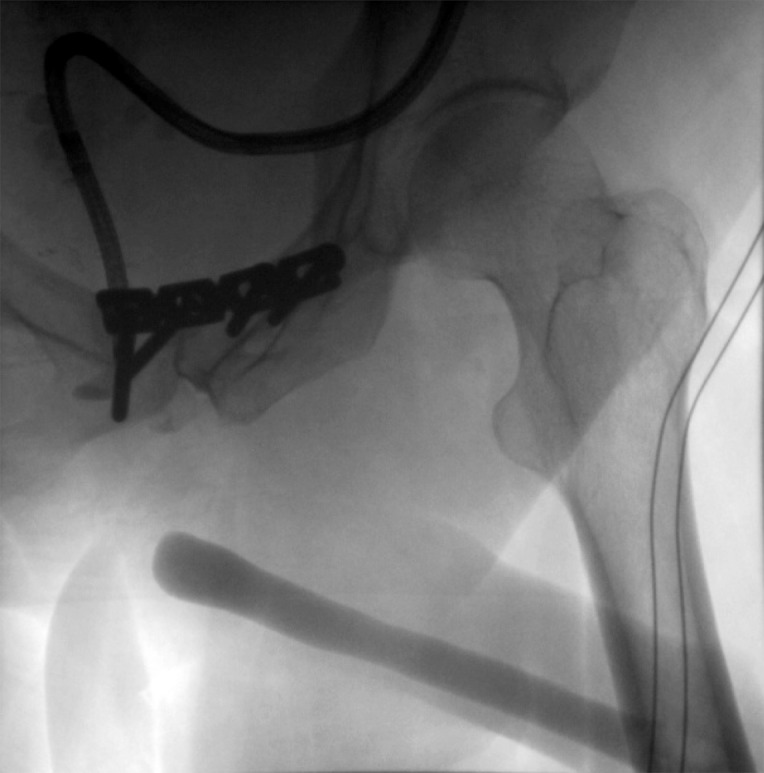
Cystourethrogram of a complete urethral obstruction in a patient with previous urethral rupture. A flexible cystoscope has been inserted into the prostatic urethra via a suprapubic access, marking the proximal end of the obstruction
The basic principle in treatment of urethral stricture is that internal urethrotomy promises success only in short, first-time strictures. In a recurrent stricture, treatment should be changed to open reconstruction, in order to avoid lengthening the defect by repeated urethrotomies.
It is important that open reconstructive surgery should be carried out at centers with adequate experience, as this is the only way to achieve the best results.
Key Messages.
Urethral stricture is a disease condition that can lead to obstructive micturition problems at any age, and over time can irreversibly damage the entire urinary tract.
Strictures are most often caused by transurethral interventions and traumatic bladder catheterization.
Strictures can be reliably diagnosed on the basis of uroflowmetry and cystourethrography.
Endoscopic treatment is minimally invasive but has a high recurrence rate.
Permanent elimination of a stricture often requires open reconstructive surgery.
Acknowledgments
Translated from the original German by Kersti Wagstaff, MA.
Footnotes
Conflict of interest statement
Dr. Tritschler, Dr. Füllhase, Prof. Stief, Dr. Roosen and Prof. Rübben declare that no conflict of interest exists.
References
- 1.Anger JT, Buckley JC, Santucci RA, Elliott SP, Saigal CS. Trends in stricture management among male Medicare beneficiaries: underuse of urethroplasty? Urology. 2011;77:481–485. doi: 10.1016/j.urology.2010.05.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sievert KD, Selent-Stier C, Wiedemann J, et al. Introducing a large animal model to create urethral stricture similar to human stricture disease: a comparative experimental microscopic study. J Urol. 2012;187:1101–1109. doi: 10.1016/j.juro.2011.10.132. [DOI] [PubMed] [Google Scholar]
- 3.Lumen N, Hoebeke P, Willemsen P, De Troyer B, Pieters R, Oosterlinck W. Etiology of urethral stricture disease in the 21st century. J Urol. 2009;182:983–987. doi: 10.1016/j.juro.2009.05.023. [DOI] [PubMed] [Google Scholar]
- 4.Fenton AS, Morey AF, Aviles R, Garcia CR. Anterior urethral strictures: etiology and characteristics. Urology. 2005;65:1055–1058. doi: 10.1016/j.urology.2004.12.018. [DOI] [PubMed] [Google Scholar]
- 5.Santucci RA, McAninch JW. Urethral reconstruction of strictures resulting from treatment of benign prostatic hypertrophy and prostate cancer. Urol Clin North Am. 2002;29:417–427. doi: 10.1016/s0094-0143(02)00031-9. viii. [DOI] [PubMed] [Google Scholar]
- 6.Tasci AI, Ilbey YO, Tugcu V, Cicekler O, Cevik C, Zoroglu F. Transurethral resection of the prostate with monopolar resectoscope: single-surgeon experience and long-term results of after 3589 procedures. Urology. 2011;78:1151–1155. doi: 10.1016/j.urology.2011.04.072. [DOI] [PubMed] [Google Scholar]
- 7.Das S, Tunuguntla HS. Balanitis xerotica obliterans—a review. World J Urol. 2000;18:382–387. doi: 10.1007/PL00007083. [DOI] [PubMed] [Google Scholar]
- 8.Park S, McAninch JW. Straddle injuries to the bulbar urethra: management and outcomes in 78 patients. J Urol. 2004;171:722–725. doi: 10.1097/01.ju.0000108894.09050.c0. [DOI] [PubMed] [Google Scholar]
- 9.Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA. 10th edition. Philadelphia: Elsevier; 2012. Campbell-Walsh Urology. [Google Scholar]
- 10.Jordan GH, Virasoro R, Eltahawy EA. Reconstruction and management of posterior urethral and straddle injuries of the urethra. Urol Clin North Am. 2006;33:97–109. doi: 10.1016/j.ucl.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 11.Brandes SB. Totowa: Humana Press; 2008. Urethral Reconstructive Surgery. [Google Scholar]
- 12.Breyer BN, McAninch JW, Whitson JM, et al. Multivariate analysis of risk factors for long-term urethroplasty outcome. J Urol. 2010;183:613–617. doi: 10.1016/j.juro.2009.10.018. [DOI] [PubMed] [Google Scholar]
- 13.Steenkamp JW, Heyns CF, de Kock ML. Internal urethrotomy versus dilation as treatment for male urethral strictures: a prospective, randomized comparison. J Urol. 1997;157:98–101. [PubMed] [Google Scholar]
- 14.Pansadoro V, Emiliozzi P. Internal urethrotomy in the management of anterior urethral strictures: long-term followup. J Urol. 1996;156:73–75. [PubMed] [Google Scholar]
- 15.Verges J, Desgrez JP, Claude JM, Cabane H. Internal urethrotomy. Resection of urethral stricture (over 5 years follow-up) Ann Urol. 1990;24:73–75. [PubMed] [Google Scholar]
- 16.Kamp S, Knoll T, Osman MM, Kohrmann KU, Michel MS, Alken P. Low-power holmium: YAG laser urethrotomy for treatment of urethral strictures: functional outcome and quality of life. J Endourol. 2006;20:38–41. doi: 10.1089/end.2006.20.38. [DOI] [PubMed] [Google Scholar]
- 17.Barbagli G, De Angelis M, Romano G, Lazzeri M. Long-term follow up of bulbar end-to-end anastomosis: a 18. retrospective analysis of 153 patients in a single center experience. J Urol. 2007;178:2470–2473. doi: 10.1016/j.juro.2007.08.018. [DOI] [PubMed] [Google Scholar]
- 18.Barbagli G, Guazzoni G, Lazzeri M. One-stage bulbar urethroplasty: retrospective analysis of the results in 375 patients. Eur Urol. 2008;53:828–833. doi: 10.1016/j.eururo.2008.01.041. [DOI] [PubMed] [Google Scholar]
- 19.Andrich DE, Mundy AR. What is the best technique for urethroplasty? Eur Urol. 2008;54:1031–1041. doi: 10.1016/j.eururo.2008.07.052. [DOI] [PubMed] [Google Scholar]
- 20.Meeks JJ, Erickson BA, Fetchev P, Crawford SE, Fine NA, Gonzalez CM. Urethroplasty with abdominal skin grafts for long segment urethral strictures. J Urol. 2010;183:1880–1884. doi: 10.1016/j.juro.2010.01.029. [DOI] [PubMed] [Google Scholar]
- 21.Schwentner C, Seibold J, Colleselli D, et al. Single-stage dorsal inlay full-thickness genital skin grafts for hypospadias reoperations: extended follow up. J Pediatr Urol. 2011;7:65–71. doi: 10.1016/j.jpurol.2010.01.016. [DOI] [PubMed] [Google Scholar]
- 22.Dalpiaz O, Kerschbaumer A, Pelzer A, et al. Single-stage dorsal inlay split-skin graft for salvage anterior urethral reconstruction. BJU Int. 2008;101:1565–1570. doi: 10.1111/j.1464-410X.2007.07436.x. [DOI] [PubMed] [Google Scholar]
- 23.Levine LA, Strom KH, Lux MM. Buccal mucosa graft urethroplasty for anterior urethral stricture repair: evaluation of the impact of stricture location and lichen sclerosus on surgical outcome. J Urol. 2007;178:2011–2015. doi: 10.1016/j.juro.2007.07.034. [DOI] [PubMed] [Google Scholar]
- 24.Barbagli G, Morgia G, Lazzeri M. Retrospective outcome analysis of one-stage penile urethroplasty using a flap or graft in a homogeneous series of patients. BJU Int. 2008;102:853–860. doi: 10.1111/j.1464-410X.2008.07741.x. [DOI] [PubMed] [Google Scholar]
- 25.Barbagli G, De Angelis M, Palminteri E, Lazzeri M. Failed hypospadias repair presenting in adults. Eur Urol. 2006;49:887–894. doi: 10.1016/j.eururo.2006.01.027. discussion 95. [DOI] [PubMed] [Google Scholar]
- 26.Dublin N, Stewart LH. Oral complications after buccal mucosal graft harvest for urethroplasty. BJU Int. 2004;94:867–869. doi: 10.1111/j.1464-410X.2004.05048.x. [DOI] [PubMed] [Google Scholar]
- 27.Song LJ, Xu YM, Lazzeri M, Barbagli G. Lingual mucosal grafts for anterior urethroplasty: a review. BJU Int. 2009;104:1052–1056. doi: 10.1111/j.1464-410X.2009.08738.x. [DOI] [PubMed] [Google Scholar]
- 28.Hussein MM, Moursy E, Gamal W, Zaki M, Rashed A, Abozaid A. The use of penile skin graft versus penile skin flap in the repair of long bulbo-penile urethral stricture: a prospective randomized study. Urology. 2011;77:1232–1237. doi: 10.1016/j.urology.2010.08.064. [DOI] [PubMed] [Google Scholar]
- 29.Dubey D, Vijjan V, Kapoor R, et al. Dorsal onlay buccal mucosa versus penile skin flap urethroplasty for anterior urethral strictures: results from a randomized prospective trial. J Urol. 2007;178:2466–2469. doi: 10.1016/j.juro.2007.08.010. [DOI] [PubMed] [Google Scholar]
- 30.Barbagli G, De Angelis M, Romano G, Lazzeri M. Clinical outcome and quality of life assessment in patients treated with perineal urethrostomy for anterior urethral stricture disease. J Urol. 2009;182:548–557. doi: 10.1016/j.juro.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 31.Johanson B. Reconstruction of the male urethra in strictures. Application of the buried intact epithelium tube. Acta Chir Scand. 1953;(176 Suppl) [Google Scholar]
- 32.Koraitim M, Sabry AA. Mechanism of continence after transpubic urethroplasty. Urology. 1986;27:187–190. doi: 10.1016/0090-4295(86)90385-7. [DOI] [PubMed] [Google Scholar]
- 33.Mundy AR. Reconstruction of the urethra after pelvic trauma. Acta Urol Belg. 1998;66 [PubMed] [Google Scholar]
- 34.Mundy AR. Pelvic fracture injuries of the posterior urethra. World J Urol. 1999;17:90–95. doi: 10.1007/s003450050112. [DOI] [PubMed] [Google Scholar]