To the editor,
Hepatic capillariasis is a serious parasitic zoonosis caused by the tissue-dwelling nematode Capillaria hepatica (C. hepatica). Humans are an accidental host; human infection is acquired by ingesting food or water contaminated with infective eggs. Hepatic capillariasis may cause clinical signs and symptoms of varying intensity from mild to severe, with a possible fatal outcome. The typical manifestations are persistent fever, hepatomegaly, and eosinophilia[1].
Although human hepatic capillariasis is cosmopolitan, it is frequently scattered in tropical and temperate zones, predominantly in Brazil, America, Mexico, India, Japan, Korea, Germany, Italy, and Czechoslovakia[2]–[4]. Up to 2012, about 40 cases of human infections had been reported in the world. In China, only three human cases were documented, respectively in Guangdong, Fujian and Sichuan provinces of southern China during 1979-2004[5],[6]. However, two cases diagnosed by liver biopsy and two clinical diagnosed cases emerged in Henan province of central China since 2004[7],[8].
In order to assess the risk of human infection with C. hepatica in this province and to strengthen public safety awareness, we conducted an investigation of C. hepatica infection on the rats in seven counties of Henan province during 2008-2011. The results showed C. hepatica eggs were found in 13.62% (157/1153) of the rats. Histologically, lots of eggs in worms were seen in the pressed preparation of liver tissues. The eggs are elliptical in shape, bioperculated, ranging from 51 to 67 mm in length and 30 to 35 mm in width; these eggs have thick shell with striation of the outer layer (Figure 1). But, the prevalence varied from 20.09% (142/707) in house rats to 3.36% (15/446) in field rats (P<0.05). By rat species, C. hepatica were found in 25.83% (109/422) of Rattus norvegicus, significantly (P<0.05) more numerous in this species than in following other species: 12.9% (20/155) in R. flavipectus, 10% (13/130) in Mus musculus, 6.12% (3/49) in R. nivivente, 4.27% (5/117) in Apodemus agrarius, and 2.5% (7/280) in Cricetulus triton. The results show that house rats are the main reservoirs of C. hepatica in Henan province.
Figure 1. Morphology of C. hepatica eggs in the liver of the infected rats (unstained).
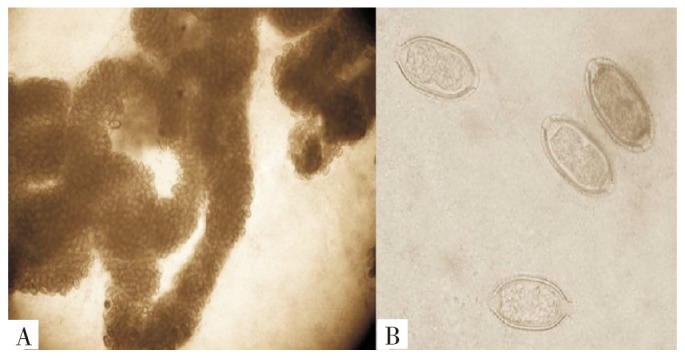
A, low-power view of the eggs in worms in pressed preparation liver tissues (100×). B, high-power view of the eggs. Note the characteristic barrel-shaped bioperculated eggs showing a thick shell with striation of the outer layer ( 400×).
In other areas of China, the prevalence of C. hepatica infection in rat hosts was higher, such as Fujian (11.35%), Zhejiang (18.3%), Yunnan (21.02%), Hubei (19.01%) and Shangdong (27.36%)[9],[10]. C. hepatica infection was also found in other mammals, such as Ochotona curzoniae in Gansu, Tibetan macaques (Macaca thibetana) in Huangshan mountain of Anhui, and the domesticated squirrels in Jingshu province[11],[12]. In addition, the prevalence of C. hepatica infection in commensal rats and shrews caught in traditional wet markets in Taichung city of Taiwan province was 94.1%[13]. However, only a few of cases were reported, it is estimated that many human cases may be neglected, undiagnosed or misdiagnosis, since the patients with fever, hepatomegaly and eosinophilia are not rare. The diagnosis of hepatica capillariasis is quite difficult because the worms and eggs in the hepatic parenchyma can not pass through the digestive tract of the patients. The definite diagnosis is established only by the histological findings in the liver biopsy of C. hepatica eggs. Therefore, the specific serological methods for diagnosis of hepatica capillariasis need to be developed.
In addition, because persons in southern China, especially in Guangdong, Hainan and Sichuan, enjoy eating the liver of field rats, 17 cases of human spurious infection with C. hepatica were reported in southern China[14]. Spurious infection occurs when humans ingest the non-embryonated eggs in the liver, these immature eggs do not cause liver disease and merely pass through the digestive tract of hosts with feces.
The results of our survey show that 13.62% of the rats infected with C. hepatica in Henan. After the infected rats and other mammals die and the liver decompose, these eggs are disseminated to the soil, where they undergo embryonation, and become the infective mature eggs in 2-6 weeks[15]–[17]. Hence, the ingestion of food or water contaminated with mature eggs poses a high risk for C. hepatica infection. Therefore, public health officials, epidemiologists, parasitologists, veterinarians, and the general public should be aware of such risks and should implement strategies to reduce or eliminate them.
Acknowledgments
This study was financially supported by Henan Major Public Research Project (No. 2008-145) and Henan Medical Science and Technology (No. 201003006).
Footnotes
Foundation Project: This study was financially supported by Henan Major Public Research Project (No. 2008-145) and Henan Medical Science and Technology (No. 201003006).
Conflict of interest statement: We declare that we have no conflict of interest.
References
- 1.Roberts LS, Janovy J, Jr, Gerald D. Foundations of parasitology. 8th ed. New York: McGraw-Hill; 2009. pp. 399–412. [Google Scholar]
- 2.Sawamura R, Fernandes MI, Peres LC, Galvão LC, Goldani HA, Jorge SM, et al. Hepatic capillariasis in children: report of 3 cases in Brazil. Am J Trop Med Hyg. 1999;61:642–647. doi: 10.4269/ajtmh.1999.61.642. [DOI] [PubMed] [Google Scholar]
- 3.González Barranco D, Peláez D, Jaramillo Rodríguez Y, Rodríguez-Martínez HA. Third case of human hepatic capillariasis in Mexico. Rev Invest Clin. 1996;48:301–315. [PubMed] [Google Scholar]
- 4.Choe G, Lee HS, Seo JK, Chail JY, Lee SH, Eom KS, et al. Hepatic capillariasis: first case report in the Republic of Korea. Am J Trop Med Hyg. 1993;48:610–625. doi: 10.4269/ajtmh.1993.48.610. [DOI] [PubMed] [Google Scholar]
- 5.Xu BK, Li DN. General condition on the rare human parasites in China. National Med J Chin. 1979;59:286–290. [Google Scholar]
- 6.Huang JN, Lin JX. The pathological diagnosis of the first case with hepatica capillariasis in Fujian province. Chin J Zoonoses. 2004;20:556. [Google Scholar]
- 7.Lin XM, Li H, Zhao XD, Deng Y. Report of one case with hepatica capillariasis. Chin J Parasit Dis Control. 2004;17:230. [Google Scholar]
- 8.Wang ZQ, Cui J, Wang Y. Persistent febrile hepatomegaly with eosinophilia due to hepatic capillariasis in China. Ann Trop Med Parasitol. 2011;105:469–472. doi: 10.1179/1364859411Y.0000000035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shen LJ, Luo ZY, Li W, Li ZH, Gao C, Yang WB, et al. Investigation on rats infected with Capillaria hepatica in Dali prefecture of Yunnan. Chin J Parasitic Dis Control. 2003;16:296–298. [Google Scholar]
- 10.Xue YS, Wu CH, Huang MS, Li RH. Investigation on rats infected with Capillaria hepatica in Fuqing county of Fujian. Strait J Preve Med. 1998;4:31–32. [Google Scholar]
- 11.Chen G, Bao GS, Han J, Jin GT. Infection of Capillaria hepaica in Ochotona curzoniae in Maqu county, Gansu province, China. Chin J Pathog Biol. 2011;6:215–216. [Google Scholar]
- 12.Zhang XJ, Ju JX, Chen J, Wang YH, Yang YF, Zhao LC, et al. Report of Capillaria hepatica infection in domesticated squirrel in Jingshu. Chin J Vet Med. 2011;47:81. [Google Scholar]
- 13.Tung KC, Hsiao FC, Wang KS, Yang CH, Lai CH. Study of the endoparasitic fauna of commensal rats and shrews caught in traditional wet markets in Taichung City, Taiwan. J Microbiol Immunol Infect. 2012 doi: 10.1016/j.jmii.2012.01.012. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 14.Xu LQ, Yang YQ, Xing YZ, Zhang CW, Jiang ZX, Yu SH, et al. Report on 7 Cases of humun spurious infection by C. Hepatica and observations on the infection from rat. Chin J Zoonoses. 1988;4:25–26. [Google Scholar]
- 15.Mowat V, Turton J, Stewart J, Lui KC, Pilling AM. Histopathological features of Capillaria hepatica infection in laboratory rabbits. Toxicol Pathol. 2009;37:661–666. doi: 10.1177/0192623309339501. [DOI] [PubMed] [Google Scholar]
- 16.Camargo LM, de Souza Almeida Aranha Camargo J, Vera L J, di Tarique Crispim Barreto P, Tourinho EK, de Souza MM. Capillariaisis (Trichurida, Trichinellidae, Capillaria hepatica) in the Brazilian Amazon: low pathogenicity, low infectivity and a novel mode of transmission. Parasit Vectors. 2010;26:3–11. doi: 10.1186/1756-3305-3-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zordan M, Tirado M, López C. Hepatic capillariasis in captive ring-tailed lemurs (Lemur catta) J Zoo Wildl Med. 2012;43:430–433. doi: 10.1638/2011-0250.1. [DOI] [PubMed] [Google Scholar]


