Table 1.
PC1 Gathers Information by Interviewing the Patient or Surrogate and Performing a Physical Examination
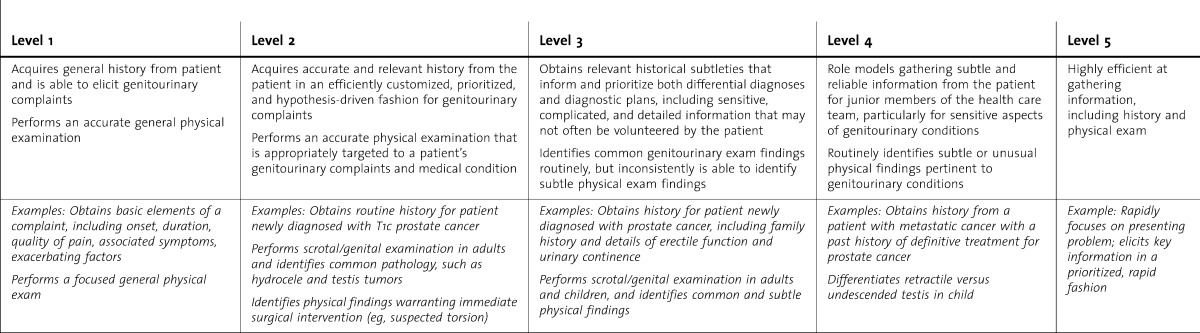
Table 2.
PC2 Uses Diagnostic Tests and Procedures, Including Performance and Interpretation of Imaging Studies
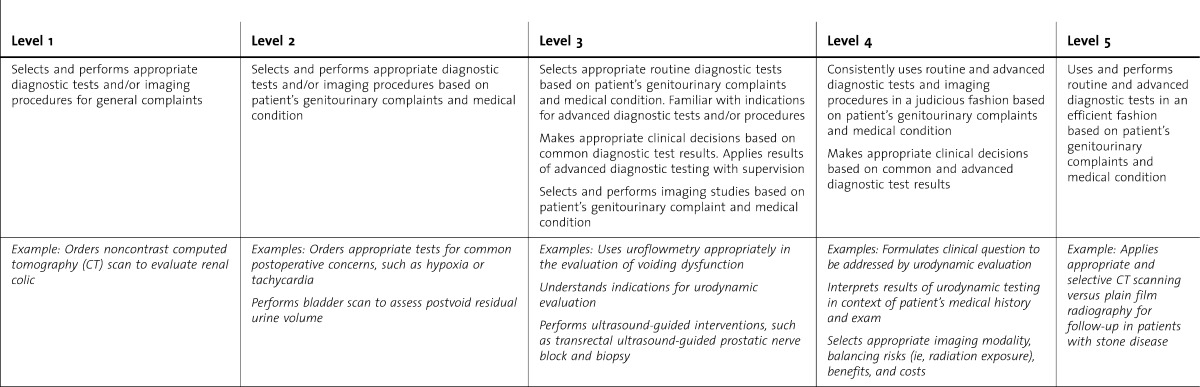
Table 3.
PC3 Generates a Differential Diagnosis
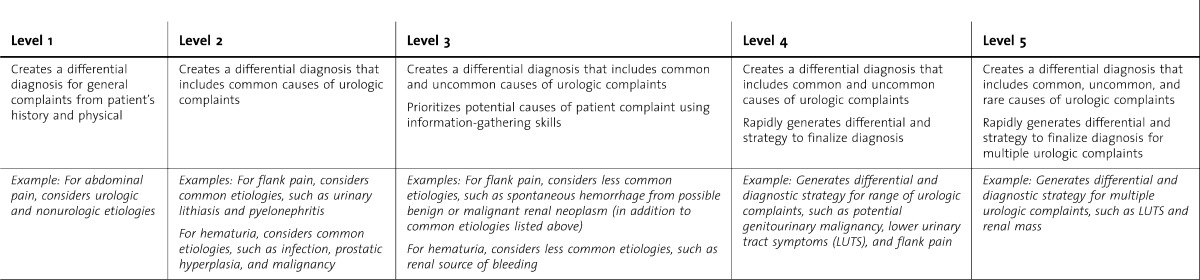
Table 4.
PC4 Develops a Patient Care Plan, Including Medical, Surgical, and/or Radiologic Interventions. Counsels Preoperative Patients Regarding Treatment Options. Discusses Risks, Benefits, and Alternatives (Informed Consent Process). Counsels Patients Regarding Potential Short- and Long-Term Impact of Interventions on Quantity and Quality of Life, as Applicable. Adapts Initial Plan as Subacute or Chronic Condition Evolves
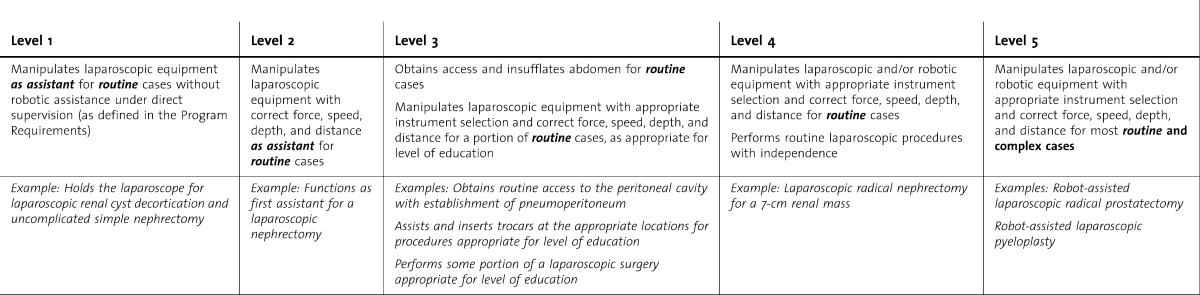
Table 5.
PC5 Performs Intraoperative and Postoperative Management of Patients, Including Recognition and Treatment of Physiologic Alterations and Complications
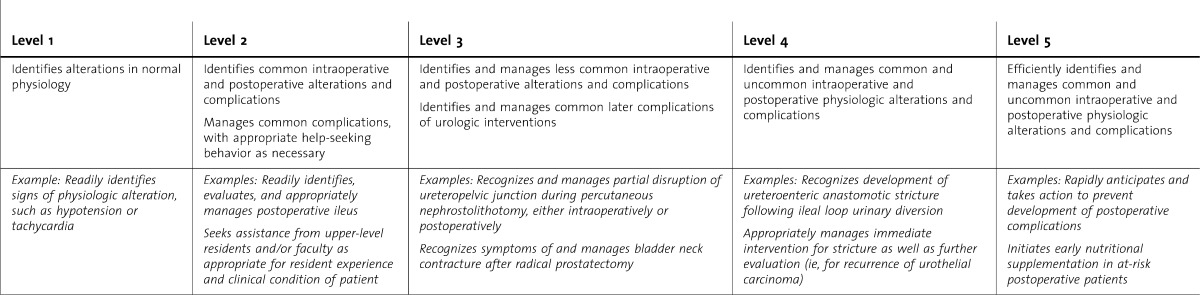
Table 6.
PC6 Performs Open Surgical Procedures
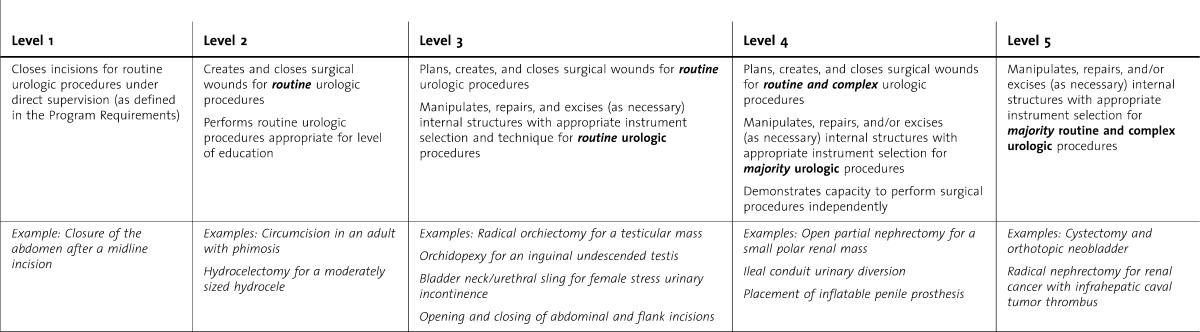
Table 7.
PC7 Performs Endoscopic Procedures of the Upper and Lower Urinary Tract
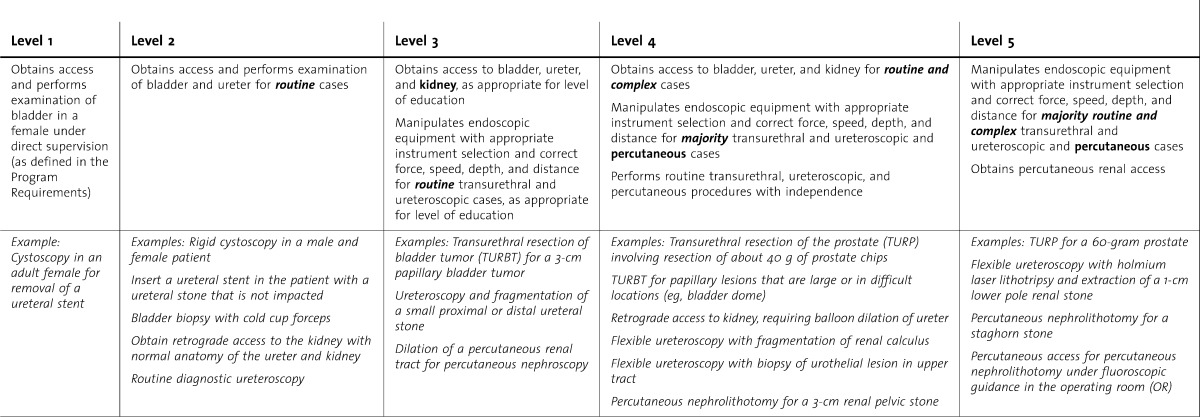
Table 8.
PC8 Performs Laparoscopic/Robot-Assisted Surgical Procedures
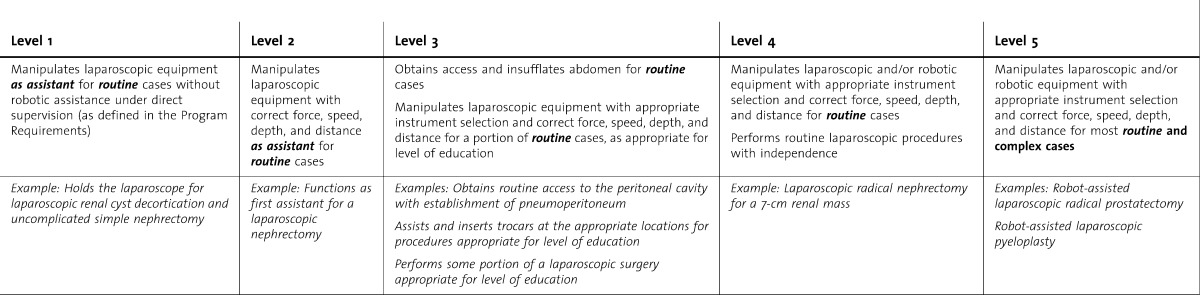
Table 9.
PC9 Performs Office-Based Procedures
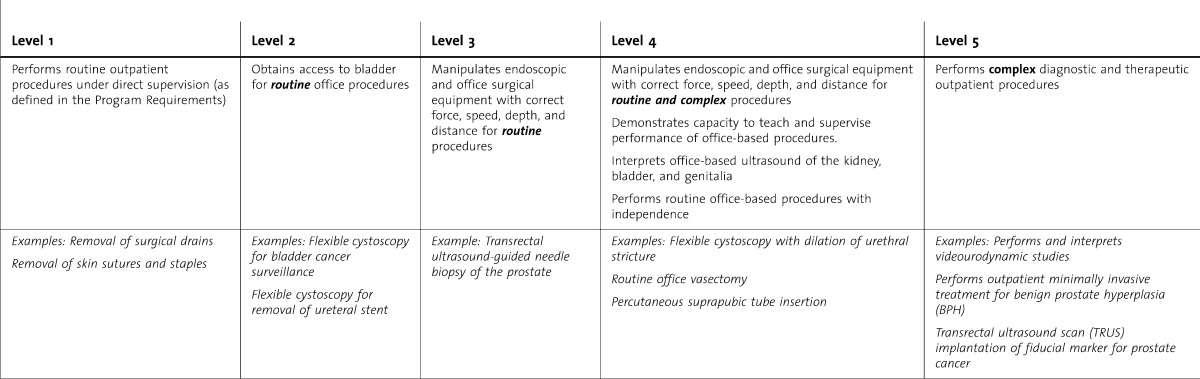
Table 10.
SBP1 Works Effectively Within and Across Health Delivery Systems
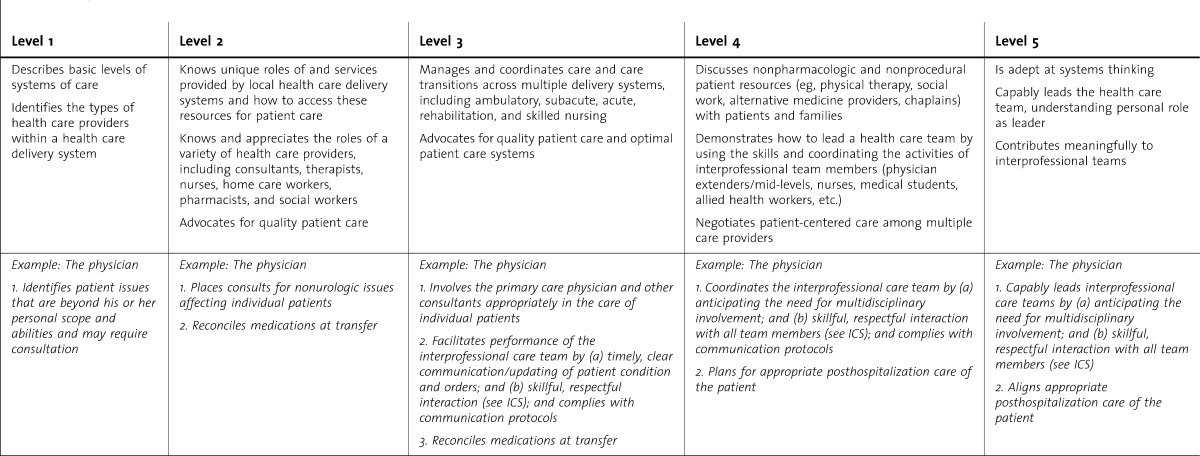
Table 11.
SBP2 Incorporates Cost Awareness and Risk-Benefit Analysis into Patient Care
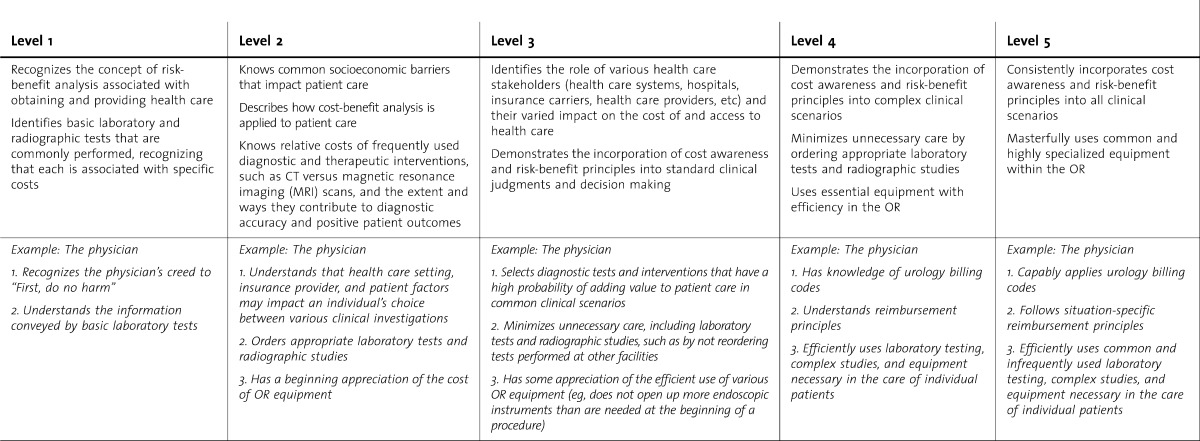
Table 12.
SBP3 Works in Interprofessional Teams to Enhance Patient Safety
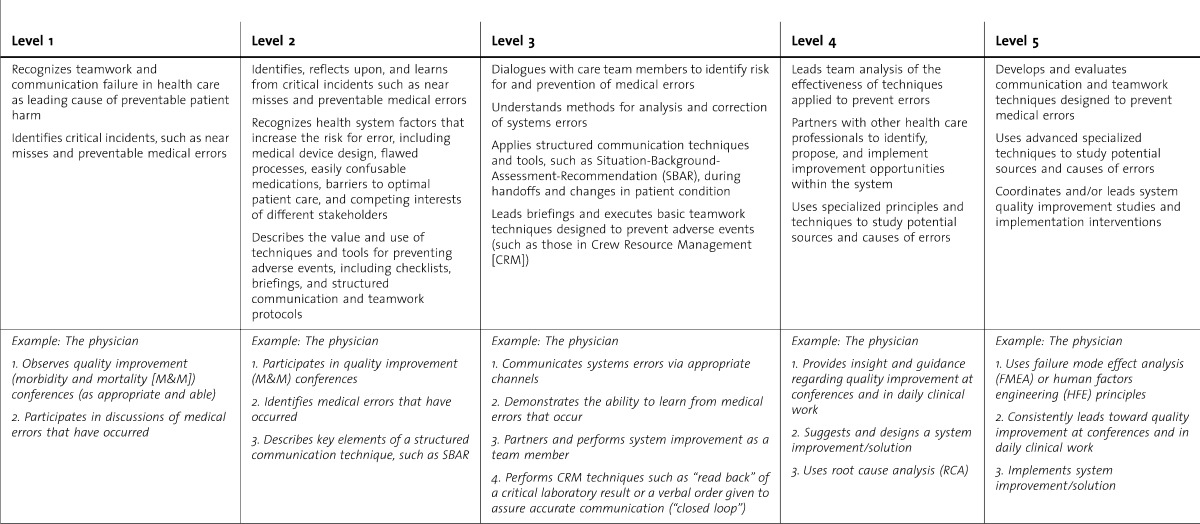
Table 13.
SBP4 Uses Technology to Accomplish Safe Health Care Delivery
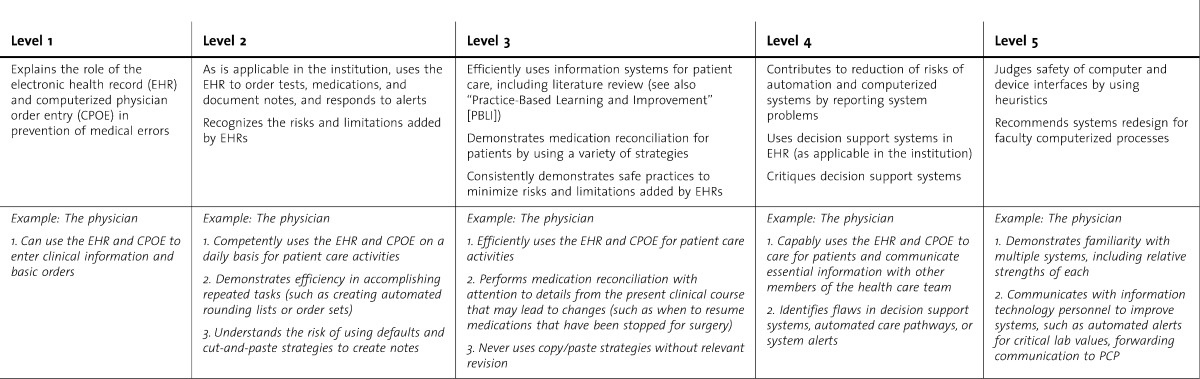
Table 14.
PBLI1 Improves via Feedback and Self-assessment

Table 15.
PBLI2 Learns and Improves by Asking and Answering Clinical Questions From a Patient Scenario
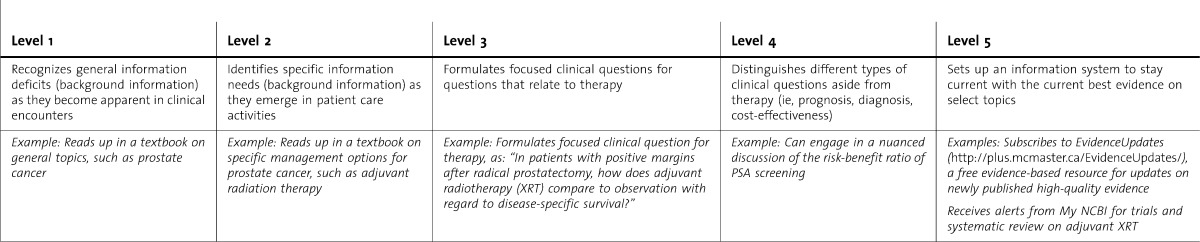
Table 16.
PBLI3 Acquires the Best Evidence

Table 17.
PBLI4 Appraises the Evidence for Validity, Impact, and Applicability
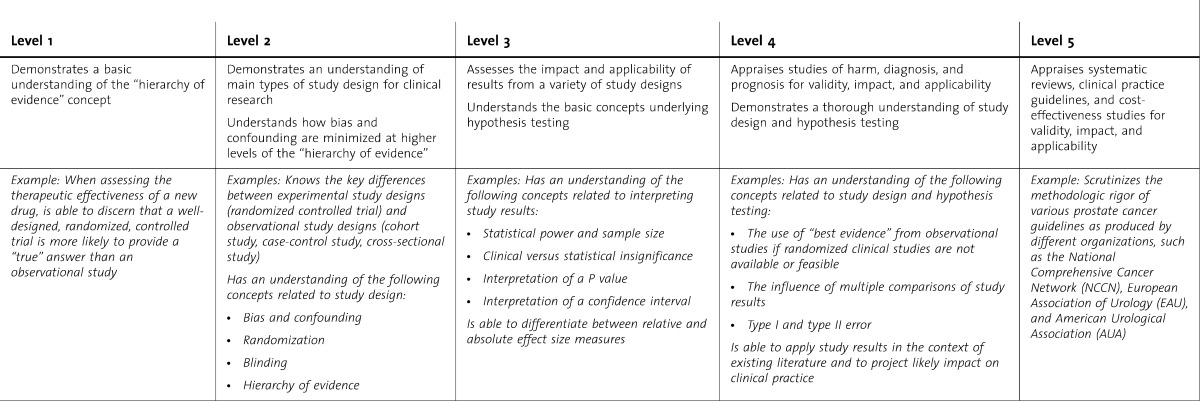
Table 18.
PBLI5 Applies the Evidence to Decision Making for Individual Patients
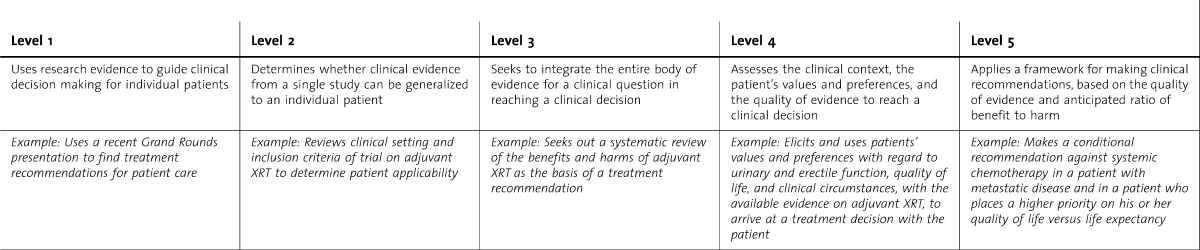
Table 19.
PBLI6 Improves the Quality of Care for a Panel of Patients
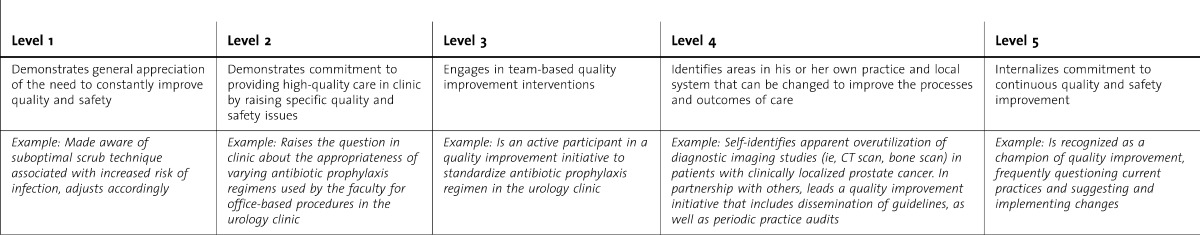
Table 20.
PBLI7 Participates in the Education of Other Team Members
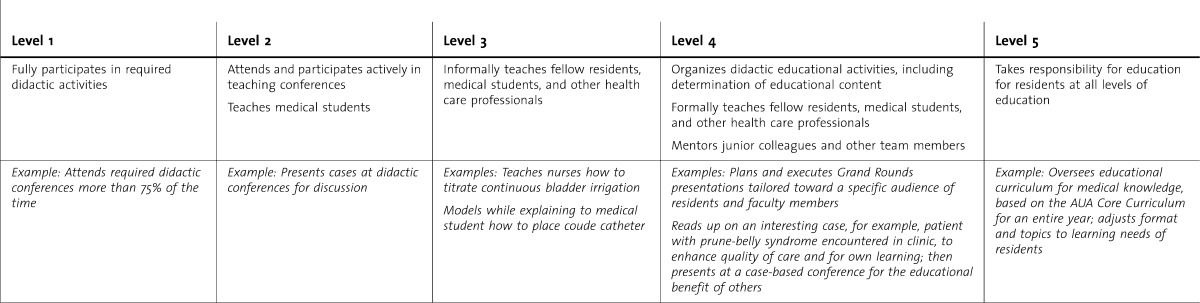
Table 21.
ICS1 Communicates Effectively With Patients and Families With Diverse Socioeconomic and Cultural Backgrounds • Medical Interviewing (also see PC) • Counseling and Education (also see PC) • Hospitalization Updates • Delivering Bad News • Informing About Medical Error

Table 22.
ICS2 Effectively Counsels, Educates, and Obtains Informed Consent (see PC )
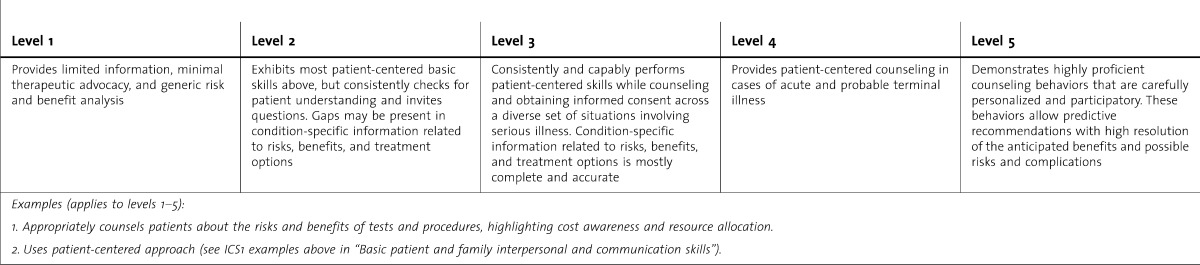
Table 23.
ICS3 Communicates Effectively With Physicians, Other Health Professionals, and Health-Related Agencies • Writing Diagnostic Reports • Referral (Oral and Written) • Consultations (Oral and Written) • Medical Records
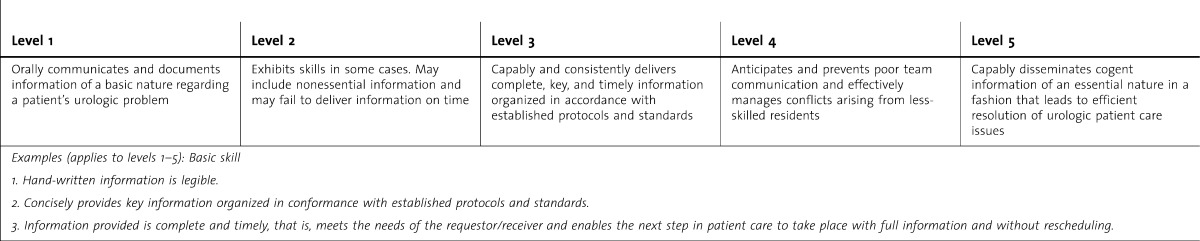
Table 24.
ICS4 Communicates Effectively During Care Transitions and Consultations With Fellow Residents
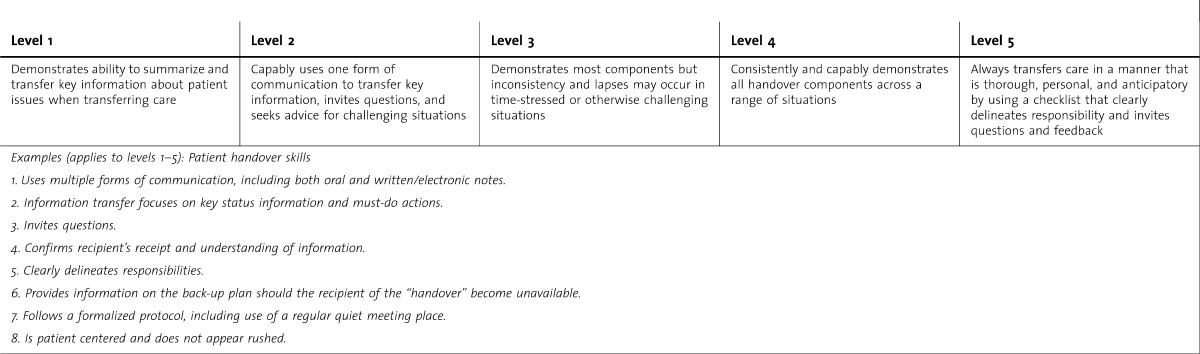
Table 25.
ICS5 Works Effectively as a Member or Leader of a Health Care Team or Other Professional Group (also see SBP3) • OR Team • Clinical Team (Office, Inpatient, or Outpatient/Clinic) • Professional Work Groups and Committees (eg, Quality Improvement, Research)
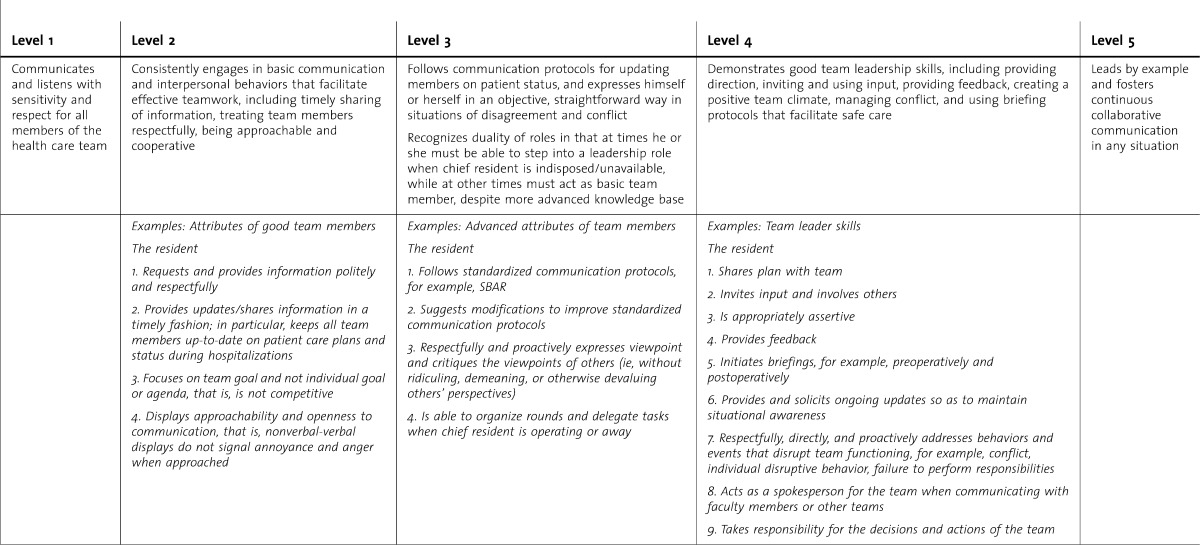
Table 26.
P1 Demonstrates Adherence to Ethical Principles
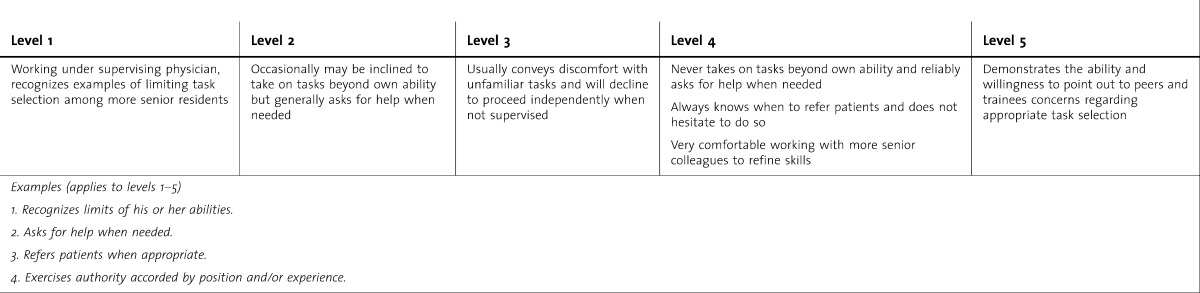
Table 27.
P2 Demonstrates Compassion, Integrity, and Respect for Others
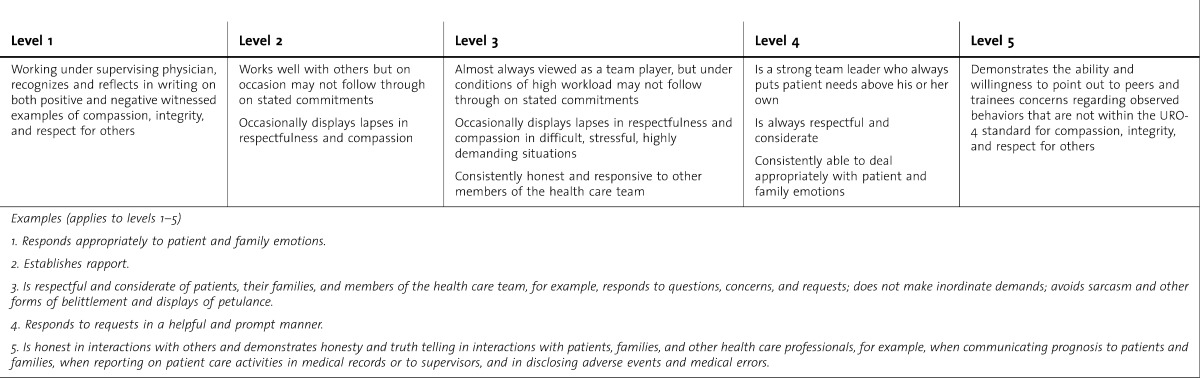
Table 28.
P3 Demonstrates Responsiveness to Patient Needs That Supersede Self-interest
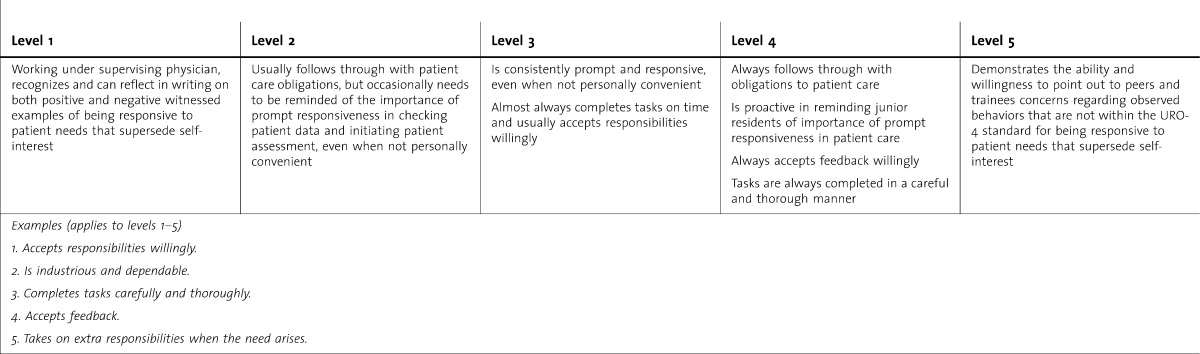
Table 29.
P4 Demonstrates Respect for Patient Privacy and Autonomy
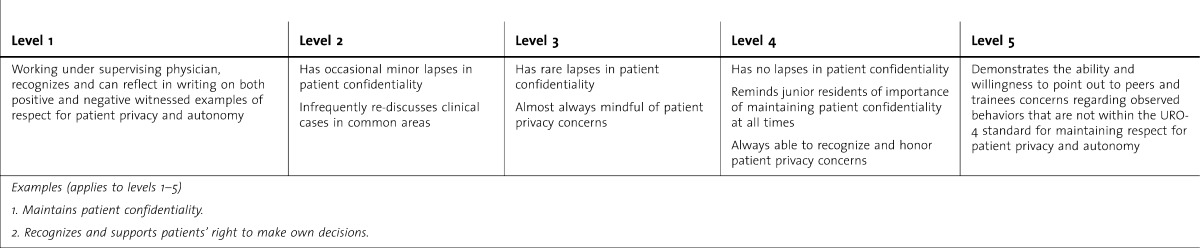
Table 30.
P5 Demonstrates Accountability to Patients, Society, and the Profession
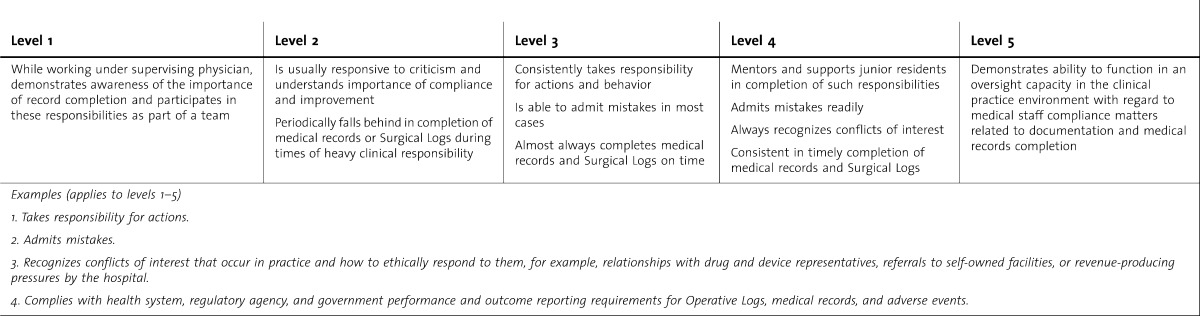
Table 31.
P6 Demonstrates Sensitivity and Responsiveness to Diverse Populations, Including Diversity in Gender, Age, Culture, Race, Religion, Disabilities, and Sexual Orientation
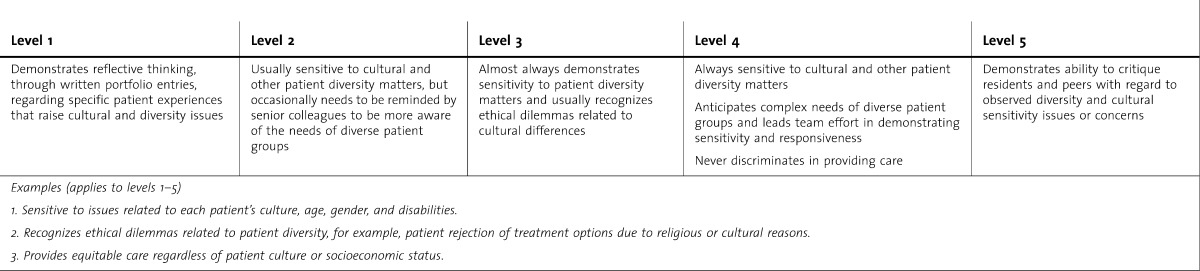
Table 32.
MK Demonstrates Level-Appropriate Competency in Core Domainsa as Indicated by Performance on the American Board of Surgery In-Training Examination (ABSITE) and AUA Resident ISE
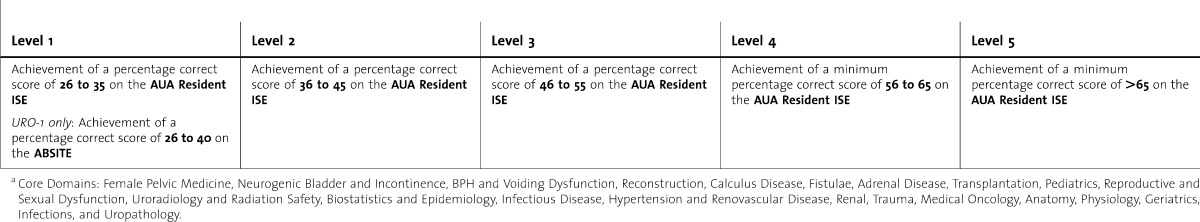
Footnotes
Michael Coburn, MD, FACS, is Professor and Chairman, Scott Department of Urology, and Urology Residency Program Director, Baylor College of Medicine; Christopher Amling, MD, is Professor and Chief, Division of Urology, Oregon Health and Science University; Robert R. Bahnson, MD, is The Dave Longaberger Chair in Urology, and Professor and Chairman, Department of Urology, Ohio State University; Philipp Dahm, MD, MHSc, is Professor of Urology and Residency Program Director, Department of Urology, University of Florida, College of Medicine; B. Price Kerfoot, MD, EdM, is Associate Professor, Surgical Service, Veterans Affairs Boston Healthcare System, Harvard Medical School; Louise King, MS, was Executive Director for the Review Committee of Urology (formerly, at the time of milestone development) and is Executive Director for the Review Committees of Psychiatry, Neurology, and Allergy and Immunology (currently), Accreditation Council for Graduate Medical Education; Brian Lane, MD, PhD, is Director, Minimally Invasive Surgery Program, Spectrum Health, and Clinical Associate Professor, Michigan State University College of Human Medicine; Michael L. Ritchey, MD, is Professor of Urology, Mayo Clinic College of Medicine; Charles D. Scales Jr, MD, MSHS, is Robert Wood Johnson Foundation/VA Clinical Scholar, Departments of Urology and Medicine, David Geffen School of Medicine, University of California, Los Angeles; Chandru P. Sundaram, MD, is Professor and Program Director, Department of Urology, Indiana University School of Medicine; and Susan R. Swing, PhD, is Vice President, Outcome Assessment, Accreditation Council for Graduate Medical Education.
The authors, all of whom participated in milestone development as members of the Urology Milestone Working Group, wish to thank the members of the Urology Milestone Advisory Group for their contributions to this work: Timothy P. Brigham, MDiv, PhD; Stuart S. Howards, MD; Michael O. Koch, MD; Gerald H. Jordan, MD; Jack W. McAninch, MD; Elspeth M. McDougall, MD; Glenn Preminger, MD; Michael Sheppard, CPA, CAE; Joseph Smith, MD; and William Steers, MD
The Milestones are designed only for use in evaluation of resident physicians in the context of their participation in ACGME-accredited residency or fellowship programs. The Milestones provide a framework for the assessment of the development of the resident physician in key dimensions of the elements of physician competency in a specialty or subspecialty. They neither represent the entirety of the dimensions of the 6 domains of physician competency, nor are they designed to be relevant in any other context.


