Abstract
Background
Perceived discrimination is associated with poor mental health and health-compromising behaviors in a range of vulnerable populations, but this link has not been assessed among pregnant women. We aimed to determine whether perceived discrimination was associated with these important targets of maternal health care among low-income pregnant women.
Methods
Face-to-face interviews were conducted in English or Spanish with 4,454 multi-ethnic, low-income, inner-city women at their first prenatal visit at public health centers in Philadelphia, Pennsylvania, USA, from 1999 to 2004. Perceived chronic everyday discrimination (moderate and high levels) in addition to experiences of major discrimination, depressive symptomatology (CES-D ≥23), smoking in pregnancy (current), and recent alcohol use (12 months before pregnancy) were assessed by patient self-report.
Results
Moderate everyday discrimination was reported by 873 (20%) women, high everyday discrimination by 238 (5%) women, and an experience of major discrimination by 789 (18%) women. Everyday discrimination was independently associated with depressive symptomatology (moderate = PR 1.58, 95% confidence interval (CI) 1.38-1.79, high = PR 1.82, 95% CI 1.49-2.21); smoking (moderate = PR 1.19, 95% CI 1.05-1.36, high = PR 1.41, 95% CI 1.15-1.74); and recent alcohol use (moderate = PR 1.23, 95% CI 1.12-1.36). However, major discrimination was not independently associated with these outcomes.
Conclusions
This study demonstrated that perceived chronic everyday discrimination, but not major discrimination, was associated with depressive symptoms and health-compromising behaviors independent of potential confounders, including race and ethnicity, among pregnant low-income women. (BIRTH 37:2 June 2010)
Keywords: alcohol drinking, depression, discrimination (psychology), health behavior, pregnant women, prenatal care, smoking
Women with low socioeconomic status are at greater risk of depressive symptomatology and health-compromising behaviors in pregnancy than women from less vulnerable populations (1-4). These characteristics are all associated with poor maternal-child outcomes, including low birthweight, developmental delay, and chronic illness in infancy (5-9). Smoking in pregnancy is associated with placental insufficiency, low birthweight, and preterm birth (5). Fetal exposure to alcohol is related to poor neurodevelopmental outcomes (7). Depressive symptoms, smoking, and alcohol use are all targets of major public health interventions for pregnant women, and the identification of social factors that contribute to their disproportional prevalence among vulnerable populations is critical to the development of effective risk reduction strategies.
Perceived discrimination, or unfair treatment based on personal characteristics identifying membership in a group perceived as inferior (e.g., racism, classism, sexism), is associated, in nonpregnant samples, with poor mental and physical health as well as health compromising behaviors among adults in low-income populations (10-13). Framed as a psychosocial stressor linking the social environment with physiologic state, perceived discrimination has been proposed to have negative consequences for mental and physical health (11). Adults who report discrimination are more likely to report greater depressive symptoms and major depression, poor cardiovascular health, and health compromising behaviors including smoking and alcohol use (13-15). Interestingly, the type of discrimination has also been suggested to influence the strength of the association with outcomes; chronic low level “everyday” discrimination has been theorized to have a stronger association with health outcomes than more severe but infrequent discrimination (13). This suggestion has important implications for the design of potential mitigating strategies.
Despite the evidence of links between depressive symptoms, health compromising behaviors, and perceived discrimination, little research has been conducted on this topic among pregnant women. In the few studies that have explored consequences of perceived discrimination in pregnancy, this exposure has been associated with higher levels of self-rated stress and adverse birth outcomes, including low birthweight and preterm birth for women with high depressive symptoms compared with women who have lower levels of symptoms (12, 16-20). In the only published study to date that assessed discrimination and depressive symptomatology in pregnancy, a positive and significant association was found (16). However, no analysis of links to health behaviors has been undertaken.
In the present study we investigated whether perceived discrimination was associated with depressive symptoms and two health-compromising behaviors -- smoking during pregnancy and recent alcohol use -- in a sample of pregnant low- income inner-city women. We also assessed the relative contribution of chronic, low level “everyday” discrimination versus reported experiences of major discrimination.
Methods
Study Population and Procedure
The data used for the current analyses were collected as part of a larger, community-based study examining maternal stress, and maternal and infant health and health-related behaviors. The larger study involved recruitment of women who enrolled for prenatal care at all of the members of a consortium of 8 health centers run by the Philadelphia Department of Public Health in Philadelphia, Pennsylvania, between February 1999 and September 2004. The prenatal sites were Federally Qualified Health Centers (FQHC), or FQHC look-alikes, which target vulnerable populations and are located throughout the city with that goal in mind. Prenatal care was provided by nurse-midwives following standard prenatal care models through contracts with local health care systems with obstetric services.
The data for this study were collected, after written consent was obtained, during a face-to- face oral interview at the time of the women's first prenatal care visit. All interviews used structured survey instruments and were conducted in English and Spanish by trained female interviewers. Eligibility criteria were: first prenatal care visit, English or Spanish speaking, and a singleton intrauterine pregnancy. Additional findings and more details about the larger study have been published elsewhere (21). Institutional Review Board approval was obtained for this study from Drexel University, the University of Pennsylvania, Thomas Jefferson University, and the Philadelphia Department of Public Health.
Independent Variables
Perceived discrimination
Perceived discrimination was assessed using two measures previously validated with similar populations: the Everyday Discrimination Scale and a modified assessment of major experiences of discrimination (13, 22, 23). The Everyday Discrimination Scale is composed of 9 items that measure the experience of chronic low-level discrimination and assess the frequency of unfair treatment in “day-to-day life.” Participants were told that discrimination refers to “being treated unfairly because of your race, ethnicity, income level, social class, sex, gender, age, sexual orientation, physical appearance, or religion” and were then asked to rate the frequency of their own experiences with the following: 1) you are treated with less courtesy than other people; 2) you are treated with less respect than other people; 3) you receive poorer service than other people at restaurants and stores; 4) people act as if they think you are not smart; 5) people act as if they are afraid of you; 6) people act as if they think you are dishonest; 7) people act as if they're better than you; 8) you are called names or insulted; and 9) you are threatened or harassed.
Frequency of these experiences was rated along a six-point Likert-like scale from “never” (0 points) to “almost everyday” (5 points). The total score was first summed and then categorized as follows: 1) none or very little discrimination (0-9 points); 2) “some” discrimination (moderate, 10-22 points); and 3) “a lot” of discrimination (high, 23-45 points). The answers were first summed at the time of the interview and participants were then asked whether the initial score reflected their actual experience. Final everyday discrimination scores were re-categorized if they did not. Ninety-six percent of the women agreed with the initial score; the remaining 4 percent were re-classified.
The experience of major discriminatory events was assessed with two questions: 1) “For unfair reasons, do you think that you have ever not been hired for a job?”; and 2) “Have you ever been unfairly stopped, searched, questioned, physically threatened or abused by the police?” Another question addressing a lack of promotion at work, a part of the original scale of major discrimination, was not used because of its lack of face validity in this sample of low-income pregnant women (11).
Other maternal characteristics
Potential confounders were identified a priori through a review of the literature on perceived discrimination, depressive symptoms, and health behaviors and included the following sociodemographic characteristics: maternal age, personal annual income, educational attainment, nativity, marital status, race/ethnicity, parity, and an objective stress scale described previously (25-31). The 13-point objective stress scale is based on self-reported difficulty in four domains: 1) housing (0-3 points); 2) intimate partner violence (0-3 points); 3) material hardship (other than housing; 0-3 points); and 4) neighborhood danger (0-4 points). This scale was categorized into tertiles as follows: 1) low (≤ 2 points); 2) moderate (3-4 points); and 3) high (≥ 5 points). Gestational age at interview and year of study enrollment were also assessed for potential confounding.
Dependent Variables
Depressive symptomatology
Depressive symptomatology was measured with the Center for Epidemiologic Studies Depression Scale (CES-D), a 20-item instrument widely used to assess depressive symptoms with scores ranging from 0-60. Because of the overlap of normal symptoms of pregnancy with those of depression, we used the commonly accepted higher cutpoint of ≥23 to indicate elevated depressive symptomatology in this study (32).
Health-compromising behaviors
Two self-reported health behaviors were selected because of their association with poor pregnancy outcomes and plausible association with perceived discrimination--smoking during the current pregnancy and recent alcohol use (30). Behaviors were assessed based on the selection of a dichotomous (Yes vs No) response to the items. Smoking during the current pregnancy was assessed by the question, “After you found out that you were pregnant this time, have you smoked at all?” Recent alcohol use was assessed with response to the question, “In the 12 months before you found out you were pregnant this time, did you have any beer, wine, 40's, coolers, liquor or other alcoholic beverages?”
Statistical Analysis
Bivariate associations between outcome and explanatory variables were assessed using Student's t test and chi-square statistics to determine statistical significance. The risk of association with each dependent variable – depressive symptoms, smoking in pregnancy, and recent alcohol use – was estimated using Poisson regression with robust standard errors rather than a more commonly used logistic regression. The choice of the Poisson model, which provides a prevalence ratio (PR), was based on the fact that the outcomes were relatively common (>20%) (33-35). The Poisson model provides a more conservative estimate of the relative risk that is closer to its sample value than when logistic regression is used in cross-sectional studies (confirmed in the present analyses, results not shown). Potential confounders were included in multiple regression models only if they had at least a weak association (p < 0.25) with perceived discrimination or the dependent variables. A two-sided significance level was set at p < 0.05. The statistical software SPSS release 12 (36) and Stata 8.2 (37) were used in all analyses.
Results
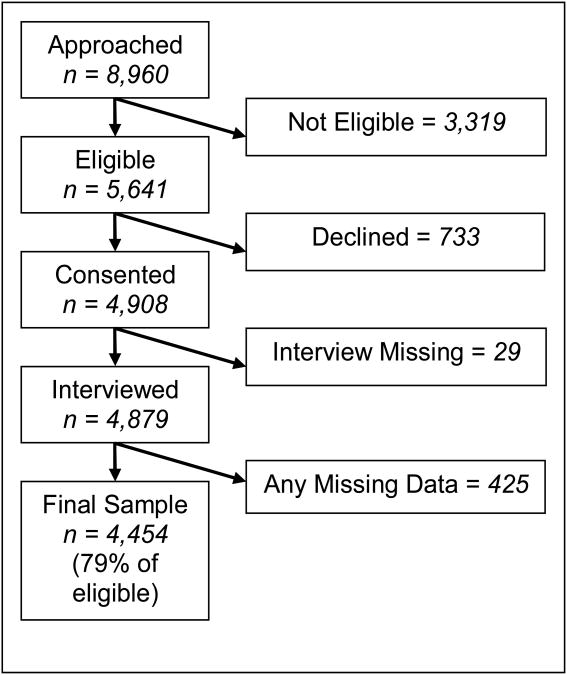
Figure 1 shows the original sample and the number of participants excluded from the final analytical sample. Of the initial 8,960 women initially identified, 5,641 were eligible, 4,908 (87%) consented to participate, and 4,879 were interviewed. Of those interviewed, 4,454 had complete data for the variables used in analyses, representing 79 percent of eligible women.
Fig. 1. Schematic representation of participant selection.
Descriptive characteristics of the final analytical study sample are shown in the first column of Table 1. Overall, the sample consisted of young, low-income, United States born, primarily non-Hispanic black women, with demographic, health, behavioral, and psychosocial characteristics consistent with a low-income urban population. Perceived discrimination was reported by a substantial proportion of the sample. Of the 4,454 pregnant women, 1,111 (25%) reported either moderate or high everyday discrimination, and 789 (18%) reported either one or two major discrimination events. A relatively large percentage of the women had depressive symptoms (959, 22%), 977 women (22%) reported smoking in the current pregnancy, and 1,561 (35%) reported recent alcohol use. Both measures of discrimination were significantly associated with all three dependent variables (p<0.001).
Table 1. Descriptive Statistics and the Associations with Depressive Symptoms, Smoking in Pregnancy, and Recent Alcohol Use.
| Independent Variables | Total n=4,454 (100%) No. (%) | CES-D ≥ 23 n=959 (22%) No. (%) | P | Current Smoking n=977 (22%) No. (%) | P | Alcohol Use in Prev 12 Months n=1561 (35%) No. (%) | P |
|---|---|---|---|---|---|---|---|
| Demographics | |||||||
| Age (yr), mean(SD) | 24.4 (5.8) | 24.4(5.7) | 0.880 | 25.5 (5.6) | <0.001 | 24.9 (5.6) | <0.001 |
| Annual income, mean(SD) | 9,241(10,000) | 9,393.3 (10324.9) | 0.630 | 9,800 (11,000) | 0.059 | 10,700 (10,721) | <0.001 |
| Education | |||||||
| >High school | 822(19) | 150(16) | 0.001 | 90 (9) | <0.001 | 304 (20) | <0.001 |
| High school/GED* | 1,966 (44) | 403(42) | 390 (40) | 720 (46) | |||
| <High school | 1,010 (23) | 149(16) | 365 (37) | 370 (24) | |||
| Still in high school | 656 (15) | 259(27) | 132 (14) | 167 (11) | |||
| Foreign Born | 1,007 (23) | 192(20) | 0.029 | 75 (7.7) | <0.001 | 236 (15) | <0.001 |
| Single | 3,351 (75) | 779(81) | <0.001 | 807 (83) | <0.001 | 1237 (79) | <0.001 |
| Race/Ethnicity | |||||||
| Black (non-Hispanic) | 3,002 (67) | 678(71) | 0.022 | 623 (64) | <0.001 | 1057 (68) | <0.001 |
| White (non-Hispanic) | 410 (9) | 92(10) | 209 (21) | 232 (15) | |||
| Latina/Hispanic | 915 (21) | 163(17) | 127 (13) | 239 (15) | |||
| Other | 132 (3) | 28(3) | 18 (1.8) | 33 (2) | |||
| Parity | |||||||
| 0 | 1831 (41) | 366(38) | 0.001 | 322 (33) | <0.001 | 640 (41) | 0.807 |
| 1 | 1320 (30) | 438(46) | 266 (27) | 455 (29) | |||
| 2+ | 1308 (30) | 157(16) | 389 (40) | 466 (30) | |||
| Objective Stress | |||||||
| Low (0-2) | 1,483 (33) | 176(18) | <0.001 | 228 (23) | <0.001 | 461 (30) | <0.001 |
| Moderate (3-4) | 1,422 (32) | 295(31) | 280 (29) | 471 (30) | |||
| High (5-14) | 1,554 (35) | 490(51) | 469 (48) | 629 (40) | |||
| Everyday Discrimination (ED) | |||||||
| None or very little | 3343(75) | 575(60) | <0.001 | 654 (67) | <0.001 | 1075 (69) | <0.001 |
| Moderate | 873(20) | 282(30) | 231 (24) | 380 (24) | |||
| High | 238(5) | 102(11) | 92 (9) | 106 (7) | |||
| Major Discrimination (MD) | |||||||
| None | 3,665(82) | 705(73.5%) | <0.001 | 758 (78) | <0.001 | 1225 (79) | <0.001 |
| One event | 678(15) | 210(21.9%) | 171 (18) | 279 (18) | |||
| Two events | 111(3) | 44(4.6%) | 48 (5) | 57 (4) |
GED = General equivalency diploma.
Depressive symptoms did not vary by age or income (p>0.05), but smoking and recent alcohol use were more prevalent among older women (p<0.001). Higher reported annual income was also associated with recent alcohol use (p<0.001). Depressive symptoms, smoking, and recent alcohol use were all associated with lower educational attainment, United States place of birth, black race/ethnicity, higher parity, and higher levels of objectively measured stressors (p<0.05).
Table 2 presents the prevalence ratios with their 95 percent confidence intervals from bivariate (model A) and multivariable (model B) regression models for each outcome of interest. In the unadjusted models, both everyday discrimination and major discrimination exhibited a significant association with each outcome. However, after adjustment for potential confounders (model B), only everyday discrimination remained significantly associated with each outcome. The prevalence ratio of moderate everyday discrimination for depressive symptomatology was 1.58 (95% CI: 1.38-1.79), and for high everyday discrimination it was 1.82 (95% CI: 1.49-2.21). For smoking in pregnancy the prevalence ratios for moderate and high everyday discrimination were 1.19 (95% CI:105-1.36) and 1.41(95% CI:1.15-1.74), respectively. The adjusted prevalence ratio for moderate and high everyday discrimination for recent alcohol use was 1.23 (95% CI: 1.12-1.36) and 1.13 (95% CI: 0.94-1.34), respectively. No significant interactions were found between either form of discrimination and race/ethnicity for the risk of depressive symptoms, smoking, or alcohol use.
Table 2. Multiple regression analyses of association between perceived discrimination and depressive symptoms, current smoking, and recent alcohol use among women in pregnancy.
| Independent Variables | CES-D ≥ 23 | Current Smoking | Recent Alcohol Use | |||
|---|---|---|---|---|---|---|
|
| ||||||
| (n=4,454) | Model-A PR (95% CI) | Model-B* aPR (95% CI) | Model A PR (95% CI) | Model B** aPR (95% CI) | Model A PR (95% CI) | Model B** aPR (95% CI) |
| Everyday discrimination | ||||||
| None or very little | Reference | Reference | Reference | Reference | Reference | Reference |
| Moderate | 1.88(1.66, 2.12) | 1.58(1.38, 1.79) | 1.35(1.19, 1.54) | 1.19(1.05-1.36) | 1.35(1.24-1.48) | 1.23(1.12-1.36) |
| High | 2.49(2.11, 2.94) | 1.82(1.49, 2.21) | 1.98(1.66, 2.35) | 1.41(1.15-1.74) | 1.38(1.19-1.61) | 1.13(0.94-1.34) |
| Major discrimination | ||||||
| None | Reference | Reference | Reference | Reference | Reference | Reference |
| One event | 1.61(1.41, 1.83) | 1.16(1.00, 1.33) | 1.22(1.06-1.41) | 0.99(0.86-1.15) | 1.23(1.11-1.36) | 1.07(0.96-1.19) |
| Two events | 2.06(1.62, 2.61) | 1.09(0.84, 1.45) | 2.09(1.67-2.62) | 1.23(0.95-1.59) | 1.54(1.27-1.85) | 1.14(0.92-1.42) |
Results in bold are statistically significant.
Model A = Unadjusted Prevalence Ratio (PR)
Model B = Adjusted Prevalence Ratio (aPR)
Variables included in the models: age, income, education, foreign born, marital status, race/ethnicity, parity, and objective stress.
Variables included in the models identical to * above with addition of CES-D (<23 vs ≥23).
Discussion
In this sample of more than 4,500 low-income, inner-city expectant women, perceived “everyday” discrimination and reported major discriminatory events were common, and both exhibited significant unadjusted association with depressive symptoms, smoking, and recent alcohol use in pregnancy. However, only everyday discrimination remained a significant predictor of depressive symptomatology and both health behaviors, after controlling for major discrimination, demographic, and other potential confounding variables, including race/ethnicity. Race/ethnicity did not moderate (no interactions were identified) the association between everyday discrimination and depression symptoms, smoking, or recent alcohol use. In the adjusted model, women with high levels of perceived everyday discrimination were nearly twice as likely as women with no or very little experience with discrimination to have depressive symptomatology. The association between perceived discrimination and smoking was also significant, although somewhat less pronounced. Only moderate everyday discrimination remained a significant predictor of recent alcohol use. Our results are consistent with previous studies proposing that chronic low-level discriminatory experiences have more detrimental consequences for emotional health than more isolated events of greater magnitude (13). This finding is important because chronic low-level discrimination may also be less recognizable to patients and health providers than isolated more dramatic events.
Previous studies have shown that although minority populations were more likely to report racial discrimination, discrimination was also reported by non-Hispanic white adults (11, 13, 17, 18, 38). Unlike our findings studies of perceived racial discrimination have shown stronger associations with smoking among minority race/ethnic populations than among whites (38). Importantly, the instruments used in our study were not limited to identifying race/ethnic discrimination; unfair treatment attributable to other characteristics such as gender, class, religion, appearance, and sexual orientation were also assessed. In fact, white and non-Hispanic black women have been found to report equal rates of gender discrimination (39). A recent study of pregnant women also found that although African American women reported higher levels of perceived discrimination, this association was greatly reduced or eliminated when adjusting for socioeconomic status (16). Several studies have also documented an association between birth outcomes and perceived discrimination, but these studies have often used measures that focus on racial bias rather than on broader forms of discrimination (12, 13, 18-20). Our findings support a broader view of potential consequences of discrimination that is not limited to racial discrimination but more widely to everyday experiences of women, particularly those in low socioeconomic groups.
The association between perceived discrimination and mental health and health behaviors has received increased attention in recent years in studies examining health disparities (22, 42-45), with most studies documenting significant associations, particularly for mental health (11, 40). We have extended previous studies to include low-income inner-city pregnant women, who are at a high risk of poor birth outcomes. The association between perceived discrimination and mental health and adverse health behaviors is of particular interest during pregnancy because of their association with negative maternal and child outcomes. At the same time, little is known about the potential contribution of perceived discrimination to health compromising behaviors during pregnancy, which have also been linked to an elevated risk of preterm birth (12, 18, 20). In the current study, we have identified significant associations between everyday discrimination and health behaviors, which themselves are associated with birth outcomes (4, 7, 30).
This study has implications both for future research and for clinical practice. The prevalence and independent association of perceived discrimination with depressive symptoms and health-compromising behaviors point to the need to address discrimination in interventions to reduce disparities in psychological health and health behaviors in pregnancy. For maternal health care practitioners these results indicate the saliency of discrimination for women experiencing emotional distress in pregnancy. The association between discrimination and these maternal health outcomes was independent of race and ethnicity, suggesting that discrimination is relevant to understanding health disparities among low-income women more generally.
Some limitations of this study should be noted. First, we use cross-sectional data and cannot assess the causal relationship between discrimination and our outcomes of interest. For example, it is possible that women with preexisting depressive symptoms are more likely to perceive discrimination. However, current evidence from longitudinal research suggests that experiences of discrimination actually increase the risk of depression rather than the other way around (12). Longitudinal studies like this one among pregnant women would provide stronger evidence for the temporal relationship of perceived discrimination with the depressive symptomatology and health behaviors assessed. Second, we assessed self-reported health behaviors rather than using direct biological measures of smoking and alcohol use, which could have resulted in their underreporting. However, self-reported health behaviors have been validated with biological measures, which generally show low misclassification of smoking status (46, 47). Alcohol use was self-reported for the 12 months prior to pregnancy and so is not precisely in pregnancy; however, behavior in this preconception period is a critical risk for alcohol-related pregnancy outcomes (48). Third, we tested for elevated depressive symptomatology rather than the clinical diagnosis of major depression. However, a CES-D score of 23 or above has been associated with increased obstetric and perinatal risk, and thus factors that may lead to elevated scores are important targets for study (44, 45). The standard cutpoint used here is also a commonly used indicator of the need for further assessment of possible major depression. Fourth, although our study population represents a low-income inner-city population and thus limits how widely our findings can be generalized, this population is also at a high risk of poor pregnancy outcomes. Our study thus extends previous work linking perceived discrimination with psychological distress and health compromising behaviors to a pregnant population. Furthermore, the large sample makes it possible to assess carefully whether perceived discrimination predicts depressive symptoms and health behaviors within this high-risk sample. We have shown that the magnitude of the association between depressive symptoms and perceived discrimination does not vary by race and ethnicity. This result may be related to the low income of our sample, and a larger study would be needed to assess this association in a population with a wider income distribution.
Conclusions
This study demonstrated that perceived chronic everyday discrimination, but not major discrimination, was associated with depressive symptoms and health-compromising behaviors independent of potential confounders, including race and ethnicity, among pregnant low-income women.
Acknowledgments
This work was partly funded by the National Institute of Child Health and Human Development (1ROl D36462-01A I), Bethesda, Maryland, and the Centers for Disease Control and Prevention (TS 312‐15/15), Atlanta, Georgia. Dr. Bennett is supported by a career development grant from the National Institute of Child Health and Human Development, National Institutes of Health (1K23HD048915-01A2), Bethesda, Maryland, USA.
Contributor Information
Ian M. Bennett, Department of Family Medicine and Community Health, Philadelphia.
Jennifer F. Culhane, Department of Obstetrics and Gynecology, Drexel University School of Medicine, Philadelphia.
David A. Webb, Department of Obstetrics and Gynecology, Drexel University School of Medicine, Philadelphia.
James C. Coyne, Department of Psychiatry, University of Pennsylvania School of Medicine, Philadelphia.
Vijaya Hogan, Gillings School of Global Public Health, University of North Carolina, Chapel Hill, North Carolina.
Leny Mathew, Children's Hospital of Philadelphia, Philadelphia.
Irma T. Elo, Department of Sociology, University of Pennsylvania, Philadelphia, Pennsylvania, USA.
References
- 1.Colman GJ, Joyce T. Trends in smoking before, during, and after pregnancy in ten states. Am J Prev Med. 2003;24:29–35. doi: 10.1016/s0749-3797(02)00574-3. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC. Epidemiology of women and depression. J Affect Disord. 2003;74:5–13. doi: 10.1016/s0165-0327(02)00426-3. [DOI] [PubMed] [Google Scholar]
- 3.Perreira KM, Cortes KE. Race/ethnicity and nativity differences in alcohol and tobacco use during pregnancy. Am J Public Health. 2006;96:1629–1636. doi: 10.2105/AJPH.2004.056598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dole N, Savitz DA, Siega-Riz AM, Hertz-Picciotto I, McMahon MJ, Buekens P. Psychosocial factors and preterm birth among African American and White women in central North Carolina. Am J Public Health. 2004;94:1358–65. doi: 10.2105/ajph.94.8.1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Higgins S. Smoking in pregnancy. Curr Opin Obstet Gynecol. 2002;14:145–51. doi: 10.1097/00001703-200204000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Albertsen K, Andersen AN, Olson J, Gronbaek M. Alcohol consumption during pregnancy and risk of preterm birth. Am J Epidemiol. 2004;159:155–61. doi: 10.1093/aje/kwh034. [DOI] [PubMed] [Google Scholar]
- 7.American Academy of Pediatrics. Committee on Substance Abuse and Committee on Children With Disabilities. Fetal alcohol syndrome and alcohol-related neurodevelopmental disorders. Pediatrics. 2000;106:358–61. [PubMed] [Google Scholar]
- 8.Pilowsky DJ, Wickramaratne PJ, Rush AJ, et al. Children of currently depressed mothers: a STAR*D ancillary study. J Clin Psychiatry. 2006;67:126–36. doi: 10.4088/jcp.v67n0119. [DOI] [PubMed] [Google Scholar]
- 9.U.S. Department of Health and Human Services. Healthy People. Washington, DC: Author; 2010. p. 2000. [Google Scholar]
- 10.Brown TN, Williams DR, Jackson JS, et al. “Being black and feeling blue”: The mental health consequences of racial discrimination. Race Soc. 2000;2:117–131. [Google Scholar]
- 11.Paradies Y. A systematic review of empirical research on self-reported racism and health. Int J Epidemiol. 2006;35:888–901. doi: 10.1093/ije/dyl056. [DOI] [PubMed] [Google Scholar]
- 12.Mustillo S, Krieger N, Gunderson EP, Sidney S, McCreath H, Kiefe CI. Self-reported experiences of racial discrimination and Black-White differences in preterm and low-birthweight deliveries: the CARDIA Study. Am J Public Health. 2004;94:2125–31. doi: 10.2105/ajph.94.12.2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams DR, Yu Y, Jackson JS. Racial differences in physical and mental health. J Health Psychol. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 14.Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans: A biopsychosocial model. Am Psychol. 1999;54:805–16. doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]
- 15.Wyatt SB, Williams DR, Calvin R, Henderson FC, Walker ER, Winters K. Racism and cardiovascular disease in African Americans. Am J Med Sci. 2003;325:315–31. doi: 10.1097/00000441-200306000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Canady RB, Bullen BL, Holzman C, Broman C, Tian Y. Discrimination and symptoms of depression in pregnancy among African American and White women. Womens Health Issues. 2008;18:292–300. doi: 10.1016/j.whi.2008.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stancil TR, Hertz-Picciotto I, Schramm M, Watt-Morse M. Stress and pregnancy among African-American women. Paediatr Perinat Epidemiol. 2000;14:127–35. doi: 10.1046/j.1365-3016.2000.00257.x. [DOI] [PubMed] [Google Scholar]
- 18.Dole N, Savitz DA, Hertz-Picciotto I, Siega-Riz AM, McMahon MJ, Buekens P. Maternal stress and preterm birth. Am J Epidemiol. 2003;157:14–24. doi: 10.1093/aje/kwf176. [DOI] [PubMed] [Google Scholar]
- 19.Rosenberg L, Palmer JR, Wise LA, Horton NJ, Corwin MJ. Perceptions of racial discrimination and the risk of preterm birth. Epidemiology. 2002;13:646–52. doi: 10.1097/00001648-200211000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Collins JW, David RJ, Handler A, Wall S, Andes S. Very low birthweight in African American infants: The role of maternal exposure to interpersonal racial discrimination. Am J Public Health. 2004;94:2132–8. doi: 10.2105/ajph.94.12.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Culhane JF, Rauh V, McCollum KF, et al. Maternal stress is associated with bacterial vaginosis in human pregnancy. Matern Child Health J. 2001;5:127–34. doi: 10.1023/a:1011305300690. [DOI] [PubMed] [Google Scholar]
- 22.Schulz AJ, Gravlee CC, Williams DR, Israel BA, Mentz G, Rowe Z. Discrimination, symptoms of depression, and self-rated health among African American women in Detroit: Results from a longitudinal analysis. Am J Public Health. 2006;96:1265–70. doi: 10.2105/AJPH.2005.064543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guthrie BJ, Young AM, Williams DR, Boyd CJ, Kintner EK. African American girls' smoking habits and day-to-day experiences with racial discrimination. Nurs Res. 2002;51:183–90. doi: 10.1097/00006199-200205000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Culhane JF, Rauh V, McCollum KF, Elo IT, Hogan V. Exposure to chronic stress and ethnic differences in rates of bacterial vaginosis among pregnant women. Am J Obstet Gynecol. 2002;187:1272–6. doi: 10.1067/mob.2002.127311. [DOI] [PubMed] [Google Scholar]
- 25.Jones RK, D J, Henshaw SK. Contraception use among U.S. women having abortions in 2000-2001. Perspect Sex Reprod Health. 2002;34:294–303. [PubMed] [Google Scholar]
- 26.Cubbin C, Braveman PA, Marchi KS, Chavez GF, Santelli JS, Gilbert BJ. Socioeconomic and racial/ethnic disparities in unintended pregnancy among postpartum women in California. Matern Child Health J. 2002;6:237–46. doi: 10.1023/a:1021158016268. [DOI] [PubMed] [Google Scholar]
- 27.Henshaw SK. Unintended pregnancy in the United States. Fam Plann Perspect. 1998;30:24-9–46. [PubMed] [Google Scholar]
- 28.Berenson AB, Breitkopf CR, Wu ZH. Reproductive correlates of depressive symptoms among low-income minority women. Obstet Gynecol. 2003;102:1310–7. doi: 10.1016/j.obstetgynecol.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 29.Gelberg L, Leake B, Lu MC, et al. Chronically homeless women's perceived deterrents to contraception. Perspect Sex Reprod Health. 2002;34:278–85. [PubMed] [Google Scholar]
- 30.Huizink AC, Mulder EJH. Maternal smoking, drinking or cannabis use during pregnancy and neurobehavioral and cognitive functioning in human offspring. Neurosci Biobehav Rev. 2006;30:24–41. doi: 10.1016/j.neubiorev.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 31.Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. Am J Public Health. 2003;93:200–8. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roberts RE. Reliability of the CES-D Scale in different ethnic contexts. Psychiatry Res. 1980;2:125–34. doi: 10.1016/0165-1781(80)90069-4. [DOI] [PubMed] [Google Scholar]
- 33.Barros AJD, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol. 2003;3:21. doi: 10.1186/1471-2288-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–6. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 35.Spiegelman D, H E. Easy SAS calculations for risk and prevalence ratios and differences. Am J Epidemiol. 2005;162:199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- 36.SPSS Inc. SPSS for Windows, Rel 12.0. Chicago: Author; 2001. [Google Scholar]
- 37.StataCorp. Stata Statistical Software: Release 8. Texas: Author; 2003. College Station. [Google Scholar]
- 38.Landrine H, Klonoff EA, Corral I, Fernandez S, Roesch S. Conceptualizing and measuring ethnic discrimination in health research. J Behav Med. 2006;29:79–94. doi: 10.1007/s10865-005-9029-0. [DOI] [PubMed] [Google Scholar]
- 39.Watson JM, Scarinci IC, Klesges RC, Slawson D, Beech BM. Race, socioeconomic status, and perceived discrimination among healthy women. J Womens Health Gend Based Med. 2002;11:441–51. doi: 10.1089/15246090260137617. [DOI] [PubMed] [Google Scholar]
- 40.Williams DR, Williams-Morris R. Racism and mental health: the African American experience. Ethn Health. 2000;5:243–68. doi: 10.1080/713667453. [DOI] [PubMed] [Google Scholar]
- 41.Barnes LL, Mendes De Leon CF, Wilson RS, Bienias JL, Bennett DA, Evans DA. Racial differences in perceived discrimination in a community population of older blacks and whites. J Aging Health. 2004;16:315–37. doi: 10.1177/0898264304264202. [DOI] [PubMed] [Google Scholar]
- 42.Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. J Health Soc Behav. 1999;40:208–30. [PubMed] [Google Scholar]
- 43.Schnittker J, Mcleod JD. The social psychology of health disparities. Ann Rev Sociol. 2005;31:75–103. [Google Scholar]
- 44.Orr ST, James SA, Blackmore Prince C. Maternal prenatal depressive symptoms and spontaneous preterm births among African-American women in Baltimore, Maryland. Am J Epidemiol. 2002;156:797–802. doi: 10.1093/aje/kwf131. [DOI] [PubMed] [Google Scholar]
- 45.Orr ST, Miller CA. Maternal depressive symptoms and the risk of poor pregnancy outcome. Review of the literature and preliminary findings. Epidemiol Rev. 1995;17:165–71. doi: 10.1093/oxfordjournals.epirev.a036172. [DOI] [PubMed] [Google Scholar]
- 46.Higgins ST, Heil SH, Badger GJ, et al. Biochemical verification of smoking status in pregnant and recently postpartum women. Exp Clin Psychopharmacol. 2007;15:58–66. doi: 10.1037/1064-1297.15.1.58. [DOI] [PubMed] [Google Scholar]
- 47.Studts JL, Ghate SR, Gill JL, et al. Validity of self-reported smoking status among participants in a lung cancer screening trial. Cancer Epidemiol Biomarkers Prev. 2006;15:1825–1828. doi: 10.1158/1055-9965.EPI-06-0393. [DOI] [PubMed] [Google Scholar]
- 48.Floyd RL, Jack BW, Cefalo R, et al. The clinical content of preconception care: Alcohol, tobacco, and illicit drug exposures. Am J Obstet Gynecol. 2008;199:S333–S339. doi: 10.1016/j.ajog.2008.09.018. [DOI] [PubMed] [Google Scholar]