Abstract
Objective
Our objective was to determine patterns, reasons for, and correlates of complementary and alternative medicine use by United States adults with migraines/severe headaches.
Background
While many patients with chronic conditions use complementary and alternative medicine, little is known about complementary and alternative medicine use by adults with migraines/severe headaches.
Methods
We compared complementary and alternative medicine use between adults with and without self-reported migraines/severe headaches using the 2007 National Health Interview Survey (n=23,393), a national cross-sectional survey.
Results
Adults with migraines/severe headaches used complementary and alternative medicine more frequently than those without (49.5% vs. 33.9%, p<0.0001); differences persisted after adjustment (adjusted odds ratio=1.29, 95% confidence interval [1.15, 1.45]). Mind-body therapies (e.g. deep breathing exercises, meditation, yoga) were used most commonly. More than 50% of adults with migraines/severe headaches reporting complementary and alternative medicine use had not discussed it with their health care provider. Nonetheless, those with migraines/severe headaches used complementary and alternative medicine more often than those without because of provider recommendation and because conventional treatments were perceived as ineffective or too costly. Correlates of complementary and alternative medicine use among adults with migraines/severe headaches included anxiety, joint or low back pain, alcohol use, higher education, and living in the western United States. Only 4.5% of adults with migraines/severe headaches reported using complementary and alternative medicine to specifically treat their migraines/severe headaches.
Conclusions
Complementary and alternative medicine is used more often among adults with migraines/severe headaches than those without. However, few report using complementary and alternative medicine to specifically treat migraines/severe headaches. Mind-body therapies are used most frequently. Further research is needed to understand the effectiveness and mechanisms of complementary and alternative medicine treatments in adults with migraines/severe headaches.
Keywords: Epidemiology, Prevalence studies, Migraine, Severe headache, Complementary and alternative medicine, Mind-body medicine
Introduction
Migraine headaches afflict 13% of the United States (U.S.) population.1 The personal and societal burden is enormous, affecting quality of life 2, 3 and costing the U.S. $11 billion annually.4 Despite available conventional treatments, many patients with migraines fail to achieve optimal control or have unacceptable medication side effects.
Complementary and alternative medicine (CAM) includes both complementary therapies used as an addition to conventional treatments and alternative treatments used instead of conventional therapies, although adults with migraines rarely use only alternative treatments.5 The National Institutes of Health defines complementary and alternative medicine (CAM) as a group of diverse medical and health care systems, practices, and products that are not generally considered conventional medicine.6 A prior national survey showed that adults with headaches judged CAM therapies to be more helpful than conventional care for treatment of headaches.7 Previously, we reported that adults with common neurological conditions used CAM more frequently than those without (44.1 vs. 32.6%, p<0.0001).8 However, little is known about the patterns of CAM use in adults with migraines. Only a few prior surveys have examined CAM use in patients with headaches, and most were conducted in outpatient headache centers with small samples.5, 9-14 Knowing the prevalence and patterns of use of CAM in adults with migraines will help to characterize areas of potential underuse and barriers to use, as well as potential risks of CAM therapies in adults with migraines. Further, recognizing discrepancies between the scientific evidence and the prevalence of CAM use for patients with migraines may aid in our understanding of the medical and psychosocial needs of patients with migraines and target future areas of research. In this context, we analyzed the 2007 National Health Interview Survey (NHIS) to examine the patterns of CAM use in adults with migraines/severe headaches in the U.S. We describe the types of CAM therapies used by adults with migraines/severe headaches, and explore their reasons for use, disclosure to health care providers, and correlates of CAM use.
Methods
Data Source
The NHIS is an annual nationally-representative health survey of the civilian U.S. population that was designed to obtain national estimates of health status, prevalence of medical conditions, and health care access and utilization.15 NHIS is made publicly available, which we accessed via the Centers for Disease Control and Prevention’s National Center for Health Statistics website.16 NHIS employs a multistage stratified sampling design to select households for face-to face interviews, conducted in English and/or Spanish.15 Hispanic, Asian, and African American populations are oversampled to obtain more precise estimates for these populations. One adult, aged ≥ 18, was randomly selected from each household to answer the Sample Adult questionnaire. In 2007, NHIS administered an alternative medicine supplement to better understand the use of CAM therapies.15 Participants were asked: “During the past 12 months, have you used (specific therapy)?” The final adult sample included 23,393 respondents, with an overall response rate of 67.8%.15
Migraines/Severe Headaches
Sampled adults were asked, “In the past three months, did you have a severe headache or migraine?”
Outcomes of Interest
Our primary outcome was use of at least one CAM therapy within the previous 12 months, excluding prayer, vitamin use, special diets, and traditional healers, exclusions common in epidemiological studies on CAM use. CAM therapies were grouped into four broad categories: alternative medical systems (Ayurveda, acupuncture, homeopathy, naturopathy), manipulation/bodywork therapies (massage, chiropractic care, Feldenkreis, Alexander technique), biologically-based therapies (herbal/other supplements, but not common vitamins or minerals; chelation therapy), and mind-body therapies (biofeedback, energy healing, hypnosis, tai chi, yoga, qi gong, meditation, guided imagery, progressive relaxation, deep breathing exercises). Among the herbal/other supplements, we further explored use of herbs and supplements commonly promoted for treatment of migraines, including feverfew and Coenzyme Q.
For each therapy used in the previous year, respondents were asked about reasons for CAM use and disclosure to conventional practitioners. Respondents then answered yes/no to seven items: (1) to improve or enhance energy; (2) for general wellness/general disease prevention; (3) to improve/enhance immune function; (4) because conventional medical treatments did not help; (5) because conventional medical treatments were too expensive; (6) it was recommended by a health care provider; (7) it was recommended by family, friends, or co-workers. Adults who reported use of a specific CAM therapy were then separately asked, “For what health problems or conditions did you use [CAM therapy]?“
Correlates of CAM Use
We considered potential correlates of CAM use reported previously.17, 18 Sociodemographic characteristics included sex, age (18-24, 25-44, 45-64, 65-74, and ≥75), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, Asian, other), region of U.S. residence (Northeast, Midwest, South, West), birthplace (U.S. born, foreign born), educational attainment (<high school, high school, >high school), imputed family income provided by NHIS19 ($0-19,999; 20-34,999; 35-64,999; and ≥65,000) and marital status (married/living with partner, widowed, divorced/separated, never married). Potential indicators of illness burden included perceived health status (excellent/very good/good, fair, poor), presence of functional limitations (difficulty performing any of the following independently: walking 3 city blocks, walking up stairs, standing for 2 hours, using fingers to grasp small objects, going shopping, or participating in social activities), number of emergency room (ER) visits in past year (0, 1, 2+), self-reported medical conditions (diabetes, cancer, coronary artery disease, myocardial infarction, hypertension, hyperlipidemia, neck pain, insomnia, arthritis, joint pain, low back pain, depression, anxiety). We did not include neck pain or insomnia because of concerns that they may be on the causal pathway for migraine. Indicators that might alter access to care included insurance status (uninsured, Medicare, Medicaid, private, other), delayed care because of worries about cost or because they could not afford it. Health habit measures included smoking status (current, former, never), physical activity, and alcohol intake. Physical activity was categorized as high (vigorous activity 2 times/week or moderate activity 4 times/week), moderate (vigorous activity 1 time/week or moderate activity 1-3 times/week), or low (no vigorous or moderate activity/week) using validated methods.20 Alcohol intake was categorized as abstainer (<12 drinks/lifetime or a former drinker/none currently), light (≤3 drinks/week), moderate (>3 and ≤ 7 drinks/week for women, >3 and ≤ 14 drinks/week for men) or heavy (>7 drinks/week for women and >14 drinks/week for men).21
Statistical Analyses
We used bivariable analyses to compare adults with and without migraines/severe headaches. We estimated the prevalence of CAM use, reasons for and disclosure of use to health care providers, and the prevalence of using CAM therapies to specifically treat migraines/severe headaches. We performed multivariable logistic regression to determine whether differences in CAM use persisted between adults with and without severe headaches/migraines after adjusting for sociodemographic characteristics, illness burden, access to care, and health habits. We used a stepwise backward elimination process that considered factors associated with CAM use with a p-value <0.15 in bivariable analyses and those found to be important in previous studies.17, 18 Factors with a Wald statistic p-value of ≤ 0.05 and conditions that were considered a priori and have been shown to be important in the literature were retained in the final model.17, 18 We considered potential confounding by examining a 10% change in the estimated β-coefficient for factors that did not meet these criteria. Next, we used logistic regression (as described above) to identify independent correlates of CAM use in adults with migraines/severe headaches adjusting for sociodemographic characteristics, illness burden, access to care, and health habits. Prevalence estimates were computed after excluding missing data; no individual variable had missing data more than 4%. Multivariable models included respondents with complete data on all covariates. SAS-callable SUDAAN version 10.1 (Research Triangle Park, NC) was used to account for the complex sampling design and analyses were weighted to reflect national estimates.15 The study was approved for exemption by our institutional review board based on 45 CFR 46.101(b) (4) because of de-identified data.
Results
Sample Characteristics
Overall, 2,886 adults (12.3%), an estimated 27.4 million U.S. adults, reported a history of migraine/severe headache within 3 months. Table 1 shows that compared to adults without migraines/severe headaches, those with migraines/severe headaches were significantly more likely to be women, younger, have lower family incomes, perceive their health as fair or poor, have functional limitations, currently smoke, visit the ER in the prior year, report a history of hypertension, hyperlipidemia, insomnia, anxiety, depression, and other conditions associated with pain, and report having delayed their care because of worries about cost or because it was not affordable.
Table 1. Characteristics of Adults by Migraines/Severe Headaches Statusa.
| Characteristic | With Migraine/Severe Headache (n=2,886) |
Without Migraine/Severe Headache (n=20,507) |
Chi-square p value |
|---|---|---|---|
| Sociodemographics | |||
| Age (years) | <0.0001 | ||
| 18-24 | 340 (13.1) | 2153 (12.8) | |
| 25-44 | 1351 (46.9) | 7185 (35.5) | |
| 45-64 | 978 (33.9) | 6787 (34.1) | |
| 65-74 | 133 (3.9) | 2279 (9.3) | |
| 75+ | 84 (2.1) | 2078 (8.3) | |
| Sex | <0.0001 | ||
| Male | 738 (29.1) | 9624 (51.0) | |
| Female | 2148 (70.9) | 10,858 (49.1) | |
| Race/Ethnicity | <0.01 | ||
| Non-Hispanic White | 1714 (69.9) | 12,183 (68.5) | |
| Non-Hispanic Black | 448 (10.7) | 3172 (11.6) | |
| Hispanic | 529 (12.7) | 3665 (13.5) | |
| Asian | 110 (3.6) | 1097 (4.6) | |
| Other | 85 (3.1) | 365 (1.8) | |
| Education | <0.05 | ||
| < High School | 544 (16.1) | 3677 (15.4) | |
| High School | 787 (28.7) | 5732 (28.6) | |
| >High School | 1537 (54.6) | 10,837 (54.9) | |
| Imputed Family Income ($) | <0.0001 | ||
| 0-19,999 | 867 (22.6) | 4858 (16.6) | |
| 20-34,999 | 597 (19.9) | 3910 (16.8) | |
| 35-64,999 | 704 (25.9) | 5455 (27.8) | |
| ≥65,000 | 717 (31.6) | 6259 (38.8) | |
| Illness Burden | |||
| History of Medical Conditions | |||
| Hypertension | 898 (29.4) | 5945 (26.8) | 0.0500 |
| Hyperlipidemia | 8011 (26.9) | 5001 (24.0) | <0.01 |
| Neck Pain | 1051 (36.1) | 2053 (9.8) | <0.0001 |
| Arthritis | 869 (30.1) | 4225 (19.5) | <0.0001 |
| Joint Pain | 1345 (45.5) | 5220 (25.1) | <0.0001 |
| Low Back Pain | 1550 (52.3) | 4515 (21.9) | <0.0001 |
| Anxiety | 891 (30.6) | 1707 (8.1) | <0.0001 |
Data are reported as samples sizes (weighted %). Percentages were weighted to reflect national estimates. Variables with missing data are: education (n=260); hypertension (n=27); hyperlipidemia (n=102); neck pain (n=25); insomnia (n=35); arthritis (n=47); joint pain (n=29); low back pain (n=27); depression (n=50); anxiety (n=46). Other variables of interest are published online, see Supplementary Table File 1.
Prevalence of CAM Use
Overall, 49.5% of U.S. adults with migraines/severe headaches reported using at least one CAM therapy within the prior 12 months, representing an estimated 13.5 million adults, compared to 33.9% without migraines/severe headaches (p<0.0001) (Table 2). Adults with migraines/severe headaches remained more likely to use CAM than those without these conditions (adjusted odds ratio=1.29, 95% confidence interval [1.15, 1.45]), after adjusting for age, sex, race/ethnicity, birthplace, imputed family income, educational attainment, insurance status, perceived health status, hyperlipidemia, diabetes, other pain syndromes, anxiety, smoking status, alcohol intake, physical activity level, number of ER visits in prior year, and delayed care because of worries about cost.
Table 2. Prevalence of Complementary and Alternative Medicine (CAM) Therapiesa Use in the Previous 12 Months.
| Modality | With Migraine/Severe Headache (n=2,886) |
Without Migraine/Severe Headache (n=20,507) |
Chi-square p-value |
|---|---|---|---|
| Any CAM Use | 1400 (49.5) | 6765 (33.9) | <0.0001 |
| Mind-Body Therapies | 858 (30.2) | 3506 (17.2) | <0.0001 |
| Deep Breathing Exercises | 630 (23.9) | 2286 (11.7) | <0.0001 |
| Meditation | 446 (16.8) | 1708 (8.8) | <0.0001 |
| Yoga | 229 (9.2) | 1113 (5.9) | <0.0001 |
| Progressive Relaxation | 142 (5.6) | 502 (2.7) | <0.0001 |
| Guided Imagery | 106 (4.2) | 375 (2.0) | <0.0001 |
| Biologically Based Therapies | 661 (23.7) | 3323 (16.6) | <0.0001 |
| Herbal/other supplementsb | 661 (26.7) | 3320 (18.4) | <0.0001 |
| Manipulation Based Therapies | 584 (20.6) | 2556 (13.2) | <0.0001 |
| Chiropractic | 339 (15.4) | 1514 (9.5) | <0.0001 |
| Massage | 371 (15.1) | 1459 (8.3) | <0.0001 |
| Alternative Medical Systems | 148 (5.2) | 579 (2.8) | <0.0001 |
| Homeopathy | 86 (3.4) | 308 (1.6) | <0.0001 |
| Acupuncture | 67 (2.4) | 276 (1.4) | 0.0016 |
Data are reported as samples sizes (weighted %). Percentages were weighted to reflect national estimates.
Does not include common vitamins and minerals.
Estimates not presented because n<50: Ayuveda, naturopathy, chelation, Feldenkrais, Alexander, Biofeedback, Hypnosis, Qi gong, tai chi, energy healing.
CAM=Complementary and Alternative Medicine.
Among adults with migraines/severe headaches, mind-body therapies were used most frequently, followed by biologically-based therapies; use of alternative medical systems were least common (Table 2). Deep breathing exercises and meditation were the individual mind-body therapies used most commonly; herbal/other supplements were the main biologically-based therapy used; chiropractic care and massage were the main types of manipulation therapies used; and homeopathy and acupuncture were the main types of alternative medical systems used. Of note, biofeedback was reported by only 5 survey respondents with migraines/severe headaches. While a large percentage (26.7%) of adults with migraines/severe headaches reported use of herbal/other supplements, usage was split across 44 different supplements. Coenzyme Q10 (CoQ10) was used similarly between those with and without migraines/severe headaches (1.4 vs. 1.3%, respectively) and feverfew was used by only 20 survey respondents, thus precluding further analyses.
Reasons for and Disclosure of CAM Use
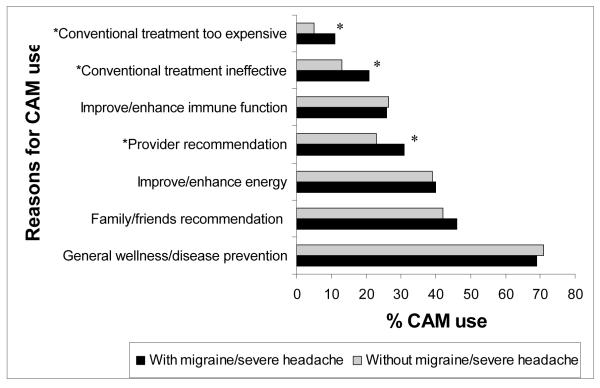
Among adults with migraines/severe headaches, when asked, “for what health problems or conditions did you use [CAM therapy]?” only 131 respondents (4.5%) reported using a CAM therapy to specifically treat their severe headaches/migraines. The top five health problems cited for use of CAM were back pain, neck pain, anxiety, arthritis, and joint pain. Other than the use for migraines/severe headaches, these top five were the same among adults with and without migraines/severe headaches. In a separate question, for both adults with migraines/severe headaches and those without, the main reasons reported for CAM use were: general wellness/disease prevention, family/friends recommendation, and to improve/enhance energy (Figure 1). Adults with migraines/severe headaches used CAM more often than those without because their provider recommended it (31.3 vs. 23.3%), conventional treatment was ineffective (21.0 vs. 12.8%), and conventional treatment was too expensive (11.1 vs. 5.2%) (p<0.0001 for all comparisons) (Figure 1). Overall, only 43% of all CAM users discussed their CAM use with their health care provider. Adults with migraines/severe headaches had a somewhat higher discloser rate than those without (47 vs. 42%, p<0.0001).
Figure 1. Reasons for Complementary and Alternative Medicine (CAM) use among adults with and without migraines/severe headaches.
*p<0.0001 by Chi-square analysis.
Correlates of CAM Use among Adults with Migraines/Severe Headaches
Independent correlates of higher CAM use among adults with migraines/severe headaches included higher educational attainment, a history of anxiety, joint or low back pain, light or heavy alcohol use, and living in the Western U.S. (Table 3). Factors independently associated with a lower likelihood of CAM use included being male, non-Hispanic Black or Hispanic, being foreign born, having Medicaid, a history of hypertension, or low physical activity.
Table 3. Independent Correlates of CAM Use among Adults with Migraines/Severe Headaches (n=2,707a).
| Factors | Adjustedb Odds Ratio | 95% Confidence Interval |
|---|---|---|
| Sex | ||
| Male | 0.67 | [0.53, 0.85] |
| Female | 1.00 (reference) | |
| Race/Ethnicity | ||
| Non-Hispanic White | 1.00 (reference) | |
| Non-Hispanic Black | 0.51 | [0.38, 0.68] |
| Hispanic | 0.60 | [0.44, 0.83] |
| Asian | 1.01 | [0.59, 1.73] |
| Other | 1.57 | [0.73, 3.34] |
| Education | ||
| <High School | 1.00 (reference) | |
| High School | 1.42 | [1.04, 1.92] |
| >High school | 2.09 | [1.56, 2.80] |
| Region of Residence | ||
| South | 1.00 (reference) | |
| Northeast | 1.08 | [0.83, 1.40] |
| Midwest | 1.33 | [0.99, 1.78] |
| West | 1.63 | [1.24, 2.14] |
| Being Foreign Born | 0.60 | [0.42, 0.86] |
| Anxiety | 1.61 | [1.27, 2.04] |
| Hypertension | 0.77 | [0.61, 0.97] |
| Joint Pain | 1.67 | [1.37, 2.05] |
| Low Back Pain | 1.33 | [1.06, 1.66] |
| Insurance | ||
| Private | 1.00 (reference) | |
| Uninsured | 0.97 | [0.73, 1.28] |
| Medicare | 0.90 | [0.54, 1.47] |
| Medicaid | 0.58 | [0.38, 0.88] |
| Other | 1.33 | [0.94, 1.87] |
| Physical Activity Level | ||
| Low | 0.44 | [0.35, 0.55] |
| Moderate | 0.78 | [0.59, 1.04] |
| High | 1.00 (reference) | |
| Alcohol Intake | ||
| Abstainers | 1.00 (reference) | |
| Light | 1.32 | [1.05, 1.66] |
| Moderate | 1.16 | [0.76, 1.75] |
| Heavy | 1.83 | [1.05, 3.19] |
Model was based on observations with complete data; 179 observations were excluded becai missing data on one or more covariates.
Adjusted for sociodemographic characteristics, illness burden, access to care, and health habits.
CAM = complementary and alternative medicine.
Discussion
Nearly one out of two U.S. adults with migraines/severe headaches use CAM, a substantially higher rate than that observed among adults without these conditions. Mind-body therapies (e.g. deep breathing exercises, meditation, and yoga), are used most frequently, whereas alternative medical systems (i.e. homeopathy and acupuncture) are used the least. Despite frequent CAM use, less than five percent of respondents reported using CAM as a treatment specifically for migraines/severe headaches. Besides their treatment of migraines/severe headaches, adults with migraines/severe headaches used CAM most commonly to treat back pain, neck pain, anxiety, arthritis, and joint pain. Adults with migraines/severe headaches are more likely than those without to report using CAM because their provider recommended it or because they perceived conventional treatments as ineffective or too expensive. More than 50% of adults with migraines/severe headaches did not discuss CAM use with their health care provider. Significant correlates of CAM use among adults with migraines/severe headaches include a history of anxiety, joint or low back pain, alcohol use, higher education, and residing in the Western U.S.
The prevalence of migraine in NHIS is consistent with previous reported national estimates.1 The unadjusted prevalence of CAM use among adults with migraines/severe headaches in this survey (49.5%) also falls within the wide range of published rates (29-84%) for adults with headaches/migraines.5, 9-11, 13, 14 Most previous studies have examined the lifetime prevalence of CAM use and not prevalence in the past year. Of the few prior surveys that reported both the lifetime and last-year prevalence,5, 10 the prevalence of use in the previous year was notably lower than lifetime CAM use (31 vs. 17% and 29 vs. 10%, respectively). Thus, our findings that about 1 out of 2 adults with migraines/severe headaches have used CAM in the previous year reflect a substantially higher prevalence than those reported previously. Furthermore, use of specific therapies differed from previous findings, i.e. prior surveys examining CAM use showed acupuncture and homeopathy to be the most commonly used therapies among adults with headaches.5, 12 The variation in prevalence estimates is likely due to methodological differences including different definitions of CAM use, different study locations (e.g., specialty headache clinics vs. general population; countries22) and in different types and severities of headaches examined. However, beyond these methodological differences, the prevalence of CAM use in adults with migraines/severe headaches is higher than that found in similar analyses among the general population (38%),23 overweight/obese adults (36%)24, or adults with cardiovascular disease (36%).18 Furthermore, our findings in adults with migraines/severe headaches are similar to those previously reported among adults with other common neurological conditions, although the overall prevalence of CAM use is higher among adults with migraines/severe headaches.8 The higher CAM use found among adults with migraines/severe headaches compared to other populations likely represents a multitude of different factors, such as the significant disease burden, the lack of 100% effective conventional treatments, and the perceived benefit of CAM therapies for migraine/severe headache sufferers. Similar to other studies, we found that CAM use was higher among women and those with higher education and incomes. 8, 17, 18
While our findings demonstrate CAM use is high among adults with migraines/severe headaches, few adults reported using CAM to specifically treat migraines/severe headaches. This finding conflicts with prior surveys showing rates of 29-84% of CAM use for the specific treatment of headaches/migraines.5, 9-11 However, most of these estimates are based on patients seen in dedicated headache centers, where more patients have severe headaches; those with more severe headaches are more likely to seek out CAM therapies.5 Additionally, in the U.S., patients may view their use of CAM as holistic rather than for the specific treatment of a medical condition. Our findings show that individuals with migraines/severe headaches cited the main reason for CAM use as general wellness/disease prevention. For example, stress is a well-known trigger for headaches,25 and pharmacological treatments often do not address stress. Thus patients with migraines may seek non-pharmacological treatments for stress-reduction and relaxation to improve their general health.11, 26 Furthermore, the most frequently used CAM therapies (deep breathing exercises, meditation, herbal/other supplements) are both self-administered and low-cost treatment options. The most common therapies used by adults with migraines/severe headaches are similar to those reported in the general population23 and in other select populations.8, 18, 24
While CAM use among adults with migraines/severe headaches is popular, evidence to support its use for migraines is limited, except for mind-body medicine, which has the strongest evidence.27 Furthermore, relaxation therapies and biofeedback are recommended by the U.S. Headache Consortium Guidelines for the treatment of migraines.28 Evidence for the guidelines is based on the Agency for Health Care Policy and Research Technical Review, which evaluated the evidence for behavioral and physical treatments for migraine and found relaxation training (progressive muscle relaxation, autogenic training, meditation or passive relaxation), EMG biofeedback, and thermal biofeedback combined with relaxation training to have high quality (Grade A) evidence from well-performed research studies for the prevention of migraine.29
There is a discrepancy between reported CAM use and evidence-based CAM therapies. For example, the number of NHIS respondents with migraines/severe headaches who reported using biofeedback was insufficient to compute a reliable estimate, despite the strong evidence to support the use of biofeedback for migraine. Likewise, although a recent Cochrane review of acupuncture for migraine prophylaxis concluded that migraine patients may benefit from acupuncture,30 we found only 2.4% of adults with migraines/severe headaches reported using acupuncture. While there is some evidence for the use of CoQ10, 31 feverfew, 32 and butterbur, 33 very few adults in this survey reported use of CoQ10 or feverfew; use of butterbur extract (Petasites hybridus root) was not queried. Conversely, use of massage was reported in 15.1% of adults with migraines/severe headaches, and while a survey has shown that massage is perceived to be one of the most efficacious CAM treatments for migraines,5 controlled trials evaluating the efficacy of massage for migraine are lacking.
Reasons for the discrepancies between what CAM therapies patients are using and the evidence to support their use for migraines remain unclear, and may represent factors at the patient, practitioner, and systems level. For example, the underuse of biofeedback may relate to a lack of guideline dissemination to practitioners, the limited availability of biofeedback, or the high level of patient participation and commitment required for its success. Furthermore, the notable use of massage among adults with migraines without scientific evidence of its efficacy is important to recognize. This may reflect either a therapy that patients find beneficial that has not yet been studied rigorously, or a possible therapy that may provide benefits that are not otherwise addressed in headache management. Recognizing these discrepancies is important and may help guide physician discussions with patients as well as identify areas in need of future research.
Another important finding is that most adults with migraines/severe headaches do not discuss their use of CAM with their providers. Clinicians should make an effort to ask patients about their CAM use, considering many adults with migraines/severe headaches use CAM because they feel conventional treatments are ineffective or too expensive (over 30%) and thus may be non-adherent to conventional interventions. Furthermore, clinicians should be aware of all treatments that their patients use. Many patients use CAM because it is congruous with their values and beliefs about health and life,34 and addressing patients’ underlying goals and beliefs about their health may improve patient-doctor communication and ultimately patient care. Further, providers can counsel their patients on the evidence for CAM therapies for migraines, address potential options that may aid in the successful treatment of migraines, and monitor for side effects. Finally, the risks of CAM therapies in migraine patients need to be addressed. For example, patients need to be made aware of herb-drug interactions, and this can only occur if physicians query patients about their use of herbs and supplements. St. John’s wort (Hypericum perforatum), an herb commonly used to treat depression, increases serotonin levels and may increase the risk of serotonin syndrome when taken concurrently with triptans.35 The US Food and Drug Administration (FDA) alerted providers in 2006 regarding the risk of serotonin syndrome when triptans are combined with serotonergic agents.36
As a cross-sectional study, NHIS is limited in that it relies on self-reporting, and is susceptible to misclassification bias and ability to recall. Because both migraines and severe headaches are asked in a single survey item in NHIS, our analyses cannot discern the two conditions. Our analyses may underestimate the prevalence of adults with migraines/severe headaches, as well as adults using CAM for migraine treatment, as participants were asked to report on migraines/severe headaches experienced in the prior 3 months. We may also underestimate the prevalence of CAM use in the U.S. as not all CAM therapies are captured by NHIS. Moreover, respondents may have different interpretations of CAM therapies asked about in NHIS, such as deep breathing exercises. It is surprising that nearly 50% of adults with headaches use CAM, and yet so few attribute their CAM use to headaches. This may be due to limitations of the survey query process. It is also unclear how migraine/severe headache sufferers interpret this question. It is possible that they attribute their CAM use to another co-morbid condition that may also be related to their headaches (e.g. anxiety). Despite these inherent limitations, our findings are the most recent data available on CAM use in adults with migraines/severe headaches in a nationally-representative sample that is generalizable to the U.S. adult population.
In summary, CAM use is significantly more common in U.S. adults with migraines/severe headaches than those without, though few report use of CAM to treat migraines/severe headaches. Mind-body therapies are the most frequently used CAM therapy in adults with migraines/severe headaches. Given the high prevalence of use of CAM therapies in adults with migraines/severe headaches and the suggestive preliminary data, definitive randomized controlled trials are needed to understand the potential therapeutic benefits, mechanisms, side effects, and risks of CAM therapies in adults with migraines/severe headaches.
Supplementary Material
Acknowledgments
Study Funding
Dr. Wells was supported by an institutional National Research Service Award Number T32AT000051 from the National Center for Complementary & Alternative Medicine (NCCAM) at the National Institutes of Health. Dr. Bertisch was supported by K23 AT005104-02 from NCCAM. Dr. Buettner was supported by K23 AR055664 from NIAMS. Dr. Phillips was supported by a Mid-Career Investigator Award K24AT000589 and Dr. McCarthy was supported by R03AT002236, also from NCCAM. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Complementary & Alternative Medicine or the National Institutes of Health.
Abbreviations
- U.S
United States
- CAM
Complementary and alternative medicine
- NHIS
National Health Interview Survey
- ER
Emergency room
- CoQ10
Coenzyme Q10
Footnotes
Conflicts of interests:
Dr. Wells reports no conflicts of interest.
Dr. Bertisch reports no conflicts of interest.
Dr. Buettner reports speaking at Harvard Medical School CME and hospital affiliated programs focused on guiding health care providers on judging the evidence on, and assessing the risks and benefits of, herbs and dietary supplements in clinical practice. She has received honorarium for some of these programs (total <$500/year).
Dr. Phillips reports no conflicts of interest.
Dr. McCarthy reports no conflicts of interest.
Contributor Information
Rebecca Erwin Wells, Department of Neurology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, 330 Brookline Avenue, Boston, MA 02215 USA, rwells@bidmc.harvard.edu, (617) 432-1593 (phone), (617) 432-1616 (fax).
Suzanne M. Bertisch, Division of General Medicine and Primary Care, Department of Medicine, Beth Israel Deaconess, Medical Center, Harvard Medical School, Boston, MA, 330 Brookline Ave, CO-1309, Boston, MA 02215 USA, sbertisc@caregroup.harvard.edu.
Catherine Buettner, Division of General Medicine and Primary Care, Department of Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, 330 Brookline Ave, Atrium Suite, Shapiro 1, Boston, MA 02215 USA, cbuettne@bidmc.harvard.edu.
Russell S. Phillips, Division of General Medicine and Primary Care, Department of Medicine, Beth Israel Deaconess, Medical Center, Harvard Medical School, Boston, MA, 330 Brookline Ave, E/Yamins 111C, Boston, MA 02215 USA, rphillip@bidmc.harvard.edu.
Ellen P. McCarthy, Division of General Medicine and Primary Care, Department of Medicine, Beth Israel Deaconess, Medical Center, Harvard Medical School, Boston, MA, 330 Brookline Ave, CO-1309, Brookline, MA 02215 USA, emccarth@bidmc.harvard.edu.
References
- 1.Victor TW, Hu X, Campbell JC, Buse DC, Lipton RB. Migraine prevalence by age and sex in the United States: a life-span study. Cephalalgia. 2010;30:1065–1072. doi: 10.1177/0333102409355601. [DOI] [PubMed] [Google Scholar]
- 2.Stovner LJ, Hagen K. Prevalence, burden, and cost of headache disorders. Curr Opin Neurol. 2006;19:281–285. doi: 10.1097/01.wco.0000227039.16071.92. [DOI] [PubMed] [Google Scholar]
- 3.Leonardi M, Raggi A, Bussone G, D’Amico D. Health-related quality of life, disability and severity of disease in patients with migraine attending to a specialty headache center. Headache. 2010;50:1576–1586. doi: 10.1111/j.1526-4610.2010.01770.x. [DOI] [PubMed] [Google Scholar]
- 4.Hawkins K, Wang S, Rupnow M. Direct cost burden among insured US employees with migraine. Headache. 2008;48:553–563. doi: 10.1111/j.1526-4610.2007.00990.x. [DOI] [PubMed] [Google Scholar]
- 5.Rossi P, Di Lorenzo G, Malpezzi MG, et al. Prevalence, pattern and predictors of use of complementary and alternative medicine (CAM) in migraine patients attending a headache clinic in Italy. Cephalalgia. 2005;25:493–506. doi: 10.1111/j.1468-2982.2005.00898.x. [DOI] [PubMed] [Google Scholar]
- 6.Barnes PM, Powell-Griner E, McFann K, Nahin RL. Complementary and alternative medicine use among adults: United States, 2002. Adv Data. 2004:1–19. [PubMed] [Google Scholar]
- 7.Eisenberg DM, Kessler RC, Van Rompay MI, et al. Perceptions about complementary therapies relative to conventional therapies among adults who use both: results from a national survey. Ann Intern Med. 2001;135:344–351. doi: 10.7326/0003-4819-135-5-200109040-00011. [DOI] [PubMed] [Google Scholar]
- 8.Wells RE, Phillips RS, Schachter SC, McCarthy EP. Complementary and alternative medicine use among US adults with common neurological conditions. J Neurol. 2010;257:1822–1831. doi: 10.1007/s00415-010-5616-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gaul C, Eismann R, Schmidt T, et al. Use of complementary and alternative medicine in patients suffering from primary headache disorders. Cephalalgia. 2009;29:1069–1078. doi: 10.1111/j.1468-2982.2009.01841.x. [DOI] [PubMed] [Google Scholar]
- 10.Rossi P, Torelli P, Di Lorenzo C, et al. Use of complementary and alternative medicine by patients with cluster headache: results of a multi-centre headache clinic survey. Complement Ther Med. 2008;16:220–227. doi: 10.1016/j.ctim.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 11.von Peter S, Ting W, Scrivani S, et al. Survey on the use of complementary and alternative medicine among patients with headache syndromes. Cephalalgia. 2002;22:395–400. doi: 10.1046/j.1468-2982.2002.00376.x. [DOI] [PubMed] [Google Scholar]
- 12.Kozak S, Gantenbein AR, Isler H, et al. Nosology and treatment of primary headache in a Swiss headache clinic. J Headache Pain. 2005;6:121–127. doi: 10.1007/s10194-005-0166-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lambert TD, Morrison KE, Edwards J, Clarke CE. The use of complementary and alternative medicine by patients attending a UK headache clinic. Complement Ther Med. 2010;18:128–134. doi: 10.1016/j.ctim.2010.05.035. [DOI] [PubMed] [Google Scholar]
- 14.Rossi P, Di Lorenzo G, Faroni J, Malpezzi MG, Cesarino F, Nappi G. Use of complementary and alternative medicine by patients with chronic tension-type headache: results of a headache clinic survey. Headache. 2006;46:622–631. doi: 10.1111/j.1526-4610.2006.00412.x. [DOI] [PubMed] [Google Scholar]
- 15. [Accessed January 8, 2009];CDC National Center for Health Statistics National Health Interview Survey 2007 Survey Description Document. Available from ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2007/srvydesc.pdf.
- 16.Centers for Disease Control and Prevention’s National Center for Health Statistics. Accessed. Available from http://www.cdc.gov/nchs/nhis.htm.
- 17.Bertisch SM, Wee CC, Phillips RS, McCarthy EP. Alternative mind-body therapies used by adults with medical conditions. J Psychosom Res. 2009;66:511–519. doi: 10.1016/j.jpsychores.2008.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yeh GY, Davis RB, Phillips RS. Use of complementary therapies in patients with cardiovascular disease. Am J Cardiol. 2006;98:673–680. doi: 10.1016/j.amjcard.2006.03.051. [DOI] [PubMed] [Google Scholar]
- 19. [Accessed January 8, 2009];CDC National Center for Health Statistics National Health Interview Survey 2007 Imputed Family Income. Available from http://www.cdc.gov/NCHS/nhis/2007imputedincome.htm.
- 20.Kushi LH, Fee RM, Folsom AR, Mink PJ, Anderson KE, Sellers TA. Physical activity and mortality in postmenopausal women. Jama. 1997;277:1287–1292. [PubMed] [Google Scholar]
- 21. [Accessed July 14, 2009];Health, United States 2007. Available from http://www.cdc.gov/nchs/data/hus/hus07.pdf.
- 22.Fisher P, Ward A. Complementary medicine in Europe. BMJ. 1994;309:107–111. doi: 10.1136/bmj.309.6947.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008:1–23. [PubMed] [Google Scholar]
- 24.Bertisch SM, Wee CC, McCarthy EP. Use of complementary and alternative therapies by overweight and obese adults. Obesity (Silver Spring) 2008;16:1610–1615. doi: 10.1038/oby.2008.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wober C, Wober-Bingol C. Triggers of migraine and tension-type headache. Handb Clin Neurol. 2010;97:161–172. doi: 10.1016/S0072-9752(10)97012-7. [DOI] [PubMed] [Google Scholar]
- 26.Dusek JA, Benson H. Mind-body medicine: a model of the comparative clinical impact of the acute stress and relaxation responses. Minn Med. 2009;92:47–50. [PMC free article] [PubMed] [Google Scholar]
- 27.Wahbeh H, Elsas SM, Oken BS. Mind-body interventions: applications in neurology. Neurology. 2008;70:2321–2328. doi: 10.1212/01.wnl.0000314667.16386.5e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Campbell JK, Penzien DB, Wall EM. [Accessed July 14, 2009];Evidence-based guidelines for migraine headache: behavioral and physical treatments. US Headache Consortium 2000. Available from http://www.aan.com.
- 29.Goslin RE, Gray RN, McCrory DC, Penzien D, Rains J, Hasselblad V. In: Behavioral and Physical Treatments for Migraine Headache. Research AfHCPa, editor. 1999. [PubMed] [Google Scholar]
- 30.Linde K, Allais G, Brinkhaus B, Manheimer E, Vickers A, White AR. Acupuncture for migraine prophylaxis. Cochrane Database Syst Rev. 2009:CD001218. doi: 10.1002/14651858.CD001218.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sandor PS, Di Clemente L, Coppola G, et al. Efficacy of coenzyme Q10 in migraine prophylaxis: a randomized controlled trial. Neurology. 2005;64:713–715. doi: 10.1212/01.WNL.0000151975.03598.ED. [DOI] [PubMed] [Google Scholar]
- 32.Diener HC, Pfaffenrath V, Schnitker J, Friede M, Henneicke-von Zepelin HH. Efficacy and safety of 6.25 mg t.i.d. feverfew CO2-extract (MIG-99) in migraine prevention--a randomized, double-blind, multicentre, placebo-controlled study. Cephalalgia. 2005;25:1031–1041. doi: 10.1111/j.1468-2982.2005.00950.x. [DOI] [PubMed] [Google Scholar]
- 33.Lipton RB, Gobel H, Einhaupl KM, Wilks K, Mauskop A. Petasites hybridus root (butterbur) is an effective preventive treatment for migraine. Neurology. 2004;63:2240–2244. doi: 10.1212/01.wnl.0000147290.68260.11. [DOI] [PubMed] [Google Scholar]
- 34.Astin JA. Why patients use alternative medicine: results of a national study. JAMA. 1998;279:1548–1553. doi: 10.1001/jama.279.19.1548. [DOI] [PubMed] [Google Scholar]
- 35.Bonetto N, Santelli L, Battistin L, Cagnin A. Serotonin syndrome and rhabdomyolysis induced by concomitant use of triptans, fluoxetine and hypericum. Cephalalgia. 2007;27:1421–1423. doi: 10.1111/j.1468-2982.2007.01430.x. [DOI] [PubMed] [Google Scholar]
- 36.Evans RW, Tepper SJ, Shapiro RE, Sun-Edelstein C, Tietjen GE. The FDA alert on serotonin syndrome with use of triptans combined with selective serotonin reuptake inhibitors or selective serotonin-norepinephrine reuptake inhibitors: American Headache Society position paper. Headache. 2010;50:1089–1099. doi: 10.1111/j.1526-4610.2010.01691.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.