Abstract
Objectives
To determine the priorities of low-income urban residents for interventions that address the socio-economic determinants of health.
Methods
We selected and estimated the cost of 16 interventions related to education, housing, nutrition, employment, health care, healthy behavior, neighborhood improvement, and transportation. Low-income residents of Washington, D.C. (N=431) participated in decision exercises to prioritize these interventions.
Results
Given a budget valued at approximately twice an estimated cost of medical and dental care ($885), the interventions ultimately prioritized by the greatest percentage of individuals were: health insurance (95%), housing vouchers (82%) dental care (82%), job training (72%), adult education (63%), counseling (68%), healthy behavior incentives (68%), and job placement (67%). The percentages of respondents who received support for housing, adult education, and job training and placement were far less than the percentage who prioritized these interventions.
Conclusions
Poor and low-income residents’ priorities may usefully inform allocation of social services that affect health.
Keywords: Health status disparity, health promotion, poverty, resource allocation, public participation
The World Health Organization’s Commission on the Social Determinants of Health released its final report in 2008 offering and recommending comprehensive strategies to reduce health inequalities associated with social factors, particularly poverty.1 The Commission suggested that communities that seek to address poverty-related health deficits ought to offer an array of policies that effectively target the numerous dimensions of poverty in local populations in a coordinated manner.2–4 The need to address the social determinants of health in the United States has been most prominently highlighted by the Robert Wood Johnson Foundation’s Commission to Build a Healthier America.5 The Commission recognized that health care alone does not make the U.S. population uniformly healthy. Poor men and women have a life expectancy that is seven years shorter than that of high-income groups.5
In one of the first efforts to translate an understanding of the importance of the socioeconomic determinants of health (SEDH) into policy, the Acheson Commission in the United Kingdom recommended that a number of policy areas be addressed to meet the needs of children and adults, including among others poverty, education, employment, housing, and the environment.6
Subsequently, prominent health policy experts in the U.S. argued for considering how the lessons of the Acheson Report might be translated to the U.S.7 Poverty rates in the U.S. during the past decade have ranged from 11.3% of the population to 13.2%.8 Poverty rates for subgroups, particularly African Americans and Latinos, have been notably higher (25% and 23%, respectively).8 Public programs to address the socioeconomic needs of the poor have not sufficed. Housing policies, for example, designed to address the supply of poverty-level affordable housing have long been unable to keep up with shortfalls in supply.9 Particularly when the economy is weak, the number of low-income individuals who need social services rises. A dramatic illustration of the magnitude of the demand is the number of people needing food assistance, which exceeded 30 million in the U.S. in 2009.10 As need expands, state and federal programs are most likely to face budgetary shortages that require cutting assistance programs.11 Persistent and at times exacerbated shortages in resources to meet the needs of the poor point to the importance of priority-setting.
With this in mind, a research project was conducted to facilitate the prioritization of interventions that address the SEDH for an urban low-income population in the U.S. This study took place in Washington, D.C., where nearly 20% of residents live at or below the poverty level.12 Health disparities between low-income and high-income segments of the population in D.C. are well documented. For example, reports of heart disease are five times higher and of stroke are 10 times higher among participants in the Behavioral Risk Factor Surveillance System who earn less than $15,000 dollars a year than for those who earn $75,000 per year.13 The city provides a stark example of the unmet socioeconomic needs of a low-income population in the U.S. The percentage of households in the District of Columbia facing the burden of unaffordable housing—the need to spend more than 30% of household income on housing—was 37% in 2003.14 In the face of recession, the city adopted cuts in its 2009 fiscal budget that involved reducing several programs for low-income residents including a program to place homeless residents in permanent housing, rent subsidies, first time homebuyer assistance, the Temporary Assistance for Needy Families program, substance abuse treatment, and services to help residents find employment.15
The project reported here focused on estimating the costs of various socioeconomic interventions and engaging low-income residents in an exploratory exercise aimed at prioritizing these interventions. We hypothesized that poor and low-income individuals would vary with regard to the interventions they chose. In particular, we expected that younger individuals would make educational interventions a higher priority given the longer impact it might have on their income-earning capacity.
The study is part of a larger effort to engage the public in priority-setting for health that has been conducted by the Department of Bioethics at the Clinical Center of the National Institutes of Health. While the study was conducted among low-income individuals in Washington, D.C., the priority-setting exercise reported here may be tailored for general use by those interested in optimizing public programs to address SEDH.
Methods
Explanatory framework
The project described here is predicated on the growing understanding that socioeconomic factors are major determinants of health. As stated by the World Health Organization, “The social determinants of health are the circumstances in which people are born, grow up, live, work and age, and the systems put in place to deal with illness. These circumstances are in turn shaped by a wider set of forces: economics, social policies, and politics.”16[p.1] This recognition of the important role that socioeconomic factors play in determining health derives from a large body of research indicating that members of lower-income groups experience poorer health and shorter life expectancy than members of higher-income groups.17 This general finding holds both in comparisons between more and less wealthy countries and comparisons within countries.18 The socioeconomic determinants generally considered to be important include income, employment, education, housing and environment, nutrition, social support, and social inclusion. Furthermore, these factors have been shown to interact in contributing to health status.19 While personal behavior, such as smoking and alcohol consumption, contribute to health, socioeconomic factors are strongly associated with health even after adjusting for these personal behaviors.20 Several mechanisms have been postulated as mediating the influence of these socioeconomic factors on health. Evidence of the biological pathways mediating the influence of socioeconomic factors suggests that stress induced by social circumstances chronically stimulates the hypothalamic-pituitary-adrenal axis, causing persistent adrenal hormones levels that predispose to obesity, diabetes, and cardiovascular disease as well as altered immune modulation.21 Another analytic strategy takes a life-course approach, building on evidence that a person’s social circumstances at each point in time accumulate over a lifetime to contribute to an individual’s health status so that repeated periods of nutritional deficiency and social factors beginning in utero and running through childhood and adult life set up a sequence of poor development at each stage, which leads to physiological damage and premature death in middle age and early old age.22 There is also evidence that social support and social cohesion contribute to health and can affect physical and psychological morbidity as well as mortality. 23
This understanding of the SEDH suggests that efforts to reduce health disparities will require a broad array of combined interventions that focus across the life course. Such combined interventions are likely to entail a combination of community-based as well as individual-based interventions. We use the term community as it is used by the U.S. Dept. of Health and Human Services in framing the goals in Healthy People 2010 and commonly used in the public health literature that refers to community as “a geographic area, a population group (e.g., a racial/ethnic group, members of an association), a school, a workplace, a group of patients served by a clinic, or a faith community.”24[p.2540] Community-based programs and services should be tailored to respond to the identified needs of a given community. The Canadian Standing Senate Committee’s Subcommittee on Population Health provides a remarkable blueprint for a national approach to addressing the SEDH and describes examples of successful community efforts.25 For example, the Stella Burry Community Services program in St. John’s, Newfoundland serves adults with social and emotional problems by providing support and counseling, develops affordable housing for low-income families, and offers training and skills development programs.25 An affiliated social enterprise (Stella’s Circle) started by the Community Service creates jobs and training in the food services industry and offers low-cost meals to members of the community who cannot afford good nutrition.
Evidence of the health impact of programs to address SEDH is far from well-developed because of the long causal pathway between the implementation of programs and any potential impact on population health, as well as the many confounding factors that make the determination of a link difficult.1 However, a growing body of research shows the effects of interventions. While we will not detail evidence for each of the determinants of health, we will mention some of the most notable. For example, studies of housing have shown that availability of affordable housing is associated with freeing up of resources for food and health care;26–28 programs that offer housing improvements are associated with reductions in respiratory, general medical, and mental illness;29 provision of housing and case management to homeless chronically ill adults is associated with reduced use of medical care;30 HIV infected individuals with housing needs who are offered housing assistance were more likely to be alive and have intact immunity.31
The evidence regarding the health effects of nutritional interventions derives from a combination of studies. Food insecurity is associated with poorer diet quality for pregnant women and children, increased obesity in children and adults, and increased atherosclerosis.32 The Pennsylvania Fresh Food Financing Initiative provided a dramatically successful effort to improve access to healthy food in poor neighborhoods that has since been replicated in other cities.33 Improvement in neighborhood conditions (i.e., a decline in concentrated disadvantage) leads to increases in children’s adult earnings for African American children of over $4,000 and increases in adult family income of over $6,000 (health outcomes were not included in this analysis).34 There is far less information about the effects of increases in income on health since a number of opportunities to study the effects of such increases in income on health outcomes have been missed.35
Identification and cost estimation of intervention options
Utilizing this explanatory framework, we identified a set of interventions for study participants to prioritize for inclusion in a package of benefits. Nine categories of interventions, each relating to an important social determinant identified in the Acheson Report,6 were included in our study: education, employment, health care, housing, mobility and transportation, nutrition, community development, health behavior promotion, and direct income subsidization. Our approach assumes that both personal behavior and living and working conditions are significant determinants of health. We also assume that it is best to offer an array of interventions that includes both individual and community interventions, because neither type of intervention alone is likely to be as effective. Teaching an individual about a healthy lifestyle that includes exercise, for example, will not promote a lifestyle change in the absence of a safe neighborhood park or gym. Economies of scale can also be achieved by providing benefits at the community level, especially since disadvantaged individuals are often clustered within specific urban neighborhoods or economically depressed rural communities. The availability of parks and recreational areas or ensuring neighborhood security may increase physical activity for the entire neighborhood.
Specific interventions within each of the categories were selected as appropriate in the U.S. context; these interventions were chosen based on a review of existing government or private sector programs, or were found during the literature review.
For more extensive discussion of the interventions that might generally be useful to reduce health disparities for low-income young adults and that were reviewed in selecting interventions for inclusion in the exercise, see Kotwani.36 One category related to promotion of healthy behavior was included in recognition of the important contribution of health behavior to health status.7 The final list of 16 interventions, as described to study participants, appears in Box 1.
Box 1. SIMPLIFIED BENEFIT DESCRIPTIONS AND MONTHLY COSTS.
| EDUCATION | |
| Adult Education | $82.23 |
| You can get money to finish high school. You can get up to 80% of the cost of college courses or professional courses at a community college. You will keep getting money if you pass your courses. | |
| Childhood Education | $110.65 |
| Your child can go to pre-school or kindergarten. This will help your child to get ready for school. Older children in low-performing schools can go to after-school programs. | |
| English Language and Literacy Training | $35.86 |
| Adults and children who do not speak English at home can learn to speak, read, and write in English. | |
| EMPLOYMENT | |
| Job Training | $27.03 |
| You will receive job training which will help you perform your job better. You will learn skills that may help you keep your job. These new skills may help you move to another job or get promoted. | |
| Job Placement Programs | $46.33 |
| You will receive help to apply for a job. You will learn skills that help you to be a better employee. | |
| Day Care for Working Parents | $58.16 |
| Your child can get free or low cost day-care if your child is younger than 13. Teenagers can go to after school programs until they are 16. Your children can also go to summer school. | |
| HEALTH AND DENTAL CARE | |
| Health Insurance | $413.00 |
| This health insurance package will cover the cost of medical care and medicines. | |
| Dental Care | $29.00 |
| This insurance plan will pay for routine dental care. | |
| Counseling Programs | $14.00 |
| You can get counseling for drug, alcohol, anger, stress, and gambling problems. Mentors for young people will help them stay in school. The mentors will help kids to stay away from drugs, crime, and unsafe sex. | |
| HOUSING | |
| Vouchers for Paying Rent and Mortgage | $77.00 |
| You will get vouchers to pay for rent or your mortgage. You may also get some money to help you buy a house or repair your home. | |
| TRANSPORTATION | |
| You will get a voucher to pay for traveling to work on public buses or trains. | $46.00 |
| NUTRITION | |
| More Grocery Store Locations | $9.00 |
| There will be more grocery stores near your home so you can buy healthy food. | |
| Food Stamps and Extra Nutrition for Women, Infants, and Children | $244.00 |
| Low income families will get electronic cards. They can use these cards to buy healthy food at some grocery stores. Poor women, babies, and children younger than five will get healthy foods. They will also learn about healthy eating and receive health care. | |
| School Meals | $28.00 |
| Your school age children will receive free or cheaper breakfast and lunch at school. | |
| NEIGHBORHOOD IMPROVEMENT | |
| Parks, bike trails, and play areas will be built near your home. Kids and adults can exercise safely in these areas. | |
| HEALTHY BEHAVIOR | |
| You enroll in programs that help you to be healthy. These programs will help you lose weight, reduce your blood pressure, or quit smoking. You will get to choose other benefits or get money for staying in these programs. | $26.00 |
| INCOME SUPPLEMENT | |
| Taxed cash supplement | Variable |
Estimates of per capita costs for the interventions included in the study were developed by researching existing programs that offered similar interventions. The report of the methods and assumptions used in this process are available online or from the authors upon request.37 Costs reported in the literature for a given year were adjusted to give an estimate appropriate for 2007.
Per capita costs for each intervention were converted to per member costs by multiplying the percentage of eligible households, the estimated number of members per household, and the percentage rate of utilization for the intervention. The resulting estimates of the monthly per member costs of the benefit options ranged from $413 for health insurance to $9 each for incentives to promote local grocery stores and neighborhood improvement (see Box 1 for more detail).
Population studied
Residents of Washington, D.C., between the ages of 18 and 65, with a personal income at or below 200% of the federal poverty threshold, or a household income at or below 200% of the federal poverty threshold for 2006 were eligible for the study.38
Sample size
A study sample size of 428 was calculated to achieve 90% power to test the hypothesis that younger participants would be more likely than older participants to select educational interventions. This hypothesis was considered plausible based on a previous study of low-income earners.39
Recruitment
Participants were recruited through English and Spanish newspaper advertisements, and flyers displayed at local businesses and doctors’ offices participating in the Howard University Practice Based Research Network. Individuals who expressed interest in participating in the study were screened for income, age, willingness to participate, and D.C. residency by a study investigator or research assistant via telephone interview. A recruiter familiar to the Latino community facilitated recruitment of Latino participants to reduce the likelihood that fears about immigration status might deter enrollment.
Human participant protection
The study was approved by the Institutional Review Boards of the National Institute for Child Health and Development at the National Institutes of Health, Howard University, and the Washington, D.C. Dept. of Health. Signed informed consent was obtained by the exercise facilitator at the outset of each group session.
Study location
English language groups (n=31) met in the Dept. of Family and Community Medicine at Howard University College of Medicine; Spanish language groups (n=12) met at two federally qualified health centers in Washington, D.C. Groups ranged in size from five to 14 people. Prior to consent, participants were assured that data collection was anonymous. After the exercises, the participants received $75.
Study instrument
To ascertain participants’ priorities, we used a paper version of the Reaching Economic Alternatives that Contribute to Health (REACH) exercise, a decision tool designed to facilitate public engagement in prioritization of socioeconomic interventions (available on request).39 This exercise is based on an earlier well-validated decision exercise called Choosing Healthplans All Together (CHAT) (more information about the exercise is available at the CHAT website, http://www.chat-health.org/chat/index2.html).40,41
The exercise was introduced with the following explanation:
Around the world public health experts have learned that people with low incomes are likely to be less healthy than people with high incomes. There are lots of reasons for this. People with low incomes often have less education. They don’t earn as much money to spend on medical care and other things they need to keep them healthy. They live in neighborhoods and houses that are less safe. The project you are participating in today was created to address this problem. Several governments are developing programs to improve the health of people with low incomes. They offer programs that help people to improve their lives and their health. But these programs are very expensive and it will be hard for any government to offer all the programs that might possibly be helpful. Today we will ask you to imagine that your city is planning programs to improve the health of low income residents. Today you get a chance to tell us which programs would be most helpful to you. You get to say which programs you would recommend for the city. We have given you an information booklet to help you learn how programs can affect your health. We hope you will use this information as you make your choices. We know, for example, that eating a healthy diet is good for your health. So if the city offered to make sure that good grocery stores were available in your neighborhood, it might be good for your health. If the city offered you safe parks where you could exercise, it might be good for your health. If the city offered to pay for school for you to learn a new skill you might be able to get a higher paying job. This might be good for your health. Perhaps this is because you would be under less financial stress. Feel free to choose benefits as you wish. We hope that the information about health will help you make your decisions. As you get a chance to pick programs today, we hope to learn from you what matters to you most.
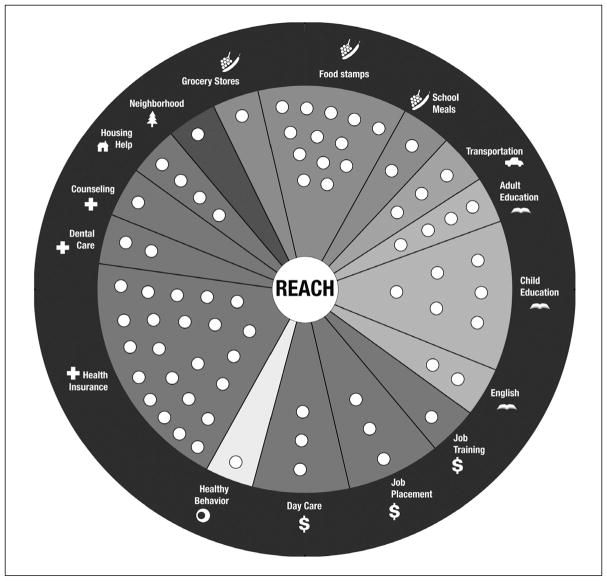
During the exercise, participants were given 50 stickers to use in picking their benefit package. The monetary value assigned to these 50 stickers was $885, which was determined as follows. The Medicaid benefit for enrollees who are under 65 and not institutionalized, disabled, or dually eligible for Medicare and Medicaid was estimated to cost approximately $442. This dollar amount was doubled so that participants could hypothetically afford to include in their package both the Medicaid health coverage and socioeconomic interventions equivalent in value to their health insurance dollar amount, to explore how an individual might spend an amount equivalent to traditional health care costs to offset SEDH. Since the 50 stickers represented $885, each sticker had a value of approximately $18. Participants chose preferred interventions by placing stickers on a pie-shaped exercise board that displayed intervention options (Figure 1).
Figure 1.
The REACH board showing intervention options to be chosen.
The relative cost for each intervention was rounded to the nearest $18 increment so that interventions could be selected by covering spots in the intervention wedge with stickers. As the 16 interventions were estimated to have a total value of $1,256/month, there were 70 spots distributed among the interventions on the exercise board. All the spots within the wedge had to be covered in order to select an intervention. The 50 allotted stickers allowed for coverage of approximately 70% of the available interventions in the exercise. The participants were asked to spend the 50 allotted stickers on those interventions that seemed to have the most impact on health. Participants could also forgo assigning any number of stickers to interventions and receive a hypothetical, taxable income subsidy instead.
Along with the oral introduction of the exercise, participants were given an information booklet explaining in lay terms the description and health impact of the various interventions written in English and Spanish at the 6th grade reading level (as determined by the Flesch-Kincaid grade level of the text). Individuals who could not read study materials were given individual assistance in reading and completion of the exercise.
Participants were instructed to make choices four times in the course of the exercise: first, individually, in order to design a benefit package for themselves and their immediate family; second, in groups of three, to make benefits for a neighborhood; third, as an entire group, through a facilitated discussion, to design program benefits for the entire city; and finally in a fourth round, individually for themselves and their families, to record any change in choices during the course of the exercise. When making selections, they were instructed that they were creating a hypothetical set of benefits that they would consider to be the best, without taking into account any actual benefits they might be receiving. Between rounds of decision-making, participants read aloud and discussed randomly assigned life-event cards. Each life-event card describes a scenario along with possible outcomes as a consequence of choosing or forgoing an intervention. The life-event cards fostered informed and prudent decision-making by clarifying how access to a particular intervention may affect their health. During the group exercise, participants took turns nominating choices. The group discussed each recommended choice, and selected by consensus, or in the absence of consensus, by vote. Qualitative analysis of group discussions will be reported elsewhere.
Questionnaire items were administered prior to the exercise to ascertain socio-demographic characteristics, health characteristics, and use of public support for housing, food, post-high school education, job training, job search, daycare, transportation, and income tax credit. After the exercise, questionnaire items ascertained participant agreement with statements about the REACH exercise to determine how easy, informative, and understandable it was and how acceptable the deliberative process during the exercise was.
Statistical analysis
Analyses were performed using the statistical package Stata version 10 (StataCorp. 2007. Stata Statistical Software: Release 10. College Station, TX: StataCorp LP). Participant characteristics were analyzed using descriptive statistics. Each intervention choice was treated as a dichotomous outcome (i.e., the intervention was or was not selected). Associations between participant characteristics and individual choices during the initial and final rounds were examined in bivariate analyses using the Pearson χ2 test. Results were calculated as the percentage of participants choosing each benefit overall and then by individual characteristic. Choices from the second round were not analyzed since this round is conducted simply to improve decision-making skills. Group choices from the third round were summarized using descriptive statistics. Changes in the percentage of individuals choosing each type of intervention between the initial and final rounds were evaluated using McNemar’s χ2 test. Finally, we used logistic regression to examine whether the bivariate results regarding individual intervention choices for the final round remained statistically significant after adjustment for other variables. Separate models were estimated for each of these outcomes. Variables were removed from a model if they were no longer statistically significant based on likelihood ratio tests. Some non-significant variables were retained in a model if dropping them substantively changed the beta estimates for the remaining variables. Results from each final reduced model were reported as adjusted percents rather than odds ratios since the outcomes were common and odds ratios would have over-estimated the size of the effect. Because these models were based on the final round after the group choices, all p-values were corrected for any intra-class correlation due to a group effect. For any analyses involving multiple comparisons, we considered p<.01 significant. Otherwise, we considered p<.05 significant. For those categories for which information had been collected about received services, we examined the association between receipt of services and prioritization for inclusion in a package of benefits in the final round of the exercise. Frequency of agreement with evaluation statements regarding the exercise was examined using descriptive statistics.
Results
Participant characteristics
A total of 431 individuals participated in the study between January and May 2008; 66% participated in English language group exercises and 34% participated in Spanish language group exercises. The mean age of participants was 45 years (Table 1). Approximately 61% of participants were female, 38% were male, and four individuals reported bisexual identity or did not specify their gender. The vast majority were either African American (57%) or Latino (34%). The majority of participants either had not completed high school (27%), or had completed high school without additional education (35%). Ten percent of participants had no health insurance; the remainder had municipal, federal, or private sources of insurance.
Table 1.
SOCIO-DEMOGRAPHIC CHARACTERISTICS OF STUDY PARTICIPANTS (N = 431)
| Characteristic | N | Mean (SD) or Percent |
|---|---|---|
| Age in years | 427a | 45.1 (11.6) |
| Gender | ||
| Male | 165 | 38.3 |
| Female | 262 | 60.4 |
| Race/Ethnicity | ||
| White (non-Latino) | 7 | 1.6 |
| Black (non-Latino) | 246 | 57.1 |
| Latino | 148 | 34.3 |
| American Indian/Native Alaskan | 7 | 1.6 |
| Asian | 1 | 0.2 |
| Native Hawaiian/Pacific Islander | 1 | 0.2 |
| Other (non-Latino) | 19 | 4.4 |
| Unknown | 2 | 0.5 |
| Insurance Source (select all that apply) | ||
| No health insurance | 45 | 10.4 |
| Work place insurance | 45 | 10.4 |
| DC alliance b | 118 | 27.4 |
| Medicare | 85 | 19.7 |
| Medicaid | 154 | 35.7 |
| VA or military | 12 | 2.8 |
| Student insurance | 0 | 0.0 |
| Other health insurance source | 20 | 4.6 |
| Marital Status | ||
| Single, never married | 189 | 43.9 |
| Married | 84 | 19.5 |
| Partnered | 28 | 6.5 |
| Separated | 45 | 10.4 |
| Divorced | 58 | 13.5 |
| Widowed | 24 | 5.6 |
| Unknown | 3 | 0.7 |
| Financial Dependents | ||
| No dependents | 126 | 29.2 |
| One | 94 | 21.8 |
| Two | 60 | 13.9 |
| Three | 63 | 14.6 |
| Four | 33 | 7.7 |
| Other/5+ | 52 | 12.1 |
| Unknown | 3 | 0.7 |
| Educational Attainment | ||
| 8th grade or less | 44 | 10.2 |
| Some HS, but didn’t graduate | 74 | 17.2 |
| HS grad or GED | 152 | 35.3 |
| Some college or 2-year degree | 115 | 26.7 |
| 4-year college graduate | 25 | 5.8 |
| Some graduate/professional | 21 | 4.9 |
| Household Annual Income | ||
| Less than $10,000 | 147 | 34.1 |
| 10,000–19,999 | 125 | 29.0 |
| 20,000–29,999 | 55 | 12.8 |
| 30,000–39,999 | 26 | 6.0 |
| 40,000–49,999 | 16 | 3.7 |
| 50,000 or more | 3 | 0.7 |
| Don’t know or missing | 59 | 13.7 |
| Ever had public support for: | ||
| Housing | 142 | 35.1 |
| Food | 218 | 51.9 |
| Post High School Education | 96 | 24.2 |
| Job training | 102 | 25.8 |
| Finding a job | 97 | 24.9 |
| Daycare | 36 | 9.6 |
| Transportation | 122 | 30.5 |
| Income tax credit | 152 | 35.8 |
| General Health Status | ||
| Excellent | 51 | 11.9 |
| Very good | 103 | 24.0 |
| Good | 155 | 36.1 |
| Fair | 98 | 22.8 |
| Poor | 23 | 5.4 |
| Have the following illnesses | ||
| High blood pressure | 134 | 32.5 |
| Diabetes | 44 | 11.3 |
| Cancer | 15 | 4.0 |
Where the numbers add up to less than the total number of participants this reflects missing data.
DC Health care Alliance is a public-private partnership1 providing free health insurance to Washington, DC residents who have no health insurance and have income at or below 200% of the federal poverty level, including those not eligible for Medicaid.
African American and Latino participants differed substantially. African Americans were more likely to be older than 30 (92% vs. 74%, p<.0001), less likely to be married (15% vs. 45%, p[=? <?].0001), less likely to have financial dependents (4% vs. 42%, p<.0001), more likely to have at least a high school diploma (39% vs. 23%, p=.008), more likely to have household incomes under $10,000 (50% vs. 19%, p<.0001), more likely to report any chronic illness (59% vs. 36%, p<.0001), and much less likely to be uninsured (4% vs. 21%, p<.0001) than Latinos.
Individual choices
Among traditional health sector benefits, health insurance was an unwavering priority for nearly all study participants (>92%) and dental care was nearly as important (82%) (Table 2). Among socioeconomic interventions, the housing intervention was most important, being consistently chosen by over 80% of participants. Employment benefits were next, with job training and job placement chosen by over 70% and 67% of participants, respectively. Among education benefits, adult education was picked by over 60% and child education was picked by over 55% of participants.
Table 2.
INTERVENTIONS CHOSEN BY INDIVIDUALS IN ROUND 1 AND ROUND 4 (N = 431)
| Benefits | % Selected Round 1 | % Selected Round 4 | p value* |
|---|---|---|---|
| Education | |||
| Adult education | 66 | 63 | 0.381 |
| Childhood education | 55 | 61 | 0.024 |
| English education | 37 | 40 | 0.143 |
| Employment | |||
| Job training programs | 74 | 72 | 0.313 |
| Job placement | 67 | 67 | 0.928 |
| Day care | 42 | 51 | 0.002 |
| Health Care | |||
| Health coverage | 92 | 95 | 0.016 |
| Dental care | 82 | 82 | 0.823 |
| Counseling | 60 | 68 | 0.009 |
| Housing | |||
| Housing | 82 | 82 | 0.916 |
| Transportation | |||
| Transportation | 55 | 50 | 0.065 |
| Nutrition | |||
| Grocery incentive locations | 60 | 54 | 0.016 |
| Food stamps | 42 | 39 | 0.155 |
| School meals | 48 | 54 | 0.061 |
| Neighborhood | |||
| Neighborhood | 61 | 66 | 0.082 |
| Healthy Behavior | |||
| Healthy behavior | 61 | 68 | 0.011 |
| Income supplements | |||
| Any stickers kept aside | 35 | 25 | <0.001 |
p value based on McNemar’s Chi-square test comparing Round 1 to Round 4 for each intervention selected
While the benefits mentioned above were selected without much variation across individuals with differing socio-demographic characteristics, other benefits were prioritized more variably, as indicated in bivariate analyses. In light of the multiple comparisons, we highlight here only those associations with significance values of p≤.01 found in the final round of individual choices. Latinos were more interested than African Americans in childhood education (72% vs. 57%, p≤.01) and English language training (81% vs. 17%, p≤.01). Participants with financial dependents were more likely than those without dependents to choose job placement (72% vs. 57%, p≤.01). Food stamps were more commonly a priority for individuals without dependents than for those with dependents (49% vs. 33%, p≤.01) and those with annual incomes under $10,000 compared with those with incomes over $20,000 (50% vs. 31%, p≤.01).
Several interventions were more likely to be included in individuals’ final packages than in their initial packages (Table 2). Daycare was initially chosen by 42% and finally chosen by 51% of participants (p=.002). Counseling was initially chosen by 60% and finally chosen by 68% of participants (p=.009). Healthy behavior was initially chosen by 61% and finally chosen by 68% (p=.011). The choice to take a cash supplement diminished between the initial and final rounds and participants became more inclined to choose additional interventions.
Multivariable logistic regression modeling was carried out to examine the association of socio-demographic variables with each final round choice of the three educational interventions, daycare, food stamps, grocery store locations, and income supplements. Race/ethnicity (African American vs. Latino) remained significantly associated with selection of the educational interventions, daycare, and income supplements (Table 3). In models where race was the only significant variable, there was some confounding by other variables, even though the other variables were not significant. The adjustment by these other variables often increased the strength of the association between African Americans and Latinos. Latinos were more likely than African Americans to choose adult education (78% vs. 56%, p=.01), childhood education (77% vs. 56%, p=.006), and English as a second language programs (85% vs. 17%, p<.001). African Americans were more likely to choose income supplements (34% vs. 6%, p<.01) (Table 3).
Table 3.
ADJUSTED PERCENTS OF BENEFITS SELECTED (FINAL ROUND) BY PARTICIPANT CHARACTERISTICSa
| % Adult Educationb | % Childhood Educationc | % English Educationb | % Day Careb | % Food Stampsb | % Store Locationb | % Income Supplementb | |
|---|---|---|---|---|---|---|---|
| Age | |||||||
| <30 | 75* | ||||||
| 30–49 | 67 | ||||||
| 50+ | 57 | ||||||
| Race/Ethnicity | |||||||
| Black (non-Latino) | 56*** | 56*** | 17*** | 46*** | 44** | 61** | 34*** |
| Latino | 78 | 77 | 85 | 69 | 23 | 38 | 6 |
| Insurance Source | |||||||
| No health insurance | 35*** | ||||||
| DC alliance | 61 | ||||||
| VA/Medicare/Medicaid | 72 | ||||||
| Private | 64 | ||||||
| Other source | 54 | ||||||
| Marital Status | |||||||
| Married or partnered | 54* | ||||||
| Not married | 36 | ||||||
| General Health Status | |||||||
| Excellent/Very Good | 47** | ||||||
| Good/Fair/Poor | 59 | ||||||
p<.10
p<.05
p<.01
Base on the beta estimates from a logistic regression model for each of the five benefit choices; only associations with p<0.1 are presented; all p values have been corrected for any intra-class correlation due to group.
Logistic regression model included variables for age, gender, race, insurance status, marital status, any financial dependents, education attainment, general health status, and any illnesses.
Logistic regression model included variables for age, race, and insurance status.
Relationship between received services and priorities
While a large proportion of participants prioritized certain interventions at the conclusion of the exercise (Table 3), fewer had received them (Table 1). For example 82% of participants prioritized housing, while only 35% reported receiving public support for housing; 72% prioritized job training, while 26% had received such support; 67% prioritized job placement, while 25% received such support. There was a better match between the percentage prioritizing and receiving food stamps (54% vs. 52%).
Group choices
During the third round of the exercise, groups picked interventions in the following order of descending frequency: health insurance (100%), housing vouchers (91%), dental care (80%), job training (75%), adult education (70%), counseling (68%), neighborhood improvement (68%), daycare (66%), childhood education (64%), school meals (59%), job placement (57%), healthy behavior incentives (55%), food stamps (39%), grocery store incentives (34%), transportation (34%), English education (32%), and income supplements (7%).
Assessment of the exercise during the post-exercise survey indicated that the vast majority of participants found it informative, easy to use, easy to understand, and a fair process for deliberation (Table 4).
Table 4.
PARTICIPANT ASSESSMENT OF THE REACH EXERCISEa
| Survey Item | Disagree strongly | Disagree Somewhat | Neither | Agree Somewhat | Agree Strongly | No Answer |
|---|---|---|---|---|---|---|
| The exercise is enjoyable | 0 | 0 | 1 | 9 | 87 | 2 |
| The exercise is easy | 1 | 3 | 1 | 14 | 77 | 3 |
| The exercise is informative | 1 | 0 | 2 | 9 | 84 | 3 |
| The way the group reached its decision was fair | 0 | 1 | 2 | 20 | 74 | 3 |
Numbers reflect percentage of study participants in each category.
Discussion
The interventions that were most important to the low-income residents of Washington, D.C. who participated in this study were health insurance, dental care, housing, job training, counseling, healthy behavior incentives, job placement, and neighborhood improvement. Latino participants, who were less educated and more likely to be married and have financial dependents, assigned priority to child education, English language training, and daycare to a greater extent than African Americans did. African Americans were more likely to prioritize income supplements. Contrary to our hypothesis, the priority assigned to education was no higher for younger participants than for older participants. It is noteworthy that many participants who considered housing, higher education, job training, and job placement important priorities had not received these types of support.
Actuarial estimates for the cost of the socioeconomic interventions offered in this exercise ranged widely from nine dollars per person per month for neighborhood improvements and for grocery stores to $207 for food stamps. In comparison, each of these socioeconomic interventions cost substantially less than the estimated cost of medical and dental care for uninsured individuals with incomes under 200% of the poverty threshold, which was estimated to be $442 per month.*
While we estimated costs as described in the methods section, we should note other methods for assessing the cost of intervention programs. One could take a first-principles approach, for example, in which a program’s design would facilitate the development of a delivery system, with assumed reimbursement levels, usage patterns, and service take-up rates. Nearly every part of each program could be explored and developed, all in justification of assessing a total cost.
Alternatively, without developing programs fully, the cost assessment method might have relied more broadly on facts about existing programs. We took this approach where possible; however, we were not able to find existing programs for all the proposed interventions. Taking this approach further would involve creating a marginal cost estimate for the intervention program operating within a current structure.
Finally, the cost assessment could have relied more heavily on eligibility criteria for each program to narrow the characteristics of individuals enrolling in each intervention. With a focused treatment group the cost assessment can rely upon the average cost of treating those conditions within the current market today. We note that using any of the alternatives to cost assessment mentioned here would not necessarily create significant differences in the choices presented to REACH exercise participants, since the relative costs for different choices would need to move significantly to change a single sticker value for any intervention. If all costs increase or decrease by the same percentage, relative costs (and the sticker values) are unchanged.
There are several strengths of this study. The study was conducted among a population that one would want to target in efforts to reduce socioeconomically determined health disparities. The exercise involved the use of a validated decision tool for group deliberation.33 Furthermore, assessment of the paper version of the REACH exercise used in this study, conducted as part of the post-exercise survey, shows that participants considered the exercise informative, easy to understand and use, as well as a fair deliberative process. The interventions offered in the exercise include the range of interventions that a distressed, poor community might find useful. They were targeted both at individuals (e.g., counseling and food stamps) and at communities (e.g., neighborhood improvements and grocery stores) and focused both on upstream interventions (e.g., education and job training) as well as downstream interventions (e.g., counseling that might be chosen in reaction to already incurred stress). The presentation of choices in the exercise was designed to be unbiased in that intervention options were presented around a circular board with no indication of a hierarchy. At the same time, the exercise permitted the incorporation of expert guidance regarding the socioeconomic interventions to be offered and their cost into the deliberative process. The evolution of participants’ choices over the course of the exercise indicates that the process allows non-expert participants to gain insights into SEDH; thus, the exercise can serve an educational function. Without such a process intended to help the public understand SEDH, the general public may be entirely unaware of the contribution of socioeconomic factors to health.42
Some limitations must be acknowledged. First, we cannot be certain that the interventions that were offered were the best ones, since there is little literature to date examining and comparing the effectiveness of many interventions.17 Second, the cost estimates for interventions were related to a particular low-income, urban population in the U.S., so that one cannot automatically assume they approximate the costs of providing interventions for other low-income populations. Third, as is always the case for research based on small-group exercises, our study participants did not constitute a random sample of the population of interest. However, the educational level and marital status of the African American and Latino participants reflect the demographic characteristics of these ethnic groups as reported in census statistics for Washington, D.C.43 We have made an effort to model the association of participant characteristics with the interventions they selected. Fourth, we cannot infer that the choices of poor and low-income residents outside of Washington, D.C. would be like those of the participants in this study.
We believe this exploratory study contributes valuable empirical data for developing strategies to prioritize interventions aimed at addressing the social determinants of health, an area that has been widely neglected.7,44 Kaplan has argued that social epidemiology can be used to identify groups that are at unequal risk and that interventions should be targeted at low socioeconomic positions, place-based limitations in opportunities and resources, stages of the life-course, and the underlying factors associated with marginalization and exclusion.45 A small number of studies of the perspectives of disadvantaged populations regarding the socioeconomic determinants of health derive from community-based participatory research.46–48 For example, a study conducted in a poor community in Detroit focused on the stresses experienced in the community and generated suggestions that grew out of these shared experiences.48 The resulting solutions, such as social support offered through social networks, focused on community-based interventions for reducing the stress and violence that often afflict these communities.
While there is little information regarding public priorities for addressing the SEDH, there is substantial research in the economics literature examining the many dimensions of poverty, their measurement, and how to aggregate them to determine the overall extent of poverty of a population.49–51 This research includes efforts to ascertain public priorities for mitigating poverty.51 It is interesting to consider whether these approaches to studying poverty might be utilized to examine priorities for addressing poverty-related health deficits.
Given the exploratory nature of our study, we must be cautious about identifying policy implications of the results. We suggest, though, that in a climate of limited budgets for planning and budgeting services, a municipality may find informed choices of their poorest residents useful, and a department of human services may find information about the priorities of clients useful. The District of Columbia makes a concerted effort to make its social services accessible to its low-income residents. Information about and applications for services are available in a streamlined form through the District of Columbia Human Services website (http://dhs.dc.gov/dhs/site/default.asp).
Several of the findings here prompt consideration of additional research questions. Are the priorities we have ascertained stable over time? Would they change as local and national economic prospects change and factors such as the ease of getting employment, the cost of housing, and household expenses vary? How would the priorities of other poor and low-income residents of other communities compare with those of Washington, D.C.? Ultimately, we must ask whether the provision of a combination of social services according to the highest priorities of a low-income population would serve to improve their health.
Acknowledgments
The study was funded by the National Center for Minority Health and Health Disparities and the Dept. of Bioethics at the National Institutes of Health. We thank Arthur L. Baldwin III, FSA, MAAA and Ben Diederich, FSA, MAAA for the actuarial estimates; Amy Tiedemann, PhD and Yvonne Chueh, PhD for review of existing intervention programs; Christopher Dame for design of the artwork for the study materials; Bamidele Olupona, MPH, for recruiting study participants and conducting many of the groups exercises; John Lee Holmes, MA, for data preparation; Kien Le, MA, for creation of the recruitment website; and Chinwe Sonia Kpaduwa for assistance in preparing the manuscript.
Footnotes
Since the program was under review at the time of the present study, the DC Alliance did not release cost data. Cost estimates of providing medical services for the low-income population in Washington, D.C. were thus based on a survey of western Medicaid states’ Temporary Aid for Needy Families (TANF) capitation reimbursement rates as documented in the Cost Analysis Report for Intervention Programs to Address Socio-Economic Determinants of Health (see reference 37, pp. 24–27).
Disclaimer: The views expressed here are those of the authors and do not necessarily reflect the policies of the National Institutes of Health or the U.S. Department of Health and Human Services. The authors do not have any affiliation with programs depicted in the exercise.
Notes
- 1.World Health Organization, Commission on the Social Determinants of Health. Closing the gap in a generation: health equity through action on the social determinants of health. Geneva, Switzerland: World Health Organization; 2008. Available at: http://www.searo.who.int/LinkFiles/SDH_SDH_FinalReport.pdf. [PubMed] [Google Scholar]
- 2.Alkire S, Foster J. Counting and multidimensional poverty measurement (Working Paper 7) Mansfield Road, Oxford, United Kingdom: Oxford Poverty and Human Development Initiative; 2008. [Google Scholar]
- 3.Stoddart GL, Eyles JD, Lavis JN, et al. Reallocating resources across public sectors to improve population health. In: Heymann J, Hertzman C, Barer ML, et al., editors. Healthier societies: from analysis to action. Oxford, United Kingdom: Oxford University Press; 2006. [Google Scholar]
- 4.Canadian Institute for Health Information. Improving the health of Canadians. Ottawa, Ontario, Canada: Canadian Institute for Health Information; 2004. [Google Scholar]
- 5.Robert Wood Johnson Foundation, Commission to Build a Healthier America. Final report. Princeton, NJ: Robert Wood Johnson Foundation; 2009. Available at: http://www.commisiononhealth.org. [Google Scholar]
- 6.Acheson D. Independent inquiry into inequalities in health. Norwich. United Kingdom: The Stationary Office; 1998. Available at: http://www.archive.official-documents.co.uk/document/doh/ih/ih.htm. [Google Scholar]
- 7.Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Aff (Millwood) 2002 Mar-Apr;21(2):60–76. doi: 10.1377/hlthaff.21.2.60. [DOI] [PubMed] [Google Scholar]
- 8.U.S. Census Bureau. Income alternative poverty estimates in the United States: 2003. Washington, DC: U.S. Census Bureau; 2003. p. 18.p. 20. (Report P60, n. 227, Tables B-1 and B-3) [Google Scholar]
- 9.Nelson KP. Whose shortage of affordable housing? Housing Policy Debate. 1994;5(4):401–42. [Google Scholar]
- 10.DeParle J, Gebeloff R. Food stamp use soars across US, and stigma fades. New York, NY: New York Times; Nov 28, 2009. Available at: http://www.nytimes.com/2009/11/29/us/29foodstamps.html. [Google Scholar]
- 11.Johnson N, Oliff P, Williams E. An update on state budget cuts: at least 45 states have imposed cuts that hurt vulnerable residents and the economy. Washington, DC: Center on Budget and Policy Priorities; 2009. Available at: http://www.cbpp.org/files/3-13-08sfp.pdf. [Google Scholar]
- 12.U.S. Census Bureau. Historical poverty tables. Washington, DC: U.S. Census Bureau; 2010. Available at: http://www.census.gov/hhes/www/poverty/data/historical/index.html. [Google Scholar]
- 13.District of Columbia Department of Health, Behavioral Risk Factor Surveillance System (BRFSS) 2006 annual report. Washington, DC: District of Columbia Department of Health; 2006. Available at: http://doh.dc.gov/doh/frames.asp?doc=/doh/lib/doh/services/administration_offices/phsa/behavioral_risk/pdf/final_2006_annual_report_033109.pdf. [Google Scholar]
- 14.Rogers A. Squeezed out: the worsening shortage of affordable housing for low-income DC households. Washington, DC: D.C. Fiscal Policy Institute; 2005. [Google Scholar]
- 15.D.C. Fiscal Policy Institute. Budget cuts adopted by the DC council fall disproportionately on programs for low income residents. Washington, DC: D.C. Fiscal Policy Institute; 2008. [Google Scholar]
- 16.World Health Organization (WHO) Social determinants of health; backgrounder 3: key concepts. Switzerland: WHO; 2010. Available at: http://www.who.int/social_determinants/final_report/key_concepts_en.pdf. [Google Scholar]
- 17.Marmot MG, Wilkinson RG, editors. Social determinants of health. 2. Oxford, United Kingdom: Oxford University Press; 2006. [Google Scholar]
- 18.Evans RG, Barer ML, Marmot TR. Why are some people healthy and others not? The determinants of health of populations. New York, NY: Aldine de Gruyter; 1994. [Google Scholar]
- 19.Lahelma E, Martikainen P, Laaksonen M, et al. Pathways between socioeconomic determinants of health. J Epidemiol Community Health. 2004 Apr;58(4):327–32. doi: 10.1136/jech.2003.011148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lantz PM, House JS, Lepkowski JM, et al. Socioeconomic factors, health behaviors, and mortality: results from a nationally representative prospective study of U.S. adults. JAMA. 1998 Jun 3;279(21):1703–8. doi: 10.1001/jama.279.21.1703. [DOI] [PubMed] [Google Scholar]
- 21.Brunner E, Marmot M. Social organization, stress, and health. In: Marmot MG, Wilkinson RG, editors. Social determinants of health. 2. Oxford, United Kingdom: Oxford University Press; 2006. [Google Scholar]
- 22.Blane D. The life course, the social gradient, and health. In: Marmot MG, Wilkinson RG, editors. Social determinants of health. 2. Oxford, United Kingdom: Oxford University Press; 2006. [Google Scholar]
- 23.Stanfeld SA. Social support and social cohesion. In: Marmot MG, Wilkinson RG, editors. Social determinants of health. 2. Oxford, United Kingdom: Oxford University Press; 2006. [Google Scholar]
- 24.Veazie MA, Galloway JM, Matson-Koffman D, et al. Taking the initiative: implementing the American Heart Association Guide for Improving Cardiovascular Health at the Community Level: Healthy People 2010 Heart Disease and Stroke Partnership Community Guideline Implementation Best Practices Workgroup. Circulation. 2005 Oct 18;112(16):2538–54. doi: 10.1161/CIRCULATIONAHA.105.169179. [DOI] [PubMed] [Google Scholar]
- 25.The Standing Committee on Social Affairs, Science and Technology. A healthy, productive Canada: a determinant of health approach (final report of Senate subcommittee on population health) Ontario, Canada: The Standing Committee on Social Affairs, Science and Technology; 2009. Available at: http://www.parl.gc.ca/40/2/parlbus/commbus/senate/com-e/popu-e/rep-e/rephealth1jun09-e.pdf. [Google Scholar]
- 26.Harkness J, Newman SJ. Housing affordability and children’s well-being: evidence from the national survey of America’s families. Housing Policy Debate. 2005;16(2):223–55. [Google Scholar]
- 27.Frank DA, Neault NB, Skalicky A, et al. Heat or eat: the Low Income Home Energy Assistance Program and nutritional and health risks among children less than 3 years of age. Pediatrics. 2006 Nov;118(5):e1293–302. doi: 10.1542/peds.2005-2943. [DOI] [PubMed] [Google Scholar]
- 28.Lipman BJ. Something’s gotta give: working families and the cost of housing. 2. Vol. 5. Washington, DC: Center for Housing Policy; 2005. pp. 1–48. Available at: http://www.nhc.org/media/documents/somethings_gotta_give.pdf. [Google Scholar]
- 29.Thomson H, Thomas S, Sellstrom E, et al. The health impact of housing improvement: a systematic review of intervention studies from 1887 to 2007. Am J Public Health. 2009 Nov;99(S3):S681–92. doi: 10.2105/AJPH.2008.143909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sadowski LS, Kee RA, VanderWeele TJ, et al. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: a randomized trial. JAMA. 2009 May 6;301(17):1771–8. doi: 10.1001/jama.2009.561. [DOI] [PubMed] [Google Scholar]
- 31.Buchanan D, Kee R, Sadowski LS, et al. The health impact of supportive housing for HIV-positive homeless patients: a randomized controlled trial. Am J Public Health. 2009 Nov;99(Suppl 3):S675–80. doi: 10.2105/AJPH.2008.137810. Epub 2009 Apr 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McIntyre L. Montreal, Quebec, Canada: Policy Options Politique; 2003. Food security: more than a determinant of health. Available at: http://communities.mysudbury.ca/Sites/foodsecurity/Food%20Security%20Reports/Lynn%20McIntyre%20-%20Food%20security.pdf. [Google Scholar]
- 33.Giang T, Karpyn A, Lsurison HB, et al. Closing the grocery gap in underserved communities: the creation of the Pennsylvania Fresh Food Financing Initiative. J Public Health Manag Pract. 2008 May-Jun;14(3):272–9. doi: 10.1097/01.PHH.0000316486.57512.bf. [DOI] [PubMed] [Google Scholar]
- 34.Sharkey P. Causal effects of neighborhood improvement on children’s economic and social trajectories. Presented at: American Sociological Association Annual Meeting; Boston (MA). Jul 31, 2008; Available at: http://www.allacademic.com/meta/p241832_index.html. [Google Scholar]
- 35.Connor J, Rodgers A, Priest P. Randomised studies of income supplementation: a lost opportunity to assess health outcomes. J Epidemiol Community Health. 1999 Nov;53(11):725–30. doi: 10.1136/jech.53.11.725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kotwani N, Danis M. Expanding the current health care reform debate: making the case for socio-economic interventions for low income young adults. J Health Care L and Pol’y. 2009;12(1) [Google Scholar]
- 37.Baldwin AL, III, Diederich B. Cost analysis report for intervention programs to address socio-economic determinants of health. Seattle, WA: Milliman Inc; 2007. Oct 9, Available at: http://www.bioethics.nih.gov/research/chat/Milliman%20Analysis%20Cost%20Report.pdf. [Google Scholar]
- 38.U.S. Department of Health and Human Services. The 2006 HHS poverty guidelines. Washington, DC: U.S. Department of Health and Human Services; 2007. Available at: http://aspe.hhs.gov/poverty/06poverty.shtml. [Google Scholar]
- 39.Danis M, Lovett F, Sabik L, et al. Low-income employees’ choices regarding employment benefits aimed at improving the socioeconomic determinants of health. Am J Public Health. 2007 Sep;97(9):1650–7. doi: 10.2105/AJPH.2006.091033. Epub 2007 Jul 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Danis M, Biddle AK, Dorr Goold S. Insurance benefit preferences of the low-income uninsured. J Gen Intern Med. 2002 Feb;17(2):125–33. doi: 10.1046/j.1525-1497.2002.10609.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Goold SD, Biddle SK, Klipp G, et al. Choosing Healthplans All Together: a deliberative exercise for allocating limited health care resources. J Health Polit Policy Law. 2005 Aug;30(4):563–601. doi: 10.1215/03616878-30-4-563. [DOI] [PubMed] [Google Scholar]
- 42.Robert SA, Booske BC, Rigby E, et al. Public views on determinants of health, interventions to improve health, and priorities of government. WMJ. 2008 May;107(3):124–30. [PubMed] [Google Scholar]
- 43.United States Census Bureau. American Community Survey (ACS) Washington, DC: U.S. Census Bureau; 2008. Available at: http://www.census.gov/acs/www/ [Google Scholar]
- 44.Public Health Agency of Canada. Crossing sectors—experiences in intersectoral action, public policy and health. Ottawa, Ontario, Canada: Public Health Agency of Canada; 2007. Available at: www.phac-aspc.gc.ca/publicat/2007/cro-sec/7ia_e.html. [Google Scholar]
- 45.Kaplan GA. Health inequalities and the welfare state: perspectives from social epidemiology. Norsk Epidemiologi. 2007;17(1):9–20. Available at: http://www.ntnu.no/ojs/index.php/norepid/article/viewFile/165/146. [Google Scholar]
- 46.Nwangwu RE. Slum dwellers’ diagnoses of their own needs: implications for community development in Nigeria. Dev Pract. 1998 May;8(2):225–8. doi: 10.1080/09614529853855. [DOI] [PubMed] [Google Scholar]
- 47.Kreiger J, Allen C, Cheadle A, et al. Using community-based participatory research to address social determinants of health: lessons learned from Seattle Partners for Healthy Communities. Health Educ Behav. 2002 Jun;29(3):361–82. doi: 10.1177/109019810202900307. [DOI] [PubMed] [Google Scholar]
- 48.Schulz AJ, Parker EA, Israel BA, et al. Addressing social determinants of health through community-based participatory research: the East Side Village Health Worker Partnership. Health Educ Behav. 2002 Jun;29(3):326–41. doi: 10.1177/109019810202900305. [DOI] [PubMed] [Google Scholar]
- 49.Bibi S. Measuring poverty in a multidimensional perspective: a review of literature (PMMA working paper 2005-7) Quebec, Canada: PEP-PMMA; 2005. Available at: https://www.gtap.agecon.purdue.edu/resources/download/2798.pdf. [Google Scholar]
- 50.Thorbecke E. Multi-dimensional poverty: conceptual and measurement issues. Brasilia, Brazil: UNDP International Poverty Centre; 2005. Available at: http://www.ipc-undp.org/md-poverty/papers/Thorbecke_.pdf. [Google Scholar]
- 51.de Kruijk H, Rutten M. Weighting dimensions of poverty based on people’s priorities: constructing a composite poverty index for the Maldives. Toronto, Canada: Centre for International Studies; 2007. Available at: http://www.q-squared.ca/pdf/Q2_WP35.pdf. [Google Scholar]