Abstract
Carotid body tumors (CBT) are rare chemical receptor tumors. We report nine cases of CBT who were diagnosed at our center during 2004 to 2008 with a literature review. Of these nine patients, eight underwent complete resection, one received palliative resection due to the malignant nature of the tumor, and the other one refused surgery. No perioperative mortality and stroke occurred. During a mean follow up of 2.2 years, no deaths related to CBT occurred. Surgical treatment for CBT is relatively safe. The surgeon should be careful to maintain the integrity of carotid artery, and prevent cerebral ischemia and cranial nerve injuries in order to improve outcome.
Keywords: Carotid body, Surgery, Therapy, Neoplasms
1. Introduction
Carotid body tumors (CBT) are rare chemical receptor tumors which accounts for 0.6% of the head and neck tumors in human. The CBT is usually benign with the incidence of malignant tumors below 10%.[1] Although surgical resection is a reliable therapeutic method for CBT, the procedure is technically challenge for surgeons due to the tumor's adjacent to great vessels and cranial nerve. We report nine cases of CBT who were treated at our center during 2004 to 2008 with a literature review.
2. Case report
From 2004 to 2008, nine patients were diagnosed as CBT at the Department of Vascular Surgery, Xuanwu Hospital, Capital Medical University. Among them, five were male, the mean age was 43 years (range from 26 to 84 years). All patients had a movable mass in the anterior cervical triangle regions. Other common symptoms included tenderness, dizziness, hoarseness and dysphasia. One patient was previously misdiagnosed as cervical liparomphalus and had unsuccessful resection operation.
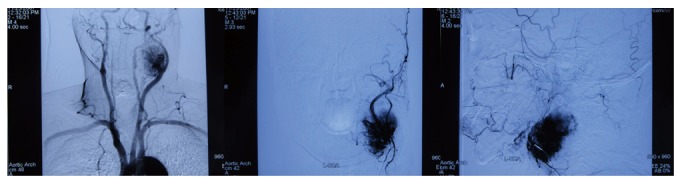
Six patients underwent color Doppler ultrasonography. Low echo-level chunks were detected in external carotid arteries and internal carotid arteries. Diameters range from 1.4 cm to 6.0 cm (Figure 1). Seven patients underwent transcranial doppler (TCD) sonography before the surgery (Figure 2). In all of these patients, the carotid artery compression test showed that blood flow in cerebral arteries decreased by 60% or more. Three patients had CT examination with angiography plus three-dimensional reconstruction, which showed that soft tissues encased the posterior lateral side of the left common carotid artery bulb. All patients had digital subtraction angiography (DSA), which showed abnormal accumulation of contrast medium at the crotch of common carotid artery.
Figure 1. Doppler ultrasonography showed carotid body tumor (2.91 cm × 2.29 cm × 1.84 cm).

Figure 2. Digital subtraction angiography reveals a tumor mass at the bifurcation of the left carotid artery (5.1 cm × 4.7 cm × 3.5 cm).
Preoperative Shambin grouping was performed according to imaging examinations. Four patients were classified as type I, two as type II and three as type III. Eight patients underwent surgical treatments under general anesthesia. Four of them underwent simple carotid body tumor resection, two underwent carotid body tumor resection and ligation of external carotid artery and two had common carotid artery-internal carotid artery artificial vascular reconstruction.
No perioperative mortality and stroke occurred. During a mean follow-up of 2.2 years (3 months to 6 years), the patient who refused surgery died three years after the diagnosis due to complications from bone fracture. The patient with malignant tumor died two years after the surgery due to multiple metastases.
3. Discussion
CBT is the most frequently diagnosed carotid body disease and is also termed as chemodectoma. It is originated from nervous crest and belongs to nonchromaffin paraganglioma, which is similar to chromaffin suprarenal medulla tumors (such as chromaffin tumors) with the same origin in histology. CBT can be found at any age and is frequently seen in those between 50 and 70 years old, which slightly higher prevalence in women than men. Bilateral disease is significantly more frequent in familial (31.8% of cases) than in non-familial CBT (4.4%).[3] The blood supply of CBT is abundant, which is mainly from external carotid artery and branches. Blood supplies from internal carotid artery, vertebral artery, ascending pharyngeal artery and superior thyroid artery have also been reported.[4] In addition to external carotid artery, multiple blood supply from internal carotid artery, thyrocervical trunk, vertebral artery and ascending pharyngeal artery were also found in two patients in our case series.
3.1. Clinical diagnosis for CBT
CBT can be preliminarily diagnosed according to history and physical examinations. Final diagnosis mainly depends on image examination. Doppler ultrasound and DSA play important roles in the clinical diagnosis of CBT. Color Doppler ultrasound, a simple and non-invasive examination, has relatively high specificity and sensitivity for CBT. Currently, DSA is the ‘golden criteria’ for final diagnosis of CB. Other diagnostic methods include aspiration-needle biopsy, CT and MRI. The accuracy of MRI is higher in comparison to that of CT. Furthermore, MRI is not radioactive, and the diagnostic rate for multiple lesions is particularly important for the patients with family history.[5]
3.2. Surgical treatment of CBT
Shamblin research group classified CBT into type I (localized type), type II (partially wrapped type) and type III (wrapped type).[6] With the higher Shamblin grading, the possibilities for injuries in cranial nerves, fragility of cervical great vessels are higher during or after operations. Recent advance in vascular imaging techniques have enabled preoperative grading for tumor size, which can be completely consistent with the Shamblin grading during operations.[6]
Surgical resection remains the treatment of choice for CBT.[7] In an earlier report, we have divided the surgery into four types according to Shamblin grading and tumor blood supply.[8] Simple resection of carotid body tumor is the most ideal operation form, which would not damage the shape and distribution of cervical arteries. Thus, it is suitable for Shamblin type I/II cases without abundant blood supply. Carotid body tumor resection and reconstructive vascular operation (including simple vascular anastomosis, internal carotid artery-common carotid artery artificial and autologous reconstructive vascular operation) are suitable for Shamblin type III cases with enormous tumors and malignant tumors involving important peripheral vessels. In the carotid body tumor resection and ligation of common carotid artery, cerebral ischemia is a relatively common complication and now is only used for emergent treatments.
3.3. Malignant CBT
Medullary chromaffinoma is always benign and the incidence of malignant tumors is lower than 10%. One case of malignant CBT in our patients had vertebral body metastasis two years after resection and finally died of the disease. Hu et al.[9] summarized 967 patients in 36 centers from 1962 to 2001 and reported that radiotherapy can be used as the adjunctive therapy for primary and metastatic foci. The efficacy for local control was equal to that for operations and the incidence of complications was significantly reduced in comparison to that for operations. However, the exposure dosage should be controlled below 45Gy. However, results from prospective studies of radiotherapy for malignant CBT are still unavailable and it is not routinely.
References
- 1.Bakoyiannis KC, Georgopoulos SE, Klonaris CN, et al. Surgical treatment of carotid body tumors without embolization. Int Angiol. 2006;25:40–45. [PubMed] [Google Scholar]
- 2.Standring S. Gray's anatomy. Churchill Livingstone; 2004. [Google Scholar]
- 3.Grufferman S, Gillman MW, Pasternak LR, et al. Familial carotid body tumors: case report and epidemiologic review. Cancer. 1980;46:2116–2122. doi: 10.1002/1097-0142(19801101)46:9<2116::aid-cncr2820460934>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 4.Bastounis E, Maltezos C, Pikoulis E, et al. Surgical treatment of carotid body tumours. Eur J Surg. 1999;165:198–202. doi: 10.1080/110241599750007045. [DOI] [PubMed] [Google Scholar]
- 5.Olsen WL, Dillon WP, Kelly WM, et al. MR imaging of paragangliomas. Am J Roentgenol. 1987;148:201–204. doi: 10.2214/ajr.148.1.201. [DOI] [PubMed] [Google Scholar]
- 6.Arya S, Rao V, Juvekar S, et al. Carotid body tumors: objective criteria to predict the Shamblin group on MR imaging. Am J Neuroradiol. 2008;29:1349–1354. doi: 10.3174/ajnr.A1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Knight T J, Gonzalez J A, Rary J M, et al. Current concepts for the surgical management of carotid body tumor. Am J Surg. 2006;191:104–110. doi: 10.1016/j.amjsurg.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 8.Wang ZG. Surgical treatment of carotid body tumor in 69 cases. Chin J Gen Surg. 2002;17:9–12. [Google Scholar]
- 9.Hu K, Persky M S. The multidisciplinary management of paragangliomas of the head and neck, Part 2. Oncology. 2003;17:1143–1161. [PubMed] [Google Scholar]


