Abstract
Objectives
To investigate the mechanism(s) of action of MBSR(BC) including reductions in fear of recurrence and other potential mediators.
Methods
Eighty-two post-treatment breast cancer survivors (stages 0-III) were randomly assigned to a 6-week MBSR(BC) program (n=40) or to Usual Care group (UC) (n=42). Psychological and physical variables were assessed as potential mediators at baseline and at 6 weeks.
Results
MBSR(BC) compared to UC experienced favorable changes for five potential mediators: (i) change in fear of recurrence problems mediated the effect of MBSR(BC) on 6-week change in perceived stress (z=2.12, p=0.03) and state anxiety (z=2.03, p=0.04); and (ii) change in physical functioning mediated the effect of MBSR(BC) on 6-week change in perceived stress (z=2.27, p=0.02) and trait anxiety (z=1.98, p=0.05).
Conclusions
MBSR(BC) reduces fear of recurrence and improves physical functioning which reduces perceived stress and anxiety. Findings support the beneficial effects of MBSR(BC) and provide insight into the possible cognitive mechanism of action.
Keywords: Fear of Recurrence, Cancer, Mindfulness-Based Stress Reduction (MBSR), Oncology
INTRODUCTION
Breast cancer is a major health problem and comprises the largest population of cancer survivors estimated at 2.6 million women in the United States (National Cancer Institute, 2010). Although some survivors of breast cancer adjust reasonably well over time to their disease-related emotional distress, fear of recurrence has been shown to chronically plague 24-89% of women with breast cancer (Girgis, Boyes, Sanson-Fisher, & Burrows, 2000; Hartl et al., 2003; Mehnert, Berg, Henrich, & Herschbach, 2009; Polinsky, 1994; Stanton et al., 2005; Stephens, Osowski, Fidale, & Spagnoli, 2008; van den Beuken-van Everdingen et al., 2008). The high prevalence of fear of recurrence as a distressing psychological and physical problem occurs regardless of risk, cancer site and can persist years after treatment (Armes et al., 2009; Baker, Denniston, Smith, & West, 2005; Deimling, Bowman, Sterns, Wagner, & Kahana, 2006; Hodges & Humphris, 2009; Humphris et al., 2003; Llewellyn, Weinman, McGurk, & Humphris, 2008; Matthews, 2003; Mehta, Lubeck, Pasta, & Litwin, 2003; Simard, Savard, & Ivers, 2010). Fear of recurrence induces particularly high morbidity among breast cancer survivors and is a complex phenomenon. Fear of recurrence is often viewed as a multidimensional phenomenon, including emotional components of anxiety and fear, and a cognitive dimension, including worry, preoccupation and intrusive thoughts (Lee-Jones, Humphris, Dixon, & Hatcher, 1997; Simard et al., 2010).
Fear of recurrence is often triggered by antecedents such as physical symptoms, or perceived risk resulting in psychological distress, decreased quality of life, and functional impairment (Simard et al., 2010; van den Beuken-van Everdingen et al., 2008) while contributing indirectly to fatigue (Minton & Stone, 2008; Young & White, 2006). For some patients this leads to behavioral consequences including increased health care visits, and double checking for recurrence (Cannon, Darrington, Reed, & Loberiza, 2011; Hawkins et al., 2010).
Since fear of recurrence is an established source of significant emotional distress among breast cancer survivors, it represents a logical, clinically-relevant target for intervention (Connell, Patterson, & Newman, 2006; Costanzo et al., 2007; Fredette, 1995; Johnson Vickberg, 2001; Oxlad, Wade, Hallsworth, & Koczwara, 2008; Schmid-Buchi, Halfens, Dassen, & van den Borne, 2008). The need for post-treatment intervention is not time dependent, per se, (Mehnert et al., 2009) in that fear of cancer recurrence has been found to persist up to 32 years after surgery (Polinsky, 1994). Additionally, in terms of appropriate intervention targeting, fear of recurrence may vary by age, with younger women having higher levels (Costanzo et al., 2007; Curran et al., 1998; Kornblith et al., 2007; Mast, 1998; Mehnert et al., 2009; van den Beuken-van Everdingen et al., 2008). Few interventions have been tested to reduce fear of recurrence, however, fear of progression was reduced among cancer survivors by short psychotherapeutic interventions of a cognitive-behavioral group therapy and supportive-experiential group therapy (Herschbach et al., 2010).
Over the past 25 years, research on mindfulness delivered through MBSR meditative practices has demonstrated effectiveness in reducing psychological and physical symptoms in a wide variety of clinical and non-clinical populations (Bohlmeijer, Prenger, Taal, & Cuijpers, 2010; Brown, Ryan, & Creswell, 2007; Chiesa & Serretti, 2009; Grossman, Niemann, Schmidt, & Walach, 2004; Matchim & Armer, 2007; Musial, Bussing, Heusser, Choi, & Ostermann, 2011). The effects of MBSR on fear of recurrence in a randomized trial by our team, was found to significantly reduce fear of recurrence among 84 breast cancer survivors (Lengacher et al., 2009) however in another pre-post study, only a trend towards reduction of fear of recurrence was found among 19 prostate cancer survivors (Chambers, Foley, Galt, Ferguson, & Clutton, 2012).
The foundations of the MBSR program are built on the healing power of “mindfulness” that is operationalized through two cognitive processes, awareness and attention (Brown & Cordon, 2009). Through the MBSR program patients learn to self-regulate awareness and attention (Bishop, 2002) and cultivate non-judging acceptance to implement change (Bishop et al., 2004; Brown et al., 2007; Kabat-Zinn, 1990, 2003). Through the “awareness” mode of cognitive processing, subjective experiences are processed such as images or feelings; these are held very briefly and are followed by appraisal or evaluation, such as being pleasant or unpleasant. These reactions are conditioned by past experiences, and can be associated with a memory; however, they are easily assimilated into other schemas. The “attention” mode of processing involves a “stepping back” process (Brown & Cordon, 2009) in which feelings and images are perceived objectively as they appear. Through attention, registration of bare facts is observed. Collectively, through cultivation of attention and awareness, persons are taught to be present in reality rather than only reacting to it and ruminating over past emotional experiences. Recent efforts have identified 3 specific components of mindfulness: 1) intention, which involves motivation and knowing why one is paying attention; 2) attention, which is knowing what is happening directly; and 3) attitude, which is paying attention through acceptance, caring qualities of mindfulness, or “affectionate attention” (Cullen, 2006; Shapiro, Oman, Thoresen, Plante, & Flinders, 2008).
For cancer survivors, the meditative approach and training in the cognitive process of mindfulness facilitates self-regulation of emotions during distress and suffering. This training emphasizes a moment-to-moment, non-judgmental and non-reactive awareness to internal and external experiences, thus reducing rumination and elaboration of distressful experiences (Baer, 2003; Bishop et al., 2004). Through the process of non-judging acceptance and focusing attention to the breath and body sensations, beneficial changes through self-regulation become evident (Perlman, Salomons, Davidson, & Lutz, 2010). Through the cognitive process of self-regulation the patient may regulate reaction to the triggers for fear of recurrence such as worry or rumination.
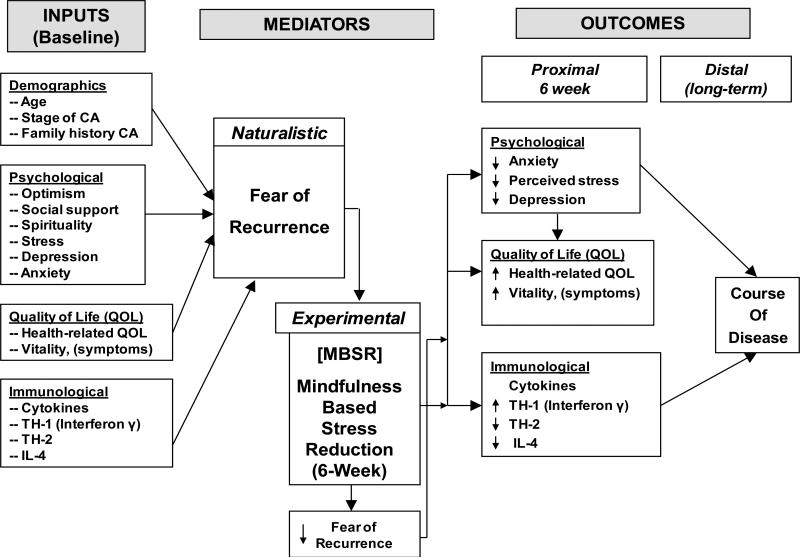
Because of the empirically-established benefits of MBSR among cancer survivors in reducing psychological distress, depression, anxiety and fear of recurrence, and improving quality of life (Lengacher et al., 2009), this current research proposed to examine and establish the mechanism(s) by which elements of MBSR (i.e. breath awareness, body scan, walking meditation, sitting meditation and yoga) lead to specific clinical improvements. In this realm, and given the significant morbidity induced by fear of cancer recurrence, it is surprising that this pervasive fear has not been examined systematically, in particular, in relation to stress reducing interventions. Therefore, in this study, we adopted the theoretical logic model by Evans (Evans, 1992), a heuristic device for psychosocial research, to postulate and examine how change in fear of recurrence as a result of participation in the MBSR program may mediate a range of positive changes in psychological and physical symptoms and quality of life (Figure 1).
Figure 1.
Hypothesized Biobehavioral Logic Model postulates how change in fear of recurrence as a result of participation in the MBSR program may mediate a range of positive changes in psychological and physical symptoms and quality of life.
METHODS
Sample and Setting
Eighty-four breast cancer survivors were recruited from the H. Lee Moffitt Cancer Center and Research Institute, in Tampa, Florida beginning March 1, 2006 through July 23, 2007. All study subjects had been diagnosed with primary stage 0, I, II, or III breast cancer, had completed treatment within the prior 18 months and were able to read and speak English at the 8th grade level. Exclusion criteria included stage IV breast cancer, mastectomy, severe psychiatric diagnosis (e.g. bipolar disorder), and breast cancer recurrence. Eighty-two of the 84 subjects (97.6%) had complete 6-week follow-up data and form the basis of this analysis.
Study Design and Random Assignment
Subjects were randomly assigned in a 1:1 ratio to either MBSR(BC) or a usual care (UC) group. Randomization was stratified in an unblocked manner using a random number generator by stage of cancer and type of treatment received (radiation alone versus radiation + chemotherapy). Study personnel (excluding the statistician) remained blinded to treatment assignment until a sufficient subgroup of patients (e.g. 10 or more) had been assembled with random assignment subsequently carried out.
Procedures
At orientation, subjects were consented, randomized, and completed baseline assessments. Subjects completed the assessments again within 2 weeks following the 6-week MBSR(BC) program or control period.
Intervention Procedures
Subjects randomized to MBSR(BC) (n=40) attended weekly 2-hour sessions conducted by an MBSR trained psychologist. Participant materials included a training manual and 4 audio tapes for home practice. Home practice consisted of sitting meditation, body scan, walking meditation, and gentle yoga. Subjects were also required to complete a diary on a daily basis documenting home practice which was collected weekly prior to class. The MBSR(BC) intervention is a 6-week program adapted specifically for breast cancer survivors and based upon Kabat-Zinn's 8-week program (Kabat-Zinn, 1990). Participants learn the use of four meditative practices including sitting meditation, walking meditation, body scan, and yoga while integrating mindful attention to self-regulate and manage stressful symptoms (Kabat-Zinn, Lipworth, & Burney, 1985; Teasdale, Segal, & Williams, 1995).
Fidelity
A training manual was developed to maintain the consistency of the intervention. Sessions were standardized and delivered by a single trained psychologist. The program was monitored each week for consistency by an independent observer who recorded the timing of activities and assessed the quality of each session through a qualitative post-observation report.
Compliance
All participants were asked to formally meditate (sitting, walking, body scan) and perform yoga exercises for 15-45 minutes per day 6 days per week for the duration of the 6-week MBSR(BC) program. They were also asked to engage in informal practice for 15-45 minutes per day. Participants recorded their practice in a diary for each day during the 6-week period.
Usual Care (UC) Group
Subjects randomized to the UC group (waitlisted control group) were offered the MBSR(BC) program after the initial 6-week study period.
Measures
In prior published data (Lengacher et al., 2009), we reported that enrollment in the 6-week MBSR(BC) program (compared to UC regimen) was associated with significantly better adjusted post-intervention scores on measures of psychological status and quality of life. Therefore, to assess fear of recurrence as a potential mediator of the effect of the MBSR program, as well as other selected variables (i.e. “how” MBSR(BC) works), we conducted the analysis using 6 outcome measures in which MBSR(BC) demonstrated evidence of efficacy: perceived stress, depressive symptoms, state anxiety, trait anxiety, and aggregate mental and physical health. Fear of recurrence (cancer) was assessed at orientation and within 2 weeks following the 6-week intervention period by the 30-item Concerns about Recurrence Scale. This assessment measures the extent and nature of women's fears about the possibility of breast cancer recurrence in two sections. The first section has four items that assess “worry” related to recurrence, scored as (1) “I don't think about it at all” to (6) “I think about it all the time.” The second section has 26 items that assess the nature of the fear regarding recurrence and extent to which they worry about each item. These items are scored on a five-point Likert scale ranging from (0) not at all, to (4) extremely. Overall, internal consistency reliability is 0.87 for breast cancer subjects (Vickberg, 2003a, 2003b). State and trait anxiety was measured by the State-Trait Anxiety Inventory a two 20-item instrument which measures both state anxiety (present anxiety) and trait anxiety (long term characteristic anxiety); higher scores are indicative of more anxiety – scored from (1) not at all to (4) almost always with possible scores for each scale range from 20 – 80. Internal consistency reliability is 0.95 (Spielberger, 1983). Depression was measured by the Center for Epidemiological Studies Depression Scale (CES-D), a 20-item measure that assesses depressive symptoms during the previous week on a four-point scale ranging from (1) Rarely or none of the time to (4) most or all of the time. Scores range from 0-60 (Radloff, 1977) Alpha coefficient reliability is 0.92 for breast cancer survivors. Optimism was measured by the Life Orientation Test-Revised (LOT-R). This instrument contains 6 target items and 4 filler items that assess expectancy for positive and negative life outcomes on a 5-point Likert scale from (0) strongly disagree to (4) strongly agree. Higher scores indicate better optimism. Coefficient alpha reliability is 0.74-0.78 (Scheier, Carver, & Bridges, 1994). Perceived stress was measured by the 14-item Perceived Stress Scale that assesses how often in the past month one appraises life situations as “stressful.” Higher scores indicate more stress. Items are scored as (0) never to (4) very often, with scores ranging from 0-56. Internal consistency reliability is 0.84-0.86 (Cohen, Kamarck, & Mermelstein, 1983). Quality of life was measured by the Medical Outcomes Studies Short-Form General Health Survey (MOS SF-36), with 36 items that assess Physical Functioning, Physical Role Functioning, Bodily Pain, General Health, Vitality, Social Functioning, Emotional Role Functioning, and Mental Health. Higher scores indicate better quality of life and subscale scores range from 0-100 with higher scores indicating a more favorable health status. Estimated internal consistency scores range from 0.62-0.94 with the majority of scores having exceeded 0.80 (Ware, Snow, Kosinski, & Gandek, 1993). Social support was measured by the Medical Outcomes Social Support Survey, which has 20 items and individual subscales of social support including tangible, affectionate, positive social interactions, and emotional or informational. Higher scores are indicative of more social support. Scores range from (0) none of the time to (5) all of the time with a total range from 0-100. Internal consistency reliability is 0.97 for the full instrument and 0.91-0.96 for the subscales(Sherbourne & Stewart, 1991). Additional measures completed by study subjects have been reported elsewhere (Lengacher et al., 2009). Standard socio-economic demographic data were collected on study subjects to allow for description of the sample on age, gender, ethnicity, highest level of education completed, marital status, income status, and employment status. Clinical history data were collected at baseline and 6 weeks to assess whether there were any new problems, whether treatment related or not. Data were collected on site of cancer diagnosis, date of cancer diagnosis, date treatment ended, number of weeks on radiation, and number of weeks on chemotherapy.
Statistical Methods
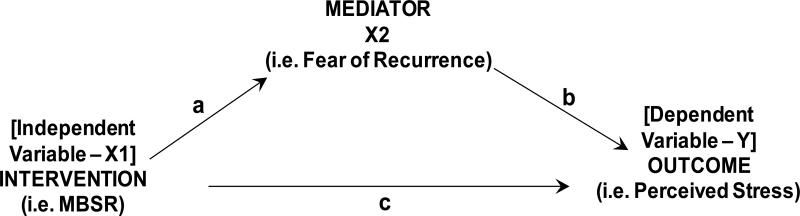
To assess mediation effects, we followed the 3-variable framework described by MacKinnon et al. (MacKinnon, Fairchild, & Fritz, 2007), and as depicted in Figure 2. In this model, MBSR (X1) is assumed to have both a direct and indirect path to the outcome perceived stress (Y). “c” is the direct path, and “a → b” is the indirect path passing through the mediating variable fear of recurrence (X2). Thus, by definition, for fear of recurrence to be a significant mediating variable, the following 2 conditions must be present: (i) the independent variable (X1) is associated with the outcome variable (Y) (i.e. path “c”, as previously reported); and (ii) the independent variable (X1) is associated with the mediating variable (X2) (path “a”). For both mediators and outcomes, we used change (difference) scores between the baseline and 6-week assessments. With respect to mediators, this was done to minimize potential confounding due to small yet possibly influential between-group differences (MBSR(BC) versus control) in baseline values. Because this analysis aimed to examine the relative change in potential mediators following MBSR(BC), both usual care and intervention subjects were required in the analysis (i.e. the full sample as opposed to MBSR(BC) subjects only).
Figure 2.
Three-variable framework used to assess mediation effects. In this model, MBSR (X1) is assumed to have both a direct and indirect path to the outcome perceived stress (Y). “c” is the direct path, and “a → b” is the indirect path passing through the mediating variable fear of recurrence (X2).
Initially, student t-tests were used to compare baseline values of potential mediators by random assignment, followed by use of the Wilcoxon Rank Sum test to compare change in mediating variables reported at 6-week follow-up (i.e. path “a”). Spearman correlation coefficients were calculated to estimate the strength of relationships between 6-week change in potential mediators and 6-week change in outcomes of interest (i.e. path “b”) for the full cohort, irrespective of random assignment. These analyses were followed by use of the Sobel test (Baron & Kenny, 1986) to examine the indirect effect of potential mediating variables (X2) taking into account the direct effect of MBSR(BC) on the outcomes of interest (i.e. “a → b” path). Wilcoxon Rank Sum tests were also used to compare 6-week change in outcome measures by change in mediators dichotomized as above or below the median (i.e. to maximize subgroup statistical power), and then stratified by random assignment.
Finally, since the Concerns about Recurrence Scale does not provide guidelines for estimating “clinically significant” changes in fear of recurrence, we calculated the reliable change index (RCI) using the method proposed by Jacobson, Follette, and Revenstorf (Jacobson, Follette, & Revenstorf, 1984). Specifically, we calculated the difference in change scores for the MBSR(BC) versus usual care group (i.e. pre-post-test scores for each group) and common standard deviation of the difference in change scores. The RCI also takes into account test-retest reliability. Since the time period between pre- and post-testing was lengthy (6-weeks), and the study involved an intervention (i.e. change is expected), we used Cronbach's internal consistency reliability coefficient as an estimate of test-retest reliability.
RESULTS
A previous article details the CONSORT diagram regarding the number of participants recruited, enrolled and lost to follow-up for this study (Lengacher et al., 2011). Although 84 participants were assessed at baseline, 82 completed the follow-up for the study, with a total of n=40 in the MBSR(BC) group and n=42 in the control group. The mean age of the 82 study subjects (with non-missing data) was 57.2 ± 9.2 years with 47 women (57.3%) age 55 or older. Fifty-nine subjects (71.9%) were non-Hispanic White, 9 (11.0%) were Hispanic-White, 10 (12.2%) were non-Hispanic Black, and the remaining 4 (4.9%) were of other race/ethnicity classification. Thirty-six women (43.9%) had a college or professional degree and 57.3% were employed. Clinically, stage of breast cancer was as follows: Stage 0 (17.1%); Stage I (52.4%); Stage II (23.2%); Stage III (7.3%). Thirty-three women (40.2%) were treated with radiation and chemotherapy and the remaining 49 women (59.8%) were treated with radiation only. The median time since treatment completion to study entry was 12.5 weeks and 50% of all women had completed treatment within the past 12 weeks. Prior to MBSR(BC) (or control condition), age was inversely associated with fear of recurrence concerns (r=-0.35, p=0.001) and fear of recurrence problems (r=-0.26, p=0.02). Full baseline and clinical demographics have been previously described elsewhere (Lengacher et al., 2009).
Potential Mediators by Random Assignment (i.e. path “a”)
At baseline, nearly all potential mediators examined had similar mean values by random assignment with the exceptions of mean perceived stress being higher in the control group compared to MBSR(BC) (19.1 versus 16.0, p=0.04), and mean state anxiety being higher in the control group (40.4 versus 35.3, p=0.05) (Table 1). From baseline to 6-weeks, the MBSR(BC) group experienced more favorable changes (differences) than the UC group for several potential mediators including fear of recurrence concerns (2.8 versus 0.2, p=0.007), fear of recurrence problems (11.4 versus 0.2, p=0.02), depression (7.2 versus 4.0, p=0.04), physical functioning (3.8 versus 0.5, p=0.01), and energy (8.8 versus 5.0, p=0.07). Thus, these 5 potential mediators were considered in subsequent analyses. Regarding the relative (between-group) magnitude of change in fear of recurrence, the RCI was 2.13 and 3.02 for fear of recurrence concerns and fear of recurrence problems, respectively. For interpretation, an RCI of ≥1.96 indicates reliable or clinically significant change (Jacobson et al., 1984).
Table 1.
Mean Values of Potential Mediators by Random Assignment (i.e. Path “a”).
| Pre-Intervention | Change at 6-Week Assessment* | |||||
|---|---|---|---|---|---|---|
| Potential Mediator | Control (n=42) | MBSR (n=40) | P-value | Control (n=42) | MBSR (n=40) | P-value |
| Perceived stress | 19.1 (7.2) | 16.0 (6.7) | 0.04 | 3.3 (4.9) | 4.7 (5.0) | 0.16 |
| Fear of recurrence concerns | 11.5 (4.9) | 12.3 (5.0) | 0.49 | 0.2 (4.0) | 2.8 (3.9) | 0.007 |
| Fear of recurrence problems | 36.1 (21.2) | 38.3 (24.6) | 0.67 | 0.2 (18.0) | 11.4 (19.3) | 0.02 |
| Optimism | 42.6 (9.0) | 44.9 (10.0) | 0.28 | 1.6 (7.9) | 2.5 (7.5) | 0.20 |
| Spirituality | 7.1 (2.5) | 7.6 (1.9) | 0.33 | 0.3 (1.8) | 0.1 (1.2) | 0.82 |
| Emotional/information support | 33.0 (6.4) | 33.1 (7.1) | 0.95 | 1.6 (5.0) | -0.1 (4.7) | 0.09 |
| Depression | 14.2 (8.5) | 13.3 (12.0) | 0.71 | 4.0 (1.7) | 7.2 (4.6) | 0.04 |
| State anxiety | 40.4 (11.9) | 35.3 (12.0) | 0.05 | 6.4 (12.1) | 7.8 (9.8) | 0.17 |
| Pain (SF-36) | 48.9 (10.5) | 49.1 (9.7) | 0.92 | 1.3 (6.0) | 3.3 (6.5) | 0.30 |
| Physical functioning (SF-36) | 46.6 (9.6) | 46.3 (9.4) | 0.90 | 0.5 (5.9) | 3.8 (5.5) | 0.01 |
| Energy (SF-36) | 43.5 (11.4) | 45.8 (11.8) | 0.44 | 5.0 (9.4) | 8.8 (10.5) | 0.07 |
| General health (SF-36) | 48.9 (9.7) | 50.3 (9.6) | 0.51 | 1.6 (6.8) | 2.5 (5.7) | 0.38 |
Positive values for baseline to 6-week change represent improvement in psychological, emotional, and physical status. P-values are based on the Wilcoxon Rank Sum test. Values presented are means and standard deviations (parentheses).
Potential Mediators and Outcomes of Interest (i.e. path “b”)
Small to modest statistically significant correlations were observed between several mediators and outcomes of interest (Table 2). This included: (i) change in depression (mediator) being associated with change in perceived stress (r=0.47), state anxiety (r=0.50), trait anxiety (r=0.51), and aggregate mental health (r=0.49); (ii) change in physical functioning (mediator) being associated with change in perceived stress (r=0.43), trait anxiety (r=0.38), and aggregate physical health (r=0.54); and (iii) change in energy (mediator) being associated with change in perceived stress (r=0.45) and aggregate mental health (r=0.59) (p<0.001 for all correlations). Change in fear of recurrence problems (mediator) was associated with change in perceived stress (r=0.34), state anxiety (r=0.34), and trait anxiety (r=0.34) (p<0.01 for all correlations).
Table 2.
Correlation Coefficients Between Potential Mediators and Outcomes of Interest (i.e. Path “b”).
| Outcome Measure (Change from baseline to 6 weeks)(n=82) | ||||||
|---|---|---|---|---|---|---|
| Potential Mediator | Perceived Stress | Depression | State Anxiety | Trait Anxiety | SF-36 Mental Health | SF-36 Physical Health |
| Δ in fear of recurrence concerns | 0.23* | 0.22* | 0.27* | 0.28* | 0.12 | 0.13 |
| Δ in fear of recurrence problems | 0.34** | 0.17 | 0.34** | 0.34** | 0.18 | 0.11 |
| Δ in depression | 0 47*** | ----- | 0.50*** | 0.51*** | 0 49*** | -0.07 |
| Δ in physical functioning (SF-36) | 0.43*** | 0.25* | 0.26* | 0.38*** | 0.01 | 0.54*** |
| Δ in energy (SF-36) | 0.45*** | 0.25* | 0.16 | 0.23* | 0.59*** | 0.27* |
p < 0.05
p < 0.01
p < 0.001.
Indirect Effects of Potential Mediating Variables
After removing direct effects of MBSR(BC) on outcomes of interest (path “c”), the strongest and most consistent evidence for mediating effects (i.e. “how” MBSR(BC) works) was for change in fear of recurrence problems and change in physical functioning. As seen in Table 3, change in fear of recurrence problems mediated the effect of the MBSR(BC) program on 6-week change in perceived stress (z=2.12, p=0.03) and state anxiety (z=2.03, p=0.04). Similarly, change in physical functioning mediated the effect of the MBSR(BC) program on 6-week change in perceived stress (z=2.27, p=0.02) and trait anxiety (z=1.98, p=0.05). Results were similar when stratified by “dose” of MBSR(BC) categorized as below or above the median in total number of minutes practiced (data not shown).
Table 3.
Estimates of Indirect Effects of Potential Mediating Variables.
| Outcome Measure (Change from baseline to 6 weeks)*(n=82) | ||||||
|---|---|---|---|---|---|---|
| Potential Mediating Path | Perceived Stress | Depression | State Anxiety | Trait Anxiety | SF-36 Mental Health | SF-36 Physical Health |
| MBSR → Δ in fear of recurrence concerns → outcome | 1.73 (0.08) | 0.78 (0.40) | 1.67 (0.10) | 0.68 (0.49) | 1.00 (0.32) | 0.03 (0.98) |
| MBSR → Δ in fear of recurrence problems → outcome | 2.12 (0.03) | 1.00 (0.32) | 2.03 (0.04) | 1.59 (0.11) | 1.59 (0.11) | 0.40 (0.69) |
| MBSR → Δ in depressions → outcome | 1.70 (0.09) | ----- | 1.75 (0.08) | 1.76 (0.08) | 1.80 (0.07) | -1.43 (0.15) |
| MBSR → Δ in physical functioning (SF-36) → outcome | 2.27 (0.02) | 1.08 (0.28) | 1.26 (0.21) | 1.98 (0.05) | 0.49 (0.62) | ----- |
| MBSR → Δ in energy (SF-36) → outcome | 1.58 (0.11) | 1.38 (0.17) | 0.96 (0.34) | 1.25 (0.21) | 1.63 (0.10) | 1.31 (0.19) |
Values presented are z-scores and p-values (parentheses) based on the Sobel test
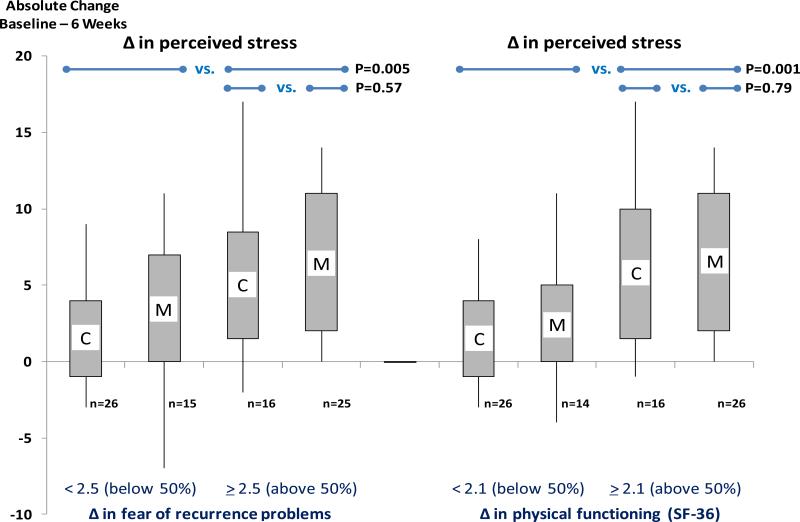
Figures 3 and 4 graphically depict mediating effects of change in fear of recurrence problems and change in physical functioning. Women who experienced a greater reduction in fear of recurrence (i.e. at or above the median value of 2.5 units) experienced greater reduction in change in perceived stress (p=0.005, Figure 3: left side). Of note, even though more women in the MBSR(BC) group experienced a greater mean reduction in fear of recurrence than in the UC group (25 versus 16 women), the concomitant mean change (reduction) in perceived stress was similar (6.0 versus 5.3 units, p=0.57). Similar results were observed for change (improvement) in physical functioning being associated with change (reduction) in perceived stress (Figure 3: right side: p=0.001) irrespective of random assignment.
Figure 3.
Baseline to 6-week changes in perceived stress by random assignment (MBSR (M) versus Usual Care (C)). The data are further stratified by baseline to 6-week change in fear of recurrence (potential mediator) using the median split of <2.5 units versus ≥2.5 units (left side of figure) and change in physical functioning (potential mediator) using the median split of <2.1 units versus ≥2.1 units (right side of figure). The shaded rectangles depict the interquartile range; the lower and upper ends of the vertical lines depict the 5th and 95th percentiles, respectively.
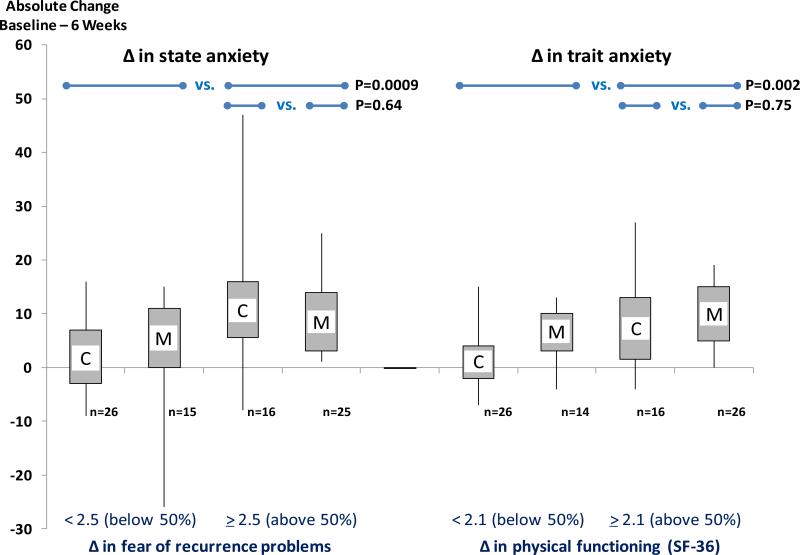
Figure 4.
Baseline to 6-week changes in state anxiety (left side) and trait anxiety (right side) by random assignment (MBSR (M) versus Usual Care (C)). The data are further stratified by baseline to 6-week change in fear of recurrence (potential mediator) using the median split of <2.5 units versus ≥2.5 units (left side of figure) and change in physical functioning (potential mediator) using the median split of <2.1 units versus ≥2.1 units (right side of figure). The shaded rectangles depict the interquartile range; the lower and upper ends of the vertical lines depict the 5th and 95th percentiles, respectively.
As seen in Figure 4 (left side), women who experienced a greater reduction in fear of recurrence (i.e. at or above the median value of 2.5 units) experienced greater reduction in change in state anxiety (p=0.0009). Similarly, women who experienced a greater improvement in physical functioning (i.e. at or above the median value of 2.1 units) experienced greater reduction in change in trait anxiety (p=0.002). Again, even though women in the MBSR(BC) group were more likely to experience large (i.e. above the median) improvements in change in fear of recurrence and change in physical functioning, when women in the UC group experienced such changes, they also experienced improvements in state and trait anxiety.
In total, these results indicate that MBSR(BC) is associated with reduced fear of recurrence and improved physical functioning which, in turn, are associated with reduced perceived stress and state and trait anxiety. However, women in the UC group who experienced reduced fear of recurrence and improved physical functioning (e.g. by mechanisms other than MBSR(BC)) also experienced significantly reduced perceived stress and anxiety.
DISCUSSION
Results from this study provide new insight into the mechanism of action of the MBSR(BC) intervention among breast cancer survivors who are in transition off treatment. This is the first randomized clinical trial to examine fear of recurrence as a potential mediator (i.e. mechanism of action). The majority of research on fear of recurrence among breast cancer survivors has investigated the psychological consequences of fear of recurrence, rather than examining fear of recurrence as a mechanism of action for an intervention by which psychological and physical symptoms may be reduced. Importantly, fear of recurrence is highly prevalent in breast cancer survivors and is associated with considerable psychological distress influenced by both family-related and individual (e.g. treatment experience) concerns (Johnson Vickberg, 2001).
While we examined fear of recurrence as a principal mediator of the MBSR(BC) program, we considered other possible mechanisms (pathways). In aggregate, our results show that among breast cancer survivors who have recently completed treatment, MBSR(BC) leads to both reduced fear of recurrence and improved physical functioning which, in turn, favorably leads to lower levels of perceived stress and anxiety. These results may indicate that one of the mechanisms of how MBSR(BC) works is through the cognitive process of self-regulation of fear of recurrence to improve stress and anxiety and improve physical functioning.
In this realm, it also provides the rationale to examine other outcome measures potentially associated with MBSR(BC), such as measures of immune function (e.g. inflammatory markers) and chronic stress (e.g. telomeres).
Participants in the MBSR(BC) group experienced greater reduction in fear of recurrence concerns, fear of recurrence problems, and depression, as well as improved physical functioning and energy. Such findings of improved physical and psychological status are consistent with other studies among breast cancer patients (Lengacher et al., 2009). Since our study included a usual care group and a MBSR(BC) group, we were able to directly compare changes in measures of fear of recurrence and in turn, changes in measures of psychological symptoms (i.e. potential mechanisms of MBSR). To our knowledge, only one other study has investigated the potential mechanism of MBSR (Nyklicek & Kuijpers, 2008). Participants were sixty males and females from a community in the Netherlands who were experiencing distress. Results showed that mindfulness mediated the positive effects on perceived stress and quality of life in the MBSR group, supporting a partial mediation effect of mindfulness (Nyklicek & Kuijpers, 2008). Our study did not include a direct measure of mindfulness – this precluded us from being able to directly examine mindfulness as a principal mediator of the MBSR(BC) program.
As anticipated, participants in the MBSR(BC) group were more likely than those in the usual care group to experience favorable reductions in fear of recurrence and improved physical functioning. Thus MBSR(BC) may be having a direct effect upon the antecedents that often trigger fear of recurrence, such as physical symptoms and reminders of cancer. Irrespective of random assignment, when participants experienced reductions in fear of recurrence and improved physical functioning, the net influence of these effects on reducing perceived stress and anxiety were similar. Thus, it appears that changes in fear of recurrence and physical functioning mediate changes in stress and anxiety regardless of whether one undergoes an MBSR program, and over time, breast cancer survivors may be expected to experience a general improvement in these mediators. Moreover, since the delivery of this MBSR(BC) program involved considerable time commitment, alternate delivery forms of the MBSR(BC) intervention should be a consideration along with other brief psychotherapy interventions tailored to reduce fear of recurrence for breast cancer survivors.
While fear of recurrence and physical functioning were the strongest mediating variables identified in our analysis, we also observed trends whereby MBSR(BC)-induced reductions in symptoms of depression and improvements in energy level appeared to mediate favorable improvements in both overall mental and physical health. The consistency of these findings provides evidence of clustering of multiple symptoms among breast cancer survivors. Future studies may wish to examine interventions designed to simultaneously reduce multiple (clusters) of symptoms, as opposed to conventional approaches aimed at single symptoms.
Limitations
A limitation of this study is that the sample included only early stage breast cancer survivors who had completed treatment; thus, findings may not generalize to advanced stage cancer patients or survivors of other types of cancer. In addition, as noted above, our study did not include a direct measure of mindfulness which, in concept, may be the principal mediator as to “how” the MBSR program works. Importantly, our study was limited to short-term effects of the MBSR(BC) program (i.e. 6 weeks). The extent to which the MBSR(BC) program at large, as well as initial MBSR-induced reductions in fear of recurrence and improvements in physical functioning impact long-term symptomatology and quality of life among breast cancer survivors is unknown. Finally, the symptoms reported at baseline were generally low for both groups, indicating a potential floor effect with little room for improvement. Therefore, the possibility exists that the effects of MBSR(BC) may be underestimated in the study and it is also possible that this sample did not have sufficiently severe symptoms to test the full extent of the effects of MBSR(BC).
Conclusions
We found that among breast cancer survivors and compared to a usual care control regimen, MBSR(BC) resulted in significant reductions in fear of recurrence and improved physical functioning which, in term, mediated significant reductions in perceived stress and anxiety. Based on an established metric (RCI), the change in fear of recurrence influenced by MBSR(BC) appeared to be reliable and clinically relevant. However, despite the positive effects attributed to the MBSR(BC) program, when control participants experienced reductions in fear of recurrence and improved physical functioning (i.e. less often and through mechanisms other than MBSR(BC)), they too tended to experience reductions in perceived stress and anxiety. These findings reinforce the beneficial health effects of the MBSR(BC) program, and provide a rationale for development of other interventions that aim specifically to reduce fear of recurrence and improve physical functioning after completion of treatment for breast cancer.
Acknowledgments
Support: Supported by the National Institutes of Health, National Cancer Institute: grant number R21CA109168.
Footnotes
Conflict of Interest: The authors have no conflicts to report.
References
- Armes J, Crowe M, Colbourne L, Morgan H, Murrells T, Oakley C, Richardson A. Patients’ supportive care needs beyond the end of cancer treatment: a prospective, longitudinal survey. Journal of Clinical Oncology. 2009;27(36):6172–6179. doi: 10.1200/JCO.2009.22.5151. doi: 10.1200/JCO.2009.22.5151. [DOI] [PubMed] [Google Scholar]
- Baer RA. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology-Science and Practice. 2003;10(2):125–143. doi: 10.1093/clipsy/bpg015. [Google Scholar]
- Baker F, Denniston M, Smith T, West MM. Adult cancer survivors: how are they faring? Cancer. 2005;104(11 Suppl):2565–2576. doi: 10.1002/cncr.21488. doi: 10.1002/cncr.21488. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bishop SR. What do we really know about mindfulness-based stress reduction? Psychosomatic Medicine. 2002;64(1):71–83. doi: 10.1097/00006842-200201000-00010. [DOI] [PubMed] [Google Scholar]
- Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, Devins G. Mindfulness: A proposed operational definition. Clinical Psychology-Science and Practice. 2004;11(3):230–241. doi: 10.1093/clipsy/bph077. [Google Scholar]
- Bohlmeijer E, Prenger R, Taal E, Cuijpers P. The effects of mindfulness-based stress reduction therapy on mental health of adults with a chronic medical disease: a meta-analysis. Journal of Psychosomatic Research. 2010;68(6):539–544. doi: 10.1016/j.jpsychores.2009.10.005. doi: 10.1016/j.jpsychores.2009.10.005. [DOI] [PubMed] [Google Scholar]
- Brown KW, Cordon S. Toward a Phenomenology of Mindfulness: Subjective Experience and Emotional Correlates. In: Didonna F, editor. Clinical Handbook of Mindfulness. Springer Science; New York: 2009. [Google Scholar]
- Brown KW, Ryan RA, Creswell JD. Mindfulness: Theoretical foundations and evidence for its salutary effects. Psychological Inquiry. 2007;18(4):211–237. [Google Scholar]
- Cannon AJ, Darrington DL, Reed EC, Loberiza FR., Jr. Spirituality, patients’ worry, and follow-up health-care utilization among cancer survivors. Journal of Supportive Oncology. 2011;9(4):141–148. doi: 10.1016/j.suponc.2011.03.001. [DOI] [PubMed] [Google Scholar]
- Chambers SK, Foley E, Galt E, Ferguson M, Clutton S. Mindfulness groups for men with advanced prostate cancer: a pilot study to assess feasibility and effectiveness and the role of peer support. Supportive Care in Cancer. 2012;20(6):1183–1192. doi: 10.1007/s00520-011-1195-8. doi: 10.1007/s00520-011-1195-8. [DOI] [PubMed] [Google Scholar]
- Chiesa A, Serretti A. Mindfulness-based stress reduction for stress management in healthy people: a review and meta-analysis. Journal of Alternative and Complementary Medicine. 2009;15(5):593–600. doi: 10.1089/acm.2008.0495. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Connell S, Patterson C, Newman B. Issues and concerns of young Australian women with breast cancer. Supportive Care in Cancer. 2006;14(5):419–426. doi: 10.1007/s00520-005-0003-8. doi: 10.1007/s00520-005-0003-8. [DOI] [PubMed] [Google Scholar]
- Costanzo ES, Lutgendorf SK, Mattes ML, Trehan S, Robinson CB, Tewfik F, Roman SL. Adjusting to life after treatment: distress and quality of life following treatment for breast cancer. British Journal of Cancer. 2007;97(12):1625–1631. doi: 10.1038/sj.bjc.6604091. doi: 10.1038/sj.bjc.6604091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cullen M. Mindfulness: The heart of Buddhist meditation? A conversation with Jan Chozen Bays, Joseph Goldstein, Jan Kabat-Zinn, and Alan Wallace. Inquiring mind. 2006;22(2):4–7. [Google Scholar]
- Curran D, van Dongen JP, Aaronson NK, Kiebert G, Fentiman IS, Mignolet F, Bartelink H. Quality of life of early-stage breast cancer patients treated with radical mastectomy or breast-conserving procedures: results of EORTC Trial 10801. The European Organization for Research and Treatment of Cancer (EORTC), Breast Cancer Co-operative Group (BCCG). European Journal of Cancer. 1998;34(3):307–314. doi: 10.1016/s0959-8049(97)00312-2. [DOI] [PubMed] [Google Scholar]
- Deimling GT, Bowman KF, Sterns S, Wagner LJ, Kahana B. Cancer-related health worries and psychological distress among older adult, long-term cancer survivors. Psychooncology. 2006;15(4):306–320. doi: 10.1002/pon.955. doi: 10.1002/pon.955. [DOI] [PubMed] [Google Scholar]
- Evans ME. Using a model to structure psychosocial nursing [corrected]. Journal of Psychosocial Nursing and Mental Health Services. 1992;30(8):27–32. doi: 10.3928/0279-3695-19920801-10. discussion 32-26. [DOI] [PubMed] [Google Scholar]
- Fredette SL. Breast cancer survivors: concerns and coping. Cancer Nursing. 1995;18(1):35–46. [PubMed] [Google Scholar]
- Girgis A, Boyes A, Sanson-Fisher RW, Burrows S. Perceived needs of women diagnosed with breast cancer: rural versus urban location. Australian and New Zealand Journal of Public Health. 2000;24(2):166–173. doi: 10.1111/j.1467-842x.2000.tb00137.x. [DOI] [PubMed] [Google Scholar]
- Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits. A meta-analysis. Journal of Psychosomatic Research. 2004;57(1):35–43. doi: 10.1016/S0022-3999(03)00573-7. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- Hartl K, Janni W, Kastner R, Sommer H, Strobl B, Rack B, Stauber M. Impact of medical and demographic factors on long-term quality of life and body image of breast cancer patients. Annals of Oncology. 2003;14(7):1064–1071. doi: 10.1093/annonc/mdg289. [DOI] [PubMed] [Google Scholar]
- Hawkins NA, Smith T, Zhao L, Rodriguez J, Berkowitz Z, Stein KD. Health-related behavior change after cancer: results of the American cancer society's studies of cancer survivors (SCS). Journal of Cancer Survivorship. 2010;4(1):20–32. doi: 10.1007/s11764-009-0104-3. doi: 10.1007/s11764-009-0104-3. [DOI] [PubMed] [Google Scholar]
- Herschbach P, Book K, Dinkel A, Berg P, Waadt S, Duran G, Henrich G. Evaluation of two group therapies to reduce fear of progression in cancer patients. Supportive Care in Cancer. 2010;18(4):471–479. doi: 10.1007/s00520-009-0696-1. doi: 10.1007/s00520-009-0696-1. [DOI] [PubMed] [Google Scholar]
- Hodges LJ, Humphris GM. Fear of recurrence and psychological distress in head and neck cancer patients and their carers. Psychooncology. 2009;18(8):841–848. doi: 10.1002/pon.1346. doi: 10.1002/pon.1346. [DOI] [PubMed] [Google Scholar]
- Humphris GM, Rogers S, McNally D, Lee-Jones C, Brown J, Vaughan D. Fear of recurrence and possible cases of anxiety and depression in orofacial cancer patients. International Journal of Oral and Maxillofacial Surgery. 2003;32(5):486–491. [PubMed] [Google Scholar]
- Jacobson NS, Follette WC, Revenstorf D. Psychotherapy Outcome Research - Methods for Reporting Variability and Evaluating Clinical-Significance. Behavior Therapy. 1984;15(4):336–352. [Google Scholar]
- Johnson Vickberg SM. Fears about breast cancer recurrence. Cancer Practice. 2001;9(5):237–243. doi: 10.1046/j.1523-5394.2001.009005237.x. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full-Catastrophe Living: Using the wisdom of your body and mind to face stress, pain and illness. Bantam Doubleday Dell Publishing; New York: 1990. [Google Scholar]
- Kabat-Zinn J. Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology-Science and Practice. 2003;10(2):144–156. doi: DOI 10.1093/clipsy/bpg016. [Google Scholar]
- Kabat-Zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. Journal of Behavioral Medicine. 1985;8(2):163–190. doi: 10.1007/BF00845519. [DOI] [PubMed] [Google Scholar]
- Kornblith AB, Powell M, Regan MM, Bennett S, Krasner C, Moy B, Winer E. Long-term psychosocial adjustment of older vs younger survivors of breast and endometrial cancer. Psychooncology. 2007;16(10):895–903. doi: 10.1002/pon.1146. doi: 10.1002/pon.1146. [DOI] [PubMed] [Google Scholar]
- Lee-Jones C, Humphris G, Dixon R, Hatcher MB. Fear of cancer recurrence--a literature review and proposed cognitive formulation to explain exacerbation of recurrence fears. Psychooncology. 1997;6(2):95–105. doi: 10.1002/(SICI)1099-1611(199706)6:2<95::AID-PON250>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- Lengacher CA, Johnson-Mallard V, Post-White J, Moscoso MS, Jacobsen PB, Klein TW, Kip KE. Randomized controlled trial of mindfulness-based stress reduction (MBSR) for survivors of breast cancer. Psychooncology. 2009;18(12):1261–1272. doi: 10.1002/pon.1529. doi: 10.1002/pon.1529. [DOI] [PubMed] [Google Scholar]
- Lengacher CA, Kip KE, Post-White J, Fitzgerald S, Newton C, Barta M, Klein TW. Lymphocyte Recovery After Breast Cancer Treatment and Mindfulness-Based Stress Reduction (MBSR) Therapy. Biological Research for Nursing. 2011 doi: 10.1177/1099800411419245. doi: 10.1177/1099800411419245. [DOI] [PubMed] [Google Scholar]
- Llewellyn CD, Weinman J, McGurk M, Humphris G. Can we predict which head and neck cancer survivors develop fears of recurrence? Journal of Psychosomatic Research. 2008;65(6):525–532. doi: 10.1016/j.jpsychores.2008.03.014. doi: 10.1016/j.jpsychores.2008.03.014. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mast ME. Survivors of breast cancer: illness uncertainty, positive reappraisal, and emotional distress. Oncology Nursing Forum. 1998;25(3):555–562. [PubMed] [Google Scholar]
- Matchim Y, Armer JM. Measuring the psychological impact of mindfulness meditation on health among patients with cancer: a literature review. Oncology Nursing Forum. 2007;34(5):1059–1066. doi: 10.1188/07.ONF.1059-1066. doi: 10.1188/07.ONF.1059-1066. [DOI] [PubMed] [Google Scholar]
- Matthews BA. Role and gender differences in cancer-related distress: a comparison of survivor and caregiver self-reports. Oncology Nursing Forum. 2003;30(3):493–499. doi: 10.1188/03.ONF.493-499. doi: 10.1188/03.ONF.493-499. [DOI] [PubMed] [Google Scholar]
- Mehnert A, Berg P, Henrich G, Herschbach P. Fear of cancer progression and cancer-related intrusive cognitions in breast cancer survivors. Psychooncology. 2009;18(12):1273–1280. doi: 10.1002/pon.1481. doi: 10.1002/pon.1481. [DOI] [PubMed] [Google Scholar]
- Mehta SS, Lubeck DP, Pasta DJ, Litwin MS. Fear of cancer recurrence in patients undergoing definitive treatment for prostate cancer: results from CaPSURE. Journal of Urology. 2003;170(5):1931–1933. doi: 10.1097/01.ju.0000091993.73842.9b. doi: 10.1097/01.ju.0000091993.73842.9b. [DOI] [PubMed] [Google Scholar]
- Minton O, Stone P. How common is fatigue in disease-free breast cancer survivors? A systematic review of the literature. Breast Cancer Research and Treatment. 2008;112(1):5–13. doi: 10.1007/s10549-007-9831-1. doi: 10.1007/s10549-007-9831-1. [DOI] [PubMed] [Google Scholar]
- Musial F, Bussing A, Heusser P, Choi KE, Ostermann T. Mindfulness-based stress reduction for integrative cancer care - a summary of evidence. Forschende Komplementarmedizin. 2011;18(4):192–202. doi: 10.1159/000330714. doi: 10.1159/000330714. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute Surveillance Epidemiology and End Results. 2010 Cancer Statistics from http://seer.cancer.gov/statistics/
- Nyklicek I, Kuijpers KF. Effects of mindfulness-based stress reduction intervention on psychological well-being and quality of life: is increased mindfulness indeed the mechanism? Annals of Behavioral Medicine. 2008;35(3):331–340. doi: 10.1007/s12160-008-9030-2. doi: 10.1007/s12160-008-9030-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oxlad M, Wade TD, Hallsworth L, Koczwara B. ‘I'm living with a chronic illness, not . . . dying with cancer’: a qualitative study of Australian women's self-identified concerns and needs following primary treatment for breast cancer. European Journal of Cancer Care (English Language Edition) 2008;17(2):157–166. doi: 10.1111/j.1365-2354.2007.00828.x. doi: 10.1111/j.1365-2354.2007.00828.x. [DOI] [PubMed] [Google Scholar]
- Perlman DM, Salomons TV, Davidson RJ, Lutz A. Differential Effects on Pain Intensity and Unpleasantness of Two Meditation Practices. Emotion. 2010;10(1):65–71. doi: 10.1037/a0018440. doi: 10.1037/A0018440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polinsky ML. Functional status of long-term breast cancer survivors: demonstrating chronicity. Health and Social Work. 1994;19(3):165–173. doi: 10.1093/hsw/19.3.165. [DOI] [PubMed] [Google Scholar]
- Radloff L. The CES-D scale: A self-report depression scale for researching the general population. Application of Psychological Measures. 1977;1:385–401. [Google Scholar]
- Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. Journal of Personality and Social Psychology. 1994;67(6):1063–1078. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- Schmid-Buchi S, Halfens RJ, Dassen T, van den Borne B. A review of psychosocial needs of breast-cancer patients and their relatives. Journal of Clinical Nursing. 2008;17(21):2895–2909. doi: 10.1111/j.1365-2702.2008.02490.x. doi: 10.1111/j.1365-2702.2008.02490.x. [DOI] [PubMed] [Google Scholar]
- Shapiro SL, Oman D, Thoresen CE, Plante TG, Flinders T. Cultivating mindfulness: Effects on well-being. Journal of Clinical Psychology. 2008;64(7):840–862. doi: 10.1002/jclp.20491. [DOI] [PubMed] [Google Scholar]
- Sherbourne CD, Stewart AL. The MOS social support survey. Social Science and Medicine. 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- Simard S, Savard J, Ivers H. Fear of cancer recurrence: specific profiles and nature of intrusive thoughts. Journal of Cancer Survivorship. 2010;4(4):361–371. doi: 10.1007/s11764-010-0136-8. doi: 10.1007/s11764-010-0136-8. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, Luschene RE. Manual for the State-trait Anxiety Inventory. Consulting Psychologists; Palo Alto, CA: 1983. [Google Scholar]
- Stanton AL, Ganz PA, Rowland JH, Meyerowitz BE, Krupnick JL, Sears SR. Promoting adjustment after treatment for cancer. Cancer. 2005;104(11 Suppl):2608–2613. doi: 10.1002/cncr.21246. doi: 10.1002/cncr.21246. [DOI] [PubMed] [Google Scholar]
- Stephens PA, Osowski M, Fidale MS, Spagnoli C. Identifying the educational needs and concerns of newly diagnosed patients with breast cancer after surgery. Clinical Journal of Oncology Nursing. 2008;12(2):253–258. doi: 10.1188/08.CJON.253-258. doi: 10.1188/08.CJON.253-258. [DOI] [PubMed] [Google Scholar]
- Teasdale JD, Segal Z, Williams JM. How does cognitive therapy prevent depressive relapse and why should attentional control (mindfulness) training help? Behaviour Research and Therapy. 1995;33(1):25–39. doi: 10.1016/0005-7967(94)e0011-7. [DOI] [PubMed] [Google Scholar]
- van den Beuken-van Everdingen MH, Peters ML, de Rijke JM, Schouten HC, van Kleef M, Patijn J. Concerns of former breast cancer patients about disease recurrence: a validation and prevalence study. Psychooncology. 2008;17(11):1137–1145. doi: 10.1002/pon.1340. doi: 10.1002/pon.1340. [DOI] [PubMed] [Google Scholar]
- Vickberg SM. The Concerns About Recurrence Scale (CARS): a systematic measure of women's fears about the possibility of breast cancer recurrence. Ann Behav Med. 2003a;25(1):16–24. doi: 10.1207/S15324796ABM2501_03. [DOI] [PubMed] [Google Scholar]
- Vickberg SM. The Concerns About Recurrence Scale (CARS): a systematic measure of women's fears about the possibility of breast cancer recurrence. Annals of Behavioral Medicine. 2003b;25(1):16–24. doi: 10.1207/S15324796ABM2501_03. [DOI] [PubMed] [Google Scholar]
- Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 survey manual and interpretation guide. New England Medical Center, The Health Institute; Boston: 1993. [Google Scholar]
- Young KE, White CA. The prevalence and moderators of fatigue in people who have been successfully treated for cancer. Journal of Psychosomatic Research. 2006;60(1):29–38. doi: 10.1016/j.jpsychores.2005.03.011. doi: 10.1016/j.jpsychores.2005.03.011. [DOI] [PubMed] [Google Scholar]