Abstract
Challenges to health care access in the US are forcing local policymakers and service delivery systems to find novel ways to address the shortage of primary care clinicians. The uninsured and underinsured face the greatest obstacles in accessing services. Geographic information systems mapping software was used to illustrate health disparities in Alachua County, FL; galvanize a community response; and direct reallocation of resources.
The University of Florida Family Data Center created “hot spot” density maps of important health and social indicators to highlight the location of disparities at the neighborhood level. Maps were produced for Medicaid births, teen births, low birth weight, domestic violence incidents, child maltreatment reports, unexcused school absences, and juvenile justice referrals. Maps were widely shared with community partners, including local elected officials, law enforcement, educators, child welfare agencies, health care providers, and service organizations. This data sharing resulted in advocacy efforts to bring resources to the greatest-need neighborhoods in the county. Novel public-private partnerships were forged between the local library district, children and family service providers, and university administrators. Two major changes are detailed: a family resource center built in the neighborhood of greatest need and a mobile clinic staffed by physicians, nurses, physician assistants, health educators, and student and faculty volunteers.
Density maps have several advantages. They require minimal explanation. Anyone familiar with local geographic features can quickly identify locations displaying health disparities. Personalizing health disparities by locating them geographically allows a community to translate data to action to improve health care access.
Introduction
Communities around the country are struggling to address the health care needs of residents. Job loss, reductions in employer-sponsored health insurance, and escalating costs of health insurance have left many uninsured. At the same time, safety net health care providers have limited capacity to provide primary care and health promotion and disease prevention services. With the passage of the Patient Protection and Affordable Care Act,1 demand for nonurgent health care access will rise; therefore, communities will need to address local needs for primary care.
The Institute of Medicine (IOM) convened a committee in 1997 to draft a set of indicators useful for monitoring community health improvement efforts.2 Supported by the US Department of Health and Human Services and the Robert Wood Johnson Foundation in Princeton, NJ, the committee produced a resource that has proved useful to local policy-makers dealing with the rapidly shifting health care landscape. Using monitoring parameters suggested by the IOM, communities can determine current health status of the population, establish goals to improve health outcomes, address observed health disparities, and assess progress toward achieving goals. Since publication of the IOM report, geographic information systems (GIS) mapping software has become widely available, providing a useful adjunct to tabulated population statistics in determining where to invest scarce resources for the greatest improvement in health care access.
Collecting local data and using GIS mapping software to display information in maps is a process that has increasingly been undertaken by communities in partnership with the agencies that supply the information. Maps are being used to depict the health characteristics of neighborhoods and identify specific areas with unmet needs.3–7 Barnard and Hu8 specify a cyclical framework of population identification, population health assessment, and description of existing service utilization and distribution to enable community members and local policymakers to interact with maps to address identified needs.
The use of GIS in decision support is now a mature field.9 Numerous authors have cited the potential of maps to characterize neighborhoods and engage individuals.10–15 However, few articles review the consequences of engaging community members by means of maps. We report here on the process and consequences of creating “hot spot” density maps as a means to engage the community of Alachua County, FL, to address health disparities. Display of maps of Alachua County spurred collaborative action between the University of Florida (UF) Health Science Center in Gainesville, FL, and city and county governments, local and regional public and private service providers, and community members. Successful formation of these partnerships between an academic health center and local agencies and government was the first step in engaging the community to improve health.16 Together, a host of novel interventions were implemented that led to greater access to health care and social services.
Methods
Setting
Alachua County is located in North Central Florida, with an estimated population in 2011 of 294,365. Gainesville (2010 population of 124,354) is the county seat and home to the UF, which has an annual enrollment of nearly 50,000 students. The large student population skews the demographic profile of Alachua County toward college-aged young adults, which is particularly relevant in health planning because students have access to high-quality health care on campus. The student population results in lower-than-average county rates of chronic illness and death. Growth in Alachua County has not been evenly distributed; the areas west and northwest of the UF campus have added more students and grown much faster than the rest of the county. Hence, the characteristics of subcounty areas or neighborhoods were important to ensure that local inequities in health outcomes would be detected.
Data Collection and Analysis
Descriptive statistics were gathered from publicly available national, state, and local data systems such as the US Census Bureau; Baltimore, Maryland-based Annie E Casey Foundation’s Kids Count; and the Florida Department of Health’s Community Health Assessment Resource Tool Set (CHARTS). Data were also obtained from a local health-planning agency (WellFlorida Council, Gainesville), on demographics, socioeconomic characteristics, and health outcomes for residents of Alachua County and its subcounty geographic units. The demographic and socioeconomic indicators included total population, percentage of persons 25 years and older without a high school diploma, median household income, percentage of population in poverty, and percentage of families headed by a single parent. The health indicators collected included births to women whose pregnancy and delivery care was paid for by Medicaid, low-birth-weight births, infant mortality, rates of sexually transmitted infection, child maltreatment, and death rates by selected causes (diabetes, heart disease, cancer, stroke, homicide, suicide, motor vehicle crash). Geocoded birth records were obtained from the Florida Department of Health and were linked by the UF Family Data Center to Florida Agency for Health Care Administration records to determine Medicaid status. The Family Data Center linked birth records to data from the Florida Department of Children and Families to ascertain the initial health status of children who were subsequently maltreated.
The Family Data Center used deterministic and probabilistic record linkage methods17 to produce a dataset with only point location coordinates derived from geocoding the mother’s address in the birth certificate. Records were exported into ArcGIS 9.3 software (Esri International; Redlands, CA) and projected onto an Alachua County census block group map using Albers projection.18 A census block group is a compact, contiguous cluster of geographic statistical units used to tabulate population data. To mask point location, the ArcGIS Spatial Analyst Kernel density estimation tool19 was used with a search radius of 1.6 km2 (1 square mile) with natural breaks used for color classification.20
Zip codes and census tract block groups were selected as the subcounty geographic unit of interest because they allow neighborhoods to be easily identified by local residents. Health disparity measures, as recommended by the IOM report, were displayed in tabular form for the county as a whole and for 16 zip codes. Zip codes associated with residence halls on the UF campus were excluded because students have access to on-campus student health care. This restriction helps correct for the impact of the student population on countywide outcome measures. Density maps of health indicators were generated for count data using a graded color ramp to indicate degree of prevalence. The density maps by census block group highlighted conditions in neighborhoods that had been hidden in the zip code-level tabular data.
The hot spot density maps were enlarged to poster size and shared … at more than 20 public venues.
Community Engagement
The maps were brought to bear in this project as part of community engagement. The hot spot density maps were enlarged to poster size and shared widely in the community. Over a 12-month period, they were viewed at more than 20 public venues. At each venue, Family Data Center staff accompanied the maps to provide an overview, highlight major findings, and answer questions. Audiences, totaling more than 1000 individuals, included the county school district leadership, county health department officials, county library branch managers, law enforcement officers, legal aid agencies, the county health care advisory board, Gainesville city mayor, county commissioners, city and county government staff, United Way of North Central Florida, Rotary International and Kiwanis International clubs, service providers, and advocacy organizations in the area.
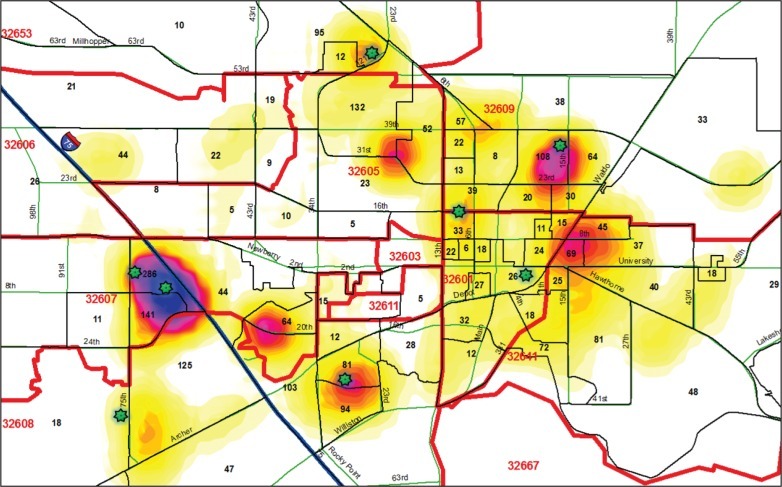
At the UF, maps were shared with the administrators of the College of Medicine Health Science Center and Shands hospital system, faculty, and student service organizations. The density maps captured the attention of both lay and professional audiences familiar with local geography. Although most community members had a grasp of health care access issues and health disparities in east Gainesville, the hot spot density maps (Figures 1 and 2) revealed areas of need in west Gainesville.
Figure 1.
Medicaid birth density and count by census block group (2007–2009). Blue and purple colors indicate higher concentration of Medicaid-paid births in that geographic area. Numbers in the block groups outlined with solid black lines indicate births to women who qualified for Medicaid during the time period. Red numbers indicate zip codes. Stars indicate location of mobile clinic bus stops.
Figure 2.
Density maps of child abuse and neglect (2005–2008) and domestic violence (2009). Left density map displays confirmed cases of child maltreatment, including abuse and neglect. Child abuse may involve physical, sexual, or emotional abuse. Right density map shows calls to law enforcement for domestic violence incidents in the Gainesville, FL, area in 2009. Domestic violence includes “domestic disturbance” and “domestic battery.” Battery can involve any dangerous weapon, including a hand or a fist.
In addition to sharing maps, assessment of services available in west Gainesville revealed that only hospital Emergency Departments were available to uninsured adults after hours, and only pediatric patients had medical homes. When the major pediatric physician in west Gainesville closed his doors, thousands of children were left without a medical home. No churches or stores were located in the largest hot spot, and the single licensed child care center, with a capacity of 50 children, also closed. For a resident of the hot spot area, a trip to the county health department in east Gainesville entails a 90-minute bus ride each way involving 2 transfers. Home visitation program providers and law enforcement officers expressed awareness and concern for the residents of this isolated neighborhood, but had not realized that other service providers shared this concern.
Results
Numerous actions occurred in the two years following the initial sharing of the density maps and assessment of services. In response to two presentations made to the county commission at which the hot spot maps were displayed, public service provider grantees were directed to pay greater attention to the area. United Way also asked its grantee agencies to consider extending services to the underserved area. The UF Department of Pediatrics relocated and expanded its clinic facility in west Gainesville. United Way and the public library system formed a steering committee with the Partnership for Strong Families, the local agency in Gainesville for Department of Children and Families’ child abuse prevention and foster care services. The steering committee also included UF faculty members and neighborhood advocates. The purpose of the committee was to seek solutions to the unmet needs of the hot spot neighborhood. A site for neighborhood-level service provision was sought. Expansion of the existing library space to include social service providers was considered. Both options required local, state, and federal funding, and steering committee members explored potential sites and funding.
Residents of the affluent areas of west Gainesville that surrounded the hot spot became concerned that their neighbors were being overlooked in the distribution of local safety net funds. With assistance from the Alachua County Sheriff’s Department community outreach staff, a grassroots organization, the Southwest Advocacy Group, was formed. This resident-led group drafted action plans to address the challenges of living in southwest Gainesville. The advocacy work of the Southwest Advocacy Group kept the maps at the forefront of public discussion and persuaded the county commission to purchase 2 buildings to serve as a neighborhood resource and health services center. The public-private steering committee strongly supported this action. Since its opening in June 2012, the resource center has offered family support services from more than 40 providers. Services include family literacy, legal aid, recreation, and parent support. The local health department agreed to renovate, staff, and operate the second building with funds made available by the county commission and local Rotary clubs.
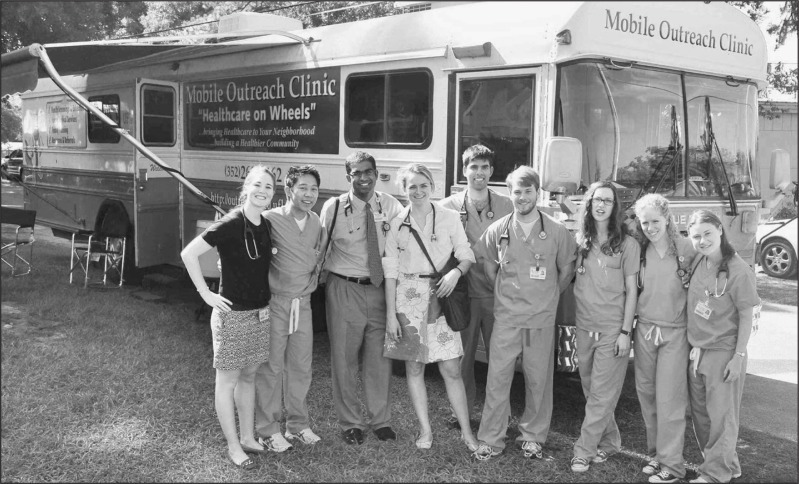
Until funding for the health clinic location could be secured, the county Health Department offered a family nurse practitioner to provide well-woman care and primary care if the collaborators could secure a facility. The university donated a “retired” Mobile Outreach Clinic that had been previously used to deliver prenatal care in rural Florida counties. The 11.1-m (37-ft) 1992 Blue Bird bus is equipped with 2 examination rooms, a restroom, a workup/laboratory station, and a counseling area. The UF medical student-run free clinic, Equal Access, solicited donations of equipment from members of the Alachua County Medical Society, and opened a weekly evening clinic in January 2010. In partnership with the nearby public library, students were granted weekly access to the library common space for intake. Medical students recruited local physicians, nurses, legal aid attorneys, law students, and social workers to volunteer. Dental students, pharmacy students, and physical therapy students provided services in the library’s common area.
In February 2010, the local health safety net taxing district (CHOICES in Gainesville) and the UF College of Medicine began aiding efforts of the Mobile Clinic. This support resulted in enlarging the Mobile Clinic’s capacity to deliver roughly 3000 primary care visits per year in hot spots identified by the maps. When the Mobile Clinic opened, undergraduate student organizations began supplying volunteers and the College of Nursing began participating to fulfill its community nursing education requirement. The Mobile Clinic has become a hands-on classroom, educating pre-professional and health professional students on care for the underserved. The mobile clinic delivered 4300 primary care services in Fiscal Year 2010 to 2011, and it is projected to deliver 5000 in 2011 to 2012 (Figure 3).
Figure 3.
Medical students staffing the Mobile Outreach Clinic. The Mobile Clinic visits neighborhood health-disparity hot spots weekly. More than 100,000 volunteer hours resulted in 4300 primary care services being delivered in Fiscal Year 2010–2011.
Left to right: Lauren Cooper, Neil Wingkun, Vikram Narayan, Elizabeth Byrne, Zahid Iqbal, Blaine Farmer, Sara Rodriguez, Melanie Adamsky, and Jennifer Goetz
In addition to operating five days a week, the Mobile Clinic is used for health fairs on weekends. During health fairs, the Mobile Clinic staff and volunteers administer free health screenings and provide health education and referrals to local safety net resources. The Mobile Clinic’s monthly calendar is posted online.21 The Mobile Clinic visits 8 locations weekly (see stars in Figure 1). Most of these locations are apartment complexes and neighborhood branch libraries specifically selected to address the health disparities in the hot spots portrayed on the GIS maps. Bringing the Mobile Clinic directly to neighborhoods diminishes the transportation barrier many patients face. At some clinic locations, the percentage of patients who walk to the bus is as high as 75%. These uninsured patients without transportation are no longer isolated from access to health care services.
Discussion
The approach that collaborators in Alachua County took is an example of community health profiling; the community is the overarching context in which all health-related variables coexist and interact, revealing the multilevel, ecologic links between people and environments.22,23 The process began with a commitment by the UF College of Medicine to assess local health disparities. The original health report and maps were created by College of Medicine faculty and staff who, while sharing health information, were, in return, given community-based education, law enforcement, and social service provider data to analyze. What was distinctive about the community health profiling in Alachua County was the extent to which GIS hot spot maps affected the entire process from beginning to end. Maps provided community residents, civic officials, and university faculty, staff, and students with information about locations of greatest need. Community partners contributed their knowledge of long-standing barriers as well as resources needed for improving health care and social services access. The repeated display of health-disparity hot spot maps ensured that multiple audiences could quickly interpret prevalence and trends. These visual representations required almost no narrative or explanation. The maps generated responses to conditions in a way that past tabular display of information did not.
The maps brought disparate groups together, a key achievement since no one organization is capable of solving complex social and health disparities.24 Because viewers could quickly identify the geographic locations depicted, local partners were able to contribute their knowledge about neighborhood assets, bus line access, pockets of poverty, and services needed or currently provided. Maps helped community members maintain attention and engagement of government officials to reallocate resources to specific neighborhoods.
With the opening of the Southwest Advocacy Group resource center and the expansion of the mobile clinic, the partnership of clients and providers will now shift to evaluating and continuously improving these assets to ensure their sustainability. GIS mapping will continue to play a vital role in this process because it can illustrate changes over time in the demographic, socioeconomic, and health indicators of neighborhoods. Maps therefore will play a key role in examining outcomes.
We are already observing high patient satisfaction with the care provided, and within one year, expect to see early indicators of health status improvement such as fewer teen pregnancies and fewer low-birth-weight infants in the neighborhood locations served. The work is far from done, and community partners continue planning for the provision of high-quality child care and employment opportunities for parents. Priorities have been and continue to be set by the community.
Conclusion
This project demonstrated how mapping of health disparities improved the delivery of primary care to residents of neighborhoods lacking access to health care.25,26 Maps provided the evidence for unmet health care and social service needs in Alachua County, FL. Hot spot maps can play a key role in galvanizing action because of their unique capacity through shape, color, and pattern to convey information at a visceral level. Neighborhood-level maps alert stakeholders to the presence of health inequities and can generate the stimulus for addressing areas of greatest need.
Acknowledgments
Kathleen Louden, ELS, of Louden Health Communications provided editorial assistance.
Footnotes
Disclosure Statement
This study was funded in part by the Jessie Ball duPont Fund and the University of Florida. The author(s) have no other conflicts of interest to disclose.
The Most Difficult Problem
Let us hope that when some … student of this confused and disconcerting period in our history comes to tell of it, he will be able to say that at the very time when such progress in their subjects was being made as never before, … the scientists and the engineers of the country temporarily abandoned the investigations dear to their hearts … to concentrate on problems the most difficult of all to solve—those that have to do with the social well-being of the community at large.
– Harvey Cushing, 1869–1939, American neurosurgeon, pioneer of neurosurgery
References
- 1.The Patient Protection and Affordable Care Act of 2010. Public Law 111-148, 111th Congress, 124 Stat 119, HR 3590, enacted 2010 Mar 23
- 2.Committee on Using Performance Monitoring to Improve Community Health, Institute of Medicine. Durch JS, Bailey LA, Stoto MA. Improving health in the community: a role for performance monitoring. Washington, DC: The National Academies Press; 1997. [PubMed] [Google Scholar]
- 3.Kruger DJ, Brady JS, Shirey LA. Using GIS to facilitate community-based public health planning of diabetes intervention efforts. Health Promot Pract. 2008 Jan;9(1):76–81. doi: 10.1177/1524839906293396. DOI: http://dx.doi.org/10.1177/1524839906293396. [DOI] [PubMed] [Google Scholar]
- 4.Cromley EK. GIS and disease. Annu Rev Public Health. 2003;24:7–24. doi: 10.1146/annurev.publhealth.24.012902.141019. DOI: http://dx.doi.org/10.1146/annurev.publhealth.24.012902.141019. [DOI] [PubMed] [Google Scholar]
- 5.Beyer KM, Rushton G. Mapping cancer for community engagement. Prev Chronic Dis. 2009 Jan;6(1):A03. [PMC free article] [PubMed] [Google Scholar]
- 6.Plescia M, Koontz S, Laurent S. Community assessment in a vertically integrated health care system. Am J Public Health. 2001 May;91(5):811–4. doi: 10.2105/ajph.91.5.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pearce J, Witten K, Bartie P. Neighbourhoods and health: a GIS approach to measuring community resource accessibility. J Epidemiol Community Health. 2006 May;60(5):389–95. doi: 10.1136/jech.2005.043281. DOI: http://dx.doi.org/10.1136/jech.2005.043281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barnard DK, Hu W. The Population Health Approach: health GIS as a bridge from theory to practice. Int J Health Geogr. 2005 Oct 6;4:23. doi: 10.1186/1476-072X-4-23. DOI: http://dx.doi.org/10.1186/1476-072X-4-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Malczewski J. GIS-based multicriteria decision analysis: a survey of the literature. Int J Geogr Inf Sci. 2006 Aug;20(7):703–26. DOI: http://dx.doi.org/10.1080/13658810600661508. [Google Scholar]
- 10.Caley LM.Using geographic information systems to design population-based interventions Public Health Nurs 2004November–Dec216547–54.DOI: http://dx.doi.org/10.1111/j.0737-1209.2004.21607.x Erratum in: Public Health Nurs 2005 Mar–Apr;22(2):186 [DOI] [PubMed] [Google Scholar]
- 11.Scotch M, Parmanto B, Gadd CS, Sharma RK. Exploring the role of GIS during community health assessment problem solving: experiences of public health professionals. Int J Health Geogr. 2006 Sep 18;5:39. doi: 10.1186/1476-072X-5-39. DOI: http://dx.doi.org/10.1186/1476-072X-5-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schuurman N, Leight M, Berube M. A Web-based graphical user interface for evidence-based decision making for health care allocations in rural areas. Int J Health Geogr. 2008 Sep 15;7:49. doi: 10.1186/1476-072X-7-49. DOI: http://dx.doi.org/10.1186/1476-072X-7-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aronson RE, Wallis AB, O’Campo PJ, Schafer P. Neighborhood mapping and evaluation: a methodology for participatory community health initiatives. Matern Child Health J. 2007 Jul;11(4):373–83. doi: 10.1007/s10995-007-0184-5. DOI: http://dx.doi.org/10.1007/s10995-007-0184-5. [DOI] [PubMed] [Google Scholar]
- 14.Beyer KM, Comstock S, Seagren R. Disease maps as context for community mapping: a methodological approach for linking confidential health information with local geographical knowledge for community health research. J Community Health. 2010 Dec;35(6):635–44. doi: 10.1007/s10900-010-9254-5. DOI: http://dx.doi.org/10.1007/s10900-010-9254-5. [DOI] [PubMed] [Google Scholar]
- 15.Sage WM, Balthazar M, Kelder S, Millea S, Pont S, Rao M.Mapping data shape community responses to childhood obesity Health Aff (Millwood) 2010March–Apr293498–502.DOI: http://dx.doi.org/10.1377/hlthaff.2010.0153 [DOI] [PubMed] [Google Scholar]
- 16.Michener L, Cook J, Ahmed SM, Yonas MA, Coyne-Beasley T, Aguilar-Gaxiola S. Aligning the goals of community-engaged research: why and how academic health centers can successfully engage with communities to improve health. Acad Med. 2012 Mar;87(3):285–91. doi: 10.1097/ACM.0b013e3182441680. DOI: http://dx.doi.org/10.1097/ACM.0b013e3182441680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blakely T, Salmond C. Probabilistic record linkage and a method to calculate the positive predictive value. Int J Epidemiol. 2002 Dec;31(6):1246–52. doi: 10.1093/ije/31.6.1246. DOI: http://dx.doi.org/10.1093/ije/31.6.1246. [DOI] [PubMed] [Google Scholar]
- 18.Snyder JP. Map projections: a working manual US Geological Survey Professional Paper: 1395 [monograph on the Internet] Washington, DC: US Government Printing Office; 1987. [cited 2012 Oct 10]. Available from: http://pubs.er.usgs.gov/publication/pp1395. [Google Scholar]
- 19.Silverman BW. Density estimation for statistics and data analysis. New York, NY: Chapman and Hall/CRC; 1986. [Google Scholar]
- 20.Jenks GF. The data model concept in statistical mapping. In: Frenzel K, editor. International yearbook of cartography. Vol. 7. Skokie, IL: Rand McNally; 1967. pp. 186–90. [Google Scholar]
- 21. outreach.med.ufl.edu [homepage on the Internet] Gainesville, FL: University of Florida College of Medicine; c2012 [updated 2012 Oct 5; cited 2012 Oct 16]. Available from: http://outreach.med.ufl.edu. [Google Scholar]
- 22.Mullner RM, Chung K, Croke KG, Mensah EK. Geographic information systems in public health and medicine. J Med Syst. 2004 Jun;28(3):215–21. doi: 10.1023/b:joms.0000032972.29060.dd. DOI: http://dx.doi.org/10.1023/B:JOMS.0000032972.29060.dd. [DOI] [PubMed] [Google Scholar]
- 23.Nykiforuk CI, Flaman LM. Geographic information systems (GIS) for health promotion and public health: a review. Health Promot Pract. 2011 Jan;12(1):63–73. doi: 10.1177/1524839909334624. DOI: http://dx.doi.org/10.1177/1524839909334624. [DOI] [PubMed] [Google Scholar]
- 24.Lasker RD, Weiss ES, Miller R, Community-Campus Partnerships for Health Promoting collaborations that improve health. Educ Health (Abingdon) 2001;14(2):163–72. doi: 10.1080/13576280110051046. [DOI] [PubMed] [Google Scholar]
- 25.McLafferty SL. GIS and health care. Annu Rev Public Health. 2003;24:25–42. doi: 10.1146/annurev.publhealth.24.012902.141012. DOI: http://dx.doi.org/10.1146/annurev.publhealth.24.012902.141012. [DOI] [PubMed] [Google Scholar]
- 26.Dulin MF, Ludden TM, Tapp H, et al. Using Geographic Information Systems (GIS) to understand a community’s primary care needs J Am Board Fam Med 2010January–Feb23113–21.DOI: http://dx.doi.org/10.3122/jabfm.2010.01.090135 [DOI] [PubMed] [Google Scholar]