Abstract
Objectives
To assess the reliability of maternally recalled birthweight and size in Entebbe, Uganda.
Methods
The study population comprised 404 mothers, who were participants in the Entebbe Mother and Baby Study (EMaBS). Mothers were recruited to EMaBS during antenatal care, maternal characteristics were recorded during pregnancy, and birthweight was recorded at delivery. Four to seven years after delivery, mothers were asked to recall the child’s birthweight and size. Their responses were compared with the birthweight recorded in the EMaBS database.
Results
Of 404 interviewed mothers, 303 (75%) were able to give an estimate of birthweight and for 265 of these EMaBS data on recorded birthweights were available. Women who were educated and whose children had low birth order were more likely to be able to give an estimate: 37 (14%) recalled the exact recorded birthweight; a further 52 (20%) were accurate to within 0.1 kg of the recorded weight. On average, mothers overestimated birthweight by 0.06 kg (95% CI: 0.00–0.13 kg, P = 0.04). Recalled and recorded birthweights showed moderate agreement with an intraclass correlation coefficient of 0.64. Four hundered mothers gave an estimate of birth size: the sensitivity and specificity of recalled birth size for classifying low birthweight were 76% (95% CI: 50–93%) and 70% (95% CI: 65–75%), respectively.
Conclusions
Mothers’ recall of birthweight was not precise but in absence of other data, recall of birthweight and size may have some value in epidemiological studies in these settings.
Keywords: birthweight, reliability, validity, uganda
Introduction
Birthweight is an important predictor of future growth patterns (Hindmarsh et al. 2008) and of mortality and morbidities later in life (Barker et al. 1989; Gofin et al. 2000; Godfrey & Barker 2001). It is also vital in assessment of population health status (Gofin et al. 2000). Records of birthweight are seldom available to researchers investigating disease aetiology in developing countries (Walton et al. 2000; Catov et al. 2006). Maternally recalled birthweight is often the only available source of birthweight information for use in retrospective epidemiological studies, and this may introduce information bias.
In developed countries, several studies have examined concordance between the birthweight recalled by the mother and the recorded birthweight and have shown that maternally recalled birthweight is a good proxy for recorded weight (Gofin et al. 2000; Walton et al. 2000; Tate et al. 2005; Van Gelder & Roeleveld 2011). However, in developing countries, there is limited information on accuracy of maternally reported birthweight and birth size. A study in Brazil reported that mothers accurately recalled birthweight 12 months after delivery but that this accuracy decreased with time after birth (Araújo et al. 2007). In Taiwan, mothers over reported birthweight even within a few months after delivery (Li et al. 2006). In Cameroon, maternal recall was very poor (Mbuagbaw & Gofin 2010), whereas in Kenya, mother’s recall of low birthweight (<2.5 kg) was very good (Mung’ala-Odera & Newton 2001). Given this variability, we have taken the opportunity provided by our birth cohort (the Entebbe Mother and Baby Study; EMaBS) to assess the reliability of maternally recalled birthweight and the validity of maternally recalled birth size and their determinants in Uganda.
Methods
Between April 2003 and November 2005, the EMaBS birth cohort was established to investigate the effect of antihelminthic treatment during pregnancy on the offspring’s response to immunisation and on susceptibility to infectious diseases. Two thousand five hundred and seven women attending antenatal care at Entebbe hospital were enrolled into the trial. Full details of the trial design and procedures are described elsewhere (Elliott et al. 2007). Babies delivered in Entebbe Hospital were weighed immediately after birth using scales graduated in 0.1 kg units (Fazzini SRL, Vimodrone, Italy) and recorded to the nearest 0.1 kg. For babies delivered elsewhere, birthweight was recorded as it appeared on the child health card. Birthweight was available for 1964 of the 2345 live births in the cohort (Ndibazza et al. 2010). The children are currently being followed up, with regular visits to the clinic both for scheduled and illness visits.
From 21 September to 8 December 2010, we interviewed sequentially the mother of each child who attended the study clinic. Children were 4–7 years old at the time of interview. Mothers were asked whether they still possessed the child health card showing the birthweight record of the child. Without reference to the health card, mothers were asked to recall the birthweight of their child and to give a categorical estimate of the birth size of the child (small, normal or large). These data were linked with antenatal and delivery information from the EMaBS database, thus allowing for comparison of recalled and recorded birthweight.
Reliability of maternal recall of birthweight was assessed by calculating the mean difference between recalled birthweight and recorded birthweight and conducting a paired t-test. The intraclass correlation coefficient was calculated as a measure of the agreement between reported and recalled birthweight. Recorded birthweight was categorised into low birthweight (<2.5 kg), normal birthweight (2.5–4.0 kg) and large birthweight (>4.0 kg). Sensitivity and specificity of a mother’s perception of small birth size in detecting low birthweight babies and of a mother’s perception of large birth size in detecting large birthweight babies were calculated.
Logistic regression was used to examine factors associated with mother’s recall of birthweight. Two binary outcomes were considered: first, ability to recall any numerical estimate of birthweight; second, ability to recall birthweight to within 0.1 kg of the recorded weight. Explanatory factors considered were mother’s age, education and socio-economic status, child’s birth order, gender, recorded birthweight and the child’s age at the time of this study. Multivariable analysis was used to adjust for the possible confounding effect of factors that were crudely associated with the outcome.
Results
Between 21 September and 8 December 2010, 404 mothers were interviewed. Mothers who were interviewed were on average slightly older, were less likely to be primigravidae and had attended more routine study visits, than the remaining mothers enrolled in the EMaBS cohort whose children did not attend the clinic during this study period. Their children were less likely to have been born at home. Of the 404 children whose mothers were interviewed, 204 (51%) were male and 200 (49%) were female, with a mean age of 5.7 years (range, 4.5–7.5 years). One hundred and ninety-seven (49%) had attended the clinic because of illness, and 207 (51%) had attended for a routine visit. The average age of mother at the time of delivery of the study baby was 25 years (range, 15–45 years), and 356 (88%) said they still had the child health card. Three hundred and three (75%) of the women were able to give an estimate of birthweight; of the remaining 101 women who were unable to give an estimate of birthweight, 11 had delivered at home, and thus, birthweight is unlikely to have been measured (although one woman who delivered at home did give an estimate of birthweight). Characteristics of those who recalled and did not recall birthweight are shown in Table 1. Women who gave an estimate for birthweight were more likely to be educated, and their children were more likely to be of low birth order. There was a crude association between younger maternal age and ability to give an estimate of birthweight, but maternal age and birth order were associated, and multivariable analyses suggested that the association between age and ability to give an estimate of birthweight was mediated through birth order (Table 1).
Table 1.
Comparison of maternal and child characteristics between mothers who gave an estimate of birthweight and those who did not
| Characteristic | Total mothers interviewed N = 404 | Number (%) mothers who estimated birthweight | Crude OR (95% CI) | P-value | Adjusted OR (95% CI)* | P-value* |
|---|---|---|---|---|---|---|
| Mother’s age at birth of child (years) | ||||||
| 15–19 | 72 | 59 (82%) | 1 | 0.004 [trend] | 1 | 0.95 |
| 20–24 | 153 | 121 (79%) | 0.83 (0.41–1.70) | 1.46 (0.63–3.39) | ||
| 25–29 | 100 | 73 (73%) | 0.60 (0.28–1.26) | 1.50 (0.54–4.13) | ||
| 30+ | 79 | 50 (63%) | 0.38 (0.18–0.81) | 1.19 (0.37–3.79) | ||
| Mother’s education† | ||||||
| None | 13 | 3 (23%) | 0.12 (0.03–0.48) | <0.001 | 0.11 (0.03–0.44) | 0.002 |
| Primary | 183 | 132 (72%) | 1 | 1 | ||
| Secondary | 169 | 138 (82%) | 1.72 (1.04–2.85) | 1.36 (0.80–2.31) | ||
| Tertiary | 38 | 29 (76%) | 1.24 (0.55–2.81) | 0.97 (0.41–2.30) | ||
| Birth order | ||||||
| 1 | 87 | 76 (87%) | 1 | <0.001 [trend] | 1 | 0.02 [trend] |
| 2 | 103 | 80 (78%) | 0.50 (0.23–1.10) | 0.51 (0.21–1.22) | ||
| 3–4 | 131 | 98 (75%) | 0.43 (0.20–0.91) | 0.40 (0.15–1.05) | ||
| ≥5 | 83 | 49 (59%) | 0.21 (0.10–0.45) | 0.23 (0.07–0.74) | ||
| Sex of child | ||||||
| Male | 204 | 149 (73%) | 1 | 0.36 | ||
| Female | 200 | 154 (77%) | 1.24 (0.79–1.94) | |||
| Age of child (years) | ||||||
| 4 | 84 | 62 (74%) | 1 | 0.68 | ||
| 5 | 175 | 133 (76%) | 1.12 (0.62–2.04) | |||
| 6 | 119 | 91 (76%) | 1.15 (0.61–2.20) | |||
| 7 | 26 | 17 (65%) | 0.67 (0.26–1.72) | |||
| Recorded birthweight (kg)‡ | ||||||
| <2.5 | 17 | 13 (76%) | 1 | 0.94 | ||
| 2.5–4 | 302 | 241 (80%) | 1.22 (0.38–3.86) | |||
| >4 | 14 | 11 (79%) | 1.13 (0.21–6.17) | |||
Multivariable model included mother’s age at birth of child, mother’s education and birth order, the adjusted estimate for mother’s age is interpreted as the independent effect of age that does not act through birth order, controlling for mother’s education.
One missing value.
Restricted to the 333 children for whom a record of birthweight was available.
Analysis of the agreement between recorded and maternally recalled birthweight was restricted to 333 (82%) of the 404 interviewed mothers who gave birth in Entebbe hospital. Sixty-eight of these women were unable to recall their child’s birthweight, leaving 265 mother–child pairs with both a recalled and a recorded birthweight. The mean (standard deviation; range) of recalled and recorded birthweights were 3.28 kg (0.68 kg; 1.50–6.40 kg) and 3.21 kg (0.50 kg; 1.50–5.50 kg), respectively: on average, mothers overestimated the birthweight by 0.06 kg (95% CI: 0.00–0.13 kg, P = 0.04, paired t-test). Agreement between recalled and recorded birthweight was moderate (intraclass correlation coefficient 0.64, Figure 1). Only 37 (14%) of mothers recalled their child’s birthweight exactly as recorded; a further 52 (20%) recalled the birthweight to within 0.10 kg of the recorded value. Of the covariates considered, none was associated with accurate recall, or with the difference between recalled and recorded birthweight.
Figure 1.
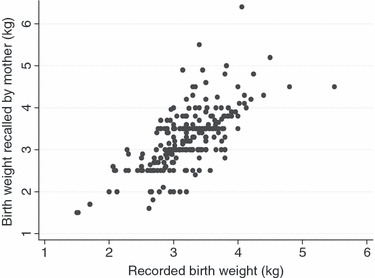
The relationship between recalled and recorded birth weights.
All but four of the 404 mothers gave a response regarding the size of the baby at birth. Thirty-five (9%) described their baby as large, 237 (59%) as normal and 128 (32%) as small. Reported size was associated with recorded birthweight (P < 0.001): the mean (SD) recorded birthweights for the recalled large, normal and small size groups were 3.73 kg (0.60 kg), 3.31 kg (0.40 kg) and 2.92 kg (0.49 kg), respectively. The sensitivity and specificity of mother’s recall of small size for low birthweight babies were 76% (95% CI: 50–93%) and 70% (95% CI: 65–75%), respectively, while the sensitivity and specificity for detecting large birthweight babies were 57% (29–82%) and 94% (91–97%), respectively.
Discussion
This study from Uganda is one of a very small number of studies in sub-Saharan Africa to have assessed mothers’ recall of birthweight and birth size. Many mothers (25%) could not recall any numerical estimate of birthweight but almost all gave an approximate birth size. Those who gave an estimate of birthweight were not very accurate as to the precise figure, but there was moderate agreement between recalled and recorded birthweight. This was consistent with findings from the Netherlands by Jaspers et al. (2010) who found maternally recalled birthweight was not very accurate. Studies from the UK showed better maternal recall, with over 92% recalling birthweight to within 0.1 kg of recorded birthweight (Tate et al. 2005) and 85% to within 0.22 kg of recorded birth (Walton et al. 2000).
Studies by Rice et al. (2007), Gofin et al. (2000), O’Sullivan et al. (2000), Tate et al. (2005), Walton et al. (2000) and Jaspers et al. (2010) reported no mean difference between mothers’ recalled birthweight and recorded birthweight. In this study, we found there was a tendency of mothers to overestimate birthweight, and this finding was consistent with results from Taiwan reported by Li et al. (2006), but in contrast to findings from Denmark where mothers underestimated the birthweight (Adegboye & Heitmann 2008).
In this community, mothers’ concerns at birth are viability, absence of congenital anomalies and child’s sex and so little emphasis is placed on birthweight. Therefore, it is perhaps not surprising that many mothers in our study were unable to give a numerical estimate of weight. Ability to recall any numerical estimate of birthweight increased with education and decreased with the birth order of the child. However, we did not identify any maternal or child factors that were associated with accurate recall of birthweight. Similar results were reported by O’Sullivan et al. (2000), McCormick and Brooks-gunn (1999) and Olson et al. (1997). However, Tate et al. (2005) found that birth order, birthweight and socio-economic status influenced accurate recall of birthweight.
Mothers’ recall of birth size was more robust, allowing classification of babies as low birthweight with sensitivity and specificity of 76% and 70%, respectively (compared to a sensitivity of 60% and specificity of 93% seen in Cameroon (Mbuagbaw & Gofin 2010).
Possible sources of error and bias in this study were considered. Only one child per mother was enrolled into the EMaBS, and to be part of this analysis, the mother and child pair had attended the study clinic together; thus, it is unlikely that the mother gave data on any non-EMaBS sibling. Mothers who participated in this study were on average slightly older and had attended more routine study visits than members of the EMaBS cohort who were not included; and only 3% of their children had been born at home compared to EMaBS (Ndibazza et al. 2010) and community (Tann et al. 2007) estimates of 11%. Thus, some elements of our source population are under-represented. However, the differences in characteristics are not large; thus, any impact is likely to be minimal.
In summary, mother’s recall of birthweight was not precise but in absence of other data, mother’s recalled birthweight and birth size have some value for epidemiological studies, as long as it is not crucial to know the exact birthweight. Clinicians and researchers using maternally recalled birthweight should be cautious when using such information. Recalled birth size should be used only where recorded birthweight is not available.
Acknowledgments
We would like to thank the study participants and the staff of Entebbe hospital and MRC/UVRI Uganda Research Unit on AIDS. The work was funded by the Wellcome Trust.
References
- Adegboye AR, Heitmann B. Accuracy and correlates of maternal recall of birthweight and gestational age. BJOG. 2008;115:886–893. doi: 10.1111/j.1471-0528.2008.01717.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araújo CLP, Dutra CLC, Hallal PC. Validity of maternal report on birth weight 11 years after delivery : the 1993 Pelotas Birth Cohort Study, Rio Grande do Sul State, Brazil. Cad, Saude Publica, Rio de Janeiro. 2007;23:2421–2427. doi: 10.1590/s0102-311x2007001000017. [DOI] [PubMed] [Google Scholar]
- Barker DJ, Osmond C, Winter PD, Margetts B, Simmonds SJ. Weight in infancy and death from ischaemic heart disease. Lancet. 1989;334:577–580. doi: 10.1016/s0140-6736(89)90710-1. [DOI] [PubMed] [Google Scholar]
- Catov JM, Newman AB, Kelsey SF, et al. Accuracy and Reliability of Maternal Recall of Infant Birth Weight Among Older Women. Annals of Epidemiology. 2006;16:429–431. doi: 10.1016/j.annepidem.2005.09.004. [DOI] [PubMed] [Google Scholar]
- Elliott AM, Kizza M, Quigley MA, et al. The impact of helminths on the response to immunization and on the incidence of infection and disease in childhood in Uganda: design of a randomized, double-blind, placebo-controlled, factorial trial of deworming interventions delivered in pregnancy and early childhood. Clinical trial. 2007;4:42–57. doi: 10.1177/1740774506075248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godfrey KM, Barker DJ. Fetal programming and adult health. Public Health. 2001;4:1–624. doi: 10.1079/phn2001145. [DOI] [PubMed] [Google Scholar]
- Gofin R, Neumark Y, Adler B. Birthweight recall by mothers of Israeli children. Public Health. 2000;114:161–163. [PubMed] [Google Scholar]
- Hindmarsh PC, Geary MPP, Rodeck CH, et al. Factors Predicting Ante- and Postnatal Growth. Pediatric Research. 2008;63:9–102. doi: 10.1203/PDR.0b013e31815b8e8f. [DOI] [PubMed] [Google Scholar]
- Jaspers M, Meer GD, Verhulst FC, et al. Limited validity of parental recall on pregnancy, birth, and early childhood at child age 10 years. Journal of Clinical Epidemiology. 2010;63:5–191. doi: 10.1016/j.jclinepi.2009.05.003. [DOI] [PubMed] [Google Scholar]
- Li C, Wei J, Lu T, et al. Mothers tended to overreport categorical infant birth weight of their children. Journal of Clinical Epidemiology. 2006;59:9–1325. doi: 10.1016/j.jclinepi.2006.02.018. [DOI] [PubMed] [Google Scholar]
- Mbuagbaw L, Gofin R. Can recall of birth size be used as a measure of birthweight in Cameroon? Paediatric and Perinatal Epidemiology. 2010;24:3–389. doi: 10.1111/j.1365-3016.2010.01128.x. [DOI] [PubMed] [Google Scholar]
- McCormick MC, Brooks-gunn J. Concurrent Child Health Status and Maternal Recall of Events in Infancy. Pediatrics. 1999;1040:6–81. [PubMed] [Google Scholar]
- Mung’ala-Odera V, Newton CRJC. Recall of Perinatal Events by Mothers Living in Rural Kenya. Epidemiology. 2001;12:6. doi: 10.1097/00001648-200105000-00021. [DOI] [PubMed] [Google Scholar]
- Ndibazza J, Muhangi L, Akishule D, et al. Effects of deworming on maternal and perinatal outcomes in Entebbe, Uganda: a randomized controlled trial. Clinical Infectious Diseases. 2010;50:1–40. doi: 10.1086/649924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson JE, Shu XO, Ross JA, Pendergrass T, Robison LL. Medical Record Validation of Maternally Reported Birth Characteristics and Pregnancy-related Events : a Report from the Children ‘s Cancer Group. American Journal of Epidemiology. 1997;145:8–67. doi: 10.1093/oxfordjournals.aje.a009032. [DOI] [PubMed] [Google Scholar]
- O’Sullivan JJ, Pearce MS, Parker L, Infirmary V. Parental recall of birth weight: how accurate is it? Journal of Abnormal and Social Psychology. 2000;82:2–203. doi: 10.1136/adc.82.3.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice F, Lewis A, Harold G, et al. Agreement between maternal report and antenatal records for a range of pre and peri-natal factors: the influence of maternal and child characteristics. Early Human Development. 2007;83:7–504. doi: 10.1016/j.earlhumdev.2006.09.015. [DOI] [PubMed] [Google Scholar]
- Tann CJ, Kizza M, Morison L, et al. Use of antenatal services and delivery care in Entebbe, Uganda: a community survey. BMC Pregnancy and Childbirth. 2007;7:23. doi: 10.1186/1471-2393-7-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tate AR, Dezateux C, Cole TJ, Davidson L. Factors affecting a mother’s recall of her baby’s birth weight. International Journal of Epidemiology. 2005;34:8–695. doi: 10.1093/ije/dyi029. [DOI] [PubMed] [Google Scholar]
- Van Gelder MMHJ, Roeleveld N. Early Human Development Validation of maternal self-report in retrospective studies. Early Human Development. 2011;87:43–44. doi: 10.1016/j.earlhumdev.2010.09.372. [DOI] [PubMed] [Google Scholar]
- Walton KA, Murray LJ, Gallagher AM, Cran GW, Savage MJ, Boreham C. Parental recall of birthweight: a good proxy for recorded birthweight? European Journal of Epidemiology. 2000;16:3–796. doi: 10.1023/a:1007625030509. [DOI] [PubMed] [Google Scholar]


