Abstract
Airway surface hydration depends on the balance between transepithelial Na+ absorption and Cl− secretion. In adult mice, absence of functional cystic fibrosis transmembrane conductance regulator (Cftr) fails to recapitulate human cystic fibrosis (CF) lung disease. In contrast, overexpression of the epithelial Na+ channel β subunit in transgenic mice (βENaC-Tg) produces unregulated Na+ hyperabsorption and results in CF-like airway surface dehydration, mucus obstruction, inflammation, and increased neonatal mortality. To investigate whether the combination of airway Na+ hyperabsorption and absent Cftr-mediated Cl− secretion resulted in more severe lung pathology, we generated double-mutant ΔF508 CF/βENaC-Tg mice. Survival of ΔF508 CF/βENaC-Tg mice was reduced compared with βENaC-Tg or ΔF508 CF mice. Absence of functional Cftr did not affect endogenous or transgenic ENaC currents but produced reduced basal components of Cl− secretion and tracheal cartilaginous defects in both ΔF508 CF and ΔF508 CF/βENaC-Tg mice. Neonatal ΔF508 CF/βENaC-Tg mice exhibited higher neutrophilic pulmonary inflammation and club cell (Clara cell) necrosis compared with βENaC-Tg littermates. Neonatal ΔF508 CF/βENaC-Tg mice also exhibited spontaneous bacterial infections, but the bacterial burden was similar to that of βENaC-Tg littermates. Adult ΔF508 CF/βENaC-Tg mice exhibited pathological changes associated with eosinophilic crystalline pneumonia, a phenotype not observed in age-matched βENaC-Tg mice. Collectively, these data suggest that the combined abnormalities in Na+ absorption and Cl− secretion produce more severe lung disease than either defect alone. Airway cartilage abnormalities, airway cell necrosis, and exaggerated neutrophil infiltration likely interact with defective mucus clearance caused by βENaC overexpression and absent CFTR-mediated Cl− secretion to produce the increased neonatal mortality observed in ΔF508 CF/βENaC-Tg mice.
Keywords: genetically modified mice, cystic fibrosis, ΔF508 CFTR, ENaC, airway inflammation, airway epithelia necrosis
hydration of airway surfaces, which is critically important for mucociliary clearance and lung health, is achieved by balancing transepithelial Cl− secretion and Na+ absorption. Defective cAMP-mediated Cl− secretion due to loss of cystic fibrosis transmembrane conductance regulator (CFTR) function and poorly regulated Na+ absorption through the epithelial Na+ channel (ENaC) both contribute to impaired airway surface hydration in cystic fibrosis (CF) (34, 42). Several Cftr-targeted murine models have been developed to study CF lung disease pathogenesis and test therapeutic strategies (reviewed in Refs. 14, 30, 44). Although Cftr-deficient mice exhibit intestinal and nasal phenotypes consistent with human CF (11), the lower airways of Cftr-deficient mice do not exhibit CF-like obstructive lung disease. Tracheas from adult CF mice also do not exhibit defects in either cAMP-mediated Cl− secretion nor Na+ hyperabsorption (39), likely due to low endogenous Cftr expression in adult tracheal tissue combined with expression of alternative Cl− channels, e.g., Tmem16a (39). In contrast, neonatal murine tracheas have a more robust Cftr mRNA expression (∼2-fold more than adult tracheas; W. K. O'Neal, unpublished observations), and CF neonatal mice exhibit the classic defect in cAMP-mediated Cl− secretion, with a forskolin response reduced approximately fourfold compared with wild-type (WT) mice (38, 39). Nonetheless, neonatal CF mice have no detectable lung disease.
In contrast to nasal epithelia, the lower airways of CF mice do not exhibit dysregulated Na+ absorption at any age (38). The importance of dyrsegulated Na+ absorption in eliciting a CF-like lung disease in the mouse lower airways is supported by the phenotype of βENaC-transgenic (βENaC-Tg) mice, in which club cell (Clara cell)-targeted overexpression of the epithelial Na+ channel β subunit (βENaC, encoded by the Scnn1b gene) produces dysregulated Na+ absorption and causes defective airway mucus clearance, susceptibility to spontaneous bacterial infection, and airway inflammation that resembles human CF lung disease (27, 31, 33). βENaC-Tg mice exhibit forskolin- and UTP-regulated Cl− secretory responses similar to WT mice (31), indicating that lung disease occurs in the presence of normal Cftr and Tmem16a function.
To test the hypothesis that the combination of defective Cl− secretion with abnormally regulated Na+ absorption would produce lung disease more severe than defects in either pathway alone, particularly in the neonatal period when Cftr is most highly expressed in mouse lower airways, we crossed βENaC-Tg mice with mice carrying the ΔF508 Cftr mutation [Cftrtm1Kth (46), hereafter referred to as ΔF508 CF]. We studied the airway bioelectric properties of neonatal and adult ΔF508 CF/βENaC-Tg mice in Ussing chambers and evaluated the severity of lung disease by measuring histopathology, inflammatory infiltrate, and lung bacterial burden.
MATERIALS AND METHODS
Animals.
Animals were maintained and studied under protocols approved by the University of North Carolina Institutional Animal Care and Use Committee, and experiments were performed according to the principles outlined by the Animal Welfare and the National Institutes of Health guidelines for the care and use of animals in biomedical research. All mice were housed in individually ventilated microisolator cages in a specific pathogen-free facility maintained at the University of North Carolina at Chapel Hill, on a 12-h day-night cycle. Mice were fed a regular chow diet and given water ad libitum. Weaned mice and breeders homozygous for the murine CftrΔF508 mutation were given water supplemented with Colyte to reduce complications due to intestinal obstruction (7).
To generate CF/βENaC-Tg mice, we sequentially bred congenic C57BL/6N βENaC-Tg mice (line 6608) (28), with congenic C57BL/6J male CftrΔF508 Cftrtm1Kth mice (46) and obtained mice of four different genotypes with respect to murine CftrΔF508 and βENaC-Tg expression: 1) ΔF508/wt, wt (referred to as WT); 2) ΔF508/wt, βENaC-Tg (referred to as βENaC-Tg); 3) ΔF508/ΔF508, wt (referred to as ΔF508 CF); 4) ΔF508/ΔF508, βENaC-Tg (referred to as ΔF508 CF/βENaC-Tg). At birth all pups were toe clipped for identification and genotyping, as previously described (31, 46). Mice studied were littermates, age matched, and of both sexes. When used for Ussing chamber experiments, all mouse pups were euthanized by an overdose of ketamine/xylazine and adult mice were euthanized by CO2 inhalation. When used for bronchoalveolar lavage and histopathology, mice were euthanized by exsanguination under deep 2,2,2-tribromoethanol (Avertin) anesthesia.
Bioelectric studies.
Mouse pups remained with the mother until time of study. Adult mice were studied at the ages indicated in figure legends. All studies were done blinded with respect to genotype. Details of the Ussing chamber preparations have been previously published (13). Amiloride (10−4 M apical addition) was used to block electrogenic Na+ absorption. Forskolin (10−5 M apical) and UTP (10−4 M apical) were used to induce anion secretion via an increase in intracellular cAMP and intracellular Ca2+ concentrations, respectively. Bumetanide (10−4 M) was added to the basolateral bath to inhibit Cl− entry through the Na-K-2Cl cotransporter (NKCC1). All drugs were purchased from Sigma Aldrich with the exception of UTP (Amersham Pharmacia Biotech).
BAL.
For 10-day-old or older mice, bronchoalveolar lavage (BAL) cell counts and lung histology were obtained from the same animal, as described in Ref. 28. Because of their small size, 5-day-old pups were subject to either whole lung lavage or fixation for histology, but not both. Routinely, lungs were immersion-fixed in 10% neutral-buffered formalin (NBF) to prevent dislodging of airway luminal contents. For lung volume measurements, lungs were inflated with 10% NBF at a constant pressure (25 cmH2O) and fixed in situ before removal en bloc. After wet trimming of the heart, lung volume was measured by water displacement, as previously described (33).
Measurement of cytokines and chemokines in BALF.
Aliquots of cell-free BAL fluid (BALF), stored at −80°C, were used to measure mouse TNF-α (tumor necrosis factor-α, Tnf), KC (keratinocyte-derived cytokine, Cxcl1), MIP-2 (macrophage inflammatory protein, Cxcl2), MIP-1α (macrophage inflammatory protein-1, Ccl3), M-CSF (macrophage colony-stimulating factor, Csf1), MCP-1 (monocyte chemoattractant protein-1, Ccl2), LIX (lipopolysaccharide-induced CXC chemokine, Cxcl5), IL-6 (interleukin-6, Il6), IL-1α (interleukin-1α, Il1a), IL-1β (interleukin-1β, Il1b), GM-CSF (granulocyte-macrophage colony-stimulating factor, Csf2), and G-CSF (granulocyte colony-stimulating factor, Csf3) via a bead-based assay (Upstate-Millipore Beadlyte multiplex assays/Luminex, Billerica, MA) according to the manufacturer instructions.
Bacteriology.
BAL was performed aseptically and plated, and colony-forming units (CFUs) were enumerated, classified on the basis of their morphology, and processed for molecular identification through ribosomal 16S gene PCR amplification and sequencing, as previously described (27).
Lung histology.
Fixed lungs were embedded, sectioned, and stained with hematoxylin and eosin (H&E) and Alcian blue-periodic acid Schiff staining (AB-PAS), and lung pathology was graded as previously described (28). Bronchiolar epithelial cell necrotic degeneration was quantified morphometrically by counting epithelial necrotic cells lining the bronchiolar airways and expressing the data per millimeter of the basement membrane, as described in Ref. 33. Tissue blocks received a numerical code at time of embedding, and scoring of the slides was performed by an investigator blinded to specimen genotype.
Immunohistochemistry.
Immunohistochemical staining for Ym1/2 and club cell secretory protein (CCSP) were performed on formalin-fixed, paraffin-embedded lung sections by using rabbit polyclonal anti-Ym1 antibody and anti-club cell secretory protein (anti-CCSP; Seven Hills Bioreagents, Cincinnati, OH) as described in Refs. 33 and 8, respectively
Statistics.
Data are shown as means ± SE, with the number of preparations or mice (n). Survival curves were compared by Kaplan-Meier log rank analysis and Holm-Sidak multiple comparison with the overall significance level = 0.05. For bioelectric studies, a one-way ANOVA was used to determine whether there was an overall significant difference among the groups, in which case the Holm-Sidak test was used for all pairwise comparisons. The χ2 test was used when comparing frequencies of observed events. ANOVA followed by Tukey's post hoc test for multiple comparisons were used to determine significant differences among groups for body weight, lung volume, cytokine levels, necrotic epithelial cells, BAL cells, and CFU counts. P < 0.05 was considered statistically significant.
RESULTS
ΔF508 CF/βENaC-Tg mice exhibited reduced survival compared with both ΔF508 CF and βENaC-Tg littermates.
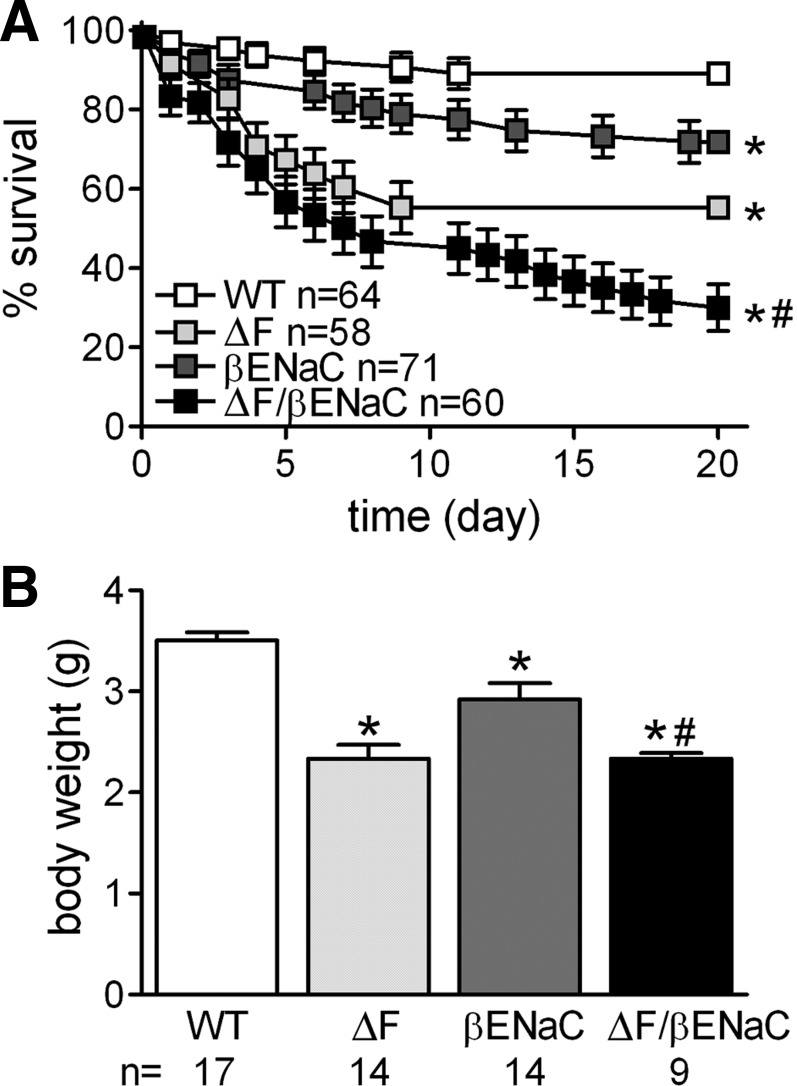
As previously reported, both genetic modifications, i.e., βENaC overexpression and functional deletion of Cftr, reduced survival compared with WT littermates [Fig. 1A, 72 ± 5%, for βENaC-Tg (26) and 55 ± 7% for ΔF508 CF (46) mice at postnatal day (PND) 20]. Notably, ΔF508 CF/βENaC-Tg mice survival was lower than either ΔF508 CF or βENaC-Tg mice. In particular, survival of ΔF508 CF/βENaC-Tg mice resembled that of ΔF508 CF mice at PND 1–10, but after PND 10 the survival of ΔF508 CF/βENaC-Tg mice significantly decreased and only 30 ± 6% survived to PND 20.
Fig. 1.
Gross findings in double-mutant ΔF508 CF/βENaC-Tg mice compared with wild-type (WT), ΔF508 CF (mice carrying the ΔF508 Cftr mutation), and βENaC-Tg (transgenic mice with overexpression of the epithelial Na+ channel β subunit) littermates. A: survival curves for mice from the ΔF508 CF × βENaC-Tg cross indicate reduced survival in ΔF508 CF/βENaC-Tg mice (ΔF/βENaC) compared with ΔF508 CF (ΔF) and βENaC-Tg (βENaC) littermates. *P < 0.05 vs. WT mice, #P < 0.05 vs. βENaC-Tg mice. B: comparison of body weights at 5 days of age shows decreased body weight in ΔF508 CF, βENaC-Tg, and ΔF508 CF/βENaC-Tg mice. *P < 0.05 vs. WT mice, #P < 0.05 vs. βENaC-Tg mice.
ΔF508 CF, βENaC-Tg, and ΔF508 CF/βENaC-Tg mice all exhibited reduced body weight at PND 5 compared with WT littermates (Fig. 1B). ΔF508 CF/βENaC-Tg mice weighed less than βENaC-Tg mice, but their body weight was not different from that of ΔF508 CF mice.
ΔF508 CF/βENaC-Tg mice airway bioelectric properties reflect the combined expression of defective Cftr-dependent Cl− secretion and excessive ENaC-dependent Na+ absorption.
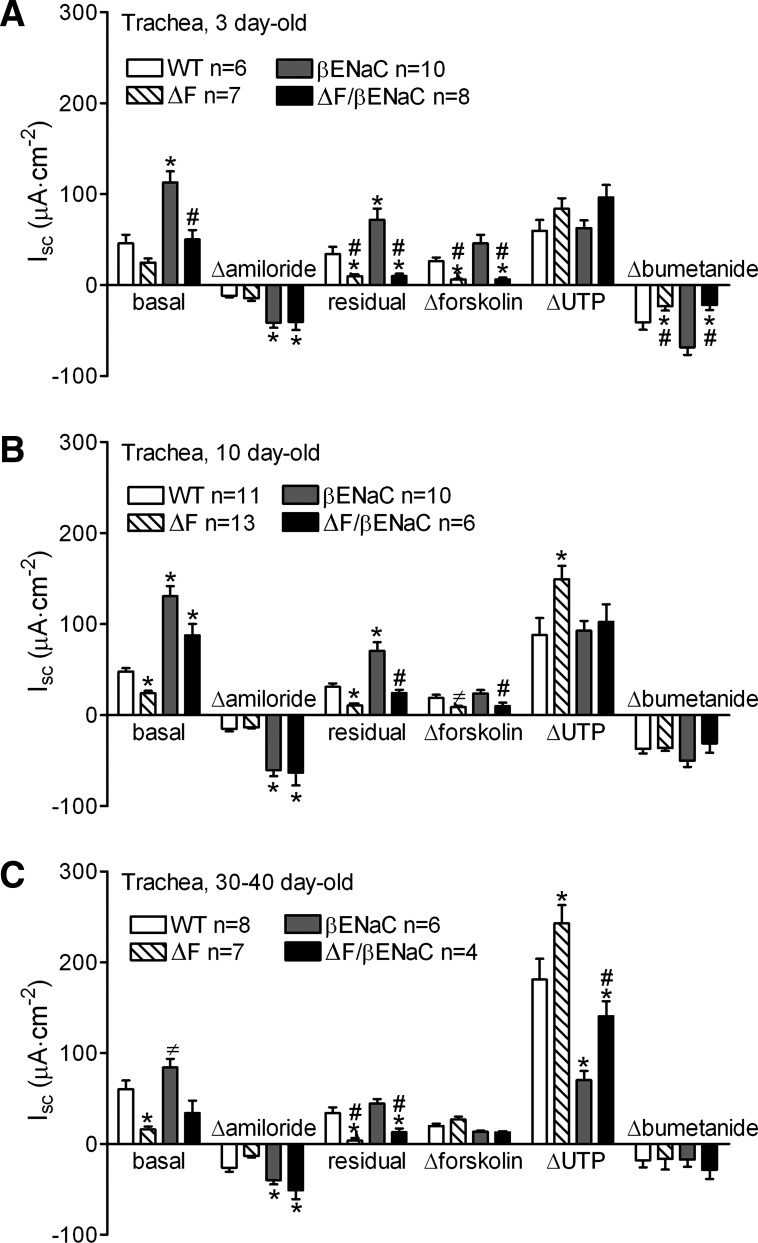
The tracheal bioelectric properties of 3-day-old mice for the four genotypes are shown in Fig. 2A. ΔF508 CF mice exhibited a trend toward reduction of the basal short-circuit current (Isc) but no change in amiloride-sensitive ENaC-mediated current compared with WT mice. The postamiloride residual Isc, the forskolin-stimulated Isc, and the bumetanide-inhibitable Isc were reduced in ΔF508 CF compared with WT mice, consistent with reduced Cftr-mediated Cl− secretion. As expected, the basal Isc and the amiloride-sensitive Isc were significantly elevated in βENaC-Tg compared with WT mice, and the fold increase in amiloride-sensitive Isc, i.e., Na+ absorption, without changes in forskolin- or UTP-stimulated Isc, was similar to that previously reported (31). ΔF508 CF/βENaC-Tg tracheas exhibit bioelectric properties of both ΔF508 CF mice, with decreased postamiloride residual Isc, forskolin-stimulated Isc, and bumetanide-sensitive Isc, and βENaC-Tg mice, with elevated amiloride-sensitive Isc. However, ΔF508 CF/βENaC-Tg tracheas did not exhibit the elevated residual Isc typical of neonatal βENaC-Tg tracheas, indicating that Cftr contributes to the basal Cl− secretory current. In addition, the basal Isc of ΔF508 CF/βENaC-Tg tracheas was significantly lower than that of βENaC-Tg tracheas and not different from WT, suggesting that the raised Na+ currents due to βENaC overexpression were offset by reduced basal Cftr-mediated Cl− secretion. Thus the 3-day-old ΔF508 CF/βENaC-Tg tracheas exhibited properties of both accelerated Na+ absorption and decreased Cl− secretion.
Fig. 2.
ΔF508 CF/βENaC-Tg mice exhibit increased Na+ absorption and defective Cl− secretion. Ion transport properties of freshly excised tracheal tissues of 3-day-old mice (A), 10-day-old mice (B), and adult mice (C) from the ΔF508 CF × βENaC-Tg cross. “Basal” indicates the short-circuit current (Isc) before drug application. The change in Isc (Δ) after sequential drug addition is shown. “Residual” Isc is the Isc remaining after amiloride application. *P < 0.05 vs. WT mice, #P < 0.05 vs. βENaC-Tg mice, ≠P < 0.05 vs. βENaC-Tg mice in B, and P < 0.05 vs. ΔF508 CF (ΔF) and ΔF508 CF/βENaC-Tg (ΔF/βENaC) mice in C.
The bioelectric properties of tracheas from pups that reached 10 days of age were similar to those at 3 days (Fig. 2B). The basal Isc of each group was significantly different from each of the other groups. The basal Isc of both groups carrying the βENaC transgene were significantly elevated compared with the other two groups, and the ΔF508 CF/βENaC-Tg mice exhibited a trend toward reduced basal Isc compared with the βENaC-Tg mice. As noted above, this trend likely reflects decreased Cftr-mediated Cl− secretion, as the basal Isc of CF mice was also reduced compared with WT mice. Unlike 3-day-old tracheas, the UTP response was significantly enhanced in 10-day-old ΔF508 CF tracheas compared with WT (P = 0.01), with all other groups being similar. There was no significant difference in the magnitude of the bumetanide responses between groups at PND 10.
Tracheas of 30-day-old mice maintained most bioelectric features observed for the different genotypes at earlier ages (Fig. 2C). The basal Isc was again significantly reduced in ΔF508 CF tracheas compared with WT and ΔF508 CF/βENaC-Tg tracheas and remained elevated in βENaC-Tg compared with WT, ΔF508 CF, and ΔF508 CF/βENaC-Tg tracheas. Again, the amiloride response was significantly greater in the two groups expressing the βENaC transgene, compared with WT and ΔF508 CF mice. The residual Isc was still significantly attenuated in both groups of ΔF508 CF mice, but the response to forskolin did not differ among the four groups. In general, the UTP responses increased with age and the individual responses in each group differed significantly from each other, with the ΔF508 CF tracheas exhibiting a significantly greater UTP response than the other groups. The response to bumetanide did not differ among the four groups at this age.
ΔF508 CF/βENaC-Tg mice exhibit tracheal abnormalities similar to ΔF508 CF mice and more severe lung pathology compared with βENaC-Tg littermates.
At dissection for Ussing chamber studies, we observed mucus plugs in 14–20% of 3-day-old ΔF508 CF/βENaC-Tg and βENaC-Tg, whereas no mucus plug was found in the tracheas of ΔF508 CF or WT pups.
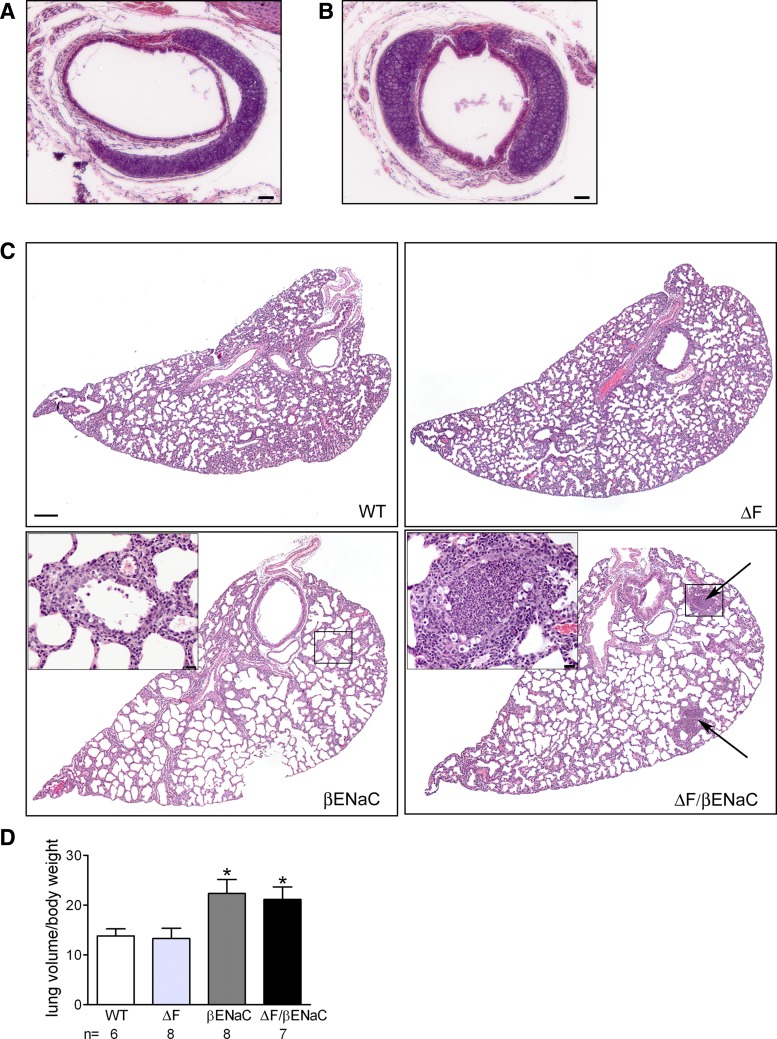
The morphology of tracheal tissues was examined and gross defects that resulted in narrowing of the trachea were observed in the cartilaginous tracheas of some ΔF508 CF and ΔF508 CF/βENaC-Tg mice (Fig. 3, A and B, comparing WT and ΔF508 CF/βENaC-Tg mice, respectively). In both ΔF508 CF and ΔF508 CF/βENaC-Tg mice exhibiting this phenotype, the cartilaginous rings in the upper trachea were discontinuous, resulting in a significantly decreased upper tracheal diameter (0.045 vs. 0.030 cm for WT, n = 3 and CF, n = 4, respectively, P = 0.007). This defect was confined to the upper third of the trachea, and there was no difference in lower tracheal or bronchial diameter between WT and Cftr-deficient pups. Although there was a trend for the ΔF508 CF/βENaC-Tg tracheas to exhibit this defect more frequently (7/9 pups; 77%) than ΔF508 CF neonatal tracheas (3/9 pups; 33%), the difference was not significant (χ2). In contrast, tracheas of WT or βENaC-Tg pups did not show tracheal defects.
Fig. 3.
ΔF508 CF/βENaC-Tg mice exhibited airway and lung pathology distinct from ΔF508 CF and βENaC-Tg mice. A and B: representative photomicrographs of tracheas from 3-day-old WT (A) and ΔF508 CF/βENaC-Tg (B) mice, illustrating tracheal abnormalities in the latter. Tracheas from ΔF508 CF mice exhibited the same tracheal defect as in B. Scale bar = 100 μm. C: representative photomicrographs of lung histology in 5-day-old WT, ΔF508 CF (ΔF), βENaC-Tg (βENaC), and ΔF508 CF/βENaC-Tg (ΔF/βENaC) mice. Hematoxylin and eosin (H&E) stain, low magnification, scale bar = 200 μm. Rectangles indicate areas shown at higher magnification in the insets, scale bar = 20 μm. Arrows indicate dense neutrophil aggregates, commonly found in ΔF508 CF/βENaC-Tg mice airway lumen. D: comparison of lung volumes at 5 days of age shows equivalent air space enlargement in βENaC-Tg and ΔF508 CF/βENaC-Tg mice. *P < 0.05 vs. WT mice.
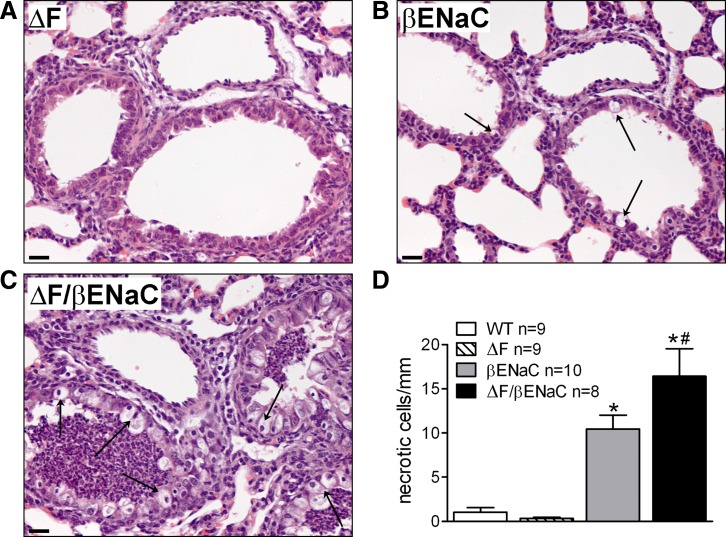
Histologically, the lungs of 5-day-old WT and ΔF508 CF pups exhibited no phenotypic abnormalities, whereas lungs of both βENaC-Tg and ΔF508 CF/βENaC-Tg pups exhibited air space enlargement, bronchial airway inflammation, and airway epithelial necrotic degeneration, which are all features of the lung phenotype originally described for neonatal βENaC-Tg mice (33). In particular, the degree of air space enlargement, observed histologically (Fig. 3C, compare WT and ΔF508 CF top with βENaC and ΔF508 CF/βENaC bottom) and measured as a function of lung volume (Fig. 3D), was similar between βENaC-Tg and ΔF508 CF/βENaC-Tg mice. In contrast, the airways of neonatal ΔF508 CF/βENaC-Tg mice were characterized by focal areas of massive intraluminal neutrophil aggregation (Fig. 3C, arrows and high magnification inset), which were never observed in βENaC-Tg, WT or ΔF508 CF mice. Moreover, ΔF508 CF/βENaC-Tg mice exhibited an increased incidence of necrotic airway epithelial cells compared with βENaC-Tg littermates (Fig. 4, A–D). Consistent with the previously described developmental pattern of airway mucus obstruction in βENaC-Tg mice (28, 33, 43), which features a progression from the trachea in the early neonatal period (PND 5–10) to the intrapulmonary bronchi as the mice age, no AB-PAS-positive material was found in the lungs of 5-day-old βENaC-Tg or ΔF508 CF/βENaC-Tg mice.
Fig. 4.
Prominent airway epithelial cell necrosis in ΔF508 CF/βENaC-Tg mice. A–C: representative photomicrographs of airway epithelia from 5-day-old ΔF508 CF (ΔF; A), βENaC-Tg (βENaC; B), and ΔF508 CF/βENaC-Tg (ΔF/βENaC; C) mice. H&E stain, scale bar = 20 μm. D: morphometric quantification of necrotic cells in 5-day-old mice. *P < 0.05 vs. WT mice, #P < 0.05 vs. βENaC-Tg mice.
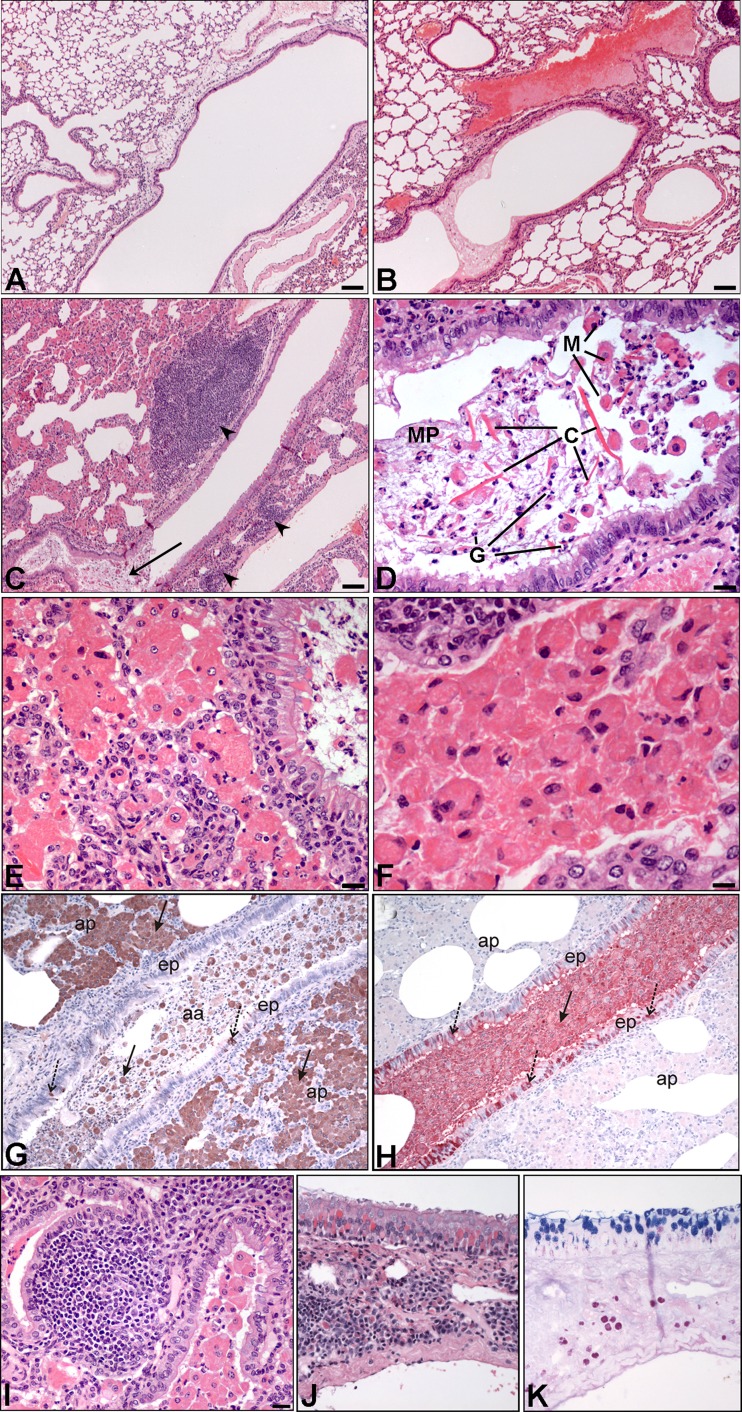
Because of the extremely poor survival of ΔF508 CF/βENaC-Tg mice (Fig. 1A), it was difficult to obtain mice at later time points. However, since Cftr-deficient mice on the C57BL/6 background have been reported to develop some lung pathology later in life (10, 21), we studied the few ΔF508 CF/βENaC-Tg mice that survived until 10 mo of age. Compared with the phenotype of age-matched ΔF508 CF and βENaC-Tg mice (Fig. 5, A and B, respectively), the lesions associated with the ΔF508 CF/βENaC-Tg genotype were much more severe. All 10-mo-old ΔF508 CF/βENaC-Tg mice exhibited multiple lung lesions (Fig. 5, C–F), strikingly resembling the pathology of eosinophilic crystalline pneumonia (18). In particular, lung histology revealed major areas of lobar consolidation (Fig. 5C). Airways and alveoli were filled with mucus and a mixed inflammatory cell exudate containing hypertrophic macrophages, neutrophils, eosinophils, and eosinophilic crystals (Fig. 5, D–F), which have been previously identified as consisting of chitinases YM1/2 (33). Strong YM1/2 immunoreactivity was found in hypertrophic macrophages and epithelial cells (Fig. 5G). Club cell secretory protein accumulated in the lumen of ΔF508 CF/βENaC-Tg mice airways and was entrapped in mucus (Fig. 5H). ΔF508 CF/βENaC-Tg mice also had significant proliferation of bronchial associated lymphoid tissue (BALT, Fig. 5, C and I) with Russell bodies, i.e., inclusions found in plasma cells undergoing excessive synthesis of immunoglobulins [these inclusions appear eosinophilic if stained with H&E (Fig. 5J) or glycoprotein-rich if stained with AB-PAS (Fig. 5K)]. These findings suggest a robust immune response in ΔF508 CF/βENaC-Tg mice.
Fig. 5.
Surviving ΔF508 CF/βENaC-Tg mice exhibit severe lung pathology reminiscent of eosinophilic crystalline pneumonia. A and B: representative micrograph of lung histopathology in 10-mo-old ΔF508 CF (A), βENaC-Tg (B), and ΔF508 CF/βENaC-Tg (C) mice. H&E stain, scale bar 100 μm. C: lung pathology in adult ΔF508 CF/βENaC-Tg mice comprised airway mucus obstruction (arrow), bronchial-associated lymphoid tissue (BALT) (arrowhead), and extensive lobar consolidation. D: intraluminal mucus plugs (MP), granulocytes (G), hypertrophic macrophages (M), and eosinophilic crystals (C), scale bar = 10 μm. E and F: dense aggregates of hypertrophic and vacuolated macrophages in the parenchyma and airway lumen, respectively. G: substantial immunoreactivity for YM1/2 in alveolar macrophages (solid arrows) and epithelial cells (dotted arrows). H: immunoreactivity for CCSP in the lumen (solid arrows) and epithelial cells (dotted arrows). ep, Epithelium; aa, airway lumen; ap, alveolar parenchyma. I: BALT, adjacent a small bronchiole filled with hypertrophic macrophages. J and K: Russell bodies, large cytoplasmic inclusions identifiable as eosinophilic if stained with H&E (J) or glycoprotein-rich if stained with Alcian blue-periodic acid Schiff staining (AB-PAS; K).
ΔF508 CF/βENaC-Tg mice exhibit increased pulmonary inflammation compared with ΔF508 CF and βENaC-Tg littermates.
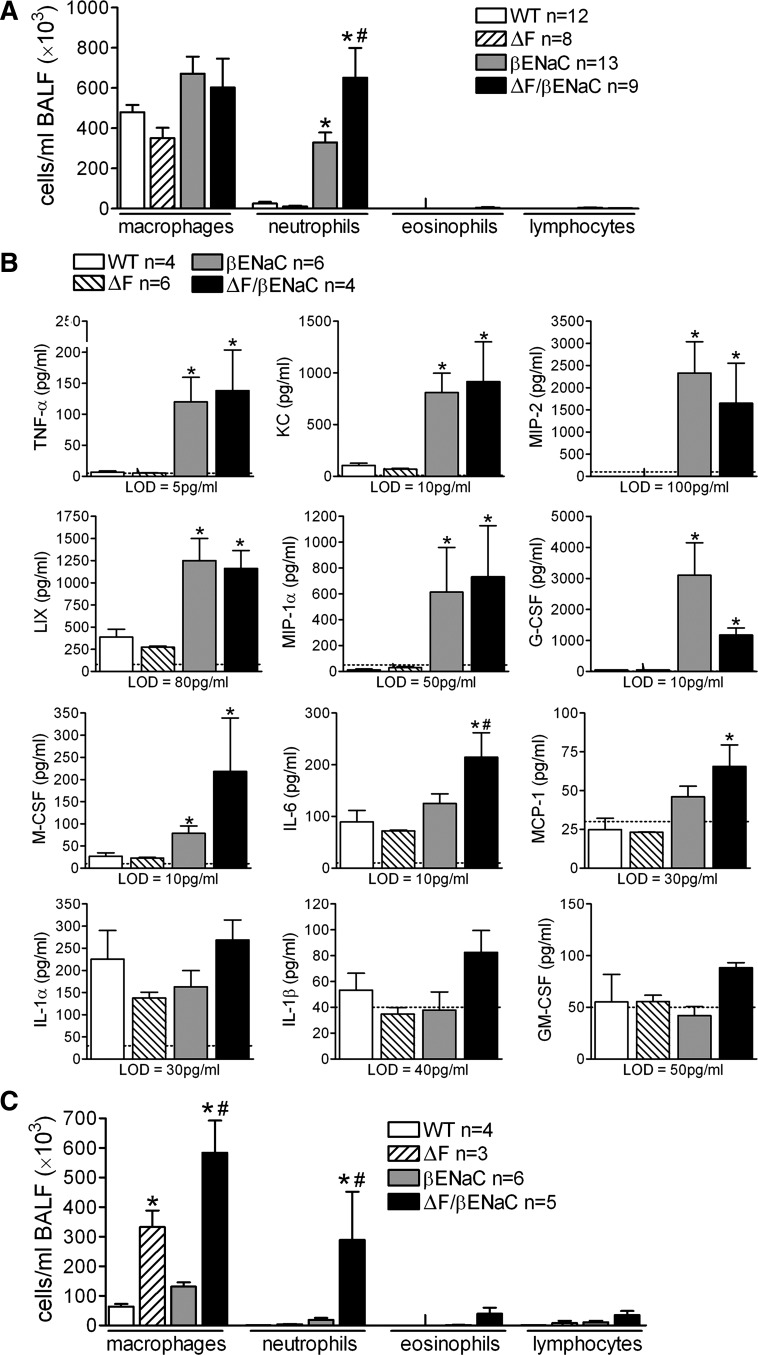
Evaluation of the inflammatory infiltrate was performed by BAL cell counts in 5-day-old pups and 10-mo-old mice from the ΔF508 CF × βENaC-Tg cross. As shown in Fig. 6A, βENaC-Tg and ΔF508 CF/βENaC-Tg pups had significantly more neutrophils than WT and ΔF508 CF mice, and ΔF508 CF/βENaC-Tg pups had more neutrophils than βENaC-Tg littermates. Note that the degree of neutrophilia shown in Fig. 6A for ΔF508 CF/βENaC-Tg mice is likely underestimated, because the luminal neutrophil aggregates present in ΔF508 CF/βENaC-Tg airways (Fig. 3C) were not readily displaced by the BAL procedure, as assessed histologically in lungs subjected to BAL (data not shown).
Fig. 6.
Quantification of airway inflammatory infiltrate and inflammatory mediators profile indicate more severe lung pathology in ΔF508 CF/βENaC-Tg mice. A: differential bronchoalveolar lavage (BAL) cell counts in 5-day-old WT, ΔF508 CF (ΔF), βENaC-Tg (βENaC), and ΔF508 CF/βENaC-Tg (ΔF/βENaC) mice. *P < 0.05 vs. WT mice, #P < 0.05 vs. βENaC-Tg mice. B: BAL fluid (BALF) cytokines in 5-day-old mice. Dotted line represents the assay lower detection limit (LOD). *P < 0.05 vs. WT mice, #P < 0.05 vs. βENaC-Tg mice. TNF-α, tumor necrosis factor-α; KC, keratinocyte-derived cytokine; MIP-2, macrophage inflammatory protein; LIX, lipopolysaccharide-induced CXC chemokine; MIP-1α, macrophage inflammatory protein-1; G-CSF, granulocyte colony-stimulating factor; M-CSF, macrophage colony-stimulating factor; IL-6, interleukin-6; MCP-1, monocyte chemoattractant protein-1; IL-1α, interleukin-1α; IL-1β, interleukin-1β; GM-CSF, granulocyte-macrophage colony-stimulating factor. C: differential BAL cell counts in 10-mo-old ΔF508 CF and ΔF508 CF/βENaC-Tg mice. BAL cell counts in 12-mo-old WT and congenic C57BL/6N βENaC-Tg mice from (26) are plotted in the same graph for comparison. *P < 0.05 vs. WT mice, #P < 0.05 vs. βENaC-Tg mice.
Multiplex profiling of inflammatory mediators in BAL fluid harvested from 5-day-old mice indicated that TNF-α, KC, MIP-2, LIX, G-CSF, M-CSF, and MIP-1α were similarly elevated in βENaC-Tg and ΔF508 CF/βENaC-Tg mice compared with either ΔF508 CF or WT mice (Fig. 6B). The only exception was IL-6, which was significantly elevated in ΔF508 CF/βENaC-Tg mice compared with WT, ΔF508 CF, or βENaC-Tg mice. ΔF508 CF/βENaC-Tg mice had higher MCP-1 compared with WT mice and, although not significant, a slight increase in IL-1β was also noted.
BAL analysis confirmed that 10-mo-old ΔF508 CF/βENaC-Tg mice had significantly more severe lung inflammation than age-matched βENaC-Tg, ΔF508 CF, or WT mice (Fig. 6C). In particular, the number of macrophages and neutrophils was significantly higher than ΔF508 CF or βENaC-Tg mice, and eosinophils were still detectable in ΔF508 CF/βENaC-Tg mice, an unusual finding, since in congenic C57BL/6N βENaC-Tg mice early postnatal eosinophilia is transient and usually wanes after 6 wk of age (26). Interestingly, ΔF508 CF mice exhibited an increase in macrophage number compared with WT or βENaC-Tg mice, in agreement with data previously reported for a different strain of CftrΔF508 mice (23). However, in this study we did not observe any appreciable pathological change in the lungs of ΔF508 CF mice (Fig. 5J).
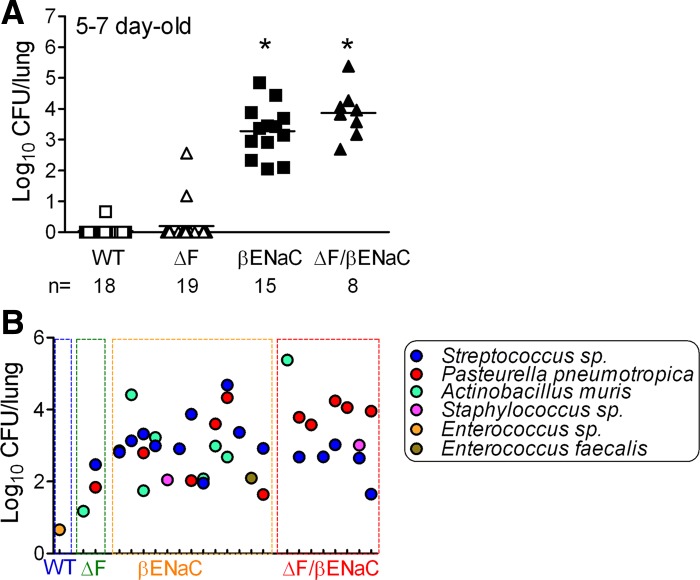
ΔF508 CF/βENaC-Tg mice exhibit spontaneous lung bacterial infection similar to βENaC-Tg littermates.
As recently reported, neonatal βENaC-Tg mice routinely exhibit spontaneous bacterial infection with a predominance of Streptococcus, Pasteurella, and Actinobacillus species (27). Quantification of the bacterial load among genotypes, using culture conditions that permitted detection of nonfastidious aerobes and microaerophilic bacteria, revealed that WT and ΔF508 CF mice exhibited little or no evidence of infection. In contrast, ΔF508 CF/βENaC-Tg mice exhibited infection, with both bacterial counts (Fig. 7A) and lung microflora composition (Fig. 7B) similar to βENaC-Tg littermates.
Fig. 7.
Spontaneous bacterial colonization in mice from the ΔF508 CF × βENaC-Tg cross. A: analysis of total colony forming units (CFU) in BAL samples from 5-day-old mice. (Log10+1)-transformed data; n = number of mice/group. *P < 0.05 vs. WT littermates. B: individual CFUs and bacterial species isolated from 5-day-old mice. Each tick on the x-axis represents an individual mouse.
DISCUSSION
Effective airway mucus clearance is dependent on adequate airway surface hydration. In CF, the pathogenic failure of mucus clearance has been attributed to inadequate airway hydration caused by both defective Cl− secretion, due to the absence of functional CFTR, and, although still controversial (6), enhanced Na+ absorption, due to unregulated ENaC activity (9). Models of inadequate airway hydration are thus needed to better understand the pathophysiology of CF and to aid the design of effective therapies.
The various CF mouse models generated thus far have not exhibited, as adults, either defective cAMP-mediated Cl− secretion nor Na+ hyperabsorption in the lower airways. We have reported, however, that neonatal CF pups do exhibit a defect in cAMP-mediated Cl− secretion (38, 39). The availability of βENaC-Tg mice, which exhibit constitutive airway ENaC hyperactivity and CF-like lung pathology (31, 33), allowed us to generate a mouse model, i.e., the ΔF508 CF/βENaC-Tg mouse, that could, at least during the early postnatal period, recapitulate both ion transport defects that likely initiate CF lung disease. The ΔF508 CF mouse model was chosen for these studies because of its availability on the C57BL/6 background and its potential usefulness in pharmacological studies with ΔF508 CFTR correctors/potentiators.
Survival analysis of mice generated from ΔF508 CF × βENaC-Tg crosses revealed distinct differences among the resulting genotypes (Fig. 1A). βENaC-Tg mice exhibited a small but significant drop in neonatal survival, which is typical for the congenic C57BL/6N strain (26). ΔF508 CF mice exhibited survival consistent with that reported for this line at 20 days, i.e., a modest decrease that precedes the more significant drop (40%) occurring after weaning (46). Conversely, the survival decline in ΔF508 CF/βENaC-Tg mice appeared to be biphasic. During the first 10 days of life, both ΔF508 CF and ΔF508 CF/βENaC-Tg pups exhibited similar declines in survival (Fig. 1A), likely reflecting a survival disadvantage due to a common dominant effect, i.e., failure to thrive imposed by the Cftr deletion (17). This notion is supported by the similar reduced weight for the two genotypes (Fig. 1B). However, after 10 days, ΔF508 CF pups' survival stabilized, whereas ΔF508 CF/βENaC-Tg pups suffered a further drop in survival. Histopathological and BAL data showed that, by PND 5, ΔF508 CF/βENaC-Tg pups had an inflammatory burden and severity of lung disease that exceeded that of βENaC-Tg pups (Fig. 3C, 4C, and 6A). Moreover, ΔF508 CF/βENaC-Tg pups exhibited the CF-related tracheal anatomical defect (Fig. 3B) previously described in CF mice (1) and pigs (35, 37). This defect may produce increased airways compliance and enhance airway closure, reducing the ability of ΔF508 CF/βENaC-Tg pups to clear lethal mucus plugs. Collectively, these data suggest that the second component of the decline in survival of ΔF508 CF/βENaC-Tg mice reflected more severe respiratory disease.
The bioelectric properties of the genetically modified mice utilized in this study revealed three distinct patterns of ion transport defects with reference to WT. First, βENaC-Tg mice exhibited consistently elevated Na+ transport rates, slightly waning with time (from 3- to 4-fold of WT mice at PND 3–10 to 1.5-fold of WT mice at PND 30–40), and normal capacity for regulated Cl− secretion. Second, ΔF508 CF mice exhibited persistent defects in basal Cl− secretion, abnormal forskolin-regulated secretion in neonates but not adults, persistent upregulation of UTP-regulated Cl− secretion and normal Na+ transport. Third, ΔF508 CF/βENaC-Tg exhibited the combined bioelectric hallmarks of βENaC-Tg and ΔF508 CF mouse airways (Fig. 2A), i.e., increased amiloride-sensitive Isc, an index of raised Na+ transport, and reduced postamiloride residual current, an index of decreased Cl− secretion. This pattern was observed in mice at PND 3 and was similar at PND 10 and PND 30–40 (Fig. 2, B and C). Notably, a selective increase in Na+ transport (βENaC-Tg mice) was associated with moderate lung disease, whereas a selective defect in Cl− secretion (ΔF508 CF mice) was not associated with disease. Importantly, despite the apparent absence of disease in ΔF508 CF mice, the combined defects in both Na+ absorption and Cl− secretion in ΔF508 CF/βENaC mice were associated with severe airways pathology.
The combined Na+ and Cl− transport defects could account for increased disease severity in ΔF508 CF/βENaC mice by multiple mechanisms. With respect to decreased survival, we speculate that mucus concentration was increased in ΔF508 CF/βENaC mice due to the combined airway surface liquid (ASL) volume deficits resulting from abnormalities in both Na+ and Cl− transport. Although direct measurements of mucus concentration in neonatal airways are not yet feasible, a recent report from Johannesson et al. (20) found increased intraluminal mucus content in the tracheas of Cftr-deficient βENaC-Tg mice compared with βENaC-Tg mice (4), a finding consistent with increased mucus adhesion to tracheal surfaces due to increased mucus concentration. Because tracheal mucus plugging is the dominant cause of death in neonatal βENaC-Tg mice, increased airway obstruction from dehydrated, i.e., concentrated, mucus likely contributed to the increased mortality of ΔF508 CF/βENaC-Tg mice. It is also plausible that the cartilage defects characteristic of CF mice contributed to poor survival of ΔF508 CF/βENaC mice if tracheal occlusion occurred in the context of dehydrated, adhesive mucus lining their excessively compliant tracheal walls.
The combined Na+ and Cl− transport defects may have also determined the increased incidence of club cell necrotic degeneration observed in ΔF508 CF/βENaC-Tg mice (Fig. 4). Previous studies have shown that club cell necrosis in the intrapulmonary airways of neonatal βENaC mice is strictly dependent on the βENaC transgene function (26) and resembles that reported in nematode neurons expressing hyperactive degenerin Na+ channels (15). We speculate that the increased abundance of necrotic cells in the airways of neonatal ΔF508 CF/βENaC mice reflected the absence of Cftr-dependent compensation for hyperactive/dysregulated βENaC-dependent club cell swelling. For example, in response to Na+-dependent cell swelling, airway epithelial cells exhibit a regulatory volume decrease response that involves release (“dumping”) of intracellular KCl (36). Genetic removal of Cftr could decrease the capacity of club cells to release intracellular Cl−, limiting their compensatory responses to ENaC-mediated unrestrained Na+ entry and increasing the likelihood of necrotic cell death. It is also possible that the more severe proximal airways mucus plugging and local hypoxia in ΔF508 CF/βENaC mice could also have increased the incidence of necrotic degeneration.
With respect to the increase inflammatory burden observed in ΔF508 CF/βENaC-Tg mice, the increased number of necrotic cells likely triggered inflammation by the IL-1R/MyD88 signaling pathway (5). Activation of this inflammatory cascade, coupled with inefficient removal of debris by mucus clearance, could produce the massive recruitment of neutrophils observed in ΔF508 CF/βENaC-Tg neonatal mice. Interestingly, the large intraluminal neutrophil influx in ΔF508 CF/βENaC-Tg mice correlated with higher BALF levels of IL-6 but was not paralleled by an increase in the levels of neutrophil chemoattractants, i.e., KC, MIP-2, or LIX, or other inflammatory mediators (Fig. 6). Increased levels of other neutrophil chemoattractants, i.e., high mobility box 1 (HMGB1) and the tripeptide proline-glycine-proline (PGP), both previously described in βENaC-Tg mice BALF (40), could have been responsible for the higher neutrophil influx exhibited by ΔF508 CF/βENaC-Tg mice, but their concentration was not assessed in the neonatal samples because of the small volume of BALF available.
In addition to sterile inflammation driven by necrotic cell death, other variables might have also contributed to the increased inflammation observed in neonatal ΔF508 CF/βENaC-Tg mice, such as bacterial burden. On the basis of quantitative bacterial cultures, no significant differences were observed in bacterial load between βENaC-Tg and ΔF508 CF/βENaC-Tg mice. These data suggest that there are no Cftr-specific defects in bacterial clearance superimposed on the muco-obstructive phenotype exhibited by βENaC-Tg mice. However, the massive neutrophilic infiltrate found in the airways of ΔF508 CF/βENaC-Tg mice, possibly recruited in response to increased epithelial necrosis, might have cleared a fraction of the bacterial burden in ΔF508 CF/βENaC-Tg mice, reducing CFUs numbers. Alternatively, as noted above for neutrophil counts, an incomplete retrieval of intraluminal contents by BAL due to patchy inflammatory airway obstructions might have decreased the recovery of bacteria in ΔF508 CF/βENaC-Tg mice, again leading to an underestimation of bacterial numbers. Thus a definitive conclusion regarding the absence of differences in bacterial load or lung microflora composition in ΔF508 CF/βENaC-Tg vs. βENaC-Tg mice may await more complete, culture-independent, microbiome analyses.
Cftr-deficient mice have been reported to have immunological defects, including altered macrophage function (3) and hyperinflammation (10, 23). However, the absence of profound differences in cytokine profiles between neonatal ΔF508 CF/βENaC-Tg and βENaC-Tg mice, as well as the absence of a proinflammatory signature in neonatal CF mice compared with WT mice, may argue against a dominant effect of CFTR-specific inflammatory pathways in determining the increased inflammatory response in the lungs of ΔF508 CF/βENaC-Tg mice (Fig. 6).
The etiology of eosinophilic crystalline pneumonia, a subclinical to fatal idiopathic disease that occurs spontaneously in inbred C57BL/6 and 129/Sv mice, remains elusive. However, this condition is known to develop in conjunction with other pulmonary diseases, and its severity tends to increase with age (18). Here, we report that eosinophilic crystalline pneumonia occurred in aged (10 mo) ΔF508 CF/βENaC-Tg mice only. This phenotype was associated with abundant production of YM1/2, members of the chitinase family associated with Th2 type inflammation in asthma and chronic obstructive pulmonary disease (16, 19, 24), and of CCSP, a small anti-inflammatory protein recently found to be involved in the regulation of macrophage function (41).
This paper represents the third report describing comparisons and/or interactions of the βENaC-Tg mouse model with other mouse models of airway ion transport processes. In the first report, the βENaC-Tg mouse was compared with mice bearing the Liddle's gain-of-function mutation in the ENaC β subunit (32). Although both βENaC-Tg and Liddle's mice exhibited elevated Na+ transport as measured in Ussing chambers, assessment of ASL volumes by confocal microscopy under “thin film” conditions revealed that ASL volume-dependent regulation of Na+ transport was preserved in Liddle's mice but not in βENaC-Tg mice. Importantly, the absence of volume-dependent regulation on ENaC function correlated with the presence of muco-obstructive lung disease.
The second report described the effects of club cell-targeted transgenic over expression of human CFTR in WT mice or in combination with the βENaC transgene (hCFTR/βENaC double transgenic mice) (12). These studies showed that expression of hCFTR-Tg produced increased Cl− secretion as measured in Ussing chambers under voltage-clamp conditions (which can generate driving forces for Cl− secretion) but failed to restore volume secretion in hCFTR/βENaC airway preparations, as assessed by thin film ASL microscopy. Again, the failure of hCFTR-Tg to restore ASL volume correlated with the failure to modulate the severity of βENaC-Tg muco-obstructive lung disease. An explanation for the failure of club cell-targeted hCFTR to restore volume secretion is that in the context of βENaC-Tg club cells, the unregulated βENaC channel prevented the generation of driving forces for Cl− secretion, so the magnitude of apical Cl− conductance was irrelevant (12, 32, 45).
In this study, we report that deletion of Cftr function in all cell types within the pulmonary epithelium increased the severity of the βENaC-Tg lung phenotype. On the basis of analogy to the hCFTR transgenic studies mentioned above, the absence of functional Cftr in club cells would not be predicted to add to the severity of the dehydration insult, owing to the absence of Cl− secretion driving forces in this cell type. However, it is likely that Cftr is also expressed in other cell types, including ciliated cells. Endogenous Cftr, coexpressed with WT ENaC in ciliated cells, is predicted to respond to ASL volume depletion with Cl− secretion. This response, however, would be absent in ΔF508 CF/βENaC-Tg mice, adding a new component to airway mucus dehydration. In preliminary studies, we have observed that double-transgenic βγENaC-Tg mice, obtained by crossing βENaC-Tg and γENaC-Tg mice, exhibited a twofold increase in Na+ transport compared with βENaC-Tg mice and had worse survival and lung phenotype (29), suggesting that the βENaC phenotype can indeed be “worsened” in response to more severe airway surface volume depletion.
Of note, it is also possible that absent Cftr function in a different lung region, i.e., the alveolus, may contribute to airway dehydration in the ΔF508 CF/βENaC-Tg mouse. Previous studies have suggested that CFTR contributes to alveolar secretion (2, 25), and its absence enhances ENaC activity in alveolar epithelial cells of ΔF508 and null CF mice (22). Although asymptomatic in ΔF508 CF mice, the reduction in alveolar secretion moving onto airways surfaces might exacerbate the severity of airway mucus dehydration in βENaC-Tg mice. The presence of a striking alveolar disease in older ΔF508 CF/βENaC-Tg mice (Fig. 5) is consistent with small airways or alveolar secretory defect.
In conclusion, generation of congenic ΔF508 CF/βENaC-Tg mice has produced an animal model with an increased severity of lung disease, consistent with the prediction that the combination of two airway epithelial ion transport defects would additively act to reduce ASL volume/airway surface hydration. This animal model will be useful 1) to test hypotheses identifying the spectrum of CFTR-dependent mechanisms that may be responsible for the severe lung inflammation observed in CF and 2) to develop both ENaC/CFTR-specific and nonspecific anti-inflammatory molecules as therapies for CF lung disease.
GRANTS
This study was funded by Cystic Fibrosis Foundation (CFF) grant RANDEL07P0 (to S. H. Randell), CFF grant LIVRAG08I0 (to A. Livraghi-Butrico), National Institute of Health (NIH) P30 DK065988 and CFF grant R026-CR02 (to W. K. O'Neal), and NIH grants P50 HL060280, P01 HL034322, P30 DK065988, and P50 HL084934 (to R. C. Boucher).
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author(s).
AUTHOR CONTRIBUTIONS
A.L.-B., R.C.B., W.K.O., and B.R.G. conception and design of research; A.L.-B., E.J.K., K.J.W., T.D.R., R.C.G., and B.R.G. performed experiments; A.L.-B., T.D.R., and B.R.G. analyzed data; A.L.-B., J.R.H., S.H.R., R.C.B., W.K.O., and B.R.G. interpreted results of experiments; A.L.-B. prepared figures; A.L.-B., W.K.O., and B.R.G. drafted manuscript; A.L.-B., J.R.H., S.H.R., R.C.B., W.K.O., and B.R.G. edited and revised manuscript; A.L.-B., E.J.K., K.J.W., R.C.G., J.R.H., S.H.R., R.C.B., W.K.O., and B.R.G. approved final version of manuscript.
ACKNOWLEDGMENTS
The authors thank Kimberly Burns, Donald Joyner, Tracy Eldred, and Lori Bramble for outstanding technical assistance with histology and immunohistochemistry; Brian Brighton for performing morphometric analysis of necrotic epithelial cells; the UNC Michael Hooker Microscopy Facility, funded by an anonymous private donor, for assistance with imaging; and the Thurston Arthritis Research Center, Clinical Proteomics Laboratory for Luminex assays.
REFERENCES
- 1. Bonvin E, Le Rouzic P, Bernaudin JF, Cottart CH, Vandebrouck C, Crie A, Leal T, Clement A, Bonora M. Congenital tracheal malformation in cystic fibrosis transmembrane conductance regulator-deficient mice. J Physiol 586: 3231–3243, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bove PF, Grubb BR, Okada SF, Ribeiro CM, Rogers TD, Randell SH, O'Neal WK, Boucher RC. Human alveolar type II cells secrete and absorb liquid in response to local nucleotide signaling. J Biol Chem 285: 34939–34949, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bruscia EM, Zhang PX, Ferreira E, Caputo C, Emerson JW, Tuck D, Krause DS, Egan ME. Macrophages directly contribute to the exaggerated inflammatory response in cystic fibrosis transmembrane conductance regulator-/- mice. Am J Respir Cell Mol Biol 40: 295–304, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Button B, Cai LH, Ehre C, Kesimer M, Hill DB, Sheehan JK, Boucher RC, Rubinstein M. A periciliary brush promotes the lung health by separating the mucus layer from airway epithelia. Science 337: 937–941, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chen CJ, Kono H, Golenbock D, Reed G, Akira S, Rock KL. Identification of a key pathway required for the sterile inflammatory response triggered by dying cells. Nat Med 13: 851–856, 2007 [DOI] [PubMed] [Google Scholar]
- 6. Chen JH, Stoltz DA, Karp PH, Ernst SE, Pezzulo AA, Moninger TO, Rector MV, Reznikov LR, Launspach JL, Chaloner K, Zabner J, Welsh MJ. Loss of anion transport without increased sodium absorption characterizes newborn porcine cystic fibrosis airway epithelia. Cell 143: 911–923, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Clarke LL, Gawenis LR, Franklin CL, Harline MC. Increased survival of CFTR knockout mice with an oral osmotic laxative. Lab Anim Sci 46: 612–618, 1996 [PubMed] [Google Scholar]
- 8. Cruzan G, Bus J, Hotchkiss J, Harkema J, Banton M, Sarang S. CYP2F2-generated metabolites, not styrene oxide, are a key event mediating the mode of action of styrene-induced mouse lung tumors. Regul Toxicol Pharmacol 62: 214–220, 2012 [DOI] [PubMed] [Google Scholar]
- 9. Donaldson SH, Boucher RC. Sodium channels and cystic fibrosis. Chest 132: 1631–1636, 2007 [DOI] [PubMed] [Google Scholar]
- 10. Durie PR, Kent G, Phillips MJ, Ackerley CA. Characteristic multiorgan pathology of cystic fibrosis in a long-living cystic fibrosis transmembrane regulator knockout murine model. Am J Pathol 164: 1481–1493, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Grubb BR, Gabriel SE. Intestinal physiology and pathology in gene-targeted mouse models of cystic fibrosis. Am J Physiol Gastrointest Liver Physiol 273: G258–G266, 1997 [DOI] [PubMed] [Google Scholar]
- 12. Grubb BR, O'Neal WK, Ostrowski LE, Kreda SM, Button B, Boucher RC. Transgenic hCFTR expression fails to correct β-ENaC mouse lung disease. Am J Physiol Lung Cell Mol Physiol 302: L238–L247, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Grubb BR, Paradiso AM, Boucher RC. Anomalies in ion transport in CF mouse tracheal epithelium. Am J Physiol Cell Physiol 267: C293–C300, 1994 [DOI] [PubMed] [Google Scholar]
- 14. Guilbault C, Saeed Z, Downey GP, Radzioch D. Cystic fibrosis mouse models. Am J Respir Cell Mol Biol 36: 1–7, 2006 [DOI] [PubMed] [Google Scholar]
- 15. Hall DH, Gu G, Garcia-Anoveros J, Gong L, Chalfie M, Driscoll M. Neuropathology of degenerative cell death in Caenorhabditis elegans. J Neurosci 17: 1033–1045, 1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hartl D, Lee CG, Da Silva CA, Chupp GL, Elias JA. Novel biomarkers in asthma: chemokines and chitinase-like proteins. Curr Opin Allergy Clin Immunol 9: 60–66, 2009 [DOI] [PubMed] [Google Scholar]
- 17. Hodges CA, Grady BR, Mishra K, Cotton CU, Drumm ML. Cystic fibrosis growth retardation is not correlated with loss of Cftr in the intestinal epithelium. Am J Physiol Gastrointest Liver Physiol 301: G528–G536, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hoenerhoff MJ, Starost MF, Ward JM. Eosinophilic crystalline pneumonia as a major cause of death in 129S4/SvJae mice. Vet Pathol 43: 682–688, 2006 [DOI] [PubMed] [Google Scholar]
- 19. Homer RJ, Zhu Z, Cohn L, Lee CG, White WI, Chen S, Elias JA. Differential expression of chitinases identify subsets of murine airway epithelial cells in allergic inflammation. Am J Physiol Lung Cell Mol Physiol 291: L502–L511, 2006 [DOI] [PubMed] [Google Scholar]
- 20. Johannesson B, Hirtz S, Schatterny J, Schultz C, Mall MA. CFTR regulates early pathogenesis of chronic obstructive lung disease in betaENaC-overexpressing mice. PLoS One 7: e44059, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kent G, Iles R, Bear CE, Huan LJ, Griesenbach U, McKerlie C, Frndova H, Ackerley C, Gosselin D, Radzioch D, O'Brodovich H, Tsui LC, Buchwald M, Tanswell AK. Lung disease in mice with cystic fibrosis. J Clin Invest 100: 3060–3069, 1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lazrak A, Jurkuvenaite A, Chen L, Keeling KM, Collawn JF, Bedwell DM, Matalon S. Enhancement of alveolar epithelial sodium channel activity with decreased cystic fibrosis transmembrane conductance regulator expression in mouse lung. Am J Physiol Lung Cell Mol Physiol 301: L557–L567, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Legssyer R, Huaux F, Lebacq J, Delos M, Marbaix E, Lebecque P, Lison D, Scholte BJ, Wallemacq P, Leal T. Azithromycin reduces spontaneous and induced inflammation in DeltaF508 cystic fibrosis mice. Respir Res 7: 134, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Letuve S, Kozhich A, Humbles A, Brewah Y, Dombret MC, Grandsaigne M, Adle H, Kolbeck R, Aubier M, Coyle AJ, Pretolani M. Lung chitinolytic activity and chitotriosidase are elevated in chronic obstructive pulmonary disease and contribute to lung inflammation. Am J Pathol 176: 638–649, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lindert J, Perlman CE, Parthasarathi K, Bhattacharya J. Chloride-dependent secretion of alveolar wall liquid determined by optical-sectioning microscopy. Am J Respir Cell Mol Biol 36: 688–696, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Livraghi-Butrico A, Grubb BR, Kelly EJ, Wilkinson KJ, Yang H, Geiser M, Randell SH, Boucher RC, O'Neal WK. Genetically determined heterogeneity of lung disease in a mouse model of airway mucus obstruction. Physiol Genomics 44: 470–484, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Livraghi-Butrico A, Kelly EJ, Klem ER, Dang H, Wolfgang MC, Boucher RC, Randell SH, O'Neal WK. Mucus clearance, MyD88-dependent and MyD88-independent immunity modulate lung susceptibility to spontaneous bacterial infection and inflammation. Mucosal Immunol 5: 397–408, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Livraghi A, Grubb BR, Hudson EJ, Wilkinson KJ, Sheehan JK, Mall MA, O'Neal WK, Boucher RC, Randell SH. Airway and lung pathology due to mucosal surface dehydration in β-epithelial Na+ channel-overexpressing mice: role of TNF-α and IL-4Rα signaling, influence of neonatal development, and limited efficacy of glucocorticoid treatment. J Immunol 182: 4357–4367, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Livraghi A, O'Neal WK, Mall M, Boucher RC, Grubb BR. Enhanced Na+ absorption in the double transgenic ENaC mouse Scnn1bg correlates with severity of lung pathology (Abstract 219). In: Abstracts of the 20th Annual North American Cystic Fibrosis Conference, November 2–5, 2006, Denver, Colorado, USA. Pediatr Pulmonol Suppl 29: 209–415, 2006 [Google Scholar]
- 30. Livraghi A, Randell SH. Cystic fibrosis and other respiratory diseases of impaired mucus clearance. Toxicol Pathol 35: 116–129, 2007 [DOI] [PubMed] [Google Scholar]
- 31. Mall M, Grubb BR, Harkema JR, O'Neal WK, Boucher RC. Increased airway epithelial Na+ absorption produces cystic fibrosis-like lung disease in mice. Nat Med 10: 487–493, 2004 [DOI] [PubMed] [Google Scholar]
- 32. Mall MA, Button B, Johannesson B, Zhou Z, Livraghi A, Caldwell RA, Schubert SC, Schultz C, O'Neal WK, Pradervand S, Hummler E, Rossier BC, Grubb BR, Boucher RC. Airway surface liquid volume regulation determines different airway phenotypes in Liddle compared with betaENaC-overexpressing mice. J Biol Chem 285: 26945–26955, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mall MA, Harkema JR, Trojanek JB, Treis D, Livraghi A, Schubert S, Zhou Z, Kreda SM, Tilley SL, Hudson EJ, O'Neal WK, Boucher RC. Development of chronic bronchitis and emphysema in beta-epithelial Na+ channel-overexpressing mice. Am J Respir Crit Care Med 177: 730–742, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Matsui H, Grubb BR, Tarran R, Randell SH, Gatzy JT, Davis CW, Boucher RC. Evidence for periciliary liquid layer depletion, not abnormal ion composition, in the pathogenesis of cystic fibrosis airways disease. Cell 95: 1005–1015, 1998 [DOI] [PubMed] [Google Scholar]
- 35. Meyerholz DK, Stoltz DA, Namati E, Ramachandran S, Pezzulo AA, Smith AR, Rector MV, Suter MJ, Kao S, McLennan G, Tearney GJ, Zabner J, McCray PB, Jr, Welsh MJ. Loss of cystic fibrosis transmembrane conductance regulator function produces abnormalities in tracheal development in neonatal pigs and young children. Am J Respir Crit Care Med 182: 1251–1261, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Okada SF, Nicholas RA, Kreda SM, Lazarowski ER, Boucher RC. Physiological regulation of ATP release at the apical surface of human airway epithelia. J Biol Chem 281: 22992–23002, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ostedgaard LS, Meyerholz DK, Chen JH, Pezzulo AA, Karp PH, Rokhlina T, Ernst SE, Hanfland RA, Reznikov LR, Ludwig PS, Rogan MP, Davis GJ, Dohrn CL, Wohlford-Lenane C, Taft PJ, Rector MV, Hornick E, Nassar BS, Samuel M, Zhang Y, Richter SS, Uc A, Shilyansky J, Prather RS, McCray PB, Jr, Zabner J, Welsh MJ, Stoltz DA. The DeltaF508 mutation causes CFTR misprocessing and cystic fibrosis-like disease in pigs. Sci Transl Med 3: 74ra24, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ostrowski LE, Yin W, Diggs PS, Rogers TD, O'Neal WK, Grubb BR. Expression of CFTR from a ciliated cell-specific promoter is ineffective at correcting nasal potential difference in CF mice. Gene Ther 14: 1492–1501, 2007 [DOI] [PubMed] [Google Scholar]
- 39. Rock JR, O'Neal WK, Gabriel SE, Randell SH, Harfe BD, Boucher RC, Grubb BR. Transmembrane protein 16A (TMEM16A) is a Ca2+-regulated Cl− secretory channel in mouse airways. J Biol Chem 284: 14875–14880, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Rowe SM, Jackson PL, Liu G, Hardison M, Livraghi A, Solomon GM, McQuaid DB, Noerager BD, Gaggar A, Clancy JP, O'Neal W, Sorscher EJ, Abraham E, Blalock JE. Potential role of high-mobility group box 1 in cystic fibrosis airway disease. Am J Respir Crit Care Med 178: 822–831, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Snyder JC, Reynolds SD, Hollingsworth JW, Li Z, Kaminski N, Stripp BR. Clara cells attenuate the inflammatory response through regulation of macrophage behavior. Am J Respir Cell Mol Biol 42: 161–171, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Tarran R, Button B, Picher M, Paradiso AM, Ribeiro CM, Lazarowski ER, Zhang L, Collins PL, Pickles RJ, Fredberg JJ, Boucher RC. Normal and cystic fibrosis airway surface liquid homeostasis. The effects of phasic shear stress and viral infections. J Biol Chem 280: 35751–35759, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Wielputz MO, Eichinger M, Zhou Z, Leotta K, Hirtz S, Bartling SH, Semmler W, Kauczor HU, Puderbach M, Mall MA. In vivo monitoring of cystic fibrosis-like lung disease in mice by volumetric computed tomography. Eur Respir J 38: 1060–1070, 2011 [DOI] [PubMed] [Google Scholar]
- 44. Wilke M, Buijs-Offerman RM, Aarbiou J, Colledge WH, Sheppard DN, Touqui L, Bot A, Jorna H, de Jonge HR, Scholte BJ. Mouse models of cystic fibrosis: phenotypic analysis and research applications. J Cyst Fibros 10, Suppl 2: S152–S171, 2011 [DOI] [PubMed] [Google Scholar]
- 45. Willumsen NJ, Davis CW, Boucher RC. Intracellular Cl− activity and cellular Cl− pathways in cultured human airway epithelium. Am J Physiol Cell Physiol 256: C1033–C1044, 1989 [DOI] [PubMed] [Google Scholar]
- 46. Zeiher BG, Eichwald E, Zabner J, Smith JJ, Puga AP, McCray PB, Jr, Capecchi MR, Welsh MJ, Thomas KR. A mouse model for the delta F508 allele of cystic fibrosis. J Clin Invest 96: 2051–2064, 1995 [DOI] [PMC free article] [PubMed] [Google Scholar]