Abstract
Objective
To summarize the literature describing computer-based interventions aimed at improving bidirectional communication between clinical and public health.
Materials and Methods
A systematic review of English articles using MEDLINE and Google Scholar. Search terms included public health, epidemiology, electronic health records, decision support, expert systems, and decision-making. Only articles that described the communication of information regarding emerging health threats from public health agencies to clinicians or provider organizations were included. Each article was independently reviewed by two authors.
Results
Ten peer-reviewed articles highlight a nascent but promising area of research and practice related to alerting clinicians about emerging threats. Current literature suggests that additional research and development in bidirectional communication infrastructure should focus on defining a coherent architecture, improving interoperability, establishing clear governance, and creating usable systems that will effectively deliver targeted, specific information to clinicians in support of patient and population decision-making.
Conclusions
Increasingly available clinical information systems make it possible to deliver timely, relevant knowledge to frontline clinicians in support of population health. Future work should focus on developing a flexible, interoperable infrastructure for bidirectional communications capable of integrating public health knowledge into clinical systems and workflows.
Keywords: Public health informatics; Disease Notification; Health Communication; Decision Support Systems, Clinical
Introduction
Computer-based clinical decision support (CDS) brings relevant knowledge to bear on decisions involving the health and wellbeing of a patient using the computer.1 The adoption of electronic health record (EHR) systems in hospitals and physician practices has introduced various forms of CDS into modern care delivery processes.2 Among other quality and safety outcomes, CDS is effective at improving clinician adherence to preventive care guidelines and alerting clinicians to potentially adverse medication outcomes.3–5
The definition of CDS can be broadened to include public health contexts and uses. Traditional examples of patient-centered CDS present clinicians with an alert or reminder when a laboratory value is out of the normal range or a prescribed medication might negatively interact with a patient's other medications. Imagine instead a clinician reading an electronic note from the local health department that describes a newly discovered contaminant in the water supply that impacts the neighborhoods near the clinic, placing her population of patients at risk of a waterborne illness. The note might suggest ordering stool samples for patients presenting with gastrointestinal symptoms. Throughout the day, when certain symptoms are entered into the computer, the EHR system would automatically recommend a stool culture by placing that test in the physician's order basket for review. This scenario is one example of what might be described as computer-based public health decision support, bringing relevant knowledge to bear on decisions involving the health and wellbeing of a population through the use of electronic information.
Adoption and use of clinical information systems and CDS is expected to increase significantly in the next few years given meaningful use incentives from the Centers for Medicare and Medicaid Services.6 The recently published final rule for stage 2 requires eligible hospitals and providers to implement CDS to improve performance on high-priority health conditions and healthcare efficiency.7 Meaningful use incentives further require eligible hospitals to submit reportable laboratory results and syndromic surveillance data electronically to public health agencies.
Increased adoption of advanced clinical systems consistent with the meaningful use requirements necessitates technologies to receive and process incoming electronic data and information into knowledge about a community, state, or nation. This is the role performed by surveillance, a core function of public health practice, which systematically collects, analyzes, and interprets data captured during routine clinical care.8 Public health traditionally has struggled to obtain accurate data consistently from clinical providers in a timely fashion.9–12 However, advances in EHR systems and the meaningful use criteria have spurred investment in a number of infrastructure projects to capture electronic data routinely from a variety of providers and clinical settings.13–16 Electronic methods that capture surveillance data from clinical settings have demonstrated improvements in public health agencies’ capabilities to monitor population health.17–21 A continued focus by the Centers for Disease Control and Prevention (CDC), among others, on increasing the adoption and use of technologies to capture and process electronic clinical data is expected in the coming years.22 23
To realize fully the potential of public health decision support, advanced clinical information systems must not only be able to send data to surveillance systems but also receive knowledge from public health. Electronically exchanging information both to and from public health, bidirectional communication,24 requires an infrastructure with components beyond those called for in meaningful use or available through existing systems such as the public health information network (PHIN).
Current public health infrastructures tend to focus on unidirectional approaches, maximizing the ability to gather and analyze surveillance data. When communicating back to providers, manually intensive methods are used. For example, when informing clinicians about events such as influenza severity and localized Salmonella outbreaks, a local health department sends printed letters via US postal mail. These messages are likely to arrive outside of clinical workflow, making the information unusable by frontline clinicians. Furthermore, current methods may render the information obsolete if clinicians do not read it until days or weeks after the threat to public health. To examine electronic, bidirectional communication infrastructures in support of public health decision support, we systematically reviewed articles that described the development, use, or evaluation of technologies that disseminated information from public health agencies to clinical providers.
Methods
We sought to identify articles describing computer-based interventions aimed at improving bidirectional communication. Two independent searches were performed in April 2010 and December 2011 of the English-language indexed and non-indexed literature in MEDLINE (1948 to December 2011) using a broad set of public health and informatics terms to maximize sensitivity. Keywords included, but were not limited to, the following: public health, epidemiology, preventative medicine, public health practice, EHRs, CDS, decision support, expert systems, and decision-making. We used MEDLINE search functionality, including the use of MeSH tree structures to broaden the scope of the searches and various combinations of the keywords using Boolean logic. Articles not available through MEDLINE were identified by searching Google Scholar, the Online Journal of Public Health Informatics, as well as personal bibliographies of the authors.
Eligibility criteria were used to identify articles that principally discuss the ability of public health to communicate information to providers using the internet or clinical information systems. Known approaches to disseminating public health knowledge to clinicians using the internet, such as using a health alert network (HAN), were targeted for inclusion. Other articles were selected if they contained specific terminology, such as ‘bidirectional communication’ and ‘situational awareness’, or if they focused on disseminating information about an emerging health threat to providers. Providers could access information from public health either through an EHR system, inbox, or other clinical information system. Information could be routed to providers automatically or via processes with manual components.
Eligibility assessment was performed independently using an unblinded, standardized manner by two reviewers. Disagreements between reviewers were resolved by consensus. Reviewers screened titles and abstracts of candidate articles identified through the use of the advanced MEDLINE search functions. Few articles (less than 10%) required full-text review to apply eligibility criteria.
Articles were synthesized using qualitative methods as our objective was to characterize approaches as opposed to summarize outcomes across trials. Two authors independently reviewed the full text of selected articles. Emergent themes were identified and summarized using analytic notes. The reviewers exchanged and discussed notes to formulate a final synthesis. Disagreements between reviewers were resolved by consensus.
Results
Study selection
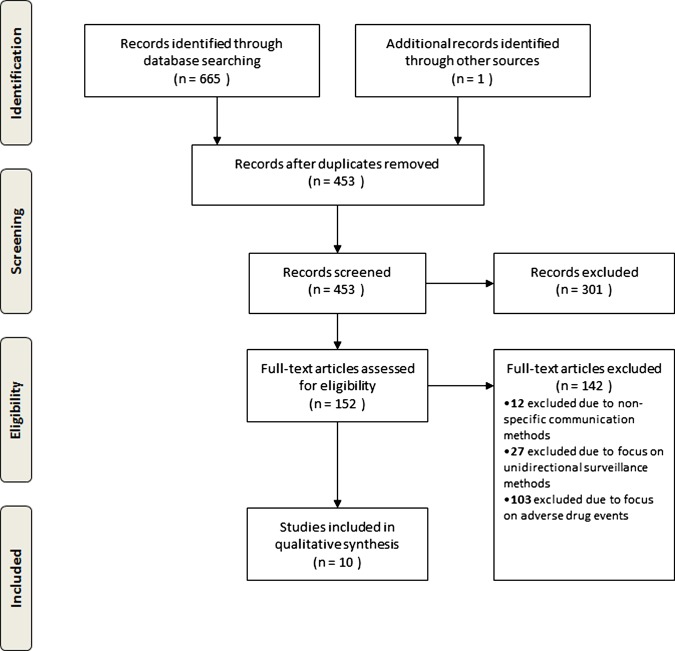
Preliminary searches of the literature for broad MeSH term phrases returned large numbers of articles. Public Health, CDS, and electronic medical record term phrases returned 123 663, 8436, and 20 444 articles, respectively. Boolean logic was applied to narrow the candidate pool to just a few hundred articles. We then reviewed the titles and abstracts of the candidate articles, applying eligibility and exclusion criteria. This process narrowed the results to 10 articles. The article selection process is summarized in figure 1.
Figure 1.
PRISMA flow diagram outlining manuscript selection process.
Articles focusing on adverse drug events are often indexed in MEDLINE using CDS or public health terms because they describe surveillance of a population for real or potential adverse events. While this is important work that contributes to the advancement of population health monitoring and decision support methodologies, it is outside the scope of this review and such articles were excluded. Articles were further excluded if they were focused solely on unidirectional surveillance methods, including statistical methods for identifying a disease outbreak or the capability to send surveillance data from clinical information systems to public health agencies. Finally, we excluded articles whose primary channel for data exchange between public health and clinicians was face-to-face communication or a broad but non-specific mailing, such as an e-newsletter updating subscribers on general health department activities.
Study characteristics
A search of the public health and informatics peer-reviewed literature revealed 10 articles whose primary subject was bidirectional communication between public health and clinicians. These articles are summarized in table 1. The table identifies the year of publication, methods described in each article to reach a specific target user audience, and target diseases if applicable. Article publication dates spanned a decade (2001–11), with half the articles published within the past 3 years (2009–11). A broad range of methods, target users, and target diseases can be found in the small set of articles.
Table 1.
Selected articles and their major characteristics
| Article | Year | Methods | Target users | Diseases |
|---|---|---|---|---|
| Amirfar et al32 | 2011 | EHR | Physicians | Various |
| Baker and Porter25 | 2005 | HAN | Public health workers | NS |
| Daniel et al24 | 2005 | HAN | Clinicians Epidemiologists | Neurologic Lower gastrointestinal Respiratory |
| Doniger et al27 | 2001 | HAN | Clinicians Emergency management services Government officials Public health workers |
NS |
| Gamache et al33 | 2010 | EHR | Clinicians | Various |
| Garrett and Yasnoff28 | 2002 | EHR | Clinicians | Various |
| Hanrahan et al26 | 2004 | HAN | Physicians (primary care) Public health laboratories Public health workers |
NS |
| Lombardo et al29 | 2009 | EHR | Clinicians | NS |
| Lurio et al30 | 2010 | EHR | Clinicians | Legionella Escherichia coli Measles |
| Young31 | 2010 | EHR | Physicians | H1N1 |
EHR, electronic health record; HAN, health alert network; NS, not specified.
Results of individual studies
The 10 articles describe a wide variety of computer-based interventions to disseminate knowledge regarding an emerging public health threat to care providers. The articles were classified into two primary groups. The first group described the use of a HAN to alert clinicians rapidly, often immediately, following the detection of an aberration (eg, increase in the number of influenza-like illness symptoms) or a natural disaster (eg, hurricane).25 The second group described methods to alert clinicians at the point-of-care via EHR or clinical information systems. Alerts were typically communicated following an initial public health investigation. Each set of articles contained a mix of evaluation studies and articles describing bidirectional communication processes or technical architectures that enabled communication.
Group 1: HAN approaches (4 articles)
Four of the selected articles described HAN designed to alert public health agencies, clinicians, and emergency management personnel rapidly during a public health event. Three of the four articles describe the architecture and methods designed to alert target users of the HAN.24 26 27 These articles discuss the development and deployment (planned or actual) of a web-based portal that serves as the nucleus of the HAN. The portals in all three cases provide a range of services, such as alerting the user through a range of modalities including email, facsimile, and alphanumeric pager. The HAN portals further provide a platform for collaboration in which users can post documents and participate in community forums. Daniel et al24 specifically referred to the collaborative aspects of the HAN as ‘bidirectional communication’. In the Massachusetts HAN, a significant syndromic surveillance event (eg, a dramatic increase in influenza-like illness symptoms) triggers the local public health jurisdiction to post a note to the HAN portal. The note details the cluster that generated the alert (eg, age ranges, genders, zip codes), and other HAN users can log in, view the information, and discuss.
Of the four articles, only Daniel et al24 provided data and discussed the use of the HAN to alert users regarding a real, emerging public health event. The article presents three case studies describing how the HAN was utilized. In all cases, an increase in the number of reported symptoms for a given category of illness produced an alert to the HAN user community. Within 3–4 h of the alert, a clinical responder pulled the affected patients’ medical records and posted a de-identified list of abstracted medical data for epidemiologist review. In each case, epidemiologic review ruled out the need for further investigation.
Group 2: EHR-based alerting approaches (6 articles)
Six articles describe approaches in which knowledge about emerging health threats and population health was disseminated through EHR systems.28–33 Three of the articles focused on describing either how EHR systems might support28 or the development of a system designed to support29 32 bidirectional communication. Garrett and Yasnoff28 examined public health guidelines to determine if they were ‘suitable’ for implementation within an EHR system. Amirfar et al32 described the process by which the New York City Department of Mental Health and Hygiene developed and deployed 40 public health decision support alerts, such as screening measures for influenza and pneumococcal vaccines, to more than 2000 physicians via commercial EHR systems. Lombardo et al29 reported the design and development of a prototype wherein clinicians access a knowledge repository of alerts created by various public health agencies through their EHR systems. The repository contains not only details on a given outbreak (eg, increased laboratory reports of Salmonella in a given jurisdiction) but also treatment guidelines from the CDC with recommended actions for treating patients in the affected area who present with similar symptoms.
The other three articles30 31 33 describe the development and initial evaluation of bidirectional communication infrastructures wherein clinicians receive public health knowledge through their EHR system or a health information exchange. In Lurio et al,30 a large ambulatory practice implemented a process by which emerging public health threats trigger the creation and display of CDS alerts. The alerts are created manually following receipt of a message via the HAN to a member of the clinical leadership. Alerts are triggered based on patient signs and symptoms, and the alert is presented to clinicians during a patient encounter. Recommended laboratory and medication order sets accompanied the alert. The article presents three case examples that occurred over an 8-month period. In one case, a multistate outbreak of Escherichia coli from contaminated ground beef resulted in alerts during 287 patient encounters. Clinicians ordered Shiga-toxin assays and routine stool cultures in response to 65 (22.6%) alerts. However, no instances of E coli were confirmed by the laboratory. Clinicians responded similarly to the other alerts described in the article.
In Young,31 the medical director at an academic health system translates knowledge communicated in daily public health emails into a clinical reminder. The case involved rapidly changing case definitions and other guidance from public health regarding the H1N1 pandemic. Clinicians type a shorthand command within the EHR to access the most up-to-date H1N1 protocol. The protocol informed clinicians about who to test, how to test, indications for treatment, and so forth. A survey of a small sample of clinicians following deployment of the protocol revealed that many clinicians were either unaware of the protocol or never used it.
In Gamache et al,33 personnel at the local health department used software provided by the regional health information exchange to communicate alerts to clinicians. Clinicians received the alerts through their EHR system or via fax, depending on the technology capability of the practice. In the first of two cases described, the health department sent messages regarding H1N1 protocols to advise clinicians on who to test, how to test, indications for treatment, and so forth. In the second case, the health department provided routine updates on a localized outbreak of Chlamydia. The study collected data on physician testing behavior in response to messages and local health department costs associated with paper versus electronic messaging. Physician testing for H1N1 went down following receipt of updated testing guidance, but there was no change in testing rates following the Chlamydia messages. Estimated cost savings were observed to be approximately US$1.17 per message.
Synthesis of results
Our analysis of the selected articles suggests four key areas important for future research and development of bidirectional communication infrastructures: architecture, interoperability, governance, and usability. These themes emerged across studies and groups to define a coherent set of items facing surveillance and informatics professionals who desire to leverage modern information technologies to enhance clinical decision-making during emergent public health events.
Architecture
Technical architecture is important given the myriad disparate clinical and public health information systems in use across the country. The technical architectures described in the selected articles varied, suggesting there is little consensus on the best practices for bidirectional communication between public health and medicine. HAN approaches generally employed a central web server in which users logged in to view details for an alert pushed out via integrated email, fax, and alphanumeric pager systems.26 27 EHR articles described public health alerts that were input into existing CDS systems deployed within the clinical enterprise. In Lombardo et al,29 a web services architecture was deployed to allow commercial EHR systems to connect to a centralized repository of public health alerts. In Gamache et al,33 commercial EHR systems already connected to a health information exchange received information through a single connection point at the local health department.
Future bidirectional communication architectures will need to connect clinical systems with public health systems, and they will need to scale from local health departments to the CDC. Bidirectional communication architectures should consider how to leverage these connections, when possible, to enable information to be sent back to clinical systems. These architectures will further need to consider how to leverage existing national infrastructures, such as PHIN and the nationwide health information network, although new components may be necessary to reach the last mile of connectivity between clinical and public health. Finally, other architectural considerations, including security, customization, and scope, will need to be considered, developed, and tested.34
Interoperability
To be effective and widely adopted, bidirectional communication infrastructures will need both semantic and system interoperability. Semantic interoperability has been defined as ‘the ability to import utterances from another computer without prior negotiation, and have your decision support, data queries and business rules continue to work reliably against these utterances’.35 Guidance on semantic interoperability and how best to represent public health knowledge was absent in the discussion of the selected articles. Articles by Garrett and Yasnoff28 and Lombardo et al29 described the potential for a repository of public health knowledge. However, neither article discussed standardized knowledge representation within the repository, nor did the articles address how standardized knowledge could be disseminated among various jurisdictions. These are issues that must be addressed, and their resolution should be coordinated with similar efforts occurring in the clinical community to avoid duplicative systems.36 37
In addition, bidirectional communication will require system interoperability, or the ability to exchange transactional messages with other connected information systems. In Lombardo et al,29 the authors described the use of the health level 7 Infobutton transaction, a recognized standard in clinical systems. Using an Infobutton approach, the knowledge repository was able to interoperate successfully with systems at the CDC, the Regenstrief Institute, and two commercial EHR systems. In Gamache et al,33 a different variety of health level 7 transaction messages were used to deliver information to commercial EHR systems. While these specifications were effective for their respective demonstrations, future bidirectional communication methods may define new use cases that go beyond these approaches. Furthermore, alignment of bidirectional communication standards with efforts including but not limited to PHIN, the nationwide health information network and the federal standards and interoperability framework38 will need to be considered.
Governance
Given different cultures and policies informing clinical and public health, appropriate governance is needed to distribute and manage disparate systems and the information and knowledge captured, stored, and communicated by those systems. Without governance, technologies simply create, maintain, and make available disconnected fragments of knowledge. The selected articles initiate discussion of important governance concepts, yet the articles leave many questions unanswered. For example, should states and/or the CDC build and maintain centralized knowledge repositories? Furthermore, what role, if any, do regional health information exchange organizations play in facilitating the creation of new alerts or the retrieval of alerts from public health repositories?
Several articles describe automated alerts based on syndromic surveillance system detection methods,24 27 30 while other articles describe manual processes to review syndromic signals before alerting end users.29 30 33 Public health agencies are likely to be the source of alerts and control their dissemination to clinical providers like those in Gamache et al.33 However, public health professionals should be aware of clinicians’ concerns about receiving false positive alerts, a known challenge with syndromic surveillance systems,39 and work to ensure HAN and similar distributed systems deliver only those alerts that are likely to improve patient care and are immediately actionable by the clinician. Human review within clinical institutions, or more sophisticated technological processes to ensure alerts are not superfluous, may be necessary to prevent ‘alert fatigue’.
Furthermore, information and knowledge become outdated over time. Effective policies and active knowledge management40 41 of bidirectional communication systems will be needed to provide for updates, deprecation, and expunging of guidelines, rules, and alerts. The active management will be critically important, as many public health alerts are likely to be temporary and local in nature (eg, food-borne outbreak in specific zip codes). If knowledge is distributed across levels of public health, each level will need to have policies and procedures in place to steward its knowledge base.
Usability
Adoption of bidirectional communication infrastructures will probably occur only if the information sent from public health is useful and usable to clinicians. The articles in this review highlight that not all alerts impact physician behavior. In Lurio et al,30 utilization of the public health knowledge-based alerts ranged from 2 to 22%. Gamache et al33 found that emergent alerts were associated more strongly with clinician responses than alerts regarding repeated, chronic outbreaks of a disease. Screenshots in Lombardo et al29 show the alert text filled more than a single screen, requiring clinician users to scroll past background information on the outbreak to access recommended actions. Furthermore, recommendations were not linked to clinical order sets within the EHR system, an approach that may increase the likelihood for action.
Disseminating alerts that physicians find confusing or unactionable may result in increased cognitive burden for busy clinicians who are currently presented with a variety of prompts and reminders.42 Focusing on usability, the extent to which a system or application can be used to achieve specified goals with effectiveness, efficiency and satisfaction in a specified context of use,43 can help bidirectional communications system and application developers create technologies that will enhance patient and population health while minimizing burden on system users.44 45
Discussion
We performed a systematic review of computer-based approaches that support bidirectional communication between clinical and public health. We identified few (N=10) examples, and only four presented data from an evaluation of an implemented intervention.
For those articles in which an evaluation was performed, conclusions were mixed. Bidirectional communication infrastructure demonstrated capacity to leverage information technologies to deliver timely messages during an emergent public health event. In Lurio et al,30 Gamache et al33 and Young,31 processing and disseminating public health alerts as well as new information about existing events appeared to be a manageable task. Similarly, Daniel et al24 found that clinicians were able to collaborate effectively with epidemiologists using a HAN to triage public health alerts. On the other hand, bidirectional communication mechanisms were not very effective at changing clinicians’ behavior or population outcomes. The alerts in Lurio et al,30 for example, did not significantly impact clinician response in the cases of Legionella and measles. In Young,31 few clinicians were aware of the protocol or chose not to use it. Alerts for a chronic outbreak of Chlamydia appeared to have no effect in Gamache et al.33 In Daniel et al,24 none of the use cases resulted in changes to clinical practice or patient treatment because the alerts were false positives.
These results suggest that bidirectional communication is a nascent but potentially promising area of public health informatics research and practice. Although the CDC and several states have taken steps towards creating bidirectional communication pathways, current efforts are only beginning to take hold. As previously noted, half of the articles identified were published in the final 3 years (2009–11) of the inclusion period. Additional investment in research and development of bidirectional communication infrastructure and methods will be necessary to enable public health agencies to participate in delivering up-to-date, actionable decision support to clinicians through care delivery systems. Without additional effort to develop and implement bidirectional communication approaches, electronic communications between public health and clinical care systems are likely to remain unidirectional. Clinical data are increasingly submitted electronically to public health surveillance programmes, but public health programmes generally lack the capacity to communicate feedback to clinicians electronically. Without new investment, public health agencies will continue to use less efficient methods including phone, fax, and postal mail. Such forms of communication may be disregarded in the increasingly digital practice of medicine and may therefore be promptly dismissed with other items deemed by clinicians to be outside of their workflow. This may further marginalize public health's ability to impact provider behavior and population health.
The issues raised in these select articles are strongly related to CDS, because bidirectional communications is a component of public health decision support. For example, the importance of regularly updating centralized repositories of knowledge is well recognized in the CDS community as a best practice.40 46 Governance and legal issues surrounding the ownership and use of shared knowledge are also issues facing the CDS community.47 48 Interoperability and usability are additional shared challenges with CDS networks and systems.49–51 Advancing bidirectional communication to achieve the aims of public health decision support therefore presents an opportunity for public health to work with clinical organizations towards a common goal: better patient and population outcomes. Multidisciplinary approaches will probably be necessary to address the broad range of technical, organizational, and cultural issues facing both CDS and public health decision support.
The methods used to identify and include articles in this review may have introduced bias. Selection of English-only articles may have resulted in language bias with potentially relevant studies published in other languages being missed. Judgment of the authors when reviewing candidate articles may have excluded articles considered by others in the biomedical informatics community to be representative of bidirectional communication.
Conclusion
This review details the emerging literature describing bidirectional communication and suggests several areas for future research and practice: architecture, interoperability, governance, and usability. These challenges present opportunities for public health and informatics professionals to work together to design and implement solutions that will meet the needs of both clinical and public health stakeholders. Research and development in these areas will advance the science and practice of informatics as well as public health. Successful development and adoption of bidirectional communication infrastructures will stimulate better clinical decisions and lead to improvements in population outcomes.
Footnotes
Funding: This work was supported by grant number R01HS020909 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and do not necessarily represent the official views of the Agency for Healthcare Research and Quality, the Department of Veterans Affairs, or the federal government.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Greenes RA. Definition, scope, and challenges. In: Greenes RA, ed. Clinical decision support: the road ahead. Burlington, MA: Elsevier, Inc., 2007:3–29 [Google Scholar]
- 2.Wright A, Sittig DF, Ash JS, et al. Clinical decision support capabilities of commercially available clinical information systems. J Am Med Inform Assoc 2009;16:637–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dexter PR, Perkins S, Overhage JM, et al. A computerized reminder system to increase the use of preventive care for hospitalized patients. N Engl J Med 2001;345:965–70 [DOI] [PubMed] [Google Scholar]
- 4.Chaudhry B, Wang J, Wu S, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med 2006;144:742–52 [DOI] [PubMed] [Google Scholar]
- 5.Jaspers MW, Smeulers M, Vermeulen H, et al. Effects of clinical decision-support systems on practitioner performance and patient outcomes: a synthesis of high-quality systematic review findings. J Am Med Inform Assoc 2011;18: 327–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Furukawa MF, Poon E. Meaningful use of health information technology: evidence suggests benefits and challenges lie ahead. Am J Manag Care 2011;17(12 Spec No.):SP76a-SP. [PubMed] [Google Scholar]
- 7.Centers for Medicare & Medicaid Services Medicare and medicaid programs; electronic health record incentive program—stage 2. Federal Register Washington: Office of the Federal Register, National Archives and Records Administration, 2012 [Google Scholar]
- 8.Lee LM, Thacker SB. The cornerstone of public health practice: public health surveillance, 1961–2011. MMWR Surveill Summ 2011;60(Suppl. 4):15–21 [PubMed] [Google Scholar]
- 9.Baxter R, Rubin R, Steinberg C, et al. Assessing Core Capacity for Infectious Diseases Surveillance. 2000. [cited 2010 March 8]. http://www.lewin.com/publications/publication/46/ (accessed 1 Feb 2013).
- 10.Doyle TJ, Glynn MK, Groseclose SL. Completeness of notifiable infectious disease reporting in the United States: an analytical literature review. Am J Epidemiol 2002;155:866–74 [DOI] [PubMed] [Google Scholar]
- 11.Silk BJ, Berkelman RL. A review of strategies for enhancing the completeness of notifiable disease reporting. J Public Health Manag Pract 2005;11:191–200 [DOI] [PubMed] [Google Scholar]
- 12.Jajosky RA, Groseclose SL. Evaluation of reporting timeliness of public health surveillance systems for infectious diseases. BMC Public Health 2004;4:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.AHRQ AHRQ Research Relevant to Bioterrorism Preparedness. 2002. March [cited 2010 March 17]. http://archive.ahrq.gov/news/focus/bioterror.htm (accessed 1 Feb 2013).
- 14.GAO Emerging infectious diseases: review of state and federal disease surveillance efforts. Washington, DC: US Government Accountability Office, 2004. Report No: GAO-04-877 [Google Scholar]
- 15.Buehler JW, Sonricker A, Paladini M, et al. Syndromic surveillance practice in the United States: findings from a survey of state, territorial, and selected local health departments. Adv Dis Surveill 2008;6:1–20 [Google Scholar]
- 16.CDC Fiscal year 2006 justification of estimates for appropriations committee. Department of Health and Human Services CDC, 2005:383 [Google Scholar]
- 17.Effler P, Ching-Lee M, Bogard A, et al. Statewide system of electronic notifiable disease reporting from clinical laboratories: comparing automated reporting with conventional methods. JAMA 1999;282:1845–50 [DOI] [PubMed] [Google Scholar]
- 18.Overhage JM, Grannis S, McDonald CJ. A comparison of the completeness and timeliness of automated electronic laboratory reporting and spontaneous reporting of notifiable conditions. Am J Public Health. 2008;98:344–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nguyen TQ, Thorpe L, Makki HA, et al. Benefits and barriers to electronic laboratory results reporting for notifiable diseases: the New York City Department of Health and Mental Hygiene experience. Am J Public Health 2007;97(Suppl. 1):S142–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dixon BE, McGowan JJ, Grannis SJ. Electronic laboratory data quality and the value of a health information exchange to support public health reporting processes. AMIA Annu Symp Proc 2011;2011:322–30 [PMC free article] [PubMed] [Google Scholar]
- 21.Gichoya J, Gamache RE, Vreeman DJ, et al. An evaluation of the rates of repeat notifiable disease reporting and patient crossover using a health information exchange-based automated electronic laboratory reporting system. AMIA Annu Symp Proc 2012;2012:1229–36 [PMC free article] [PubMed] [Google Scholar]
- 22.Savel TG, Foldy S. The role of public health informatics in enhancing public health surveillance. MMWR Surveill Summ 2012;61:20–4 [PubMed] [Google Scholar]
- 23.Thacker SB, Qualters JR, Lee LM. Public health surveillance in the United States: evolution and challenges. MMWR Surveill Summ 2012;61:3–9 [PubMed] [Google Scholar]
- 24.Daniel JB, Heisey-Grove D, Gadam P, et al. Connecting health departments and providers: syndromic surveillance's last mile. MMWR Morb Mortal Wkly Rep 2005(Suppl.);54:147–50 [PubMed] [Google Scholar]
- 25.Baker EL, Porter J. The health alert network: partnerships, politics, and preparedness. J Public Health Manag Pract 2005;11:574–6 [DOI] [PubMed] [Google Scholar]
- 26.Hanrahan LP, Anderson HA, Busby B, et al. Wisconsin's environmental public health tracking network: information systems design for childhood cancer surveillance. Environ Health Perspect 2004;112:1434–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Doniger AS, Labowitz D, Mershon S, et al. Design and implementation of a local Health Alert Network. J Public Health Manag Pract 2001;7:64–74 [DOI] [PubMed] [Google Scholar]
- 28.Garrett NY, Yasnoff WA. Disseminating public health practice guidelines in electronic medical record systems. J Public Health Manag Pract 2002;8:1–10 [DOI] [PubMed] [Google Scholar]
- 29.Lombardo JS, Garrett N, Loschen W, et al. An informatics solution for informing care delivery of immediate public health risks to their patients. Online J Public Health Inform 2009;1:1–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lurio J, Morrison FP, Pichardo M, et al. Using electronic health record alerts to provide public health situational awareness to clinicians. J Am Med Inform Assoc 2010;17:217–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Young A. ‘SWINEUPDATE’: using EMR charting tools as a clinical decision support tool during the H1N1 outbreak. WMJ 2010;109:222–3 [PMC free article] [PubMed] [Google Scholar]
- 32.Amirfar S, Taverna J, Anane S, et al. Developing public health clinical decision support systems (CDSS) for the outpatient community in New York City: our experience. BMC Public Health 2011;11:753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gamache R, Stevens KC, Merriwether R, et al. Development and assessment of a public health alert delivered through a community health information exchange. Online J Public Health Inform 2010;2:2. http://ojphi.org/htbin/cgiwrap/bin/ojs/index.php/ojphi/article/view/3214/2638 Accessed 2013 Feb 1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kawamoto K. Integration of knowledge resources into applications to enable clinical decision support: architectual considerations. In: Greenes RA, ed. Clinical decision support: the road ahead. Burlington, MA: Elsevier, 2007 [Google Scholar]
- 35.Dolin RH, Alschuler L. Approaching semantic interoperability in Health Level Seven. J Am Med Inform Assoc 2011;18:99–103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Osheroff JA, Teich JM, Middleton B, et al. A roadmap for national action on clinical decision support. J Am Med Inform Assoc 2007;14:141–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Paterno MD, Maviglia SM, Ramelson HZ, et al. Creating shareable decision support services: an interdisciplinary challenge. AMIA Annu Symp Proc 2010;2010:602–6 [PMC free article] [PubMed] [Google Scholar]
- 38.Williams C, Mostashari F, Mertz K, et al. From the Office of the National Coordinator: the strategy for advancing the exchange of health information. Health Aff (Project Hope) 2012;31:527–36 [DOI] [PubMed] [Google Scholar]
- 39.Bravata DM, McDonald KM, Smith WM, et al. Systematic review: surveillance systems for early detection of bioterrorism-related diseases. Ann Intern Med 2004;140:910–22 [DOI] [PubMed] [Google Scholar]
- 40.Sittig DF, Wright A, Simonaitis L, et al. The state of the art in clinical knowledge management: an inventory of tools and techniques. Int J Med Inform 2010;79:44–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dixon BE, McGowan JJ, Cravens GD. Knowledge sharing using codification and collaboration technologies to improve health care: lessons from the public sector. Knowledge Manage Res Pract 2009;7:249–59 [Google Scholar]
- 42.Kukafka R, Ancker JS, Chan C, et al. Redesigning electronic health record systems to support public health. J Biomed Inform 2007;40:398–409 [DOI] [PubMed] [Google Scholar]
- 43.Bolchini D, Finkelstein A, Perrone V, et al. Better bioinformatics through usability analysis. Bioinformatics 2009;25:406–12 [DOI] [PubMed] [Google Scholar]
- 44.Dixon BE. Enhancing the informatics evaluation toolkit with remote usability testing. AMIA Annu Symp Proc 2009;2009:147–51 [PMC free article] [PubMed] [Google Scholar]
- 45.Saleem JJ, Russ AL, Sanderson P, et al. Current challenges and opportunities for better integration of human factors research with development of clinical information systems. Yearb Med Inform 2009;2009:48–58 [PubMed] [Google Scholar]
- 46.Ash JS, Sittig DF, Dykstra R, et al. Identifying best practices for clinical decision support and knowledge management in the field. Stud Health Technol Inform 2010;160:806–10 [PMC free article] [PubMed] [Google Scholar]
- 47.Wright A, Sittig DF, Ash JS, et al. Governance for clinical decision support: case studies and recommended practices from leading institutions. J Am Med Inform Assoc 2011;18:187–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hongsermeier T, Maviglia S, Tsurikova L, et al. A legal framework to enable sharing of Clinical Decision Support knowledge and services across institutional boundaries. AMIA Annu Symp Proc 2011;2011:925–33 [PMC free article] [PubMed] [Google Scholar]
- 49.Dixon BE, Simonaitis L, Goldberg HS, et al. A pilot study of distributed knowledge management and clinical decision support in the cloud. Artif Intell Med In press [DOI] [PubMed] [Google Scholar]
- 50.Boxwala AA, Rocha BH, Maviglia S, et al. A multi-layered framework for disseminating knowledge for computer-based decision support. J Am Med Inform Assoc 2011;18(Suppl. 1):i132–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Richardson JE, Ash JS. A clinical decision support needs assessment of community-based physicians. J Am Med Inform Assoc 2011;18(Suppl. 1): i28–35 [DOI] [PMC free article] [PubMed] [Google Scholar]