Abstract
OBJECTIVES
Our goal was to objectively assess total steps and minutes active in the first and last 24-hours of hospitalization and examine associations with survival post-discharge in hospitalized older patients.
DESIGN
A prospective study.
SETTING
A 20-bed Acute Care for Elders (ACE) hospital unit.
PARTICIPANTS
Two hundred and twenty-four older adults admitted to an ACE hospital unit.
MEASUREMENTS
A StepWatch Activity Monitor collected information on total steps and minutes of activity in the first and last 24-hours of hospitalization. The main outcome was 2-year survival from hospital discharge date.
RESULTS
Patients were active for about 80 minutes in the first 24-hours of hospitalization. Minutes active increased about 28 minutes in the last 24-hours of hospitalization for patients aged 65–84, but were essentially unchanged for those aged 85 or older. The median step count for patients was low, with a median of 478 and 846 steps in the first and last 24-hours of hospitalization, respectively. Multivariate survival models showed that in the first and last 24-hours of hospitalization each 100 step increase was associated with a 2% (HR 0.98; 95% CI 0.96–1.00) and 3% (HR 0.97; 95% CI 0.94–0.99) decreased risk of death over 2-years, respectively. A decline in steps from first to last 24-hours of hospitalization was associated with more than a four-fold increase risk of death (HR 4.21; 95% CI 1.65–10.77) two-years post discharge.
CONCLUSION
Accelerometers could provide meaningful information about the walking activity of patients. Of importance is the potential to apply objective information about the patient’s functional status to improve the delivery of healthcare and health outcomes.
Keywords: Aging, Mobility, Hospitalization
INTRODUCTION
Among older patients, immobility can worsen the physiological and clinical complications of hospitalization1, 2 and increase the risk for poor health outcomes, including mortality.3–5 Of equal concern, about one- to two-thirds of older patients lose mobility during hospitalization, with many failing to regain lost abilities after discharge.3, 6, 7 Therefore, routine mobility assessment should be part of a standard daily clinical evaluation of the hospitalized older patient. Daily assessments could monitor mobility and track change, and set therapeutic goals to prevent or minimize loss of functional abilities. Mobility assessments may also serve as a functional indicator of health outcome.8, 9 An effective method that can quantify patient mobility in the hospital may have considerable value in prevention and recovery programs. Many physicians rely on nursing reports or patient self-reports,10, 11 which are subject to bias and may under or over estimate the patient’s true functional ability, making accurate decisions relative to the future health and well-being of the patient more difficult.
It is not presently known how mobile patients are on a day-to-day basis, when patients are most and least active, or factors associated with change in mobility. A more precise estimate of mobility, with a determination of normal and abnormal ranges, could help advance standards of care for preventing or delaying functional losses that many patients experience while hospitalized. Also, with growing demand for greater accountability in heath care, showing mobility as a clinically meaningful indicator of health outcome could promote its use on geriatric hospital units.12 Objectives of the current study were to assess mobility in hospitalized older patients using accelerometer technology and to evaluate the prognostic value of step activity in the first and last 24-hours of hospitalization as well as change in step activity from first to last 24-hours on 2-year survival post hospital discharge.
METHODS
Study Population
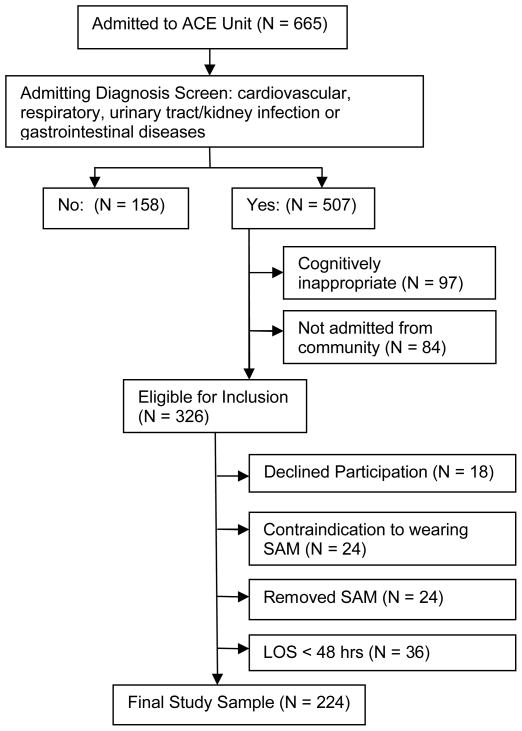
Subjects included adults aged 65 years or older admitted to a 20-bed Acute Care for Elders (ACE) hospital unit at the University of Texas Medical Branch (UTMB) teaching hospital from March, 2008 to October, 2009. An ACE hospital unit is a specialized unit for elderly patients that consists of a multidisciplinary team of geriatricians, nurses, pharmacists, social workers and occupational/physical therapists. To increase the study’s generalizability to geriatric hospital units and other ACE hospital units, only patients with an admitting diagnosis of cardiovascular, respiratory, urinary tract/kidney infection or gastrointestinal diseases were included.13 Patients with a musculoskeletal (n=86), neurological (n=13) endocrine/ metabolic (n=13) or ‘other’ e.g., skin diagnoses or injuries, psychosocial problems (n=46) diagnosis at admission were excluded. Five-hundred and seven patients with an admitting diagnosis of cardiovascular, respiratory, urinary tract/kidney infection or gastrointestinal diseases were eligible for inclusion in the current study. Of these, 97 were excluded because they were not cognitively appropriate per nursing admission assessment; and 84 were excluded because they were not admitted from the community. These included transfers from nursing homes or intensive care units or those scheduled for day surgery. Of the 326 eligible patients, 18 declined participation, 24 had a contraindication to wearing a StepWatchTM Activity Monitor (SAM) around the ankle, such as bilateral leg cellulitis or edema, and 24 removed the SAM or had the SAM removed by clinical staff for medical procedures or tests. Thirty-six patients with lengths of stay of less than 48 hours were also excluded from analyses. Two-hundred and twenty-four patients were enrolled (Figure 1). The study received approval from the University of Texas Medical Branch Institutional Review Board, and all subjects provided written informed consent.
Figure 1.
Enrollment Flow Diagram (N = 224).
Data and Data Collection
For each enrolled patient, a structured face-to-face interview was completed in the first 24 hours of admission to the ACE hospital unit, and included information on age, sex, marital status (married and unmarried), years of formal education, and race/ethnic group (white, black and Hispanic). A trained clinical interviewer with more than 5-years of experience interviewing patients conducted the chart reviews via the electronic medical record. The chart review was completed within 24 hours of discharge and specifically assessed diagnoses used to score the Charlson comorbidity index and obtain information on discharge diagnosis and height and weight to calculate body mass index (BMI). Length of stay was calculated as number of days on the ACE hospital unit.
A StepWatchTM Activity Monitor (SAM) is a waterproof dual-axis accelerometer that attaches to the patient’s ankle with a Velcro strap. This device, placed on the patient at time of consent and worn till discharge, was used to assess ambulatory activity (i.e., total steps and minutes active). The SAM has been shown to be 98% accurate in a variety of clinical populations, including those with slow or shuffling gait, and will not record leg movements while the patient is lying in bed.8, 14, 15 The SAM provides no direct feedback to the patient. Steps were recorded in 1-minute intervals synchronized to a 24-hour clock, resulting in a temporal series of 1,440 observations (i.e., minutes) per 24 hours. Total steps were calculated in the first and last 24 hours of hospitalization for each patient, and used as a continuous and categorical measure. Patient activity was calculated as the number of 1-minute intervals recorded in a 24-hour period with a step count greater than 0.
Vital status was determined by a review of medical records and a National Death Index search (NDI, National Center for Health Statistics, Hyattsville, Md). Survival 2-years from hospital discharge date was coded as yes or no; date of death was recorded if the person had died.
Statistical Analysis
Patient activity was presented as number of minutes active and percent active in the first and last 24-hours of hospitalization, stratified by age (65–74, 75–84, ≥ 85 years). Medians (and interquartile range) were used to describe total steps in the first and last 24-hours of hospitalization and change in steps from first to last 24 hours. A Wilcoxon signed rank test examined whether step count differed significantly from zero from first to last 24-hours of hospitalization stratified by individual sociodemographic and clinical characteristics. Unadjusted 2-dimensional scatterplots were used to graphically display correlations between total steps in the first and last 24-hours of hospitalization. Mean steps in each 1-hour interval were determined for the first and last 24-hours of hospitalization and fitted using spline regression. Total steps in the first and last 24-hours of hospitalization were also used to assess 2-year post discharge survival after adjusting for patient characteristics. Cumulative survival rates were calculated by the Kaplan-Meier method. Patients were censored 2-years post discharge.
Relative risks (hazard ratios) and 95% confidence intervals (CIs) were estimated with maximum likelihood estimates using Cox Proportional Hazard Models. To assess the functional form of 3 step measures (total steps in first and last 24-hours of hospitalization as well as change in steps) on mortality, we plotted the cumulative Martingale residuals against each step measure. Because the functional form for step change was not linear, a 4-level step change measure based on quartiles was created (≤ −59, −58 – 174, 175 – 819, ≥ 820 steps). The proportional hazard assumption of the three step measures were assessed by Shoenfeld residuals as the interaction between step and log of time and by an adjusted hazard plot by quartile of step measures. Testing was 2-sided and p < 0.05 was considered significant. All analyses were performed using commercially available software (SAS statistical software, version 9.2, SAS Institute, Inc., Cary, NC).
RESULTS
In the first 24-hours of hospitalization, patients were active about 80 minutes out of a possible 1440 minutes (i.e., < 6% of the time). Patient activity in the first 24-hours did not significantly differ by age. In the last 24-hours of hospitalization, patients aged 65–74 and 75–84 increased their activity from 81.9 (5.7%) and 81.2 (5.6%) minutes to 107.5 (7.5%) and 109.4 (7.6%) minutes, respectively. Patients aged 85 years or older showed only a small increase in activity, from 80.3 (5.6%) to 83.2 (5.8%) minutes.
Table 1 presents the median step count (and interquartile range) in the first and last 24-hours of hospitalization and step change from first to last 24-hours for the total sample and by each sociodemographic and clinical characteristic. The median step count for the total sample was 478 steps and 846 steps in the first and last 24-hours of hospitalization, respectively. The trend was for an increase in steps, with a median change of 174 more steps taken in the last 24-hours than in the first 24-hours of hospitalization. However, about a quarter of patients had a decline in step count from first to last 24 hours of hospitalization. The step count for married patients was significantly higher than for unmarried patients (p = 0.03).
Table 1.
Median (Md) Step Count in First and Last 24-hours of Hospitalization, and Change in Step Count from First to Last 24-Hours by Sociodemographic and Clinical Characteristic (N = 224).
| Total Steps | |||||
|---|---|---|---|---|---|
| First 24 hrs | Last 24 hrs | Δ in Steps First to Last 24-hrs† | |||
| Characteristic | N (%) | Md (Q1, Q3) | Md (Q1, Q3) | Md (Q1, Q3) | p-value‡ |
|
| |||||
| Total | 224 | 478 (72, 1486) | 846 (230, 2189) | 174 (−59, 820)** | |
|
| |||||
| Age (y) | 0.1457 | ||||
| 65–74 | 108 (48.2) | 497 (59, 1763) | 913 (198, 2464) | 187 (−49, 995)** | |
| 75–84 | 86 (38.4) | 458 (76, 1196) | 882 (268, 1918) | 216 (−64, 814)** | |
| ≥ 85 | 30 (13.4) | 660 (78, 1442) | 688 (118, 1676) | 38 (−264, 350) | |
| Gender | 0.5724 | ||||
| Women | 148 (66.1) | 516 (66, 1331) | 809 (209, 2189) | 181 (−12, 848)** | |
| Men | 76 (33.9) | 433 (77, 1814) | 919 (241, 2224) | 90 (−125, 796)* | |
| Race/Ethnicity | 0.1775 | ||||
| Non-Hispanic white | 146 (65.2) | 456 ( 64, 1562) | 809 (242, 2184) | 198 (−48, 882)** | |
| Non-Hispanic black | 51 (22.8) | 620 (140, 1306) | 1200 (302, 2414) | 182 (−288, 1030)* | |
| Hispanic | 27 (12.0) | 468 ( 24, 2350) | 630 (108, 1402) | 32 (−148, 590) | |
| Marital Status | 0.0300 | ||||
| Married | 94 (42.1) | 516 (90, 1562) | 1100 (368, 2360) | 352 (0, 970)** | |
| Unmarried | 129 (57.9) | 462 (62, 1400) | 692 (186, 2024) | 112 (−102, 590)* | |
| Education | 0.0743 | ||||
| ≥ High School | 134 (59.8) | 597 (94, 1562) | 1054 (298, 2476) | 256 (−24, 1192)** | |
| < High School | 90 (40.2) | 450 (64, 1400) | 596 (140, 1402) | 132 (−58, 590)* | |
| Comorbid conditions | 0.1496 | ||||
| 0 – 1 | 63 (28.2) | 466 (50, 1134) | 720 (238, 2360) | 320 (4, 1204)** | |
| 2 – 3 | 92 (41.3) | 497 (99, 1727) | 913 (225, 2413) | 142 (−82, 757)* | |
| ≥ 4 | 68 (30.5) | 368 (82, 1338) | 788 (212, 1965) | 108 (−160, 522) | |
| BMI (kg/m2) | 0.8602 | ||||
| ≤ 21 | 38 (17.0) | 472 (270, 1400) | 863 (244, 1676) | 196 (−112, 784)* | |
| 21.1 – 29.9 | 72 (32.3) | 319 (45, 1272) | 555 (158, 1695) | 131 (−39, 627)** | |
| ≥ 30 | 113 (50.7) | 538 (76, 2074) | 1200 (238, 2574) | 160 (−48, 1048)** | |
| Length of stay (days) | 0.2244 | ||||
| 2–3 | 105 (47.7) | 718 (174, 2542) | 1542 (560, 2986) | 242 (−122, | |
| ≥ 4 | 115 (52.3) | 306 (28, 1134) | 516 (162, 1504) | 1212)** 132 (−48, 668)** |
|
| Discharge diagnosis | 0.7305† | ||||
| Cardiovascular | 67 (29.9) | 688 (90, 1562) | 864 (250, 1978) | 114 (−138, 606) | |
| Respiratory | 36 (16.1) | 755 (341, 1866) | 1095 (318, 2406) | 172 (−485, 1120) | |
| Urinary tract /Kidney infection | 22 (9.8) | 555 (140, 2724) | 844 (140, 4292) | 158 (−4, 646) | |
| Gastrointestinal | 64 (28.6) | 213 (10, 1191) | 585 (186, 2100) | 187 (0, 814)** | |
| Other | 35 (15.6) | 328 (64 – 1582) | 788 (244 – 3436) | 354 (16, 1666)** | |
Wilcoxon signed rank test assessed statistically significant change in total steps from first and last 24 hours of hospitalization for each level of sociodemographic and clinical characteristic.
Statistically different from 0: p< 0.001,
p<0.05
Median regression analysis assessed median step change from first to last 24-hours of hospitalization across different levels of sociodemographic and clinical characteristic.
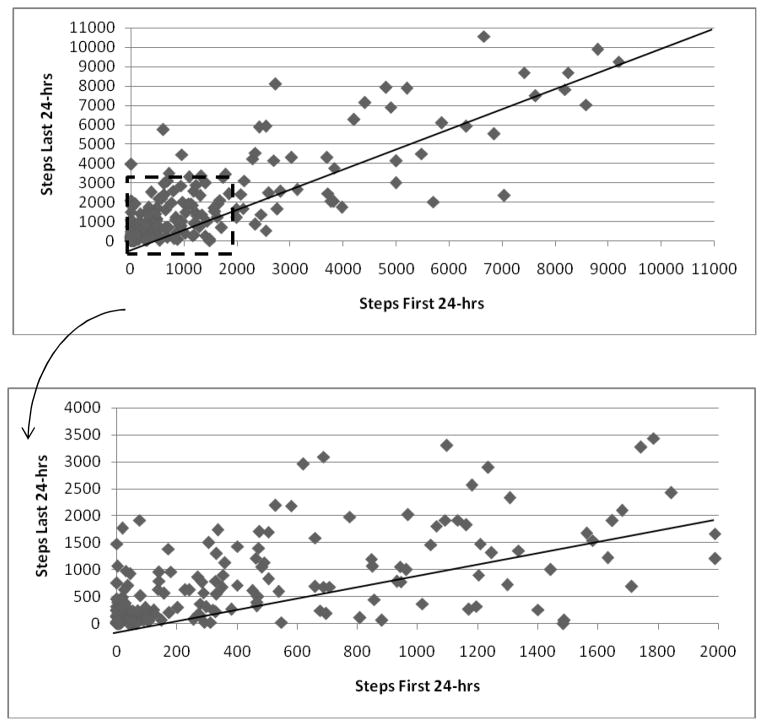
About 8 steps are needed to transfer from bed to chair, 44 steps to move from bed to bathroom and 152 steps to walk once around our ACE hospital unit.9 Most of the step activity occurred from 9 am to 7 pm. Figure 2a graphs the total steps in the first and last 24-hours of hospitalization for each patient. Most patients (80.3%) had a step count of less than 2000 steps in the first 24-hours of hospitalization. Of the 170 patients with a step count of 2000 or fewer steps, 136 increased their step count and 34 decreased their step count by discharge (Figure 2b). Of the 98 patients (43.8%) with a step count of less than 500 in the first 24-hours of hospitalization, 72 increased their step count and 16 decreased their step count by discharge.
Figure 2.
Scatterplots of Steps in the First and Last 24-hrs of Hospitalization for the Total Sample (Figure 2a), and for Patients with a Step Count of 2000 or Fewer Steps in the first 24-hours of hospitalization (Figure 2b.) (N =224).
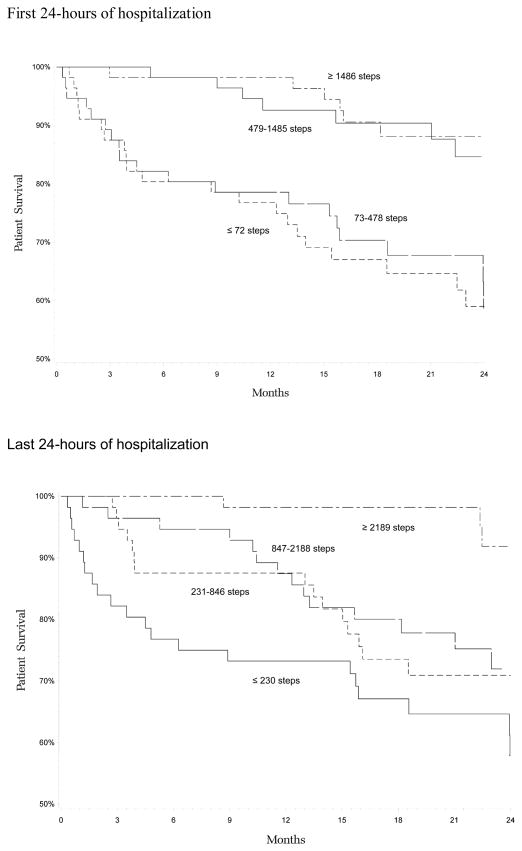
Unadjusted Kaplan-Meier estimates for the probability of death 2-years post discharge are presented for patient step count in the first (Figure 3a) and last (Figure 3b) 24-hours of hospitalization. Patients in the lowest 2 quartiles, with a step count of 478 or fewer steps in the first 24-hours of hospitalization were at a similarly increased risk for death compared with patients in the highest 2 quartiles, with a step count of 479 steps or more (Figure 3a). Figure 3b shows a gradient of risk by step quartile. Patients with the lowest step count (quartile 1, ≤ 230 steps) in the last 24-hours of hospitalization were at the greatest risk for death and those with the highest step count (quartile 4, ≥ 2189 steps) at the least risk.
Figure 3.
Unadjusted Survival Curves Assessing Death 2-years Post Discharge by Steps in the First (Figure 3a.) and Last (Figure 3b.) 24-Hours of Hospitalization (N = 224).
Table 2 summarizes the results of three separate multivariable survival analysis predicting survival 2-years post discharge. In the first 24-hours of hospitalization (Model 1), each 100 step increase was associated with a 2% decreased hazard of death (95% CI 0.96 –1.00). In the last 24-hours of hospitalization (Model 2), each 100 step increase was significantly associated with a 3% decreased hazard of death (95% CI 0.94 – 0.99). Adjusting for steps in the first 24-hours of hospitalization, there was more than a four-fold increased hazard of death (HR 4.21; 95% CI 1.65 – 10.77) among patients whose step count decreased from first to last 24-hours of hospitalization compared with those that increased their step count by 820 or more steps (Model 3). Patients with a minimal change in steps (i.e., −58 to 174 steps) also had a significantly increased hazard of death (HR 3.24; CI: 1.27 – 8.30). Other factors significantly associated with survival in all three models included female sex and fewer comorbid conditions.
Table 2.
Survival analysis assessing Death 2-years Post Hospital Discharge for Steps in the First and Last 24-Hours of Hospitalization and Change in Steps from First to Last 24-Hours of Hospitalization (N = 224).
| Patient Characteristic | HR (95% CI) | HR (95% CI) | HR (95% CI) |
|---|---|---|---|
|
| |||
| First 24-hrs | Last 24-hrs | Δ First to Last 24- hrs | |
|
| |||
| Per 100 Steps | 0.98 (0.96, 1.00) | 0.97 (0.94, 0.99) | |
| Δ in Steps first to last 24-hrs | |||
| Q1: ≤ −59 vs. ≥ 820 (Ref) | 4.21 (1.65, 10.77) | ||
| Q2: −58 to 174 vs. ≥ 820 | 3.24 (1.27, 8.30) | ||
| Q3: 175 to 819 vs. ≥ 820 | 0.75 (0.24, 2.31) | ||
| Age (con’t) | 1.04 (0.99, 1.08) | 1.03 (0.99, 1.07) | 1.03 (0.99, 1.06) |
| Women (vs. men) | 0.28 (0.16, 0.52) | 0.27 (0.15, 0.50) | 0.28 (0.15, 0.51) |
| Married (vs. unmarried) | 0.63 (0.35, 1.14) | 0.69 (0.38, 1.26) | 0.99 (0.52, 1.87) |
| White (vs. non-White) | 1.43 (0.75, 2.72) | 1.36 (0.71, 2.61) | 1.43 (0.73, 2.77) |
| Body Mass Index (con’t) | 0.98 (0.95, 1.02) | 0.98 (0.94, 1.02) | 0.98 (0.95, 1.02) |
| Length of stay (con’t) | 1.02 (0.98, 1.07) | 1.02 (0.98, 1.07) | 1.01 (0.96, 1.06) |
| Comorbid condition (0 to 4 category) | 1.30 (1.16, 1.44) | 1.28 (1.15, 1.42) | 1.30 (1.16, 1.45) |
| Discharge diagnosis | |||
| Respiratory (vs. cardiovascular) | 1.28 (0.59, 2.78) | 1.44 (0.66, 3.13) | 1.38 (0.62, 3.04) |
| Urinary tract/Kidney infection (vs. cardiovascular) | 0.63 (0.22, 1.86) | 0.60 (0.20, 1.74) | 0.48 (0.16, 1.48) |
| Gastrointestinal (vs. cardiovascular) | 0.69 (0.32, 1.50) | 0.73 (0.34, 1.60) | 0.82 (0.37, 1.84) |
| Other (vs. cardiovascular) | 1.45 (0.61, 3.46) | 1.71 (0.71, 4.09) | 1.49 (0.60, 3.70) |
| Steps First 24-hrs (per 100 steps) | 0.97 (0.94, 0.99) | ||
DISCUSSION
This study provides evidence that a StepWatch Activity Monitor (SAM) can be a practical device for the continuous monitoring of mobility in hospitalized older patients. The SAM was well-tolerated by patients and no adverse events were reported. Most patients were active for only a small portion of time, with a majority walking fewer than 2000 steps in a 24-hour period. Nonetheless, most patients increased their step activity during hospitalization, although about a quarter did decline. Step activity was an independent predictor of death; patients walking the fewest steps in the last 24-hours of hospitalization or those who had a decline in steps from admission to discharge were at significantly greater risk for death post discharge.
Often, clinicians provide little information to the patient on the consequences of low mobility.16, 17 To increase patient awareness and plan for care there may be value in quantifying daily step activity and establishing normal and abnormal ranges, which could be used not only to promote mobility but also alert clinical staff to those patients potentially at risk for complications related to immobilization such pressure ulcers, falls, deep vein thrombosis, and muscle loss. The admitting diagnoses used in this study were comparable to other geriatric hospital units, suggesting that most older patients are functionally inactive in the hospital. The data suggest that patients on geriatric hospital units take less than 15% of the steps taken by community-living older persons. A meta-analysis in 2007 reported a daily step count of 6566 steps (95% CI 4897 –8233) for persons 65 years and older living in the community,18 with other independent studies reporting similar results.14, 19 Of potential importance is to assess the dynamic nature of mobility and the extent to which discharged patients are able to regain lost mobility and have a step count similar to individuals in community-based studies.
Data from the current study indicate that step activity may be an independent predictor of health outcomes important to the patient. A comparison of step activity in the first and last 24-hours of hospitalization produced similar results, showing higher step counts at each time point, and an increase in step count over the two time points were associated with reduced risk of death 2-years post discharge, independent of other factors including comorbidity. These results are comparable to a study using nursing observation where lower category of mobility activity was shown as a significant independent predictor of death 1-year post discharge in hospitalized medical patients aged 70 and older.1
Assessment of mobility within the first 24-hours of hospital admission could identify subgroups of patients at low and high risk for poor health outcomes in addition to death, such as rehospitalization, loss of independence and reduced quality of life. Patients falling below a certain threshold of daily steps, for example, might be characterized as having preclinical mobility disability, and would potentially benefit from increased clinical attention to mobility deficits.
Part of the predictive power of our findings may be because sicker patients walk less and are at an increased risk for death, although multivariate analysis did adjust for discharge diagnosis and comorbid conditions. Given that physical activity affects the vitality of the person and the integrated functioning of many bodily systems,20 it is also possible that low mobility activity is causative of poor health outcomes, including death. Although the adoption of interventions at this point is premature, the observed impact of low mobility or mobility decline during hospitalization suggests important targets for preventive intervention. While some interventions could be considered for patients with specific admitting illnesses or chronic conditions, other interventions may be more broadly applied to include all hospitalized older patients. Interventions could further be developed to determine an optimal level or threshold of daily steps needed to protect against hospital-associated physical and functional losses, maximizing the patient’s ability to remain independent.
Strengths of the study include the relatively large and racially/ethnically diverse sample with admitting illnesses13 similar to other geriatric hospital units. Step values from the accelerometer were shown to accurately count steps actually walked from bed to bathroom, bed to chair, and once around our ACE unit, and to not count movements in bed. A limitation of this study is that patient were enrolled from a single ACE hospital unit, and results may be not generalizable to other geriatric hospital units as regional and other contextual differences may exist. Therefore, it would be important to replicate and expand our findings to ACE hospital units in other areas of the country. A second limitation was that we excluded patients with cognitive difficulties. Further work specifically targeting this patient group is warranted. Third, although the SAM provided no direct feedback to the patient, wearing the SAM could have caused or encouraged some patients to walk more than otherwise would have occurred. However, for the majority of our sample, step activity was low.
Efforts are needed to implement a simple and practical assessment of mobility that is reliable and reflects patient activity while hospitalized. By accurately evaluating mobility a physician can identify at-risk patients, and anticipate and plan future interventions that may prevent or slow functional declines. Accelerometers have the potential to quantify mobility and change in mobility, and to predict health outcomes highly relevant to older patients.
Acknowledgments
This research was supported in part by grants P30 AG024832 and R01-AG031178 from the National Institute on Aging.
Sponsor's Role: The funding sources had no role in the design and conduct of the study; in the collection, management, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript.
Footnotes
Author Contributions: Glenn Ostir: Study concept and design, acquisition of subjects and/or data, analysis and interpretation of data, manuscript preparation. Ivonne Berges: Analysis and interpretation of data, and manuscript preparation. James Goodwin: Concept and design, interpretation of data, manuscript preparation. Steven Fisher: Interpretation of data, and manuscript preparation. Yong-Fang Kuo: Analysis and interpretation of data, and manuscript preparation. Jack Guralnik: Concept and design, interpretation of data, manuscript preparation.
Conflict of Interest: The authors are not aware of any affiliations, memberships, funding, or financial holdings that might be perceived as affecting the objectivity of this review.
References
- 1.Brown CJ, Friedkin RJ, Inouye SK. Prevalence and outcomes of low mobility in hospitalized older patients. J Am Geriatr Soc. 2004;52:1263–1270. doi: 10.1111/j.1532-5415.2004.52354.x. [DOI] [PubMed] [Google Scholar]
- 2.Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med. 1993;118:219–223. doi: 10.7326/0003-4819-118-3-199302010-00011. [DOI] [PubMed] [Google Scholar]
- 3.Covinsky KE, Palmer RM, Fortinsky RH, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: Increased vulnerability with age. J Am Geriatr Soc. 2003;51:451–458. doi: 10.1046/j.1532-5415.2003.51152.x. [DOI] [PubMed] [Google Scholar]
- 4.Hirsch CH, Sommers L, Olsen A, et al. The natural history of functional morbidity in hospitalized older patients. J Am Geriatr Soc. 1990;38:1296–1303. doi: 10.1111/j.1532-5415.1990.tb03451.x. [DOI] [PubMed] [Google Scholar]
- 5.Inouye SK, Peduzzi PN, Robison JT, et al. Importance of functional measures in predicting mortality among older hospitalized patients. JAMA. 1998;279:1187–1193. doi: 10.1001/jama.279.15.1187. [DOI] [PubMed] [Google Scholar]
- 6.Gill TM, Gahbauer EA, Han L, et al. The relationship between intervening hospitalizations and transitions between frailty states. J Gerontol A Biol Sci Med Sci. 2011;66:1238–1243. doi: 10.1093/gerona/glr142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gill TM, Allore HG, Holford TR, et al. Hospitalization, restricted activity, and the development of disability among older persons. JAMA. 2004;292:2115–2124. doi: 10.1001/jama.292.17.2115. [DOI] [PubMed] [Google Scholar]
- 8.Fisher SR, Kuo YF, Graham JE, et al. Early Ambulation and Length of Stay in Older Adults Hospitalized for Acute Illness. Arch Intern Med. 2010;170:1942–1943. doi: 10.1001/archinternmed.2010.422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fisher SR, Goodwin JS, Protas EJ, et al. Ambulatory activity of older adults hospitalized with acute medical illness. J Am Geriatr Soc. 2011;59:91–95. doi: 10.1111/j.1532-5415.2010.03202.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lazarus BA, Murphy JB, Coletta EM, et al. The provision of physical activity to hospitalized elderly patients. Arch Intern Med. 1991;151:2452–2456. [PubMed] [Google Scholar]
- 11.Simonsick EM, Montgomery PS, Newman AB, et al. Measuring fitness in healthy older adults: The Health ABC Long Distance Corridor Walk. J Am Geriatr Soc. 2001;49:1544–1548. doi: 10.1046/j.1532-5415.2001.4911247.x. [DOI] [PubMed] [Google Scholar]
- 12.Hall WJ. Update in geriatrics. Ann Intern Med. 2006;145:538–543. doi: 10.7326/0003-4819-145-7-200610030-00012. [DOI] [PubMed] [Google Scholar]
- 13.Jayadevappa R, Bloom BS, Raziano DB, et al. Dissemination and characteristics of acute care for elders (ACE) units in the United States. Int J Technol Assess Health Care. 2003;19:220–227. doi: 10.1017/s0266462303000205. [DOI] [PubMed] [Google Scholar]
- 14.Cavanaugh JT, Coleman KL, Gaines JM, et al. Using step activity monitoring to characterize ambulatory activity in community-dwelling older adults. J Am Geriatr Soc. 2007;55:120–124. doi: 10.1111/j.1532-5415.2006.00997.x. [DOI] [PubMed] [Google Scholar]
- 15.Foster RC, Lanningham-Foster LM, Manohar C, et al. Precision and accuracy of an ankle-worn accelerometer-based pedometer in step counting and energy expenditure. Preventive Med. 2005;41:778–783. doi: 10.1016/j.ypmed.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 16.Bogardus ST, Jr, Towle V, Williams CS, et al. What does the medical record reveal about functional status? A comparison of medical record and interview data. J Gen Intern Med. 2001;16:728–736. doi: 10.1111/j.1525-1497.2001.00625.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: "She was probably able to ambulate, but I'm not sure". JAMA. 2011;306:1782–1793. doi: 10.1001/jama.2011.1556. [DOI] [PubMed] [Google Scholar]
- 18.Bohannon RW. Comfortable and maximum walking speed of adults aged 20–79 years: reference values and determinants. Age Ageing. 1997;26:15–19. doi: 10.1093/ageing/26.1.15. [DOI] [PubMed] [Google Scholar]
- 19.Tudor-Locke CE, Myers AM. Methodological considerations for researchers and practitioners using pedometers to measure physical (ambulatory) activity. Res Q Exerc Sport. 2001;72:1–12. doi: 10.1080/02701367.2001.10608926. [DOI] [PubMed] [Google Scholar]
- 20.Ferrucci L, Bandinelli S, Benvenuti E, et al. Subsystems contributing to the decline in ability to walk: Bridging the gap between epidemiology and geriatric practice in the InCHIANTI study. J Am Geriatr Soc. 2000;48:1618–1625. doi: 10.1111/j.1532-5415.2000.tb03873.x. [DOI] [PubMed] [Google Scholar]