Abstract
Background
Most older cancer survivors (OCS) do not engage in regular physical activity (PA) despite well-known health benefits. With the increased use of mobile technologies among older adults, mobile tools may be an effective method to deliver PA promotion programs for OCS.
Objective
To document the process of designing an OCS-friendly mobile-enabled Web application of PA promotion program.
Methods
Mixed methods encompassing group discussions, individual interviews, and brief surveys with community leaders, OCS, cancer care providers, and software professionals were used in this formative research.
Results
The varied stakeholders welcomed the idea of developing an online tool to promote PA in OCS. Our formative research revealed several major barriers to regular PA including limited access to senior-friendly PA resources, lack of motivation and social support, and insufficient knowledge and skills on building safe and appropriate workout plans. This feedback was incorporated into the development of iCanFit, a mobile-enabled Web application, designed specifically for OCS. The iCanFit online tools allow users to locate PA resources, set and track goals for PA, network with peer OCS in a secure online space, and receive practical and evidence-informed healthy tips.
Conclusions
Our mixed-method formative research led to the design of iCanFit protocol to promote PA and well-being of OCS. The involvement of stakeholders is critical in the planning and design of the mobile application in order to enhance program relevance, appeal, and match with the needs of target users.
Keywords: older cancer survivors; physical activity, survivorship, mHealth, website design; user-computer interface; protocol development; formative research
Introduction
Early detection and improved treatment for cancer has resulted in approximately 13 million survivors in the Unites States today. It has been estimated that these numbers will increase by nearly a third to 18 million by 2022 [1]. Most cancer survivors are 60 years of age or older, and the population of older cancer survivors (OCS) is increasing, resulting in many challenges associated with the continuity of care and resultant quality of life [2,3]. Countering these challenges, numerous studies point to the physiological and psychosocial benefits of physical activity (PA) for cancer survivors [4,5]. These benefits include improved physical endurance, capacity and strength, higher immune function and hemoglobin concentration, decreased risk of cancer recurrence, and improved quality of life as indicated by decreased fatigue and depression [6-10]. Several guidelines on PA for cancer survivors have been recently issued, recommending cancer survivors to engage in low to moderate impact PA regularly, specifically, at least 30 minutes of exercise a day for 5 days a week [11,12].
Despite the recognized importance of PA for cancer survivors, evidence suggests that the level of adherence to PA guidelines among cancer survivors is very low. Smith and Chagpar reported that only 4.6% of breast cancer survivors followed PA guidelines, compared to 12% of women without breast cancer [13]. The majority of cancer survivors are not participating in the recommended levels of PA, resulting in a greater disease risk and health care costs [14]. In a review of existing programs to promote PA among cancer survivors, Schmitz and colleagues observed that most existing programs are limited to walking only, and that there is a lack of diversity in types of PA for cancer survivors [15]. In addition, most existing studies of interventions to increase PA have relied on individual or small group counseling approaches, typically offered by nurses or health educators. Such face-to-face approaches, although promising, have encountered problems of high personnel cost and limited reach. Thus, a critical need exists for more cost-effective strategies to reach a large number of OCS with effective strategies for promoting PA [12,16].
In the exploration of interventions to promote PA among OCS, mobile technologies are gaining increased attention across all age groups. As of 2012, about 88% of US adults and nearly 70% of people older than 50 accessed the Internet. 85% of US adults owned cell phones, of those, 53% owned smartphones [17]. Approximately 70% of adults over 50 owned a cell phone, and more than 42% owned a laptop or tablet computer [18]. The percentage of older smartphones or mobile computer owners is expected to accelerate in the coming years. Further, recent surveys by National Cancer Institute indicated that more than 60% of cancer survivors access the Internet; and once online, they are more likely to use it for health-related purposes than general users [19, 20]. Among cancer survivors, the Internet has become the second most used resource for finding health-related information (the primary resource was physicians) [21,22]. The ubiquity of Internet access in the US and the rapid penetration of smartphones and tablets suggests the feasibility of using mobile technologies to promote PA among OCS. In a recent review of existing Web and mobile applications for PA promotion, we found that most websites or applications were designed for general and younger populations. Few online PA programs were designed for cancer survivors, not to mention OCS. The purpose of this article was to describe a formative study we conducted to inform the design of a mobile or Web application for the purpose of promoting PA among OCS.
Methods
Overview
A multidisciplinary research team from Communities of Texas: Cancer • Activity • Research • Education • Support (CTxCARES) program representing public health, medicine, health education, and technology development worked collaboratively to design the formative research protocol. A mixed-method approach was used to collect data to inform the structure and content of the mobile or Web application. Our team met regularly to discuss the data collected from field, enabling prompt feedback for project development and refinement. Data collection in formative research spanned from November 2011 to September 2012. We held group discussions with community leaders, individual interviews with cancer care providers, and conducted a brief survey and interviews with OCS. Table 1 lists all the data collection methods utilized. The study protocol was approved by the Institutional Review Boards at the Texas A&M University and Scott & White Healthcare.
Table 1.
Data sources of formative research in the iCanFit program.
| Data collection method | Participants | Recruitment venues | Data collection mode |
| Group discussion |
Community leaders (n=20) |
Community centers | Face-to-face |
| Individual interview |
Cancer care providers (n=14) |
Conferences, clinics | Face-to-face, phone |
| Individual interview | Older cancer survivors (n=20) | Communities, clinics, cancer-related events | Face-to-face, phone |
| Questionnaire | Older cancer survivors (n=92) | Communities, cancer-related events | Paper-pencil |
Group Discussions with Community Leaders
The CTxCARES program has collaborated with local cancer communities and senior communities for several years, leading to established relationships. At the planning stage of the project, we communicated about our intention to develop a mobile or Web application for OCS to local senior and cancer community leaders and obtained their support. In our formative research, we had 2 group discussions with local community leaders to get their input on the feasibility of a website to engage OCS and promote their PA. The discussions took place in informal expanded meetings of community organizations in which community leaders and members were present. These discussions were not taped, but detailed notes were taken during and after the meeting.
Interviews with Cancer Care Providers
We also interviewed practicing cancer care providers who have patients either in active cancer treatment or are cancer survivors. The provider’s interview guide was developed based on the literature review and informal discussions with community leaders. The guide focused on: (1) perceptions on OCS’ barriers to regular PA, (2) current counseling of PA with OCS, (3) suggested contents of a mobile or online program, and (4) strategies to disseminate the program after piloting. The interview guide was piloted with 2 physicians before field use. A total of 14 cancer care providers were recruited during a large state cancer conference, representing surgeons, oncologists, family physicians, internists, health educators, and counselors. One-on-one interviews ranging from 20-45 minutes were conducted in a private space. All conversations were audio-taped and transcribed verbatim.
Survey with OCS
We conducted a brief survey with OCS who were at least 60 years old, had a cancer diagnoses, and had completed initial treatment. Surveys were distributed at local health fairs and cancer survivors’ events. Participants reported on their Internet and cell phone use, current PA behaviors, access to health information, and attitudes toward mobile-based PA promotion program. It took the OCS approximately 10 minutes to complete the brief paper-pencil survey. A total of 92 OCS (mean age 62) provided oral consent and completed the survey. All survey data were entered into SPSS 16.0 (SPSS Inc, Chicago, IL, USA).
Interviews with OCS
Our third strategy was to conduct in-depth individual interviews with OCS. We developed an interview guide for OCS based on the brief survey with OCS and the in-depth interviews with cancer care providers. The interview guide consisted of the following domains: (1) current PA including type, intensity, duration, and frequency, (2) barriers to regular PA, (3) preferred PA and facilitators to regular PA, (4) attitudes toward an online or mobile PA promotion program, (5) suggestions on content and features of the mobile program, and (6) suggestions on program implementation and evaluation. A total of 11 OCS in Central Texas were recruited through community outreach strategies. The interviews were conducted face-to-face or over the phone, lasted 25-45 minutes, and were audio-taped. Each participant provided consent and received a $15 gift card.
Data Analysis and Interpretation
The data collected in the formative research included: (1) notes from the research team’s regular meeting discussions, (2) detailed notes from discussions with community leaders, (3) transcripts from interviews with cancer care providers, (4) survey data from OCS, and (5) transcripts from interviews with OCS. Quantitative data were saved in SPSS and descriptive statistical methods were used to analyze frequency of key variables. Qualitative data were saved in Microsoft Word; thematic content analysis was used to identify the major themes and key exemplary quotes [23]. Findings from each data set were used to inform analysis and interpretation of other data sets. The data analysis was iterative and continued throughout the formative research; the findings were used to inform the design, content, and structure of the iCanFit mobile-enabled Web application.
Results
Feasibility of Mobile PA Promotion Program for OCS
The survey and interviews with OCS and discussions with community leaders revealed the current online behaviors of OCS. Most of OCS accessed the Internet, and the Internet was a major source of health information for the participants. For example, more than 80% of OCS in our interviews indicated that they would participate in an online PA promotion program or OCS support program. OCS also suggested that compared to younger people, they had shorter online duration and that they were more likely to visit the same authoritative sites. Less than 10% of OCS accessed the Internet through their cell phones frequently, but many had tablets such as iPads and many accessed the Internet through their mobile devices.
I use Internet many times a day, and I search for health information for myself and my family. I search the Internet using both my desktop and my iPhone…People have misconceptions about seniors using mobile technologies, many of us are computer savvy.
61 year old OCS
Some OCS, especially those over 75 years old, reported less use of Internet themselves, but they relied on their families to access the Internet and obtain health information. More than 80% of the OCS we talked to have easy access to health information and could easily obtain this information from the Internet.
Barriers to PA Among OCS
The interviews with cancer care providers indicated that most of them were aware of regular PA as part of healthy living for cancer survivors, but very few discussed PA with their survivor patients. Care providers identified the lack of motivation to carry out PA from survivors as the major barrier to regular PA. For example, a physician related, “If they want to do it, they’ll do it. If they don’t, they won’t.” Most cancer care providers listed time constraint as a major barrier to discussing PA with their cancer survivor patients. As one physician indicated, “The conversation doesn’t get that in-depth because we have so many other issues to discuss.”
The interviews with OCS confirmed that most did not participate in regular PA. Four personal and structural level barriers to PA were identified. First, some survivors were not aware of the benefits of PA.
For myself, since I got colon cancer, I became more cautious with what I eat. I see nutrition is more important for me…Physical activity? I do some yard work, and when I shop in Wal-Mart, I walk fast with my shopping cart
60 year old OCS
Second, some understood the importance of regular PA, but lacked motivation to be more physically active.
After all the treatments, I just want to go back to my normal life. I know exercise is good for health, but it is probably the last thing in the mind now. I just want to get back to normal, rather than an enhancement or set up new goals.
67 year old OCS
Third, many OCS had limited access to information on local, senior-friendly PA programs and resources. They expressed frustration in finding senior-friendly PA resources.
There is a senior center here in [omitted], but I’ve been there and looked into their exercise room and it’s about twice the size of my hall bathroom; and it is so confined that I am not inspired to get in there and do anything.
70 year old OCS
Another OCS who had tried some programs said, “It did help a little but I quit going because they did not treat me as an individual but they just do everybody in mass.” In addition, since PA was rarely discussed in their visit with health care providers, OCS did not know how to set up individualized plans that fit their health and needs. Fourth, some OCS did not have enough social support, especially peer support, to engage in regular PA. For instance, some OCS commented, “I am basically lazy…and I need somebody to crack the whip…If I had an exercise partner, I may go more often.” Our brief survey with OCS suggested that only a small number of OCS were part of the online cancer support groups but most were willing to join one.
Key Functions and Structure of the Online PA Promotion Program
In addition to identifying barriers to regular PA, our participants of community leaders, cancer care providers, and OCS also provided suggestions on how to design the online program to address these barriers. Their input was incorporated into the design of a mobile-enabled Web application called iCanFit. The reason for a Web application instead of a mobile application is to fulfill the goal of making iCanFit accessible through all mobile devices with Internet connections. Most mobile applications are limited to certain devices or platforms. For example, iPhone apps will not work on Android phones. Our mobile-enabled interactive website allows seniors to access the program through their various mobile devices with minimal restrictions.
Table 2 lists input from stakeholders on the barriers and corresponding functions on the Web application to address stakeholder feedback. The interactive iCanFit has the following 6 major functions addressing the needs and barriers to regular PA in OCS:
Table 2.
Proposed key iCanFit functions based on inputs from stakeholders.
| Input | Proposed iCanFit function |
Purpose |
| OCS: Limited safe and senior-friendly physical activity resources. CL: Lack of access to information on community resources and events. |
Locator |
|
| CCP: Insufficient time to discuss PA or make specific plans with patients. OCS: Need assistance in setting individualized plans. |
Goals |
|
| OCS: OCS need social support, especially peer support to start and maintain regular physical activity. OCP: Social support is an important factor for OCS to stay physically active. CL: Online community can expand OCS social networks, especially for rural residents. |
Community (Chatter) |
|
| CCP: OCS lack motivation to stay physically active. OCS: Need constant reminders to continue the momentum. CL: Simple tips can make small changes, and small changes can add up. |
Healthy Tips |
|
| OCS: Many OCS are unaware of necessity and benefits of regular PA. CCP: Do not have enough time to carry out patient education. |
Library |
|
1. “Locator”, a function that allows easy search for local resources of PA, including parks, facilities, and programs. Users can set their preferences for searching, for example, indoors, free, group activity, etc.
2. “Goals”, a function that allows users to set long- and short-term goals of PA. They can track their PA by entering their weekly PA. The iCanFit system will provide tailored feedback on their progress and suggestions on changing on short-term goals. iCanFit sends weekly reports to the users tracking their goals and providing tailored tips and kudos. Those who met their goals were congratulated by a virtual coach and those who did not meet their goals received motivational messages from the virtual coach.
3. “Community”, a function that offers social support through virtual networking. Users are able to create a profile, post images, and start and follow discussions and to connect with peers users. Users are also able to create a profile, post images, and start and follow discussions and to connect with peers users. Those who exceed the short-term PA goals will also be recognized and congratulated in the online community.
4. “Healthy Tips”, a function that sends regular health tips to users. These consist of tips for seniors to make small changes in daily life and make incremental progress toward an active and healthy living.
5. “Library”, is a function that provides convenient access to authoritative health information. In addition to links to major senior health and cancer survivor organizations, this function also allows keyword search for specific health information.
6. “Support”, is a function where users can seek help and technical support when using iCanFit programs.
We included some screen shots to help visualize how iCan Fit works. Figure 1 depicts iCanFit homepage on a desktop, Figure 2 displays the key functions of iCanFit on a laptop, and Figure 3 shows iCanFit functions on an iPhone interface. In line with stakeholders’ suggestions and the National Library of Medicine guidelines of “making your website senior friendly” [24], the iCanFit interface is simple with bigger icons, bigger fonts, more space between lines, and clear background in contrast with the main texts. The iCanFit protocol is currently being developed into active Web application.
Figure 1.
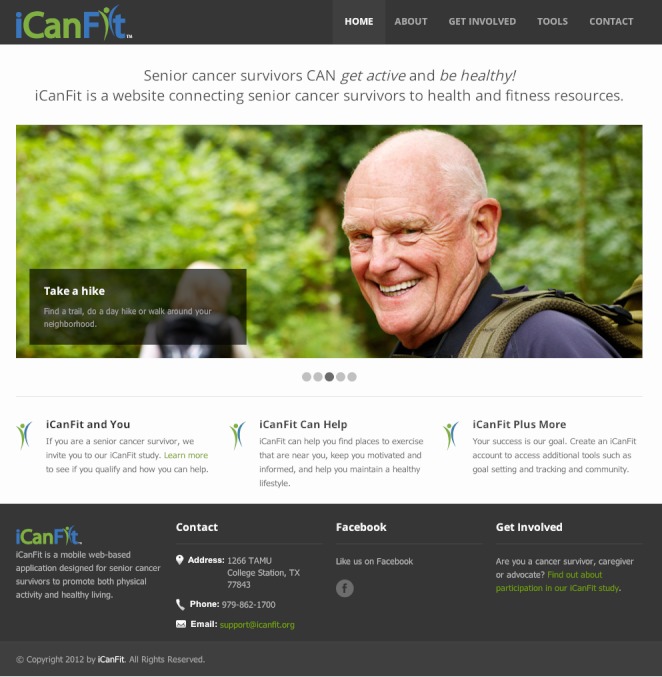
iCanFit webpage interface on a desktop computer.
Figure 2.
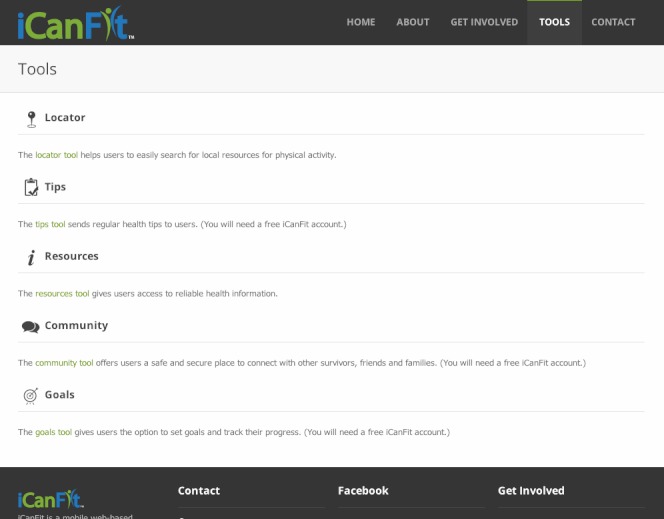
Major functions of iCanFit on desktop interface.
Figure 3.
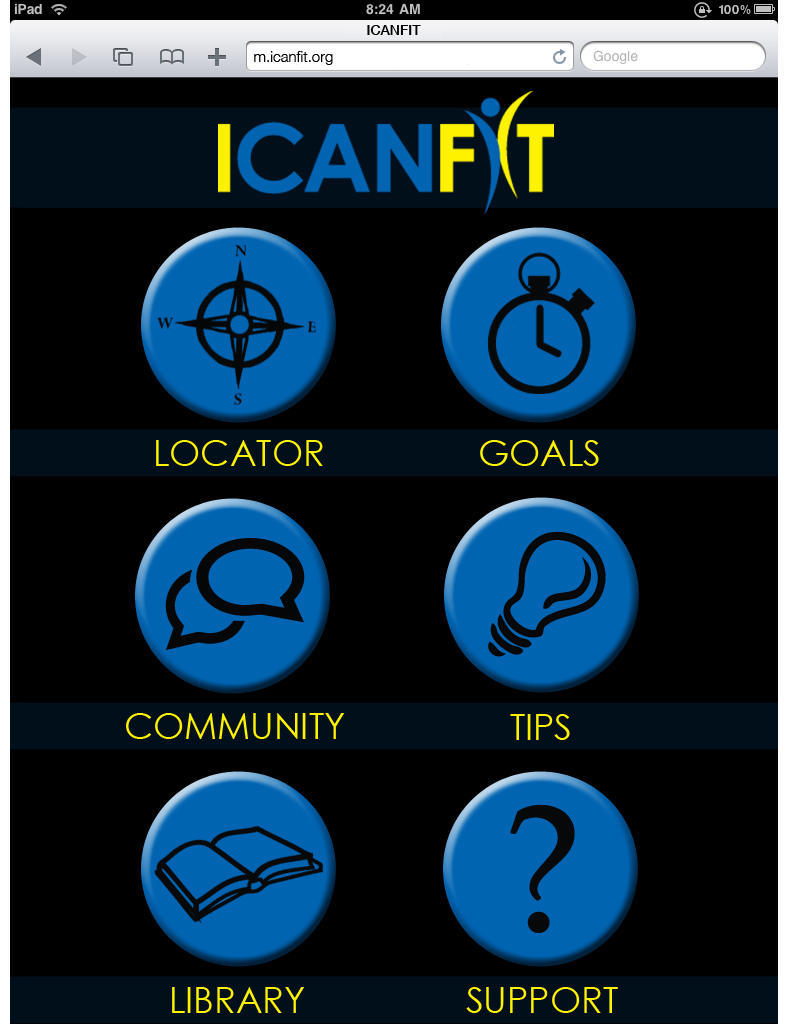
Major functions of iCanFIt on an iPhone interface.
Discussion
With the population of OCS expanding and few OCS having regular PA, a strong need exists for a cost-effective health promotion program targeting this population. Online access is increasingly common among older adults, and mobile use is also accelerating, thus offering a potential mode of widespread intervention delivery. A combination of Web and mobile technology that incorporates the best principles of chronic care management—including identifying patient preferences, addressing barriers to lifestyle changes, enhancing self-management skills, providing coaching and feedback, and facilitating peer support—offers an excellent opportunity to meet this need [25,26].
Although the number of online health promotion programs is skyrocketing with demonstrated efficacy [27,28], very few programs are available for OCS. This study documents the process necessary to develop a PA promotion program for OCS. It has long been recognized that employing user-centered design and development process is essential for ensuring a quality user experience [29-31]. Our formative research has involved the key stakeholders from very beginning and throughout the phase of protocol development. The resulting iCanFit protocol addresses OCS’ barriers to regular PA. It provides an engaging venue for achieving behavioral change through easy access to community resources, goal setting and reinforcement, and peer support. It is important that these functions are relevant to OCS and presented in a format that appeal to the intended audience.
Several limitations should be noted for this study. First, we had a relatively small sample size in both quantitative and qualitative data collection, which might introduce potential reporting bias. However, our participants were drawn from a diverse background and the data suggested saturation. Second, as our participants were recruited from communities in Texas, the findings may not be generalizable to OCS from other locations. We employed community outreach versus online recruitment because we needed to conduct an in-depth and sometimes repeated interviews with OCS to obtain their feedback. Third, our program only addressed 3 key barriers to regular PA identified by OCS and their care providers. Whether the program met their expectations and could promote regular PA and health outcomes requires a long-term study. We are now developing the iCanFit protocol to the active Web application. Once beta-testing is completed, we will conduct an efficacy trial to assess whether it can promote PA and other health outcomes of OCS.
The design of online health promotion programs, especially behavioral change programs, should reflect collaborative efforts between researchers, computer software designers, and key stakeholders. Through this formative research, we learned the importance of setting a realistic timeline and recruiting participants from diverse backgrounds. We also appreciate the value of a mixed-method study that involves key stakeholders to understand target users’ needs and preferences in order to identify best strategies for program development and evaluation of this new mobile-enabled Web application.
Acknowledgments
This study was supported from a pilot grant from Scott & White Healthcare Senior Health Program, and Mobile Application Program Award from National Library of Medicine South Central Region Network and CTxCARES, which is supported by Cooperative Agreement Number 1U48 DP001924 from the Center for Disease Control and Prevention. The findings and conclusions in this manuscript are those of the authors and do not necessarily represent the official positions of the funding agencies. We appreciate support from Gabriel Laguillo, Richard Wood, Debra Kellstedt, and Lorie Thibodeaux in data collection and thank all participants in our study.
Abbreviations
- CCP
cancer care providers
- CL
community leaders
- CTxCARES
Communities of Texas: Cancer • Activity • Research • Education • Support
- OCS
older cancer survivors
- PA
physical activity
Footnotes
Conflicts of Interest: None declared.
References
- 1.Siegel R, DeSantis C, Virgo K, Stein K, Mariotto A, Smith T, Cooper D, Gansler T, Lerro C, Fedewa S, Lin C, Leach C, Cannady RS, Cho H, Scoppa S, Hachey M, Kirch R, Jemal A, Ward E. CA Cancer J Clin. CA: A Cancer Journal for Clinicians. 2012; 2012. Cancer treatment and survivorship statistics, 2012; pp. 220–41. [DOI] [PubMed] [Google Scholar]
- 2.DeSantis C, Siegel R, Jemal A. Society AC. 2012. [2012-06-16]. Cancer treatment and survivorship facts and figures 2012-2013 http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-033876.pdf.
- 3.Ershler WB. Cancer: a disease of the elderly. J Support Oncol. 2003;1(4 Suppl 2):5–10. [PubMed] [Google Scholar]
- 4.Schmitz KH, Holtzman J, Courneya KS, Mâsse LC, Duval S, Kane R. Controlled physical activity trials in cancer survivors: a systematic review and meta-analysis. Cancer Epidemiol Biomarkers Prev. 2005 Jul;14(7):1588–95. doi: 10.1158/1055-9965.EPI-04-0703. http://cebp.aacrjournals.org/cgi/pmidlookup?view=long&pmid=16030088. [DOI] [PubMed] [Google Scholar]
- 5.Speck RM, Courneya KS, Mâsse LC, Duval S, Schmitz KH. An update of controlled physical activity trials in cancer survivors: a systematic review and meta-analysis. J Cancer Surviv. 2010 Jun;4(2):87–100. doi: 10.1007/s11764-009-0110-5. [DOI] [PubMed] [Google Scholar]
- 6.Courneya KS, Segal RJ, Mackey JR, Gelmon K, Reid RD, Friedenreich CM, Ladha AB, Proulx C, Vallance JK, Lane K, Yasui Y, McKenzie DC. Effects of aerobic and resistance exercise in breast cancer patients receiving adjuvant chemotherapy: a multicenter randomized controlled trial. J Clin Oncol. 2007 Oct 1;25(28):4396–404. doi: 10.1200/JCO.2006.08.2024. [DOI] [PubMed] [Google Scholar]
- 7.Holmes MD, Chen WY, Feskanich D, Kroenke CH, Colditz GA. Physical activity and survival after breast cancer diagnosis. JAMA. 2005 May 25;293(20):2479–86. doi: 10.1001/jama.293.20.2479. [DOI] [PubMed] [Google Scholar]
- 8.Courneya KS, Friedenreich CM. Physical exercise and quality of life following cancer diagnosis: a literature review. Ann Behav Med. 1999;21(2):171–9. doi: 10.1007/BF02908298. [DOI] [PubMed] [Google Scholar]
- 9.Ahmed RL, Thomas W, Yee D, Schmitz KH. Randomized controlled trial of weight training and lymphedema in breast cancer survivors. J Clin Oncol. 2006 Jun 20;24(18):2765–72. doi: 10.1200/JCO.2005.03.6749. [DOI] [PubMed] [Google Scholar]
- 10.Spence RR, Heesch KC, Brown WJ. Exercise and cancer rehabilitation: a systematic review. Cancer Treat Rev. 2010 Apr;36(2):185–94. doi: 10.1016/j.ctrv.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 11.Doyle C, Kushi LH, Byers T, Courneya KS, Demark-Wahnefried W, Grant B, McTiernan A, Rock CL, Thompson C, Gansler T, Andrews KS. Nutrition and physical activity during and after cancer treatment: an American Cancer Society guide for informed choices. CA Cancer J Clin. 2006;56(6):323–53. doi: 10.3322/canjclin.56.6.323. [DOI] [PubMed] [Google Scholar]
- 12.Schmitz KH, Courneya KS, Matthews C, Demark-Wahnefried W, Galvão DA, Pinto BM, Irwin ML, Wolin KY, Segal RJ, Lucia A, Schneider CM, von Gruenigen VE, Schwartz AL. American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Med Sci Sports Exerc. 2010 Jul;42(7):1409–26. doi: 10.1249/MSS.0b013e3181e0c112. [DOI] [PubMed] [Google Scholar]
- 13.Smith SG, Chagpar AB. Adherence to physical activity guidelines in breast cancer survivors. Am Surg. 2010 Sep;76(9):962–5. [PubMed] [Google Scholar]
- 14.Irwin ML. Physical activity interventions for cancer survivors. Br J Sports Med. 2009 Jan;43(1):32–8. doi: 10.1136/bjsm.2008.053843. [DOI] [PubMed] [Google Scholar]
- 15.Schmitz K. Physical activity and breast cancer survivorship. Recent Results Cancer Res. 2011;186:189–215. doi: 10.1007/978-3-642-04231-7_8. [DOI] [PubMed] [Google Scholar]
- 16.Irwin ML, Mayne ST. Impact of nutrition and exercise on cancer survival. Cancer J. 2008 Dec;14(6):435–41. doi: 10.1097/PPO.0b013e31818daeee. [DOI] [PubMed] [Google Scholar]
- 17.Brenner J PewInternet. 2012. [2013-02-06]. Pew Internet: Mobile http://pewinternet.org/Commentary/2012/February/Pew-Internet-Mobile.aspx.
- 18.Barrett L. AARP Research and Strategic Analysis. 2011. [2013-02-05]. Health and caregiving among 50+: ownership, use and interest in mobile technology http://assets.aarp.org/rgcenter/general/health-caregiving-mobile-technology.pdf.
- 19.Hesse BW, Moser RP, Rutten LJ, Kreps GL. The health information national trends survey: research from the baseline. J Health Commun. 2006;11 Suppl 1:vii–xvi. doi: 10.1080/10810730600692553. [DOI] [PubMed] [Google Scholar]
- 20.Chou WY, Liu B, Post S, Hesse B. Health-related Internet use among cancer survivors: data from the Health Information National Trends Survey, 2003-2008. J Cancer Surviv. 2011 Sep;5(3):263–70. doi: 10.1007/s11764-011-0179-5. [DOI] [PubMed] [Google Scholar]
- 21.Satterlund MJ, McCaul KD, Sandgren AK. Information gathering over time by breast cancer patients. J Med Internet Res. 2003;5(3) doi: 10.2196/jmir.5.3.e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peterson MW, Fretz PC. Patient use of the internet for information in a lung cancer clinic. Chest. 2003 Feb;123(2):452–7. doi: 10.1378/chest.123.2.452. [DOI] [PubMed] [Google Scholar]
- 23.Miles MB, Huberman AM. Qualitative data analysis: An expanded sourcebook. California: Sage Publications, Incorporated; 1994. [Google Scholar]
- 24.Hodes RJ. Planning and Evaluating Health Information Outreach Projects. 2011. [2013-02-05]. http://www.nlm.nih.gov/pubs/checklist.pdf.
- 25.Ory M, Jordan P, Bazzarre T. The Behavior Change Consortium: setting the stage for a new century of health behavior-change research. Health education research. 2002;17(5):500. doi: 10.1093/her/17.5.500. [DOI] [PubMed] [Google Scholar]
- 26.Ory MG, Lee Smith M, Mier N, Wernicke MM. The science of sustaining health behavior change: the health maintenance consortium. Am J Health Behav. 2010;34(6):647–59. doi: 10.5993/ajhb.34.6.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Webb TL, Joseph J, Yardley L, Michie S. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J Med Internet Res. 2010;12(1):e4. doi: 10.2196/jmir.1376. http://www.jmir.org/2010/1/e4/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hansen AW, Grønbæk M, Helge JW, Severin M, Curtis T, Tolstrup JS. Effect of a Web-based intervention to promote physical activity and improve health among physically inactive adults: a population-based randomized controlled trial. J Med Internet Res. 2012;14(5):e145. doi: 10.2196/jmir.2109. http://www.jmir.org/2012/5/e145/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wixon D, Ramey J. Field methods casebook for software design. New York: Wiley & Sons; 1996. [Google Scholar]
- 30.Mayhew DJ, editor The usability engineering lifecycle. CHI 98 conference summary on Human factors in computing systems; : ACM; 1998; Los Angeles. 1983. Apr 18, [Google Scholar]
- 31.Nielsen J. Designing Web Usability : The Practice of Simplicity. Indianapolis: New Riders Press; 1999. Dec 30, [Google Scholar]


