Abstract
We report a case of a-15-days-old infant presenting with firm palpable thickening of the left leg soft tissues along with induration. Radiographs of the leg revealed generalized calcification of soft tissues. No obvious underlying cause could be identified for tissue calcification and hence termed as Idiopathic calcinois cutis. There are reports of this condition in Pediatric and Dermatology literature, but very few reports in orthopedic literature. The aim of this report is to highlight the pathogenesis, course and review of literature of this relatively uncommon condition which can easily be mistaken by Orthopedic or General Surgeons for infective bony of soft tissue infection.
Keywords: Soft tissue infection, Calcinosis, Calcification, Infant
Introduction
Calcinosis is a term used to describe a group of disorders characterized by the deposition of calcium and phosphates in the organic matrix of soft tissues; skin (calcinosis cutis), dermis, muscles, periarticular tissues, and the visceral organs in rare occasions.1 It is a rare disorder with varying pathogenesis. The cause cannot be identified in some cases, and it is then labeled as idiopathic calcinosis. We report one such case in a neonate which was mistaken for soft tissue infection in an extremity.
Case Report
A 15-days-old girl born out of a non-consanguineous marriage to a 50 year-old mother G15 P13 at 38 weeks by assisted vaginal delivery for abruption placentae was presented to the Department of Surgery, Nizwa Regional Referral Hospital. On delivery, the baby had an Apgar score of 3/10 and was treated for birth asphyxia in NICU for 9 days. The child was readmitted to the pediatric surgical ward after 2 days of discharge with swelling and erythema of the left leg noticed by the mother since the first day of discharge. A provisional diagnosis of left leg soft tissue infection underlying acute osteomyelitis of the tibia was made and the patient was started on intravenous broad spectrum antibiotics. On admission, the neonate weighed 3.2 kg without any dysmorphic features. She was afebrile, non toxic, aerodynamically stable but irritable. Local examination of the left leg showed diffuse swelling of the whole leg with erythema, local warmth and tenderness. There was no local fluctuation or regional lymphadenopathy. (Fig 1)
Figure 1.
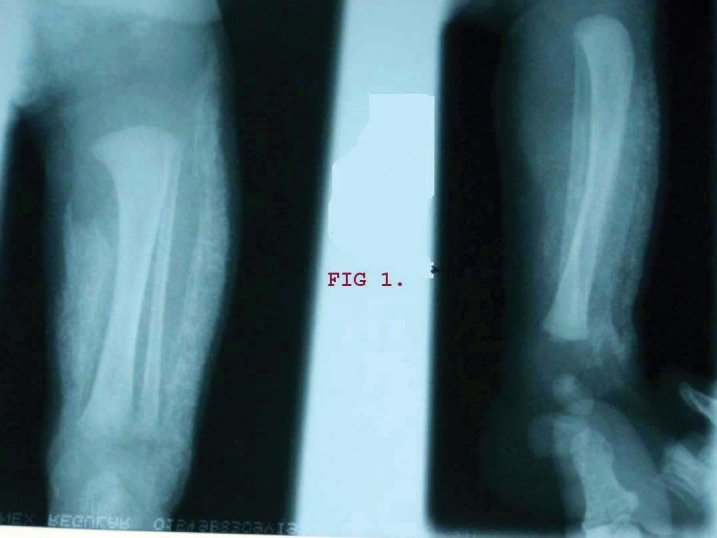
Anterio posterior and Lateral Radiographs of Left leg showing extraosseous ossification.
Investigations showed normal complete hierogram, ESR, liver and renal functions. Serum calcium, phosphorus, uric acid, electrolytes and alkaline phosphatase, as well as serum parathyroid levels were all normal. Plain radiograph of the left leg revealed generalized calcification of soft tissues of the leg involving muscle and subcutaneous tissues. Infantogram showed no other calcific deposits. Thus, the neonate was diagnosed to have isolated idiopathic calcinosis of the left leg and was treated symptomatically.
Discussion
Soft tissue calcification or calcinosis is an uncommon benign disorder described in the literature by Virchow as early as 1855.2 It is classified into four types according to etiology: Dystrophic, Metastatic, Iatrogenic and Idiopathic.3 The classification of other types varies in the literature but include Calcinosis cutis circumscripta, Calcinosis universalis, tumoral calcinois and transplant associated calcinosis cutis.
Dystrophic calcinosis is the most common type associated with connective tissue disorders and in traumatized tissues e.g., Dermatomyositis and Ehlers Danlos syndrome. The serum calcium and phosphorus ratio tends to be normal. Metastatic calcinosis occurs in the presence of disturbed calcium and phosphorus metabolism as in hypocalcemia and hyperphosphatemia. Patients with hypervitaminosis D, hyperparathyroidism, sarcoidosis, and chronic renal failure may have metastatic deposits of calcium in their soft tissues.4,5 Visceral involvement is common in this condition. Iatrogenic Calcinosis occurs due to the extravasation of calcium in tissues seen after intravenous calcium chloride or gluconate infusion; In the literature, Sandra et al. reported the first case in orthopedics.6
The rare Idiopathic Calcinosis is a condtion witout any identifiable cause of tissue calcification with normal serum calcium and phosphorus levels.7
Review of literature shows numerous theories to explain the pathogenesis of calcinosis. These include; local tissue damage leading to the release of alkaline phosphatase with increased local tissue pH resulting in calcium salt precipitation.8 In idiopathic calcinosis, there is no identifiable cause and it appears to be multifactorial in origin, ranging from hypothermia leading to subcutaneous fat necrosis and calcification. Other factors which can be contributory are phlebitis at the cannulation site, extravasation of solution in the surrounding tissues, especially calcium salts. Its use with anions such as sulphates, bicarbonates and phosphates should be avoided. Calcium gluconate should be preferred to calcium chloride as it is less likely to precipitate. Subcutaneous and intramuscular administration of drugs should be avoided due to the risk of developing tissue necrosis.6 Radiological changes can appear as early as 4-5 days with maximal roentgen graphic changes at 2 weeks. Resolution may take several months.5
In our case Idiopathic calcinois was diagnosed after dystrophic, metastatic and iatrogenic calcinosis were ruled out by the absence of history of trauma, parental therapy, normal serum calcium and phosphorus values. In addition, there was no evidence of connective tissue disorders. The condition can be mistaken for underlying soft tissue or bony infection during the initial stages and patient can be subjected to surgery.9
Conclusion
Idiopathic calcification although rare can be mistaken for infections of soft tissues, bones and joints. The etiology in such cases is not known and clinical presentation may be confusing. Early recognition is key to diagnosis. Regular follow up is mandatory in such cases.
Acknowledgements
The authors reported no competing interests and no funding was received for this study.
References
- 1.Sardesai VR, Gharpuray MB. Calcinosis cutis. Indian J Dermatol Venereol Leprol 2003. Jan-Feb;69(1):45-46 [PubMed] [Google Scholar]
- 2.Kalk-Metastasen VR. Virchows Arch Pathol Anat 1855;8(1):103-113 . 10.1007/BF01935316 [DOI] [Google Scholar]
- 3.Hussmann J, Russell RC, Kucan JO, Khardori R, Steinau HU. Soft-tissue calcifications: differential diagnosis and therapeutic approaches. Ann Plast Surg 1995. Feb;34(2):138-147 10.1097/00000637-199502000-00005 [DOI] [PubMed] [Google Scholar]
- 4.Koul PA, Ahmad SH, Ahmad F, Jan RA, Shah SU, Khan UH. Vitamin d toxicity in adults: a case series from an area with endemic hypovitaminosis d. Oman Med J 2011. May;26(3):201-204 10.5001/omj.2011.49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Puvabanditsin S, Garrow E, Titapiwatanakun R, Getachew R, Patel JB. Severe calcinosis cutis in an infant. Pediatr Radiol 2005. May;35(5):539-542 10.1007/s00247-004-1363-9 [DOI] [PubMed] [Google Scholar]
- 6.Propst-Proctor SL, Jones RB, Nagel DA. Iatrogenic soft-tissue calcification in an extremity. A case report. J Bone Joint Surg Am 1982. Mar;64(3):449-450 [PubMed] [Google Scholar]
- 7.Lanka P, Lanka LR, Ethirajan N, Krishnaswamy B, Manohar U. Idiopathic calcinosis cutis. Indian J Dermatol 2009;54(4):388-389 10.4103/0019-5154.57624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anderson HC. Calcification processes. Pathol Annu 1980;15(Pt 2):45-75 [PubMed] [Google Scholar]
- 9.Arora A, Agarwal A, Kumar S, Gupta SK. Iatrogenic calcinosis cutis–a rare differential diagnosis of soft-tissue infection in a neonate: a case report. J Orthop Surg (Hong Kong) 2005. Aug;13(2):195-198 [DOI] [PubMed] [Google Scholar]


