Abstract
Background:
Acute respiratory infections (ARI) are leading global cause of under-five mortality and morbidity.
Objective:
To elicit the prevalence and risk factors associated with ARI among under-five children.
Materials and Methods:
A community-based cross-sectional study was undertaken in 21 registered urban slums of Guwahati in Assam to determine the prevalence and risk factors associated with ARI among 370 under-five children from 184 households and 370 families.
Results:
The prevalence of ARI was found to be 26.22%; infants and female children were more affected. Majority of the ARI cases were from nuclear families (84.54%), living in kutcha houses (90.72%) with inadequate ventilation (84.54%), overcrowded living condition (81.44%), with kitchen attached to the living room (65.98%) and using biomass fuel for cooking (89.69%). ARI was significantly associated with ventilation, location of kitchen in household; presence of overcrowding, nutritional status, and primary immunization status also had impacts on ARI.
Conclusion:
The present study had identified a high prevalence of the disease among under-fives. It also pointed out various socio-demographic, nutritional, and environmental modifiable risk factors which can be tackled by effective education of the community.
Keywords: Acute respiratory infections, Immunization, Nutrition, Overcrowding, Under-five children
INTRODUCTION
A child constitutes the most priority and vulnerable group in terms of survival, growth, and development. Acute respiratory infections (ARI), particularly lower respiratory tract infections (LRTI), are the leading cause of under-five morbidity for an estimated just about two million childhood deaths globally.[1] ARI contributes to one-fifths of all under-five deaths in developing countries which is around 12 million every year.[2] It is estimated that Bangladesh, India, Indonesia, and Nepal together account for 40% of the global ARI mortality. ARI is responsible for about 30-50% of visits to health facilities and for about 20- 40% of admissions to hospitals.[3] In developed countries also physicians frequently encounter acute respiratory tract involvements in children.[4] In Indian slums, ARI constitutes more than two-third of all childhood illness.[5]
Childhood ARI is a significant public health problem in India, although robust epidemiological data are not available on its incidence. Higher risk is seen among young infants, malnourished children, non-exclusively breastfed children, and those with exposure to solid biomass fuel use.[6,7]
Studies in developing countries have identified risk factors to be among others crowding, nutritional factors, and parental smoking. Because of major differences in living conditions and environmental exposures, the certainty of these factors remains controversial.[8–11]
Population in the urban slums is a heterogeneous conglomerate of all caste, creed, and religion with a diversified lifestyle. In addition, the risk factors for childhood ARI is also present in respect to the environmental, socioeconomic, and health seeking behavior of the inhabitants. With this background, the study was undertaken in urban slums of Guwahati to elicit the prevalence and risk factors of ARI among under-five children.
MATERIALS AND METHODS
Study design and study period
A population based analytical cross-sectional study was undertaken in the urban slums of Guwahati from 15 September to 30 December 2004.
Study design
A population based analytical cross-sectional study was undertaken in the urban slums of Guwahati.
Study period
From 15 September to 30 December 2004.
Sample size
The sample size for the study was calculated using the formula n = 4 pq/l2, with 4%, where P = known prevalence, q = 1-p, and l = allowable permissible (absolute) error, set at 4%. Considering the prevalence of ARI in the age group under five in children in Assam to be 18% as reported by National Family Health Survey – 2 (NFHS- 2), 370 under-five children were recruited for the study. The list of registered slums was taken from the Town and Country Planning Department, Government of Assam. Out of 21 registered slums, seven slums were selected by simple random sampling and the number of participants selected per slum was based on “probability proportionate to size” technique.
The study instrument
This data collection tool was an interview schedule that was developed at the institute with the assistance from the faculty members and other experts of Department of Community Medicine, Guwahati Medical College. Detailed information regarding socio-demographic characteristics, socio-economic status, and health parameters were collected using this structured schedule for each household, regarding housing condition, family information, literacy and occupation, and parent's income, hygienic condition. By initial translation, back-translation, re-translation followed by pilot study, the questionnaire was custom-made for the study.
Method of data collection
Institutional ethical committee approved the study. The respondents were the caregivers of the children. So, all the caregivers were explained the purpose of the study and were ensured strict confidentiality. Written informed consents were taken from respective caregiver prior to the study. They were given the option not to participate in the study if they wanted. The principal investigator collected the data using the interview technique by house to house visits in the households of the selected slums. Children below five years were surveyed, with an average of five to six children per day, till 370 children from 184 families were covered. All efforts were made to collect the correct age of the child on the basis of parents information, age of other siblings, birth certificate etc. The nutritional status was assessed and graded on the basis of expected weight for age, by plotting in growth chart as classified by Indian Academy of Pediatrics. The weight of the children was measured with a standardized weighing scale (bathroom scale) with minimal clothes and bare foot. When the child was unable to stand, the weight of the child with the caregiver was taken and then the weight of the caregiver was deducted to get the weight to nearest 500 g.
Inclusion criteria
Under-five children and either a positive or negative history of ARI at the time of interview or within last 2 weeks recall period were included in the study.
Exclusion criteria
The cases with chronic respiratory ailments and in case of non-consenting caregivers were excluded from the study.
OPERATIONAL DEFINITION
Acute respiratory infections
Children with any one or combinations of symptoms and signs like cough and cold, running or blocked nose, sore throat, rapid breathing, noisy breathing, stops feeding and or drinking, chest indrawing etc, A new episode was taken as one occurring in an individual who had been free of symptoms for at least three consecutive days or more as per WHO (1997) definition of ARI.[12]
Immunization
Immunization status of the participants were obtained from immunization cards and for the evaluation of the immunization status, the criterion described by Narain was followed.[13]
Completely immunized: Three doses of DPT and three doses of OPV taken between 6 weeks to 9 months at an interval of 4 weeks, plus one dose of BCG, plus one dose of measles within 1 year of life.
Partially immunized: Not completely immunized but received one or more doses of the above vaccines.
Not immunized: Did not receive any vaccine dose.
Nutritional status
The nutritional status was assessed and the grading of malnutrition was calculated on the basis of expected weight for age, by plotting in Growth Chart, as classified by Indian Academy of Pediatrics.[14]
80-100% Normal
71-80% Grade I
61-70% Grade II
51-60% Grade III
<50-% Grade IV
Ventilation
Adequate: Window area one-fifth of the floor area or doors and windows combined two-fifth of the floor area.
Inadequate: Failing to fulfill the above criteria.[15]
Overcrowding
Overcrowding is when the per capita floor space area of the living room is below 50 sq foot, or otherwise when there is no sex separation in case of individuals more than 9 years of age, not husband and wife.[15]
Type of house
Pucca house: Houses where floor paved, walls are stone or brick-built and roof is tin, asbestos or concrete.
Kutcha house: Where floor packed earth, walls are dried mud or thatched, and roof is thatched, slate or other stone.
Semi-pucca: Houses where floor packed earth, walls are stone or brick-built and roof either tin or thatched.
Statistical analysis
The collected data were entered into MS-Excel spread sheets for analysis. The statistical analyses were done using Graph Pad In Stat version 3 soft ware. Percentages and Chi square tests were used in this study to analyze epidemiological variables.
RESULTS
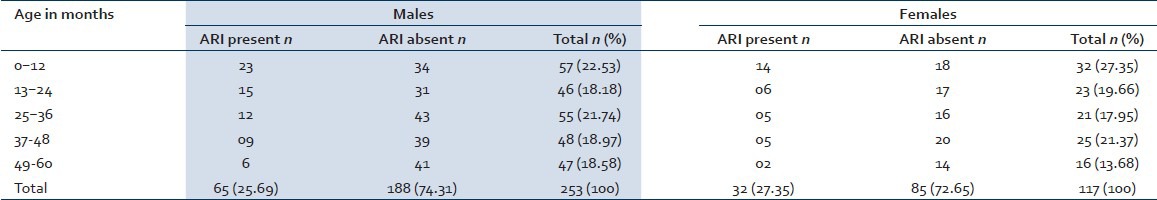
The study population consisted of children in the age group of less than 5 years from a heterogeneous group in terms of religion, language, place of origin, occupation, and income. Majority of the study participants were in the age group of 1-12 months and the prevalence of ARI was also common in that group (38.14%) followed by 13- 24 months (21.65%). The overall prevalence of ARI was found to be 26.22%. Among all participants, females were more affected with ARI (27.35%) than males (25.69%). As the children grew older, the prevalence of ARI gradually decreased in our study participants [Table 1].
Table 1.
Demographic profile of the study participants
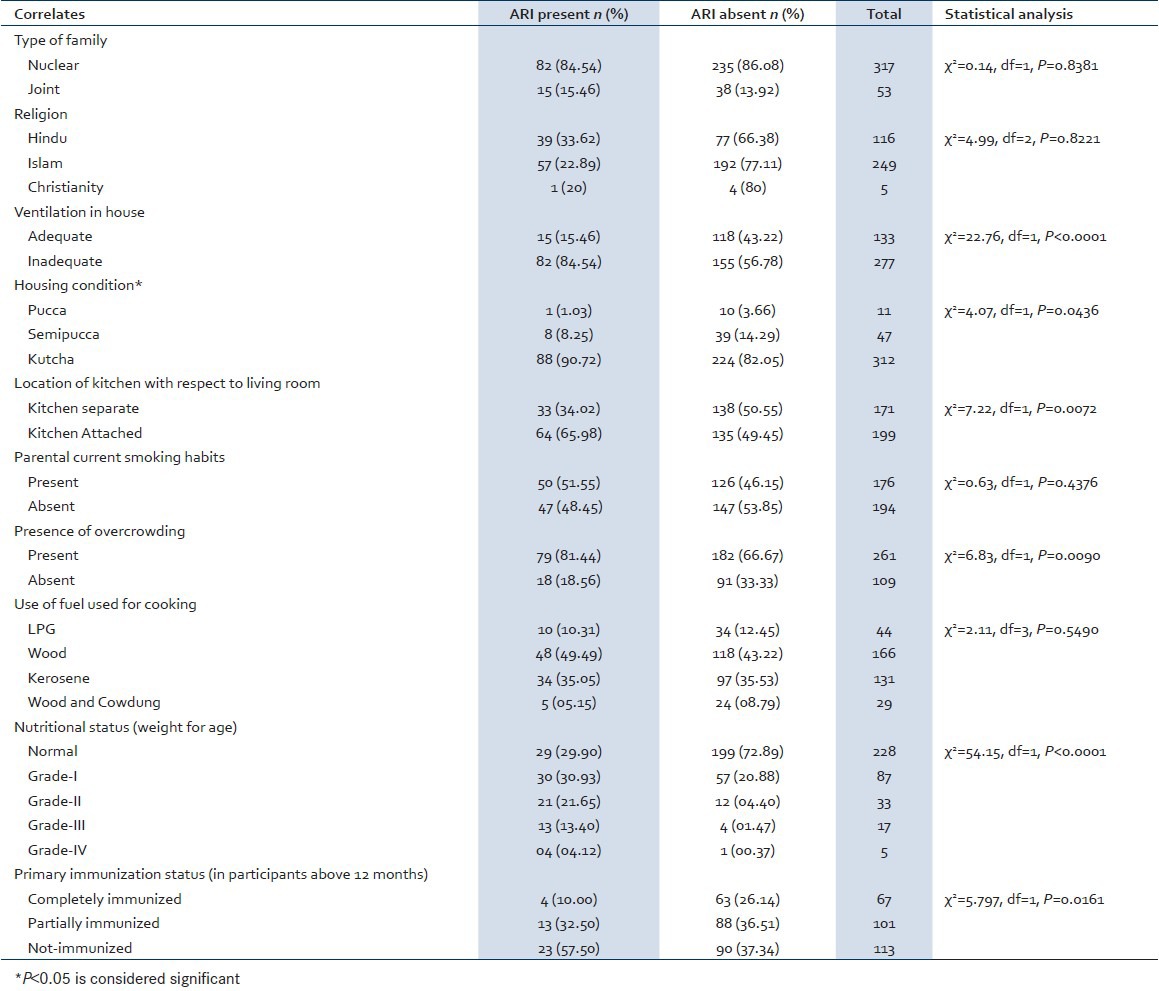
ARI was seen mostly in children from nuclear families (84.54%), living in kutcha houses (90.72%), with inadequate ventilation (84.54%), overcrowded (81.44%) with kitchen attached to the living room (65.98%), and using biomass fuel for cooking (89.69%).
Undernourished children had an increased risk of ARI as compared to normal participants (RR = 3.76). Any sort of undernourishment in terms of decreased weight of the child was compared with normal nutritional status as per Gomez classification. Similarly non-immunized kids had more chances of developing ARI. (RR = 2.01). Complete immunization among ARI cases was only 10%. In the non-immunized group ARI cases was noted as 57.5%. Children with completed primary immunization status were combined with those partially immunized and were compared with non-immunized children in determining the risk for ARI in relation to immunization status. A strong statistical difference exists between diseased and non-diseased participants in terms of ventilation in house location of kitchen in household, type of house, the presence of overcrowding, nutritional, and immunization status of the child. However, there was no significant statistical difference among the two groups in terms of type of family, religion, parental current smoking habits, and use of fuels for cooking [Table 2].
Table 2.
Correlates of ARI among the study participants
DISCUSSION
The present study has identified a high prevalence of ARI among under-fives and pointed out various socio-demographic, nutritional, and environmental as the modifiable risk factors. The overall prevalence of ARI was found to be 26.22%. In our study, the age group of 1-12 months were mostly affected with ARI. As the children grew older, the prevalence of ARI gradually decreased.
A study from Delhi reported that 14.6% in all children surveyed, had an attack of ARI in the preceding 2 weeks.[16] A cross-sectional study from Brazil reported that ARI in children under-five years was 25.6%, among which 76.4% had upper and 23.6% lower respiratory infections; no associations in respect to nutritional status or passive smoking in the family.[17] A study from Zambia reported that 6.9% of under-five children had ARI in the last 2 weeks; age of child and sex of child were significantly associated.[18] Related study reported that among under-five children prevalence of ARI was 49.8% where hospitalization was required in 7.6% of cases.[19] A comparable study in a rural community in Bangladesh reported that the prevalence of ARI in the community was 58.7%; the mean of ARI episodes was less than two per child per year.[20] Another community-based study carried out in a rural area of Delhi also reported the prevalence of ARI of 12.1% among under-fives that declined with increasing age; the incidence was 2.5 episodes per child per year.[21] A cross sectional study from Ahmadabad reported that prevalence of ARI was 22%. Age group of 4-5 years were mostly affected (47.3%).[22] A community-based study in a coastal village of Karnataka reported 6.42 episodes of ARI per child per year; the incidence of pneumonia was significantly higher among infants.[23] An epidemiological study carried out in West Tripura reported that the incidence of pneumonia was 16 per 1000 children in urban area. The incidence of pneumonia was found to be the highest in infant group.[24] A community-based study carried out in Maharashtra noted that the average incidence of ARI was 3.67 episodes/child/year.[25]
Sex
Among all participants in our study, females were more affected with ARI (27.35%) than males (25.69%). The study from Zambia observed that in the under-five children ARI was significantly associated with sex of child.[18] Bangladesh study reported that ARI in the rural community was 14.9 and 14.4% in males and females respectively in the ARI episodes.[18] Researchers concluded in the community-based study in a rural area of Delhi that among under-fives ARI episodes had no difference between sexes.[21] A hospital based case control study from Delhi reported that sex of the child was not documented to be significant risk factors of ARI.[26]
Ventilation in house
Inadequate ventilation (84.54%) was found to be significantly associated with ARI in our study. Similar findings were seen by Researchers from Ahmadabad where the prevalence of ARI in under-fives was significantly associated with inadequate ventilation.[20] Similar study from Mysore study reported that lack of adequate ventilation was significantly related with ARI in under-fives.[27] A study from rural Delhi reported that ARI incidence was significantly lower among children living in well-ventilated homes (1.79 episodes/child/year) than those living in poorly ventilated homes (2.87 episodes/child/year).[28] Another study from Maharashtra reported that inadequate ventilation was found to influence the incidence of ARI.[25]
Housing condition
Our study reflected a strong statistical association between occurrences of ARI with those living in kutcha houses (90.72%). The Delhi study reported that, type of housing was not documented to be significant risk factors of ARI.[26] The Karnataka noted that children of poor housing conditions suffered more frequently from ARI.[23]
Researchers from Maharashtra noted that incidence of ARI among under-five children was influenced by environmental factors like type of house.[25]
Presence of overcrowding
Our study reflected an association of overcrowding (81.44%) with risk of ARI. The Bangladesh study observed that the prevalence of ARI in under-fives in a rural community was significantly higher in overcrowded condition than not (62 vs. 38%).[20] Similar study from Ahmadabad reported that significant statistical association of ARI was seen in regard to overcrowding.[22] Mysore study on ARI in under-fives reported overcrowding as a significant socio-demographic risk factor.[27]
Parental current smoking habits
Our study could not find any significant statistical association between ARI and parental current smoking habits. A study from Brazil noted that ARI in children under five years was not associated with the passive smoking in the family.[17] The Bangladesh study noted that the prevalence of ARI in under-fives in the community was significantly associated with parental smoking (61 vs. 39%) when compared to those without ARI.[20] However, in the prevalence of ARI in under-five years of age, significant difference was not observed with parental smoking in a study from Ahmadabad.[22]
Use of fuel used for cooking
Though our study showed that use of biomass fuel for cooking was higher (89.69%) in the study area, however, there was no significant statistical association of prevalence of ARI with use of biomass fuels for cooking. The Ahmadabad study reported that prevalence of ARI in under-fives, significant statistical association was seen with the use of biomass fuel and smoky chullhas in the family.[22] The study from Delhi reported that cooking fuel other than liquid petroleum gas was the significant contributors of ARI in children under 5 years.[26] Mysore study on ARI reported that significant socio-demographic risk factors were use of biomass fuel pollution.[27] Similar Karnataka study reported higher ARI episode with smoke producing conditions.[23] A study from Zimbabwe reported that about two-thirds (66%) of children lived in households using biomass fuels and 16% suffered from ARI during the 2 weeks preceding the survey. After adjusting for child's age, sex, nutritional status, religion, household living standard, children in households using wood, dung, or straw for cooking were more than twice as likely to have suffered from ARI as children from households using LPG/natural gas or electricity.[29] Study carried out in Maharashtra found that incidence of ARI was closely associated with biomass fuel used for cooking.[25]
Nutritional status (weight for age)
Our study reflected that undernourished children had an increased risk of ARI as compared to normal participants (RR = 3.77). A strong statistical difference exists between diseased and non-diseased participants in terms of the poor nutritional status of the child. The study from Brazil reported that ARI was not associated with the nutritional status in under-five years children.[17] Researchers from Bangladesh reported that the prevalence of ARI in the rural community was significantly higher in ARI cases compared to those without ARI when malnutrition (63 vs. 37%) was a risk correlate.[20] The study from Ahmadabad reported in the prevalence of under-five, significant statistical association of ARI was seen in regard to malnutrition.[22] The Delhi study observed that severe malnutrition was a significant contributor of ARI in children under-five years.[21] Mysore study on ARI reported that significant socio-demographic risk factors were overcrowding and partial immunization. Significant risk factors were use of biomass fuel pollution, lack of ventilation, and malnutrition.[27] A study from rural Delhi, that, the annual ARI incidence was 3.27 episodes per child in the moderate to severely malnourished children. Lower respiratory infection was more affected by adverse nutritional status than upper respiratory infection.[28] A similar study from West Tripura reported that Malnourished under-five children had higher likelihood for developing respiratory infection.[24] The incidence of ARI was found to be closely associated with nutritional status of the child as reported by researchers in Maharashtra[25] The researchers from Kolkata opined that malnutrition is significantly associated with occurrence of ARI among under-five children.[30]
Primary immunization status (in participants above 12 months)
Non-immunized kids were found to be at an increased risk for ARI in our study (RR = 2.01). Complete immunization among ARI cases was only 10%. In the non-immunized group, ARI cases were noted as 57.5%. Inappropriate immunization for age was significantly related with ARI in under-five children in Delhi study.[26] Mysore study on ARI reported that significant socio-demographic risk factors were overcrowding and partial immunization. Significant risk factors were the use of biomass fuel pollution, lack of ventilation, and malnutrition.[27] Similarly, a study from West Tripura noted that the incidence of respiratory infection was higher among non-immunized children.[24] A hospital-based prospective study conducted in Kolkata found that non-immunization was a significant risk factor for ARI.[30]
We found that ARI was mostly seen in children from nuclear families (84.54%). However, there was no significant statistical difference among the two groups in terms of type of family. Further, our study documented a strong correlation ARI with location of kitchen. But, our study failed to find any association between episodes of ARI with the religion of the child. We have yet to find comparable references in the published literature on these two variables.
Strength of the study
ARI is still a public health problem killing millions of our future citizens. The study would be an eye-opener for further research in this part of country with resource poor health care settings. The risk factors identified for ARI would help the planners and program managers of our state of Assam and neighboring states to select and plan approaches in curbing the menace in North eastern states.
Limitations of the study
The study was undertaken in the urban slums of Guwahati city. Due to diversity of slum population in different parts of India and also the living condition, the findings cannot be generalized. Farther, it could have been better if other related risk variables could be included in the study that was not possible due to manpower, money, and time constraints.
Future directions of the study
There is a need to carry out extensive multi centric studies involving both rural and urban areas to identify all the risk factors precipitating ARI, so that preventive program becomes more successful in India. Not only the array of socio-demographic, socio-economic, and environmental factors along with the health seeking behavior, but also other physiological and behavioral risk factors need to be explored for effective control of ARI in under-five segment of population.
CONCLUSION
The present study had identified a high prevalence of ARI among under-fives. It also pointed out various socio-demographic, nutritional, and environmental modifiable risk factors which can be tackled by effective education of the community.
ACKNOWLEDGEMENTS
We acknowledge co-operation of Faculties of the department of Com Med, Guwahati Medical College and the participants of the study in undertaking the project.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Madhi SA, Klugman KP. Acute Respiratory Infections. Copyright © 2006. The International Bank for Reconstruction and Development. The World Bank. [PubMed] [Google Scholar]
- 2.WHO and UNICEF: Management of childhood illness in developing countries-rationale for an integrated strategy, WHO. 1998 [Google Scholar]
- 3.Vashishtha VM. Current status of tuberculosis and acute respiratory infections in India: Much more needs to be done. Indian J Pediatr. 2010;47:88–9. doi: 10.1007/s13312-010-0005-6. [DOI] [PubMed] [Google Scholar]
- 4.Frese T, Klauss S, Herrmann K, Sandholzer H. Children and adolescents as patients in general practice – The reasons for encounter. J Clin Med Res. 2011;3:177–82. doi: 10.4021/jocmr597w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rahman MM, Shahidullah M. Risk factors for acute respiratory infection among the slum infants of Dhaka city. Bangladesh Med Res Counc Bull. 2001;27:55–62. [PubMed] [Google Scholar]
- 6.Mathew JL, Patwari AK, Gupta P, Shah D, Gera T, Gogia S, et al. Acute respiratory infection and pneumonia in India: A systematic review of literature for advocacy and action: UNICEF-PHFI series on newborn and child health, India. Indian Pediatr. 2011;48:191–218. doi: 10.1007/s13312-011-0051-8. [DOI] [PubMed] [Google Scholar]
- 7.Dhimal M, Dhakal P, Shrestha N, Baral K, Maskey M. Environmental burden of acute respiratory infection and pneumonia due to indoor smoke in Dhading. J Nepal Health Res Counc. 2010;8:1–4. [PubMed] [Google Scholar]
- 8.Azizi BH, Zulkifli HI. Kasim MS: Protective and risk factors for acute respiratory infections in hospitalized urban Malaysian children: A case control study Southeast Asian. J Trop Med Public Health. 1995;26:280–5. [PubMed] [Google Scholar]
- 9.Campbell H, Armstrong JR. Byass P: Indoor air pollution in developing countries and acute respiratory infection in children. Lancet. 1989;1:1012. doi: 10.1016/s0140-6736(89)92647-0. [DOI] [PubMed] [Google Scholar]
- 10.Vathanophas K, Sangchai R, Raktham S, Pariyanonda A, Thangsuvan J, Bunyaratabhandu P, et al. A community-based study of acute respiratory tract infection in Thai children. Rev Infect Dis. 1990;12:S957–65. doi: 10.1093/clinids/12.supplement_8.s957. [DOI] [PubMed] [Google Scholar]
- 11.Weber MW, Milligan P, Hilton S, Lahai G, Whittle H, Mulholland EK. Greenwood BM: Risk factors for severe respiratory syncytial virus infection leading to hospital admission in children in the Western Region of The Gambia. Int J Epidemiol. 1999;28:157–62. doi: 10.1093/ije/28.1.157. [DOI] [PubMed] [Google Scholar]
- 12.Banerjee KB, Venghese T. J. NICD (DGHS) G.O.I. Delhi: 1991. ARI and its control in under-fives. [Google Scholar]
- 13.Narain JP, Banerjee KB. Epidemiology of ARI. Ind J Pediatrics. 1987;54:153–60. doi: 10.1007/BF02750800. [DOI] [PubMed] [Google Scholar]
- 14.Ghai OP, Gupta P, Paul VK. Essential Pediatrics. 6th ed. New Delhi: 2005. Nutrition and macronutrient disorders; pp. 101–6. [Google Scholar]
- 15.Park K. Park's textbook of preventive and social medicine. 21st ed. Jabalpur: Banarsidas Bhanot Publishers; 2011. Environment and health; pp. 681–94. [Google Scholar]
- 16.Gupta N, Jain SK, Ratnesh , Chawla U, Hossain S, Venkatesh S. An evaluation of diarrheal diseases and acute respiratory infections control programmes in a Delhi slum. Indian J Pediatr. 2007;74:471–6. doi: 10.1007/s12098-007-0080-4. [DOI] [PubMed] [Google Scholar]
- 17.Duarte DM, Botelho C. Clinical profile in children under five year old with acute respiratory tract infections. J Pediatr (Rio J) 2000;76:207–12. doi: 10.2223/jped.55. [DOI] [PubMed] [Google Scholar]
- 18.Siziya S, Muula AS, Rudatsikira E. Diarrhoea and acute respiratory infections prevalence and risk factors among under-five children in Iraq in 2000. Ital J Pediatr. 2009;25;35:8. doi: 10.1186/1824-7288-35-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Botelho C, Correia AL, da Silva AM, Macedo AG, Silva CO. Environmental factors and hospitalization of under-five children with acute respiratory infection. Cad Saude Publica. 2003;19:1771–80. doi: 10.1590/s0102-311x2003000600021. [DOI] [PubMed] [Google Scholar]
- 20.Rahman MM, Rahman AM. Prevalence of acute respiratory tract infection and its risk factors in under-five children. Bangladesh Med Res Counc Bull. 1997;23:47–50. [PubMed] [Google Scholar]
- 21.Chhabra P, Garg S, Mittal SK, Satyanarayan L, Mehra M, Sharma N. Magnitude of acute respiratory infections in under five. Indian Pediatr. 1993;30:1315–9. [PubMed] [Google Scholar]
- 22.Bipin P, Nitiben Talsania Sonaliya KN. A study on prevalence of acute respiratory tract infections (ARI) in under five children in urban and rural communities of Ahmedabad district, Gujarat. Natl J Community Med. 2011;2:255–9. [Google Scholar]
- 23.Acharya D, Prasanna KS, Nair S, Rao RS. Acute respiratory infections in children: A community based longitudinal study in south India. Indian J Public Health. 2003;47:7–13. [PubMed] [Google Scholar]
- 24.Deb SK. Acute respiratory disease survey in Tripura in case of children below five years of age. J Indian Med Assoc. 1998;96:111–6. [PubMed] [Google Scholar]
- 25.Singh MP, Nayar S. Magnitude of acute respiratory infections in under five children. J Commun Dis. 1996;28:273–8. [PubMed] [Google Scholar]
- 26.Broor S, Pandey RM, Ghosh M, Maitreyi RS, Lodha R, Singhal T, et al. Risk factors for severe acute lower respiratory tract infection in under-five children. Indian Pediatr. 2001;38:1361–9. [PubMed] [Google Scholar]
- 27.Savitha MR, Nandeeshwara SB, Pradeep Kumar MJ, ul-Haque F, Raju CK. Modifiable risk factors for acute lower respiratory tract infections. Indian J Pediatr. 2007;74:477–82. doi: 10.1007/s12098-007-0081-3. [DOI] [PubMed] [Google Scholar]
- 28.Chhabra P, Garg S, Mittal SK, Chhabra SK. Risk factors for acute respiratory infections in underfives in a rural community. Indian J Matern Child Health. 1997;8:13–7. [PubMed] [Google Scholar]
- 29.Mishra V. Indoor air pollution from biomass combustion and acute respiratory illness in preschool age children in Zimbabwe. Int J Epidemiol. 2003;32:847–53. doi: 10.1093/ije/dyg240. [DOI] [PubMed] [Google Scholar]
- 30.Das PK, Saha JB, Basu K, Lahiri S, Sarkar GN. Some clinic-epidemiological aspect of bronchiolitis among infants and young children-A hospital based study. Indian J Public Health. 2003;47:66–71. [PubMed] [Google Scholar]


