Abstract
This study examined the influence of trauma history and PTSD symptoms on the behavior of veterans and their intimate partners (287 couples; N = 574) observed during conflict discussions and coded using the Rapid Marital Interaction Coding System (Heyman, 2004). Dyadic structural equation modeling analyses showed that PTSD was associated with more frequent displays of hostility and psychological abuse and fewer expressions of acceptance and humor in both veterans and their partners. Findings provide new insight into the social and emotional deficits associated with PTSD and emphasize the importance of addressing the trauma histories and PTSD of both partners when treating veteran couples with relationship disturbance.
Relationship conflict is an all-too-frequent consequence of deployments for military couples. Studies of veterans and their intimate partners have found posttraumatic stress disorder (PTSD) to be a significant contributor to these problems and linked to increased relationship discord, poor relationship adjustment, and elevated psychological and physical aggression toward partners (Byrne & Riggs, 1996; Carroll, Rueger, Foy, & Donahoe, 1985; Dekel & Monson, 2010; Monson, Taft, & Fredman, 2009; Taft et al., 2005; Taft et al., 2009; Taft, Watkins, Stafford, Street, & Monson, 2011). In a recent meta-analysis, Taft et al. (2011) examined the strength of associations between PTSD severity and measures of couple conflict across 31 studies and found mean observed correlations in the range of .32 to .36. These associations were stronger in veteran samples and in males compared to civilian samples and females, respectively. Other research has found that veterans with PTSD divorce at higher rates than trauma-exposed veterans without PTSD (Cook, Riggs, Thompson, Coyne, & Sheikh, 2004; Jordan et al., 1992; Whisman, 1999) and that during the first years of the wars in Iraq and Afghanistan, divorce rates in U.S. Army personnel increased by approximately 100% (Miles, 2005).
Findings of several studies indicate that trauma exposure itself may not be a direct cause of relationship disturbance and/or partner violence, but rather, suggest that PTSD plays a mediating role in this association (Orcutt, King and King, 2003; Taft, Schumm, Marshall, Panuzio, & Holtzworth-Munroe, 2008; Taft, Schumm, Panuzio & Proctor, 2008). For example, Orcutt et al. (2003) examined the impact of early-life stressors, war-zone stressors, and PTSD symptom severity on intimate partner violence among 376 Vietnam veteran couples. Analyses revealed significant indirect effects of combat exposure and perceived warzone threat on intimate partner violence that were mediated via PTSD severity. Other investigators have found that gender, age, type of trauma, personality traits and other factors moderate the strength of associations between trauma, PTSD, and relationship disturbance (for a review see, Monson et al., 2009). For instance, Taft, Schumm, Panuzio et al. (2008) reported that while PTSD symptoms mediated the association between combat exposure and poor family adjustment in male and female veterans, analyses based on a female veteran subsample revealed significant direct effects of combat exposure on family adjustment while controlling for PTSD. Furthermore, childhood trauma has long been implicated in the etiology of adult attachment problems and evidence suggests that repeated trauma in childhood predicts poor interpersonal relationships and intimacy problems in adulthood even when controlling for the influence of current PTSD on these outcomes (Davis, Petretic-Jackson & Ting, 2001).
Most prior studies in this area have relied on self- and/or partner-reports of relationship conflict using the Conflict Tactics Scale (CTS or CTS-2; Straus, Hamby, Boney-McCoy, & Sugarman, 1996; Taft et al., 2011). One significant limitation of this approach is that social desirability biases and other distortions inherent to self-report measures tend to yield low rates of inter-partner agreement on this measure and thus limits the usefulness of such reports (e.g., Heyman, Feldbau-Kohn, Ehrensaft, Langhinrichsen-Rohling, & O’Leary, 2001; Simpson, & Christensen, 2005). In addition, when the assessment of psychiatric symptoms and relationship functioning are both based on self-report, estimates of the association between these measures tend to be inflated by common method variance. One solution to these limitations is to study relationship conflict directly via behavioral observations of couples’ interactions. Over the past forty years, researchers in the area of couples and family psychology have developed sophisticated and reliable methods for measuring couples’ behavior while they are engaged in conversation about sources of conflict in their relationships. These methods aim to capture essential processes that underlie relationship disturbance and, therefore, are the focus of many of the major theories of, and therapies for, intimate relationship problems (Heyman, 2001).
Couples observational coding methods involve recording and describing behavioral events and, as noted by Gottman and Notarius (2000), can “reveal a replicable portrait of complex social interaction that lies beyond the natural awareness of even the most keenly sensitive spouse or partner and thus lies beyond assessment with self-report instruments” (p. 927). The external validity of couples conflict interactions observed in the laboratory is supported by the substantial similarity of home and lab observations (Gottman, 1979) and by couples’ reports that their interactions during observation were typical of their home interactions (Foster, Caplan, & Howe, 1997; Margolin, John, & Gleberman, 1988). These methods can be used to identify and quantify observable conflict tactics and behaviors that may lead to episodes of physical and psychological abuse as well as longer-term relationship outcomes such as divorce. These findings can, in turn, be used to identify new targets and methods for intervention in couples therapy. However, despite the scientific and clinical appeal of these approaches, to our knowledge, no prior study has used behavioral observation to study relationship disturbance in veterans and their partners or to examine the influence of trauma exposure and PTSD on their interactions.
Positive and Negative Affect, Couples’ Interactions, and PTSD
The experience, expression, and exchange of positive and negative affect are fundamental to couples’ interactions (Gottman & Levenson, 1986; Gottman & Levenson, 1992). Conflict discussions are characterized by a bi-directional interplay of positive and negative emotions, and the sequence and balance of these exchanges are essential indicators and determinants of relationship quality. Positive and negative emotional behaviors observed during conflict discussions have been shown to reliably discriminate distressed from non-distressed couples (Heyman, 2001), and the ratio of positive to negative behaviors prospectively predicts long-term relationship satisfaction and divorce outcomes (Gottman, Coan, Carrére, & Swanson, 1998; Gottman, & Krokoff, 1989). In couples in which one or both partners are emotionally impaired these interactions may be profoundly disrupted. For example, couples with a depressed or alcoholic partner express less positive and more negative communications compared to couples without an impaired partner (Jacob, & Krahn, 1988; Johnson & Jacob, 1997; Linden, Hautzinger, & Hoffman, 1983; Ruscher & Gotlib, 1988). Depressed individuals tend to be more tense, negative, and self-preoccupied in communications with their partners despite exhibiting a capacity for healthy socialization with strangers (Hooper, Roberts, Hinchcliffe, & Vaughn, 1977). In addition, while it is normal for couples to exhibit an equal exchange of expressed emotion, couples with a depressed partner show an asymmetrical pattern characterized by more negative evaluations directed toward the depressed than the non-depressed partner (Linden et al., 1983).
Research has shown that the expression and exchange of positive affect (i.e., through humor, acceptance, affection, and demonstrations of interest) plays a key role in sustaining intimate relationships. For example, Gottman et al. (1998) evaluated competing hypotheses regarding relationship processes predictive of marital outcomes in newlywed couples and found that the amount of positive affective expression observed during conflict discussions predicted divorce status 6 years later. Furthermore, these investigators found that humor expressed by the wife, as well as humor, affection, and validation expressed by the husband, were the strongest predictors of whether couples divorced or stayed together during this interval. Other research has shown that couples who use affiliative humor during conflict discussions are more satisfied with their relationship (Campbell, Martin, & Ward, 2008), and that those who express acceptance of each others’ self-disclosures enjoy greater relationship satisfaction and well-being (Gottman & Notarius, 2000).
Like depression, PTSD is associated with alterations in emotional behavior that contribute to functional impairment in various domains, including intimate relationships. The DSM-IV (American Psychiatric Association, 1994) definition of the diagnosis lists several symptoms that would be expected to adversely affect the expression and exchange of emotion in intimate relationships including symptom C6 “restricted range of affect” which includes the language “unable to have loving feelings,” symptom C5 “detachment or estrangement from others,” and, in the domain of negative emotions, symptom D2 “irritability or outbursts of anger.” Thus, PTSD is characterized not only by symptoms of distress and heightened negative emotionality (e.g., trauma-cue reactivity, anxiety and anger) but also by anhedonia (e.g., Kashdan, Elhai, & Frueh, 2006; Frewen, Dozois, & Lanius, 2012) and deficits in the domain of positive emotionality (Wolf et al., 2008) including social closeness (i.e., the tendency to foster and enjoy close affiliations; Miller, Greif, & Smith, 2003; Wolf, Miller, Harrington, & Reardon, 2012). Prior research has shown that veterans with chronic PTSD report greater anxiety related to intimacy (Riggs, Byrne, Weathers, & Litz, 1998). They are less self-disclosing and emotionally expressive with their partners compared to their counterparts without the diagnosis (Carroll et al., 1985) and this association appears to be accounted for primarily by the emotional numbing cluster of PTSD symptoms (Cook et al., 2004). However, virtually all prior studies on this topic has been based on associations among self-report measures, so little is known about the influence of PTSD symptoms on observable behavior during interactions between veterans with PTSD and their intimate partners.
Study Aims and Hypotheses
The primary aim of this study was to examine the behavior of trauma-exposed veterans and their intimate partners during conflict discussions and test hypotheses about the influence of trauma and PTSD on the nature and quality of their interactions. Based on the foregoing, we hypothesized that PTSD would be associated with elevated negative and reduced positive expressions during conflict discussions. Our approach to hypothesis testing was based on the Actor-Partner Interdependence Model (APIM; Cook & Kenny, 2005) which is a method of dyadic data analysis that distinguishes between actor effects (involving associations among within-subject variables) and partner effects (involving the influence of one member of a couple on the other). We also simultaneously compared the direct and indirect effects of trauma and PTSD on conflict behavior. On the basis of prior research (e.g., Taft, Schumm, Panuzio & Proctor, 2008), we predicted that the influence of an individual’s trauma history on his/her own behavior during conflict discussions would be mediated by his or her PTSD severity (i.e., an indirect actor effect). We also examined the alternative direct actor effect hypothesis suggesting that an individual’s trauma history is directly related to his/her conflict behavior, independent of PTSD (c.f., Davis et al, 2001).
The second aim of the study was to evaluate the relative contribution of the veteran’s versus spouse’s1 PTSD symptoms on observed behavior during conflict discussions. Here again, the extant literature suggested competing hypotheses: On the one hand, prior studies suggesting that depressed women are more expressive of negative affect in their relationships than are depressed men (Padesky & Hammen, 1981) suggested that spouses (who were predominantly female in this study) would evidence a stronger association PTSD and negative conflict behavior compared to veterans. On the other hand, Taft et al.’s (2011) meta-analysis indicated that the strength of the PTSD-relationship disturbance association was greater for men than for women, so we also tested the alternative hypothesis that stronger effects of PTSD severity on conflict behavior would be observed in veterans compared to their spouses. Finally, we also evaluated an “equal effects” or mutual influence model in which regressive actor and partner effects associated with both members of the couple were constrained to be equal to one another.
Method
Participants
Veterans were recruited at two U.S. Department of Veterans Affairs medical centers via flyers, mailings, and clinician referrals. The study was approved and reviewed annually by the appropriate Institutional Review Board (IRB) and research committees at both institutions. Study eligibility was determined during a telephone screen and required the veteran to (a) have been cohabitating with an intimate partner for the 12 months prior to study enrollment, and (b) endorse a history of exposure to a traumatic event meeting the DSM-IV PTSD Criterion A. In addition, the veteran’s partner must have been willing to participate in the study. Recruitment yielded 298 couples (i.e., 596 individuals); 177 pairs were enrolled at VA Boston Healthcare System and 121 at New Mexico VA Healthcare System. Data for 11 couples who enrolled in the study were omitted from analyses for the following reasons: 3 voluntarily withdrew before completing the study protocol, 2 were found ineligible after being consented and 6 couples were terminated by study staff because one or both members were unable to conform their behavior to protocol requirements. Thus, the final sample comprised 287 couples (N = 574 individuals) with 87% (n = 249 couples) including a veteran and a non-veteran spouse. In the remaining 13% (n = 36 couples), both members of the couple were veterans. In these cases, the individual who made initial contact with study staff and was screened for study eligibility (14 male; 22 female) was designated as the “veteran” and the other as the “spouse”. In seven couples, both participants were female; all other couples were male-female pairs.
Veterans were predominantly male (n = 258, 89.9%) and the spouses female (n = 265, 92.3%). Veterans ranged in age from 22 to 74 (M = 52.5, SD = 10.9), their spouses ranged in age from 19 to 75 (M = 50.3, SD = 11.0). Self-reported race and ethnicity of the sample was predominantly White, not Hispanic (80.7%), 9.8% was Black, 9.4% was American Indian or Alaskan Native, 1.6% was Asian, 0.7% was Hawaiian or Pacific Islander, and 7% reported unknown racial origin (demographic categories were not mutually exclusive so totals exceed 100%). Hispanic or Latino ethnicity was endorsed by 19.5% of the sample.
Most of the relationships in this study were longstanding: 40.1% of couples reported being together for more than 20 years and 24% had been together for more than 10 years. Eighty-eight percent had earned at least a high school degree and 26.8% earned a bachelor’s or graduate degree. A substantial proportion (42.8%) was unemployed or receiving disability payments, 33.4% worked full or part-time, 19.9% were retired, and 3.1% were students. Twenty-four percent of the sample reported an annual income of $15,000 or less, while 31% reported annual income greater than $45,000.
With regard to veteran’s branch of military service, 51.4% reported serving in the Army, 16.7% in the Navy, 15.8% in the Marines, 17.3% in the Air Force, and 3.4% in the Coast Guard. Eras of military service were: 10.2% World War II, 41.2% Vietnam War, 15.5% Operation Desert Storm, 15.2% Operation Iraqi Freedom or Operation Enduring Freedom, 0.6% Korean War, and 17% other eras.
Of the final sample, 42.9% (n = 123) of the veterans and 14.3% (n = 41) of spouses met criteria for a current diagnosis of PTSD and 65.5% (n = 188) of veterans and 32.8% (n = 94) of spouses met criteria for a lifetime diagnosis of PTSD. The index Criterion A event was determined through clinical interview; 29.1% participants endorsed combat-related trauma, 9.8% sudden death of a friend or loved one, 7.2% childhood sexual trauma, 6.9% physical assault, 6.6% motor vehicle accident, 4.7% childhood physical punishment, and 4% adult sexual trauma as their index trauma (i.e., the event on which the CAPS administration was based). Several additional index trauma types were endorsed (e.g., natural disaster, or serious accident), each occurring in less than 4% of the sample.
Procedure
The study was conducted in one or two sessions and involved administration of a series of self-report measures and diagnostic interviews (with partners located in separate rooms) and two 10-minute conflict discussions. The conflict discussions took place in a private suite and were video-recorded. The duration of the discussions was based on parametric research by Heyman et al. (2001) who found this interval to be sufficient to make reliable frequency estimations of the relevant behaviors. Discussion topics were selected using the Desired Changes Questionnaire (described below; Heavey, Layne, & Christensen,1993) which asked participants to rate and then rank-order the degree to which they wished that their partners would change in various domains. Each partner’s most important topic was then chosen for the discussion unless either partner indicated that they were uncomfortable discussing it. If both partners chose the same topic, the veteran’s second most important topic was used. Participants were instructed to discuss and stay on the topic for the entire 10 minute period of each discussion. They were also given instructions about how to terminate the procedure if they became uncomfortable. The two discussions were separated by a 5-minute break during which partners completed self-report questionnaires.
The Clinician Administered PTSD Scale (CAPS; Blake et al, 1995) interviews were administered by advanced psychology graduate students, postdoctoral-level clinical psychology trainees, or licensed clinical psychologists. Interviewers and secondary CAPS coders underwent training that involved review of interview manuals and viewing and scoring of previously-recorded and scored CAPS interviews. Competency was established by scoring a “gold standard” recorded interview that had been developed previously by a consensus team of experienced clinicians. All interviewers and secondary raters achieved perfect diagnostic agreement on this certification. Throughout the course of the study, weekly diagnostic reliability meetings were held to review discrepancies between interviewer and secondary rater scores with the video-recordings used as the basis for discussion. The interviewer’s original scores were not altered in this process.
RMICS coding was completed by two different cohorts of raters with 3 or 4 raters in each cohort. The first cohort underwent 16 hours of training led by the head RMICS coder from the developer’s (Dr. Heyman) research group. The training involved viewing example RMICS videos and discussing individual codes, practicing coding and discussing discrepancies, and ended in the completion of a practice test with few or no discrepancies relative to the trainer’s codes. Once trained and experienced, these coders later developed a set of scored discussions via consensus for use as future “gold standard” training recordings. Training for the second cohort of raters followed the same general approach as the first, but used the gold standards as tests to establish competency and reliability. All raters in the second cohort were required to score the gold standard videos within 15% of the proportion of total negative codes (defined below) relative to the gold standards before coding actual data.
A minimum of two trained raters independently coded each video-recorded conflict discussion. After coding each floor change (also defined below), the rater computed the proportion of negative codes (psychological abuse, distress-maintaining attributions, hostility, and withdrawal) relative to the total number of floor changes. If the proportion of negative codes differed between the two raters by more than 15%, a third rater then coded the discussion and the two closest ratings were used for data analysis.
Measures
Clinician Administered PTSD Scale (CAPS; Blake et al, 1995)
The CAPS is a 30-item structured interview that assesses the frequency and severity of the 17 DSM-IV PTSD symptoms and five associated features. Current and lifetime PTSD diagnostic status was determined according to the DSM-IV (APA, 1994) criteria using a validated scoring rule (i.e., at least one reexperiencing symptom, three avoidance and numbing symptoms, and two hyperarousal symptoms scored with a frequency of one or greater and an intensity of two or greater). Dimensional severity scores were calculated by summing the frequency and intensity ratings (each range from 0-4) for each of the 17 items (range 0-136). The CAPS has demonstrated excellent reliability and validity (Blake et al., 1995; Keane, Brief, Pratt, & Miller, 2007). All CAPS interviews in this study were video-recorded and 23% were randomly selected for review and re-coding by an independent rater for purposes of quality control and estimating diagnostic reliability. Kappa for a current diagnosis based on these secondary ratings was κ = .84 for current PTSD diagnosis and the intraclass correlation coefficient for severity scores was r = .99.
Desired Changes Questionnaire (DCQ; Heavey et al., 1993)
The DCQ was used to determine topics for the two conflict discussions and lists twenty behaviors relevant to intimate relationships. Participants rated the degree to which they wished their partners would change in each behavior domain using a 7-point Likert-type scale, ranging from no change (1) to much more change (7). Participants were also asked to write-in at least two additional desired changes; they then rank-ordered the three problems of greatest importance to them. The topics most commonly selected for discussion were from the write-in categories and generally fell into three broad categories of wishing that the partner would: (a) reduce the frequency of an undesired behavior, (b) increase the frequency of a desired behavior, or (c) take better care of his or herself.
Rapid Marital Interaction Coding System (RMICS: Heyman, 2004; Heyman & Vivian, 2000; Heyman et al., 2001; Heyman, Weiss, & Eddy, 1995)
Video recordings of the conflict discussions were coded using the Rapid Marital Interaction Coding System (RMICS; Heyman & Vivian, 2000; Heyman, 2004), an observational coding system adapted from the Marital Interaction Coding System (MICS) developed by Robert Weiss and colleagues at the University of Oregon in the late 1960s. The MICS was designed to provide a system for coding observed behavior, broadly defined, to include all observable actions (i.e., affective, motoric, paralinguistic, and linguistic) and it is the oldest and most widely used couples observation system. The RMICS was developed on the basis of a factor analysis of 1,088 couple interactions coded with the MICS over a 5 year period; it distilled the original 37 microbehavioral MICS codes down to 5 more general negative codes (psychological abuse, distress maintaining attribution, hostility, dysphoric affect and withdrawal), 3 positive codes (acceptance, relationship enhancing attribution, and self-disclosure), and 1 neutral code (constructive problem discussion/solution) for more reliable and valid use. The basic coding unit of the RMICS is the speaker turn. In RMICS terminology, the speaking individual “has the floor” until he/she completes a statement or the other speaker interrupts. The number of times this occurs during each 10 minute session is the total number of floor changes. If a speaker turn lasts longer than 30 seconds, it is broken down into 30-second intervals with each one given a code. Coders assign only one of the eleven codes to each speaker turn; if two or more codes are present, a theoretically derived hierarchy is applied to determine which code to use (i.e., with the more negative code assigned). Inter-rater agreement (intraclass correlations) for individual RMICS codes from this study is presented in Table 1.
Table 1.
Relationship Quality, Trauma and PTSD by Veteran Status and PTSD Diagnosis
| By Measure |
ANOVA |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| PTSD | No PTSD | Total Sample | Veteran Status | PTSD Status | ||||||
|
|
|
|||||||||
| Measure | M | SD | M | SD | M | SD | F | p | F | p |
| Relationship Measures | ||||||||||
| Desired Changes | 5.53 | .019 | 10.45 | .001 | ||||||
| Veteran | 3.17 | 1.33 | 2.80 | 1.21 | 2.94 | 1.27 | ||||
| Spouse | 3.53 | 1.33 | 3.06 | 1.25 | 3.12 | 1.27 | ||||
| Total sample | 3.27 | 1.33 | 2.95 | 1.24 | ||||||
| Typicality: Support | 0.50 | .48 | 0.11 | .74 | ||||||
| Veteran | 3.46 | 0.50 | 3.42 | 0.52 | 3.44 | 0.51 | ||||
| Spouse | 3.36 | 0.48 | 3.44 | 0.59 | 3.42 | 0.58 | ||||
| Total sample | 3.43 | 0.49 | 3.43 | 0.56 | ||||||
| Typicality: Undermining | 0.54 | .46 | 0.84 | .36 | ||||||
| Veteran | 2.84 | 0.55 | 2.80 | 0.59 | 2.82 | 0.57 | ||||
| Spouse | 2.81 | 0.54 | 2.73 | 0.52 | 2.74 | 0.53 | ||||
| Total sample | 2.83 | 0.55 | 2.76 | 0.55 | ||||||
| Quality of Marriage | 4.19 | .04 | 9.76 | .002 | ||||||
| Veteran | 30.80 | 7.96 | 34.04 | 7.33 | 32.73 | 7.91 | ||||
| Spouse | 29.48 | 8.42 | 31.75 | 7.82 | 31.38 | 7.95 | ||||
| Total sample | 30.45 | 8.07 | 32.72 | 7.69 | ||||||
|
Trauma & PTSD
Measures |
||||||||||
| Traumatic Life Events | 3.59 | .06 | 82.71 | <.001 | ||||||
| Veteran | 29.80 | 20.24 | 18.71 | 14.83 | 23.14 | 18.10 | ||||
| Spouse | 30.22 | 17.57 | 12.24 | 12.40 | 14.75 | 14.61 | ||||
| Total sample | 29.92 | 19.47 | 14.94 | 13.82 | ||||||
| CAPS PTSD Severity | 48.23 | <.001 | 696.91 | <.001 | ||||||
| Veteran | 70.10 | 16.97 | 27.86 | 21.35 | 43.91 | 28.51 | ||||
| Spouse | 62.63 | 19.15 | 10.51 | 12.81 | 18.09 | 23.05 | ||||
| Total sample | 68.02 | 17.86 | 20.31 | 18.93 | ||||||
Note. Veteran status X PTSD interactions were tested for all measures; only TLEQ [F (1,545 = 4.64, p = .032] and PTSD Severity [F (1,545 = 7.65, p = .006] were significant. PTSD = posttraumatic stress disorder; M = mean; SD = standard deviation; ANOVA = analysis of variance; CAPS = Clinician Administered PTSD Scale.
The RMICS has been shown to discriminate distressed versus nondistressed relationships in numerous samples and it shows convergent validity with the Dyadic Adjustment Scale (Spanier, 1976). It has also been found to predict improvement and drop-out in group treatment for partner-aggression (Heyman, 2004; Heyman, Brown, Feldbau, & O’Leary, 1999) and future marital declines including separation/divorce (Heyman, 2001). Previously published internal consistency values for the RMICS codes are above .90 and inter-rater agreement coefficients are above 0.70 (Heyman, 2004).
Traumatic Life Events Questionnaire (TLEQ; Kubany et al., 2000)
The TLEQ is a self-report measure that assesses exposure to 22 different traumatic events that meet the DSM-IV PTSD Criterion A1 definition for a traumatic event. A follow-up question assesses whether the event meets DSM-IV PTSD Criterion A2 by asking if the individual experienced intense fear, helplessness, or horror in response to the event. In addition, the frequency of occurrence of each event is assessed on a 7-point scale ranging from “never” to “more than five times.” The TLEQ has been shown to have good test-retest reliability over a two-week interval (mean kappa = .63, mean percent agreement = 86%), excellent content and convergent validity with interview-based measures of trauma exposure (mean percent agreement = 92%) and to be predictive of PTSD status (Kubany et al., 2000).
Typicality Questionnaire (Foster et al., 1997)
The Typicality Questionnaire was administered after each conflict discussion and used to assess participants’ perception of the representativeness of their partner’s behavior during the conflict discussions. Participants rated the typicality of their partner’s behavior on a 5-point scale ranging from 1 = much less than usual to 3 = about usual to 5 = much more than usual. Based on previous research (e.g., Foster et al., 1997; Owen, Heyman, & Smith Slep, 2006), two typicality subscales were scored: social support and social undermining. Cronbach’s alphas for the two subscales averaged across both discussions were .60 for social support (5 items) and .85 for social undermining (3 items).
Quality of Marriage Index (QMI; Norton, 1983)
The QMI is a six-item measure of global relationship satisfaction. High internal reliability has been reported in prior studies (α = .94 for men, α = .95 for women; Doss et al., 2011) along with evidence for convergent and discriminant validity (Heyman, Sayers, & Bellack, 1994). The QMI correlates highly (r = .85 for women, .87 for men) with the widely used 32-item Dyadic Adjustment Scale (Spanier, 1976), and has been found to be equivalent to that measure for many purposes (Heyman et al., 1994).
Statistical Analyses
Measurement Model
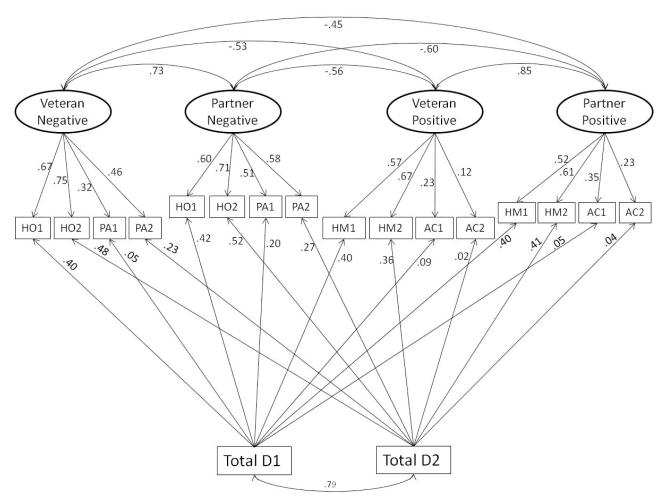
To test our hypothesis we set out to develop latent variables reflecting positive and negative discussion behavior. Analysis of the matrix of bivariate correlations among the RMICS codes suggested that it would be possible to develop a measurement model using hostility and psychological abuse as indicators of a latent Negative Conflict Behavior variable and humor and acceptance as indicators of a latent Positive Conflict Behavior variable for veteran and spouse2. Each latent variable was defined by four indicators (i.e., 2 codes from 2 discussions) with each indicator representing the mean score from the two RMICS raters for that code within that discussion. Because there was considerable inter-couple variation in the frequency of floor changes within each discussion, we included the total number of floor changes within each discussion as a covariate of each code (see Figure 1 for a diagram of this model). We specified correlated residuals for the same code across members of a couple within a given discussion and the four latent variables were allowed to correlate with one another. Due to the complexity of the model, we represented PTSD as a single latent variable (as opposed to modeling each symptom cluster separately) with four indicators corresponding to summary scores on the four symptom clusters (reexperiencing, avoidance, emotional numbing, and hyperarousal as defined in prior confirmatory factor analytic studies; e.g., King, Leskin, King, & Weathers, 1998).
Figure 1.
Note. The figure shows the measurement model for RMICS codes evaluated in this study. HO = hostility; PA = psychological abuse; HM = humor; AC = acceptance; D1 = total changes . floor for discussion 1; D2 = total floor changes for discussion 2. Not shown are correlated residuals of the same code within a discussion across members of the couple (these values are available from the first author).
Structural Models
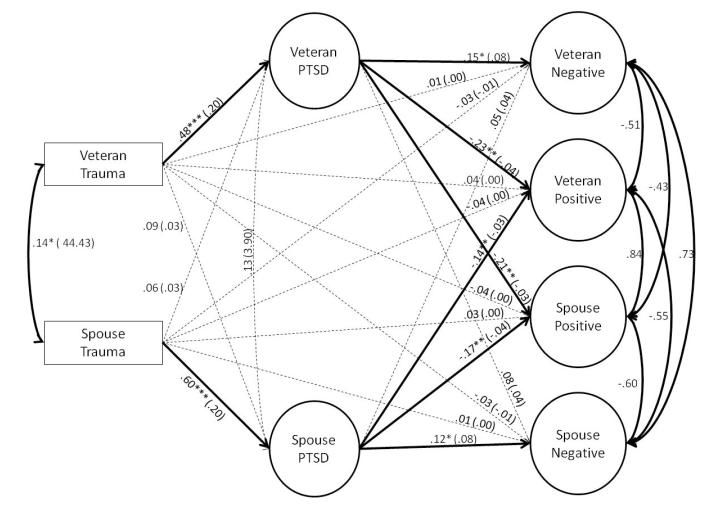
After determining that the measurement model provided adequate fit to the data we then proceeded to evaluate our structural hypotheses. We began by evaluating a structurally-saturated mediation model that included all possible direct and indirect effects of trauma exposure (indexed by the TLEQ total score) and PTSD on the RMICS variables (see Figure 2). In this and all subsequent models, the disturbances of veteran and spouse PTSD factors were allowed to freely covary with one another (as these variables were expected to be correlated even after controlling for the shared effects of trauma). Similarly, since the various RMICS factors are inter-related by definition, their disturbances were also all allowed to freely correlate with one another.
Figure 2.
Note. The figure shows the standardized (and unstandardized) parameter estimates of the structural elements of the final model, w hich included equal actor and partner effects across members of a couple. Parameter estimates that were statistically significant are shown in solid lines and parameter estimates that did not achieve statistical significance are shown in dotted lines. The disturbances among the latent discussion behavior variables were all correlated with one another at p < .001. The measurement model for the latent dependent variables is shown in Figure 1. *p < .05. **p < .01. ***p < .001.
We then evaluated competing hypotheses regarding the relative contribution of the veteran’s versus spouse’s PTSD symptoms on conflict behavior by comparing the fit of the structurally saturated model with 3 alternative, nested models. First, we tested the hypothesis that the veteran’s trauma history and PTSD symptoms are the primary sources of relationship disturbance by setting all of the regressive paths from the spouse’s trauma history and PTSD symptoms to the RMICS variables to zero. We then tested the opposite hypothesis (i.e., that the spouse’s trauma history and PTSD symptoms are the primary sources of disturbance in their relationships) by setting all paths from the veteran’s side of the equation to the RMICS variables to zero. Finally, we tested an “equal effects” model in which all complementary regressive paths for veterans and spouses were constrained to be equal (e.g., the path from the veteran’s PTSD symptoms to the veterans’ negative behavior was held equal to the path from the spouse’s PTSD symptoms to the spouse’s negative behavior, etc.).
Model Estimation and Evaluation
Structural equation modeling was performed in the Mplus statistical modeling software (version 5.2; Muthén & Muthén, 2008) using a robust maximum likelihood estimator (MLR) to account for the non-normal distributions of some variables. Cases with missing data were not eliminated but instead modeled under direct maximum likelihood estimation; no variable had more than 5% missing data. Models were evaluated using standard fit indices and cut-off scores recommended by Hu and Bentler (1999). Specifically, we examined: (a) the chi-square test of model fit (which should be small and non-significant, although in large applied datasets this is often difficult to achieve); (b) the root mean square error of approximation (RMSEA; values less than or equal to .06 are consistent with good model fit); (c) the standardized root mean squared residual (SRMR; values less than or equal to .08 are consistent with good model fit); (d) the comparative fit index (CFI; values of .90 and greater are consistent with adequate model fit with values of .95 or greater suggestive of good model fit); and (e) the Tucker-Lewis index (TLI; interpreted in the same fashion as the CFI). The relative fit of competing models was evaluated using the chi-square difference test (corrected for the use of the MLR estimator); nested models contain fewer free parameters (i.e., are more parsimonious) and if the reduction in free parameters does not result in degraded model fit, then the more parsimonious model is preferred. We also compared the Akaike (Akaike, 1987) and Bayesian (Schwartz, 1978) information criteria (AIC and BIC, respectively). With these statistics, the preferred model is the one with lower relative values. These population based fit indices favor model parsimony and fit. We were unable to evaluate bootstrapped standard errors for indirect effects because bootstrapping is not available when the MLR estimator is employed in Mplus 5.2.
Results
Descriptive Statistics by Veteran and PTSD Status
Table 1 lists mean scores on measures of relationship quality, trauma, and PTSD by veteran status and current PTSD diagnostic status. Analyses revealed that individuals with current PTSD reported a greater number of lifetime traumas on the TLEQ and lower levels of relationship satisfaction as indexed by their scores on the Quality of Marriage Inventory and Desired Changes Questionnaire. Veterans on average produced significantly higher PTSD severity scores on the CAPS than spouses and there was a non-significant trend (p = .06) toward a greater number of lifetime traumas among veterans compared to spouses. We also examined veteran status × PTSD diagnosis interactions for each variable and results yielded significant interactions only for TLEQ scores and PTSD severity. As shown in Table 1, both interactions were based on the finding that the difference between veterans and spouses in the no PTSD group was greater than the corresponding difference between veterans and spouses in the PTSD group. In addition, spouses on average endorsed significantly lower ratings of relationship satisfaction relative to the veterans. Finally, participants’ ratings of the typicality of partners’ behavior during the conflict discussions did not vary significantly as a function of veteran status or PTSD diagnosis.
Table 2 lists mean RMICS code proportions by veteran status and PTSD diagnosis and the intraclass correlation coefficient for each code, averaged across the two discussions and across both members of the couple. Analyses revealed that individuals with PTSD exhibited a significantly higher proportion of distress maintaining attributions, hostility, and dysphoric affect and a lower proportion of humor and constructive problem discussion codes compared to those without the diagnosis. In addition, spouses exhibited higher levels of hostility, distress maintaining attributions and fewer self-disclosure and constructive problem discussion codes on average than veterans.
Table 2.
RMICS Codes by Veteran Status and PTSD Diagnosis
| Inter-Rater Agreement |
Mean RMICS Code Proportions |
ANOVA |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| PTSD |
No PTSD |
Total Sample |
Veteran Status |
PTSD Status |
|||||||
| Code | ICC | M% | SD | M% | SD | M% | SD | F | p | F | p |
| Psychological Abuse | .58 | 0.45 | .51 | 3.54 | .06 | ||||||
| Veteran | 0.31 | 1.04 | 0.21 | 1.75 | 0.25 | 1.48 | |||||
| Spouse | 0.55 | 2.10 | 0.15 | 0.65 | 0.33 | 1.33 | |||||
| Total sample | 0.36 | 1.48 | 0.18 | 1.01 | |||||||
| Distress-Maintaining Attributions | .69 | 16.82 | <.001 | 4.96 | .03 | ||||||
| Veteran | 4.37 | 4.44 | 3.21 | 3.22 | 3.72 | 3.84 | |||||
| Spouse | 6.17 | 4.76 | 5.24 | 4.97 | 6.02 | 5.55 | |||||
| Total sample | 5.04 | 3.89 | 4.29 | 3.19 | |||||||
| Hostility | .91 | 10.25 | .001 | 5.72 | .02 | ||||||
| Veteran | 10.38 | 13.24 | 7.56 | 10.55 | 8.79 | 11.86 | |||||
| Spouse | 15.02 | 16.44 | 11.47 | 12.82 | 12.96 | 14.53 | |||||
| Total sample | 11.91 | 12.40 | 9.97 | 11.04 | |||||||
| Dysphoric Affect | .81 | 1.93 | .17 | 11.58 | .001 | ||||||
| Veteran | 4.31 | 6.32 | 2.58 | 5.88 | 3.33 | 6.13 | |||||
| Spouse | 5.63 | 6.38 | 3.03 | 5.85 | 4.23 | 6.50 | |||||
| Total sample | 4.13 | 4.61 | 3.03 | 4.29 | |||||||
| Withdrawal | .54 | 0.00 | .95 | 3.09 | .08 | ||||||
| Veteran | 1.01 | 2.09 | 0.59 | 1.37 | .77 | 1.73 | |||||
| Spouse | 0.93 | 2.60 | 0.64 | 1.91 | .83 | 2.38 | |||||
| Total sample | 1.64 | 1.72 | 1.28 | 1.38 | |||||||
| Relationship-Enhancing Attributions | .59 | 0.64 | .42 | 0.04 | .84 | ||||||
| Veteran | 5.25 | 4.43 | 5.42 | 4.55 | 5.34 | 4.49 | |||||
| Spouse | 4.95 | 4.23 | 4.97 | 4.28 | 4.92 | 4.39 | |||||
| Total sample | 5.19 | 3.72 | 5.06 | 3.28 | |||||||
| Acceptance | .70 | 0.86 | .35 | 0.001 | .98 | ||||||
| Veteran | 2.92 | 2.70 | 1.72 | 2.90 | 1.74 | 2.81 | |||||
| Spouse | 1.45 | 2.05 | 1.52 | 2.54 | 1.75 | 2.45 | |||||
| Total sample | 1.78 | 2.09 | 1.56 | 1.97 | |||||||
| Self-Disclosure | .64 | 8.83 | .003 | 0.28 | .60 | ||||||
| Veteran | 12.34 | 7.91 | 12.06 | 7.88 | 12.18 | 7.88 | |||||
| Spouse | 10.24 | 6.66 | 9.75 | 5.92 | 9.66 | 6.05 | |||||
| Total sample | 10.98 | 6.01 | 11.01 | 5.77 | |||||||
| Humor | .72 | 0.96 | .33 | 13.19 | <.001 | ||||||
| Veteran | 2.92 | 4.17 | 4.36 | 4.88 | 3.73 | 4.63 | |||||
| Spouse | 2.11 | 2.48 | 4.22 | 4.92 | 2.73 | 3.45 | |||||
| Total sample | 2.80 | 3.44 | 4.28 | 4.63 | |||||||
| Constructive Problem Discussion & Solution | .92 | 5.19 | .02 | 9.78 | .002 | ||||||
| Veteran | 55.68 | 14.07 | 59.64 | 13.68 | 57.91 | 13.96 | |||||
| Spouse | 51.48 | 17.05 | 56.96 | 14.26 | 54.94 | 15.52 | |||||
| Total sample | 55.27 | 12.24 | 57.65 | 12.07 | |||||||
| Other | .77 | 0.96 | .33 | 3.93 | .05 | ||||||
| Veteran | 1.66 | 2.97 | 2.66 | 4.42 | 2.22 | 3.88 | |||||
| Spouse | 1.49 | 2.61 | 2.05 | 3.75 | 1.63 | 3.03 | |||||
| Total sample | 1.64 | 3.00 | 2.35 | 4.02 | |||||||
Note. All veteran status X PTSD interactions were tested but none were significant. RMICS = Rapid Marital Interaction Coding System; PTSD = posttraumatic stress disorder; M = mean; SD = standard deviation; ANOVA = analysis of variance; ICC = intraclass correlation coefficient.
Measurement Models
The hypothesized RMICS factor structure using the acceptance, humor, hostility and psychological abuse codes (with number of floor changes per discussion as a covariate of each code) provided good fit to the data. The fit of this model is shown in Table 3 and the standardized loadings, factor correlations and covariate paths are shown in Figure 1. All fit indices fell within the range of acceptable model fit with the exception of the TLI value (.87) which fell just short of the recommended cut point of .90. Given the preponderance of evidence for adequate model fit and no hypothesis-based rationale for freeing additional parameters, we proceeded to further evaluate this model in our structural analyses. As shown in Figure 1, the observed variables evidenced mostly moderate to strong loadings on the latent variables and the total number of codes in a discussion was a significant covariate of all of the indicators except for the acceptance codes. The negative and positive RMICS variables were strongly and inversely related to each other and there were strong positive correlations between veteran and spouse factors of the same type.
Table 3.
Fit of Measurement and Structural Models
| Model | χ2 (df) | RMSEA (90% CI) |
SRMR | CFI | TLI | AIC | BIC | Model Comparison |
Δ χ2 (Δ df) p-value |
|---|---|---|---|---|---|---|---|---|---|
| Measurement | |||||||||
| RMICS | 226.94*** (106) |
.06 (.05 -.08) |
.06 | .91 | .87 | ||||
| PTSD | 33.76* (19) |
.05 (.02 -.08) |
.03 | .98 | .98 | ||||
| Structural/Mediation | |||||||||
| 1. Structural Saturated | 581.24*** (301) |
.06 (.05-.06) |
.06 | .91 | .88 | 36529 | 37016 | ||
| 2. Veteran Only Effects | 592.59*** (310) |
.06 (.05 -.06) |
.06 | .91 | .89 | 36525 | 36979 | 1 vs. 2 | 5.87 (9) p = .75 |
| 3. Partner Only Effects | 599.65*** (310) |
.06 (.05 -.06) |
.07 | .90 | .88 | 36528 | 36981 | 1 vs. 3 | 18.48 (9) p = .03 |
| 4. Equal Effects | 585.38*** (311) |
.06 (.05 -.06) |
.06 | .91 | .89 | 36517 | 36968 | 1 vs. 4 | 6.96 (10) p = .73 |
| 5. Model 4 with Covariates | 851.40*** (445) |
.06 (.05 - .06) |
.07 | .88 | .86 | 41400 | 41948 | ||
| 6. Model 4 in Male/Female Couples | 575.34*** (311) |
.06 (.05 - .07) |
.06 | .90 | .89 | 33002 | 33439 |
Note. AIC= Akaike information criterion; BIC=Bayesian information criterion; df = degrees of freedom; RMSEA = root mean square error of approximation; SRMR = standardized root mean squared residual; CFI = comparative fit index; TLI = Tucker-Lewis index; RMICS = Rapid Marital Interaction Coding System; PTSD = posttraumatic stress disorder; vs = versus.
p < .001.
We next tested a measurement model for PTSD in which CAPS summary scores for the reexperiencing, avoidance, emotional numbing, and hyperarousal symptoms were used as indicators (parcels) of a one-factor latent PTSD variable for each partner. The model provided good fit to the data (see Table 3). The four veteran indicators loaded on the veteran PTSD factor between .76-.82 (all p < .001) and the four partner indicators loaded on the partner PTSD factor between .76-.85 (all p < .001). The veteran and partner PTSD factors correlated with one another in this model at r = .20 (p = .012).
Structural Equation Models
Saturated model
The first SEM estimated all possible direct and indirect effects of trauma history and PTSD on the RMICS variables. Fit statistics for this and all subsequent models are listed in Table 3. Results showed veteran trauma to be significant predictor of Veteran PTSD (β = .44, p < .001), and likewise, spouse trauma was significant predictor of Spouse PTSD (β = .62, p < .001). Veteran PTSD was, in turn, negatively associated with both Veteran and Spouse Positive Behavior (β = −. 19, p = .032 and β = −.21, p = .021, respectively) and Spouse PTSD was negatively associated with Spouse Positive Behavior (β = −.25, p = .017). In addition to these direct effects, three significant indirect (i.e., mediated) effects were found: veteran trauma was associated with Veteran and Spouse Positive Behavior via Veteran PTSD (indirect effects = −.08 and −.09, ps = .041 and .030, respectively). Similarly, there was also a significant indirect effect of Spouse Trauma on Spouse Positive Behavior via Spouse PTSD (indirect effect = −.15; p = .020).
Veteran-effects only model
We next evaluated the fit of a nested model that examined the hypothesis that the veteran’s trauma history and PTSD symptoms were the primary sources of observed conflict behavior (by setting all paths from spouse trauma and spouse PTSD to zero). The chi-square difference test suggested that these constraints did not significantly damage fit relative to the structurally saturated parent model and the AIC and BIC values improved relative to the saturated model.
Spouse-effects only model
We then tested the opposite model in which all veteran effects were eliminated by setting them to 0 and spouse effects were freely estimated. Doing so significantly degraded model fit relative to the saturated model so this model was rejected.
Equal effects model
We then tested the equal effects model in which corresponding actor and partner effects were held equivalent across members of the couple. This model, which is more parsimonious than any of the preceding models because it estimates 10 fewer paths than the saturated model and 1 less path than the veteran- and partner-effects only models, provided good fit to the data. The nested chi-square test suggested that this model did not damage fit relative to the structurally saturated model and the AIC and BIC values were both substantially lower than previous models. The model contained six significant indirect effects (i.e., three sets of equivalent effects across members of the couple) 3: (a) veteran trauma to Veteran Negative Behavior via Veteran PTSD = .07, p = .019; (b) spouse trauma to Spouse Negative Behavior via Spouse PTSD = .07, p = .018; (c) veteran trauma to Veteran Positive Behavior via Veteran PTSD = −.11, p = .001; (d) spouse trauma to Spouse Positive Behavior via Spouse PTSD = −.10, p = .002; (e) veteran trauma to Spouse Positive Behavior via Veteran PTSD = −.10, p = .009; and (f) spouse trauma to Veteran Positive Behavior via Spouse PTSD = −.08, p = .007. In total, this model explained 24% and 38% in Veteran and Spouse PTSD, respectively, 3% and 2% in Veteran and Spouse Negative Behavior, respectively, and 8% and 9% in Veteran and Partner Positive Behavior, respectively.
Demographic Covariates
We then evaluated the extent to which participant sex, age, and length of relationship influenced these associations by adding these variables as covariates of the four latent RMICS variables in the final (equal effects) model. In this analysis, veteran and spouse age were allowed to covary with one another and with length of relationship. This model yielded acceptable fit though was not directly comparable with prior models due to the addition of new variables. There was only one instance in which one of these covariates yielded a significant relationship with an RMICS variable: spouse sex was inversely associated with Spouse Negative Behavior (β = −.07, p = .02), suggesting that female spouses produced slightly lower scores on this factor relative to male spouses. Given this, we re-evaluated the equal effects model in a restricted sample in which the veteran was always male and the spouse was always female (n = 258 couples). This model provided virtually identical fit to the equal effects model that was run in the full sample and all significant paths depicted in Figure 2 were retained. The magnitude of the indirect effects were within .05 of those reported for the full sample (details available from the first author), suggesting that the model depicted in Figure 2 fit the data equally well for male/female couples.
Depression Model
Finally, we wondered whether the effects that we found were specific to PTSD or whether they would also be in relation to other forms of psychopathology. Though a comprehensive examination of multiple disorders was beyond the scope of this study, we addressed this question by running an additional analysis in which we substituted PTSD with depression in the final model (i.e., the equal effects model depicted in Figure 2). We focused on depression symptom severity because it was the second most common disorder in this sample (after PTSD), and was diagnosed in 23% of the veterans and 12% of the spouses. The latent depression variable was indicated by three parcels of items from the SCID depression module reflecting depressed mood and behavior (depressed mood, diminished interest, and suicidal ideation), somatic and vegetative problems (weight loss/gain, insomnia, psychomotor agitation/retardation, and fatigue) and cognitive distortions and problems (worthlessness/inappropriate guilt, and diminished ability to think or concentrate). The model provided acceptable fit to the data (Χ2 = 466.68, df = 260, p < .001, RMSEA = .05, SRMR = .06, CFI = .92, TLI = .91) and several aspects of the model did, in fact, differ from the PTSD model. Specifically, there were no significant partner effects of depression (i.e., no effects of one partner’s depressive symptoms on the other’s behavior) only actor effects were found (i.e., effects of depression on one’s own behavior). Indirect effects were evident for the path from Veteran Trauma history to Veteran Negative RMICS behavior via Veteran Depression (standardized β = .07, p = .004) and the strength of that path was equivalent to the corresponding one for Spouse Trauma history to Spouse Negative RMICS behavior via Spouse Depression (standardized β = .07, p = .008). There were significant actor effects of Veteran Trauma history to Veteran Positive RMICS behavior via Veteran Depression (standardized β= −.08, p = .001) and Spouse Trauma history to Spouse Positive RMICS behavior via Spouse Depression (standardized β = −.07, p = .001) and these effects were equivalent in magnitude to each other. In total, the model explained 15% and 19% of the variance in Veteran and Spouse Depression, respectively, 5% of the variance in both Veteran and Spouse Negative RMICS behavior, and 7% and 6% of the variance in Veteran and Spouse Positive RMICS behavior, respectively.
Discussion
This study examined the influence of trauma history and PTSD symptoms on interactions between intimate partners and, to our knowledge, was the first to examine these associations using behavioral coding of couples’ observed behavior. The sample comprised U.S. military veterans with a high prevalence of PTSD and their spouses or cohabitating partners. Couples participated in video-recorded conflict discussions that they later rated as typical of their interactions at home. The recordings were then coded using the RMICS and comparison of group means showed that individuals with PTSD exhibited less humor, were more hostile and dysphoric, and verbalized more distress-maintaining attributions than those without the disorder. This implies that individuals with PTSD exhibited more unconstructive criticisms, unelaborated disagreements, and verbal and nonverbal expressions of externalized negative affect (hostility). They voiced more self-complaints, self-deprecation, exhibited more depressive behaviors (dysphoria) and their explanations for relationship events served to maintain or exacerbate, rather than mitigate, conflict with their partners. Individuals with PTSD showed a reduced capacity to make use of, or respond to, humor in their exchanges with their spouses and a smaller proportion of their behaviors were coded as reflecting constructive problem solving. These findings offer new insights into, and behavioral evidence for, the social and emotional deficits of individuals with PTSD and they contribute to a growing literature on PTSD and couples functioning which, to date, has been based exclusively on studies using self-report measures of relationship disturbance.
Analyses that compared the behavior of veterans (who were predominantly male) to spouses (who were predominantly female) revealed that, on average, spouses voiced more distress-maintaining attributions and expressed more hostility during conflict discussions than veterans. Spouses were also less likely to make statements that offered insight into their feelings, wishes, or beliefs (i.e., less self-disclosure)—a finding that runs contrary to anecdotal observations about the reticence of male veterans. Spouses also reported lower ratings of relationship quality and higher levels of desired change for their relationships relative to the veterans. Given our hypotheses about the central role of PTSD in veterans’ relationship disturbance, and the fact that PTSD prevalence was less common in spouses (14%) than in veterans (43%), these findings were unexpected. However, a review of the literature revealed that they were not entirely unprecedented since several prior studies have found partners of veterans with PTSD to report poorer psychological adjustment, more caregiver burden, and lower relationship satisfaction than spouses of veterans without PTSD (e.g., Beckham, Lytle & Feldman, 1996; Manguno-Mire et al., 2007). We suspect that our findings reflect the long-term adverse effects of PTSD on relationship functioning. Though our cross-sectional data do not speak to this longitudinal interpretation directly, it is clear from our results that PTSD is associated with negative patterns of behavioral interaction between intimate partners and it is reasonable to suspect that, over time, these behaviors would take a toll on relationship quality.
The primary aim of this study was to model hypothesized multivariate associations between trauma history, PTSD, and couples’ positive and negative emotional behavior during interactions. To do so, we developed latent positive and negative behavior variables based on select RMICS codes. Positive behavior was defined by the RMICS humor and acceptance codes; the latter referring to expressions of empathy, understanding, or appreciation towards the partner. Negative behavior was defined by hostility and psychological abuse. The latter is the most negative code in the RMICS code hierarchy and is applied to destructive communications intended to hurt the partner’s feelings. Together, these codes defined a latent variable reflecting antagonistic, relationship-damaging, and distressed behaviors and communications. Analyses showed the positive and negative RMICS factors to be moderately negatively correlated, with the same factors were highly correlated between spouses (e.g., spouse negative with veteran negative) indicating a high degree of symmetry or mirroring of partner’s expressions. Though empathy and emotional reflection is a fundamental aspect of intimacy, prior research has shown negative affect reciprocity to contribute to conflict escalation and relationship failure and therefore is an important target for interventions (Gottman, 1998).
Dyadic SEMs using the APIM framework revealed that PTSD was associated with significant actor (i.e., within subject) and partner (i.e., between subject) effects on discussion behavior. Specifically, results showed that PTSD predicted not only more negative and fewer positive behaviors on the part of the individual (i.e., an actor effect) but also significantly lower levels of positive behavior on the part of the spouse (i.e., a partner effect). These findings underscore the role of deficits of positive emotionality in PTSD and its negative effects on intimate partner communication and they replicate and extend, to a new patient population, results of prior studies underscoring deficits in the exchange of positive affect in couples with psychiatrically distressed partners (Jacob, & Krahn, 1988; Johnson & Jacob, 1997; Linden, Hautzinger, & Hoffman, 1983; Ruscher & Gotlib, 1988). Given the key role that positive affect, humor, and acceptance plays in sustaining intimate relationships (e.g., Campbell et al., 2008; Gottman et al., 1998; Gottman & Notarius, 2000) these findings highlight the importance of understanding the mechanisms underlying these deficits and enhancing our methods for treating them.
Results of this study are consistent with research on the “stress-generative” effects of psychopathology (i.e., that individuals influence their surroundings in ways that may contribute to conflict and adversity). For example, prior studies have shown that individuals with depression tend to invite criticism or engage in other behaviors that precipitate interpersonal conflict in ways that reflect processes inherent to the disorder (Biglan et al., 1985; Hammen, 1991; Wamboldt & Wamboldt, 2000) and that symptoms of depression prospectively predict higher levels of negative interpersonal life stressors (Harkness & Stewart, 2009). Similarly twin studies suggest that individuals with histories of major depression tend to select themselves into difficult enviroments such as conflicted relationships (e.g., Kendler, Karkowski, & Prescott, 1999). Thus, findings of this study are in accord with a growing body of research which suggests that individuals with psychopathology tend to interact with significant others in ways that serve to promote, rather than alleviate, their distress.
On a related note, when we ran an analysis that substituted depression for PTSD, we found no direct effect of depressive severity on the partner’s overt behavior. That is, while PTSD was associated with fewer positive expressions on the part of the individual, and fewer reciprocal expressions of humor and acceptance by the spouse, depression significantly affected only the individuals own behavior. Though these differential patterns may be unique to our PTSD-enriched sample and any conclusions that may be drawn from them should be considered tentative pending replication, they suggest that PTSD exerted a more profound effect on partner’s interactions. Though novel, this may not be altogether surprising given the larger number and wider scope of symptoms (including ones that specifically reference impairment in interpersonal functioning) subsumed under the PTSD diagnosis.
Finally, analyses also evaluate alternative hypotheses for associations between trauma history, current PTSD, and positive and negative discussion behaviors. On the basis of prior research (e.g., Taft, Schumm, Panuzio et al., 2008), we predicted that the influence of trauma history on behavior during conflict discussions would be mediated by PTSD. Results supported this hypothesis thereby supporting the rationale behind treatments that target PTSD as a method for reducing conflict between veterans and their spouses (e.g., Monson, Fredman, & Adair, 2008) as well PTSD treatments interventions that incorporate social skills training and/or anger management components (e.g., Beidel, Frueh, Uhde, Wong, Mentrikoski, 2011). Furthermore, the finding that the strengths of association between PTSD and discussion behavior were equivalent for veterans and spouses emphasizes the importance of addressing the trauma history and psychopathology of both members of a couple. Results suggest that in distressed veteran couples, targeting the veteran’s trauma history and PTSD symptoms solely may be insufficient since it fails to recognize the partner’s significant contribution to relationship distress. Thus, assessment and treatment of the trauma history and PTSD symptoms of both members of the couple may be warranted (see Galovski & Lyons, 2004; Monson et al., 2008).
Study conclusions should be considered in light of its limitations. First, our structural equation models were based on two directional assumptions, (a) trauma severity is causally linked to PTSD severity, and (b) PTSD is an individual difference characteristic that exerts a causal influence on behavior. Though both assumptions are logical and based on published precedent, reciprocal relationships between these variables that were not modeled in this study may also exist. For example, it is conceivable that reports of past trauma exposure were biased by factors that were confounded with PTSD symptomatology (c.f., Koenen, Stellman, Dohrenwend, Sommer & Stellman, 2007). It is also possible that relationship conflict is part of a vicious cycle that serves to exacerbate or maintain PTSD symptoms and contributes to making the disorder self-sustaining and self-propagating (Pettit & Joiner, 2005; Weiss & Heyman, 2004). Indeed, prior studies have shown relationship distress to be a significant predictor of the development and/or exacerbation of psychopathology in vulnerable individuals (South & Krueger, 2008). Additional longitudinal research is needed to evaluate these alternative conceptualizations of these phenomena. A second limitation was that the RMICS analyses were based on the proportion of floor changes within a discussion that received a given code; thus, we were only able to incorporate four of the codes into our measurement model, and we have yet to undertake any sequential analyses that might further clarify the nature of moment-to-moment exchanges between partners. That said, a noteworthy strength of our approach was the use of two raters for all codes, a novel approach to modeling latent dimensions of positive and negative observed behavior, and a sophisticated method for statistically controlling for inter-couple differences in the number of speaker turns per discussion.
To conclude, results of this study clarify the nature of the social and emotional impairments associated with PTSD, underscore the mutual contribution of both partners’ trauma history and PTSD to relationship conflict, and show how the study of couples behavior provides a unique context in which to examine the consequences of trauma and PTSD on behavior.
Acknowledgments
Funding for this study was provided by National Institute on Mental Health award RO1 MH079806 to Mark W. Miller. Erika J. Wolf is supported by a VA Career Development Award.
Footnotes
Eighty percent of couples were married. Though the term “spouse” traditionally refers to married partners, we use the term “spouse” throughout this paper to refer the non-veteran member of the couple to avoid confusion when discussing the APIM models which distinguish between “actor effects” and “partner effects”.
We also evaluated whether other RMICS codes could be included as indicators of these variables, but no other codes loaded on them without damaging model fit.
Constraining corresponding paths sets the unstandardized parameter estimates to be perfectly equal to one another. Standardized estimates differed slightly due to differences in the standard deviation of the measures across members of the couple, but for all intents and purposes, the standardized parameter estimates for corresponding paths are also equivalent.
Contributor Information
Mark W. Miller, National Center for PTSD at VA Boston Healthcare System & Department of Psychiatry, Boston University School of Medicine
Erika J. Wolf, National Center for PTSD at VA Boston Healthcare System & Department of Psychiatry, Boston University School of Medicine
Annemarie F. Reardon, National Center for PTSD at VA Boston Healthcare System
Kelly M. Harrington, National Center for PTSD at VA Boston Healthcare System & Department of Psychiatry, Boston University School of Medicine
Karen Ryabchenko, National Center for PTSD at VA Boston Healthcare System & Department of Psychiatry, Boston University School of Medicine.
Diane Castillo, New Mexico VA Healthcare System.
Rachel Freund, New Mexico VA Healthcare System.
Richard Heyman, New York University.
References
- Akaike H. Factor analysis and AIC. Psychometrika. 1987;52:317–332. doi: 10.1007/BF02294359. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed Author; Washington DC: 1994. [Google Scholar]
- Beckham JC, Lytle BL, Feldman ME. Caregiver burden in partners of Vietnam War veterans with posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 1996;64:1068–1072. doi: 10.1037//0022-006x.64.5.1068. doi:10.1037/0022-006X.64.5.1068. [DOI] [PubMed] [Google Scholar]
- Beidel DC, Frueh BC, Uhde TW, Wong N, Mentrikoski J. Multicomponent behavioral treatment for chronic combat-related posttraumatic stress disorder: A randomized controlled trial. Journal of Anxiety Disorders. 2011;25:224–231. doi: 10.1016/j.janxdis.2010.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biglan A, Hops H, Sherman L, Friedman LS, Arthur J, Osteen V. Problem-solving interactions of depressed women and their husbands. Behavior Therapy. 1985;16:4–451. doi:10.1016/S0005-7894(85)80023-X. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. doi:10.1002/jts.2490080106. [DOI] [PubMed] [Google Scholar]
- Byrne CA, Riggs DS. The cycle of trauma: Relationship aggression in male Vietnam veterans with symptoms of posttraumatic stress disorder. Violence and Victims. 1996;11:213–225. [PubMed] [Google Scholar]
- Campbell L, Martin RA, Ward JR. An observational study of humor use while resolving conflict in dating couples. Personal Relationships. 2008;15:41–55. doi: 10.1111/j.1475-6811.2007.00183.x. [Google Scholar]
- Carroll EM, Rueger DB, Foy DW, Donahoe CP. Vietnam combat veterans with posttraumatic stress disorder: Analysis of marital and cohabitating adjustment. Journal of Abnormal Psychology. 1985;94:329–337. doi: 10.1037//0021-843x.94.3.329. doi:10.1037/0021-843X.94.3.329. [DOI] [PubMed] [Google Scholar]
- Cook JM, Riggs DS, Thompson R, Coyne JC, Sheikh JI. Posttraumatic stress disorder and current relationship functioning among World War II ex-prisoners of war. Journal of Family Psychology. 2004;18:36–45. doi: 10.1037/0893-3200.18.1.36. doi:10.1037/0893-3200.18.1.36. [DOI] [PubMed] [Google Scholar]
- Cook WL, Kenny DA. The Actor-Partner Interdependence Model: A model of bidirectional effects in developmental studies. International Journal of Behavioral Development. 2005;29:101–109. doi:10.1080/01650250444000405. [Google Scholar]
- Davis JL, Petretic-Jackson PA, Ting L. Intimacy dysfunction and trauma symptomatology: Long-term correlates of different types of child abuse. Journal of Traumatic Stress. 2001;14:63–79. doi:10.1023/A:1007835531614. [Google Scholar]
- Dekel R, Monson CM. Military-related post-traumatic stress disorder and family relations: Current knowledge and future directions. Aggression and Violent Behavior. 2010;15:303–309. doi:10.1016/j.avb.2010.03.001. [Google Scholar]
- Depue RA, Morrone-Strupinsky JV. A neurobehavioral model of affiliative bonding: Implications for conceptualizing a human trait of affiliation. Behavioral and Brain Sciences. 2005;28:313–395. doi: 10.1017/S0140525X05000063. doi:10.1017/S0140525X05000063. [DOI] [PubMed] [Google Scholar]
- Doss BD, Simpson Rowe L, Morrison KR, Libet J, Birchler GR, Madsen JW, McQuaid JR. Couple therapy for military veterans: Overall effectiveness and predictors of response. Behavior Therapy. 2012;43:216–227. doi: 10.1016/j.beth.2011.06.006. doi:10.1016/j.beth.2011.06.006. [DOI] [PubMed] [Google Scholar]
- Foster DA, Caplan RD, Howe GW. Representativeness of observed couple interaction: Couples can tell, and it does make a difference. Psychological Assessment. 1997;9:285–294. doi: 10.1037/1040-3590.9.3.285. [Google Scholar]
- Frewen PA, Dozois DJA, Lanius RA. Assessment of anhedonia in psychological trauma: psychometric and neuroimaging perspectives. European Journal of Psychotraumatology. 2012;3:8587. doi: 10.3402/ejpt.v3i0.8587. doi: 10.3402/ejpt.v3i0.8587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galovski TE, Lyons J. The psychological sequelae of exposure to combat violence: A review of the impact on the veteran’s family. Aggression and Violent Behavior: A Review Journal. 2004;9:477–501. doi:10.1016/S1359-1789(03)00045-4. [Google Scholar]
- Gottman JM. Marital interaction: Experimental investigations. Academic Press; New York: 1979. [Google Scholar]
- Gottman JM. Psychology and the study of marital processes. Annual Review of Psychology. 1998;49:169–197. doi: 10.1146/annurev.psych.49.1.169. doi:10.1146/annurev.psych.49.1.169. [DOI] [PubMed] [Google Scholar]
- Gottman JM, Coan J, Carrére S, Swanson C. Predicting marital happiness and stability from newlywed interactions. Journal of Marriage and Family. 1998;60:5–22. doi: 10.1037/1040-3590.15.3.392. [Google Scholar]
- Gottman JM, Krokoff LJ. Marital interaction and satisfaction: A longitudinal view. Journal of Consulting and Clinical Psychology. 1989;57:47–52. doi: 10.1037//0022-006x.57.1.47. doi: 10.1037/0022-006X.57.1.47. [DOI] [PubMed] [Google Scholar]
- Gottman JM, Levenson RW. Assessing the role of emotion in marriage. Behavioral Assessment. 1986;8:31–48. [Google Scholar]
- Gottman JM, Levenson RW. Marital processes predictive of later dissolution: Behavior, physiology, and health. Journal of Personality and Social Psychology. 1992;63:221–233. doi: 10.1037//0022-3514.63.2.221. doi:10.1037/0022-3514.63.2.221. [DOI] [PubMed] [Google Scholar]
- Gottman JM, Notarius CI. Decade Review: Observing Marital Interaction. Journal of Marriage and Family. 2000;62:927–947. doi:10.1111/j.1741-3737.2000.00927.x. [Google Scholar]
- Hammen C. Generation of stress in the course of unipolar depression. Journal of Abnormal Psychology. 1991;100:555–561. doi: 10.1037//0021-843x.100.4.555. doi:10.1037/0021-843X.100.4.555. [DOI] [PubMed] [Google Scholar]
- Harkness KL, Stewart JG. Symptom specificity and the prospective generation of life events in adolescence. Journal of Abnormal Psychology. 2009;118:278–287. doi: 10.1037/a0015749. doi:10.1037/a0015749. [DOI] [PubMed] [Google Scholar]
- Heavey CL, Layne C, Christensen A. Gender and conflict structure in marital interaction: A replication and extension. Journal of Consulting and Clinical Psychology. 1993;61:16–27. doi: 10.1037//0022-006x.61.1.16. doi:10.1037/0022-006X.61.1.16. [DOI] [PubMed] [Google Scholar]
- Heyman RE. Observation of couple conflicts: Clinical assessment applications, stubborn truths, and shaky foundations. Psychological Assessment. 2001;13:5–35. doi: 10.1037//1040-3590.13.1.5. doi:10.1037/1040-3590.13.1.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heyman RE. Rapid Marital Interaction Coding System. In: Kerig PK, Baucom DH, editors. Couple observational coding systems. Lawrence Erlbaum Associates; Mahwah, NJ: 2004. [Google Scholar]
- Heyman RE, Brown PD, Feldbau SR, O’Leary KD. Couples’ communication variables as predictors of dropout and treatment response in wife abuse treatment programs. Behavior Therapy. 1999;30:165–190. doi:10.1016/S0005-7894(99)80002-1. [Google Scholar]
- Heyman RE, Feldbau-Kohn SR, Ehrensaft MK, Langhinrichsen-Rohling J, O’Leary K. Can questionnaire reports correctly classify relationship distress and partner physical abuse? Journal of Family Psychology. 2001;15:334–346. doi: 10.1037//0893-3200.15.2.334. doi:10.1037/0893-3200.15.2.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heyman RE, Sayers SL, Bellack AS. Global marital satisfaction versus marital adjustment: An empirical comparison of three measures. Journal of Family Psychology. 1994;8:432–446. doi: 10.1037/0893-3200.8.4.432. [Google Scholar]
- Heyman RE, Vivian D. Training Manual for Coders. Version 1.7. University Marital Clinic, State University of New York; Stony Brook, NY: 2000. RMICS: Rapid Marital Interaction Coding System. [Google Scholar]
- Heyman RE, Weiss RL, Eddy JM. Marital Interaction Coding System: Revision and empirical evaluation. Behaviour Research and Therapy. 1995;33:737–746. doi: 10.1016/0005-7967(95)00003-g. doi: http://dx.doi.org/10.1016/0005-7967(95)00003-G. [DOI] [PubMed] [Google Scholar]
- Hooper D, Roberts JR, Hinchcliffe MK, Vaughan PW. The melancholy marriage: An inquiry into the interaction of depression. British Journal of Psychiatry. 1977;50:113–124. doi: 10.1111/j.2044-8341.1977.tb02405.x. doi: 10.1111/j.2044-8341.1978.tb02441.x. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. doi:10.1080/10705519909540118. [Google Scholar]
- Iacoboni M. Imitation, empathy, and mirror neurons. Annual Review of Psychology. 2009;60:653–670. doi: 10.1146/annurev.psych.60.110707.163604. doi:10.1146/annurev.psych.60.110707.163604. [DOI] [PubMed] [Google Scholar]
- Jacob T, Krahn G. Marital interaction of alcoholic couples: Comparison with depressed and nondistressed couples. Journal of Consulting and Clinical Psychology. 1988;56:73–79. doi: 10.1037//0022-006x.56.1.73. doi:10.1037/0022-006X.56.1.73. [DOI] [PubMed] [Google Scholar]
- Johnson SL, Jacob T. Marital interactions of depressed men and women. Journal of Consulting and Clinical Psychology. 1997;65:15–23. doi: 10.1037//0022-006x.65.1.15. doi: 10.1037/0022-006X.65.1.15. [DOI] [PubMed] [Google Scholar]
- Jordan KB, Marmar CR, Fairbank JA, Schlenger WE, Kulka RA, Hough RL, Weiss DS. Problems in families of male Vietnam veterans with posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 1992;60:916–926. doi: 10.1037//0022-006x.60.6.916. doi:10.1037/0022-006X.60.6.916. [DOI] [PubMed] [Google Scholar]
- Kashdan TB, Elhai JD, Frueh BC. Anhedonia and emotional numbing in combat veterans with PTSD. Behaviour Research & Therapy. 2006;44:457–467. doi: 10.1016/j.brat.2005.03.001. doi:10.1016/j.brat.2005.03.001. [DOI] [PubMed] [Google Scholar]
- Keane TM, Brief D, Pratt L, Miller MW. Assessment of PTSD and its comorbidities in adults. In: Friedman MJ, Keane TM, Resick PA, editors. Handbook of PTSD: Science and Practice. Guilford Press; New York: 2007. [Google Scholar]
- Kendler KS, Karkowski LM, Prescott CA. Causal relationship between stressful life events and the onset of major depression. American Journal of Psychiatry. 1999;156:837–848. doi: 10.1176/ajp.156.6.837. [DOI] [PubMed] [Google Scholar]
- King DW, Leskin GA, King LA, Weathers FW. Confirmatory factor analysis of the clinician-administered PTSD Scale: Evidence for the dimensionality of posttraumatic stress disorder. Psychological Assessment. 1998;10:90–96. doi:10.1037/1040-3590.10.2.90. [Google Scholar]
- Koenen K, Stellman S, Dohrenwend B, Sommer J, Stellman J. The consistency of combat exposure reporting and course of PTSD in Vietnam veterans. Journal of Traumatic Stress. 2007;20:3–13. doi: 10.1002/jts.20191. doi:10.1002/jts.20191. [DOI] [PubMed] [Google Scholar]
- Kubany ES, Haynes SN, Leisen MB, Owens JA, Kaplan AS, Watson SB, Burns K. Development and preliminary validation of a brief-broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psychological Assessment. 2000;12:411–424. doi: 10.1037//1040-3590.12.2.210. doi:10.1037/1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- Linden M, Hautzinger M, Hoffman N. Discriminant analysis of depressive interactions. Behavior Modification. 1983;7:403–422. doi: 10.1177/01454455830073007. doi:10.1177/01454455830073007. [DOI] [PubMed] [Google Scholar]
- Manguno-Mire G, Sautter F, Lyons J, Myers L, Perry D, Sherman M, Sullivan G. Psychological distress and burden among female partners of combat veterans with PTSD. Journal of Nervous and Mental Disease. 2007;195:144–151. doi: 10.1097/01.nmd.0000254755.53549.69. doi:10.1097/01.nmd.0000254755.53549.69. [DOI] [PubMed] [Google Scholar]
- Margolin G, John RS, Gleberman L. Affective responses to conflictual discussions in violent and nonviolent couples. Journal of Consulting and Clinical Psychology. 1988;56:24–33. doi: 10.1037//0022-006x.56.1.24. doi: 10.1037/0022-006X.56.1.24. [DOI] [PubMed] [Google Scholar]
- Miller MW, Greif JL, Smith AA. Multidimensional Personality Questionnaire profiles of veterans with traumatic combat exposure: Internalizing and externalizing subtypes. Psychological Assessment. 2003;15:205–215. doi: 10.1037/1040-3590.15.2.205. doi:10.1037/1040-3590.15.2.205. [DOI] [PubMed] [Google Scholar]
- Miles D. Reducing the military divorce rate. American Forces Press Service; Jun 13, 2005. [Google Scholar]
- Monson CM, Fredman SJ, Adair KC. Cognitive-behavioral conjoint therapy for posttraumatic stress disorder: application to Operation Enduring and Iraqi Freedom veterans. Journal of Clinical Psychology. 2008;64:958–971. doi: 10.1002/jclp.20511. doi:10.1002/jclp.20511. [DOI] [PubMed] [Google Scholar]
- Monson CM, Taft CT, Fredman SJ. Military-related PTSD and intimate relationships: From description to theory-driven research and intervention development. Clinical Psychology Review. 2009;29:707–714. doi: 10.1016/j.cpr.2009.09.002. doi:10.1016/j.cpr.2009.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. Fifth Edition Muthén & Muthén; Los Angeles, CA: 1998-2008. [Google Scholar]
- Norton E. Measuring marital quality: A critical look at the dependent variable. Journal of Marriage and Family. 1983;45:141–151. doi:10.2307/351302. [Google Scholar]
- Orcutt HK, King LA, King DW. Male-perpetrated violence among Vietnam veteran couples: Relationships with veterans’ early life characteristics, trauma history, and PTSD symptomatology. Journal of Traumatic Stress. 2003;16:381–390. doi: 10.1023/A:1024470103325. doi:10.1023/A:1024470103325. [DOI] [PubMed] [Google Scholar]
- Owen D, Heyman R, Smith Slep A. The Risk of Partner Aggression Research: Impact of Laboratory Couples Conflict Protocols on Participants. Violence and Victims. 2006;21:483–497. doi: http://dx.doi.org/10.1891/0886-6708.21.4.483. [PMC free article] [PubMed] [Google Scholar]
- Padesky CA, Hammen CL. Sex differences in depressive symptom expression and help-seeking among college students. Sex Roles. 1981;7:309–320. doi: 10.1007/BF00287545. [Google Scholar]
- Pettit J, Joiner TE. The interpersonal solution to depression. New Harbinger; Oakland, CA: 2005. [Google Scholar]
- Riggs DS, Byrne CA, Weathers FW, Litz BT. The quality of the intimate relationships of male Vietnam veterans: Problems associated with posttraumatic stress disorder. Journal of Traumatic Stress. 1998;11:87–101. doi: 10.1023/A:1024409200155. doi:10.1023/A:1024409200155. [DOI] [PubMed] [Google Scholar]
- Ruscher SM, Gotlib IH. Marital interaction patterns of couples with and without a depressed partner. Behavior Therapy. 1988;19:455–470. doi:10.1016/S0005-7894(88)80016-9. [Google Scholar]
- Schwartz G. Estimating the dimension of a model. The Annals of Statistics. 1978;6:461–464. doi:10.1214/aos/1176344136. [Google Scholar]
- Simpson LE, Christensen A. Spousal agreement regarding relationship aggression on the Conflict Tactics Scale-2. Psychological Assessment. 2005;17:423–432. doi: 10.1037/1040-3590.17.4.423. doi:10.1037/1040-3590.17.4.423. [DOI] [PubMed] [Google Scholar]
- South SC, Krueger RF. Marital quality moderates genetic and environmental influences on the internalizing spectrum. Journal of Abnormal Psychology. 2008;117:826–837. doi: 10.1037/a0013499. doi: 10.1037/a0013499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spanier GB. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. Journal of Marriage and the Family. 1976;38:15–28. doi:10.2307/350547. [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised Conflict Tactics Scales (CTS2): Development and preliminary psychometric data. Journal of Family Issues. 1996;17:283–316. doi:10.1177/019251396017003001. [Google Scholar]
- Taft CT, Pless AP, Stalans LJ, Koenen KC, King LA, King DW. Risk factors for partner violence among a national sample of combat veterans. Journal of Consulting and Clinical Psychology. 2005;73:151–159. doi: 10.1037/0022-006X.73.1.151. doi:10.1037/0022-006X.73.1.151. [DOI] [PubMed] [Google Scholar]
- Taft CT, Schumm JA, Marshall AD, Panuzio J, Holtzworth-Munroe A. Family-of-origin maltreatment, posttraumatic stress disorder symptoms, social information processing deficits, and relationship abuse perpetration. Journal of Abnormal Psychology. 2008;117:637–646. doi: 10.1037/0021-843X.117.3.637. doi:10.1037/0021-843X.117.3.637. [DOI] [PubMed] [Google Scholar]
- Taft CT, Schumm JA, Panuzio J, Proctor SP. An examination of family adjustment among Operation Desert Storm veterans. Journal of Consulting and Clinical Psychology. 2008;76:648–656. doi: 10.1037/a0012576. doi:10.1037/a0012576. [DOI] [PubMed] [Google Scholar]
- Taft CT, Weatherill RP, Woodward HE, Pinto LA, Watkins LE, Miller MW, Dekel R. Intimate partner and general aggression perpetration among combat veterans presenting to a posttraumatic stress disorder clinic. American Journal of Orthopsychiatry. 2009;79:461–468. doi: 10.1037/a0016657. doi: 10.1037/a0016657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taft CT, Watkins LE, Stafford J, Street AE, Monson CM. Posttraumatic stress disorder and intimate relationship problems: A meta-analysis. Journal of Consulting and Clinical Psychology. 2011;79:22–33. doi: 10.1037/a0022196. doi:10.1037/a0022196. [DOI] [PubMed] [Google Scholar]
- Wamboldt MZ, Wamboldt FS. Role of the family in the onset and outcome of childhood disorders: Selected research findings. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:1212–1219. doi: 10.1097/00004583-200010000-00006. doi:10.1097/00004583-200010000-00006. [DOI] [PubMed] [Google Scholar]
- Weiss RL, Heyman RE. Couples observational research: An impertinent, critical overview. In: Kerig PK, Baucom DH, editors. Couple Observational Coding Systems. Lawrence Erlbaum Associates; Mahwah, New Jersey: 2004. [Google Scholar]
- Whisman MA. Marital dissatisfaction and psychiatric disorders: Results from the National Comorbidity Survey. Journal of Abnormal Psychology. 1999;108:701–706. doi: 10.1037//0021-843x.108.4.701. doi:10.1037/0021-843X.108.4.701. [DOI] [PubMed] [Google Scholar]
- Wolf EJ, Miller MW, Harrington K, Reardon A. Personality-based latent classes of posttraumatic psychopathology: Personality disorders and the Internalizing/Externalizing model. Journal of Abnormal Psychology. 2012;121:256–262. doi: 10.1037/a0023237. doi:10.1037/a0023237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf EJ, Miller MW, Orazem R, Weirich M, Castillo DT, Milford J, Keane TM. The MMPI-2 Restructured Clinical Scales in the assessment of posttraumatic stress disorder and comorbid disorders. Psychological Assessment. 2008;20:327–340. doi: 10.1037/a0012948. doi:10.1037/a0012948. [DOI] [PMC free article] [PubMed] [Google Scholar]