Abstract
The northwest border city of Tijuana is Mexico’s fifth largest and is experiencing burgeoning drug use and human immunodeficiency virus (HIV) epidemics. Since local geography influences disease risk, we explored the spatial distribution of HIV among injection drug users (IDUs). From 2006–2007, 1056 IDUs were recruited using respondent-driven sampling, and then followed for eighteen months. Participants underwent semi-annual surveys, mapping, and testing for HIV, tuberculosis, and syphilis. Using Average Nearest Neighbor and Getis-Ord Gi* statistics, locations where participants lived, worked, bought and injected drugs were compared with HIV status and environmental and behavioral factors. Median age was thirty-seven years; 85 percent were male. Females had higher HIV prevalence than males (10.2 percent vs. 3.4 percent; p=0.001). HIV cases at baseline (n=47) most strongly clustered by drug injection sites (Z-Score −6.173; p < 0.001), with a 16 km2 hotspot near the Mexico/U.S. border, encompassing the red-light district. Spatial correlates of HIV included syphilis infection, female gender, younger age, increased hours on the street per day, and higher number of injection partners. Almost all HIV seroconverters injected within a 2.5 block radius of each other immediately prior to seroconversion. Only history of syphilis infection and female gender were strongly associated with HIV in the area where incident cases injected. Directional trends suggested a largely static epidemic until July–December 2008, when HIV spread to the southeast, possibly related to intensified violence and policing that spiked in the latter half of 2008. While clustering allows for targeting interventions, the dynamic nature of epidemics suggests the importance of mobile treatment and harm reduction programs.
Keywords: HIV, spatial epidemiology, injection drug use, local geography
Introduction
Infectious disease rates are often reported at a state or national level, yet transmission operates at a much finer spatial scale. In the case of an infection such as the human immunodeficiency virus (HIV), which is influenced by social stigma and frequently concentrated in marginalized populations, exploring local geography may help to elucidate factors driving transmission. Spatial analysis can also assist in better allocation of scarce public health resources.
Injection drug use accounts for nearly 10 percent of HIV cases globally, with an estimated 20 percent of all injection drug users (IDUs) being infected (UNAIDS/WHO 2010). There is growing recognition of the importance of “place,” in terms of its physical, social, and geographical characteristics, on HIV risk (Rhodes et al. 1999). For IDUs, “unsafe places” associated with risky behaviors, such as needle sharing, include parks, alleys, abandoned buildings and “shooting galleries” (where drugs may be obtained and injected with other IDUs) (Small et al. 2007; Tempalski and McQuie 2009). Injecting outdoors may increase exposure to authorities, and fear of arrest or police harassment has been associated with needle sharing, injection in riskier environments, rushed injections, and unsafe syringe disposal (Koester 1994; Bluthenthal et al. 1997; Feldman and Biernacki 1998; Cooper et al. 2011). Social, structural, and economic disparities between neighborhoods and laws governing substance use and access to clean syringes also influence HIV transmission (Friedman, Perlis and Des Jarlais 2001; Tempalski et al. 2007). Further, geographic proximity (which can be a correlate for social interactions) to social networks with high prevalence of infection or risky injection groups norms may increase one’s risk of HIV (Unger et al. 2006; Davey-Rothwell and Latkin 2007; Wylie, Shah and Jolly 2007).
The HIV epidemic in Mexico is concentrated in at-risk groups, such as IDUs (CENSIDA 2010). While drug use is not common in Mexico, Tijuana - a metropolitan area of 1.8 million adjacent to San Diego, CA, USA (INEGI 2010) - is situated on a major northbound drug trafficking route, with spillover use becoming entrenched in the urban environment (Bucardo et al. 2005; Brouwer et al. 2006a). Tijuana is also on the busiest land border crossing in the world (for source of data, see Weeks, Jankowski and Stoler 2011). Greater exposure to U.S. media (music, TV, etc.) and interactions with those from the United States have been associated with higher drug use intentions and recent drug use among Tijuana adolescents (Becerra 2011). In 2003, it was estimated that approximately 6,000 IDUs attend shooting galleries in Tijuana, with the total reaching 10,000 (Magis-Rodriguez et al. 2005).
HIV among IDUs can increase exponentially. In Jakarta, Indonesia, HIV prevalence in IDUs rose from 0 percent in 1997 to 48 percent in 2002 (Monitoring the AIDS Pandemic (MAP) Network 2004). We found crude HIV prevalence among Tijuana IDUs to be 1.9 percent in 2005 (Frost et al. 2006), 4.5 percent in 2007, and 10.2 percent among female IDUs in 2008 (Brouwer et al. 2006b; Strathdee et al. 2008a; Iniguez-Stevens et al. 2009), indicating the importance of vigilance to prevent a more generalized epidemic (Strathdee and Magis-Rodriguez 2008). In multivariate analysis, correlates of HIV infection among Tijuana IDUs included being female, syphilis titers suggestive of an active infection, increased numbers of injection partners, shorter time in Tijuana, and arrest for having track-marks (Strathdee et al. 2008b). A subsequent analysis stratified by sex found additional associations, including younger age, lifetime syphilis infection and longer time in Tijuana for females, and history of deportation for males (Strathdee et al. 2008a). In the present analysis, we explore HIV among IDUs from a spatial perspective, in order to better understand the distribution of cases over time and contextual factors associated with infection.
Methods
Study Population
From 2006–2007, 1056 IDUs residing in Tijuana, Mexico were enrolled into a study examining behavioral and contextual factors associated with HIV, syphilis, and tuberculosis infection, as described previously (Strathdee et al. 2008b). Participants were recruited through respondent-driven sampling (RDS), in order to achieve a more representative sample of this hard-to-reach population (Heckathorn 1997). Briefly, a group of “seeds” was selected based on diversity of neighborhoods, gender, and drug preferences, and given three uniquely coded coupons to refer IDUs in their social networks, who were themselves given coupons to recruit three peers. Eligibility criteria included being 18 years or older and a Spanish or English speaker, having injected drugs within the previous month, providing informed consent, and having no plans to move out of the city in the next 18 months. The Ethics Board of the Tijuana General Hospital and Institutional Review Board of the University of California, San Diego approved the study.
Data Collection
At baseline and every 6 months thereafter, staff from a municipal HIV/AIDS program (Patronato ProCOMUSIDA A.C.) administered a quantitative survey to elicit information on demographic and economic factors, drug use practices, sexual behaviors, and HIV testing history. Additionally, participants were asked where they live (or most often sleep at night), earn money, and most commonly buy or use drugs. Mapping took place in an interactive manner with interviewers helping to narrow down locations from colonias or “neighborhoods” to more precise locations based on a discussion of landmarks and major cross-roads. Data were digitized in ArcMap 9.3 (ESRI, Redlands, CA).
Participants were tested for HIV, tuberculosis, and syphilis, as described previously (Strathdee et al. 2008a; Strathdee et al. 2008b). Pre- and post-test counseling were provided to all participants and those testing positive were referred to local public health care providers for free care, if indicated. Additionally, those with syphilis titers ≥1:8 were given antibiotic treatment and counseling on risk behaviors.
Data Analysis
Using Average Nearest Neighbor and Getis-Ord Gi* statistics and analytical extensions in ArcGIS version 9.3 software (ESRI, Redlands, CA), spatial distribution of where participants lived, worked, bought, and injected drugs were compared with HIV status and in relation to contextual factors. The Getis-Ord Gi* analysis was based on a fixed Euclidean distance band of 3000 m. This distance was derived from a previous analysis of this population indicating 3 km to be a natural break point in the data with respect to intra-urban mobility (Brouwer et al. 2012). It is also the distance an average person walks in 30–40 minutes (Knoblauch, Pietrucha and Nitzburg 1996; Marx et al. 2000), which is how most of our participants travel. Results were corrected for multiple testing using the False Discovery Rate statistic (Benjamini and Hochberg 1995; Castro and Singer 2006).
Truncated spatial correlograms were constructed using Spatial Analysis in Macroecology v.4.0 (Rangel, Diniz-Filho and Bini 2010) to estimate the spatial correlation between HIV and variables previously found associated with HIV in this population (Strathdee et al. 2008a; Strathdee et al. 2008b). The effective number of degrees of freedom was estimated using Duttileul's estimator (Dutilleul 1993). The mean center and directional distribution (standard deviational ellipse) of HIV cases were calculated for each six-month time period of the study. Characteristics of colonias with more versus fewer than expected numbers of HIV cases were compared based on year 2000 census data (INEGI 2000) or data from health service or other registries. In most cases, such analyses were performed using the Mann Whitney U test to compare distributions across groups. Two-sided P-values < 0.05 were considered statistically significant.
Results
Characteristics of the study population
Median age of participants was 37 years (interquartile range (IQR) 31–42), with 85 percent being male and 69 percent single (unmarried, divorced, widowed, or separated). Two thirds (67 percent) were born outside of Baja California (the state where Tijuana is located) and 39 percent had come to Tijuana because of deportation from the United States. While most (78 percent) had ever traveled to the United States, 7 percent did so in the past year, with 6 percent accessing U.S. health services and 10 percent buying syringes. Nearly half (48 percent) reported ever injecting drugs with someone from the United States. While 13.4 percent were homeless, median amount of time spent on the street/24h was ten hours (IQR 7–12). Participants reported having twenty friends who also inject drugs (IQR 10–50), although the usual number of injection partners was two (IQR 1–3). HIV prevalence was higher in females compared to males (10.2 percent vs. 3.4 percent; p=0.001) and over 15 percent of participants had a history of syphilis infection, with half of these having titers suggestive of an active infection. Participants reported that they most commonly injected heroin (57.1 percent) or methamphetamine with heroin (39.6 percent), and 83 percent injected drugs at least daily. These demographics and drug behaviors did not change significantly over time, although the first and last time periods of the study deviated the most from mean values. Of the 1056 participants, 943 (89 percent) had at least one follow-up interview, with 82 percent still represented by month 18. A total of twenty participants (1.9 percent) died between baseline and 18 months of follow-up, of which five were HIV-positive.
HIV Distribution
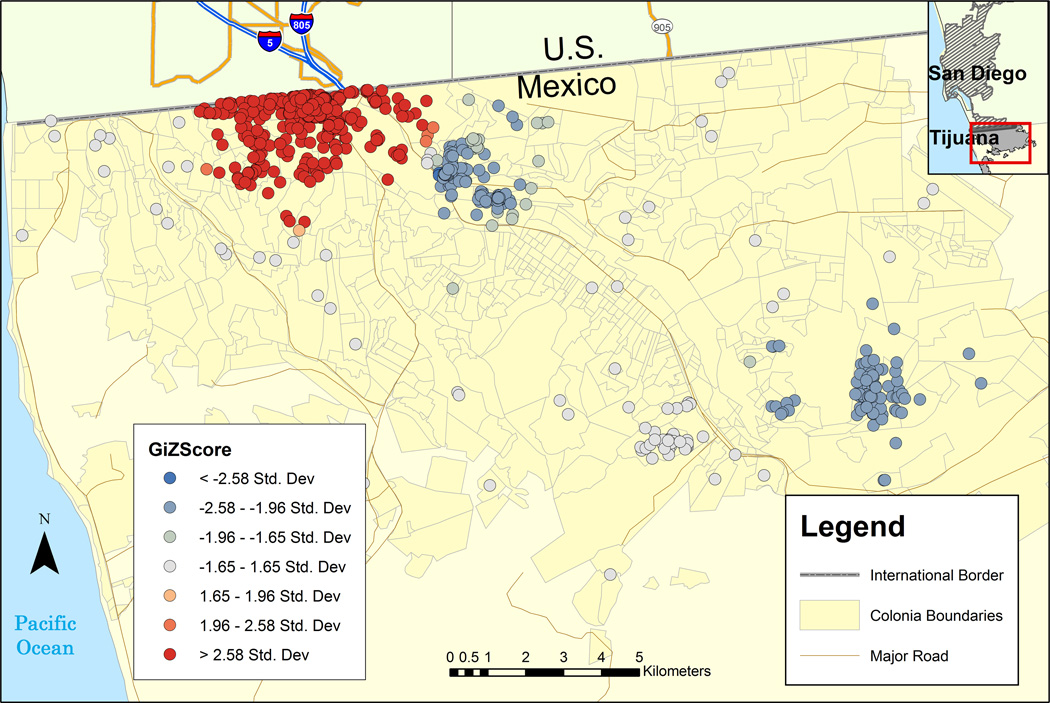
In comparing where one lives, works/earns money, buys or injects drugs, HIV cases at baseline (n=47) most strongly clustered by drug injection site, followed by residence (Table 1). There was no global clustering by work site. Drug use was unevenly spread throughout the city (Figure 1); certain injection locations had a higher than expected number of HIV-positive participants (Figure 1, red circles), with a ~16 km2 hotspot near the Mexico/U.S. border encompassing the red-light district. Other neighborhoods, especially to the southeast, had fewer cases than expected (Figure 1, blue circles). Local clustering of HIV was not as extensive for IDU residences, work, or drug purchase sites; did not reveal new clusters; and tended to occur when injection and the other activity overlapped. In examining the distribution of HIV by sex, males most strongly clustered by injection site-- with many traveling between their main injection site and where they lived or worked. For females, the four types of activities generally occurred in the same place or in very close proximity to each other (data not shown).
Table 1.
Clustering of HIV-positive participants at baseline by activity location (n=47) a
| Activity | Z-Score | p -value |
|---|---|---|
| Live | −4.447 | <0.001 |
| Buy Drugs | −2.113 | 0.035 |
| Inject Drugs | −6.173 | <0.001 |
| Work | −1.535 | 0.125 |
Average Nearest Neighbor
Figure 1.
HIV hot and cold spots of injection sites among substance using participants at baseline (n=1056) in Tijuana, Mexico.
Incident HIV cases
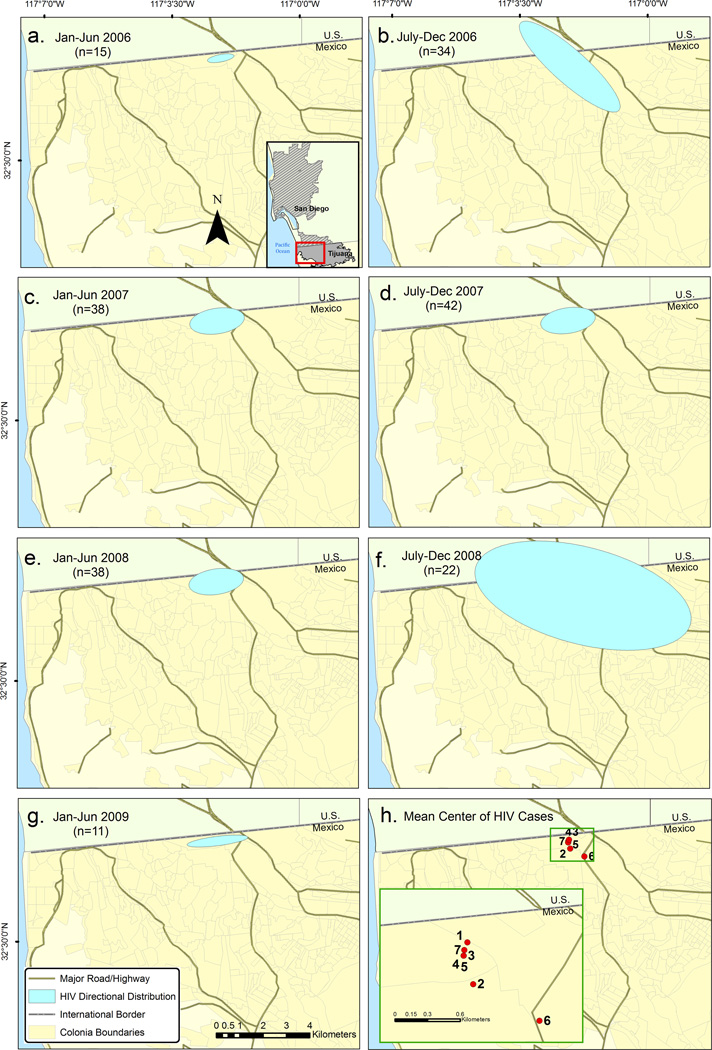
Eleven of the twelve who seroconverted during follow-up injected within 2.5 blocks (380 m) of the mean center of each other during the study visit immediately prior to seroconversion. After some initial changes in distribution (Figure 2, panels a and b), directional trends suggested a largely static epidemic until July–December 2008, when HIV cases spread to the southeast (Figure 2). To explore whether these changes were due to movement of HIV-positive participants or a change in the underlying sample comprising a particular period, we measured the distance each individual’s injection sites shifted over consecutive follow-up visits. The median distance moved was <350 m for all time periods, with the exception of July–December 2008, with a median of zero for July–December 2007 and January–June 2008 (Figure 2, panels d and e). For the time periods with the largest ellipses (Figure 2, panels b and f), median distance injection sites moved was just 113.5 m IQR (72, 218) for July–December 2006 but 1674 m IQR (609.5,5343.5) for July–December 2008. Most (68 percent) of the 2006 period was comprised of new enrollees (not attending a follow-up visit), suggesting that the ellipse size might reflect an evolving study population as it became established through RDS. However, during the July–December 2008 time period there was a sudden shift in preferred injection sites of a number of individuals. The period at the close of the study (January–June 2009) does not suggest a continuation of the dispersion seen in the July–December 2008; however, the follow-up period for the participants who had moved from the HIV core in the latter half of 2008 had ended by 2009, so their data is not included in this final period.
Figure 2.
Panels a and b represent January–June 2006 and July–December 2006, respectively. Panel c and d are the respective 6 month time periods for 2007, panels e and f represent 2008, and panel g represents January–June 2009. Red dots in panel h denote the mean center of HIV cases at each of the time periods indicated in the previous panels. The scale and legend in panel g applies to all maps.
Associations with HIV distribution
To better understand the distribution of HIV and incident cases, we explored a number of variables for spatial correlation with HIV. Those with significant or marginally significant correlations are listed in Table 2. Rxr diagonal maps (data not shown) showed that only lifetime syphilis infection and gender showed strong correlation in the area where most incident cases occurred.
Table 2.
Spatial correlations with HIV distribution (n=1056)
| Characteristic | Pearson's r | p-value |
|---|---|---|
| Age | −0.063 | 0.041 |
| Hours on street per day | 0.093 | 0.003 |
| Born in Baja California | −0.060 | 0.059 |
| History of Deportation | 0.057 | 0.061 |
| Female gender | 0.119 | <0.001 |
| Number of injection partners (past 6 mo) | 0.075 | 0.014 |
| History of syphilis infection | 0.163 | <0.001 |
| Active syphilis infection (titer ≥ 1:8) | 0.144 | <0.001 |
In comparing neighborhood characteristics, those comprising the HIV hot spot had higher divorce and female headed household rates, but lower home ownership and health insurance rates (Table 3). Fewer residents in the “hot spot” area had an educational deficit. Although of marginal significance, population density was lower and drug treatment centers more plentiful in the HIV hotspot (Table 3).
Table 3.
Characteristics of HIV hot spot vs. cold spot neighborhoods (colonias)
| Colonia characteristic | Hot spot | Cold spot 1a |
Cold spot 2a |
|---|---|---|---|
| density per km2 | |||
| Population density | 5452 | 9501 | 10451 |
| Public health centers | 0.43 | 0 | 0.18 |
| Drug treatment centers | 0.98 | 0* | 0.18 |
| median % | |||
| Colonias considered high crime areas by police | 50.0 | 14.3 | 50.0 |
| Divorced | 6.3 | 5.1* | 4.5** |
| Population living in female headed households | 24.1 | 22.5* | 19.5** |
| Catholic | 85.1 | 84.3 | 78.6** |
| Employed | 59.6 | 58.7 | 62.8 |
| Home ownership | 45.4 | 54.4** | 71.4** |
| Born outside of Baja California | 49.5 | 50.7 | 56.5 |
| Residents living in Tijuana at least 5 years | 80.9 | 81.1 | 76.8** |
| Adult literacy | 97.7 | 97.2 | 96.1* |
| Population >15 yrs with less than 9th grade education | 38.2 | 48.2* | 56.2** |
| Population with health insurance | 37.4 | 44.7* | 50.8** |
Cold spot 2 refers to the neighborhoods furthest to the southeast in Figure 1, whereas cold spot 1 is closer to the HIV hot spot
p < 0.05;
p < 0.01, based on a Mann Whitney U or t-test
Discussion
From a unique compilation of longitudinal survey, biological, and spatial data, our study demonstrates how spatial analysis can lead to a better understanding of HIV transmission mechanisms among IDUs in Tijuana. While previous work by our group identified correlates of HIV infection using traditional database methods, examining the spatial distribution of cases provided further insights into environmental factors that might influence transmission and how the epidemic might be changing over time.
As is common in other cities, drug use was concentrated in certain neighborhoods (Veldhuizen, Urbanoski and Cairney 2007); however, HIV cases clustered even more strongly. HIV-positive participants clustered most strongly by injection locations compared with residence, work site, or drug purchase location -- perhaps reflecting transmission foci. Most spatial analyses of infections are based on residential addresses at a single point in time, but our study indicates the importance of gathering a variety of activity locations to improve understanding of disease transmission. We also found differences between activity locations by sex, with females tending to stay in one location and males traveling between sites. This reflects prior qualitative work by us, which revealed that female IDUs often obtained drugs from someone who delivered them, be it a sexual partner or a drug dealer. Male IDUs, however, reported several buying locations and more often injected in shooting galleries far from their residence (Firestone Cruz et al. 2006; Brouwer et al. 2012). This suggests that different strategies may be needed to reach male and female IDUs for educational and harm reduction campaigns.
Studies employing geographic tools allow one to identify and explore the influence of important environmental factors. For instance, our study also identified a number of differences in HIV “hot” vs. “cold” spot neighborhoods. Lower home ownership and insurance and higher divorce and female-headed household rates in the hot spot may suggest more social instability and less social support, while lower population density might reflect large numbers of abandoned buildings in the area -- often used as shooting galleries. As discussed earlier, the social and structural environment in which substance use takes place plays a critical role in shaping risk behaviors that predispose to blood-borne and sexually transmitted infections (Rhodes et al. 2005). HIV prevention interventions incorporating changes to the physical, social, economic, and legal environments to facilitate individual and community-level behavior change have had the most success (Rhodes et al. 2005).
The highly concentrated distribution of incident HIV cases suggests that targeting only a small area in Tijuana could have a large impact on incidence of HIV. Proximity to syringe exchange programs and drug treatment has been linked with increased use (Rockwell et al. 1999; Sarang, Rhodes and Platt 2008; Cooper et al. 2011). However, resource availability does not guarantee full access or utilization. Fear of police or being identified as an IDU, stigma, operating hours, and local social and political conditions can shape access (Bluthenthal et al. 1997; Tempalski et al. 2007; Simmonds and Coomber 2009; Tempalski and McQuie 2009). The border region is particularly complicated in that migratory and legal status might affect access and continuity of care (Moyer et al. 2008; Brouwer et al. 2009; Volkmann et al. 2011). This speaks to the importance of cross-border HIV health policies.
Clustering of incident cases also facilitated identification of structural factors possibly associated with transmission. For instance, female sex and syphilis infection were the primary spatial associations with HIV where incident cases occurred, and this area overlaps with the Zona Roja (‘red light district’) of Tijuana. Previous work by us and others indicates considerable overlap between drug use and the sex trade, with HIV prevalence among FSW-IDUs in Tijuana surpassing twelve percent (Strathdee et al. 2008c). Since the Zona Roja is a major attractor of sexual tourism, drawing clients from the United States, Asia, and elsewhere, potential for further spread of HIV in the region is also a concern.
Injection locations of HIV-positive participants remained fairly static until July–December 2008, when HIV cases shifted to the southeast. The reasons for this are unclear but may relate to changes in the local environment, such as economic conditions, drug availability, etc. In recent years, there has been a tremendous increase in the number of murders in Tijuana (Negron 2008; Welch 2009), which peaked at 843 in the latter half of 2008 -- up 2.5 fold from 2007 (Welch 2009). At the same time, military presence increased, creating an uneasy relationship between local police and federal forces. Anecdotal reports from participants suggested that this led to a number of police “sweeps” through the canal area near the Mexico/U.S. border, where many participants resided or injected drugs. Due to an end in the follow-up periods of a number of participants, it is uncertain if the directional trend seen in the latter half of 2008 continued or if HIV cases who had shifted injection sites eventually moved back to the HIV hot spot. If they did remain outside of the main HIV core, one of the unintended consequences of enforcement activities may have been displacement of HIV cases to other parts of the city, facilitating HIV to penetrate new social networks. Displaced persons have been shown to be particularly vulnerable to HIV (Friedman, Rossi and Braine 2009; Kim et al. 2009; Marshall et al. 2009). Likewise, political-economic events and transitions are theorized to create risk environments that may facilitate drug use and HIV outbreaks (Friedman et al. 2009). Since the HIV risk environment in northern Mexico/U.S. border cities is constantly shifting due to drug-related violence, migration, economic factors, and policing, their individual and joint impact on transmission of HIV and sexually transmitted infections (STIs) warrants continued surveillance.
The present analysis was limited in that it focused on the locations where a subject “most often” participated in an activity in the past six months. Such data may fail to capture exposures of participants who often move or inject in a variety of locations. Although RDS seeds were selected to promote geographic diversity, more socially isolated IDUs may be under-represented and network bottlenecks may have affected the spatial patterns observed. However our fairly large sample (n=1056) compared to the estimated number of IDUs in the city (10,000), may have tempered this. Another possible limitation is that not all participants were enrolled at the same time, so their follow-up period may represent exposure to different environmental circumstances. Further, not every 6 month time period in the longitudinal analysis reflects the same participants, due to rolling enrollment as well as loss to follow-up or death. In particular, the first and last time periods were based on fewer participants due to study initiation and subsequent closure. Despite these limitations, the stability of the HIV epidemic for most of the study suggests that such changes did not greatly affect our results.
Our study highlighted spatial and environmental factors related to the IDU HIV epidemic in Tijuana, Mexico. Spatial clustering of HIV cases by injection site, but less so by other activity locations, suggests the importance of collecting the most pertinent location data possible when exploring disease distribution. Our study also indicates the importance of collecting longitudinal data and exploring spatial data by sex. The dynamic nature of this epidemic suggests the need for intensified prevention efforts involving community outreach, mobile treatment and harm reduction programs. A high correlation with syphilis infection suggests that treatment of STIs, in addition to efforts to reduce drug related harm, is needed. Additional studies are necessary to determine the consequences and causes of the dispersion of HIV cases in the latter half of 2008, and whether this trend has continued.
References
- Becerra D. 14th Annual Conference of the Socity for Social Work Research. San Francisco, CA: 2011. The relationship between pre-migration acculturation and substance use. [Google Scholar]
- Benjamini Y, Hochberg Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. Journal of the Royal Statistical Society. 1995;57:289–300. [Google Scholar]
- Bluthenthal RN, Kral AH, Lorvick J, Watters JK. Impact of law enforcement on syringe exchange programs: a look at Oakland and San Francisco. Medical anthropology. 1997;18:61–83. doi: 10.1080/01459740.1997.9966150. [DOI] [PubMed] [Google Scholar]
- Brouwer KC, Case P, Ramos R, Magis-Rodriguez C, Bucardo J, Patterson TL, Strathdee SA. Trends in Production, Trafficking and Consumption of Methamphetamine and Cocaine in Mexico. Substance Use and Misuse. 2006a;41:707–727. doi: 10.1080/10826080500411478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brouwer KC, Lozada R, Cornelius WA, Firestone Cruz M, Magis-Rodriguez C, Zuniga de Nuncio ML, Strathdee SA. Deportation along the U.S.-Mexico border: its relation to drug use patterns and accessing care. Journal of Immigrant and Minority Health. 2009;11:1–6. doi: 10.1007/s10903-008-9119-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brouwer KC, Lozada R, Weeks JR, Magis-Rodriguez C, Firestone M, Strathdee SA. Intra-Urban Mobility and its Potential Impact on the Spread of Blood-Borne Infections among Drug Injectors in Tijuana, Mexico. Substance Use and Misuse. 2012 doi: 10.3109/10826084.2011.632465. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brouwer KC, Strathdee SA, Magis-Rodriguez C, Bravo-Garcia E, Gayet C, Patterson TL, Bertozzi SM, Hogg RS. Estimated numbers of men and women infected with HIV/AIDS in Tijuana, Mexico RS. Journal of Urban Health. 2006b;83:299–307. doi: 10.1007/s11524-005-9027-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucardo J, Brouwer KC, Magis-Rodriguez C, Ramos R, Fraga M, Perez SG, Patterson TL, Strathdee SA. Historical trends in the production and consumption of illicit drugs in Mexico: implications for the prevention of blood borne infections. Drug Alcohol Depend. 2005;79:281–293. doi: 10.1016/j.drugalcdep.2005.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castro MC, Singer BH. A new approach to account for multiple and dependent tests in local statistics of spatial association: controlling the false discovery rate. Geographical Analysis. 2006;38:180–208. [Google Scholar]
- CENSIDA. [HIV/AIDS in Mexico 2010]. Mexico City: Centro Nacional para la Prevención y el Control del VIH/SIDA (CENSIDA) 2010
- Cooper HL, Des Jarlais DC, Ross Z, Tempalski B, Bossak B, Friedman SR. Spatial access to syringe exchange programs and pharmacies selling over-the-counter syringes as predictors of drug injectors' use of sterile syringes. Am J Public Health. 2011;101:1118–1125. doi: 10.2105/AJPH.2009.184580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davey-Rothwell MA, Latkin CA. Gender differences in social network influence among injection drug users: Perceived norms and needle sharing. Journal of Urban Health. 2007;84:691–703. doi: 10.1007/s11524-007-9215-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutilleul P. Modifying the t test for assessing the correlation between two spatial processes. Biometrics. 1993;49:305–314. [Google Scholar]
- Feldman HW, Biernacki P. The ethnography of needle sharing among intravenous drug users and implications for public policies and intervention strategies. NIDA research monograph. 1998;80:28–39. [PubMed] [Google Scholar]
- Firestone Cruz M, Mantsios A, Ramos R, Case P, Brouwer KC, Ramos ME, Fraga WD, Latkin CA, Miller CL, Strathdee SA. A Qualitative Exploration of Gender in the Context of Injection Drug Use in Two US-Mexico Border Cities. AIDS and Behavior. 2006 doi: 10.1007/s10461-006-9148-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman SR, Perlis T, Des Jarlais DC. Laws prohibiting over-the-counter syringe sales to injection drug users: relations to population density, HIV prevalence, and HIV incidence. Am J Public Health. 2001;91:791–793. doi: 10.2105/ajph.91.5.791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman SR, Rossi D, Braine N. Theorizing "Big Events" as a potential risk environment for drug use, drug-related harm and HIV epidemic outbreaks. International Journal of Drug Policy. 2009;20:283–291. doi: 10.1016/j.drugpo.2008.10.006. [DOI] [PubMed] [Google Scholar]
- Frost SD, Brouwer KC, Firestone Cruz MA, Ramos R, Ramos ME, Lozada RM, Magis-Rodriguez C, Strathdee SA. Respondent-driven sampling of injection drug users in two U.S.-Mexico border cities: recruitment dynamics and impact on estimates of HIV and syphilis prevalence. Journal of Urban Health. 2006;83:i83–i97. doi: 10.1007/s11524-006-9104-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckathorn DD. Respondent-driven sampling: A new approach to the study of hidden populations. Social Problems. 1997;44:174–199. [Google Scholar]
- INEGI. México: 2000. XII Censo General de Población y Vivienda 2000. [Google Scholar]
- INEGI. Mexico City: 2010. Censo de Poblacion y Vivienda 2010: Estados Unidos Mexicanos Resultados Preliminares. [Google Scholar]
- Iniguez-Stevens E, Brouwer KC, Hogg RS, Patterson TL, Lozada R, Magis-Rodriguez C, Elder JP, Viani RM, Strathdee SA. Estimating the 2006 prevalence of HIV by gender and risk groups in Tijuana, Mexico. Gaceta Medica de Mexico. 2009;145:189–195. [PMC free article] [PubMed] [Google Scholar]
- Kim AA, Malele F, Kaiser R, Mama N, Kinkela T, Mantshumba JC, Hynes M, De Jesus S, Musema G, Kayembe PK, Hawkins Reed K, Diaz T. HIV infection among internally displaced women and women residing in river populations along the Congo River, Democratic Republic of Congo. AIDS and Behavior. 2009;13:914–920. doi: 10.1007/s10461-009-9536-z. [DOI] [PubMed] [Google Scholar]
- Knoblauch RL, Pietrucha MT, Nitzburg M. Field Studies of Pedestrian Walking Speed and Start-Up Time. Transportation Research Record, Pedestrian and Bicycle Research. 1996:1538. [Google Scholar]
- Koester SK. The context of risk: ethnographic contributions to the study of drug use and HIV. NIDA research monograph. 1994;143:202–217. [PubMed] [Google Scholar]
- Magis-Rodriguez C, Brouwer KC, Morales S, Gayet C, Lozada R, Ortiz-Mondragon R, Ricketts EP, Strathdee SA. HIV prevalence and correlates of receptive needle sharing among injection drug users in the Mexican-U.s. border city of Tijuana. Journal of psychoactive drugs. 2005;37:333–339. doi: 10.1080/02791072.2005.10400528. [DOI] [PubMed] [Google Scholar]
- Marshall BD, Kerr T, Shoveller JA, Montaner JS, Wood E. Structural factors associated with an increased risk of HIV and sexually transmitted infection transmission among street-involved youth. BMC Public Health. 2009;9:7. doi: 10.1186/1471-2458-9-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marx MA, Crape B, Brookmeyer RS, Junge B, Latkin C, Vlahov D, Strathdee SA. Trends in crime and the introduction of a needle exchange program. Am J Public Health. 2000;90:1933–1936. doi: 10.2105/ajph.90.12.1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monitoring the AIDS Pandemic (MAP) Network. AIDS in Asia: Face the Facts. 2004 [Google Scholar]
- Moyer LB, Brouwer KC, Brodine SK, Ramos R, Lozada R, Cruz MF, Magis-Rodriguez C, Strathdee SA. Barriers and missed opportunities to HIV testing among injection drug users in two Mexico--US border cities. Drug and alcohol review. 2008;27:39–45. doi: 10.1080/09595230701710845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Negron S. Baghdad, Mexico. Texas Monthly. 2008 Dec [Google Scholar]
- Rangel TF, Diniz-Filho JAF, Bini LM. SAM: a comprehensive application for Spatial Analysis in Macroecology. Ecography. 2010;33:46–50. [Google Scholar]
- Rhodes T, Singer M, Bourgois P, Friedman SR, Strathdee SA. The social structural production of HIV risk among injecting drug users. Social Science & Medicine. 2005;61:1026–1044. doi: 10.1016/j.socscimed.2004.12.024. [DOI] [PubMed] [Google Scholar]
- Rhodes T, Stimson GV, Crofts N, Ball A, Dehne K, Khodakevich L. Drug injecting, rapid HIV spread, and the 'risk environment': implications for assessment and response. AIDS. 1999;13(Suppl A):S259–S269. [PubMed] [Google Scholar]
- Rockwell R, Des Jarlais DC, Friedman SR, Perlis TE, Paone D. Geographic proximity, policy and utilization of syringe exchange programmes. AIDS Care. 1999;11:437–442. doi: 10.1080/09540129947811. [DOI] [PubMed] [Google Scholar]
- Sarang A, Rhodes T, Platt L. Access to syringes in three Russian cities: implications for syringe distribution and coverage. International Journal of Drug Policy. 2008;19(Suppl 1):S25–S36. doi: 10.1016/j.drugpo.2007.11.008. [DOI] [PubMed] [Google Scholar]
- Simmonds L, Coomber R. Injecting drug users: a stigmatised and stigmatising population. International Journal of Drug Policy. 2009;20:121–130. doi: 10.1016/j.drugpo.2007.09.002. [DOI] [PubMed] [Google Scholar]
- Small W, Rhodes T, Wood E, Kerr T. Public injection settings in Vancouver: physical environment, social context and risk. International Journal of Drug Policy. 2007;18:27–36. doi: 10.1016/j.drugpo.2006.11.019. [DOI] [PubMed] [Google Scholar]
- Strathdee SA, Lozada R, Ojeda VD, Pollini RA, Brouwer KC, Vera A, Cornelius W, Nguyen L, Magis-Rodriguez C, Patterson TL. Differential effects of migration and deportation on HIV infection among male and female injection drug users in Tijuana, Mexico. PLoS One. 2008a;3:e2690. doi: 10.1371/journal.pone.0002690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strathdee SA, Lozada R, Pollini RA, Brouwer KC, Mantsios A, Abramovitz DA, Rhodes T, Latkin CA, Loza O, Alvelais J, Magis-Rodriguez C, Patterson TL. Individual, social, and environmental influences associated with HIV infection among injection drug users in Tijuana, Mexico. Journal of Acquired Immune Deficiency Syndromes. 2008b;47:369–376. doi: 10.1097/QAI.0b013e318160d5ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strathdee SA, Magis-Rodriguez C. Mexico's evolving HIV epidemic. Journal of the American Medical Association. 2008;300:571–573. doi: 10.1001/jama.300.5.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strathdee SA, Philbin MM, Semple SJ, Pu M, Orozovich P, Martinez G, Lozada R, Fraga M, de la Torre A, Staines H, Magis-Rodriguez C, Patterson TL. Correlates of injection drug use among female sex workers in two Mexico-U.S. border cities. Drug and Alcohol Dependence. 2008c;92:132–140. doi: 10.1016/j.drugalcdep.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tempalski B, Friedman R, Keem M, Cooper H, Friedman SR. NIMBY localism and national inequitable exclusion alliances: The case of syringe exchange programs in the United States. Geoforum. 2007;38:1250–1263. doi: 10.1016/j.geoforum.2007.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tempalski B, McQuie H. Drugscapes and the role of place and space in injection drug use-related HIV risk environments. International Journal of Drug Policy. 2009;20:4–13. doi: 10.1016/j.drugpo.2008.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS/WHO. Geneva, Switzerland: 2010. Report on the global AIDS epidemic|2010. [Google Scholar]
- Unger JB, Kipke MD, De Rosa CJ, Hyde J, Ritt-Olson A, Montgomery S. Needle-sharing among young IV drug users and their social network members: The influence of the injection partner's characteristics on HIV risk behavior. Addictive behaviors. 2006;31:1607–1618. doi: 10.1016/j.addbeh.2005.12.007. [DOI] [PubMed] [Google Scholar]
- Veldhuizen S, Urbanoski K, Cairney J. Geographical variation in the prevalence of problematic substance use in Canada. Can J Psychiatry. 2007;52:426–433. doi: 10.1177/070674370705200704. [DOI] [PubMed] [Google Scholar]
- Volkmann T, Lozada R, Anderson CM, Patterson TL, Vera A, Strathdee SA. Factors associated with drug-related harms related to policing in Tijuana, Mexico. Harm Reduct J. 2011;8:7. doi: 10.1186/1477-7517-8-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weeks JR, Jankowski P, Stoler J. Who's Knocking at the Door? New Data on Undocumented Immigrants to the United States. Population, Space and Place. 2011;17:1–26. [Google Scholar]
- Welch WM. Tijuana off-limits to U.S. Marines. USA Today. 2009 Jan 21; [Google Scholar]
- Wylie JL, Shah L, Jolly A. Incorporating geographic settings into a social network analysis of injection drug use and bloodborne pathogen prevalence. Health Place. 2007;13:617–628. doi: 10.1016/j.healthplace.2006.09.002. [DOI] [PubMed] [Google Scholar]