Abstract
BACKGROUND:
Loud snoring is a common symptom in the general population. The evidence-based literature indicates that snoring may be associated with sleep fragmentation and sleep apnea, which may affect cognitive function and predispose to occupational injury. High rates of occupational injury occur on farms and may be related to personal and health factors. Thus, loud snoring may not be a trivial symptom and should be considered as important in medical assessments.
METHODS:
A prospective cohort study was conducted in Saskatchewan. Baseline questionnaires were completed for 5502 individuals by representatives from 2390 farms. Sleep patterns at baseline were categorized as the following: no reported sleep disorders; physician-diagnosed sleep apnea (treatment unknown); and loud snoring. Survival analyses were used to relate sleep patterns with subsequent injury.
RESULTS:
A total of 6.7% (369 of 5502) of participants reported a possible sleep disorder. Of these, 69.4% (256 of 369) reported loud snoring only. Loud snoring was only associated with a consistent increase in risk (eg, HR 1.45 [95 CI 1.07 to 1.99 for work-related injury]) for five farm injury outcomes. Relationships between physician-diagnosed sleep apnea and time to first injury were not significant, presumably because a diagnosis of sleep apnea implied treatment for sleep apnea.
DISCUSSION:
Sleep disorders are an important potential risk factor for occupational injury on farms. Substantial proportions of farm residents report loud snoring and this is related to subsequent injury. Some of these cases may represent sleep fragmentation or undiagnosed obstructive sleep apnea. Identification and clinical management of sleep disorders related to snoring should be part of health assessments conducted by physicians.
Keywords: Agriculture, Farming, Injury, Occupational health, Sleep disorders, Snoring
Abstract
HISTORIQUE :
Les ronflements bruyants sont un symptôme courant dans l’ensemble de la population. D’après les publications probantes, les ronflements peuvent s’associer à une fragmentation et une apnée du sommeil, qui peuvent nuire à la fonction cognitive et prédisposer aux blessures professionnelles. On constate un taux élevé de blessures professionnelles dans les exploitations agricoles, lesquelles peuvent être liées à des facteurs personnels et à des facteurs de santé. Ainsi, les ronflements bruyants ne sont peut-être pas un symptôme négligeable. Il faudrait tenir compte de leur importance lors des évaluations médicales.
MÉTHODOLOGIE :
Les chercheurs ont procédé à une étude de cohorte prospective en Saskatchewan. Des représentants de 2 390 exploitations agricoles ont rempli des questionnaires de départ à l’égard de 5 502 individus. Ils ont classé les profils de sommeil en début d’étude comme suit : aucun trouble du sommeil déclaré, apnée du sommeil diagnostiquée par le médecin (traitement inconnu) et ronflements bruyants seulement. Des analyses de suivi ont permis de lier les profils du sommeil aux blessures subséquentes.
RÉSULTATS :
Au total, 6,7 % (369 sur 5 502) des participants ont signalé un trouble du sommeil possible. De ce nombre, 69,4 % (256 sur 369) n’ont signalé que des ronflements bruyants. Les ronflements bruyants s’associaient à une augmentation constante du risque (p. ex., rapport de risque 1,45 [95 % IC 1,07 à 1,99 pour les blessures professionnelles]) dans seulement cinq issues de blessures subies dans une exploitation agricole. Le lien entre l’apnée du sommeil diagnostiquée par le médecin et le délai jusqu’à la première blessure n’était pas significatif, probablement parce qu’un diagnostic d’apnée du sommeil s’associe au traitement du problème.
EXPOSÉ :
Les troubles du sommeil constituent un important facteur de risque potentiel de blessures professionnelles dans les exploitations agricoles. Une proportion importante des résidents de ces exploitations déclarent des ronflements bruyants, qui sont liés à des blessures subséquentes. Certains de ces cas pourraient représenter une fragmentation du sommeil ou une apnée obstructive du sommeil non diagnostiquée. Le dépistage et la prise en charge clinique des troubles du sommeil liés aux ronflements devraient faire partie des évaluations de santé effectuées par les médecins.
Loud snoring is a common symptom in the general population, and obstructive sleep apnea, often occurring with the symptom of snoring, is being increasingly recognized as having several possible health effects (1). Obstructive sleep apnea is classically associated with loud snoring, episodes of breathing cessation and frequent arousals during sleep (2). Resulting fragmentation of sleep and loss of sleep may be associated with daytime somnolence and impaired cognition (2). Previous research has established the importance of suspected and diagnosed obstructive sleep apnea as a risk factor for occupational injury (3–9), including injury that occurs among farm populations (10,11). However, a related clinical concern is the high proportion of cases of loud snoring that may be an indication of fractionated sleep and/or obstructive sleep apnea and that remain undiagnosed and, therefore, untreated. The effects of undiagnosed sleep apnea could include higher rates of injury (12); however, such risks can be minimized when treated (13). Thus, loud snoring may not be a trivial symptom and may place individuals at increased risk of occupational injury, particularly in a high-risk industry, such as agriculture, which is characterized by elevated injury rates.
Previous research describing relationships between sleep disorders and injury is limited and represents an important gap in clinical knowledge. Farming is an inherently dangerous occupation, with high rates of both sleep disorders (14) and work-related injury (15). Therefore, we used a large occupational cohort of Saskatchewan farm people to conduct a prospective study. Our objectives were to document the prevalence of physician-diagnosed sleep apnea and also possible cases of undiagnosed sleep disorders as represented by loud snoring among farmers, and to relate the occurrence of these two categories of sleep disorders with subsequent occurrence of farm injury.
METHODS
Study protocol
An existing cohort was used to conduct the present study. The study procedures, sampling methods and analytic plans have been described in full elsewhere (16), and were approved by the Behavioral Research Ethics Board of the University of Saskatchewan (Saskatoon, Saskatchewan) (Beh #06-57) and included the publication of results in section 9 of the ethics application. Briefly, a baseline mail survey of an occupational cohort of 5502 individuals (adults and children) was conducted on 2390 farms in February through April 2007. Baseline mail survey questionnaires were completed following informed consent and returned by a single informant per farm. Data that were collected included a short health survey including information on snoring and sleep apnea, demographic information and a history of farm work injuries that occurred in the 12 months before survey. A representative from each participating farm was asked to provide follow-up information on subsequent farm injury events to all participants. Accordingly, these farms were contacted again by mail on four occasions over approximately two years. The injury data from the baseline survey were subsequently combined with the four follow-up assessments (Figure 1). In total, the injury experiences of each member of the cohort were described over a study period that spanned up to 39 months (36 months for most participants).
Figure 1).
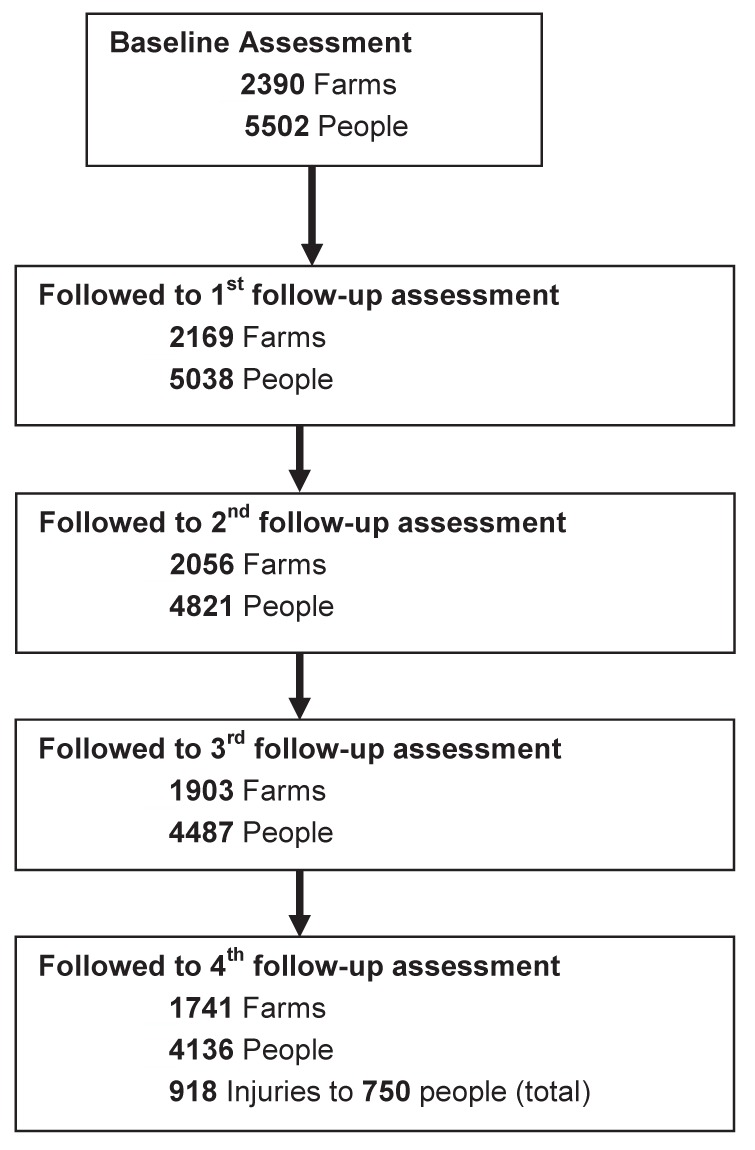
Flow diagram describing participants in the Saskatchewan Farm Injury Cohort Study: Longitudinal Component
Measures
Possible sleep disorders were self-reported at baseline and consisted of the following: reports of physician-diagnosed sleep apnea (yes to “has a doctor diagnosed this person with sleep apnea”); and reports of loud snoring (yes to “loud snoring”). The questionnaire did not query whether the physician-diagnosed sleep apnea was treated or untreated. Key study outcomes were time to the occurrence of farm work injury, operationally defined as any injury that occurred in a farm environment or during the course of farm work, and that resulted in treatment of that injury by a doctor or nurse, or the victim missing at least 4 h from work or usual activities due to the physical effects of the injury (16). If one or more injuries were reported, respondents provided additional detail regarding month of injury, external causes and initial treatment. Specific injury outcomes under study were time to initial farm work injury, medically treated farm work injury, farm machinery injury, farm animal-related injury and farm fall-related injury.
The principal covariates were identified based on theoretical considerations surrounding confounding, as well as existing evidence about known risk factors for farm injury (17–19). The covariates included the following: age, sex, education level, a standard comorbidity index, use of medications (ie, recent use of blood pressure medications, tranquilizers, sleeping pills and/or antidepressants), typical sleep duration (in hours), hours engaged in farm work, hours engaged in tractor operations as a proxy for machinery work and hours engaged in large animal work. The origins and descriptions of these items are also published elsewhere (16).
Statistical analysis
From the baseline survey, three groups were identified: farm people with no reported sleep disorders; individuals with physician-diagnosed sleep apnea; and individuals with loud snoring only (suspected undiagnosed sleep apnea). The distribution of demographic, farm operational, medical and work-related factors within and across these three groups were described using contingency table analyses. The proportions of both physician-diagnosed sleep apnea and loud snoring were estimated only in the full study cohort. Subsequently, a series of Cox regression analyses were conducted to estimate unadjusted and adjusted HRs for time to the occurrence of first injury (first the general category of farm work injury, then specific types of farm work injury). The modelling strategy included adjustment for suspected confounders and known risk factors that are listed in the Methods (Measures) section. Risks were presented as HRs and associated 95% CIs, with robust SEs used to account for the (minimally) clustered nature of the data because individual observations were nested within farms.
RESULTS
A total of 5502 individuals on 2390 farms were recruited at baseline (Figure 1). Follow-up surveys were completed by mail on four occasions. Response rates of 91.5%, 87.9%, 81.5% and 75.1%, respectively, were achieved for the four periods of follow-up. By the fourth follow-up assessment, a total of 918 injuries to 750 people were documented over a time period that included 12 months before the baseline assessment and 24 months following, for a total of 36 months. A small number of late questionnaires were included, and this extended this time to 39 months in total.
Characteristics of the study population at baseline are summarized in Table 1 and stratified according to the three categories of no sleep disorder, diagnosed sleep apnea and loud snoring. Participants with diagnosed sleep apnea were more likely to be older, male, farm owner-operators, report more comorbidities and poorer sleep duration, and contribute full-time work hours on the farm. Characteristics of participants with loud snoring only were more similar to the diagnosed sleep apnea group than to those with no reported sleep disorder symptoms.
TABLE 1.
Individuals involved in the Saskatchewan Farm Injury Cohort Study, 2007 to 2009
| Variable | No sleep disorder (n=5133) | Diagnosed apnea (n=113) | Loud snoring (n=256) | P |
|---|---|---|---|---|
| Age, years | <0.001 | |||
| <50 | 2539 (49.5) | 32 (28.3) | 78 (30.5) | |
| 51–60 | 1379 (26.9) | 41 (36.3) | 102 (39.8) | |
| 61–70 | 716 (13.9) | 27 (23.9) | 48 (18.8) | |
| 71–80 | 340 (6.6) | 9 (8.0) | 23 (9.0) | |
| ≥80 | 88 (1.7) | 4 (3.5) | 2 (0.8) | |
| Education level | 0.56 | |||
| Data missing | 55 (1.1) | 0 (0.0) | 1 (0.4) | |
| Less than high school | 1457 (28.4) | 29 (25.7) | 63 (24.6) | |
| Completed high school | 1847 (36.0) | 41 (36.3) | 107 (41.8) | |
| Completed university | 767 (14.9) | 18 (15.9) | 33 (12.9) | |
| Institution other than above | 1007 (19.6) | 25 (22.1) | 52 (20.3) | |
| Relationship to owner-operator | <0.001 | |||
| Data missing | 44 (0.9) | 1 (0.9) | 2 (0.8) | |
| Owner-operator | 2223 (43.3) | 70 (61.9) | 167 (65.2) | |
| Spouse | 1642 (32.0) | 26 (23.0) | 65 (25.4) | |
| Parent | 111 (2.2) | 6 (5.3) | 6 (2.3) | |
| Child | 982 (19.1) | 8 (7.1) | 12 (4.7) | |
| Other | 131 (2.6) | 2 (1.8) | 4 (1.6) | |
| Comorbidity index | <0.001 | |||
| 0 | 3446 (67.1) | 0 (0.0) | 0 (0.0) | |
| 1 | 1175 (22.9) | 15 (13.3) | 117 (45.7) | |
| ≥2 | 512 (10.9) | 98 (86.7) | 139 (54.3) | |
| Diagnosed high blood pressure | 817 (15.9) | 48 (42.5) | 71 (27.7) | <0.001 |
| Diagnosed heart disease | 189 (3.7) | 13 (11.5) | 14 (5.5) | <0.001 |
| Heart/blood pressure medication | 859 (16.7) | 49 (43.4) | 66 (25.8) | <0.001 |
| Typical sleep, h/night | <0.001 | |||
| Data missing | 45 (0.9) | 0 (0.0) | 2 (0.8) | |
| >7 | 2713 (52.9) | 46 (40.7) | 119 (46.5) | |
| 6–7 | 2177 (42.4) | 46 (40.7) | 118 (46.1) | |
| 4–5 | 181 (3.5) | 19 (16.8) | 17 (6.6) | |
| <4 | 17 (0.3) | 2 (1.8) | 0 (0.0) | |
| Sleep during busy seasons, h/night | <0.001 | |||
| Data missing | 58 (1.1) | 0 (0.0) | 8 (3.1) | |
| >7 | 1667 (32.5) | 21 (18.6) | 53 (20.7) | |
| 6–7 | 2512 (48.9) | 56 (49.6) | 137 (53.5) | |
| 4–5 | 810 (15.8) | 32 (28.3) | 51 (19.9) | |
| <4 | 86 (1.7) | 4 (3.5) | 7 (2.7) | |
| Work status across the four seasons | <0.001 | |||
| Data missing | 536 (10.4) | 11 (9.7) | 22 (8.6) | |
| None | 440 (8.6) | 9 (8.0) | 13 (5.1) | |
| Part-time | 1925 (37.5) | 32 (28.3) | 79 (30.9) | |
| Full-time | 2232 (43.5) | 61 (54.0) | 142 (55.5) | |
| Total acreage in production | <0.001 | |||
| Data missing | 262 (5.1) | 5 (4.4) | 10 (3.9) | |
| 0–500 | 934 (18.2) | 22 (19.5) | 59 (23.0) | |
| 501–1500 | 1653 (32.2) | 41 (36.3) | 84 (32.8) | |
| 1501–2500 | 1036 (20.2) | 20 (17.7) | 55 (21.5) | |
| >2500 | 1248 (24.3) | 25 (22.1) | 48 (18.8) | |
Data presented as n (%) unless otherwise indicated
In addition to the main effects under study, the analysis identified several other variables that were risk or protective factors for the injury outcomes during the process of adjusting for potential confounders. These included: compared with owner-operators, being a spouse (HR 0.29 [95% CI 0.24 to 0.36]), child (HR 0.30 [95% CI 0.19 to 0.46]) or parent (HR 0.33 [95% CI 0.15 to 0.71]) of an owner-operator; reporting two or more comorbidities (HR 1.43 [95% CI 1.08 to 1.89]); regular use of heart or blood pressure medications (HR 0.68 [95% CI 0.53 to 0.87]); reporting <6 h of sleep typically (HR 1.51 [95% CI 1.08 to 2.13]), and being on a farm that raised beef as a commodity (HR 1.53 [95% CI 1.30 to 1.79]).
Prevalence values for physician-diagnosed sleep apnea and loud snoring are shown in Table 2. A total of 6.7% (369 of 5502) (95% CI 6.1% to 7.4%) of the total study population reported either of the two sleep conditions. Of those with either condition, 69.4% (256 of 369) (95% CI 64.7% to 74.1%) reported loud snoring only.
TABLE 2.
Prevalence of diagnosed sleep apnea and loud snoring among members of the Saskatchewan Farm Injury Cohort Study, 2007
| n (%) | 95% CI | |
|---|---|---|
| Diagnosed sleep apnea | 113 (2.1) | 1.7–2.4 |
| Loud snoring only | 256 (4.7) | 4.1–5.2 |
| Total | 369 (6.7) | 6.1–7.4 |
| Loud snoring/total, n/n (%) | 256/369 (69.4) | 64.7–74.1 |
Relationships among the three sleep categories and time to the occurrence of various types of farm injury are summarized in Table 3. Based on the adjusted HRs, participants in the loud snoring category experienced consistent increases in risk for each of the five outcomes, with most injury outcomes achieving statistical significance. Relationships between diagnosed sleep apnea and time to first injury were not statistically significant.
TABLE 3.
Results of Cox proportional hazards modelling for different types of injury
|
Risk estimates
|
||||
|---|---|---|---|---|
|
Unadjusted
|
Adjusted
|
|||
| Injuries, n (%) | HR (95% CI) | Injuries, n (%) | HR (95% CI) | |
| Farm work injury | ||||
| No sleep apnea (n=5133) | 603 (11.7) | 1.00 | 603 (11.7) | 1.00 |
| Diagnosed apnea (n=113) | 15 (13.3) | 1.15 (0.69–1.92) | 15 (13.3) | 0.79 (0.43–1.47) |
| Loud snoring (n=256) | 55 (21.5) | 1.96 (1.49–2.58) | 55 (21.5) | 1.45 (1.07–1.99) |
| Medically treated injury | ||||
| No sleep apnea (n=5133) | 447 (8.7) | 1.00 | 447 (8.7) | 1.00 |
| Diagnosed apnea (n=113) | 18 (15.9) | 1.91 (1.19–3.07) | 18 (15.9) | 1.44 (0.82–2.55) |
| Loud snoring (n=256) | 39 (15.2) | 1.84 (1.33–2.74) | 39 (15.2) | 1.46 (1.01–2.10) |
| Farm machinery injury | ||||
| No sleep apnea (n=5133) | 295 (5.8) | 1.00 | 295 (5.8) | 1.00 |
| Diagnosed apnea (n=113) | 7 (6.2) | 1.08 (0.51–2.27) | 7 (6.2) | 0.67 (0.27–1.63) |
| Loud snoring (n=256) | 26 (10.2) | 1.84 (1.23–2.74) | 26 (10.2) | 1.36 (0.86–2.13) |
| Farm animal injury | ||||
| No sleep apnea (n=5133) | 141 (2.8) | 1.00 | 141 (2.8) | 1.00 |
| Diagnosed apnea (n=113) | 6 (5.3) | 2.00 (0.88–4.55) | 6 (5.3) | 1.83 (0.67–5.04) |
| Loud snoring (n=256) | 11 (4.3) | 1.61 (0.87–2.97) | 11 (4.3) | 1.23 (0.64–2.34) |
| Fall injury | ||||
| No sleep apnea (n=5133) | 179 (3.5) | 1.00 | 179 (3.5) | 1.00 |
| Diagnosed apnea (n=113) | 6 (5.3) | 1.57 (0.69–3.55) | 6 (5.3) | 1.27 (0.49–3.26) |
| Loud snoring (n=256) | 21 (8.2) | 2.43 (1.55–3.81) | 21 (8.2) | 1.92 (1.17–3.14) |
Stratified according to average hours per week worked over four seasons and adjusted according to relationship with owner-operator, beef commodity raised on farm, heart or blood pressure medications, typical sleep duration (in h) and comorbidity index
DISCUSSION
Interpretation
The results of our study suggest that snoring may not be a trivial symptom because it may be indicative of a more serious sleep disorder such as sleep apnea. Physicians should take the symptom seriously, particularly among populations that are at increased risk of injury in the workplace.
The present study had three important results. First, we identified a modest prevalence of physician-diagnosed sleep apnea in an occupational cohort in which the true prevalence is likely much higher. Second, we observed that a large percentage of the sleep disorder cases had loud snoring only, without a physician diagnosis of sleep apnea. We suspect that some of these may represent undiagnosed cases of obstructive sleep apnea, particularly because the loud snoring group shared several characteristics that were similar to the sleep apnea group, as shown in Table 1. Our third and most salient observation was that we identified consistent relationships between loud snoring and the occurrence of various types of farm injury. We did not observe relationships between diagnosed cases of sleep apnea and injury. Our working assumption (admittedly in the absence of treatment data) was that once diagnosed, these cases were being treated.
Our results confirm and extend the observations of others concerning the importance of sleep disorders as predictors of injury in occupational contexts (3–9), and specifically in farm populations (10,11). Impaired sleep has deleterious effects on daytime somnolence and fatigue, both of which leave workers vulnerable to injury (2). Furthermore, sleep loss and fragmented sleep patterns associated with apnea can produce deleterious effects on cognitive function, analogous to those demonstrated in association with shift work (20), which also confer risk on affected workers in occupational contexts.
Our results show that a considerable proportion of persons with sleep disorders on farms report loud snoring, but have not been diagnosed by a physician as having obstructive sleep apnea. Consequences of this situation may be important. Our adjusted risk estimates suggest that persons with snoring (but not diagnosed sleep apnea) experienced consistent elevations in risk for specific types of farm work injury. These relationships were present even after adjustment for multiple covariates, including measures describing typical durations of sleep. When left untreated, sleep disorders that include symptoms of loud snoring alone may lead to higher rates of injury (12). When treated, risks for injury can be reduced (13), and this is also supported by our results for the sleep apnea category. Respondents in our study who reported diagnosed sleep apnea did not experience elevated risks for injury.
Limitations
The limitations of our study warrant comment. Our data did not permit us to explore the relationship between obesity, loud snoring and injury outcomes because body mass index data were unavailable in this cohort. However, even if body mass index data were available and was related to loud snoring, it is still unlikely that obesity itself would have accounted for the observed relationships between loud snoring and injury. Second, our measures of sleep disorders were based on self-reports. We did not obtain more conventional measures of the effects of sleep disorders such as daytime somnolence inferred from Epworth Sleepiness Scale scores (21,22). We did not validate the self-reports of physician-diagnosed sleep apnea. We recognize that our self-reported measures could be subject to misclassification that might attenuate associations. Finally, our results may not be generalizable beyond the farm occupational environments in the grain and cattle growing areas of Saskatchewan.
CONCLUSION
Collectively, our study results suggest that prevention efforts should be focused on the identification and clinical management of sleep disorders in farm populations and that the single symptom of loud snoring may be a useful marker in this regard. Workers who present to primary care with the symptom of snoring should be suspected of having obstructive sleep apnea. This would be particularly true of cases in which snoring is associated with daytime somnolence as measured by a high Epworth Sleepiness Scale score. The latter should be readily available to clinicians for use in their medical practice. We also need to understand more about barriers to diagnosis of sleep disorders, including perceived stigma associated with snoring and lack of access to respiratory medicine specialists and diagnostic care in rural areas. These should be amenable to intervention and should remain a focus of clinical research and associated health policy efforts.
Acknowledgments
The authors thank Phyllis Snodgrass, Iris Rugg, Deborah Emerton, Lynette Epp, Murray Purcell, Debra Gronning, Louise Singer, Suzanne Dostaler, Matthew King and Catherine Isaacs, as well as the Saskatchewan Association of Rural Municipalities, the 50 participating Saskatchewan rural municipal councils and the farm families from Central Saskatchewan who took the time to assist us with this research. The cohort and this analysis was supported financially in part by a research agreement with the Canadian Institutes of Health Research (Operating Grant: MOP-145294) and a pilot study grant from the Canadian Centre for Health and Safety in Agriculture (also funded by the Canadian Institutes of Health Research, Operating Grant CDA-66151).
Footnotes
SASKATCHEWAN FARM INJURY COHORT STUDY TEAM: William Pickett phd and James Dosman md (co-principal investigators), Louise Hagel msc, Robert Brison md, Barbara Marlenga phd, Lesley Day phd, Punam Pahwa phd, Andrew G Day msc, Xiaoqun Sun msc, Niels Koehncke md, Trever Crowe phd and Donald C Voaklander phd.
REFERENCES
- 1.Bresnitz EA, Goldberg R, Kosinski RM. Epidemiology of obstructive sleep apnea. Epidemiol Rev. 1994;16:210–27. doi: 10.1093/oxfordjournals.epirev.a036151. [DOI] [PubMed] [Google Scholar]
- 2.Johnson JT, Gluckman JL, Sanders MH, editors. Management of Obstructive Sleep Apnea. London: Martin Dunitz; 2002. [Google Scholar]
- 3.Howard JE, Desai AV, Grunstein FF, et al. Sleepiness, sleep-disordered breathing, and accident risk factors in commercial vehicle drivers. Am J Respir Crit Care Med. 2004;170:1014–21. doi: 10.1164/rccm.200312-1782OC. [DOI] [PubMed] [Google Scholar]
- 4.Lindberg E, Carter N, Gislason T, Janson C. Role of snoring and daytime sleepiness in occupational accidents. Am J Respir Crit Care Med. 2001;164:2031–5. doi: 10.1164/ajrccm.164.11.2102028. [DOI] [PubMed] [Google Scholar]
- 5.Teran-Santos J, Jimenez-Gomez A, Cordero-Guevara J. The association between sleep apnea and the risk of traffic accidents. N Engl J Med. 1999;340:847–51. doi: 10.1056/NEJM199903183401104. [DOI] [PubMed] [Google Scholar]
- 6.Chau N, Mur JM, Benamghar L, et al. Relationships between some individual characteristics and occupational accidents in the construction industry: A case-control study on 880 victims of accidents occurred during a two-year period. J Occup Health. 2002;44:131–9. [Google Scholar]
- 7.Ulfberg J, Carter N, Edling C. Sleep-disordered breathing and occupational accidents. Scand J Work Environ Health. 2000;26:237–42. doi: 10.5271/sjweh.537. [DOI] [PubMed] [Google Scholar]
- 8.Carter N, Ulfberg J, Nystrom B, Edling C. Sleep debt, sleepiness and accidents among males in the general population and male professional drivers. Accid Anal Prev. 2003;35:613–17. doi: 10.1016/s0001-4575(02)00033-7. [DOI] [PubMed] [Google Scholar]
- 9.Akerstedt R, Fredlund P, Gillberg M, Jansson B. A prospective study of fatal occupation accidents – relationship to sleeping difficulties and occupational factors. J Sleep Res. 2002;11:69–71. doi: 10.1046/j.1365-2869.2002.00287.x. [DOI] [PubMed] [Google Scholar]
- 10.Spengler SE, Browning SR, Reed DB. Sleep deprivation and injuries in part-time Kentucky farmers: Impact of self reported sleep habits and sleep problems on injury risk. AAOHN J. 2004;52:373–82. [PubMed] [Google Scholar]
- 11.Heaton K, Azeuro A, Reed D. Obstructive sleep apnea indicators and injury in older farmers. J Agromedicine. 2010;15:148–56. doi: 10.1080/10599241003636020. [DOI] [PubMed] [Google Scholar]
- 12.Horstman S, Hess CW, Bassetti C, Gugger M, Mathis J. Sleepiness-related accidents in sleep apnea patients. Sleep. 2000;23:383–9. [PubMed] [Google Scholar]
- 13.Melamed S, Oksenberg A. Excessive daytime sleepiness and risk of occupational injuries in non-shift daytime workers. Sleep. 2002;25:315–22. doi: 10.1093/sleep/25.3.315. [DOI] [PubMed] [Google Scholar]
- 14.LaBrash LF, Pahwa P, Hagel LM, Snodgrass PR, Dosman JA, Pickett W, for the Saskatchewan Farm Injury Cohort Study Team Relationship between sleep loss and economic worry among farmers: A survey of 94 active Saskatchewan noncorporate farms. J Agromedicine. 2008;13:149–54. doi: 10.1080/10599240802371862. [DOI] [PubMed] [Google Scholar]
- 15.Canadian Agricultural Injury Surveillance Program. Agricultural injuries in Canada for 1990–2005. Kingston (ON): Queen’s University; ISBN 978-0-9784872-3-2. [Google Scholar]
- 16.Pickett W, Day L, Hagel L, et al. The Saskatchewan farm injury cohort: Rationale and methodology. Public Health Rep. 2008;123:567–75. doi: 10.1177/003335490812300506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Voaklander DC, Dosman JA, Hagel LM, Warsh J, Pickett W. Farm work exposure of older male farmers in Saskatchewan. Am J Ind Med. 2010;53:706–15. doi: 10.1002/ajim.20811. [DOI] [PubMed] [Google Scholar]
- 18.Pickett W, Brison RJ, Niezgoda H, Chipman ML. Nonfatal farm injuries in Ontario: A population based survey. Accid Anal Prev. 1995;27:425–33. doi: 10.1016/0001-4575(94)00080-6. [DOI] [PubMed] [Google Scholar]
- 19.Anderson P, Cremona A, Paton A, Turner C, Wallace P. The risk of alcohol. Addiction. 1993;88:1493–508. doi: 10.1111/j.1360-0443.1993.tb03135.x. [DOI] [PubMed] [Google Scholar]
- 20.Kling RN, McLeod CB, Koehoorn M. Sleep problems and workplace injuries in Canada. Sleep. 2010;33:611–8. doi: 10.1093/sleep/33.5.611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.John MW. A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep. 1991;14:540–45. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 22.Nguyen AR, Baltzon MA, Small D, Wokove N, Gillian S, Palayew M. Clinical reproducibility of the Epworth Sleepiness Scale. J Clin Sleep Med. 2006;2:170–4. [PubMed] [Google Scholar]


