Abstract
Background
Recently, instruments for the measurement of wavefront aberration in the living human eye have been widely available for clinical applications. Despite the extensive background experience on wavefront sensing for research purposes, the information derived from such instrumentation in a clinical setting should not be considered a priori precise. We report on the variability of such an instrument at two different pupil sizes.
Methods
A clinical aberrometer (COAS Wavefront Scienses, Ltd) based on the Shack-Hartmann principle was employed in this study. Fifty consecutive measurements were perfomed on each right eye of four subjects. We compared the variance of individual Zernike expansion coefficients as determined by the aberrometer with the variance of coefficients calculated using a mathematical method for scaling the expansion coefficients to reconstruct wavefront aberration for a reduced-size pupil.
Results
Wavefront aberration exhibits a marked variance of the order of 0.45 microns near the edge of the pupil whereas the central part appears to be measured more consistently. Dispersion of Zernike expansion coefficients was lower when calculated by the scaling method for a pupil diameter of 3 mm as compared to the one introduced when only the central 3 mm of the Shack – Hartmann image was evaluated. Signal-to-noise ratio was lower for higher order aberrations than for low order coefficients corresponding to the sphero-cylindrical error. For each subject a number of Zernike expansion coefficients was below noise level and should not be considered trustworthy.
Conclusion
Wavefront aberration data used in clinical care should not be extracted from a single measurement, which represents only a static snapshot of a dynamically changing aberration pattern. This observation must be taken into account in order to prevent ambiguous conclusions in clinical practice and especially in refractive surgery.
Background
Since the application of excimer laser technology for the correction of eye's simple refractive errors (i.e. defocus and astigmatism), there has been a considerable debate concerning the visual impact of correcting the higher order monochromatic aberrations of the eye (e.g. spherical aberration, coma and secondary astigmatism), which also degrade retinal image quality [1-4]. Advances in the measurement of the eye's wave aberration have led to the emergence of sophisticated instrumentation for the clinical evaluation of the ocular higher-order aberrations. In general, these devices typically represent the aberrations as a wavefront-error map at the corneal or pupil plane.
Among other subjective and objective techniques which are now available for measuring ocular aberrations (e.g. the Spatially Resolved Refractometer (SRR)[5,6], the Tscherning aberrometer[7] and the Retinal ray-tracing[8], Shack-Hartmann based instruments [9-11] have become the most widely adopted. Aberrometry is rapidly making its way into the clinic and has already been applied in measuring aberrations of normal[12,13] or clinically abnormal eyes (eg dry, keratoconic) [14-16], eyes undergone refractive surgery [17-20], as well as in situ aberration structures of soft and RGP contact lenses [21,22] and intraocular lenses (IOLs)[23,24].
Recently, the clinical measurement of higher-order aberrations has become important for patient care. There is currently a major ongoing effort to refine laser refractive surgery, with the aim to eliminate higher order aberrations. In principle, wavefront aberration is measured using devices such as the Hartmann-Shack wavefront sensor. This information is then fed to a computer that generates the excimer laser's scanning pattern to allow simple refractive errors as well as higher order aberrations to be corrected. Preliminary results are still tentative as no clinically significant difference between conventional and wavefront-guided ablations has been demonstrated[17,25-27].
Moreover, there have been studies using state-of-the-art aberrometers to evaluate the refractive state[12,13,28] and the accommodative response[29,30] of the human eye. Therefore, an obvious requirement of each of these devices is accuracy and repeatability of the measurement of the low order (sphero-cylindrical error) as well as the higher-order aberrations of the eye. Several studies have addressed the accuracy and the repeatability of static measurements of wavefront aberration[10,11,31,32]. These studies have shown that, although there is some variation arising from a combination of misalignment errors and small drifts in the measuring equipment, these are well beyond the clinicians' normal operation range. However, the use of a single measurement of the wavefront error in the planning of a custom correction is not recommended[32].
In this study, we used a clinical aberrometer to evaluate the variability of low and higher order aberrations at different pupil sizes, since no standard pupil has been established for reporting ocular aberrations. Morever, we compared the variance of individual Zernike coefficients as determined by the aberrometer with the variance of coefficients calculated with a matrix method that reconstructs a new set of expansion coefficients appropriate for any reduced-size pupil.
Methods
Subjects
Four right eyes of four subjects aged between 23 and 33 years (mean age: 29.2 years) were tested. One subject was emmetropic (AP: plano), two were low myopes (SP: -2.00 / -0.25 × 30, HG: -1.75 / -1.25 × 86), and one was an intermediate myope (OL: -4.75 / -0.25 × 10). None of the subjects had any ocular pathology or had undergone any kind of refractive surgery. Subjects were familiarised with the measurements. Prior to data collection, institutional research board approval was obtained.
Instrumentation
The monochromatic aberration function of the eye was measured using the Complete Ophthalmic Analysis System (COAS, Wavefront Sciences Ltd), which is based on the Shack-Hartmann principle as described elsewhere[9]. COAS also provides a real time display of the pupil image, which is used to objectively measure pupil size to the nearest 0.1 mm. COAS uses an 840 nm infrared super-luminescent diode as the light source and utilises a square lenslet array of 33 × 44 (a total of 1452 lenslets). The diameter of each lenslet is 144 μm. According to the manufacturers the pupil magnification factor is about 0.685, which means that the lenslet array samples the exiting wavefront every 210 μm in the pupil plane. This allows approximately 600 sample points within a 6.0 mm diameter pupil (150 sample point within a 3.0 mm diameter pupil), providing very high resolution sampling of the aberration. The software allows continuous recording of Shack – Hartmann images and pupil size with an exposure time of about 130 ms for each frame capture, i.e. a temporal frequency of 7.7 Hz. The data extracted from COAS, consist of a set of Zernike coefficients (up to 4th order) in Malacara format, that quantify the type and the magnitude of aberrations present. The ordering of Zernike coefficients was transposed to the format recommended by the Optical Society of America (OSA)[33].
Procedure
All measurements were performed on natural pupils without the use of any dilating or cycloplegic drug. Room illuminance was set at mesopic light levels. Large pupil analysis was based on the full pupil, which, at these lighting conditions, varied for each subject (ranged between 4.5 and 7.1 mm). The subject positioned his head on the chin rest and fixated on the centre of a circular grid. The operator manually aligned the subject's pupil centre with the optical axis of the device by means of six dots (that lie on a circle concentric with the pupil) displayed on a video monitor. This ensured that subject's line-of-sight was coaxial with the instrument's optical axis. A series of fifty consecutive measurements (total recording time 6.5 sec) for each eye were taken for the full pupil without re-alignment. Subjects were asked to blink prior to the measurement. In addition to subjects, we measured the wave aberration of an artificial eye supplied by the manufacturer as a test object.
Data analysis
Data analysis was performed using MATLAB (V 5.2, The Mathworks, Inc Natick, MA) mathematical software. The Zernike expansion coefficients derived from the wave inclination data for the full pupil, were initially transposed to the OSA format and then corrected for chromatic aberration (from 840 to 550 nm) (see Appendix A).
The corrected coefficients were "scaled" to a smaller pupil diameter (3 mm) using two different techniques: (i) the "direct" technique (the standard employed by COAS software), which re-calculated Zernike expansion coefficients (up to 4th order) after discarding the Shack-Hartmann image outside the 3 mm zone (ii) the "scaling" technique, which uses a matrix method to reconstruct a new set of Zernike coefficients that describe a wavefront aberration corresponding to the central 3 mm of the pupil using all available raw data. To achieve this, we used formulas developed by Schwiegerling[34] implemented in a MATLAB file, as previously described by Campbell[35].
Figure 1 depicts wavefront difference map of the central 3 mm of the full-size pupil and the calculated central 3 mm as obtained by the "direct" and the "scaling" methods. It is evident that the difference map for the "scaling" method is practically zero for every point of the entrance pupil. In contrast, the "direct" method produces a map that does not correspond closely to the initial data. Apparently, the calculated Zernike polynomial coefficients are different when peripheral data points are discarded.
Figure 1.
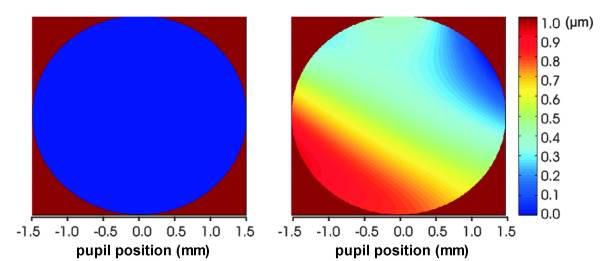
Difference maps. Wavefront aberration difference maps between the central 3 mm pupil of the full-size pupil and the re-calculated central 3 mm as obtained by the "scaling" (left) and "direct" (right) methods. The vertical colour bar on the right shows corresponding wavefront aberration error in micrometers.
Results
Variance of the wave aberration data for the full-size pupil
Prior to the presentation of the results for the scaled pupils it is of interest to report on the variance of the raw wavefront aberration data (50 measurements) for the full-size pupil of each subject. Figure 2 illustrates the spatial distribution of the standard deviation of the measured wavefront aberration as a function of pupil position.
Figure 2.
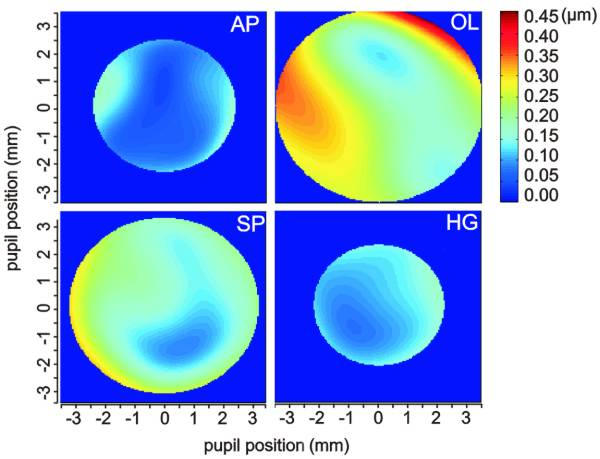
Colour patterns of wavefront aberration at full-size pupils. Colour patterns of the standard deviation of the wavefront error as a function of horizontal (x) and vertical (y) pupil position for the full-size pupils of the four subjects tested. Map size is 150 × 150 pixels.
It is obvious that wavefront aberration variance at peripheral points of the pupil and especially near the edge of the pupil, is increased. Reasonably, this effect is more pronounced for subjects OL and SP having larger pupil diameters.
Comparison of the two scaling methods
Figure 3 shows the variation with time of Zernike expansion coefficients C20 and C40, determined for a pupil diameter of 3 mm. The upper graphs correspond to fifty consecutive measurements made on an artificial eye. There is little doubt that discarding peripheral pupil data points in the "direct" method does not affect the variance of the low order coefficient, C20. However, it does introduce noise to the value determined for the higher order coefficient, C40. On the other hand, the "scaling" method produces minimal noise in both coefficients. It is noteworthy that noise introduced by the direct method is not observed in the coefficients corresponding to the large pupil.
Figure 3.
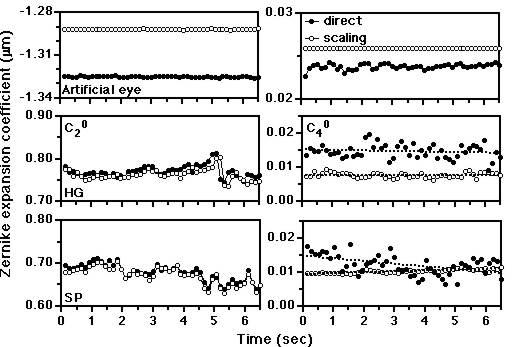
Variation of aberration coefficients C20 and C40 with time. Variation of wavefront aberration coefficient C20 (left) and C40 (right) with time for a 3 mm pupil as calculated by the direct (filled symbols) and scaling (open symbols) methods. Data from an artificial eye (upper graphs) and two subjects are shown. The dotted lines are least-square regression coefficients. Note, that the scaling of y axis is different for the artificial eye.
The two lower graphs depict similar plots for two of the subjects tested. The variance for the C20 is much higher in this case, as would be expected due to the dynamic nature of the human eye. Moreover, note that there is no difference between the two methods, which also supports the above statement. For the 4th order term, the "scaling" method improves substantially the dispersion of the coefficient. Similar improvement in the variability of all higher order aberration coefficients is observed when the scaling method is applied for the calculation at 3 mm pupil.
Another point worth mentioning is that a drift in the value of the C40 with time indicated by the direct method (see subject SP) may be ambiguous, as this is not the case when the scaling method is used. Moreover, there is no evidence of change of any aberration coefficient with time, as no statistically significant correlation can be established. This implies that during time period of the recordings (6.5 sec) needed to capture the fifty measurements, subjects maintained fixation and wavefront changes related to the tear film quality as well as accommodation state did not interfere significantly with the estimated dispersion.
Figures 4a and 4b show frequency histograms of the spherical aberration coefficient (C40) and the higher-order RMS error for all subjects tested. It is clear from these data that the dispersion of the values is wider when the direct method is used, where as the scaling method calculates coefficients with higher variability. Furthermore, there is an obvious difference in the mean value, with a trend of the direct method to overestimate the amount of the wavefront error.
Figure 4.
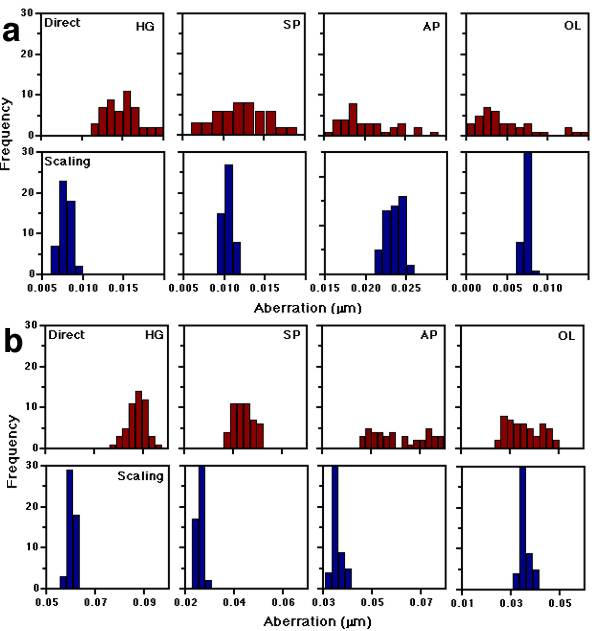
Frequency histograms of C40 and higher-order RMS error. (a) Frequency histograms of the spherical aberration coefficient, C40 for all subjects tested. Comparison between results derived from the direct (upper) and scaling (lower) methods for a 3 mm pupil. Bin width is 0.001. (b) Frequency histograms of the higher-order RMS error for all subjects tested. Comparison between results derived from the direct (upper) and scaling (lower) methods for a 3 mm pupil. Bin width is 0.0025.
Impact of error on different aberration terms and radial orders
Figure 5 presents signal-to-noise (S/N) ratio charts (mean / SD) for different radial orders of the wavefront aberration for all subjects tested. High S/N values imply high variability of the measured order of aberration. For example, subject's HG 2nd order terms are measured to have a value about thirty times higher than their standard deviation (noise level), whereas the magnitude of the 4th order terms is only five times higher than the standard deviation. There are three points to note from these data. First, the signal-to-noise ratios are much higher for the 2nd order compared to the higher-order coefficients for all the subjects. Second, there is some substantial variation between subjects for the 2nd order coefficients, while this is not the case for the higher order terms. This is mainly due to the fact that the amount of the sphero-cylindrical error (determining the 2nd order terms) varies between the subjects, while there is little variation in the magnitude of 3rd and 4th order coefficients. Third, the scaling method improves the signal-to-noise ratio in all cases, but this is more profound in the higher-order terms, as also displayed in figure 3.
Figure 5.
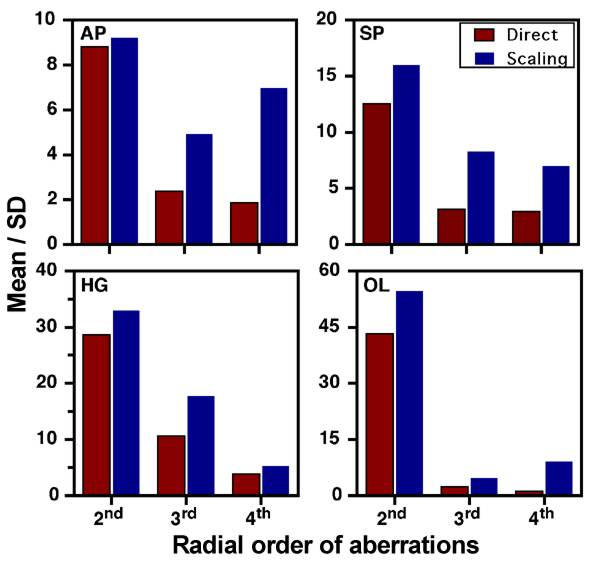
Signal-to-noise ratios for different radial order. Signal-to-noise ratios (mean / SD) for different radial orders of the wavefront aberration at 3 mm pupil as calculated by the direct and scaling methods. Data for all subjects are shown.
The improvement of S/N for each expansion coefficient is depicted in figure 6, which uses the standard graph that describes the radial and angular modes of the Zernike polynomial expansion. Determination of coefficients having values smaller than two times the noise level, (S/N < 2) are below the detection limit, regarded imprecise and are therefore displayed by red color. This graph corresponds to measurements of subject OL. We derived similar results for the other subjects.
Figure 6.
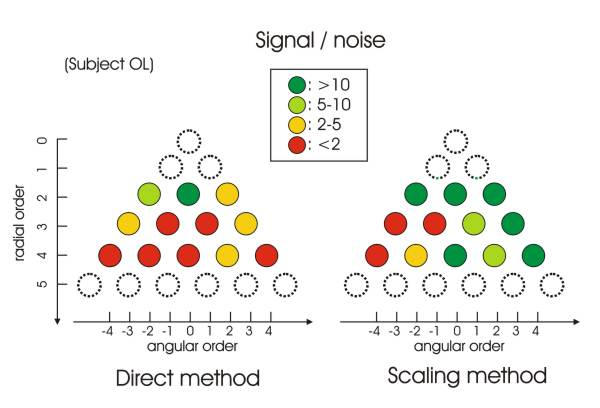
Signal-to-noise ratio for individual Zernike coefficients. Signal-to-noise (S/N) ratio in the standard pyramidical layout of Zernike expansion coefficients for one subject (OL) as calculated by the two methods. Green colours show high S/N ratio, red colours show low S/N ratio.
Discussion
The aim of this study was to use a Shack-Hartmann clinical aberrometer (COAS, Wavefront Sciences Ltd) to evaluate the variability of low- and higher-order aberration measurement of the eye. Using the wave aberration polynomial determined for a full-size pupil we compared the Zernike expansion coefficients for a smaller, 3 mm pupil derived by two methods: first, by re-calculating the wave aberration coefficients to the reduced sampled points corresponding to that pupil ("direct" method), and, second, by using a matrix method to reconstruct a new set of coefficients appropriate for the reduced pupil ("scaling" method) (see figure 1).
Our results suggest that, for full-size pupil, the efficiency of the measurements varies across x and y pupil position: where the wavefront is larger, measurement variance is higher, especially near the margins of the pupil, where increased standard deviation results to higher wave-aberration error. Some of this increased variance may have been due to poorer image quality in parts of the Shack-Hartmann images[36]. Also, it may be partially attributed to the fact that saccadic movements, during the time required for data collection, lead to alignment errors that continuously change the set of sensor elements contributing to wavefront sensing. Although such displacements in respect to the optical axis of the instrument cannot justify significant fluctuations of the wavefront aberration[37], we cannot exclude the possibility that the algorithm employed in COAS software may generate the increased noise in periphery during wavefront expansion, since pupil translation magnitude (~100 μm) is comparable to lenslet array spacing (as magnified by the conjugating optics) in the particular instrument.
The increased standard deviation of wavefront aberration at the periphery has implications in calculating wavefront-guided ablation patterns. An error of 0.45 μm in the measured wavefront aberration at the periphery of the treatment zone may lead to a substantial error in the calculated shot pattern depending on the laser beam delivery (scanning) method as well as beam parameters and compensation for corneal curvature[38].
As pupil becomes smaller, the magnitude of wavefront aberrations decreases. At 3 mm pupil, the "direct" method (employed by COAS) induces considerable variance in the measurement of higher-order aberration coefficients attributed to inherent fitting error. This results from the small number of sensor elements involved in the wavefront inclination measurement. Moreover, there is a clear shift in the magnitude of each coefficient to higher values, which may lead to inaccurate determination of higher-order terms. In contrast, the "scaling" method produces coefficients of higher variability, and this is not surprising since it allows the use of the information from a larger set of sensor elements, reducing instrument noise.
On the other hand, second-order terms, and especially C20, are measured with higher variability (see figure 5), and this is an interesting feature as the coefficients C20, C2-2, C2+2 can be used in the calculation of the conventional sphero-cylindrical correction[33]. This observation, in conjuction with the high accuracy of the refraction estimated objectively from wavefront aberration data when small (~3 mm) pupils are used[13,39,40], is of considerable importance, as this means that the COAS clinical aberrometer may be used as a reliable and accurate autorefractor. However, care must be taken when large pupils are tested, as the objective estimation of refractive error may lead to ambiguous results, due to the influence of higher-order aberrations on the determination of correction[40,41].
Another finding is that the variability of C20 (corresponding to defocus) improves only slightly when the "scaling" method is used. This probably occurs because the defocus term is mostly contained in the Shack-Hartmann spots at the centre of pupil. In contrast, spherical aberration, for example, depends on the 4th power of pupil radius, which means that most of the information is outside the central 3 mm and what is measured with a small pupil is mostly noise. Another reason may be the fact that the variance in C20 is not related to the inherent noise of the instrument itself, but to the dynamic characteristics of the human visual system, such as accommodation micro-fluctuations[42,43], tear film changes[44], and eye movements leading to alignment errors[32,45].
Although instruments based on the Shack – Hartmann sensor have been extensively validated for experimental work[11,13,31,32,40], our results indicate that special care should be taken when measurement of aberration is used in clinical applications, such as refractive surgery, either decision making or outcome evaluation. The diversity of the measured values of various coefficients suggest that a number of measurements should be taken and averaged for each subject in order to calculate coefficients of higher efficiency[32]. This is of major importance in customized laser surgery, where aberration data are used to correct higher-order aberrations for the potential enhancement of visual performance [46-48].
Conclusions
Wavefront aberration of the eye, as derived from Shack-Hartmann images is determined with a certain degree of accuracy that varies considerably with pupil position. Zernike expansion coefficients are determined with less accuracy when re-calculated at "cropped" pupils with the use of the algorithm employed in COAS. This study shows that these errors attributed to the reduced number of sensor elements could be, at least partially, overcome using an appropriate algorithm that calculates the aberration coefficients for smaller pupils based on full-size pupil set of data. Moreover, micro – fluctuations observed in the C20 corresponding to defocus, are probably inherent characteristics of the eye and therefore show no improvement when the algorithm is applied.
Consequently, it must be emphasised that wavefront aberration data used in clinical care should not be extracted from a single measurement, which represents only a static snapshot of a dynamically changing aberration pattern.
Appendix A
Correcting Zernike coefficients for chromatic aberration
All Zernike coefficients, except the coefficient of defocus (C20), were adjusted to appropriate values for 550 nm, using a chromatic correction factor, K (equation 1):
K = (n1-1)/(n2-1) (1)
Where n1 and n2 are the refractive index values for 550 nm and 840 nm, respondingly. These were calculated using equation 2[49], where the wavelength λ is written in nm.
nλ = 1.320535 - (4.685/ (λ - 214.102)) (2)
The C20 was corrected for wavelength, using equations (3) and (4). This is necessary because infrared light used for measurements is not reflected from the photoreceptors plane, where the subjective focal plane lies, but passes through to deeper layers and is reflected from the choroid[50]. Equation (3) calculates the spherical equivalent power corrected at 550 nm (S550), assuming that the 840-nm light is reflected from a plane 0.125 mm posterior to the retina of a 60D model eye (with a focal length of 16.667 mm). Equation (4) is used to derive C20 (in OSA format) from the spherical equivalent (S) for a specific pupil diameter (d) at each wavelength.
![]()
![]()
Competing interests (medicine)
None declared.
Authors' contributions
HG participated in data analysis, manuscript preparation and study design. SP carried out measurements, performed data analysis and participated in manuscript and figure preparation. AP performed wavefront measurements, implemented the MATLAB code, participated in figure preparation and created the attached computer program. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Supplementary Material
This zip file containes two MATLAB (v 5.2) files used for Zernike coefficient scaling to different pupil sizes. To run these files, MATLAB needs to be installed. This was tested for versions 5.2 for Macintosh and 6.1 for windows. Instructions for use as well as author credits are included in the files.
This zip file contains three files that form a Windows utility (an executable) used for Zernike coefficient scaling. Instructions for use, as well as author credits and a disclaimer, are included in the files.
Acknowledgments
Acknowledgements
This work was supported by the EU, through the Research Training Network "Adaptive optics for retinal imaging and improved vision" under contract number HPRN-CT-2002-00301. Authors would like to thank Oleksandr Lutsenko for his involvement in data acquisition and Professor Ioannis Pallikaris for his valuable comments.
Contributor Information
Harilaos S Ginis, Email: ginis@med.uoc.gr.
Sotiris Plainis, Email: plainis@med.uoc.gr.
Aristophanis Pallikaris, Email: apallik@med.uoc.gr.
References
- Ivanoff A. About the spherical aberration of the eye. Journal of the Optical Society of America. 1956;46:901–903. doi: 10.1364/josa.46.0901_1. [DOI] [PubMed] [Google Scholar]
- Jenkins TCA. Aberrations of the human eye and their effects on vision: Part I. British Journal of Physiological Optics. 1963;20:59–91. [PubMed] [Google Scholar]
- Charman WN. The retinal image in the human eye. Progress in Retinal and Eye Research. 1983;2:1–50. doi: 10.1016/0278-4327(83)90002-0. [DOI] [Google Scholar]
- Guirao A, Porter J, Williams DR, Cox IG. Calculated impact of higher-order monochromatic aberrations on retinal image quality in a population of human eyes. Journal of the Optical Society of America a-Optics Image Science and Vision. 2002;19:1–9. doi: 10.1364/josaa.19.000001. [DOI] [PubMed] [Google Scholar]
- Webb RH, Penney CM, Sobiech J, Staver PR, Burns SA. SSR (spatially resolved refractometer): a null-seeking aberrometer. Applied Optics. 2003;42:736–744. doi: 10.1364/ao.42.000736. [DOI] [PubMed] [Google Scholar]
- Burns SA. The spatially resolved refractometer. Journal of Refractive Surgery. 2000;16:S566–S569. doi: 10.3928/1081-597X-20000901-15. [DOI] [PubMed] [Google Scholar]
- Mrochen M, Kaemmerer M, Mierdel P, Krinke HE, Seiler T. Principles of Tscherning aberrometry. Journal of Refractive Surgery. 2000;16:S570–S571. doi: 10.3928/1081-597X-20000901-16. [DOI] [PubMed] [Google Scholar]
- Pallikaris IG, Panagopoulou SI, Molebny VV. Evaluation of TRACEY technology for total eye refraction mapping. Reproducibility tests. Investigative Ophthalmology & Visual Science. 2000;41:1588B1963. [Google Scholar]
- Thibos LN. Principles of Hartmann-Shack aberrometry. Journal of Refractive Surgery. 2000;16:S563–S565. doi: 10.3928/1081-597X-20000901-14. [DOI] [PubMed] [Google Scholar]
- Hament WJ, Nabar VA, Nuijts R. Repeatability and validity of Zywave aberrometer measurements. Journal of Cataract and Refractive Surgery. 2002;28:2135–2141. doi: 10.1016/S0886-3350(02)01333-0. [DOI] [PubMed] [Google Scholar]
- Cheng X, Himebaugh NL, Kollbaum PS, Thibos LN, Bradley A. Validation of a clinical Shack-Hartmann aberrometer. Optometry and Vision Science. 2003;80:587–595. doi: 10.1097/00006324-200308000-00013. [DOI] [PubMed] [Google Scholar]
- Cheng X, Bradley A, Hong X, Thibos LN. Relationship between refractive error and monochromatic aberrations of the eye. Optometry and Vision Science. 2003;80:43–49. doi: 10.1097/00006324-200301000-00007. [DOI] [PubMed] [Google Scholar]
- Salmon TO, West RW, Gasser W, Kenmore T. Measurement of refractive errors in young myopes using the COAS Shack-Hartmann aberrometer. Optometry and Vision Science. 2003;80:6–14. doi: 10.1097/00006324-200301000-00003. [DOI] [PubMed] [Google Scholar]
- Thibos LN, Hong X, Bradley A, Begley C. Deterioration of retinal image quality due to breakup of the corneal tear film. Investigative Ophthalmology & Visual Science. 1999;40:2875B2750. [Google Scholar]
- Hori Y, Maeda N, Kuroda T, Koh S, Nishida K, Watanabe H, Inoue Y, Tano Y, Mihashi T. Measurement of wavefront aberrations in the patients with dry eye. Investigative Ophthalmology & Visual Science. 2001;42:189. doi: 10.1167/iovs.07-0762. [DOI] [PubMed] [Google Scholar]
- Munson K, Hong X, Thibos LN. Use of a Shack-Hartmann aberrometer to assess the optical outcome of corneal transplantation in a keratoconic eye. Optometry and Vision Science. 2001;78:866–871. doi: 10.1097/00006324-200112000-00008. [DOI] [PubMed] [Google Scholar]
- Mrochen M, Kaemmerer M, Mierdel P, Seiler T. Increased higher-order optical aberrations after laser refractive surgery – A problem of subclinical decentration. Journal of Cataract and Refractive Surgery. 2001;27:362–369. doi: 10.1016/S0886-3350(00)00806-3. [DOI] [PubMed] [Google Scholar]
- Moreno-Barriuso E, Merayo-Lloves JM, Marcos S, Navarro R. Ocular aberrations after refractive surgery measured with a laser ray tracing technique. Investigative Ophthalmology & Visual Science. 2000;41:1601B1976. [PubMed] [Google Scholar]
- Moreno-Barriuso E, Lloves JM, Marcos S, Navarro R, Llorente L, Barbero S. Ocular aberrations before and after myopic corneal refractive surgery: LASIK-induced changes measured with laser ray tracing. Investigative Ophthalmology & Visual Science. 2001;42:1396–1403. [PubMed] [Google Scholar]
- Panagopoulou SI, Pallikaris IG. Wavefront customized ablations with the WASCA Asclepion workstation. Journal of Refractive Surgery. 2001;17:S608–S612. doi: 10.3928/1081-597X-20010901-21. [DOI] [PubMed] [Google Scholar]
- Lu F, Mao XJ, Qu J, Xu D, He JC. Monochromatic wavefront aberrations in the human eye with contact lenses. Optometry and Vision Science. 2003;80:135–141. doi: 10.1097/00006324-200302000-00009. [DOI] [PubMed] [Google Scholar]
- Dietze HH, Cox MJ. On- and off-eye spherical aberration of soft contact lenses and consequent changes of effective lens power. Optometry and Vision Science. 2003;80:126–134. doi: 10.1097/00006324-200302000-00008. [DOI] [PubMed] [Google Scholar]
- Miller JM, Anwaruddin R, Straub J, Schwiegerling J. Higher order aberrations in normal, dilated, intraocular lens, and laser in situ keratomileusis corneas. Journal of Refractive Surgery. 2002;18:S579–S583. doi: 10.3928/1081-597X-20020901-16. [DOI] [PubMed] [Google Scholar]
- Guirao A, Redondo M, Geraghty E, Piers P, Norrby S, Artal P. Corneal optical aberrations and retinal image quality in patients in whom monofocal intraocular lenses were implanted. Archives of Ophthalmology. 2002;120:1143–1151. doi: 10.1001/archopht.120.9.1143. [DOI] [PubMed] [Google Scholar]
- Pallikaris IG, Kymionis GD, Panagopoulou SI, Siganos CS, Theodorakis MA, Pallikaris AI. Induced optical aberrations following formation of a laser in situ keratomileusis flap. Journal of Cataract and Refractive Surgery. 2002;28:1737–1741. doi: 10.1016/S0886-3350(02)01507-9. [DOI] [PubMed] [Google Scholar]
- Nuijts R, Nabar VA, Hament WJ, Eggink F. Wavefront-guided versus standard laser in situ keratomileusis to correct low to moderate myopia. Journal of Cataract and Refractive Surgery. 2002;28:1907–1913. doi: 10.1016/S0886-3350(02)01511-0. [DOI] [PubMed] [Google Scholar]
- Nagy ZZ, Palagyi-Deak I, Kovacs A, Kelemen E, Forster W. First results with wavefront-guided photorefractive keratectomy for hyperopia. Journal of Refractive Surgery. 2002;18:S620–S623. doi: 10.3928/1081-597X-20020901-24. [DOI] [PubMed] [Google Scholar]
- Wang L, Wang N, Koch DD. Evaluation of refractive error measurements of the WaveScan WaveFront system and the Tracey wavefront aberrometer. Journal of Cataract and Refractive Surgery. 2003;29:970–979. doi: 10.1016/S0886-3350(02)01967-3. [DOI] [PubMed] [Google Scholar]
- Pallikaris IG, Panagopoulou SI, Siganos CS, Molebny VV. Objective measurement of wavefront aberrations with and without accommodation. Journal of Refractive Surgery. 2001;17:S602–S607. doi: 10.3928/1081-597X-20010901-20. [DOI] [PubMed] [Google Scholar]
- Ninomiya S, Fujikado T, Kuroda T, Maeda N, Tano Y, Oshika T, Hirohara Y, Mihashi T. Changes of ocular aberration with accommodation. American Journal of Ophthalmology. 2002;134:924–926. doi: 10.1016/S0002-9394(02)01856-1. [DOI] [PubMed] [Google Scholar]
- Prieto PM, Vargas-Martin F, Goelz S, Artal P. Analysis of the performance of the Hartmann-Shack sensor in the human eye. Journal of the Optical Society of America a-Optics Image Science and Vision. 2000;17:1388–1398. doi: 10.1364/josaa.17.001388. [DOI] [PubMed] [Google Scholar]
- Davies N, Diaz-Santana L, Lara-Saucedo D. Repeatability of ocular wavefront measurement. Optometry and Vision Science. 2003;80:142–150. doi: 10.1097/00006324-200302000-00010. [DOI] [PubMed] [Google Scholar]
- Thibos LN, Applegate RA, Schwiegerling JT, Webb R. Report from the VSIA taskforce on standards for reporting optical aberrations of the eye. Journal of Refractive Surgery. 2000;16:S654–S655. doi: 10.3928/1081-597X-20000901-34. [DOI] [PubMed] [Google Scholar]
- Schwiegerling J. Scaling Zernike expansion coefficients to different pupil sizes. Journal of the Optical Society of America a-Optics Image Science and Vision. 2002;19:1937–1945. doi: 10.1364/josaa.19.001937. [DOI] [PubMed] [Google Scholar]
- Campbell CE. Matrix method to find a new set of Zernike coefficients from an original set when the aperture radius is changed. Journal of the Optical Society of America a-Optics Image Science and Vision. 2003;20:209–217. doi: 10.1364/josaa.20.000209. [DOI] [PubMed] [Google Scholar]
- Salmon TO, Thibos LN, Bradley A. Comparison of the eye's wave-front aberration measured psychophysically and with the Shack-Hartmann wave-front sensor. Journal of the Optical Society of America a-Optics Image Science and Vision. 1998;15:2457–2465. doi: 10.1364/josaa.15.002457. [DOI] [PubMed] [Google Scholar]
- Hofer H, Artal P, Singer B, Aragon JL, Williams DR. Dynamics of the eye's wave aberration. Journal of the Optical Society of America a-Optics Image Science and Vision. 2001;18:497–506. doi: 10.1364/josaa.18.000497. [DOI] [PubMed] [Google Scholar]
- Ginis HS, Katsanevaki VJ, Pallikaris IG. Influence of ablation parameters on refractive changes after phototherapeutic keratectomy. Journal of Refractive Surgery. 2003;19:443–448. doi: 10.3928/1081-597X-20030701-11. [DOI] [PubMed] [Google Scholar]
- Thibos LN, Hong X, Bradley A, Cheng X. Statistical variation of aberration structure and image quality in a normal population of healthy eyes. Journal of the Optical Society of America a-Optics Image Science and Vision. 2002;19:2329–2348. doi: 10.1364/josaa.19.002329. [DOI] [PubMed] [Google Scholar]
- Atchison DA, Scott DH, Charman WN. Hartmann-Shack technique and refraction across the horizontal visual field. Journal of the Optical Society of America a-Optics Image Science and Vision. 2003;20:965–973. doi: 10.1364/josaa.20.000965. [DOI] [PubMed] [Google Scholar]
- Guirao A, Cox IG, Williams DR. Method for optimizing the correction of the eye's higher-order aberrations in the presence of decentrations. Journal of the Optical Society of America a-Optics Image Science and Vision. 2002;19:126–128. doi: 10.1364/josaa.19.000126. [DOI] [PubMed] [Google Scholar]
- Charman WN, Heron G. Fluctuations in Accommodation – a Review. Ophthalmic and Physiological Optics. 1988;8:153–164. doi: 10.1111/j.1475-1313.1988.tb01031.x. [DOI] [PubMed] [Google Scholar]
- Winn B, Charman WN, Pugh JR, Heron G, Eadie AS. Perceptual Detectability of Ocular Accommodation Microfluctuations. Journal of the Optical Society of America a-Optics Image Science and Vision. 1989;6:459–462. doi: 10.1364/josaa.6.000459. [DOI] [PubMed] [Google Scholar]
- Himebaugh NL, Thibos LN, Begley CG, Bradley A, Wilson G. Predicting optical effects of tear film break up on retinal image quality using the Shack-Hartmann aberrometer and computational optical modeling. Lacrimal Gland, Tear Film, and Dry Eye Syndromes 3: Basic Science and Clinical Relevance, Pts a & B. 2002;506:1141–1147. doi: 10.1007/978-1-4615-0717-8_160. [DOI] [PubMed] [Google Scholar]
- Applegate RA, Ballentine CS, Roorda A. Is a bite-bar needed for Hartmann-Shack (H/S) wavefront sensing? Investigative Ophthalmology & Visual Science. 2001;42:3243. [Google Scholar]
- Charman WN. Will correction of ocular aberration lead to "super acuity"? CE Optometry. 2001;4:33–36. [Google Scholar]
- Williams DR, Yoon GY, Porter J, Guirao A, Hofer H, Cox I. Visual benefit of correcting higher order aberrations of the eye. Journal of Refractive Surgery. 2000;16:S554–S559. doi: 10.3928/1081-597X-20000901-12. [DOI] [PubMed] [Google Scholar]
- Schwiegerling J. Theoretical limits to visual performance. Survey of Ophthalmology. 2000;45:139–146. doi: 10.1016/S0039-6257(00)00145-4. [DOI] [PubMed] [Google Scholar]
- Thibos LN, Ye M, Zhang XX, Bradley A. The Chromatic Eye – a New Reduced-Eye Model of Ocular Chromatic Aberration in Humans. Applied Optics. 1992;31:3594–3600. doi: 10.1364/AO.31.003594. [DOI] [PubMed] [Google Scholar]
- Elsner AE, Burns SA, Weiter JJ, Delori FC. Infrared imaging of sub-retinal structures in the human ocular fundus. Vision Res. 1996;36:191–205. doi: 10.1016/0042-6989(95)00100-E. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This zip file containes two MATLAB (v 5.2) files used for Zernike coefficient scaling to different pupil sizes. To run these files, MATLAB needs to be installed. This was tested for versions 5.2 for Macintosh and 6.1 for windows. Instructions for use as well as author credits are included in the files.
This zip file contains three files that form a Windows utility (an executable) used for Zernike coefficient scaling. Instructions for use, as well as author credits and a disclaimer, are included in the files.


