Abstract
Background
Spaceflight causes changes in the cardiovascular control system. The aim of this study was to evaluate postflight recovery of linear and nonlinear neural markers of heart rate modulation, with a special focus on day-night variations.
Material/Methods
Twenty-four-hour Holter ECG recordings were obtained in 8 astronauts participating in space missions aboard the International Space Station (ISS). Data recording was performed 1 month before launch, and 5 and 30 days after return to Earth from short- and long-term flights. Cardiovascular control was inferred from linear and nonlinear heart rate variability (HRV) parameters, separately during 2-hour day and 2-hour night recordings.
Results
No remarkable differences were found in the postflight recovery between astronauts from short- and long-duration spaceflights. Five days after return to Earth, vagal modulation was significantly decreased compared to the preflight condition (day: p=0.001; night: p=0.019), while the sympathovagal balance was strongly increased, but only at night (p=0.017). A few nonlinear parameters were reduced early postflight compared to preflight values, but these were not always statistically significant. No significant differences remained after 30 days of postflight recovery.
Conclusions
Our results show that 5 days after return from both short- and long-duration space missions, neural mechanisms of heart rate regulation are still disturbed. After 1 month, autonomic control of heart rate recovered almost completely.
Keywords: microgravitational adaptations, heart rate variability, autonomic regulation, nonlinear dynamics
Background
In astronauts, the human cardiovascular control system is altered due to their long exposure to microgravity. The transition from weightlessness in space to normal gravity on Earth causes, postflight, a decrease in blood and stroke volume and a cardiac and vascular remodeling to maintain blood pressure. The overall result of these physiological adaptations is a reduction in cardiac output and vasoconstrictor reserve, the 2 main contributors to orthostatic intolerance after spaceflight [1]. Although many astronauts experience no physical problems after spaceflight, the literature shows that their heart rate (HR) and autonomic nervous system (ANS) are not completely recovered in the first days after returning to Earth, lasting between 5 days [2] and 25 days [3]. The ANS affects the heart rate by a continuous interaction between the sympathetic and parasympathetic branches.
Heart rate variability (HRV) has proven to be an adequate non-invasive tool to address the autonomic modulation of heart rate by the ANS [4]. This autonomic modulation is often studied by linear parameters, although several nonlinear techniques have been developed since the 1990s. While conventional spectral analysis of HRV provides analytical features of its cyclic variations but fails to show the dynamic properties of heart rate fluctuations, nonlinear methods are typically designed to assess the quality, scaling, and correlation properties. Moreover, it has been shown that the ANS induces the nonlinearity and the possible chaos of normal HRV [5]. An important feature of a healthy cardiovascular system is adaptability, which can be defined as the capacity to respond to unpredictable stimuli. Consequently, a nonlinear behavior would indicate a greater flexibility and less predictability than a linear behavior.
Postflight changes in HR and HRV have been frequently studied by linear parameters. Often, a sympathetic dominance after spaceflight is reported due to a reduced vagal modulation [2,6]. To the best of our knowledge, nonlinear analysis was only applied in 2 previous studies, both using approximate entropy as the measure [7,8]. No significant change after spaceflight was found compared to preflight. Nevertheless, we expect that changes in autonomic heart rate control are not only reflected in linear HRV parameters, but also in the more subtle nonlinear parameters. In particular, we hypothesize a reduction of the nonlinear parameter values shortly after spaceflight, increasing afterwards towards the preflight values. The goal of this study was to investigate how all parts of the autonomic nervous system are influenced when astronauts return to Earth after spaceflight and how it recovers afterwards. We specifically focused on the change in cardiovascular dynamics induced by microgravity by quantifying HRV using nonlinear methods. Additionally, day and night periods were examined separately. The knowledge obtained by HRV can then be used to develop countermeasures that astronauts can use during their space mission to reduce orthostatic intolerance problems.
Material and Methods
Subjects
Eight male astronauts (age: 43.2±4.4 years, height: 1.79±0.04 m, weight: 76.0±12.4 kg, BMI: 23.7±3.7 kg/m2) who went to the International Space Station (ISS) participated in the study. Five were in space for a long-term mission of 6 months, and the other 3 were in space for 10 days during the Odissea, Cervantes, and Delta missions. Each astronaut was measured at 3 different times: preflight (L-30: 1 month before launch), early postflight (R+5: 5 days after return), and late postflight (R+30: 1 month after return). No fixed time schedule was imposed on the astronauts due to several obligations before launch and after return.
The experimental protocol was approved in advance by the local ethics committee and the European Space Agency (ESA) Medical Board. Each subject provided written informed consent before participating. The study complied with the Declaration of Helsinki.
Data collection and preprocessing
Twenty-four-hour ECG recordings were obtained using Holter monitoring (ELA Medical, LCC Plymouth, MN, USA) with a sample rate of 200 Hz on a PC-based platform. Although the measurements were done across 24 hours, 2 blocks of 2 hours (1 for day and 1 for night) were selected to meet the following criteria: (1) no baseline trends, (2) no measurement discontinuities, (3) no movement artifacts, and (4) high-quality R peak detections. As no activity log was available, these blocks were selected based on visual inspection of RR interval trends to exclude periods of physical exercise or other stressful conditions that might affect results. The selection of the 2-hour night recordings was based on the typical stepwise decrease in the heart rate that is present during sleep. In this way, equal data length for the day and night period, as well as for all astronauts, was guaranteed in order to extract consistent, reliable, and comparable HRV parameters. Each heart beat was automatically annotated by SyneTec© software (ELA Medical, MN, USA) delivered with the Holter system: N = normal, A = artifact, C = calibration and V = premature ventricular beats. For each recording, a file containing the consecutive RR intervals with corresponding annotations was exported and checked manually.
Linear HRV parameters
All standard HRV parameters were calculated in agreement with the standards of measurement proposed by the Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology [4]. As time domain measures, we calculated mean RR [ms], SDNN [ms], RMSSD [ms], and pNN50 [%]. After resampling of the tachogram at 4 Hz [9] with the use of a cubic spline approximation [10], power spectra were obtained using the Welch method. The direct current component was removed by subtracting the mean value of each data set. A sliding Hamming window of 1024 points, corresponding to 256 seconds, with 50% overlap was used. Two frequency bands were defined: a low frequency (LF) band from 0.04 to 0.15 Hz and a high frequency (HF) band from 0.16 to 0.40 Hz. The spectral power within each frequency band, as well as the total power (TP), are expressed in absolute values [ms2]. LF and HF power are also given in normalized units [nu], which represent the relative value of each power component in proportion to the total power minus the very low frequency component, defined as below 0.04 Hz. This relative representation minimizes the influence of changes in total power. Additionally, a low-to-high frequency power ratio was calculated to reflect the sympathovagal balance (LF/HF).
Nonlinear HRV parameters
Because nonlinear HRV techniques have not been standardized as much as the linear ones [4], the most commonly used nonlinear parameters were computed. The scaling of a system is quantified by the fractal dimension (FD) and detrended fluctuation analysis (DFA α1 & α2). In order to address the complexity of the signals, sample entropy (SampEn), correlation dimension (CD), and maximal Lyapunov exponents (LE) were calculated.
Fractal dimension (FD)
The fractal dimension describes the planar extent of the time series and is computed via Castiglioni’s correction [11] on the algorithm of Katz [12]. The higher the FD is, the more irregular, but self-similar the signal. FD is linked to vagal modulation [13].
Detrended fluctuation analysis (DFA)
Detrended fluctuation analysis quantifies fractal-like correlation properties of the time series and uncovers short- and long-range correlations. The root mean square fluctuation of the integrated and detrended data are measured within observation windows of various sizes and then plotted against the window size on a log-log scale [14]. The scaling exponent DFA α indicates the slope of this line, which relates log(fluctuation) to log(window size). Both the short-term (4–11 beats) DFA α1 and the long-term (11–64 beats) DFA α2 scaling exponents were calculated. The scaling exponent can be seen as a self-similarity parameter, which is characteristic of a fractal. Values of α around 1 are an indication of scaling behavior.
Sample entropy (SampEn)
Entropy refers to system randomness, regularity, and predictability and allows systems to be quantified by rate of information loss or generation. SampEn quantifies the entropy of the system in a better way than the earlier used approximate entropy (ApEn) as it is not sensitive to data length [15]. More specifically, it measures the likelihood that runs of patterns that are close will remain close for subsequent incremental comparisons. It was calculated according to the formula of Richman & Moorman [15] with fixed input variables m=2 and r=0.2×SDNN (m being the length of compared runs and r the tolerance level). Higher values of SampEn indicate a more complex structure in the time series.
Correlation dimension (CD)
In the presence of chaos, an attractor in phase space characterizes the dynamics of the system, and its complexity can be quantified in terms of the properties of the attractor. The correlation dimension (CD) can be considered as a measure of the number of independent variables needed to define the total system in phase space. Here, CD was calculated according to the algorithm of Judd [16], as the maximum of the function with an embedding dimension of 8. When a finite value is found for the CD of a time series, correlations are present in the signal.
Lyapunov exponent (LE)
The largest Lyapunov exponent LE was calculated based on the algorithm of Rosenstein et al [17], which allows the calculation of this parameter on short data sets. The trajectories of chaotic signals in phase space follow typical patterns. Closely spaced trajectories converge and diverge exponentially relative to each other. For dynamic systems, sensitivity to initial conditions is quantified by the LE, which characterizes the average rate of divergence of these neighboring trajectories. A positive LE can be taken as a definition of chaos, provided the system is known to be deterministic. Larger LE values indicate more complex behavior.
All linear and nonlinear HRV parameters were computed using MATLAB (The MathWorks, Natick, MA, USA).
Statistical analysis
Statistical analysis was performed with SPSS Windows version 16.0 (Scientific Packages for Social Sciences, Chicago, IL, USA). Advice about the correct test statistics was given by the Biostatistical and Statistical Bioinformatics Centre in Leuven. In general, a significance level of α=0.05 was applied.
To compare the different time moments, the nonparametric Friedman test was performed for each HRV parameter. The nonparametric Wilcoxon Signed Rank test was used to investigate the day-night differences. In order to correctly interpret these results over the different time moments, the Bonferroni correction was used to counteract for multiple comparisons.
As the number of subjects was very small, the results of different parameters relating to the same aspect of autonomic heart rate modulation were combined into 1 group via the Friedman test with repeated measures, in order to obtain more robust results. Therefore, all parameter values were transformed to z-scores by subtracting the mean value and dividing by the standard deviation. In particular, TP and SDNN were taken as repeated measures to describe the total variability, while RMSSD, pNN50 and HF on the one hand, and LF/HF and LF [nu] on the other hand represent vagal modulation and sympathovagal balance, respectively. Regarding nonlinear HRV parameters, the model assessing the scaling behavior of the ANS consists of FD, DFA α1 and DFA α2, and SampEn, CD, and LE are grouped to reflect the cardiac complexity. This test statistic offers a solid testing method to determine whether weightlessness had a significant influence on a certain group of parameters and therefore on a specific part of the ANS.
Results
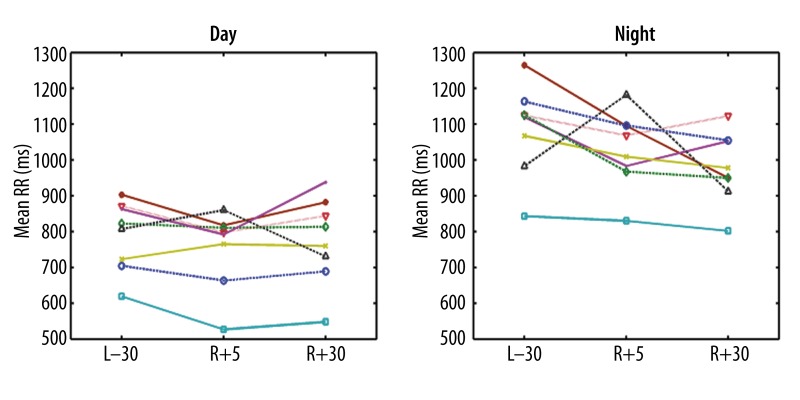
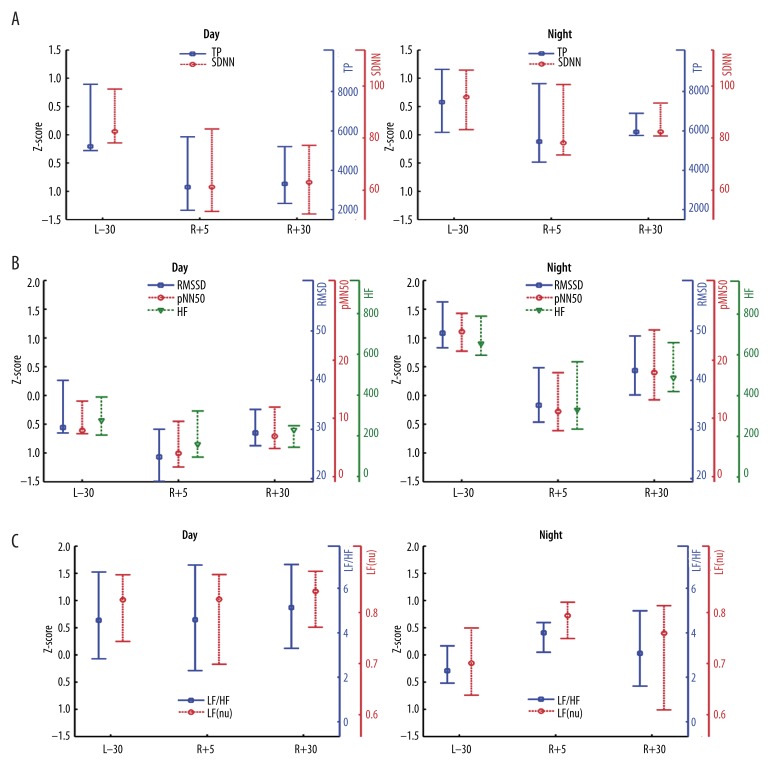
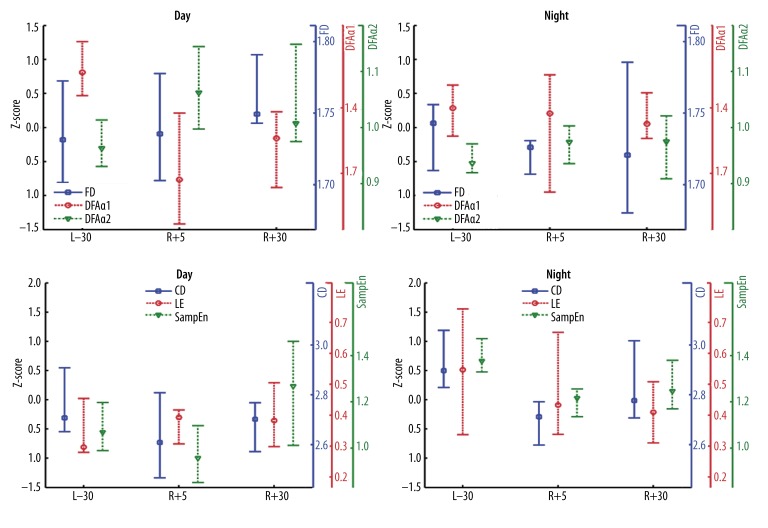
As no remarkable difference was found between astronauts from short- (n=3) and long-term (n=5) space missions, no distinction is made. Results from 1 group of 8 subjects are statistically also more robust than those of 2 smaller groups. Figure 1 displays the mean RR intervals, indicating the time evolution for the complete study. An overview of linear and nonlinear HRV parameters is given in Figures 2 and 3, respectively. The medians and interquartile ranges are indicated in z-scores and in absolute values.
Figure 1.
Mean RR preflight (L−30), early postflight (R+5) and late postflight (R+30) during day (left) and night periods (right), over all subjects.
Figure 2.
Linear HRV parameters over pre- (L−30), early post- (R+5) and late postflight (R+30), related to total variability (A), vagal modulation (B) and sympathovagal balance (C) during day (left) and night periods (right). The medians and interquartile ranges are given in z-scores as well as in absolute values. Abbreviations: see Methods. (A) Total Variability; (B) Vagal Modulation; (C) Sympathovagal balance.
Figure 3.
Nonlinear HRV parameters over pre- (L−30), early post- (R+5) and late postflight (R+30), related to scaling behavior (A) and complexity (B) during day (left) and night periods (right). The medians and interquartile ranges are given in z-scores as well as in absolute values. Abbreviations: see Methods. (A) Scaling Behavior; (B) Complexity.
Day-night variation
As expected, heart rate was significantly higher during day than at night (Table 1, Figure 1). The differences between day and night were reproduced for most parameters, with higher values during the night for all time domain measures, though not always significantly taking into account the Bonferroni correction. HF increased during the night due to the respiratory sinus arrhythmia (RSA), and LF/HF decreased. As for the nonlinear parameters, only CD and SampEn showed significant differences between day and night recordings; however, these differences were not statistically significant at each measurement moment.
Table 1.
Overview of statistical differences (p values) between day- and nighttime measurements of all linear and nonlinear HRV parameters at preflight (L−30), early postflight (R+5) and late postflight (R+30). Statistical analysis between day and night is performed by the nonparametric Wilcoxon Signed Rank test. Significant differences are indicated in italic. Significant results, taking into account the Bonferroni correction for multiple comparisons (α′=0.05/3), are given in bold.
| L−30 | R+5 | R+30 | |
|---|---|---|---|
| Mean RR [ms] | 0.012 | 0.011 | 0.012 |
| SDNN [ms] | 0.161 | 0.025 | 0.036 |
| RMSSD [ms] | 0.017 | 0.012 | 0.012 |
| pNN50 [%] | 0.010 | 0.012 | 0.010 |
| TP [ms2] | 0.208 | 0.017 | 0.036 |
| LF [ms2] | 0.484 | 0.017 | 0.017 |
| HF [ms2] | 0.012 | 0.011 | 0.012 |
| LF/HF [−] | 0.036 | 0.575 | 0.010 |
| LF [nu] | 0.036 | 0.889 | 0.012 |
| HF [nu] | 0.036 | 0.889 | 0.012 |
| DFA α1 | 0.093 | 0.889 | 0.161 |
| DFA a2 | 0.176 | 0.093 | 0.017 |
| FD | 0.844 | 0.812 | 0.078 |
| CD | 0.401 | 0.012 | 0.025 |
| SampEn | 0.008 | 0.031 | 0.578 |
| LE | 0.036 | 0.208 | 0.123 |
Abbreviations: see Methods.
Linear HRV parameters
In the 2-hour daytime recordings, no significant differences in heart rate were found between the pre- and postflight time moments (Figure 1). Only RMSSD and pNN50 showed significant results (p=0.030 and 0.034, respectively). The post-hoc test indicated that RMSSD was lower 5 days after spaceflight compared to preflight, whereas pNN50 showed significantly lower values early postflight compared to both pre- and late postflight (Figure 2B). During the nighttime recordings, no differences were observed.
Figure 2 shows the time evolution for several linear HRV parameters, indicating the median and interquartile ranges over the complete population and clustered in groups based on its physiological meaning. Microgravity caused a fall in the total variability (TP, SDNN) 5 days after spaceflight, although this was only significant during the day (p=0.012) (Figure 2A). Indices of vagal modulation (RMSSD, pNN50, HF) were significantly decreased (day: p=0.001, night: p=0.019) early postflight (Figure 2B), but the sympathovagal balance (LF/HF, LF [nu]) was strongly increased (p=0.017) at night 5 days after returning to Earth (Figure 2C). No significant difference in sympathovagal balance was found in the daytime recordings (p=0.498). All these effects seemed to have disappeared 30 days after return.
Nonlinear HRV parameters
The results of the nonlinear parameters were less consistent compared to the linear ones. For the individual parameters, no significant differences between the time moments were found. The nonlinear parameters were also grouped in either scaling behavior or complexity measures, as shown in Figure 3 by means of z-scores. Although the scaling behavior (Figure 3A) did not differ significantly, a significant decrease in the complexity measures (Figure 3B) was observed early postflight compared to preflight (p=0.020) at night. The complexity of the daytime recordings were not significantly different (p=0.148).
Discussion
In this study, the autonomic modulation of heart rate was examined in 8 astronauts before and after spaceflight. While most studies in the literature used short-time measurements of 5 or 10 minutes, here 2 blocks of 2-hour recordings were investigated, enabling us to study ANS changes due to microgravity separately during the day and night. This is very important, as the cardiovascular system is controlled differently by the ANS when awake and sleeping [18,19]. Moreover, the results clearly show that heart rate regulation was still influenced 5 days after return to Earth, but differently for day and night. Secondly, these longer measurements of 2 hours allowed us to use nonlinear HRV methods. Significant changes were found early postflight compared to preflight, indicating that nonlinear characteristics of cardiac modulation were influenced by microgravity.
Autonomic modulation early postflight is affected differently during day and night: linear HRV
Heart rate only increased slightly at early postflight compared to preflight. Probably, the heart rate was much higher during the first days after landing [3,20], but this tachycardia response was not detected at R+5. Although the heart rate seemed to be already restored 5 days after returning to Earth, we still observed significant changes in heart rate modulation. During the daytime, the total variability (TP, SDNN) decreased early preflight. In addition, vagal modulation (RMSSD, pNN50, HF) dropped significantly, but the sympathovagal balance (LF/HF, LF [nu]) did not change compared to preflight, which means that sympathetic modulation dropped as much as vagal modulation did. This reduced activity of the sympathetic pathways is at odds with many studies describing sympathetic dominance after spaceflight. The hemodynamically instable situation during the daytime may be an explanation. Even when carefully selecting the data, external influences still occurred, as well as changing postures inherent in Holter recordings. In addition, early postflight the day’s schedule was very busy, possibly leading to mental stress that might have influenced the measurements.
During nighttime, we found early postflight an excessive decrease in vagal modulation, but instead of an approximately equal sympathovagal balance as noted during day, at night there was a significant increase in LF/HF and LF [nu] compared to preflight. This means that sympathetic modulation of heart rate became relatively more important at R+5 when sleeping at night. Norsk et al. [21] suggested that the sympathetic dominance after spaceflight might result from decreased stroke volume and cardiac output due to gravity on Earth. Beckers et al. [2] observed changes in heart rate modulation and baroreflex sensitivity (BRS) early postflight, and linked them with a postural reduction in pulse pressure (PP). This suggests thoracic hypovolemia early postflight, requiring increased heart rate and sympathetic drive to maintain orthostatic blood pressure. According to our results, the findings of these previous studies are confirmed, but only during sleep. However, none of those studies used long-term monitoring; in the best case, astronauts were measured for 10 minutes in supine and standing position, causing only a profound effect on HRV after spaceflight in the standing position [2]. Nevertheless, our study showed significant changes in cardiac control during the day (~standing) as well as at night (~supine).
The grouped variables show a different day and night response of the ANS after spaceflight; this can also be observed when day-night variations are analyzed (eg, in the sympathovagal balance). Preflight, this balance is slightly lower when sleeping. However, early postflight, no difference can be found between day and night. In addition, at night, an increase was previously observed, indicating that no difference in sympathovagal balance is present when compared to daytime recordings. This result is in contrast with the vagal predominance expected at night. Furthermore, it is observed that preflight, there are no differences in SDNN and TP between day and night. However, as in early postflight, the total variability decreased significantly during the day (Figure 2A). These results show that there are some differences between day and night.
Long-term recovery of linear HRV parameters
Although symptoms of reduced orthostatic tolerance disappear rather quickly after return from microgravity conditions, the cardiovascular control system might recover much slower. Despite the unknown duration of recovery, most studies have only performed a follow-up of a maximum 1 week [22,23], and just a few studies did measurements up to 18 days. Recently, we showed that 25 days of recovery after short-duration space flight is sufficient to restore vagal-cardiac outflow to preflight conditions [3]. Here, at R+30, none of the described HRV parameters was still significantly different from the preflight values. There seems to be an almost complete recovery (eg, when looking at the sympathovagal balance at night). However, there are some indications that there might not be a full recovery compared to preflight. This can be observed by the total variability during the day. Although there is no significant difference between preflight and late postflight, it can be noticed that late postflight the total variability measures were not restored to the initial preflight values. The vagal modulation shows a similar behavior, indicating that the vagal recovery still persists late postflight. Although a recent study [2] showed no significant differences in cardiovascular control in supine position, and even a restored vagal modulation in standing position 4 days after returning, this study shows that the autonomic recovery in astronauts can last much longer. This slow (mostly vagal) recovery after return to Earth was also found by others after short- [24] and long-term [6,25] space missions. This recovery period does not seem to be strongly related to the duration of the spaceflight, as no remarkable differences could be found between astronauts from short- and long-term space missions.
Effect of microgravity on nonlinear dynamics of autonomic modulation
The influence of microgravity on nonlinear heart rate dynamics in astronauts was investigated for the first time in 1994 by Goldberger et al. [8], using approximate entropy as the complexity measure and 1/f slope as the spectral scaling measure. Neither parameter changed over time, thus HR dynamics appear remarkably stable during long-term spaceflight. Afterwards, to the best of our knowledge, only 1 study [7] used nonlinear HRV techniques (again, approximate entropy).
This study used a series of nonlinear techniques, reflecting scaling behavior and complexity of the underlying autonomic nervous system. Instead of approximate entropy, sample entropy (SampEn) was used, as it is not sensitive to the data length [15]. The nonlinear parameters separately did not show any significant result between the different time moments. However, CD and SampEn showed interesting trends, but not statistically significant (both p=0.072). During the daytime recordings, these parameters showed a decreasing trend early postflight. One month after return to Earth, those values were back in the same range as the preflight measurements. However, these trends should be confirmed by including data of other astronauts.
The grouped parameters showed a significantly decreased complexity (CD, LE, SampEn) at night early postflight. This difference disappeared late postflight. Concerning the scaling behavior measures, they did not show any consistent alignment and were in general rather stable over time.
When the day-night differences of the nonlinear parameters are analyzed, some interesting observations can be made. CD initially did not differ between day and night. Early postflight, a significant decrease in CD was detected at night, but late postflight this difference between day and night disappeared. As for SampEn, significantly higher entropy is found preflight at night. Early and late postflight, there was no difference anymore between day and night recordings.
One month after retuning to Earth, the nonlinear dynamics of heart rate control were mainly restored, acting again as in normal conditions, though not completely, as there are still differences preflight and late postflight in day-night results (eg, for SampEn). Some trends in CD and SampEn indicate no complete recovery, though statistically not significant. Consequently, our hypothesis was only partly confirmed by the nonlinear results.
Nonlinear HRV parameters give additional information about the nonlinear dynamics in the cardiovascular system, which cannot be reflected by standard HRV analysis. It is important to note that nonlinear HRV techniques will not replace linear analysis, but have to be considered as an extension, yielding information about a specific aspect of scaling behavior or complexity. Therefore, in contrast to the linear techniques that show a similar behavior between the different time moments when they are grouped, clustering of the nonlinear parameters in groups is not advised because there is a high variability between the measures (Figure 3); the separate interpretation is recommended. Nonlinear techniques have an advantage over linear techniques in providing better repeatability and reliability across measurements (small random error) [26]. Therefore, nonlinear indices may be more suitable for diagnostic purposes and for assessing individual treatment effects. In this application, the importance of the results lies in the possibility of developing specific countermeasures based on the described changes in cardiovascular control. This way, astronauts can be better assisted during their spaceflight.
Limitations
The number of subjects available in spaceflight experiments is very limited, especially in the post-Columbia accident era. However, having data of 8 astronauts with completed measurements at 3 time points is more than in most similar previous studies [2,3,8,20,21,25], resulting in more reliable conclusions on a group level. Although we have imposed standardization of experimental procedures between the different space missions, we cannot control differences in workload between these missions, nor the quantity and quality of sleep. Personal exercise tasks, fluid intake, and nutrition before, during and after space flight could not be controlled. Unfortunately, there was also no activity log available. Therefore we cannot guarantee that the astronauts were sleeping during the night recordings. However, we selected the night data based on the typical decrease in heart rate that occurs during sleep. As no Holter data were available at R+1, we cannot make any statement about the cardiovascular adaptation immediately after spaceflight. Therefore, we restrict our results and conclusions to the time period from 5 to 30 days after returning to Earth.
Nowadays, the meaning of the indices used for nonlinear dynamics is not as clear as those derived from time or frequency domain methods. Moreover, spectral analysis is superior in visualizing the results. Future research will need to focus on determining clear physiological interpretations for all indices. Some physiological relations are already given by Beckers et al. [27] and Aubert et al. [28].
Conclusions
The influence of microgravity on cardiovascular control was confirmed in this study; however no remarkable difference was found between astronauts from short- and long-term spaceflights. While vagal modulation was significantly decreased during day and night early postflight, the sympathovagal balance did not differ during daytime, but was strongly increased at night. Therefore, our results confirmed the sympathetic dominance early postflight, but only at night. This study also observed a change in nonlinear heart rate dynamics, present 5 days after return to Earth. Those nonlinear HRV parameters will not replace linear analysis, but have to be considered as a complement, yielding extra information about a specific aspect of scaling behavior or complexity of the underlying cardiovascular system. One month after return to Earth, an almost complete cardiovascular recovery was found.
Acknowledgements
We thank the astronauts and cosmonauts who took part in the study for their efforts during the measurements before and after space flight. In particular, we acknowledge the space agencies ESA and Roskosmos in supporting these missions and sharing the data. We also thank Dr. Bart Verheyden for his advice on the physiological interpretation.
Footnotes
The scientific responsibility is assumed by its authors.
Source of support: Research Council KUL: GOA MaNet, PFV/10/002 (OPTEC), IDO 08/013 Autism, several PhD/postdoc & fellow grants;, Flemish Government: – FWO: PhD/postdoc grants, projects: G.0427.10N (Integrated EEG-fMRI), G.0108.11 (Compressed Sensing) G.0869.12N (Tumor imaging); – IWT: TBM070713-Accelero, TBM080658-MRI (EEG-fMRI), TBM110697-NeoGuard, D.Widjaja is supported by an IWT PhD grant; – iMinds 2012; – Flanders Care: Demonstratieproject Tele-Rehab III (2012-2014);, Belgian Federal Science Policy Office: IUAP P7/(DYSCO, ‘Dynamical systems, control and optimization’, 2012-2017); ESA-PRODEX-AO-PGPF-01 CardioControl (C4000103224), ESA-PRODEX-8-C90242;, EU: RECAP 209G within INTERREG IVB NWE programme, EU HIP Trial FP7-HEALTH/2007–2013 (n° 260777), EU ITN Transact 2012
References
- 1.Fu Q, Witkowski S, Levine BD. Vasoconstrictor reserve and sympathetic neural control of orthostasis. Circulation. 2004;110:2931–37. doi: 10.1161/01.CIR.0000146384.91715.B5. [DOI] [PubMed] [Google Scholar]
- 2.Beckers F, Verheyden B, Liu J, Aubert AE. Cardiovascular autonomic control after short-duration spaceflights. Acta Astronautica. 2009;65:804–12. [Google Scholar]
- 3.Verheyden B, Beckers F, Couckuyt K, et al. Respiratory modulation of cardiovascular rhythms before and after short-duration human spaceflight. Acta Physiol. 2007;191:297–308. doi: 10.1111/j.1748-1716.2007.01744.x. [DOI] [PubMed] [Google Scholar]
- 4.Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability standards of measurement, physiological interpretation and clinical use. Circulation. 1996;93:1043–65. [PubMed] [Google Scholar]
- 5.Goldberger AL, Rigney DR, West BJ. Chaos and fractals in human physiology. Sci Am. 1990;262:42–49. doi: 10.1038/scientificamerican0290-42. [DOI] [PubMed] [Google Scholar]
- 6.Baevsky RM, Baranov VM, Funtova II, et al. Autonomic cardiovascular and respiratory control during prolonged spaceflights aboard the International Space Station. J Appl Physiol. 2007;103(1):156–61. doi: 10.1152/japplphysiol.00137.2007. [DOI] [PubMed] [Google Scholar]
- 7.Beckers F, Verheyden B, Couckuyt K, Aubert AE. Non-linear heart rate control in orthostatic tolerant cosmonauts after short-duration spaceflight. Microgravity Sci Technol. 2007;19(5):98–101. [Google Scholar]
- 8.Goldberger AL, Bungo MW, Baevsky RM, et al. Heart rate dynamics during long-term spaceflight: report on MIR cosmonauts. Am Heart J. 1994;128(1):202–4. doi: 10.1016/0002-8703(94)90033-7. [DOI] [PubMed] [Google Scholar]
- 9.Singh D, Vinod K, Saxena SC. Sampling frequency of the RR interval time series for spectral analysis of heart rate variability. J Med Eng Techn. 2004;28(6):263–72. doi: 10.1080/03091900410001662350. [DOI] [PubMed] [Google Scholar]
- 10.Aubert AE, Ramaekers D, Beckers F, et al. The analysis of heart rate variability in unrestrained rats. Validation of method and results. Comput Methods Programs Biomed. 1999;60(3):197–213. doi: 10.1016/s0169-2607(99)00017-6. [DOI] [PubMed] [Google Scholar]
- 11.Castiglioni P. What is wrong in Katz’s method? Comments on: “A note on fractal dimensions of biomedical waveforms”. Comput Biol Med. 2010;40(11):950–52. doi: 10.1016/j.compbiomed.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 12.Katz MJ. Fractals and the analysis of waveforms. Comput Biol Med. 1988;18(3):145–56. doi: 10.1016/0010-4825(88)90041-8. [DOI] [PubMed] [Google Scholar]
- 13.Yeragani VK, Srinivasan K, Vempati S, et al. Fractal dimension of heart rate time series: an effective measure of autonomic function. J Appl Physiol. 1993;75(6):2429–38. doi: 10.1152/jappl.1993.75.6.2429. [DOI] [PubMed] [Google Scholar]
- 14.Peng CK, Havlin S, Hausdorff JM, et al. Fractal mechanisms and heart rate dynamics. J Electrocardiol. 1995;28(Suppl):59–65. doi: 10.1016/s0022-0736(95)80017-4. [DOI] [PubMed] [Google Scholar]
- 15.Richman JS, Moorman RJ. Physiological time-series analysis using approximate entropy and sample entropy. Am J Physiol Heart Circ Physiol. 2000;278(6):H2039–49. doi: 10.1152/ajpheart.2000.278.6.H2039. [DOI] [PubMed] [Google Scholar]
- 16.Judd K. An improved estimator of dimension and some comments on providing confidence intervals. Physica D. 1992;56(2):216–28. [Google Scholar]
- 17.Rosenstein M, Collins JJ, De Luca CJ. A practical method for calculating largest Lyapunov exponents from small data sets. Physica D. 1993;65(1):117–34. [Google Scholar]
- 18.Malpas SC, Purdie GL. Circadian variation of heart rate variability. Cardiovascular Research. 1990;24(3):210–13. doi: 10.1093/cvr/24.3.210. [DOI] [PubMed] [Google Scholar]
- 19.Stefíková H, Sovcíková E, Bronis M. The circadian rhythm of selected parameters of heart rate variability. Physiol Bohemoslov. 1986;35(3):227–32. [PubMed] [Google Scholar]
- 20.Gisolf J, Immink RV, van Lieshout JJ, et al. Orthostatic blood pressure control before and after spaceflight, determined by time-domain baroreflex method. J Appl Physiol. 2005;98(5):1682–90. doi: 10.1152/japplphysiol.01219.2004. [DOI] [PubMed] [Google Scholar]
- 21.Norsk P, Damgaard M, Petersen L, et al. Vasorelaxation in space. Hypertension. 2006;47:69–73. doi: 10.1161/01.HYP.0000194332.98674.57. [DOI] [PubMed] [Google Scholar]
- 22.Cox JF, Tahvanainen KUO, Kuusela TA, et al. Influence of microgravity on astronauts’ sympathetic and vagal responses to Valsalva’s manoeuvre. J Physiol. 2002;538(1):309–20. doi: 10.1113/jphysiol.2001.012574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sigaudo-Roussel D, Custaud MA, Maillet A, et al. Heart rate variability after prolonged spaceflights. Eur J Appl Physiol. 2002;86(3):258–65. doi: 10.1007/s00421-001-0551-7. [DOI] [PubMed] [Google Scholar]
- 24.Fritsch JM, Charles JB, Bennett BS, et al. Short-duration spaceflight impairs human carotid baroreceptor-cardiac reflex responses. J Appl Physiol. 1992;73(2):664–71. doi: 10.1152/jappl.1992.73.2.664. [DOI] [PubMed] [Google Scholar]
- 25.Cooke WH, Iv JEA, Crossman AA, et al. Nine months in space: effects on human autonomic cardiovascular regulation. J Appl Physiol. 2000;89(3):1039–45. doi: 10.1152/jappl.2000.89.3.1039. [DOI] [PubMed] [Google Scholar]
- 26.Maestri R, Pinna GD, Porta A, et al. Assessing nonlinear properties of heart rate variability from short-term recordings: are these measurements reliable? Physiol Meas. 2007;28(9):1067–77. doi: 10.1088/0967-3334/28/9/008. [DOI] [PubMed] [Google Scholar]
- 27.Beckers F, Verheyden B, Aubert AE. Aging and nonlinear heart rate control in a healthy population. J Physiol Heart Circ Physiol. 2006;290(6):H2560–70. doi: 10.1152/ajpheart.00903.2005. [DOI] [PubMed] [Google Scholar]
- 28.Aubert AE, Vandeput S, Beckers F, et al. Complexity of cardiovascular regulation in small animals. Phil Trans R Soc A. 2009;367:1239–50. doi: 10.1098/rsta.2008.0276. [DOI] [PubMed] [Google Scholar]