Abstract
Aims
Social norms are a key source of influence on health behaviors. This study examined changes in social norms and relationships between HIV injection risk behaviors and social norms among injection drug users (IDUs) involved in an experimental intervention.
Design
Randomized clinical trial.
Setting
An HIV Prevention Trials Network study, Philadelphia, USA.
Participants
IDUs, called indexes, and their social network members, who were drug or sex partners, were recruited for an HIV prevention intervention and followed for up to 30 months (N=652). Indexes were randomized into a peer education intervention or control condition.
Measurements
Outcomes of injection related HIV risk behaviors (sharing needles, sharing cookers, sharing cotton, front/back-loaded) were measured every 6 months and social norm of these 4 risk behaviors were assessed every 12 months.
Findings
There was a statistically significant intervention effect on all four social norms of injection behaviors, with participants in the intervention reporting less risky social norms compared with controls (changes in mean score: needles, -0.24, p.<01; cookers, -0.33, p.<01; cottons, -0.28, p.<05; front/back loading, -0.23, p.<01). There was also a statistically significant bidirectional association with social norms predicting injection risk behaviors at the next assessment and risk behaviors predicting social norms at the subsequent visit.
Conclusions
Through social network interventions it is feasible to change both injection risk behaviors and associated social norms. However, it is critical that social network interventions focus on publically highlighting behavior changes since changing social norms without awareness of behaviors change may lead to relapse of risk behaviors.
Introduction
One key factor in explaining and understanding how societal factors influence individual health behaviors is through social norms. It is well documented that social norms predict a range of health behaviors, including exercise, tobacco, alcohol, and illicit drug use (1-7). In the field of HIV prevention, there is also convincing evidence that norms are associated with risk behaviors (8-12). Yet less is known about the dynamic interplay and causal links between social norms and health behaviors. Laws to reduce exposure of secondhand smoke appear to have influenced both social norms and smoking behaviors but it is difficult to establish the direction of causal path between smoking norms and behaviors (13). Often, social norms approaches to behavior change focus on the directionality of norms influencing behavior. For example, interventions to change alcohol consumption among college students have typically presented information to students on the normative drinking at their college in hopes of reducing the likelihood that students will increase their alcohol consumption (14,15). However, it is unlikely that the relationship between norms is unidirectional.
Actual and perceived behaviors are likely to influence social norms. Understanding how social norms change is of more than theoretical interest. Although norms may be difficult to change, once they are altered they can help maintain behavior change and hence interventions that change norms are likely to be sustainable. Moreover, most of the intervention studies that utilize social norms to reduce substance use have been with youth and young adults, and it is important to examine the influence of social norms on adults and especially drug users who may be less influenced by social factors as compared to individuals who are not drug dependent.
The current study examined the bidirectional relationship between descriptive social norms, which are perceptions of how peers or reference group members act, and behaviors among a sample of injection drug users (IDUs) who were enrolled in a social network oriented HIV prevention intervention in Philadelphia and interviewed every 6 months for up to 30 months. A prior outcome analysis indicated that there was a significant decrease in injection risk behaviors among intervention participants as compared to those in the control condition (16,17).
The intervention targeted injection and sexual risk behaviors associated with HIV and HCV transmission among injection drug users (18,19). During the intervention, peer educators were trained in small groups to promote behavior change among their risk network members. Risk networks include individuals that a person engages in HIV risk behaviors with such as sex partners or drug partners (20). The study evaluated the behavior change among both the peer educators and their risk network members. In the prior analyses the impact of the intervention on descriptive social norms was not assessed. In the current analyses, we first examined the impact of the intervention on social norms of HIV-related injection risk behavior and then assessed the pathway between norms and behaviors; namely, we examined if the social norms at a prior visit predicted current behaviors and vice versa. The intervention was designed to encourage peers to discuss and model injection risk reduction with their risk network members. It was anticipated that within small networks these social interaction that promoted risk reduction would lead network members to view risk reduction as an important set of behaviors practiced and endorsed by their peers. Moreover, these perceptions of peer norms would then be internalized, leading to a reduction is risk behaviors. It was also anticipated that the change in risk behaviors would help to perpetuate new social norms.
Methods
Recruitment
The current study is part of the HIV Prevention Trials Network (HPTN) study that implemented a social network-based intervention in Chiang Mai, Thailand and Philadelphia, PA, USA. This analysis is a report on Philadelphia participants, where significant decreases in risk behaviors were observed, and have previously been reported, as a result of the intervention (21). No intervention effects were observed in Chiang Mai, which was in the midst of the campaign against drug use that included large-scale incarcerations and extra-judicial killing (21).
Potential participants were identified through a community-based recruitment, which included ethnography and outreach in zip codes with high rates of HIV/AIDS cases based on data from the Philadelphia Department of Public Health. Outreach workers disseminated verbal and written information about the study. Participants were paid $25 per study visit. Recruitment began in December 2002 with follow-up ending in August 2006. Follow-up visits occurred every six months for up to 30 months.
Eligibility criteria
The study included two types of participants: index and network participants. Index participants were actively recruited and had the opportunity to be randomized into the intervention or control condition. Network participants were social network members of the index participants who were referred to the study. Network participants did not receive the intervention. Study eligibility criteria for index participants included 1) being age 18 or older, 2) providing written informed consent for research, 3) injected drugs at least 12 times in the last three months, 4) been out of methadone maintenance treatment for at least 3 months and have relapsed, 5) HIV negative antibody test results within 60 days prior to randomization (seronegatives were chosen due to the potential to examine change in serostatus) , and 6) willing to identify and attempt to recruit at least two network members with whom they had injected drugs or had sex with within the prior three months. After participants completed the baseline visit and returned for HIV test results, index participants were required to recruit into the study at least one eligible HIV risk network member. The index participants were provided cards to give to eligible network members. Then, the network member presented the card at the clinic and their information was verified with the data on the network inventory. Eligibility requirements for the network members included 1) being 18 years of age or old, 2) providing informed consent, and 3) recruited for the study by an eligible index participant. The present sample was limited to index participants and network participants who reported injecting drugs.
Intervention
All participants received a two-session voluntary HIV counseling and testing (VCT), modeled on Project RESPECT (22). Only index participants were randomized into the two study conditions: either a peer education condition or a control condition. The treatment intervention consisted of six 2-hour peer-educator sessions during a four week period and two booster sessions at 6 and 12 months after the intervention was completed. The index participants were trained to be peer educators. The intervention manual is available at http://www.hptn.org/research_studies/HPTN037InterventionManual.asp. The training focused on teaching indexes 1) how to promote safer sex and drug injection skills among network members, and 2) communication strategies to conduct peer outreach and promote norms about HIV risk reduction with their drug and sex network members. Participants engaged in role-plays to practice their peer education and risk reduction skills. Participants were encouraged to model safer behaviors when they were with their peers. A major component of the training focused on developing communication skills on how to talk with network members about risk reduction. Participants randomized into the control condition did not participate in any intervention sessions. One of the intervention’s primary goals was to alter the social norms of injection risk behaviors. It was anticipated that peers’ modeling and discussing methods of reducing HIV risks within their social networks would lead to a greater perception of network members engagement in and endorsement of risk reduction, and hence, alter and lead to an internalization of social norms that were favorable to HIV prevention. It was also anticipated that the peer educators would perceive the greatest change in social norms since they would perceive that their network members agreed with them and endorsed these norms.
Monitoring and oversight
All study protocols and procedures were approved by the IRB at the University of Pennsylvania. A study specific community advisory board and a Data Safety and Monitoring Board (DSMB) monitored the study outcomes, adverse events, and social harms. Study monitors visited the sites to verify compliance with human subjects and other research regulations, assess adherence to the study protocol and procedures manual, and confirm data quality and accuracy. All surveys and HIV test results were sent to the statistical center (SCHARP, Seattle WA). The study was terminated early when the DSMB determined that the study could not reliably access the impact of the intervention on HIV because of low incidence rates, however, participants were enrolled for up to 30 months.
Measures
Participants entered the study either as an index, who received the intervention directly, or as a risk network member, who was recruited by an index and received the intervention indirectly through their index. For both indexes and network members at each study visit, the interviewer administered a behavioral survey that included self-report of the following HIV risk behaviors in the prior month: needle sharing, sharing cooker, sharing cotton, and front/back loading (Table 1). For front-loading, the drug solution is squirted from one syringe into another syringe though the front of the recipient syringe after removing the needle. For back-loading, the solution is squirted into the back of the syringe after removing the plunger.
Table 1.
HPTN 037 Study Measures of Social Norms and HIV Risk Behaviors
| Behaviors | Social Norms | Risk Behaviors |
|---|---|---|
| Share Needle | How many of your friends who shoot drugs use a needle after someone else, without bleaching or cleaning? |
Did you use a needle after someone else in the last month? |
| Share Cooker | How many of your friends who shoot drugs use a cooker that someone else has already used? |
In the last month, how many times did you use a cooker that others had used? |
| Share Cotton | How many of your friends who shoot drugs use filter cotton that someone else has already used? |
In the last month, how many times did you use cotton that others had used? |
| Front/back loaded |
How many of your friends who shoot drugs use drugs that are front-loaded or back-loaded with a shared syringe? |
In the last month, how many times did you use a front/back-loaded Syringe? |
Descriptive social norms for these four behaviors, collected only once per year, were paired with the behaviors self-reported by the participants, which were collected twice per year (shown in Table 1). While injection behaviors were measured every 6 months (0, 6, 13, 18, 24), social norms about these behaviors were only collected at (0, 12, 24) months. The response categories for the social norms were “none”, “some”, “about half”, “most”, and “all”.
Statistical Analysis
Three sets of analyses were conducted for this study. First, linear mixed-effects models (LMEM) were used to test for an intervention effect on participants’ perception of their friends’ behavior (social norm). Analyses were performed separately for each social norm, with social norms coded as a score ranging from 1=none, 2= some, 3 =about half, 4 = most, 5 = all friends. Network was included as a random effect, with treatment arm, visit and role (index or network member) as fixed effects. Second, logistic regression with generalized estimating equations (GEE) estimation assessed whether social norms at one visit predicted behavior at the next follow-up assessment, after adjusting for randomization arm. Social norm data from baseline, months 12 and 24 were used to predict injection behaviors at months 6, 18, and 30, respectively. In this analysis, based on the highly skewed distributions, social norms responses were coded as none vs. any friends with risk behavior, and risk behaviors were assessed as any/none for the previous month based on an intention to explore the relationship of participants with strong adverse risk social norms (no friends with HIV risk behaviors) and their own risk behaviors. In the final set of analyses, logistic regression, using GEE methods, assessed whether participants’ behavior predicted their perception of their friends’ behavior (social norms) at the next 6 month assessment. As in the previous analysis, both behavioral (at 6 and 18 months) and social norms (for 12 and 24 months) data were dichotomized. The model was adjusted for randomization arm. Participants without information on either one particular norm or behavior are excluded from the analysis of that norm/behavior. In assessing the outcomes, we focused on four hypotheses: (1) we anticipated greater change in social norms among those in the experimental condition as compared to those in the control group, (2) greater change in index versus network members, (3) changes in social norms would predict changes in risk behavior at subsequent waves, and (4) changes in risk behaviors would predict changes in social norms at subsequent waves.
Results
HPTN 037 screened 1779 participants in Philadelphia, of whom 696 met eligibility criteria and were enrolled. Of these 696 participants, 652 were IDUs and hence included in this analysis, 232 (36%) were index participants. Among expected visits, 522 6-month visits were completed (80%), 437 12-month visits were completed (80%), 350 18-month visits were completed (80%), 234 24-month visits were completed (78%), and 131 30-month visits were completed (72%). The overall follow-up rate was 79%. Note that since the study was terminated early, administrative censoring occurred at later visits.
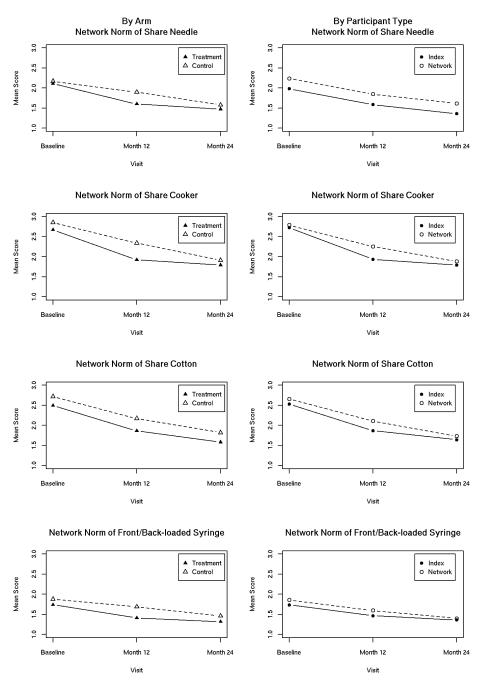
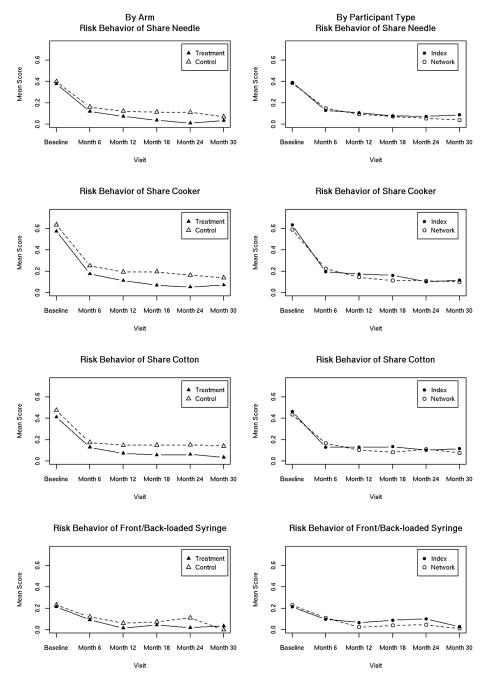
The majority of participants was male, unemployed, and injected daily (Table 2). Figures 1 and 2 show the change in social norms and risk behaviors during the study by treatment arm and participant role (index vs. network member). Table 3 describes the social norms vs. sexual behaviors among the 435 participants who completed month 12 and/or month 24 visits. Three comparisons are made for each norm: 1) All participants’ changes from 12 to 24 month, 2) Index participants vs. network participants, and 3) Treatment (i.e. intervention) vs. control index participants. The intervention effect on social norms was statistically significant for all four social norms (Table 3). Comparing the four mean norm scores between the month 12 and month 24 visits, it was found that the mean scores were significantly higher (i.e. likely to report more friends with risky behaviors) in the month 12 visit. Index participants had lower mean social norm scores compared to network member participants in all four social norms, but only sharing needle and sharing cooker were significant (p=0.001 and p=0.018, respectively). Participants in the treatment arm had lower mean norm scores compared to those in the control arm. Although there were significant reductions in all four norms and differences between treatment and controls over time, for sharing cotton and front/back loading, the differences between index participants and network members were not statistically significant. The presence of interactions between treatment and role (i.e. index vs. network member) was tested for each model, and none were found.
Table 2.
Baseline Demographic and Risk Behaviors Characteristics of Philadelphia IDU Participants (Bold font indicates p-value < 0.05)
| Arm | Role | |||
|---|---|---|---|---|
| Characteristics | Treatment N/Total(%) |
Control N/Total(%) |
Index N/Total(%) |
Network Member N/Total(%) |
| Age (years) | ||||
| 18 to 25 | 27/314 (9%) | 30/338 (9%) | 17/232 (7%) | 40/420 (10%) |
| 25+ to 35 | 65/314 (21%) | 86/338 (25%) | 56/232 (24%) | 95/420 (23%) |
| 35+ to 45 | 100/314 (32%) | 103/338 (30%) | 81/232 (35%) | 122/420 (29%) |
| 45+ to 55 | 106/314 (34%) | 110/338 (33%) | 72/232 (31%) | 144/420 (34%) |
| Over 55 | 16/314 (5%) | 9/338 (3%) | 6/232 (3%) | 19/420 (5%) |
| Gender | ||||
| Male | 225/314 (72%) | 243/338 (72%) | 184/232 (79%) | 284/420 (68%) |
| Female | 89/314 (28%) | 95/338 (28%) | 48/232 (21%) | 136/420 (32%) |
| Race | ||||
| White | 132/314 (42%) | 174/338 (51%) | 117/232 (50%) | 189/420 (45%) |
| Black/African American | 169/314 (54%) | 131/338 (39%) | 102/232 (44%) | 198/420 (47%) |
| Marital Status | ||||
| Single | 191/314 (61%) | 214/338 (63%) | 146/232 (63%) | 259/420 (62%) |
| Married | 33/314 (11%) | 32/338 (9%) | 24/232 (10%) | 41/420 (10%) |
| Living with partner/not married | 23/314 (7%) | 27/338 (8%) | 23/232 (10%) | 27/420 (6%) |
| Divorced or separated | 58/314 (18%) | 52/338 (15%) | 32/232 (14%) | 78/420 (19%) |
| Widowed | 9/314 (3%) | 13/338 (4%) | 7/232 (3%) | 15/420 (4%) |
| Education | ||||
| No schooling or primary schooling |
5/314 (2%) | 7/338 (2%) | 5/232 (2%) | 7/420 (2%) |
| Any secondary schooling | 239/314 (76%) | 263/338 (78%) | 177/232 (76%) | 325/420 (77%) |
| Vocational or trade schooling | 4/314 (1%) | 10/338 (3%) | 3/232 (1%) | 11/420 (3%) |
| College/university/graduate schooling |
66/314 (21%) | 58/338 (17%) | 47/232 (20%) | 77/420 (18%) |
| Employment | ||||
| Full-time | 25/314 (8%) | 29/338 (9%) | 22/232 (9%) | 32/420 (8%) |
| Part-time/occasional/time-to- time |
31/314 (10%) | 39/338 (12%) | 31/232 (13%) | 39/420 (9%) |
| Unemployed | 258/314 (82%) | 270/338 (80%) | 179/232 (77%) | 349/420 (83%) |
| Injection Last Month | ||||
| Not Injected Daily | 128/314 (41%) | 119/337 (35%) | 79/232 (34%) | 168/419 (40%) |
| Injected Daily | 186/314 (59%) | 218/337 (65%) | 153/232 (66%) | 251/419 (60%) |
| Risk Behavior | ||||
| Shared Needle | 117/310 (38%) | 131/328 (40%) | 90/229 (39%) | 158/409 (39%) |
| Shared Cooker | 178/310 (57%) | 208/328 (63%) | 145/229 (63%) | 241/409 (59%) |
| Shared Cotton | 128/310 (41%) | 156/328 (48%) | 106/229 (46%) | 178/409 (44%) |
| Front/Back-loaded | 67/310 (22%) | 76/328 (23%) | 49/229 (21%) | 94/409 (23%) |
Figure 1.
Social norms for each risk behavior by treatment arm and participant role in the study.
Figure 2.
HIV risk behaviors by treatment arm and participant’s study role.
Table 3.
Change in Social Norm Scores over 24 Months among Index and Network Members and Experimental and Control Participants in Philadelphia.
| Social Norm Item |
Comparison | Change in mean score |
p-Value |
|---|---|---|---|
| Share Needle | Month 12 vs. Month 24 | 0.22 | 0.009 |
| Index vs. Network Member | −0.26 | 0.001 | |
| Treatment vs. Control | −0.24 | 0.007 | |
| Share Cooker | Month 12 vs. Month 24 | 0.28 | 0.008 |
| Index vs. Network Member | −0.24 | 0.018 | |
| Treatment vs. Control | −0.33 | 0.004 | |
| Share Cotton | Month 12 vs. Month 24 | 0.30 | 0.004 |
| Index vs. Network Member | −0.19 | 0.055 | |
| Treatment vs. Control | −0.28 | 0.016 | |
| Front/Back- loaded |
Month 12 vs. Month 24 | 0.16 | 0.028 |
| Index vs. Network Member | −0.11 | 0.138 | |
| Treatment vs. Control | −0.23 | 0.002 |
Social norms were found to predict subsequent risk behaviors on 532 participants who provided information of both baseline and month 6 visits, both month 12 and month 18 visits, or both month 24 and month 30 visits (Table 4). Social norms reported at baseline were strongly associated with self-reported behavior at follow-up assessments, after adjusting for randomization arm. There were increased odds of reporting a risk behavior at 6 months when reporting friends with that behavior at baseline, with very high odds for shared cooker (OR = 8.79, 95% CI=(3.39, 22.75)) and shared cotton (OR = 4.49, 95% CI=(1.89, 10.69)). Social norms at 12 months remained strongly predictive of self reported behaviors at 18 months for shared cooker and cotton, though not for shared needles and syringes.
Table 4.
Social Norms as predictors of Risk Behavior at Subsequent Visits
| Behavior | Effect | Adjusted OR* |
95% CI | p-Value |
|---|---|---|---|---|
| Share Needle | Baseline norm | 2.08 | ( 1.16, 3.71) | 0.014 |
| Follow-up norm | 1.18 | ( 0.56, 2.48) | 0.660 | |
| Share Cooker | Baseline norm | 8.79 | ( 3.39, 22.75) | <.001 |
| Follow-up norm | 5.99 | ( 2.29, 15.63) | <.001 | |
| Share Cotton | Baseline norm | 4.49 | ( 1.89, 10.69) | <.001 |
| Follow-up norm | 4.16 | ( 1.63, 10.59) | 0.003 | |
| Front/Back- loaded |
Baseline norm | 2.81 | ( 1.44, 5.47) | 0.002 |
| Follow-up norm | 1.72 | ( 0.77, 3.81) | 0.183 |
Adjusted for randomization arm
At every follow-up visit during the study, risk behaviors predicted subsequent social norms (Table 5). Among 407 people who completed both month 6 and month 12 visits, or both month 18 and month 24 visits, participants who reported high levels of injection risk behaviors tended to report at the subsequent visit that a larger proportion of their friends engaged in risky injection practices: the odds ratio of reporting friends who share needles was 2.7 95% CI= (1.35, 5.40) for those who self-reported sharing needles at the previous visit; for sharing cookers the OR = 3.14, 95% CI= ( 1.57, 6.29) and for sharing cotton, OR = 2.26, 95% CI = ( 1.21, 4.22). An OR = 1.93 (0.97, 3.83)) was observed for sharing syringes, although it is not statistically significant (p = 0.06).
Table 5.
Self-Reported Injection Risk Behavior as Predictors of Subsequent Report of Social Norms among Study Participants in Philadelphia.
| Behavior | Adjusted OR* | 95% CI | p-Value |
|---|---|---|---|
| Share Needle | 2.70 | ( 1.35, 5.40) | 0.005 |
| Share Cooker | 3.14 | ( 1.57, 6.29) | 0.001 |
| Share Cotton | 2.26 | ( 1.21, 4.22) | 0.011 |
| Front/Back-loaded | 1.93 | ( 0.97, 3.83) | 0.060 |
Adjusted for randomization arm
Discussion
The results of this study suggest that peer based interventions to reduce HIV injection behaviors can change social norms as well as behaviors. We also found that social norms not only predict health behaviors, but also self-reported behaviors predict the social norms that coincide with the behaviors. Thus, participants who practiced risky injection behaviors believed their friends practiced risky behaviors and vice-versa. These finding replicate prior studies on the relationship between social norms and HIV risk behaviors and add to our understanding of how social network intervention may alter behaviors through changing social norms and that the relationship between norms and behaviors is bidirectional. The results suggest that in order to develop interventions that sustain behavior change, it is important to focus on changing social norms. Norms may be changed through participants’ modeling behaviors and having conversations that highlight health promoting norms which can be observed by peers so that the behaviors reinforce the risk reduction norms.
In the current intervention, peer educators were trained to discuss and model safer injection behaviors with their network members. It is likely that these social influence actions led to both behavior and norm change, which were sustained and increased for over two years. Social norms may be a powerful factor in promoting behavior change, yet it cannot be assumed that social norms will lead to sustained behavior change without individuals being cognizant of the behavior change. The findings also suggest that in order to promote and maintain social norm changes it is important to highlight actual changes in individuals’ behaviors.
Social network analyses suggest that health behaviors within networks are clustered as are social norms (12,23). It is likely that within social networks, behaviors and norms are mutually reinforcing. Consequently, one method to diffuse behavior change through social networks is to highlight both the norms and the behaviors followed by individuals in the network. As HIV risk behaviors are mostly social behaviors it is likely that individuals engage in risk behaviors with others and hence perceive that these behaviors are normative especially if others do not indicate their disapproval of such behaviors. Structuring conversations that emphasize health promotion norms and ensuring that close network members are aware of their peers’ positive health behaviors may enhance network level behavior change.
Although social norms may have a strong influence on behaviors, normative approaches to behavior change may not be universally effective. Normative pressure may lead to reactance and subgroups defining themselves in opposition to prevailing norms or health messages, such as barebackers, who are men who seek out unprotected sex with other men (24,25). Moreover, it may be difficult to intervene in close, dense networks. It should also be cautioned that norms of health promotion might lead to stigmatizing those whose image and behaviors do not coincide with this social norm (26,27).
This study is subject to limitations based on sampling and self-report biases, including the possible influence of repeated survey questions on social norms. The sample was limited to HIV negative injectors who could recruit risk network members and their drug and sex risk network members. The assessment of social norms may have overlap with some of the risk behaviors. Since these behaviors are social behaviors, the basis of making judgments about social norms may be due in part to observations of one’s own behaviors. Moreover, in the data analyses, collapsing norms and behaviors into dichotomous variables reduced our ability to examine linear trends. The survey only assessed descriptive norms and not proscriptive norms. However, prior research suggests that descriptive norms have a strong influence on risk behaviors (28). We also did not examine the relative contribution of certain peers on norms and behaviors. It is likely that some peers, based on relationship, trust, and frequency of contact have more or less social influence on both norms and behaviors. Another limitation is social desirability biases. It is possible that the intervention changed the norms of self-reports but did not change the actual risk behaviors.
In this experimental intervention, both norms and their associated behaviors were found to be malleable and predict each other over a two year period. Future research should examine the relative effectiveness of interventions that promote norm change, behavior change, or both. Moreover, additional research is needed into delineating the dimensions of social norms, their specificity, and how they are best transmitted and maintained through social networks and other communication channels. Finally, although we did find a temporal pattern between social norms and behaviors, we do not know the mechanism that lead to these changes.
Acknowledgments
Declaration of interest: This study was supported by the HIV Prevention Trials Network and sponsored by the National Institute of Allergy and Infectious Diseases, National Institute of Child Health and Human Development, National Institute on Drug Abuse, National Institute of Mental Health, and Office of AIDS Research, of the National Institutes of Health, US Department of Health and Human Services, through cooperative agreement U01-AI-46749 with Family Health International, U01-AI-46702 with Fred Hutchinson Cancer Research Center, U01-AI-47984 and DA016555 with Johns Hopkins University, and U01-AI-48014 with the University of Pennsylvania.
Footnotes
Clinical trial registration: ClinicalTrials.gov Identifier: NCT00038688
References
- (1).DeJong W, Schneider SK, Towvim LG, Murphy MJ, Doerr EE, Simonsen NR, et al. A multisite randomized trial of social norms marketing campaigns to reduce college student drinking. J Stud Alcohol. 2006 Nov;67(6):868–879. doi: 10.15288/jsa.2006.67.868. [DOI] [PubMed] [Google Scholar]
- (2).Eisenberg ME, Neumark-Sztainer D, Story M, Perry C. The role of social norms and friends’ influences on unhealthy weight-control behaviors among adolescent girls. Soc Sci Med. 2005 Mar;60(6):1165–1173. doi: 10.1016/j.socscimed.2004.06.055. [DOI] [PubMed] [Google Scholar]
- (3).Buhi ER, Goodson P. Predictors of adolescent sexual behavior and intention: a theory-guided systematic review. J Adolesc Health. 2007 Jan;40(1):4–21. doi: 10.1016/j.jadohealth.2006.09.027. [DOI] [PubMed] [Google Scholar]
- (4).Cox JM, Bates SC. Referent group proximity, social norms, and context: alcohol use in a low-use environment. J Am Coll Health. 2011 Jan;59(4):252–259. doi: 10.1080/07448481.2010.502192. [DOI] [PubMed] [Google Scholar]
- (5).Buckner JD, Ecker AH, Proctor SL. Social anxiety and alcohol problems: The roles of perceived descriptive and injunctive peer norms. J Anxiety Disord. 2011 Feb 13;25(5):631–638. doi: 10.1016/j.janxdis.2011.02.003. [DOI] [PubMed] [Google Scholar]
- (6).Dohnke B, Weiss-Gerlach E, Spies CD. Social influences on the motivation to quit smoking: main and moderating effects of social norms. Addict Behav. 2011 Apr;36(4):286–293. doi: 10.1016/j.addbeh.2010.11.001. [DOI] [PubMed] [Google Scholar]
- (7).Hamilton K, White KM. Extending the theory of planned behavior: the role of self and social influences in predicting adolescent regular moderate-to-vigorous physical activity. J Sport Exerc Psychol. 2008 Feb;30(1):56–74. doi: 10.1123/jsep.30.1.56. [DOI] [PubMed] [Google Scholar]
- (8).Wagner KD, Unger JB, Bluthenthal RN, Andreeva VA, Pentz MA. Cognitive behavioral theories used to explain injection risk behavior among injection drug users: a review and suggestions for the integration of cognitive and environmental models. Health Educ Behav. 2010 Aug;37(4):504–532. doi: 10.1177/1090198109357319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (9).Harrison A, Newell ML, Imrie J, Hoddinott G. HIV prevention for South African youth: which interventions work? A systematic review of current evidence. BMC Public Health. 2010 Feb 26;10:102. doi: 10.1186/1471-2458-10-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (10).Miner MH, Peterson JL, Welles SL, Jacoby SM, Rosser BR. How do social norms impact HIV sexual risk behavior in HIV-positive men who have sex with men?: multiple mediator effects. J Health Psychol. 2009 Sep;14(6):761–770. doi: 10.1177/1359105309338976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (11).Davey-Rothwell MA, Latkin CA, Tobin KE. Longitudinal analysis of the relationship between perceived norms and sharing injection paraphernalia. AIDS Behav. 2010 Aug;14(4):878–884. doi: 10.1007/s10461-008-9520-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (12).Latkin CA, Donnell D, Celentano DD, Aramrattna A, Liu TY, Vongchak T, et al. Relationships between social norms, social network characteristics, and HIV risk behaviors in Thailand and the United States. Health Psychol. 2009 May;28(3):323–329. doi: 10.1037/a0014707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (13).Nyborg K, Rege M. On social norms: The evolution of considerate smoking behavior. J Econ Behav Organ. 2003;52(3):323–340. [Google Scholar]
- (14).LaBrie JW, Hummer JF, Grant S, Lac A. Immediate reductions in misperceived social norms among high-risk college student groups. Addict Behav. 2010 Dec;35(12):1094–1101. doi: 10.1016/j.addbeh.2010.08.003. [DOI] [PubMed] [Google Scholar]
- (15).Clapp JD, Lange JE. Success and failure in social norms interventions. J Stud Alcohol. 2006 May;67(3):482–3. doi: 10.15288/jsa.2006.67.482. author reply 483-4. [DOI] [PubMed] [Google Scholar]
- (16).Vongchak T, Kawichai S, Sherman S, Celentano DD, Sirisanthana T, Latkin C, et al. The influence of Thailand’s 2003 ’war on drugs’ policy on self-reported drug use among injection drug users in Chiang Mai, Thailand. Int J Drug Policy. 2005;16(2):115–121. [Google Scholar]
- (17).Daosodsai P, Bellis MA, Hughes K, Hughes S, Daosodsai S, Syed Q. Thai War on Drugs: measuring changes in methamphetamine and other substance use by school students through matched cross sectional surveys. Addict Behav. 2007 Aug;32(8):1733–1739. doi: 10.1016/j.addbeh.2006.12.002. [DOI] [PubMed] [Google Scholar]
- (18).Des Jarlais DC, Friedman SR, Stoneburner RL. HIV infection and intravenous drug use: critical issues in transmission dynamics, infection outcomes, and prevention. Rev Infect Dis. 1988 Jan-Feb;10(1):151–158. doi: 10.1093/clinids/10.1.151. [DOI] [PubMed] [Google Scholar]
- (19).Pouget ER, Hagan H, Des Jarlais DC. Meta-analysis of hepatitis C seroconversion in relation to shared syringes and drug preparation equipment. Addiction. 2012 Jun;107(6):1057–1065. doi: 10.1111/j.1360-0443.2011.03765.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (20).Neaigus A, Friedman SR, Curtis R, Des Jarlais DC, Furst RT, Jose B, et al. The relevance of drug injectors’ social and risk networks for understanding and preventing HIV infection. Soc Sci Med. 1994 Jan;38(1):67–78. doi: 10.1016/0277-9536(94)90301-8. [DOI] [PubMed] [Google Scholar]
- (21).Latkin CA, Donnell D, Metzger D, Sherman S, Aramrattna A, Davis-Vogel A, et al. The efficacy of a network intervention to reduce HIV risk behaviors among drug users and risk partners in Chiang Mai, Thailand and Philadelphia, USA. Soc Sci Med. 2009 Feb;68(4):740–748. doi: 10.1016/j.socscimed.2008.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (22).Kamb ML, Fishbein M, Douglas JM, Jr, Rhodes F, Rogers J, Bolan G, et al. Efficacy of risk-reduction counseling to prevent human immunodeficiency virus and sexually transmitted diseases: a randomized controlled trial. Project RESPECT Study Group. JAMA. 1998 Oct 7;280(13):1161–1167. doi: 10.1001/jama.280.13.1161. [DOI] [PubMed] [Google Scholar]
- (23).Latkin CA, Kuramoto SJ, Davey-Rothwell MA, Tobin KE. Social norms, social networks, and HIV risk behavior among injection drug users. AIDS Behav. 2010 Oct;14(5):1159–1168. doi: 10.1007/s10461-009-9576-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (24).Crawford MT, McConnell AR, Lewis AC, Sherman SJ. Reactance, compliance, and anticipated regret. J Exp Soc Psychol. 2002;38(1):56–63. [Google Scholar]
- (25).Berg RC. Barebacking: a review of the literature. Arch Sex Behav. 2009 Oct;38(5):754–764. doi: 10.1007/s10508-008-9462-6. [DOI] [PubMed] [Google Scholar]
- (26).Bayer R. Stigma and the ethics of public health: not can we but should we. Soc Sci Med. 2008 Aug;67(3):463–472. doi: 10.1016/j.socscimed.2008.03.017. [DOI] [PubMed] [Google Scholar]
- (27).Stuber J, Galea S, Link BG. Smoking and the emergence of a stigmatized social status. Soc Sci Med. 2008 Aug;67(3):420–430. doi: 10.1016/j.socscimed.2008.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (28).Davey-Rothwell MA, Latkin CA. Gender differences in social network influence among injection drug users: perceived norms and needle sharing. J Urban Health. 2007 Sep;84(5):691–703. doi: 10.1007/s11524-007-9215-1. [DOI] [PMC free article] [PubMed] [Google Scholar]