To the Editor,
Biologically variable ventilation (BVV) involves the delivery of a fixed minute ventilation but with a variable respiratory rate and a correspondingly variable tidal volume. This type of ventilation introduces a more physiological breathing pattern than traditional types of mechanical ventilation. It has been shown to improve oxygenation and ventilation in various animal models of lung injury when compared with conventional monotonous assist control ventilation (AC).1-3
We report our preliminary experience with BVV in eight critically ill patients. With BVV, the ventilator is configured so that the product of the respiratory rate and tidal volume is constant. The average coefficient of variation in the size of tidal volume was 30%.
The local Research and Ethics Board of the University of Manitoba approved this study in February 2006, and informed consent was obtained from the patients’ legal representatives. The eight patients in this study were intubated and ventilated for at least 72 hr in the medical or surgical intensive care units at the Health Sciences Centre in Winnipeg. Their baseline ratio of partial pressure of arterial oxygen to the fraction of inspired oxygen (PaO2/FiO2) was 100-300 mmHg. The study was conducted as a crossover trial with patients acting as their own control. The patients were randomized to begin with either BVV or AC, and their lungs were ventilated for a four-hour period in each mode of ventilation.
The baseline tidal volume was set at 6 mL·kg−1 to comply with the adult respiratory distress syndrome (ARDS) protocol. The patients were switched to a modified Esprit® ventilator (Respironics, Carlsbad, CA, USA) that could be controlled by computer software. The computer ran a variability file that was recorded from a healthy individual and consisted of 1,489 breaths. Arterial blood gases, static lung compliance, and dead space (VD/VT) were measured every hour. After completion of the study, the patients were returned to their baseline mode of ventilation. Continuous variables were compared using repeated measures one-way analysis of variance with post hoc least squares matrices to enable between group and within group comparisons. For within group comparisons, a Bonferroni correction for multiple comparisons was used.
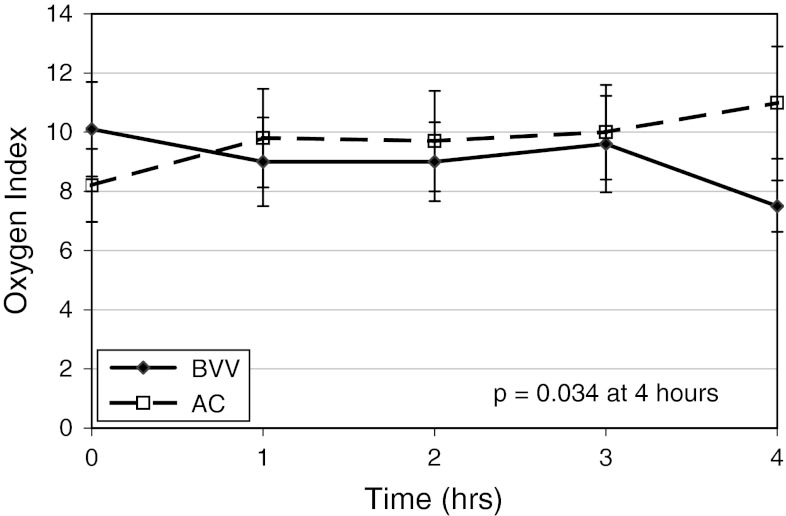
None of the patients required an increase in FiO2 or change in the level of positive end-expiratory pressure during the study. There was improvement in the oxygen index (FiO2 × mean airway pressure × 100 /PaO2) after four hours of BVV compared with AC (7.1 vs 11.5 cm H2O·mmHg−1, respectively; P = 0.034) (Figure). There was no statistically significant change in arterial PaCO2 after four hours of BVV. The VD/VT ratio decreased after four hours of BVV compared with AC (0.64 vs 0.68, respectively; P = 0.017) and lung compliance improved (0.36 vs 0.34 mL·cm H2O−1·kg−1, respectively; P = 0.049).
Figure.
Oxygen index vs time. The oxygen index (FiO2 × mean airway pressure × 100/PaO2, expressed in cm H2O·mmHg−1) in patients ventilated with biologically variable ventilation (BVV) compared with assist control ventilation (AC). At four hours, there was an improved oxygen index with BVV compared with AC (7.1 vs 11.5 cm H2O·mmHg−1, respectively; P = 0.034)
A series of mechanisms have been proposed to account for the improved ventilation with BVV in the setting of ARDS. A presumed mechanism is thought to be enhanced alveolar recruitment. Evidence for alveolar recruitment with BVV has been shown by computed tomography scanning in a porcine model of ARDS.3 If alveoli can be recruited and kept open, improved gas exchange and lung compliance would be expected with BVV. By using a variety of tidal volumes and respiratory rates, the probability of selecting the appropriate time constant for a given subpopulation of alveolar units is greatly increased. Recent editorials advocate for the role of “noisy” or physiological variability to aid ventilation of patients.4,5 This pilot project suggests that BVV may warrant further study as a mode of ventilation in patients who require controlled ventilation.
Acknowledgments
Competing interests
None declared.
References
- 1.Lefevre GR, Kowalski SE, Girling LG, Thiessen DB, Mutch WA. Improved arterial oxygenation after oleic acid lung injury in the pig using a computer-controlled mechanical ventilator. Am J Respir Crit Care Med. 1996;154:1567–1572. doi: 10.1164/ajrccm.154.5.8912782. [DOI] [PubMed] [Google Scholar]
- 2.Mutch WA, Harms S, Graham MR, Kowalski SE, Girling LG, Lefevre GR. Biologically variable or naturally noisy mechanical ventilation recruits atelectatic lung. Am J Respir Crit Care Med. 2000;162:319–323. doi: 10.1164/ajrccm.162.1.9903120. [DOI] [PubMed] [Google Scholar]
- 3.Graham MR, Gulati H, Kha L, Girling LG, Goertzen A, Mutch WA. Resolution of pulmonary edema with variable mechanical ventilation in a porcine model of acute lung injury. Can J Anesth. 2011;58:740–750. doi: 10.1007/s12630-011-9517-3. [DOI] [PubMed] [Google Scholar]
- 4.Shimabukuro DW, Gropper MA. Noisy mechanical ventilation: listen to the melody. Anesthesiology. 2009;110:214–215. doi: 10.1097/ALN.0b013e3181945b63. [DOI] [PubMed] [Google Scholar]
- 5.Allardet-Servent J. Adding noise to mechanical ventilation: so obvious! Crit Care Med. 2012;40:2725–2726. doi: 10.1097/CCM.0b013e31825bc827. [DOI] [PubMed] [Google Scholar]