Abstract
Many studies have provided strong evidence of a fundamental and complex role for sleep disturbances in adult posttraumatic stress disorder (PTSD). Investigations of adult PTSD using subjective and objective measures document sleep architecture abnormalities and high prevalence of sleep disordered breathing, periodic limb movement disorder, nightmares, and insomnia. PTSD treatment methods do appear to significantly improve sleep disturbance, and also studies suggest that treatments for sleep disorders often result in improvements in PTSD symptoms. Further, the most recent evidence suggests sleep abnormalities may precede the development of PTSD. Given the importance of sleep disorders to the onset, course, and treatment of adult PTSD, examination of sleep disturbances far earlier in the life course is imperative. Here we review the literature on what we know about sleep disturbances and disorders in pediatric PTSD. Our review indicates that the extant, empirical data examining sleep disturbance and disorders in pediatric PTSD is limited. Yet, this literature suggests there are significantly higher reports of sleep disturbances and nightmares in children and adolescents exposed to trauma and/or diagnosed with PTSD than in non-trauma-exposed samples. Sleep questionnaires are predominantly employed to assess sleep disorders in pediatric PTSD, with few studies utilizing objective measures. Given the important, complex relationship being uncovered between adult PTSD and sleep, this review calls for further research of sleep in children with PTSD using more specific subjective measures and also objective measures, such as polysomnography and eventually treatment trial studies.
Citation:
Kovachy B; O'Hara R; Hawkins N; Gershon A; Primeau MM; Madej J; Carrion V. Sleep disturbance in pediatric PTSD: current findings and future directions. J Clin Sleep Med 2013;9(5):501-510.
Keywords: Pediatric, PTSD, sleep disturbance, subjective measures, objective measures
Traditionally, sleep disorders have been understood as a secondary symptom of posttraumatic stress disorder (PTSD). Further, it was presumed that treatment of the overarching PTSD disorder would eliminate these sleep disturbances.1 Studies now suggest that sleep disturbances, including insomnia, nightmares, sleep disordered breathing (SDB), and periodic limb movement (PLM), play a central, complex role in PTSD with accompanying diagnostic, treatment, and neurobiological implications. However, far more empirical data exist on the prevalence and nature of sleep disturbances in adults diagnosed with PTSD than in youth diagnosed with PTSD.
Significance of Sleep Disorders to PTSD: Summary of Evidence From Adult Studies
Sleep disturbances are a frequent occurrence in adults with PTSD, with one study finding 70% to 91% of PTSD patients have sleep disturbances.2 In a comparison to healthy controls, patients with PTSD report much higher initial, middle, and terminal insomnia.3,4 Ohayon and Shapiro found that 18.8% of patients with PTSD reported nightmares, as opposed to their non-patient comparison group, in which only 4.2% reported nightmares.4 SDB and PLM are sleep disorders that have also been frequently observed among PSTD patients. Sleep architecture profiles also appear different in patients with PTSD (for review see Kobayashi5).
Further, after a trauma, individuals who would develop PTSD experienced shorter, more frequent REM sleep periods, which were associated with both insomnia and PTSD severity.6,7 Similarly, a prospective investigation of car accident victims revealed that severity of sleep complaints 1 month after the accident was significantly associated with the subsequent development of PTSD a year after the accident.8 The culminating evidence from investigations of adults with PTSD suggests that not only are specific sleep disorders and specific sleep architecture profiles more prevalent in PTSD, they may also precede and/or predict the development and severity of PTSD.6–12
Further evidence of the important yet complex relationship between sleep disturbances and adult PTSD stems from treatment results for both disorders.13 Evidence suggests that although PTSD-focused treatment may lead to some improvement in co-occurring sleep disorders, it does not lead to complete remission of the sleep disorder and may also leave patients vulnerable to recurrence of PTSD symptoms.14,15 These findings highlight the intrinsic severity of sleep problems, or alternatively, our gap in knowledge in identifying targets for sleep treatments. They also challenge the notion that sleep disorders in PTSD are merely secondary symptoms best treated by treatment of the overarching disorder.
The utilization of specific treatments for sleep disturbances that accompany PTSD appears to lead to significant improvements in both sleep disturbances and global PTSD symptoms.13,16–19 For example, the use of the drug prazosin to treat sleep disturbances significantly improved nightmare severity, insomnia, and also other PTSD symptom clusters such as re-experiencing and hyperarousal (measured by the Clinician-Administered PTSD Scale) in comparison to controls.20 In a placebo-controlled trial, Germain et al. found that treatment of sleep disturbances with prazosin or cognitive behavioral therapy (CBT) improved sleep disturbances and daytime PTSD symptoms in a sample of veterans (n = 50).21 Ulmer et al. found that the use of CBT for insomnia and imagery rehearsal therapy for nightmares significantly reduced insomnia and global PTSD symptoms.22 Similarly, treatment of SDB with continuous positive airway pressure has been found to reduce nightmares and improve overall PTSD symptoms.17,23 Given that poor sleep quality is associated with increased stress and anxiety, perhaps sleep treatments are successful in reducing global symptoms of PTSD because improvements in sleep quality result in improved resilience to new stressors and, in turn, reduced stress and anxiety. Taken together, these studies indicate the importance of targeting sleep disturbances to successfully treat PTSD and further suggest a fundamental role of sleep dysregulation in the maintenance of PTSD.16–24
In sum, the literature from adult studies of PTSD suggest that (a) sleep disturbances, particularly nightmares, are frequent symptoms of PTSD; (b) sleep disturbances often occur following a trauma prior to PTSD onset and may confer increased vulnerability for development of PTSD; (c) sleep disturbances predict global PTSD symptom severity; (d) sleep disturbances are often a residual symptom following treatment of PTSD; and (e) treatment of sleep disorders yields strong improvement in PTSD symptoms. Given the importance of sleep disorders to the onset, course, and treatment of adult PTSD, examination of sleep disturbances far earlier in the life course is imperative. Sleep disturbances may serve as a critical bio-marker for the development of pediatric PTSD. Indeed, sleep disturbances in childhood may increase the vulnerability for developing PTSD at any stage of the lifespan. At least, identification of the types of sleep disturbances and/or sleep disorders that occur in pediatric PTSD can provide key therapeutic targets, as most sleep disorders have available treatments. By normalizing sleep patterns, such treatments may in turn alleviate the symptoms of PTSD. Here we summarize the main findings on sleep in pediatric PTSD.
Pediatric PTSD and Sleep Disorders
Currently, our knowledge about the fundamental sleep disorders, sleep dysregulation, and sleep architecture abnormalities that occur in children with PTSD is limited. Few studies have investigated the prevalence of pediatric PTSD. One investigation by Kilpatrick et al. found that 3.7% of males and 6.3% of females in a nationally representative sample of 4,023 children aged 12 to 17 years met DSM-IV diagnostic criteria for PTSD.25,26 However, studies specifically examining children exposed to trauma reveal much higher rates of PTSD. For example, in a Pynoos et al. study of 159 child witnesses of a sniper attack, 60.4% were diagnosed with PTSD.27 In children exposed to trauma, PTSD may be very prevalent and underestimated.
Sleep Disturbances in Pediatric PTSD: Evidence from Subjective Measures
To date, the most extensively used methods for measuring sleep disturbances in children with PTSD are self-report questionnaires, parent-report questionnaires, and clinical interviews. Many studies use the Child Post-Traumatic Stress Reaction Index (CPTSD-RI), a self-report questionnaire that assesses for nightmares and sleep disturbances, along with other PTSD symptoms.
In children exposed to trauma, the frequency of sleep disturbances as measured by self-report or parent-report is higher than in non-trauma exposed populations of children (see Tables 1 and 2; for additional review see Charuvastra and Cloitre28). Noll et al. examined sleep in 78 sexually abused children and 68 control comparison children using 6 self-report questions that asked about trouble falling asleep, staying asleep, middle of the night awakenings, nightmares, and feeling rested.29 The subjects were 6 to 16 years at the time of abuse, and the mean age for the participants at the time of the study was 20.41 (SD = 3.38). The results revealed significantly more sleep disturbances, including insomnia and nightmares, in the sexually abused group and more instances of PTSD in the sexually abused group.29
Table 1.
Nightmares and sleep disturbance in average populations of children
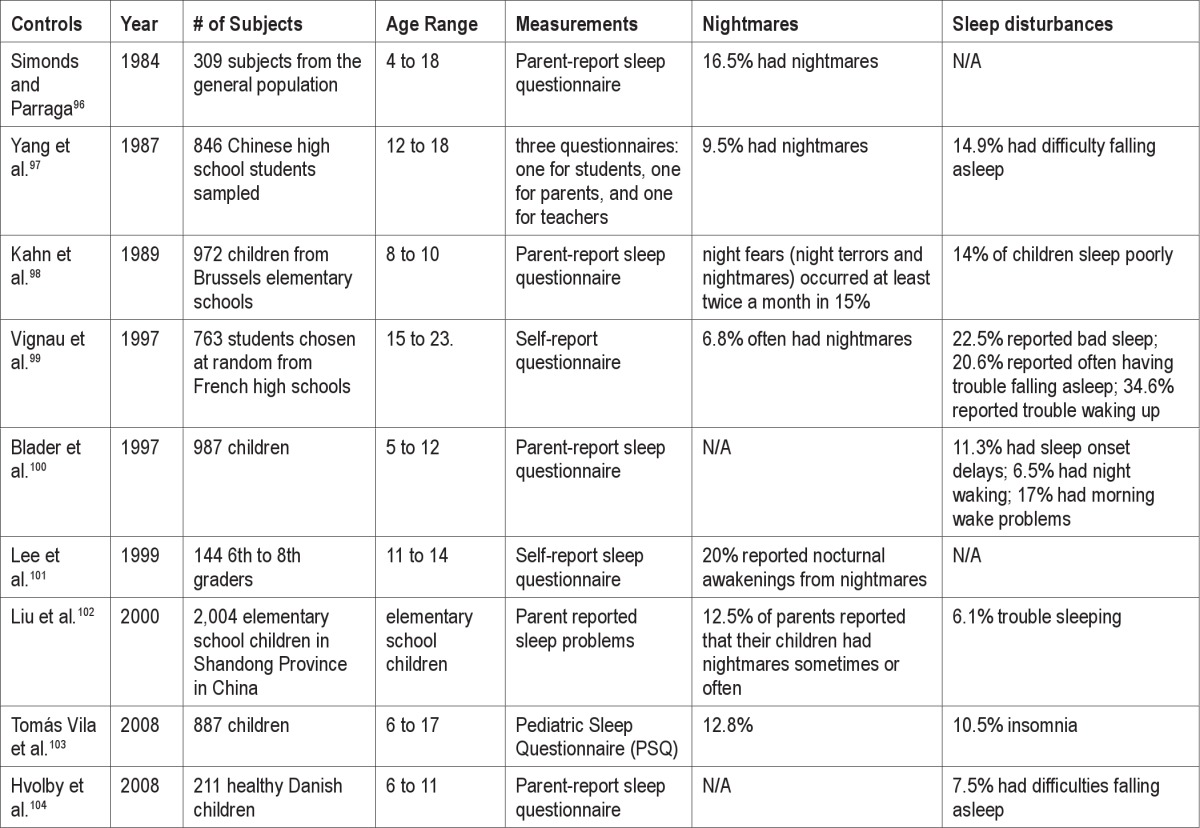
Table 2.
Nightmares and sleep disturbances in children exposed to trauma
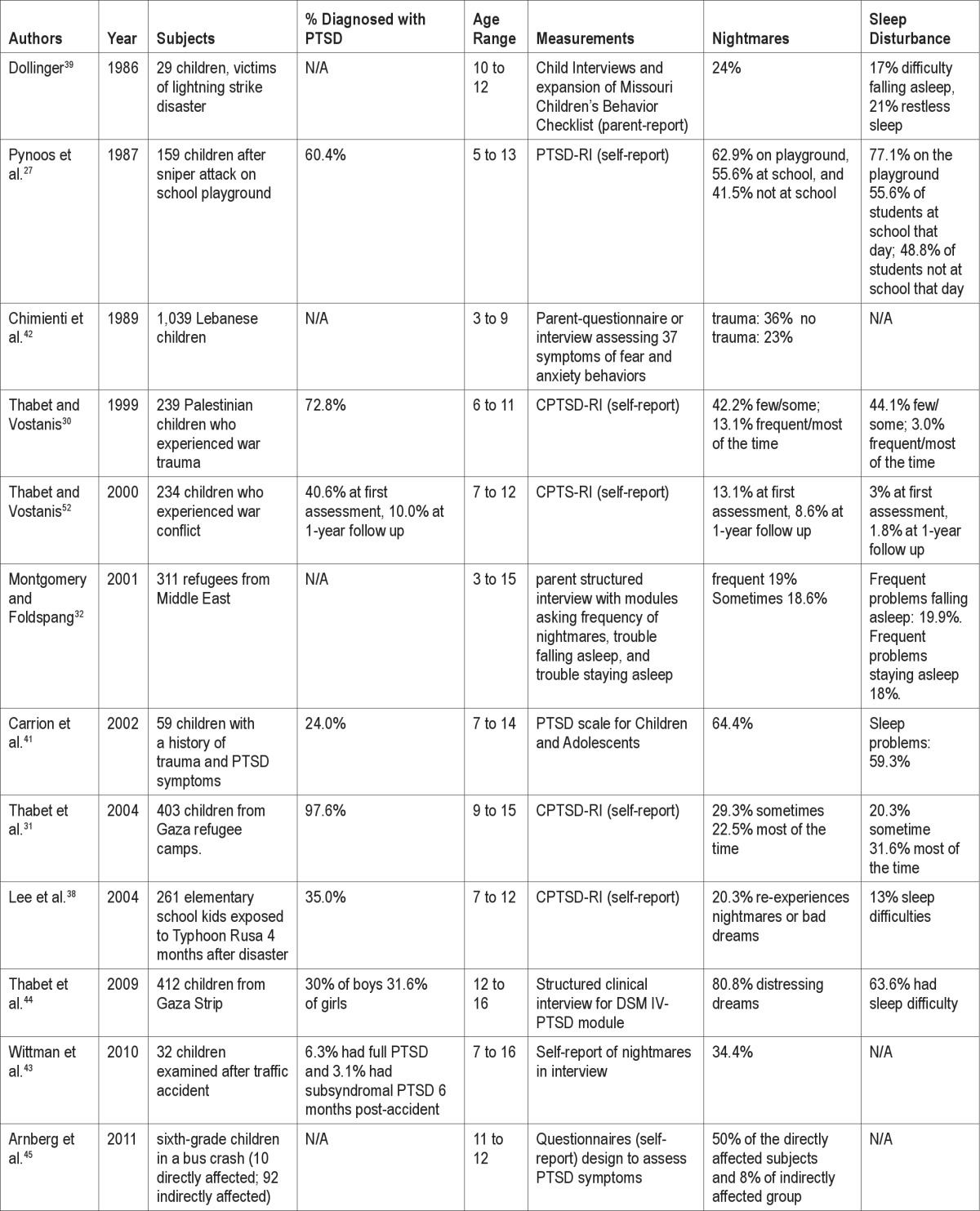
Children exposed to war trauma and/or violence often have sleep disturbances.27,30–37 Thabet et al. examined 403 children aged 9-15 years living in refugee camps and found that 20.3% reported sleep disturbances “sometimes” and 31.6% reported sleep trouble “mostly, most of the time.” 31 Similar rates of sleep disturbance were found among 311 Middle East refugee children aged 3-15 years. Specifically, sleep symptoms, such as nightmares and difficulties falling and staying asleep, were reported as “frequent” by nearly 20% of the children's parents.32 Following a playground sniper attack in Los Angeles, Pynoos et al. found that 77.1% of children on the playground reported sleep disturbances one month following the trauma.27 Nineteen children who were on the playground were followed longitudinally. At 14-month follow-up, 57.9% of this sample still reported sleep disturbances.33 A sample of 120 preadolescent Kuwaiti boys and girls (9-12 years old) who were initially assessed for exposure to war-related trauma during the Iraqi occupation and Gulf war of 1990 were reassessed for general health and sleep, using the Pittsburgh Sleep Quality Index (PSQI), approximately 10 years later. Findings showed direct effects between exposure to war related trauma and sleep difficulties, even after controlling for stressful life events experienced in the interim.34
A national phone survey of adults (N = 560) administered within 5 days of the 9/11 terrorist attacks in New York City attacks found 10% reporting that their children were experiencing difficulty falling or staying sleeping.35 Approximately one-fifth of residents living close to the World Trade Center, including children and adolescents, suffered symptoms of PTSD.36 A longitudinal study of preschoolers (N = 116) who were exposed to the World Trade Center attacks found that three years following the exposure, children who were exposed to “high-intensity” events of the attacks (e.g., witnessing the towers collapse, injured people, dead bodies, or people jumping out of the building) were approximately 5 times more likely to have sleep problems (assessed using the Child Behavior Checklist or CBCL) than those who had not been exposed to high-intensity events.37 Furthermore, a dose-response relationship was found, such that the greater the number of high-intensity events a child was exposed to, the greater the risk for sleep problems.37
Studies with children who experienced natural disasters similarly reveal associated sleep disturbance.38–40 After a typhoon in South Korea, 13% of a local sample of elementary school children (N = 261) experienced sleep disturbances.38 Following a lightning strike during a children's soccer game, 17% of exposed children (N = 29) experienced difficulty falling asleep and 21% had restless sleep.39 In an important recent longitudinal investigation, Brown et al. assessed sleep disturbance and fear of sleeping using the Revised Child Anxiety and Depression Scales in a sample of 202 children (aged 8 to 15 years) 24 months after they experienced trauma from Hurricane Katrina.40 Severity of sleep disturbance was associated with severity of PTS (post traumatic stress) symptoms. In addition, the presence of sleep disturbances 24 months after the hurricane was positively associated with the severity of PTS symptoms 30 months after the hurricane. In their analysis the authors controlled for age, sex, and severity of PTS symptoms at 24 months.40 Severely traumatic events have been shown to have both an immediate and long-term adverse impact on sleep in exposed youth. Findings further suggest that sleep disturbance after a trauma may serve as biomarker for subsequent PTSD in children,40 consistent with findings from the adult investigations discussed earlier.6–12
In both adult and child PTSD samples, self-reported nightmares also appear to play a role and may contribute to sleep disturbance in this disorder. According to the DSM IV, three of the main symptomatic groups for PTSD after exposure to a trauma are re-experiencing trauma symptoms, avoidance symptoms, and hyperarousal symptoms. Many nightmares experienced by PTSD patients are re-enactments of the trauma and thus account for the first DSM-IV PTSD symptomatic group.26
Many studies find nightmares occur in about 10% to 20% of the general pediatric population (Table 1). In addition, younger children tend to have more nightmares than adolescents (Table 1). In pediatric PTSD and trauma-exposed populations, parent-report, self-report, and clinician-administered questionnaires reveal higher reports of nightmares than in average populations (Table 2). Carrion and colleagues utilized a structured interview, the Clinician Administered PTSD Scale for Children and Adolescents (CAPS-CA), to assess posttraumatic symptomatology in a group of youth exposed to interpersonal violence. Sixty-four percent of the sample experienced distressing nightmares that were not only frequent but also intense in nature.41 Chimienti et al. compared the sleep reports from parents of Lebanese children, ages 3 to 9 years, who had experienced a trauma (n = 312) to reports from parents of children who had not experienced a trauma (n = 727).42 Thirty-six percent of parents in the trauma-exposed group reported nightmares in their children, which was significantly different from the 23% of parents in the no-trauma group who reported nightmares in their children.42
Several studies have documented similar rates of nightmares in children after a trauma,30,31,32,38,39,43 with some studies reporting prevalence rates as high as 50% to 80%.27,41,44 Arnberg et al. found that 50% of a group of sixth-grade children (ages 11 to 12 years) who were involved in a serious bus accident reported nightmares 9 months after the accident, compared to only 8% of indirectly affected children (classmates of the children in the crash).45 Cumulatively, these data strongly indicate high prevalence of nightmares among children exposed to trauma (Table 2). However, it should be noted that use of control groups is rare in these studies.
Some investigators have published their experiences with use of prazosin, clonidine, and guanfacine in individual case studies of children with PTSD, demonstrating modest improvement in sleep assessed subjectively, mostly in reducing nightmares.46–50 Behavioral treatments form the cornerstone of treatment of pediatric PTSD, yet little work has been done evaluating the impact of such treatments on sleep symptoms specifically. One behavioral treatment, image rehearsal therapy (IRT), a treatment for nightmares with demonstrated effectiveness in adult patients with PTSD, has been modified for treatment in adolescent populations.51 Krakow et al. adapted IRT for adolescent girls (ages 13-18) sentenced to Wyoming Girls School. They were able to decrease nightmare frequency and subjective distress, though PTSD symptoms and overall sleep complaints did not improve.51
Together, self-report studies find significantly higher reports of sleep disturbances and nightmares in children and adolescents who were exposed to trauma and/or diagnosed with PTSD than in non-trauma-exposed samples. However, there is considerable variability among these studies in the amount of sleep disturbances reported, ranging from 3% to 77.1%, and in the amount of nightmares reported, ranging from 20.3% to 80.8% (Table 2). This variability may reflect the use of unspecific, brief sleep questionnaires and the different study methods used across studies, including different populations examined, differing levels of PTSD severity and diagnosis, nature and duration of trauma, sample size, age, and other cultural and demographic variables.
For example, most studies measure subjective sleep disturbances in children exposed to a trauma. Thus, not all subjects examined have developed or will develop PTSD even if they experience some PTSD symptoms after the trauma. In fact, in some of the studies, only a minority of the sample have diagnosable PTSD.38,41,43,44,52 Other studies do not distinguish between disturbance of individuals who have been exposed to a trauma and individuals who have developed PTSD.32,39,42,45 In addition, the nature, intensity, and duration of the trauma experienced by the populations vary greatly across studies. Some subjects directly experienced a traumatic event, while others were witnesses. Additionally, whether the trauma is an acute event (e.g., lightning strike) or a chronically ongoing trauma (e.g., sexual or physical abuse) could significantly influence the degree and type of sleep dysregulation reported. Studies also varied in the temporal duration between the trauma exposure and the time of the sleep assessment, which may also contribute to variable outcomes.
A significant limitation to these approaches is that the measures used to assess sleep are often designed for clinical assessment of PTSD symptoms and as such, contain only a minimal subset of questions addressing the child's sleep. Many studies examined in this review assess sleep in pediatric PTSD using the CPTSDRI,27,30,31,38,52 which is the pediatric version of the PTSD-RI intended to diagnose PTSD in pediatric populations. The CPTSD-RI asks the subject to rate degree of sleep disturbance and nightmares but does not ask more targeted questions about the nature and frequency of these sleep disturbances. Some ask nonspecifically about any sleep disturbance covering the general sleep patterns of the child, while others may be more specifically oriented to circadian tendency, SDB, or insomnia. Even when subjective assessments focus on a specific sleep disorder, they can vary with respect to the type and quality of sleep disturbance they assess. However, subjective sleep measures can be extremely valuable for indicating that the child's sleep is indeed disturbed.
While some pediatric studies will simply employ subjective measures of sleep that are validated for adults,34 e.g., the PSQI, several subjective assessments of pediatric sleep exist. In a recent review, Spruyt and Gozal identified 183 available measures, of which 57 had been psychometrically evaluated to some degree.53 These questionnaires are self-report or parent-report. As pointed out by Spruyt and Gozal, there is little consensus as to which questionnaire is most appropriate to evaluate sleep in pediatric populations. As these measures often focus on a specific sleep disturbance or disorder, it makes comparisons among studies difficult. However, each of these scales can provide information that is useful depending upon the clinical or research setting.53
Potential subjective specific sleep measures which can enhance the understanding of sleep disorders in pediatric PTSD include the Child Behavior Checklist (CBCL),54,55 the Pediatric Sleep Questionnaire (PSQ),56 the Sleep Disturbance Scale for Children (SDSC),57 Sleep Disorders Inventory for Students-Child and Adolescent form (SDIS),58 Childhood Sleep Habit Questionnaire (CSHQ),59 the Nightmare Frequency Questionnaire (NFQ),60 the Nightmare Distress Questionnaire (NDQ),61 and sleep diaries.
The CBCL is a parent-report subjective questionnaire that assesses child behavior difficulties and includes certain items on sleep including: “sleeps less than most kids,” “sleeps more than most kids during day and/or night,” “trouble sleeping,” “nightmares,” and “talks or walks in sleep.”54,55 In a sample of 122 youth, ages 7-17 years, with anxiety disorders (19%), major depressive disorder (MDD) (9%), both anxiety and depression (26%), or no history of any psychiatric disorder (46%), Gregory et al. examined how sleep items in the CBCL corresponded to sleep measured via sleep diaries (4-6 days), actigraphy (1 week), and polysomnography (2 consecutive nights).62 After controlling for age, gender, and diagnostic status, specific items (e.g. being overtired, sleeps less, sleeps more, and trouble sleeping items) correlated well with objective sleep measures of sleep latency and number of arousals. However, some items did not correlate with objective measures; for example, “sleeps more” was not associated with total sleep time (TST) as assessed by objective polysomnography.62 Overall, the CBCL can be a valuable tool in assessing broad sleep disturbance subjectively. However, similar to the PTSD scales mentioned above, the CBCL ultimately is not designed to thoroughly evaluate sleep, and thus cannot always provide important information on the source of sleep disturbances such as breathing related sleep disorders.
As Spruyt and Gozal53 point out, 3 well-validated subjective assessments of pediatric sleep include the PSQ, the SDSC, and the SDIS. The PSQ is a 22-item questionnaire, well documented to be a reliable and valid measure for assessing snoring, insomnia, sleepiness, and associated daytime behaviors. It is considered to be a valuable alternative when polysomnography is not realistically available to measure specific sleep disorders in pediatric populations.56 Similarly, the SDSC is a 27-item parent questionnaire designed to assess disorders of initiating and maintaining sleep, insomnia, SRBDs, arousal disorders, sleep-wake transition disorders, sleepiness, and sleep hyperhidrosis in children.57,63 The SDIS evaluates SDB, excessive sleepiness, PLM, delayed sleep phase syndrome, and narcolepsy. It was designed for children aged 2-18 years, it is a parent-report questionnaire, and it includes computer scoring.53,58 However, it was developed to be used as a screening tool to determine which children should be referred to a sleep physician and not for the assessment of sleep disorders per se (although the scale is moderately accurate at determining the specific sleep disorder a subject has).64
The CSHQ is 45-item parent-report subjective questionnaire with 7 components assessing bedtime behavior, sleep onset, sleep duration, anxiety related to sleep, sleep and night waking behavior, SDB, parasomnias, and morning waking and daytime sleepiness.59 In a community sample of 469 children and 154 children with diagnosed sleep disorders, aged 4-10 years, sensitivity and specificity were 0.80 and 0.72, respectively.59 The CSHQ has also been employed to examine sleep in children aged 2 to 5.5 years old with autism diagnoses (n = 68), developmental delay (n = 57), and normal development (n = 69).65 This indicates that the CSHQ can be clinically utilized in even younger populations than children aged 4 to 10 years and in populations with developmental disorders. However, as yet, the CSHQ has not been utilized in pediatric populations of PTSD.
To assess frequency of nightmares and the level of associated daytime distress these nightmares cause, several questionnaires are employed. The Nightmare Frequency Questionnaire (NFQ) consists of 2 brief sections, and was validated in a sample of adults with PTSD who experienced sexual assault.60 Further, correlations between frequency of nightmares as determined by the NFQ and by prospective nightmare dream logs were highly significant.60 However, the NFQ has not yet been validated for pediatric populations. While the NFQ measures nightmare frequency, the Nightmare Distress Questionnaire (NDQ) is a 13-item questionnaire that measures the distress individuals experience during the day about their nightmares. It has been employed in pediatric as well as adult samples.61,66 One investigation in children aged 5 to 11 years used 3 simple, child-appropriate questions as follows: (1) Have you ever had a nightmare?; (2) How frequently do you experience nightmares?; (3) How scary would you rate the nightmare to be?67 While these methods have not been psychometrically evaluated in children, they may provide a useful, brief assessment regarding the frequency of nightmares and the subsequent distress associated with the nightmares in pediatric PTSD populations.
Sleep diaries are well documented to be an important means to assess sleep-wake and circadian rhythm patterns, and have been effectively used in pediatric populations, including children with autism spectrum disorders.68 Yet, in pediatric populations, discrepancies between sleep time scored by actigraphy and sleep time reported in sleep diaries have been identified.69 The authors suggest that this may occur because actigraphy measurement can overestimate wake after sleep onset time and underestimate total sleep time in pediatric populations. The authors also found that sleep characterization by sleep diary was well correlated with sleepiness and fatigue, but actigraphy recordings were not.69 Sleep diaries are considered important for the fuller characterization of sleep-wake patterns when employed in conjunction with actigraphy.
Subjective assessments of healthy and traumatized children do not always specify the frequency of sleep disturbances, which can be important for differentiating normal sleep from a clinically significant condition. Also, subjectively assessed sleep disturbances can reflect a broad range of sleep disorders, such as PLM, insomnia, restless leg syndrome, circadian rhythm disturbance, and SDB.70 Sleep questionnaires do not always provide sufficient information to identify which sleep disorders the subjects may suffer from, although more specific, targeted sleep questionnaires are evolving, such as the Pediatric Restless Legs Syndrome Severity Scale,71 to better characterize specific sleep disorders in youth. Even the most comprehensive subjective sleep measures cannot fully characterize sleep architecture, or capture the full spectrum of sleep disorders potentially underlying any identified sleep disturbance. However, when objective studies of sleep are not a realistic option—because of funding issues, population dynamics, or large samples in epidemiological studies—specific subjective sleep measures can provide a valuable, valid, and reliable assessment of sleep. As such, subjective measures of pediatric sleep could be used to significantly increase our understanding of sleep in psychiatric disorders in children who are already undergoing clinical assessment. Further, a comprehensive clinical interview in combination with pediatric sleep questionnaires and diaries represents a particularly reliable and valid approach for identifying specific sleep disorders, such as circadian rhythm disorders and insomnia.
Subjective measures and questionnaires also identify a significant problem in pediatric PTSD that needs further examination: namely, children with PTSD report having more sleep disturbances and nightmares than do normal populations of children. Given the methodological limitations of the subjective understanding of pediatric PTSD and sleep, studies employing more specific sleep questionnaires and interviews to assess nightmares and objective measures to assess sleep disturbance would provide a more complete understanding of the sleep dysregulation in pediatric PTSD. To date, however, very few studies have utilized objective measures to record sleep in children with PTSD.
Sleep Disturbances in Pediatric PTSD: Evidence from Objective Measures
Actigraphy and polysomnography are the most common methods of objectively measuring sleep. Actigraphic methods measure sleep-wake activity, which during the night includes TST, sleep onset latency, sleep efficiency, and number of awakenings. Studies using actigraphy in children with psychiatric disorders tend to support the findings of subjective sleep questionnaires. In a sample of 122 children aged 7 to 17 years diagnosed with MDD, an anxiety disorder, or both, those who reported “trouble sleeping” were also more likely to have longer sleep onset latency as recorded by actigraphy.62 Sadeh et al. performed actigraphic measurements on 39 children (7 to 14 years old) in a psychiatric inpatient unit. The children were divided into 3 groups, those who had experienced physical abuse, sexual abuse, or no abuse. Children who experienced physical abuse had significantly more fragmented sleep than the children who had experienced no abuse or sexual abuse. The physical abuse group had a quiet sleep percentage (the percent of sleep without movement) of 58.3%, which was significantly lower than the 67.8% of quiet sleep of the group with no abuse and 67.3% of the sexual abuse group. These results suggest physical abuse may lead to greater fragmentation of sleep and poorer overall sleep quality. Although the authors used actigraphy on 8 children with PTSD, they did not differentiate between those with and without PTSD in their analysis, so no direct relationship between disturbed sleep and childhood PTSD can be inferred.72
Using actigraphy, Glod et al. measured sleep over 3 consecutive nights in a sample of 19 abused children (13 were diagnosed with PTSD), 10 depressed children, and 15 non-abused controls.73 The children were aged 6 to 12 years. The abused children with PTSD had significantly higher sleep onset latencies compared to both the depressed and the control groups. Further, the nocturnal activity in the group with PTSD and abuse was almost twice that of controls. Although abused children with and without PTSD had significantly more sleep impairments than controls, when the authors compared the abused PTSD and non-PTSD groups, they found more sleep impairments in the non-PTSD group.73 This suggests that the sleep disturbances observed may be more related to abuse than to the presence of PTSD per se. Still, the sample sizes were quite small in both these studies,72,73 and more in-depth, larger studies are required to further address this important issue.
Overall, the extant data from actigraphic investigations of pediatric PTSD suggest that this population experiences increased sleep onset latency, nocturnal activity, and fragmentation of sleep. That said, it remains to be determined which specific aspects of sleep-wake activity, specifically nocturnal activity, are disturbed in children with PTSD, given the limited amount of research using actigraphy to investigate sleep in children with PTSD.
Polysomnography is considered the gold standard for characterizing sleep architecture. It provides measurements of sleep architecture including REM sleep, stages 1 and 2 sleep, slow wave sleep (SWS), REM latency, sleep latency, and sleep efficiency. To date, there are no studies that have specifically employed polysomnography to measure sleep disturbances, disorders, and architecture in children with PTSD. However, several polysomnography studies have been conducted on adults with PTSD. These studies reveal high rates of SDB and PLM in adult PTSD patients—disorders that could help explain the sleep disturbances frequently reported by adults with PTSD.9,74,75 Further, among this population, abnormalities in REM and SWS are frequently observed. Yet, the results of the studies are sometimes inconsistent. A recent meta-analytic review of twenty polysomnographic studies5 found overall modest differences in sleep in adult patients with PTSD. Adult PTSD patients typically exhibit less SWS, higher REM density, and more stage 1 sleep than do controls.5,28 The authors suggest that their findings support previous findings of centrally measured hyperarousal in PTSD patients.5 The authors also found a significant moderating effect of age, with reduced TST in the younger patients and decreased SWS and REM density in older adults, suggesting different sleep architecture profiles at different stages of the lifespan. These age effects suggest the modest differences observed in the sleep of adults with PTSD cannot be taken as evidence that substantial differences may not exist in the sleep of children with PTSD. Further, the authors were not able to fully disentangle the effects of age and time since the index trauma.5 Since children likely are closer to the index trauma temporally, by virtue of their age, the effects on sleep and sleep architecture may be more profound.
The meta-analysis also identified comorbid depression as an important moderating factor of the relationship between PTSD and sleep disturbances. Specifically, studies in which adult PTSD patients had lower rates of comorbid depression tended to show greater sleep abnormalities.5 As such, comorbid psychiatric symptoms may contribute to differences in sleep in patients with PTSD.
Better characterization of sleep in children exposed to trauma may provide further insights into the development of PTSD in adults as well as guidance for areas of potential intervention or prevention. To date, we are aware of no polysomnographic study of pediatric PTSD. Polysomnography studies of healthy populations of children provide a base for comparison.76–78 One study by Ohayon et al. examined many studies of control populations of all ages. They found that TST, SWS, and REM latency decreased as age increased for the entire lifespan as well as for childhood through adolescence. Additionally, their meta-analysis revealed that stage 2 sleep percentage slightly increased with age. Across the life span, sleep latency and stage 1 sleep percentage increased with age and sleep efficiency decreased with age, although no significant changes with age were found within childhood and adolescence. Lastly, they found that REM sleep time increased until adolescence and then decreased throughout adult life.78
While there are no polysomnography studies on children with PTSD, Forbes et al. utilized polysomnography to investigate groups of children from 7 to 17 years old: 24 with anxiety disorders, 128 with major depressive disorder, and 101 with no psychiatric disorder.79 The authors found that the children with anxiety disorders had less SWS, greater sleep onset latency, and more awakenings than the control or major depressive disorder group. While this study examined children with any anxiety disorders and not specifically PTSD, the general trends are consistent with those found in adults with PTSD.79
Longitudinal studies have implicated a connection between childhood sleep problems and future neuropsychological functioning and psychiatric symptomatology, including depression and anxiety.81–84 For example, one study found in a sample of 6,000 twins pairs followed at ages 3, 4, and then again at age 7, that sleep disturbance reported at ages 3 and 4 predicted anxiety at age 7.82 In yet another investigation, the sleep and behavioral/ emotional problems of 499 children were measured by the CBCL. Reported sleep problems at age 4 were predictive of behavioral/ emotional problems in mid adolescence.83 A bidirectional and interactive relationship between sleep and stress-related psychiatric symptoms and disorders has been proposed.85,86 The authors suggest that patterns of sleep disturbance early in life may actually increase vulnerability to the subsequent development of stress-related behavioral and psychiatric disorders, while stressful events and associated symptoms may increase the risk for the development of sleep disturbance and sleep disorders later in life. Indeed, recent empirical evidence suggests that nightmares increase the risk for the development of PTSD.86 Specific aspects of sleep wake patterns, sleep macroarchitecture, and microarchitecture including sleep spindles may serve as important biomarkers of developmental and psychiatric disorders.87–90 For example, Buckley et al. found that children with autism spectrum disorder had reduced REM sleep and increased REM latency relative to typically developing children and those with developmental delay, and have begun to consider pharmacological approaches for augmentation of REM in autism spectrum disorder.91,92 Similar approaches may be valuable for increasing our understanding and treatment of pediatric PTSD.
Polysomnography is required to measure sleep macro and microarchitecture, and as a result, we know little about these features in pediatric PTSD. Further, while a comprehensive clinical interview, combined with sleep questionnaires and sleep diaries, can help diagnose circadian rhythm disorders and insomnia, subsets of the bioparameters measured by polysomnography, such as electroencephalogram (EEG), electrooculogram (EOG), submental electromyogram (EMG), expiratory/inspiratory nasal airway pressure, nasal/oral airflow, finger pulse oximetry, electrocardiogram (ECG), movements of the rib cage and abdomen, snoring, and body position, are integral to the diagnosis of many sleep disorders, including sleep apnea, REM disturbance, and PLMs. Sleep disturbance can reflect very different sleep disorders. Highly effective treatment approaches are available for many of these sleep disorders, not only ameliorating and alleviating the sleep disturbance itself, but also improving daytime functioning. Treatment of sleep complaints in adult PTSD patients has been shown to be effective at reducing symptoms of insomnia and nightmares as well as improving daytime PTSD symptoms.93 However, most of the current research discussing treatment of pediatric PTSD does not address sleep disturbances, and we are aware of no sleep treatment studies in pediatric PTSD.94,95 Indeed, due to a lack of objective sleep measures, we often lack knowledge as to which specific sleep disorders underlie the sleep disturbance observed in youth with PTSD, and as a consequence, appropriate targeted treatments are not always provided.
However, conducting full objective, overnight measures of sleep, such as polysomnography in children with PTSD, has significant challenges. These pediatric patients often have extreme difficulty with novel procedures and strange environments that are typically involved when conducting polysomnography. Techniques, such as systematic desensitization, in which individuals learn to cope and overcome their anxiety regarding a process in a sequence of steps in a hierarchy of increased exposure to the source of the anxiety, eventually leading to overcoming anxiety regarding the procedure or process, may represent a valuable approach to enhancing the ability of children with PTSD to overcome their fear regarding polysomnography assessment.
Conclusion and Future Directions
To date, studies have predominately used subjective questionnaires and interviews to measure sleep disturbance in children with PTSD. These investigations strongly suggest that there are higher rates of sleep disturbance and nightmares in pediatric PTSD populations than in normal pediatric populations. Consistent with subjective reports of sleep disturbance, studies using actigraphy document increased sleep onset latency, nocturnal activity, and sleep fragmentation in pediatric PTSD populations.
The current understanding of sleep disturbances in pediatric PTSD and their connection to development of PTSD over the lifespan is limited and warrants further investigation. Although studies to date have demonstrated sleep disturbance as a fundamental issue in trauma-exposed pediatric populations, the current research into pediatric PTSD and sleep disorders is limited in that (a) almost all measures of sleep in this population are from subjective questionnaires or interviews; (b) these subjective measures often do not provide specific information about the nature, duration, and frequency of sleep disturbances; (c) thus, these measures do not provide sufficient enough information to assess which sleep disturbances trauma-exposed populations are experiencing and if there are abnormal sleep architecture patterns as well; (d) in pediatric PTSD the effect of comorbidity with other psychiatric disorders that are associated with sleep disturbance, such as depression, needs exploration; (e) no studies with large sample sizes have examined the sleep of this population using actigraphy, and none have employed polysomnography, a method that can identify the specific sleep mechanisms disrupted and provide a better understanding of the associated sleep disorders; and (f) the longitudinal implications of sleep disturbance in childhood for PTSD onset across the lifespan have not been investigated.
Future investigations employing full polysomnography are critical for diagnosing the underlying sleep disorders in pediatric PTSD. Actigraphy does provide an objective assessment of activity during the night, providing reasonable estimates of total time in bed and sleep efficiency. However, it does not provide qualitative information on the type of activity nor does it provide many of the bioparameters that are routinely derived from polysomnography and are required for the diagnosis of many sleep disorders. Only full polysomnography provides measures of sleep stage and architecture, using recordings of EEG, EOG, submental EMG, and typically includes expiratory/inspiratory nasal airway pressure, nasal/oral airflow, finger pulse oximetry, ECG, movements of the rib cage and abdomen, snoring, and body position. These measures are integral to the diagnosis of most sleep disorders, including sleep apnea, REM disturbance, and PLMs. Further, as identified by polysomnography, abnormal sleep architecture patterns in pediatric PTSD populations may serve as a critical biomarker for onset of PTSD and other sleep disorders after a trauma.
As a result, a multi-method, longitudinal study examining phenomenology and utilizing polysomnography on children with PTSD would greatly contribute to our current understanding of sleep disorders in pediatric PTSD. Once the specific sleep disorders in pediatric PTSD have been objectively determined, treatment development and outcome studies would be crucial for not only reducing negative symptoms in patients but also for identifying sleep disturbance as a biomarker for development of PTSD. In adults, studies have already demonstrated that sleep disruption does predict severity and onset of PTSD.6–8,11,12 Treating sleep dysregulation early in life, as well as after a trauma at any age, could have significant implications for reducing risk of PTSD onset both in childhood and across the lifespan.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no finanical conflicts of interest.
REFERENCES
- 1.Krakow B, Melendrez D, Warner TD, Dorin R, Harper R, Hollifield M. To breathe, perchance to sleep: sleep-disordered breathing and chronic insomnia among trauma survivors. Sleep Breath. 2002;06:189–202. doi: 10.1007/s11325-002-0189-7. [DOI] [PubMed] [Google Scholar]
- 2.Maher MJ, Rego SA, Asnis GM. Sleep disturbances in patients with post-traumatic stress disorder: epidemiology, impact and approaches to management. CNS Drugs. 2006;20:567–90. doi: 10.2165/00023210-200620070-00003. [DOI] [PubMed] [Google Scholar]
- 3.Neylan T, Marmar C, Metzler T, et al. Sleep disturbances in the Vietnam generation: Findings from a nationally representative sample of male Vietnam veterans. Am J Psychiatry. 1998;155:929–33. doi: 10.1176/ajp.155.7.929. [DOI] [PubMed] [Google Scholar]
- 4.Ohayon MM, Shapiro CM. Sleep disturbances and psychiatric disorders associated with posttraumatic stress disorder in the general population. Compr Psychiatry. 2000;41:469–78. doi: 10.1053/comp.2000.16568. [DOI] [PubMed] [Google Scholar]
- 5.Kobayashi I, Boarts JM, Delahanty DL. Polysomnographically measured sleep abnormalities in PTSD: a meta-analytic review. Psychophysiology. 2007;44:660–9. doi: 10.1111/j.1469-8986.2007.537.x. [DOI] [PubMed] [Google Scholar]
- 6.Mellman TA, Bustamante V, Fins AI, Pigeon WR, Nolan B. REM sleep and the early development of posttraumatic stress disorder. Am J Psychiatry. 2002;159:1696–701. doi: 10.1176/appi.ajp.159.10.1696. [DOI] [PubMed] [Google Scholar]
- 7.Mellman TA, Pigeon WR, Nowell PD, Nolan B. Relationships between REM sleep findings and PTSD symptoms during the early aftermath of trauma. J Trauma Stress. 2007;20:893–901. doi: 10.1002/jts.20246. [DOI] [PubMed] [Google Scholar]
- 8.Koren D, Arnon I, Lavie P, Klein E. Sleep complaints as early predictors of post-traumatic stress disorder: a 1-year prospective study of injured survivors of motor vehicle accidents. Am J Psychiatry. 2002;159:855–7. doi: 10.1176/appi.ajp.159.5.855. [DOI] [PubMed] [Google Scholar]
- 9.Lamarche LJ, De Koninck J. Sleep disturbance in adults with posttraumatic stress disorder: a review. J Clin Psychiatry. 2007;68:1257–70. doi: 10.4088/jcp.v68n0813. [DOI] [PubMed] [Google Scholar]
- 10.Spoormaker VI, Montgomery P. Disturbed sleep in post-traumatic stress disorder: secondary symptom or core feature? Sleep Med Rev. 2008;12:169–84. doi: 10.1016/j.smrv.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 11.Krakow B, Haynes PL, Warner TD, et al. Nightmares, insomnia, and sleep-disordered breathing in fire evacuees seeking treatment for posttraumatic sleep disturbance. J Trauma Stress. 2004;17:257–68. doi: 10.1023/B:JOTS.0000029269.29098.67. [DOI] [PubMed] [Google Scholar]
- 12.Krakow B, Germain A, Warner TD, et al. The relationship of sleep quality and posttraumatic stress to potential sleep disorders in sexual assault survivors with nightmares, insomnia, and PTSD. J Trauma Stress. 2001;14:647–65. doi: 10.1023/A:1013029819358. [DOI] [PubMed] [Google Scholar]
- 13.Nappi CM, Drummond SPA, Hall JMH. Treating nightmares and insomnia in posttraumatic stress disorder: A review of current evidence. Neuropharmacology. 2012;62:576–85. doi: 10.1016/j.neuropharm.2011.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Galovski TE, Monson C, Bruce SE, Resick PA. Does cognitive-behavioral therapy for PTSD improve perceived health and sleep impairment? J Trauma Stress. 2009;22:197–204. doi: 10.1002/jts.20418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zayfert C, DeViva JC. Residual insomnia following cognitive behavioral therapy for PTSD. J Trauma Stress. 2004;17:69–73. doi: 10.1023/B:JOTS.0000014679.31799.e7. [DOI] [PubMed] [Google Scholar]
- 16.Krakow B, Hollifield M, Schrader R, et al. A controlled study of imagery rehearsal for chronic nightmares in sexual assault survivors with PTSD: a preliminary report. J Trauma Stress. 2000;13:589–609. doi: 10.1023/A:1007854015481. [DOI] [PubMed] [Google Scholar]
- 17.Krakow B, Lowry C, Germain A, et al. A retrospective study on improvements in nightmares and post-traumatic stress disorder following treatment for co-morbid sleep-disordered breathing. J Psychosom Res. 2000;49:291–8. doi: 10.1016/s0022-3999(00)00147-1. [DOI] [PubMed] [Google Scholar]
- 18.Krakow B, Johnston L, Melendrez D, et al. An open-label trial of evidence-based cognitive behavior therapy for nightmares and insomnia in crime victims with PTSD. Am J Psychiatry. 2001;158:2043–7. doi: 10.1176/appi.ajp.158.12.2043. [DOI] [PubMed] [Google Scholar]
- 19.Krakow BJ, Melendrez DC, Johnston LG, et al. Sleep dynamic therapy for Cerro Grande Fire evacuees with posttraumatic stress symptoms: a preliminary report. J Clin Psychiatry. 2002;63:673–84. doi: 10.4088/jcp.v63n0804. [DOI] [PubMed] [Google Scholar]
- 20.Raskind MA, Peskind ER, Kanter ED, et al. Reduction of nightmares and other PTSD symptoms in combat veterans by prazosin: a placebo-controlled study. Am J Psychiatry. 2003;160:371–3. doi: 10.1176/appi.ajp.160.2.371. [DOI] [PubMed] [Google Scholar]
- 21.Germain A, Richardson R, Moul DE, et al. Placebo-controlled comparison of prazosin and cognitive-behavioral treatments for sleep disturbances in US Military Veterans. J Psychosom Res. 2012;72:89–96. doi: 10.1016/j.jpsychores.2011.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ulmer CS, Edinger JD, Calhoun PS. A multi-component cognitive-behavioral intervention for sleep disturbance in veterans with PTSD: a pilot study. J Clin Sleep Med. 2011;7:57–68. [PMC free article] [PubMed] [Google Scholar]
- 23.Youakim JM, Doghramji K, Schutte SL. Posttraumatic stress disorder and obstructive sleep apnea syndrome. Psychosomatics. 1998;39:168–71. doi: 10.1016/S0033-3182(98)71365-9. [DOI] [PubMed] [Google Scholar]
- 24.Babson KA, Feldner MT. Temporal relations between sleep problems and both traumatic event exposure and PTSD: a critical review of the empirical literature. J Anxiety Disord. 2010;24:1–15. doi: 10.1016/j.janxdis.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, Best CL. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: results from the National Survey of Adolescents. J Consult Clin Psychol. 2003;71:692–700. doi: 10.1037/0022-006x.71.4.692. [DOI] [PubMed] [Google Scholar]
- 26.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 27.Pynoos RS, Frederick C, Nader K, et al. Life threat and posttraumatic stress in school-age children. Arch Gen Psychiatry. 1987;44:1057–63. doi: 10.1001/archpsyc.1987.01800240031005. [DOI] [PubMed] [Google Scholar]
- 28.Charuvastra A, Cloitre M. Safe enough to sleep: sleep disruptions associated with trauma, posttraumatic stress, and anxiety in children and adolescents. Child Adolesc Psychiatr Clin N Am. 2009;18:877–91. doi: 10.1016/j.chc.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 29.Noll JG, Trickett PK, Susman EJ, Putnam FW. Sleep disturbances and childhood sexual abuse. J Pediatr Psychol. 2005;31:469–80. doi: 10.1093/jpepsy/jsj040. [DOI] [PubMed] [Google Scholar]
- 30.Thabet AA, Vostanis P. Post-traumatic stress reactions in children of war. J Child Psychol Psychiatry. 1999;40:385–91. [PubMed] [Google Scholar]
- 31.Thabet AA, Abed Y, Vostanis P. Comorbidity of PTSD and depression among refugee children during war conflict. J Child Psychol Psychiatry. 2004;45:533–42. doi: 10.1111/j.1469-7610.2004.00243.x. [DOI] [PubMed] [Google Scholar]
- 32.Montgomery E, Foldspang A. Traumatic experience and sleep disturbance in refugee children from the Middle East. Eur J Public Health. 2001;11:18–22. doi: 10.1093/eurpub/11.1.18. [DOI] [PubMed] [Google Scholar]
- 33.Nader K, Pynoos R, Fairbanks L, Frederick C. Children's PTSD reactions one year after a sniper attack at their school. Am J Psychiatry. 1990;147:1526–30. doi: 10.1176/ajp.147.11.1526. [DOI] [PubMed] [Google Scholar]
- 34.Llabre MM, Hadi F. War-related exposure and psychological distress as predictors of health and sleep: a longitudinal study of Kuwaiti children. Psychosom Med. 2009;71:776–83. doi: 10.1097/PSY.0b013e3181ae6aee. [DOI] [PubMed] [Google Scholar]
- 35.Schuster MA, Stein BD, Jaycox LH, et al. A national survey of stress reactions after the September 11, 2001, terrorist attacks. New Engl J Med. 2001;345:1507–12. doi: 10.1056/NEJM200111153452024. [DOI] [PubMed] [Google Scholar]
- 36.Galea S, Resnick H, Ahern J, et al. Posttraumatic stress disorder in Manhattan, New York City, after the September 11th terrorist attacks. J Urban Health. 2002;79:340–53. doi: 10.1093/jurban/79.3.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chemtob CM, Nomura Y, Abramovitz RA. Impact of conjoined exposure to the world trade center attacks and to other traumatic events on the behavioral problems of preschool children. Arch Pediatr Adolesc Med. 2008;162:126–33. doi: 10.1001/archpediatrics.2007.36. [DOI] [PubMed] [Google Scholar]
- 38.Lee I, Ha YS, Kim YA, Kwon YH. PTSD symptoms in elementary school children after Typhoon Rusa. Taehan Kanho Hakhoe Chi. 2004;34:636–45. doi: 10.4040/jkan.2004.34.4.636. [DOI] [PubMed] [Google Scholar]
- 39.Dollinger SJ. The measurement of children's sleep disturbances and somatic complaints following a disaster. Child Psychiatry Hum Dev. 1986;16:148–53. doi: 10.1007/BF00706172. [DOI] [PubMed] [Google Scholar]
- 40.Brown TH, Mellman TA, Alfano CA, Weems CF. Sleep fears, sleep disturbance, and PTSD symptoms in minority youth exposed to Hurricane Katrina. J Trauma Stress. 2011;24:575–80. doi: 10.1002/jts.20680. [DOI] [PubMed] [Google Scholar]
- 41.Carrion VG, Weems CF, Ray R, Reiss AL. Toward an empirical definition of pediatric PTSD: the phenomenology of PTSD symptoms in youth. J Am Acad Child Adolesc Psychiatry. 2002;41:166–73. doi: 10.1097/00004583-200202000-00010. [DOI] [PubMed] [Google Scholar]
- 42.Chimienti G, Nasr JA, Khalifeh I. Children's reactions to war-related stress. Affective symptoms and behaviour problems. Soc Psychiatry Psychiatr Epidemiol. 1989;24:282–7. doi: 10.1007/BF01788030. [DOI] [PubMed] [Google Scholar]
- 43.Wittmann L, Zehnder D, Schredl M, Jenni OG, Landolt MA. Posttraumatic nightmares and psychopathology in children after road traffic accidents. J Trauma Stress. 2010;23:232–9. doi: 10.1002/jts.20514. [DOI] [PubMed] [Google Scholar]
- 44.Thabet AA, Ibraheem AN, Shivram R, Winter EA, Vostanis P. Parenting support and PTSD in children of a war zone. Int J Soc Psychiatry. 2009;55:226–37. doi: 10.1177/0020764008096100. [DOI] [PubMed] [Google Scholar]
- 45.Arnberg FK, Rydelius P-A, Lundin T. A longitudinal follow-up of posttraumatic stress: from 9 months to 20 years after a major road traffic accident. Child Adolesc Psychiatry Ment Health. 2011;5:8. doi: 10.1186/1753-2000-5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Strawn JR, Keeshin BR. Successful treatment of posttraumatic stress disorder with prazosin in a young child. Ann Pharmacother. 2011;45:1590–1. doi: 10.1345/aph.1Q548. [DOI] [PubMed] [Google Scholar]
- 47.Fraleigh LA, Hendratta VD, Ford JD, Connor DF. Prazosin for the treatment of posttraumatic stress disorder-related nightmares in an adolescent male. J Child Adolesc Psychopharmacol. 2009;19:475–6. doi: 10.1089/cap.2009.0002. [DOI] [PubMed] [Google Scholar]
- 48.Brkanac Z, Pastor JF, Storck M. Prazosin in PTSD. J Am Acad Child Adolesc Psychiatry. 2003;42:384–5. doi: 10.1097/01.CHI.0000052509.98293.97. [DOI] [PubMed] [Google Scholar]
- 49.De Bellis MD, Keshavan MS, Harenski KA. Anterior cingulate n-acetylaspartate/ creatine ratios during clonidine treatment in a maltreated child with posttraumatic stress disorder. J Child Adolesc Psychopharmacol. 2001;11:311–6. doi: 10.1089/10445460152595649. [DOI] [PubMed] [Google Scholar]
- 50.Horrigan JP. Guanfacine for PTSD nightmares. J Am Acad Child Adolesc Psychiatry. 1996;35:975–6. doi: 10.1097/00004583-199608000-00006. [DOI] [PubMed] [Google Scholar]
- 51.Krakow B, Sandoval D, Schrader R, et al. Treatment of chronic nightmares in adjudicated adolescent girls in a residential facility. J Adolesc Health. 2001;29:94–100. doi: 10.1016/s1054-139x(00)00195-6. [DOI] [PubMed] [Google Scholar]
- 52.Thabet AA, Vostanis P. Post traumatic stress disorder reactions in children of war: a longitudinal study. Child Abuse Neglect. 2000;24:291–8. doi: 10.1016/s0145-2134(99)00127-1. [DOI] [PubMed] [Google Scholar]
- 53.Spruyt K, Gozal D. Pediatric sleep questionnaires as diagnostic or epidemiological tools: a review of currently available instruments. Sleep Med Rev. 2011;15:19–32. doi: 10.1016/j.smrv.2010.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Achenbach TM. Integrative Guide for the 1991 CBCL/4-18, YSR, and TRF profiles. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- 55.Achenbach TM, Edelbrock C. Manual for the Child Behavior Checklist and Revised Child Behavior Profile. Burlington, VT: University of Vermont Press; 1983. [Google Scholar]
- 56.Chervin, Hedger, Dillon, Pituch Pediatric sleep questionnaire (PSQ): validity and reliability of scales for sleep-disordered breathing, snoring, sleepiness, and behavioral problems. Sleep Med. 2000;1:21–32. doi: 10.1016/s1389-9457(99)00009-x. [DOI] [PubMed] [Google Scholar]
- 57.Bruni O, Ottaviano S, Guidetti V, et al. The sleep disturbance scale for children (SDSC) construction and validation of an instrument to evaluate sleep disturbances in childhood and adolescence. J Sleep Res. 1996;5:251–61. doi: 10.1111/j.1365-2869.1996.00251.x. [DOI] [PubMed] [Google Scholar]
- 58.Luginbuehl M, Batsche G, Bradley-Klug K, et al. The initial development and validation study of the sleep disorders inventory for students (SDIS) Sleep. 2003;26:A399–400. [Google Scholar]
- 59.Owens JA, Spirito A, McGuinn M. The Children's Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep. 2000;23:1043–51. [PubMed] [Google Scholar]
- 60.Krakow B, Schrader R, Tandberg D, et al. Nightmare frequency in sexual assault survivors with PTSD. J Anxiety Disord. 2002;16:175–90. doi: 10.1016/s0887-6185(02)00093-2. [DOI] [PubMed] [Google Scholar]
- 61.Belicki K. Nightmare frequency versus nightmare distress: relations to psycho-pathology and cognitive style. J Abnorm Psychol. 1992;101:592–7. doi: 10.1037//0021-843x.101.3.592. [DOI] [PubMed] [Google Scholar]
- 62.Gregory AM, Cousins JC, Forbes EE, et al. Sleep items in the child behavior checklist: a comparison with sleep diaries, actigraphy, and polysomnography. J Am Acad Child Adolesc Psychiatry. 2011;50:499–507. doi: 10.1016/j.jaac.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.De la Vega R, Miró J. The assessment of sleep in pediatric chronic pain sufferers. Sleep Med Rev. 2012 Jun 29; doi: 10.1016/j.smrv.2012.04.002. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 64.Luginbuehl M, Bradley-Klug KL, Ferron J, Anderson WM, Benbadis SR. Pediatric sleep disorders: Validation of the Sleep Disorders Inventory for Students. Sch Psychol Rev. 2008;37:409–31. [Google Scholar]
- 65.Goodlin-Jones BL, Sitnick SL, Tang K, Liu J, Anders TF. The Children's Sleep Habits Questionnaire in toddlers and preschool children. J Dev Behav Pediatr. 2008;29:82–8. doi: 10.1097/dbp.0b013e318163c39a. [DOI] [PubMed] [Google Scholar]
- 66.St-Onge M, Mercier P, De Koninck J. Imagery rehearsal therapy for frequent nightmares in children. Behav Sleep Med. 2009;7:81–98. doi: 10.1080/15402000902762360. [DOI] [PubMed] [Google Scholar]
- 67.Mindell JA, Barrett KM. Nightmares and anxiety in elementary-aged children: is there a relationship. Child Care Health Dev. 2002;28:317–22. doi: 10.1046/j.1365-2214.2002.00274.x. [DOI] [PubMed] [Google Scholar]
- 68.Souders MC, Mason TBA, Valladares O, et al. Sleep behaviors and sleep quality in children with autism spectrum disorders. Sleep. 2009;32:1566. doi: 10.1093/sleep/32.12.1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Short MA, Gradisar M, Lack LC, Wright H, Carskadon MA. The discrepancy between actigraphic and sleep diary measures of sleep in adolescents. Sleep Med. 2012;13:378–84. doi: 10.1016/j.sleep.2011.11.005. [DOI] [PubMed] [Google Scholar]
- 70.O'Hara R, Schroder C. What sleep problems are common in children with ASC, and how can they be treated? In: Bolte S, Hallmayer J, editors. Autism spectrum conditions: FAQs on autism, Asperger syndrome, and atypical autism answered by international experts. Cambridge, MA: Hogrefe Publishing; 2010. pp. 180–3. [Google Scholar]
- 71.Arbuckle R, Abetz L, Durmer JS, et al. Development of the Pediatric Restless Legs Syndrome Severity Scale (P-RLS-SS): a patient-reported outcome measure of pediatric RLS symptoms and impact. Sleep Med. 2010;11:897–906. doi: 10.1016/j.sleep.2010.03.016. [DOI] [PubMed] [Google Scholar]
- 72.Sadeh A, McGuire JPD, Sachs H, et al. Sleep and psychological characteristics of children on a psychiatric inpatient unit. J Am Acad Child Adolesc Psychiatry. 1995;34:813–9. doi: 10.1097/00004583-199506000-00023. [DOI] [PubMed] [Google Scholar]
- 73.Glod CA, Teicher MH, Hartman CR, Harakal T. Increased nocturnal activity and impaired sleep maintenance in abused children. J Am Acad Child Adolesc Psychiatry. 1997;36:1236–43. doi: 10.1097/00004583-199709000-00016. [DOI] [PubMed] [Google Scholar]
- 74.Yesavage JA, Kinoshita LM, Kimball T, et al. Sleep-disordered breathing in Vietnam veterans with posttraumatic stress disorder. Am J Geriatr Psychiatry. 2012;20:199–204. doi: 10.1097/JGP.0b013e3181e446ea. [DOI] [PubMed] [Google Scholar]
- 75.Brown TM, Boudewyns PA. Periodic limb movements of sleep in combat veterans with posttraumatic stress disorder. J Trauma Stress. 1996;9:129–36. doi: 10.1007/BF02116838. [DOI] [PubMed] [Google Scholar]
- 76.Quan SF, Goodwin JL, Babar SI, et al. Sleep architecture in normal Caucasian and Hispanic children aged 6-11 years recorded during unattended home polysomnography: experience from the Tucson Children's Assessment of Sleep Apnea Study (TuCASA) Sleep Med. 2003;4:13–9. doi: 10.1016/s1389-9457(02)00235-6. [DOI] [PubMed] [Google Scholar]
- 77.Montgomery-Downs HE, O'Brien LM, Gulliver TE, Gozal D. Polysomnographic characteristics in normal preschool and early school-aged children. Pediatrics. 2006;117:741–53. doi: 10.1542/peds.2005-1067. [DOI] [PubMed] [Google Scholar]
- 78.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27:1255–73. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- 79.Forbes EE, Bertocci MA, Gregory AM, et al. Objective sleep in pediatric anxiety disorders and major depressive disorder. J Am Acad Child Adolesc Psychiatry. 2008;47:148–55. doi: 10.1097/chi.0b013e31815cd9bc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Gregory AM, Sadeh A. Sleep, emotional and behavioral difficulties in children and adolescents. Sleep Med Rev. 2012;16:129–36. doi: 10.1016/j.smrv.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 81.Gregory AM, Caspi A, Moffitt TE, Poulton R. Sleep problems in childhood predict neuropsychological functioning in adolescence. Pediatrics. 2009;123:1171–6. doi: 10.1542/peds.2008-0825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gregory AM, Eley TC, O'Connor TG, Plomin R. Etiologies of associations between childhood sleep and behavioral problems in a large twin sample. J Am Acad Child Adolesc Psychiatry. 2004;43:744–51. doi: 10.1097/01.chi/0000122798.47863.a5. [DOI] [PubMed] [Google Scholar]
- 83.Gregory AM, O'Connor TG. Sleep problems in childhood: a longitudinal study of developmental change and association with behavioral problems. J Am Acad Child Adolesc Psychiatry. 2002;41:964–71. doi: 10.1097/00004583-200208000-00015. [DOI] [PubMed] [Google Scholar]
- 84.Gregory AM, Rijsdijk FV, Lau JYF, Dahl RE, Eley TC. The direction of longitudinal associations between sleep problems and depression symptoms: a study of twins aged 8 and 10 years. Sleep. 2009;32:189–99. doi: 10.1093/sleep/32.2.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Willis TA, Gregory AM. Childhood contributions to adult sleep problems. Sleep Med. 2010;11:818–9. doi: 10.1016/j.sleep.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 86.Van Liempt S. Sleep disturbances and PTSD: a perpetual circle? Eur J Psychotraumatol. 2012. p. 3. http://dx.doi.org/10.3402/ejpt.v3i0.19142. [DOI] [PMC free article] [PubMed]
- 87.Bruni O, Novelli L, Curatolo P, et al. Sleep spindles and learning: new insights from dyslexia. Sleep. 2009;32:A106. [Google Scholar]
- 88.Germain A. Sleep disturbances as the hallmark of PTSD: where are we now? Am J Psychiatry. 2013;170:372–82. doi: 10.1176/appi.ajp.2012.12040432. http://dx.doi.org/10.1176/appi.ajp.2012.12040432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Rao V, Bergey A, Hill H, Efron D, McCann U. Sleep disturbance after mild traumatic brain injury: indicator of injury? J Neuropsychiatry Clin Neurosci. 2011;23:201–5. doi: 10.1176/jnp.23.2.jnp201. [DOI] [PubMed] [Google Scholar]
- 90.Wamsley EJ, Tucker MA, Shinn AK, et al. Reduced sleep spindles and spindle coherence in schizophrenia: mechanisms of impaired memory consolidation? Biol Psychiatry. 2012;71:154–61. doi: 10.1016/j.biopsych.2011.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Buckley A, Jennison K, Buckley J, et al. Polysomnographic abnormalities and parent report in young children with autism. Sleep. 2009;32:A352. [Google Scholar]
- 92.Buckley AW, Sassower K, Rodriguez AJ, et al. An open label trial of donepezil for enhancement of rapid eye movement sleep in young children with autism spectrum disorders. J Child Adolesc Psychopharmacol. 2011;21:353–7. doi: 10.1089/cap.2010.0121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Schoenfeld F, DeViva J, Manber R. Treatment of sleep disturbances in posttraumatic stress disorder: a review. J Rehabil Res Dev. 2012;49:729–52. doi: 10.1682/jrrd.2011.09.0164. [DOI] [PubMed] [Google Scholar]
- 94.Donnelly CL. Pharmacologic treatment approaches for children and adolescents with posttraumatic stress disorder. Child Adolesc Psychiatr Clin N Am. 2003;12:251–69. doi: 10.1016/s1056-4993(02)00102-5. [DOI] [PubMed] [Google Scholar]
- 95.Kowalik J, Weller J, Venter J, Drachman D. Cognitive behavioral therapy for the treatment of pediatric posttraumatic stress disorder: a review and meta-analysis. J Behav Ther Exp Psychiatry. 2011;42:405–13. doi: 10.1016/j.jbtep.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 96.Simonds JF, Parraga H. Sleep behaviors and disorders in children and adolescents evaluated at psychiatric clinics. J Dev Behav Pediatr. 1984;5:6–10. [PubMed] [Google Scholar]
- 97.Yang L, Zuo C, Eaton LF. Research note: sleep problems of normal Chinese adolescents. J Child Psychol Psychiatry. 1987;28:167–72. doi: 10.1111/j.1469-7610.1987.tb00660.x. [DOI] [PubMed] [Google Scholar]
- 98.Kahn A, Van de Merckt C, Rebuffat E, et al. Sleep problems in healthy preadolescents. Pediatrics. 1989;84:542–6. [PubMed] [Google Scholar]
- 99.Vignau J, Bailly D, Duhamel A, Vervaecke P, Beuscart R, Collinet C. Epidemio-logic study of sleep quality and troubles in French secondary school adolescents. J Adolesc Health. 1997;21:343–50. doi: 10.1016/S1054-139X(97)00109-2. [DOI] [PubMed] [Google Scholar]
- 100.Blader JC, Koplewicz HS, Abikoff H, Foley C. Sleep problems of elementary school children: a community survey. Arch Pediatr Adolesc Med. 1997;151:473–80. doi: 10.1001/archpedi.1997.02170420043007. [DOI] [PubMed] [Google Scholar]
- 101.Lee KA, Mcenany G, Weekes D. Gender differences in sleep patterns for early adolescents. J Adolesc Health. 1999;24:16–20. doi: 10.1016/s1054-139x(98)00074-3. [DOI] [PubMed] [Google Scholar]
- 102.Liu X, Sun Z, Uchiyama M, Shibui K, Kim K, Okawa M. Prevalence and correlates of sleep problems in Chinese schoolchildren. Sleep. 2000;23:1053–62. [PubMed] [Google Scholar]
- 103.Tomás Vila M, Miralles Torres A, Beseler Soto B, Revert Gomar M, Sala Langa MJ, Uribelarrea Sierra AI. [Sleep patterns and sleep disturbances among school-children in the town of Gandia] An Pediatr (Barc) 2008;68:250–6. doi: 10.1157/13116705. [DOI] [PubMed] [Google Scholar]
- 104.Hvolby A, Jørgensen J, Bilenberg N. [Sleep and sleep difficulties in Danish children aged 6-11 years] Ugeskr Laeg. 2008;170:448–51. [PubMed] [Google Scholar]


