Abstract
Pseudoaneurysm of the abdominal wall is a possible but very rare clinical entity. It is a known complication of surgery, trauma, or arterial puncture, but it is rarely spontaneous. Even though it can usually present with a wide range of local symptoms, it can cause referred pain via spinal cord, which is cross-excited with afferent sympathetic nervous system. We report a case of right arm pain which was referred from a small abdominal pseudoaneurysm like a referred pain from gall bladder. This rare entity should be considered in the differential for pain management in case that the pain does not resolve with medication or interventional pain management.
Keywords: abdominal pseudoaneurysm, referred pain, ultrasonography
The expression "referred pain" indicates that pain is perceived in an area other than that in which the noxious stimulation takes place [1]. Pain can be referred to muscles from both visceral and somatic structures [2]. Referred pain from viscera is explained on the basis of the convergence of visceral and somatic afferent fibers on the same central neurons. These phenomena, such as left shoulder pain from heart or right shoulder pain from gallbladder, are well known in the clinical setting.
Cardiac pain often results from ischemic episodes that excite the receptors of the sympathetic and vagal afferent pathways. Sympathetic afferent fibers from the heart enter the upper thoracic spinal cord and synapse on spinothalamic tract cells of the ascending pathways. Excitation of spinothalamic tract cells in the upper thoracic and in lower cervical segments can contribute to the anginal pain experienced in the chest and the referred pain in the ipsilateral arm [3].
Abdominal pseudoaneurysm is not only a rare complication of the abdominal wall surgery, but also it is not easy to recognize it at the surgical scar. Since vascular smooth muscle is innervated primarily by the sympathetic nervous system, it may cause a referred pain at topographically distinct body region through the cross-excitation of the spinal cord. However, it usually undergoes spontaneous resolution by thrombosis without any treatment because of small size [4]. Therefore, referred pain from pseudoaneurysm at the abdominal wall is an extremely rare condition.
Here, we introduce our case with a pseudoaneurysm of the abdominal wall that is accompanied by complaints of constant and pulsatile pain at the right upper abdomen, which referred to the ipsilateral upper arm.
CASE REPORT
A 48-year-old male patient (height 165 cm, weight 76 kg) visited our clinic with abdominal pain on the right upper abdomen. The patient had exploratory laparotomy for abdominal abscess 25 years ago, but there was no acute complication from the operation. However, the patient has felt localized pain and allodynia around the surgical scar since 4 years ago. The pain nature was continuous, throbbing, and pulsatile, and the pain was aggravated by overwork or alcohol consumption; relieved by compression of the scar. On rest, the pain was 4 out of 10 and when aggravated, went as high as 8 out of 10 on 11-points numeric rating scale. Whenever aggravated, the pain had radiated to his right upper arm once every 2-3 seconds. The nature and intensity of radiating pain was similar with the original pain. The pain has accompanied by heated sensation of the abdomen and right upper arm.
The patient had been taking aspirin and hypoglycemic medications for diabetes mellitus. However, his pain was regarded as different with diabetic truncal neuropathy that causes burning pain or dysthesias with multi-dermatomal distributions. Before visiting our clinic, he had taken CT scanning of abdomen twice and MRI of cervical spine and received conservative treatments, including oral analgesics (i.e. acetaminophen, tramadol, opioids), ketamine infusion therapy, intercostal nerve blocks, pulsed radiofrequency therapy of thoracic dorsal root ganglia in several other hospitals for 18 months. Abdominal CTs and cervical MRI did not show any abnormal conditions and his pain was not only alleviated temporarily, but he also suffered from drug adverse effects, including hepatitis and light-headedness.
Physical examination revealed 3 cm long surgical scar on the right upper abdomen and focal tenderness, allodynia and hyperesthesia around the scar. Contrastively, there were no abnormal findings in the right upper arm. Subsequently, gray-scale ultrasonography coupled with color Doppler flow imaging was performed to find any soft tissue lesion, such as inflammation and neuroma.
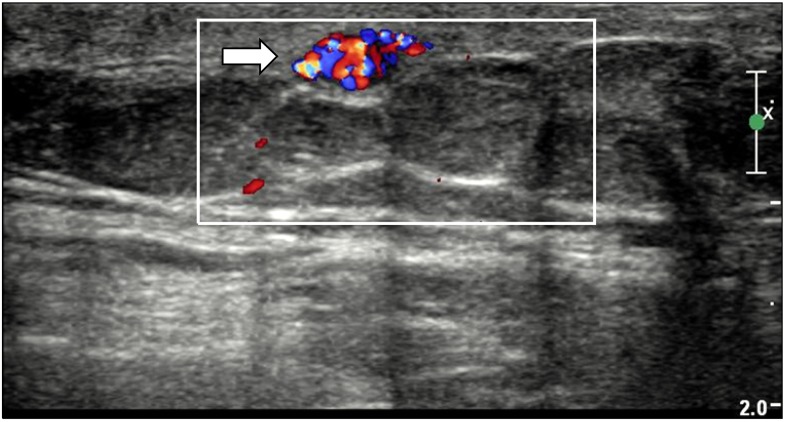
Color Doppler US showed a vascular mass with turbulent blood flow, which was a 0.62×0.27×0.69 cm sized mass in the subcutaneous layer of the mid-surgical scar (Fig. 1). The lesion was suspected to be a symptomatic pseudoaneurysm originating from an artery or possibly an arteriovenous fistula, while there was no demonstrable entering or exiting vessel. So, the patient was transferred to a vascular surgeon for treatment of it.
Fig. 1.
Color doppler ultrasound demonstrates active blood flow in the pseudoaneurysm (arrow).
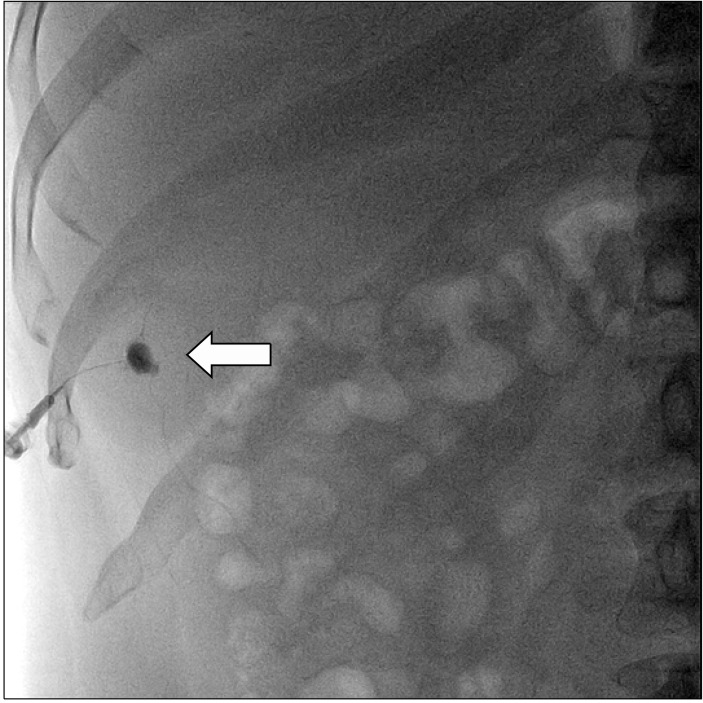
Sclerotherapy was decided for pseudoaneurysm under US guidance. Skin was punctured by medicut under US guidance and the mass was enhanced using contrast media under fluoroscopy (Fig. 2). A mixed material (glue:lipidol = 1:2) was used for embolization of pseudoaneurysm. The day after the procedure, US showed that a mixture of glue and lipidol had filled the pseudoaneurysm with posterior acoustic shadow. Patient was discharged with substantially diminished tenderness. Two weeks later, his symptoms, including referred pain to the right upper arm, were completely subsided without any medications.
Fig. 2.
An oval mass which is filled with contrast media is shown at the right upper abdomen on the anteroposterior view of fluoroscopy (arrow).
DISCUSSION
The present case showed that pseudoaneurysms at the abdominal wall can produce referred pain to the ipsilateral upper arm, as well as abdominal tenderness. Pseudoaneurysms results from injury to the blood vessel wall [5], accompanying with surgery, trauma, or arterial puncture [6]. Clinically, pseudoaneurysms can be associated with pain or tenderness, as well as aneurysmal bruit on ausculatation or a palpable pulsatile mass on palpation [7]. Even though a simple radiographic examination may not reveal the soft tissue mass before rim calcification, US can be used for diagnosis with a sensitivity of 94% and a specificity of 97% [8]. Typical color Doppler US findings of a pseudoaneurysm include a swirling color flow in a mass and a typical "to-and-fro" Doppler waveform in the neck of pseudoaneurysm [9].
Pseudoaneurysms of inferior epigastric artery are well recognized complications of the abdominal wall surgery or trauma [10]. In this case, however, we inferred that it derived from others rather than inferior epigastric artery, according to the anatomical location although we could not confirm the feeding and the exiting vessels because superior abdominal wall is supplied by superior epigastric artery, musculophrenic artery and thoracic intercostal artery. Vascular smooth muscle is innervated primarily by the sympathetic nervous system. It is considered that pseudoaneurysmal pain is transmitted through sympathetic nerve to the spinal cord.
Sympathetic afferent fibers from the arteries of superior abdominal wall may enter the spinal cord via sympathetic trunk in the thoracic regions [11]. Then, they may synapse on spinothalamic tract of the ascending pathway in the lower cervical segments. This convergence of visceral and somatic input onto a common pool of spinothalamic cells may provide a substrate for explaining the mechanism of referred pain to arm derived from arterial pseudoaneurysm of the abdominal wall [3]. Actually, the patient's symptoms were worsening by increasing of the sympathetic tone like overstrain or alcohol drinking, and this could give an amplification of sympathetic mediated pain in nature.
Diabetic polyneuropathy might be considered in any diabetic patient presenting with atypical abdominal pain. Involvement of the nervous system that originate from the thoracic spinal cord causes deep burning pain associated with cutaneous hyperaesthesia [12], and may be associated with a dermatomal pattern of sensory loss [13]. If palpation reveals no localized tenderness or pulsatile mass, and cutaneous sensory examination reveals hypesthesia or hyperesthesia in multiple adjacent dermatomes, diabetic polyneuropathy should be considered rather than pseudoaneurysm of the abdominal wall. Small sized (< 1.8 cm in diameter) pseudoaneurysm usually resolves spontaneously by thrombosis formation [4]. But, it might be sustained due to taking aspirin for medication of diabetes mellitus in this case.
In conclusion, the pseudoaneurysm of abdominal wall can cause referred pain to the arm by convergence of visceral and somatic input onto a common pool of spinothalamic cells of lower cervical segments. Therefore, we consider using ultrasonography during physical examination in case of abdominal wall tenderness after previous abdominal surgery.
References
- 1.Vecchiet L, Vecchiet J, Giamberardino MA. Referred muscle pain: clinical and pathophysiologic aspects. Curr Rev Pain. 1999;3:489–498. doi: 10.1007/s11916-999-0077-y. [DOI] [PubMed] [Google Scholar]
- 2.Procacci P, Maresca M. Referred pain from somatic and visceral structures. Curr Rev Pain. 1999;3:96–99. [Google Scholar]
- 3.Foreman RD. Mechanisms of cardiac pain. Annu Rev Physiol. 1999;61:143–167. doi: 10.1146/annurev.physiol.61.1.143. [DOI] [PubMed] [Google Scholar]
- 4.Kent KC, McArdle CR, Kennedy B, Baim DS, Anninos E, Skillman JJ. A prospective study of the clinical outcome of femoral pseudoaneurysms and arteriovenous fistulas induced by arterial puncture. J Vasc Surg. 1993;17:125–131. doi: 10.1067/mva.1993.41707. [DOI] [PubMed] [Google Scholar]
- 5.Sadat U, Jah A, Ward N, Gaunt M. Superior epigastric artery pseudoaneurysm--a rare complication of chest drain insertion in coronary artery bypass grafting. J Cardiothorac Surg. 2007;2:21. doi: 10.1186/1749-8090-2-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ferrer JV, Soriano P, Zazpe C, Vicente F, Herrera J, Lera JM. Pseudoaneurysm of the inferior epigastric artery. Pathogenesis, diagnosis, and treatment. Arch Surg. 1996;131:102–103. doi: 10.1001/archsurg.1996.01430130104024. [DOI] [PubMed] [Google Scholar]
- 7.Lenartova M, Tak T. Iatrogenic pseudoaneurysm of femoral artery: case report and literature review. Clin Med Res. 2003;1:243–247. doi: 10.3121/cmr.1.3.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coughlin BF, Paushter DM. Peripheral pseudoaneurysms: evaluation with duplex US. Radiology. 1988;168:339–342. doi: 10.1148/radiology.168.2.3293107. [DOI] [PubMed] [Google Scholar]
- 9.Schwartz RA, Kerns DB, Mitchell DG. Color Doppler ultrasound imaging in iatrogenic arterial injuries. Am J Surg. 1991;162:4–8. doi: 10.1016/0002-9610(91)90192-g. [DOI] [PubMed] [Google Scholar]
- 10.Georgiadis GS, Souftas VD, Papas TT, Lazarides MK, Prassopoulos P. Inferior epigastric artery false aneurysms: review of the literature and case report. Eur J Vasc Endovasc Surg. 2007;33:182–186. doi: 10.1016/j.ejvs.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 11.Guyton AC, Hall JE. Guyton and Hall textbook of medical physiology. 12th ed. Philadelphia, PA: Saunders Elsevier; 2011. pp. 730–731. [Google Scholar]
- 12.Boulton AJ, Ward JD. Diabetic neuropathies and pain. Clin Endocrinol Metab. 1986;15:917–931. doi: 10.1016/s0300-595x(86)80080-9. [DOI] [PubMed] [Google Scholar]
- 13.Longstreth GF. Diabetic thoracic polyradiculopathy. Best Pract Res Clin Gastroenterol. 2005;19:275–281. doi: 10.1016/j.bpg.2004.09.003. [DOI] [PubMed] [Google Scholar]