Abstract
There have been reports of abnormalities in the lumbosacral region involving a lower-than-normal termination of the dural sac, which is caused by disease or anatomical variation. Inadvertent dural puncture or other unexpected complications can occur during caudal epidural block or adhesiolysis in patients with these variations, but only a small number of case reports have described this issue. We report a case of dural puncture by the introducer needle before attempting caudal epidural adhesiolysis, which occurred even though the needle was not advanced upward after penetrating the sacrococcygeal ligament. Dural puncture was caused by a morphological abnormality in the lumbosacral region, with no pathological condition; the dural sac terminal was located more distally than normal. However, dural puncture could have been prevented if we had checked for such an abnormality in the magnetic resonance imaging (MRI) taken before the procedure.
Keywords: anatomical variation, caudal block, dural puncture
There are reports that dural puncture can occur during caudal block owing to abnormalities in the sacral vertebrae caused by disease or anatomical variation [1-3]. Therefore, unexpected complications can occur during the placement of the introducer needle via the caudal approach to epidural adhesiolysis in these patients. Dural puncture occurs because the spinal cord terminates abnormally low, with the dural sac tip located in the lower sacrum; this can be accompanied by pathological conditions such as cystic structures [4].
The authors saw a 51-year-old male patient complaining of radiating pain in the lower extremities. To attempt caudal epidural adhesiolysis, the sacrococcygeal ligament was punctured with the introducer needle, but unexpected dural puncture occurred even though the needle was not pushed upward. The lumbar magnetic resonance imaging (MRI) studied afterwards showed that the dural sac tip was abnormally extended to the lower sacrum. We are reporting this case to advise others to consider the possibility of dural puncture and complications due to anatomical variation when using the caudal approach.
CASE REPORT
A 51-year-old male patient came to the hospital complaining of bilateral buttock pain that had begun 5 years earlier and bilateral radiating pain in the lower extremities. The patient history showed that he had been in manual labor for 10 years, and he had undergone a L4-5 discectomy in another hospital for the above symptoms 2 years previously. The pain had not been relieved, however, and he had been receiving drug and physical therapy, but the pain had recently worsened. The pain was exacerbated when the patient remained in one position or walked for a long time, whereas the pain was relieved when he kept still. The pain was characterized as a continual tingling pain, with a degree of 7/10 on the visual analogue scale (VAS).
The physical examination showed no mobility or sensory disorder, and the deep tendon reflex was also normal. There were no abnormalities other than a reduction to approximately 60 degrees on both sides in the straight leg raise test. Basic pre-operative testing results were normal, and only mild degenerative spondylosis was observed in the lumbar x-ray. The lumbar MRI revealed disc extrusion from the L4-5 center to the left intervertebral foramen and small disc protrusion in the L5-S1 right center, but the patient's symptoms were limited to the bilateral L5 dermatome. Recurred lumbar disc herniation and failed back surgery syndrome were suspected.
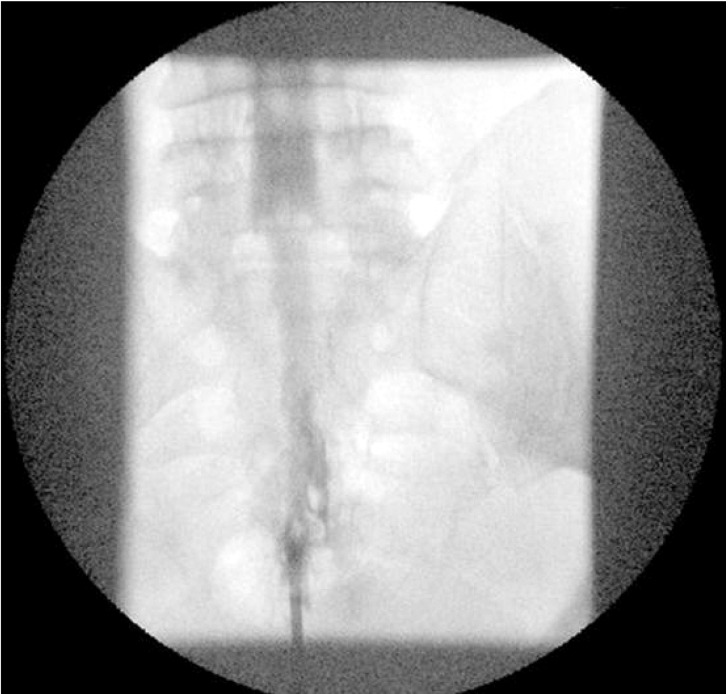
L5-selective transforaminal epidural block was performed twice in the clinic, but the improvement in symptoms did not continue for more than 5 days. Therefore, caudal epidural adhesiolysis was scheduled, and the patient was hospitalized. Before the operation, the patient was placed in the prone position, and the sacral hiatus area was disinfected with 10% povidone-iodine solution and chlorhexidine. The operating area was covered with a surgical drape. The sacral hiatus was identified with C-arm, and infiltration anesthesia was performed with 4 ml of 1% lidocaine. Then, as the 17-G introducer needle punctured the sacrococcygeal ligament, a clear fluid flowed out through the needle, with a loss of resistance. The length that the introducer needle was pushed in was approximately 2 cm from the skin, and 3 ml of the contrast medium iopamidol (Iopamiro 370®, Ilsung Pharm Co., Seoul, Korea) was injected through the needle to observe the myelogram spreading to the L4 level or above (Fig. 1). We concluded that unexpected dural puncture had occurred, and the patient was placed under observation after removal of the introducer needle.
Fig. 1.
Contrast dye injection to the introducer needle showed a myelogram in the anteroposterior view.
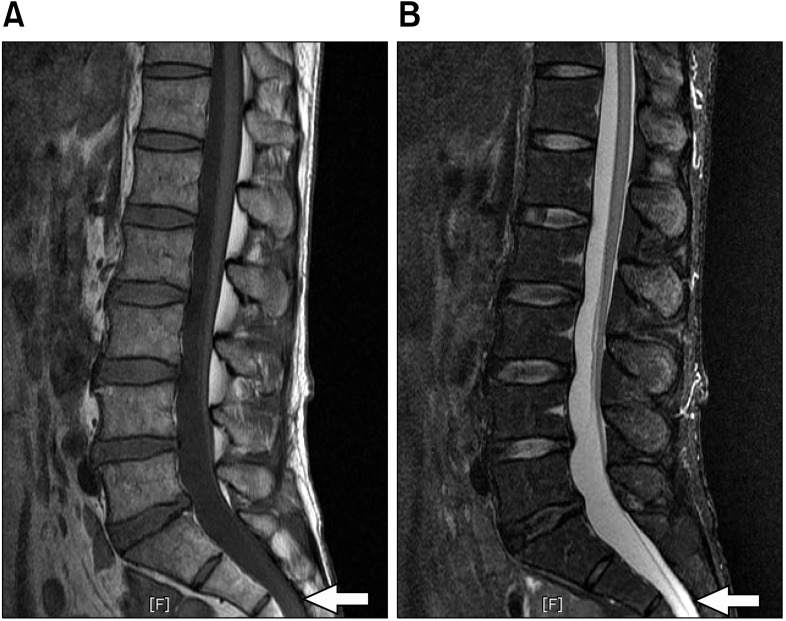
The patient's MRI was examined again, and it showed a low termination of the dural sac, with the dural sac tip located below the S3 level (Fig. 2). However, there were no accompanying pathological conditions, such as ameningeal structure forming cystic structures. The patient was observed for three days, but there were no symptoms such as postdural puncture headache. Therefore, the patient was discharged with follow-up observations scheduled to be performed at the clinic.
Fig. 2.
Sagittal T1-weighted (A) and T2-weighted (B) MR images show extension of dural sac to the lower level of sacrum.
DISCUSSION
Epidural adhesiolysis eliminates fibrous tissue from the epidural space and injects medication into this area. It is an effective pain treatment method that blocks nerve activity in the scarred area and reduces infection and edema. The reason for preferring the caudal approach in epidural adhesiolysis is that the lumbar approach carries a 0.82% risk of entering the subdural space, while there is less possibility of this occurring with the caudal approach [5]. In addition, the solution injected into the lumbar epidural space is spread to the less resistant buttocks, and not enough solution will reach the epidural adhesions [6].
There are reports that unexpected dural punctures can occur during a caudal block due to anatomical abnormalities in the lumbar area. Broadly, there are two situations in which dural puncture can occur. First, it can occur when the cystic structure, including the cerebrospinal fluid, is extended to the lower sacrum due to pathological conditions such as sacral meningocele or perineural cyst. Second, it can occur when the dural sac terminates abnormally low, with the dural sac tip located at the lower sacrum, due to simple anatomical variation [2]. Therefore, using a longer needle in a caudal block or excessively advancing the block needle through the sacrococcygeal ligament to reach the S2 level can cause venipuncture or unexpected dural puncture [1]. In our case, the sacrococcygeal ligament was punctured with an introducer needle for epidural adhesiolysis, and dural puncture occurred even though the needle was advanced no farther. Myer [1] and Park [2] reported similar situations.
The dural sac with spinal fluid generally extends down to the S1-S2 level, but there can be large variation among individuals. Evison et al. [7] and Larsen and Olsen [8] even described patients in whom the dural sac reached the S4-S5 intervertebral space in a myelographic study. Macdonald et al. [9] investigated the distribution of dural sac tip levels in the lumbar MRIs of 136 male and female patients and reported that 10% were in the upper S3, 4% were in the lower S3, and 1% was in the upper S4; thus, a total of 15% of patients had dural sac tip levels reaching the lower sacrum. On the other hand, by investigating the lumbar MRIs of patients who visited our pain clinic in the last year, we found that 2.5% had simple anatomical variation and 1% had a pathological condition, resulting in a total of 3.5% of patients with dural sac tip levels reaching S3 or lower. In addition, MRI study of 2,669 male and female Korean patients complaining of back pain or sciatica, found that 0.8% had simple anatomical variation and 0.8% had a perineural cyst at or below the S3 level, resulting in a total 1.6% of patients with dural sac levels at or below S3. When the dural sac tip simply happens to be located at the lower sacrum, there are no particular symptoms caused by the dural sac itself, and specific treatment is not necessary.
In some cases, the dural sac is abnormally extended to the lower sacrum due to a pathological condition, and sacral meningeal cysts can be observed. Pathologically, these conditions can be differentiated into sacral meningocele, perineural cyst, meningeal diverticulum, or extradural meningeal cyst, but the radiographic findings and clinical observations are generally similar for each [3]. Most cysts are asymptomatic and do not require treatment, but when there are neurological symptoms, treatments such as decompressive laminectomy, lumboperitoneal shunting, or percutaneous drainage of cysts are necessary.
Aggarwal et al. [10] investigated the sacral hiatus anatomy in 49 adult male Indian cadavers. The length from the apex of the hiatus to the dural end had a mean value of 31.6 mm. However,as the minimum value was 5.76 mm, the needle should not advance more than 5 mm from the sacrococcygeal ligament during a caudal block to prevent dural puncture. In addition, in the MRI study of Joo et al. [4], the distance from the lower margin of the third sacral vertebra to the sacral hiatus was on average 3 cm; therefore, in patients whose dural sac tip is located at or below the S3 level, needle depths within 3 cm can cause dural punctures. Therefore, it is safer to avoid using needles longer than 4 cm [11]. In addition, when the needle is too thin, aspiration of the cerebrospinal fluid might not be identified even when there is a dural puncture, which can lead to a total spinal block.
As can be seen, dural puncture can occur unexpectedly in rare situations while attempting an epidural block or epidural adhesiolysis using the caudal approach. Therefore, anatomical understanding and suitable countermeasures regarding accidental dural puncture are necessary. To prevent such situations, imaging studies such as MRI should be performed and closely reviewed to identify anatomical variations in the dural sac.
References
- 1.Meyer RJ. Dural puncture via the sacral hiatus. Anaesthesia. 1984;39:610. doi: 10.1111/j.1365-2044.1984.tb07393.x. [DOI] [PubMed] [Google Scholar]
- 2.Park BC, Kim BS, Hwang WJ, Lee J, Moon DE. Anatomical variations which can result in inadvertent dural puncture when performing caudal block: a report of 3 cases. Korean J Anesthesiol. 2006;50:332–336. [Google Scholar]
- 3.Kang MS, Lim YJ, Lee SC. Sacral meningeal cyst detected during caudal epidural block. J Korean Pain Soc. 1999;12:258–262. [Google Scholar]
- 4.Joo J, Kim J, Lee J. The prevalence of anatomical variations that can cause inadvertent dural puncture when performing caudal block in Koreans: a study using magnetic resonance imaging. Anaesthesia. 2010;65:23–26. doi: 10.1111/j.1365-2044.2009.06168.x. [DOI] [PubMed] [Google Scholar]
- 5.Lubenow T, Keh-Wong E, Kristof K, Ivankovich O, Ivankovich AD. Inadvertent subdural injection: a complication of an epidural block. Anesth Analg. 1988;67:175–179. [PubMed] [Google Scholar]
- 6.Racz GB, Holubec JT. Techniques of neurolysis. Boston: Kluwer Academic; 1989. Lysis of adhesion in the epidural space; pp. 57–72. [Google Scholar]
- 7.Evison G, Windsor P, Duck F. Myelographic features of the normal sacral sac. Br J Radiol. 1979;52:777–780. doi: 10.1259/0007-1285-52-622-777. [DOI] [PubMed] [Google Scholar]
- 8.Larsen JL, Olsen KO. Radiographic anatomy of the distal dural sac. A myelographic investigation of dimensions and termination. Acta Radiol. 1991;32:214–219. [PubMed] [Google Scholar]
- 9.Macdonald A, Chatrath P, Spector T, Ellis H. Level of termination of the spinal cord and the dural sac: a magnetic resonance study. Clin Anat. 1999;12:149–152. doi: 10.1002/(SICI)1098-2353(1999)12:3<149::AID-CA1>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 10.Aggarwal A, Kaur H, Batra YK, Aggarwal AK, Rajeev S, Sahni D. Anatomic consideration of caudal epidural space: a cadaver study. Clin Anat. 2009;22:730–737. doi: 10.1002/ca.20832. [DOI] [PubMed] [Google Scholar]
- 11.Waldman JD. Pain management. 2nd ed. Philadelphia: Elsevier Saunders; 2011. pp. 248–256. [Google Scholar]