Abstract
Background:
Epithelial cell adhesion molecule (EpCAM) is frequently expressed in breast cancer, and its expression has been associated with poor prognosis. Breast cancer can be subdivided into intrinsic subtypes, differing in prognosis and response to therapy.
Methods:
To investigate the association between EpCAM expression and prognosis in the intrinsic subtypes of breast cancer, we performed immunohistochemical studies on a tissue microarray encompassing a total of 1365 breast cancers with detailed clinicopathological annotation and outcomes data.
Results:
We observed EpCAM expression in 660 out of 1365 (48%) cases. EpCAM expression varied significantly in the different intrinsic subtypes. In univariate analyses of all cases, EpCAM expression was associated with a significantly worse overall survival. In the intrinsic subtypes, EpCAM expression was associated with an unfavourable prognosis in the basal-like and luminal B HER2+ subtypes but associated with a favourable prognosis in the HER2 subtype. Consistently, specific ablation of EpCAM resulted in increased cell viability in the breast cancer cell line SKBR3 (ER−, PR−, and HER2+) but decreased viability in the breast cancer cell line MDA-MB-231 (ER−, PR−, and HER2− ).
Conclusion:
The differential association of EpCAM expression with prognosis in intrinsic subtypes has important implications for the development of EpCAM-targeted therapies in breast cancer.
Keywords: EpCAM, breast cancer, intrinsic subtypes, prognostic factor
The epithelial cell adhesion molecule (EpCAM, also designated TACSTD1, CD326) is a type I transmembrane protein of 314 amino acids that is localised to the basolateral membrane in the majority of normal epithelial tissues. The functional role of EpCAM in cell adhesion was the focus of early studies, and EpCAM has been demonstrated to be a calcium-independent homophilic cell adhesion molecule (Litvinov et al, 1994). Recent studies have also demonstrated a role for EpCAM in cell signalling and carcinogenesis (Munz et al, 2004; Osta et al, 2004; Maetzel et al, 2009). EpCAM is perhaps best known for the fact that it is expressed in the majority of human epithelial cancers, including colorectal, breast, gastric, prostate, ovarian, and lung cancer (Spizzo et al, 2004; Went et al, 2004). EpCAM was the first human tumour-associated antigen to be identified with monoclonal antibodies (Herlyn et al, 1979) and was the first target of monoclonal antibody therapy in humans (Sears et al, 1982). EpCAM expression has also been used to enrich circulating tumour cells before microscopic evaluation in the only FDA-approved assay for detection of circulating tumour cells in breast cancer (Cristofanilli et al, 2004). Finally, EpCAM-targeted therapies remain under active investigation, and a recent report highlighted at least seven different molecular therapies targeting EpCAM in various cancer types, including breast, gastric, ovarian, and lung cancer (Baeuerle and Gires, 2007). Particular effort is being made for breast cancer patients, where EpCAM expression appears to predict response to EpCAM-targeting antibodies (Schmidt et al, 2010; Schmidt et al, 2012).
EpCAM expression in primary cancer specimens has been associated with a favourable prognosis in some cancer types and an unfavourable prognosis in other cancer types. For instance, EpCAM expression in primary breast and ovarian cancers as measured by immunohistochemistry is associated with poor overall survival (OS; Spizzo et al, 2002; Spizzo et al, 2004; Spizzo et al, 2006; Schmidt et al, 2008), while EpCAM expression in colorectal and gastric cancer is associated with more favourable prognosis (Songun et al, 2005; Went et al, 2006). All of these studies were performed using standardised assay conditions and several used tissue microarrays (TMAs); taken together, these studies include specimens from over 6000 cancer patients. This differential association between EpCAM expression and prognosis is paralleled in functional studies of EpCAM biology performed both in vitro and in vivo. Loss-of-function analyses using RNA interference suggest that EpCAM expression is associated with increased invasion in breast cancer (Osta et al, 2004; Sankpal et al, 2009a, 2009b, 2011), and gain-of-function analyses in colorectal and lung cancer suggest that EpCAM expression is associated with decreased cancer invasion (Basak et al, 1998; Tai et al, 2007). Moreover, in breast cancer cell lines, the impact of EpCAM expression on proliferation has been recently shown to depend on the epithelial and mesenchymal phenotype of these cells (Martowicz et al, 2012). Taken together, these studies suggest that the impact of EpCAM expression on cancer biology may be context-dependent (reviewed in van der Gun et al, 2010).
Breast cancer is a heterogeneous disease. Recent advances in molecular biology, including the development of sophisticated techniques for gene expression profiling, have established a new taxonomy of breast cancer, defining the breast cancer intrinsic subtypes (Perou et al, 2000). This new taxonomy has had a profound impact on the clinical management of breast cancer, as the intrinsic subtypes differ markedly in prognosis and response to therapy. As gene expression profiling data are not always available, a recent international consensus conference defined an approximation, using immunohistochemical expression of oestrogen receptor (ER) and progesterone receptor (PR), overexpression, and/or amplification of the human epidermal growth factor receptor 2 (HER2) and Ki67 labelling index to approximate the breast cancer intrinsic subtypes (Goldhirsch et al, 2011).
Although EpCAM expression is associated with poor prognosis in breast cancer, the impact of EpCAM expression on prognosis in the breast cancer intrinsic subtypes remains to be defined. As noted above, this is an important question, as the breast cancer intrinsic subtypes have distinct biology, and there is strong evidence suggesting that the impact of EpCAM in cancer is context-dependent. To definitively address this question, we performed immunohistochemical studies on a breast cancer TMA encompassing a total of 1365 breast cancer cases with detailed clinical annotation and outcomes data. A better understanding of the relationship between EpCAM expression and prognosis in the breast cancer intrinsic subtypes has important implications for the design and successful application of molecular therapies targeting EpCAM in breast cancer.
Materials and methods
Tissue microarray
We used a TMA encompassing a total of 2020 breast cancer tissue punches from 1579 formalin-fixed and paraffin-embedded tumour samples. These samples were collected from patients diagnosed with primary breast cancer between 1985 and 2007 at the University of Basel and the Viollier Institute in Basel, Switzerland. Of these 2020 tissue punches, a total of 1365 cases were evaluable for our study. The tissue samples were brought into a TMA format as previously described (Bubendorf et al, 2001). Briefly, 0.6-mm tissue cylinders were punched out of donor tumour tissue blocks and transferred into a recipient paraffin block using a semi-automated tissue arrayer. Each TMA contained a number of tumour punches ranging from 159 to 522. Histopathological data were obtained from the original pathology reports, and patient outcomes data were obtained from the Cancer Registry of Basel or from the patient's attending physician. Retrieval of tissue and clinical data was performed in accordance with the regulations of the local institutional review boards, with specific attention to ethical standards and patient confidentiality.
Immunohistochemistry
Immunohistochemical staining of the TMA was performed as described previously (Tapia et al, 2011). For EpCAM immunohistochemistry, 4 μm sections of the TMA blocks were incubated overnight with a primary anti-EpCAM monoclonal antibody (1 : 800; clone VU-1D9, Novocastra, Newcastle, UK) after heat-induced antigen retrieval. Standard ABC-technique (ABC-Elite-Kit, Vector Laboratories, Burlingham, CA, USA) was used for immunostaining, and diaminobenzidine was used as chromogen. Counterstaining was performed with hematoxylin solution. The staining intensity of ER, PR, and HER2 was scored as previously described (Tapia et al, 2011). EpCAM expression was quantified using the modified Histo-score (H-score) (McCarty et al, 1985), with a range of possible scores from 0–300. Frequency and staining intensity of EpCAM on tumour cells were analysed, and EpCAM expression was dichotomised into two groups according to the frequency distributions of the H-scores, using a cut-off score of ⩾100 (H-score 0–99=negative/low expression and 100–300=positive expression).
Statistical analysis
The distribution of patient and clinical characteristics between EpCAM-positive and EpCAM-negative tumours was compared using the Chi-square test, Wilcoxon's rank sum test, or two-sample t-test, as appropriate. OS was defined as the time from the first operation to death due to any cause. Survivors were censored at the date of last contact. Survival curves by EpCAM status were estimated using the Kaplan–Meier product-limit method and compared by log-rank test. Univariate Cox proportional hazard models were fit to identify factors significantly related to OS. To assess whether EpCAM was an independent predictor of survival, a multivariate Cox model was constructed to adjust other patient/clinical characteristics that were significant in the univariate analyses. Two-way interaction terms between EpCAM and other factors in the multivariate Cox model were also assessed. All analyses were two-sided and significance was set at a P-value of 0.05. Statistical analyses were performed using SAS (SAS Institutes, Cary, NC, USA).
Cell culture
All breast cancer cell lines were obtained from the American Type Culture Collection (Rockville, MD, USA). MCF-10A cells were grown in DMEM/F12 medium supplemented with 5% donor horse serum, 20 ng ml−1 epidermal growth factor, 10 μg ml−1 insulin, 100 μg ml−1 hydrocortisone, and 1 ng ml−1 cholera toxin. MDA-MB-231 and SKBR3 cells were grown in DMEM medium supplemented with 10% FBS.
Antibodies and western blot analysis
Western blotting was performed by standard procedures. Cell lysates were harvested with RIPA buffer (50 mℳ Tris HCl pH 7.4, 150 mℳ NaCl, 2 mℳ EDTA, 1% NP40, 0.1% SDS, 0.5% sodium deoxycholate, 1 × complete protease inhibitors (Roche, Basel, Switzerland), and phosphatase inhibitors, including sodium orthovanadate (Sigma, St. Louis, MO, USA) and sodium fluoride (Sigma). Protein concentration was measured using the BCA protein assay (Thermo Scientific, Rockford, IL, USA). Equal loading of each sample of protein (20 μg) was then subjected to SDS–PAGE (NuPAGE, Invitrogen, Carlsbad, CA, USA) and transferred by electrophoresis to a PVDF membrane. Antibodies against EpCAM C-10 (Santa Cruz, Dallas, TX, USA) and Actin C-4 (Santa Cruz) were used at ratios of 1 : 1000 and 1 : 5000, respectively, and detection was performed with HRP-conjugated antisera and chemiluminescence (Thermo Scientific, Rockford, IL, USA).
Lentiviral shRNA production and infections
Lentiviral vectors encoding shRNAs specific for EpCAM as well as control GFP sequences are part of The RNAi Consortium shRNA Library (http://www.broadinstitute.org/rnai/trc). Sequences are as follows: for shRNA EpCAM, 5′GCAAATGGACACAAATTACAA3′ and for shRNA GFP, 5′ACAACAGCCACAACGTCTATA3′. Lentivirus was produced by transfection of 293T cells with vectors encoding gene-specific shRNAs (1 μg) together with the packaging plasmids encoding Δ8.9 and VSV-G using Fugene 6 (Roche). Culture supernatants containing lentivirus were collected 48 and 72 h post transfection. Virus was pooled and stored at −80 °C. Cells were infected using a 1 : 11 dilution of virus in polybrene-containing media. Following centrifugation at 1000 g for 15 min, all breast cancer cell lines were selected in puromycin (1 μg ml−1) starting 24 h post infection. Viability assays were conducted 10 days post infection using crystal violet. Protein lysates were harvested 72 h following shRNA expression to evaluate gene suppression.
Crystal violet cell proliferation assay
Cell proliferation assays were performed in six-well plates. Cells were plated to achieve 50% cell density on day of lentiviral infection. Puromycin selection 24 h post infection was performed. On day 3 post infection, cells were re-plated onto 60-mm dishes. On day 10, plates were stained with crystal violet (crystal violet 0.2%, ethanol 2%) and photographed. The crystal violet stain was then solubilised in 1% SDS solution with incubation on a shaker for 1 h at room temperature. Optical density was measured at 595 nm. Cell proliferation effects for SK-BR-3 after exposure to EpCAM shRNA and GFP shRNA were analysed as percentages. The solubilised dye from the EpCAM shRNA sample was read at 100% and then serially diluted to 75%, 50%, and 25% to generate a crystal violet curve to extrapolate the percentage for the GFP shRNA sample. Data presented are representative of three independent experiments.
Results
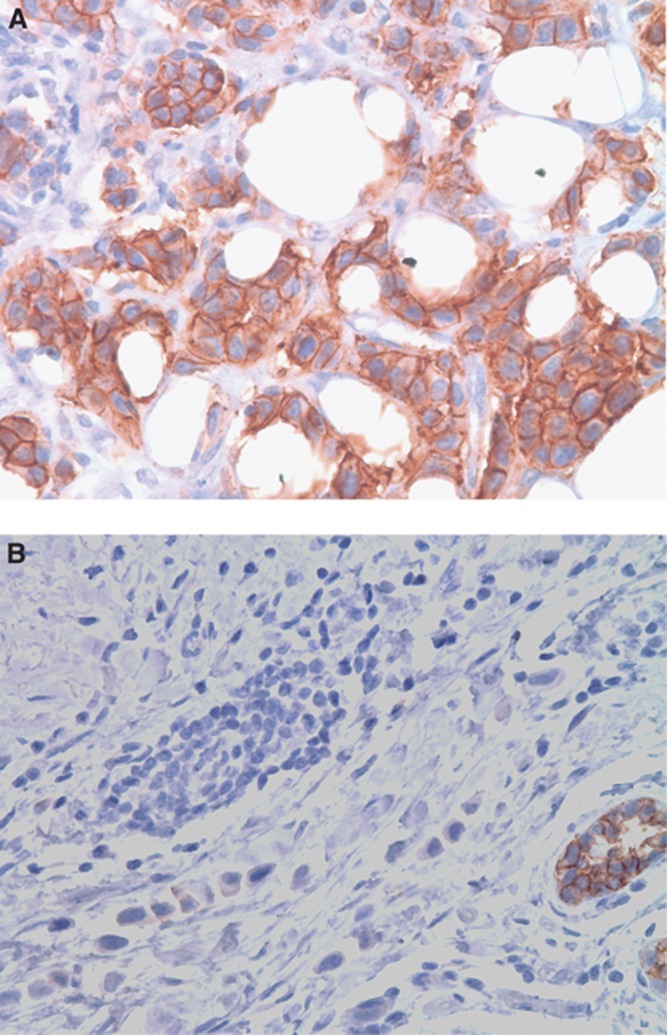
The expression of EpCAM could be evaluated in 1365 cases in this cohort. Basic demographic information for the 1365 evaluable cases is presented in Table 1. The mean age at diagnosis was 63.5 years (range 27–101 years), and the mean follow-up time was 80.8 months (range 1–263 months). Expression of EpCAM was confined to the membrane of breast cancer cells in all the cases (Figure 1). EpCAM expression was defined using the H-score, a score integrating the intensity of EpCAM staining, and the percentage of breast cancer cells expressing EpCAM. With an H-score threshold of ⩾100, a total of 660 breast cancers (48.3%) expressed EpCAM. Consistent with previous studies, EpCAM expression was significantly associated with greater tumour size, lymph node involvement, tumour stage, and tumour grade (Table 2; Gastl et al, 2000; Schmidt et al, 2008; Agboola et al, 2011; Spizzo et al, 2011). EpCAM expression was significantly higher in ER-negative (ER−) cases (EpCAM expression 65.1% in ER− cancers vs 42.9% in ER+ cancers, P<0.0001, Table 2) and in HER2+ cases (EpCAM expression 54.3% in HER2+ cancers vs 46.9% in HER2− cancers, P=0.0298, Table 2). EpCAM expression was also significantly associated with histological subtype (P<0.0001); EpCAM expression was higher in the invasive ductal (51%) and medullary (84%) histological types and lower in the invasive lobular (26%) and cribiform (29%) subtypes (Table 3). EpCAM expression varied significantly between the intrinsic subtypes of breast cancer, as defined by the St. Gallen Consensus Conference criteria (Goldhirsch et al, 2011). EpCAM overexpression was highest in the basal-like (64%) and HER2 (73%) subtypes and lowest in the luminal A subtype (23%, P<0.0001; Table 4). Furthermore, EpCAM expression was highly correlated with the expression of Ki-67 in all of the intrinsic subtypes except for luminal A (data not shown).
Table 1. Basic demographic data for 1365 evaluable breast cancer cases.
| Mean tumour size (mm) |
31.0 |
|
| Mean age at diagnosis (years) |
63.5 |
|
|
Tumour stage | ||
| |
Number (n) |
% |
| pT1 |
364 |
26.7 |
| pT2 |
728 |
53.4 |
| pT3 |
104 |
7.6 |
| pT4 |
169 |
12.3 |
|
Lymph node involvement | ||
| pN0 |
701 |
51.5 |
| pN1 |
529 |
38.8 |
| pN2 |
132 |
9.7 |
|
Tumour grade | ||
| 1 |
318 |
23.3 |
| 2 |
551 |
40.4 |
| 3 |
496 |
36.3 |
|
Histological subtype | ||
| Invasive ductal |
977 |
71.6 |
| Invasive lobular |
187 |
13.7 |
| Mucinous |
38 |
2.8 |
| Apocrine |
17 |
1.2 |
| Cribriform |
41 |
3.0 |
| Papillary |
18 |
1.3 |
| Medullary |
43 |
3.2 |
| Other |
43 |
3.2 |
|
Intrinsic subtype | ||
| Luminal A (ER+ and/or PR+, HER2−, Ki-67<14%) |
213 |
15.6 |
| Luminal B (HER2-negative) ER+ and/or PR+, HER2−, Ki-67⩾14%) |
673 |
49.3 |
| Luminal B (HER2-positive) (ER+ and/or PR+, HER2+) |
154 |
11.3 |
| HER2 type (ER− or PR−, HER2+) |
111 |
8.2 |
| Basal-like (ER−, PR−, HER2−) | 213 | 15.6 |
Abbreviations: ER=oestrogen receptor; HER2=human epidermal growth factor receptor 2; pr=progesterone receptor.
Figure 1.
Representative photographs of EpCAM expression in breast cancer. (A) Strong membranous expression in 100% of tumour cells. (B) Negative expression on tumour cells with positive expression in normal mammary glands as an internal positive control. Original magnification × 400. A full color version of this figure is available at the British Journal of Cancer online.
Table 2. Association between EpCAM expression and clinicopathological parameters.
| Clinicopathological parameter | EpCAM-positive | EpCAM-negative | P value | ||
|---|---|---|---|---|---|
| Mean tumour size (mm) |
34.2 |
27.8 |
<0.0001 |
||
| Mean age age at diagnosis (years) |
63.7 |
63.3 |
0.6220 |
||
|
Tumour stage |
|
|
|
|
<0.0001 |
| pT1 |
132 |
36.3 |
232 |
63.7 |
|
| pT2 |
366 |
50.3 |
362 |
49.7 |
|
| pT3 |
65 |
62.5 |
39 |
37.5 |
|
| pT4 |
97 |
57.4 |
72 |
42.6 |
|
|
Lymph node involvement |
|
|
|
|
0.0023 |
| pN0 |
329 |
46.9 |
372 |
53.1 |
|
| pN1 |
248 |
46.9 |
281 |
53.1 |
|
| pN2 |
83 |
62.9 |
49 |
37.1 |
|
|
Tumour grade |
|
|
|
|
<0.0001 |
| 1 |
99 |
31.1 |
219 |
68.9 |
|
| 2 |
234 |
42.5 |
317 |
57.5 |
|
| 3 |
327 |
65.9 |
169 |
34.1 |
|
|
Oestrogen receptor |
|
|
|
|
<0.0001 |
| ER+ |
439 |
42.9 |
583 |
57.1 |
|
| ER− |
221 |
65.2 |
118 |
34.8 |
|
|
HER2 |
|
|
|
|
0.0298 |
| HER2+ |
144 |
54.3 |
121 |
45.7 |
|
| HER2− |
516 |
46.9 |
584 |
53.1 |
|
|
Ki67 |
|
|
|
|
<0.0001 |
| Ki67+ |
593 |
55.4 |
477 |
44.6 |
|
| Ki67− | 66 | 23.0 | 221 | 77.0 | |
Abbreviations: EpCAM=epithelial cell adhesion molecule; ER=oestrogen receptor; HER2=human epidermal growth factor receptor 2; PR=progesterone receptor.
Table 3. Association between EpCAM expression and histological subtype.
| |
EpCAM-positive |
EpCAM-negative |
P-value |
||
|---|---|---|---|---|---|
| Histological subtype | n | % | n | % | <0.0001 |
| Invasive ductal |
496 |
50.8 |
481 |
49.2 |
|
| Lobular |
48 |
25.7 |
139 |
74.3 |
|
| Mucinous |
20 |
52.6 |
18 |
47.4 |
|
| Apocrine |
13 |
76.5 |
4 |
23.5 |
|
| Cribiform |
12 |
29.3 |
29 |
70.7 |
|
| Papillary |
12 |
66.7 |
6 |
33.3 |
|
| Medullary |
36 |
83.7 |
7 |
16.3 |
|
| Other | 23 | 53.5 | 20 | 46.5 | |
Abbreviation: EpCAM=epithelial cell adhesion molecule.
Table 4. Association between EpCAM expression and breast cancer intrinsic subtype.
|
EpCAM-positive |
EpCAM-negative |
P-value |
|||
|---|---|---|---|---|---|
| Intrinsic subtype | n | % | n | % | <0.0001 |
| Luminal A (ER+ and/or PR+, HER2−, Ki-67<14%) |
48 |
22.5 |
165 |
77.5 |
|
| Luminal B (HER2-negative) (ER+ and/or PR+, HER2−, Ki-67⩾14%) |
332 |
49.3 |
341 |
50.7 |
|
| Luminal B (HER2-positive) (ER+ and/or PR+, HER2+) |
63 |
40.9 |
91 |
59.1 |
|
| HER2 type (ER−, PR−, HER2+) |
81 |
73.0 |
30 |
27.0 |
|
| Basal-like (ER−, PR−, HER2−) | 136 | 63.8 | 77 | 36.2 | |
Abbreviations: EpCAM=epithelial cell adhesion molecule; ER=oestrogen receptor; HER2=human epidermal growth factor receptor 2; PR=progesterone receptor.
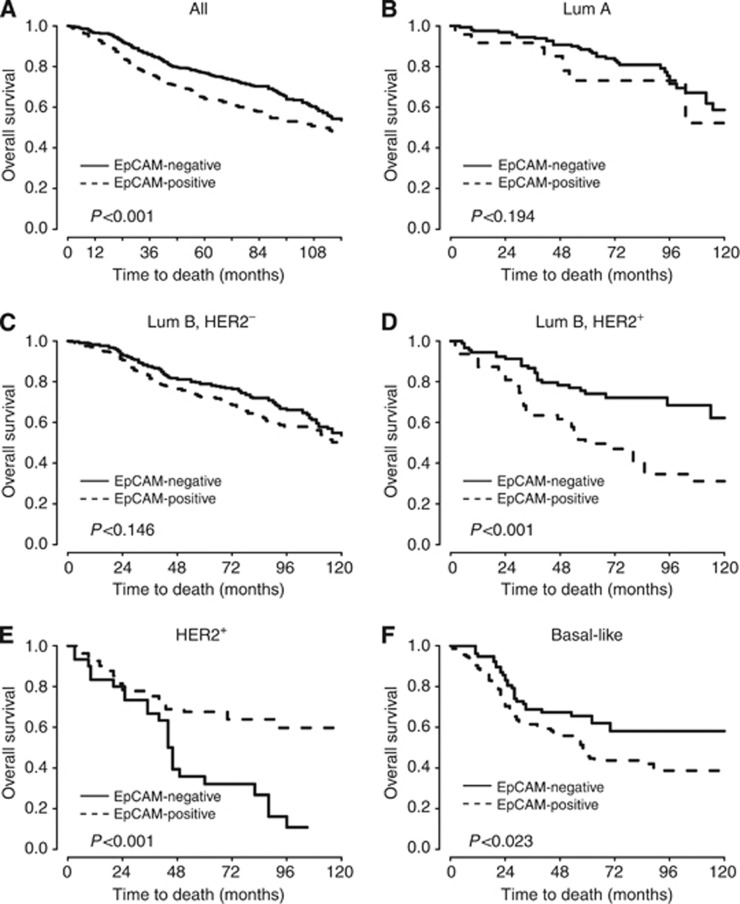
In univariate survival analyses, we could demonstrate that breast cancer cases with EpCAM expression had a significantly worse OS (hazard ratio (HR)=1.402, P=0.0001; Table 5 and Figure 2). In univariate analyses of the breast cancer intrinsic subtypes, EpCAM expression was associated with significantly decreased OS in the luminal B HER2+ subtype (HR=2.4, P=0.0006) and the basal-like subtype (HR=1.634, P=0.023; Table 5 and Figure 2). The luminal A and the luminal B HER2− subtypes also showed a trend towards decreased OS with EpCAM expression (Table 5 and Figure 2), but this was not statistically significant. Of particular interest, EpCAM expression was significantly associated with improved OS in the HER2 subtype (HR=0.374, P=0.0004; Table 5 and Figure 2). In multivariate analysis, after adjusting for age, tumour size, lymph node involvement, tumour grade, and intrinsic subtype, EpCAM expression remained significantly associated with improved OS in the HER2 subtype (HR=0.329, P<0.0001) and showed a trend toward decreased OS in the luminal B HER2+ subtype (HR=1.546, P=0.094) and the basal-like subtype (HR=1.437, P=0.096; Table 6).
Table 5. Univariate analyses for all cases, and by intrinsic subtype, for the effect of EpCAM expression on overall survival.
| EpCAM expression, all cases | Hazard ratio (95% CI) | P-value |
|---|---|---|
| EpCAM-positive |
1.402 (1.178–1.668) |
0.0001 |
|
EpCAM expression, by intrinsic subtype | ||
| Luminal A |
1.487 (0.817–2.707) |
0.1937 |
| Luminal B (HER2−) |
1.208 (0.936–1.560) |
0.1464 |
| Luminal B (HER2+) |
2.400 (1.451–3.971) |
0.0006 |
| HER2 type |
0.374 (0.217–0.644) |
0.0004 |
| Basal-like | 1.634 (1.070–2.497) | 0.0231 |
Abbreviations: EpCAM=epithelial cell adhesion molecule; CI=confidence interval; HER2=human epidermal growth factor receptor 2.
Figure 2.
Kaplan–Meier survival curves. (A) Kaplan–Meier survival curve for overall survival depending on EpCAM overexpression (univariate analysis). (B–F) Kaplan–Meier survival curves for overall survival depending on EpCAM overexpression for indivdual intrinsic breast cancer subtypes.
Table 6. Multivariate analysis for the effect of clinicopathological parameters and EpCAM expression on overall survival.
| Clinicopathological parameter | Hazard ratio (95% CI) | P-value |
|---|---|---|
| Age (per 1 year ) |
1.037 (1.029–1.044) |
<0.0001 |
|
Tumour stage | ||
| pT1 (reference) |
1 |
|
| pT2 |
1.603 (1.226–2.097) |
0.0006 |
| pT3 |
2.089 (1.437–3.037) |
0.0001 |
| pT4 |
2.208 (1.581–3.083) |
<0.0001 |
|
Lymph node involvement | ||
| pN1 (reference) |
1 |
|
| pN1 |
1.427 (1.168–1.745) |
0.0005 |
| pN2 |
2.782 (2.103–3.680) |
<0.0001 |
|
Tumour grade | ||
| BRE grade 1 (reference) |
1 |
|
| Grade 2 |
1.631 (1.230–3.454) |
0.0006 |
| Grade 3 |
2.571 (1.914–3.454) |
<0.0001 |
|
Intrinsic subtype | ||
| Luminal A (reference) |
1 |
|
| Luminal B (HER2−) |
1.081 (0.792–1.475) |
0.6237 |
| Luminal B (HER2+) |
1.263 (0.864–1.848) |
0.2283 |
| HER2 type |
1.193 (0.784–1.815) |
0.4097 |
| Basal-like |
2.031 (1.419–2.906) |
0.0001 |
|
EpCAM expression, by intrinsic subtype | ||
| Luminal A |
1.404 (0.771–2.557) |
0.2666 |
| Luminal B (HER2−) |
0.860 (0.660–1.119) |
0.2614 |
| Luminal B (HER2+) |
1.546 (0.928–2.575) |
0.0941 |
| HER2 type |
0.329 (0.190–0.570) |
<0.0001 |
| Basal-like | 1.437 (0.938–2.201) | 0.0958 |
Abbreviations: EpCAM=epithelial cell adhesion molecule; BRE=Elsten's modification of Bloom and Richardson; CI=confidence interval; HER2=human epidermal growth factor receptor 2.
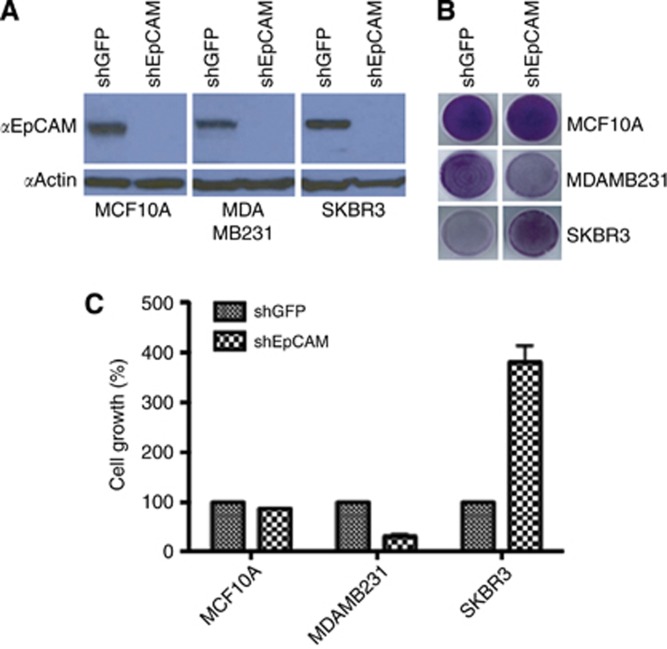
Previously, we demonstrated that specific ablation of EpCAM significantly decreased proliferation of the basal-like breast cancer cell line MDA-MB-231, with minimal impact on proliferation of the breast epithelial cell line MCF10A. Given the differential association between EpCAM and prognosis in the HER2 and basal-like intrinsic subtypes of breast cancer, we sought to evaluate the impact of EpCAM expression on proliferation in representative breast cancer cell lines in vitro. We specifically ablated EpCAM expression in the MCF10A, MDA-MB-231, and SKBR3 (ER−/PR−/HER2+) cell lines (Figure 3). Of note, we not only confirmed that specific ablation of EpCAM decreases proliferation in the MDA-MB-231 cell line but also demonstrated that specific ablation of EpCAM results in an almost four-fold increase in proliferation in the SKBR3 cell line, consistent with the IHC analyses.
Figure 3.
Specific ablation of EpCAM results in increased SKBR3 breast cancer cell viability. (A) EpCAM-shRNA specifically ablates EpCAM protein levels in MCF-10A, MDA-MB-231, and SKBR3 cells 72 h post infection relative to shGFP control vector. (B) Crystal violet-stained plates depicting cell growth differences in MCF10A, MDA-MB-231, and SKBR3 cells 14 days post infection. Plates representative of three independent experiments. (C) Crystal violet growth assay used to quantify the growth differences between the breast cancer cell lines. A full color version of this figure is available at the British Journal of Cancer online.
Discussion
EpCAM is commonly expressed in breast cancer, and EpCAM expression in primary breast cancers has been widely reported to be associated with poor prognosis. However, breast cancer is a heterogeneous disease, and the impact of EpCAM expression on prognosis in the breast cancer intrinsic subtypes remains to be investigated. Here, we studied EpCAM expression in a large cohort of primary breast cancers, with a particular focus on defining the potential associations between EpCAM expression and the breast cancer intrinsic subtypes, as defined by the most recent St. Gallen Consensus Conference (Goldhirsch et al, 2011). Of note, we demonstrate for the first time that EpCAM expression varies significantly between the intrinsic subtypes of breast cancer, ranging from 22.5% in luminal A to 73.0% in the HER2 subtype. We have also made the surprising observation that the impact of EpCAM expression on prognosis in breast cancer is dependent on intrinsic subtype. In the basal-like and luminal B HER2+ subtypes, EpCAM expression is associated with an unfavourable prognosis; in the HER2 subtype, EpCAM expression is associated with a favourable prognosis.
Our study confirms the results of previous studies demonstrating that EpCAM expression is associated with tumour size, lymph node involvement, tumour grade, and prognosis in breast cancer (Tandon et al, 1990; Schmidt et al, 2008; Spizzo et al, 2011; Agboola et al, 2011). In addition, we observed that EpCAM expression is inversely associated with expression of ER (P<0.0001) and positively associated with HER2 expression (P=0.0298), findings that have been previously reported by others (Spizzo et al, 2002; Schmidt et al, 2008; Agboola et al, 2011). Although multiple studies have suggested that EpCAM expression is an independent predictor of disease-free survival and OS (Spizzo et al, 2002; Schmidt et al, 2008; Agboola et al, 2011), we did not observe this finding in our collective (P=0.7824 in multivariate analysis). This may be related to the strong association we observed between EpCAM expression and traditional predictors of prognosis in breast cancer, such as tumour size, lymph node involvement, tumour grade, ER status, HER2 status, intrinsic subtype, and Ki67 labelling index.
This study is the first to evaluate the association between EpCAM expression and prognosis in the intrinsic subtypes of breast cancer. To do this, we used well-recognised criteria for approximating the intrinsic subtypes using immunohistochemical criteria (ER status, PR status, HER2, Ki67 labelling index). Because of the large sample size (n=1365 cases), we had adequate power to meaningfully evaluate potential associations between EpCAM expression and prognosis in the breast cancer intrinsic subtypes, demonstrating a surprising differential impact on prognosis between the basal-like, luminal B HER2+, and HER2 subtypes. Recently, Agboola et al (2011) investigated the impact of EpCAM expression on prognosis in a cohort of 726 primary breast cancer cases. They observed that EpCAM expression is associated with tumour size and tumour grade and is an independent predictor of disease-free and OS. They also evaluated the potential association between EpCAM expression and other biomarkers, including ER, HER2, p53, CK5/6, and CK14. Of note, they defined basal-like breast cancer as CK5/6 and/or CK14-positive and demonstrated that EpCAM expression is an independent predictor of poor prognosis in basal-like breast cancer. Although Agboola et al (2011) use a different criteria to define basal-like breast cancer, their results are consistent with the results reported here, confirming the importance of EpCAM expression in this intrinsic subtype. EpCAM-targeted therapies may be particularly appropriate in this subtype, because EpCAM is expressed in the majority of basal-like breast cancers and treatment options are otherwise limited for patients with basal-like breast cancer.
One limitation of our study is that we defined breast cancer intrinsic subtype using the St. Gallen Consensus Conference criteria. These criteria provide only an approximation of intrinsic subtype. For instance, not all triple-negative breast cancers identified by immunohistochemistry correspond to the intrinsic basal-like subtype. Although there is an approximately 80% overlap between triple-negative and intrinsic basal-like subtype, triple-negative cancers also include special histological subtypes, such as medullary and adenoid cystic carcinoma with a much lower risk of recurrence (Goldhirsch et al, 2011; Penault-Llorca and Viale, 2012). Thus, using the triple-negative phenotype as an approximation for basal-like breast cancer may underestimate the impact of EpCAM on this intrinsic subtype.
In this study, we demonstrate, for the first time, that EpCAM is highly expressed in the HER2 subtype (73.0%). Surprisingly, EpCAM expression in the HER2 subtype was associated with a significantly improved OS (P=0.0004). Consistent with these findings were the results of in vitro studies, where downregulation of EpCAM with shRNA led to increased viability and cell growth in the SKBR3 breast cancer cell line. This cell line corresponds to the HER2 subtype (ER- and PR−, HER2+), and its increased viability after specific ablation of EpCAM supports our finding that EpCAM is associated with favourable prognosis in this breast cancer subtype. The reason for this differential association with survival in the HER2 subtype is not known to date. Of note, a study by Spizzo et al (2002) suggests that concurrent EpCAM and HER2 expression may be associated with an additive negative impact on disease-related OS. In their study, however, the HER2+ cases were evaluated as a single group. The current taxonomy of breast cancer suggests that HER2+ cases should be divided into two subtypes, the luminal B HER2+ subtype (ER+ and/or PR+, HER2+) and the HER2 subtype (ER− and PR−, HER2+). In addition, Spizzo et al (2002) observed simultaneous expression of HER2 and EpCAM in a much smaller number of cases (13.2% vs 54.3% in our study). However, our study contains significantly more patient samples, and for this reason, our observations might have more power in this regard. Our data clearly suggest that EpCAM expression in the HER2 subtype is associated with a favourable prognosis. Therefore, targeting EpCAM in this group of patients should be performed with caution, particularly if the therapy is aimed at abrogating EpCAM-dependent signalling pathways.
A second limitation of this study is that we evaluated expression of extracellular EpCAM only. Recent evidence suggests that EpCAM can be cleaved at the cell surface, with nuclear translocation of the intracellular portion (Maetzel et al, 2009). Although we believe that expression of extracellular EpCAM is a surrogate for EpCAM-dependent signalling, staining with an antibody to the intracellular portion may provide better insight into the extent of EpCAM-dependent signalling. Further studies with a particular emphasis on defining EpCAM signalling may provide additional insights into the relationship between EpCAM expression and breast cancer biology.
In summary, we demonstrate that EpCAM expression is variably expressed in the breast cancer intrinsic subtypes and is differentially associated with OS in the luminal B HER2+, HER2, and basal-like intrinsic subtypes. This result is consistent with the hypothesis that the impact of EpCAM expression on cancer biology is context-dependent and has important implications for the rational development of novel therapeutics targeting EpCAM currently under clinical investigation.
Acknowledgments
We wish to acknowledge the support of the Biostatistics Core, Siteman Cancer Centre and Washington University School of Medicine, and the NCI Cancer Centre Support Grant P30 CA091842.
Footnotes
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
References
- Agboola AJ, Paish EC, Rakha EA, Powe DG, Macmillan RD, Ellis IO, Green AR. EpCAM expression is an indicator of recurrence in basal-like breast cancer. Breast Cancer Res Treat. 2011;133 (2:575–582. doi: 10.1007/s10549-011-1813-7. [DOI] [PubMed] [Google Scholar]
- Baeuerle PA, Gires O. EpCAM (CD326) finding its role in cancer. Br J Cancer. 2007;96:417–423. doi: 10.1038/sj.bjc.6603494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basak S, Speicher D, Eck S, Wunner W, Maul G, Simmons MS, Herlyn D. Colorectal carcinoma invasion inhibition by CO17-1A/GA733 antigen and its murine homologue. J Natl Cancer Inst. 1998;90:691–697. doi: 10.1093/jnci/90.9.691. [DOI] [PubMed] [Google Scholar]
- Bubendorf L, Nocito A, Moch H, Sauter G. Tissue microarray (TMA) technology: miniaturized pathology archives for high-throughput in situ studies. J Pathol. 2001;195:72–79. doi: 10.1002/path.893. [DOI] [PubMed] [Google Scholar]
- Cristofanilli M, Budd GT, Ellis MJ, Stopeck A, Matera J, Miller MC, Reuben JM, Doyle GV, Allard WJ, Terstappen LW, Hayes DF. Circulating tumor cells, disease progression, and survival in metastatic breast cancer. N Engl J Med. 2004;351:781–791. doi: 10.1056/NEJMoa040766. [DOI] [PubMed] [Google Scholar]
- Gastl G, Spizzo G, Obrist P, Dunser M, Mikuz G. Ep-CAM overexpression in breast cancer as a predictor of survival. Lancet. 2000;356:1981–1982. doi: 10.1016/S0140-6736(00)03312-2. [DOI] [PubMed] [Google Scholar]
- Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thurlimann B, Senn HJ. Strategies for subtypes—dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol. 2011;22:1736–1747. doi: 10.1093/annonc/mdr304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herlyn M, Steplewski Z, Herlyn D, Koprowski H. Colorectal carcinoma-specific antigen: detection by means of monoclonal antibodies. Proc Natl Acad Sci USA. 1979;76:1438–1442. doi: 10.1073/pnas.76.3.1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litvinov SV, Bakker HA, Gourevitch MM, Velders MP, Warnaar SO. Evidence for a role of the epithelial glycoprotein 40 (Ep-CAM) in epithelial cell-cell adhesion. Cell Adhes Commun. 1994;2:417–428. doi: 10.3109/15419069409004452. [DOI] [PubMed] [Google Scholar]
- Maetzel D, DenzeL S, Mack B, Canis M, Went P, Benk M, Kieu C, Papior P, Baeuerle PA, Munz M, Gires O. Nuclear signalling by tumour-associated antigen EpCAM. Nat Cell Biol. 2009;11:162–171. doi: 10.1038/ncb1824. [DOI] [PubMed] [Google Scholar]
- Martowicz A, Spizzo G, Gastl G, Untergasser G. Phenotype-dependent effects of EpCAM expression on growth and invasion of human breast cancer cell lines. BMC Cancer. 2012;12:501. doi: 10.1186/1471-2407-12-501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarty KS, Miller LS, Cox EB, Konrath J, McCarty KS. Estrogen receptor analyses. Correlation of biochemical and immunohistochemical methods using monoclonal antireceptor antibodies. Arch Pathol Lab Med. 1985;109:716–721. [PubMed] [Google Scholar]
- Munz M, Kieu C, Mack B, Schmitt B, Zeidler R, Gires O. The carcinoma-associated antigen EpCAM upregulates c-myc and induces cell proliferation. Oncogene. 2004;23:5748–5758. doi: 10.1038/sj.onc.1207610. [DOI] [PubMed] [Google Scholar]
- Osta WA, Chen Y, Mikhitarian K, Mitas M, Salem M, Hannun YA, Cole DJ, Gillanders WE. EpCAM is overexpressed in breast cancer and is a potential target for breast cancer gene therapy. Cancer Res. 2004;64:5818–5824. doi: 10.1158/0008-5472.CAN-04-0754. [DOI] [PubMed] [Google Scholar]
- Penault-Llorca F, Viale G. Pathological and molecular diagnosis of triple-negative breast cancer: a clinical perspective. Ann Oncol. 2012;23 Suppl 6:vi19–vi22. doi: 10.1093/annonc/mds190. [DOI] [PubMed] [Google Scholar]
- Perou CM, Sorlie T, Eisen MB, Van de rijn M, Jeffrey SS, Rees CA, Pollack JR, Ross DT, Johnsen H, Akslen LA, Fluge O, Pergamenschikov A, Williams C, Zhu SX, Lonning PE, Borresen-Dale AL, Brown PO, Botstein D. Molecular portraits of human breast tumours. Nature. 2000;406:747–752. doi: 10.1038/35021093. [DOI] [PubMed] [Google Scholar]
- Sankpal NV, Fleming TP, Gillanders WE. Dual expression lentiviral vectors for concurrent RNA interference and rescue. J Surg Res. 2009a;156:50–56. doi: 10.1016/j.jss.2009.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sankpal NV, Willman MW, Fleming TP, Mayfield JD, Gillanders WE. Transcriptional repression of epithelial cell adhesion molecule contributes to p53 control of breast cancer invasion. Cancer Res. 2009b;69:753–757. doi: 10.1158/0008-5472.CAN-08-2708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sankpal NV, Mayfield JD, Willman MW, Fleming TP, Gillanders WE. Activator protein 1 (AP-1) contributes to EpCAM-dependent breast cancer invasion. Breast Cancer Res. 2011;13:R124. doi: 10.1186/bcr3070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt M, Hasenclever D, Schaeffer M, Boehm D, Cotarelo C, Steiner E, Lebrecht A, Siggelkow W, WeikeL W, Schiffer-PETRY I, Gebhard S, Pilch H, Gehrmann M, Lehr HA, Koelbl H, Hengstler JG, Schuler M. Prognostic effect of epithelial cell adhesion molecule overexpression in untreated node-negative breast cancer. Clin Cancer Res. 2008;14:5849–5855. doi: 10.1158/1078-0432.CCR-08-0669. [DOI] [PubMed] [Google Scholar]
- Schmidt M, Ruttinger D, Sebastian M, Hanusch CA, Marschner N, Baeuerle PA, Wolf A, Goppel G, Oruzio D, Schlimok G, Steger GG, Wolf C, Eiermann W, Lang A, Schuler M. Phase IB study of the EpCAM antibody adecatumumab combined with docetaxel in patients with EpCAM-positive relapsed or refractory advanced-stage breast cancer. Ann Oncol. 2012;23:2306–2313. doi: 10.1093/annonc/mdr625. [DOI] [PubMed] [Google Scholar]
- Schmidt M, Scheulen ME, Dittrich C, Obrist P, Marschner N, Dirix L, Ruttinger D, Schuler M, Reinhardt C, Awada A. An open-label, randomized phase II study of adecatumumab, a fully human anti-EpCAM antibody, as monotherapy in patients with metastatic breast cancer. Ann Oncol. 2010;21:275–282. doi: 10.1093/annonc/mdp314. [DOI] [PubMed] [Google Scholar]
- Sears HF, Atkinson B, Mattis J, Ernst C, Herlyn D, Steplewski Z, Hayry P, Koprowski H. Phase-I clinical trial of monoclonal antibody in treatment of gastrointestinal tumours. Lancet. 1982;1:762–765. doi: 10.1016/s0140-6736(82)91811-6. [DOI] [PubMed] [Google Scholar]
- Songun I, Litvinov SV, Van de velde CJ, Pals ST, Hermans J, Van krieken JH. Loss of Ep-CAM (CO17-1A) expression predicts survival in patients with gastric cancer. Br J Cancer. 2005;92:1767–1772. doi: 10.1038/sj.bjc.6602519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spizzo G, Fong D, Wurm M, Ensinger C, Obrist P, Hofer C, Mazzoleni G, Gastl G, Went P. EpCAM expression in primary tumour tissues and metastases: an immunohistochemical analysis. J Clin Pathol. 2011;64:415–420. doi: 10.1136/jcp.2011.090274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spizzo G, Obrist P, Ensinger C, Theurl I, Dunser M, Ramoni A, Gunsilius E, Eibl G, Mikuz G, Gastl G. Prognostic significance of Ep-CAM AND Her-2/neu overexpression in invasive breast cancer. Int J Cancer. 2002;98:883–888. doi: 10.1002/ijc.10270. [DOI] [PubMed] [Google Scholar]
- Spizzo G, Went P, Dirnhofer S, Obrist P, Moch H, Baeuerle PA, Mueller-Holzner E, Marth C, Gastl G, Zeimet AG. Overexpression of epithelial cell adhesion molecule (Ep-CAM) is an independent prognostic marker for reduced survival of patients with epithelial ovarian cancer. Gynecol Oncol. 2006;103:483–488. doi: 10.1016/j.ygyno.2006.03.035. [DOI] [PubMed] [Google Scholar]
- Spizzo G, Went P, Dirnhofer S, Obrist P, Simon R, Spichtin H, Maurer R, Metzger U, Von castelberg B, Bart R, Stopatschinskaya S, Kochli OR, Haas P, Mross F, Zuber M, Dietrich H, Bischoff S, Mirlacher M, Sauter G, Gastl G. High Ep-CAM expression is associated with poor prognosis in node-positive breast cancer. Breast Cancer Res Treat. 2004;86:207–213. doi: 10.1023/B:BREA.0000036787.59816.01. [DOI] [PubMed] [Google Scholar]
- Tai KY, Shiah SG, Shieh YS, Kao YR, Chi CY, Huang E, Lee HS, Chang LC, Yang PC, Wu CW. DNA methylation and histone modification regulate silencing of epithelial cell adhesion molecule for tumor invasion and progression. Oncogene. 2007;26:3989–3997. doi: 10.1038/sj.onc.1210176. [DOI] [PubMed] [Google Scholar]
- Tandon AK, Clark GM, Chamness GC, Mcguire WL. Association of the 323/A3 surface glycoprotein with tumor characteristics and behavior in human breast cancer. Cancer Res. 1990;50:3317–3321. [PubMed] [Google Scholar]
- Tapia C, Zlobec I, Schneider S, Kilic E, Guth U, Bubendorf L, Kim S. Deletion of the inhibitor of growth 4 (ING4) tumor suppressor gene is prevalent in human epidermal growth factor 2 (HER2)-positive breast cancer. Hum Pathol. 2011;42:983–990. doi: 10.1016/j.humpath.2010.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Gun BT, Melchers LJ, Ruiters MH, De leij LF, Mclaughlin PM, Rots MG. EpCAM in carcinogenesis: the good, the bad or the ugly. Carcinogenesis. 2010;31:1913–1921. doi: 10.1093/carcin/bgq187. [DOI] [PubMed] [Google Scholar]
- Went P, Vasei M, Bubendorf L, Terracciano L, Tornillo L, Riede U, Kononen J, Simon R, Sauter G, Baeuerle PA. Frequent high-level expression of the immunotherapeutic target Ep-CAM in colon, stomach, prostate and lung cancers. Br J Cancer. 2006;94:128–135. doi: 10.1038/sj.bjc.6602924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Went PT, Lugli A, Meier S, Bundi M, Mirlacher M, Sauter G, Dirnhofer S. Frequent EpCam protein expression in human carcinomas. Hum Pathol. 2004;35:122–128. doi: 10.1016/j.humpath.2003.08.026. [DOI] [PubMed] [Google Scholar]