Abstract
The World Health Organization has promoted health impact assessment (HIA) for over 20 years. At the 2012 United Nations Conference on Sustainable Development (Rio+20), HIA was discussed as a critical method for linking health to “green economy” and “institutional framework” strategies for sustainable development. In countries having a high human development index (HDI), HIA has been added to the overall assessment suite that typically includes potential environmental and social impacts, but it is rarely required as part of the environmental and social impact assessment for large development projects. When they are performed, project-driven HIAs are governed by a combination of project proponent and multilateral lender performance standards rather than host country requirements. Not surprisingly, in low-HDI countries HIA is missing from the programme and policy arena in the absence of an external project driver. Major drivers of global change (e.g. population growth and urbanization, growing pressure on natural resources and climate change) inordinately affect low- and medium-HDI countries; however, in such countries HIA is conspicuously absent. If the cloak of HIA invisibility is to be removed, it must be shown that HIA is useful and beneficial and, hence, an essential component of the 21st century’s sustainable development agenda. We analyse where and how HIA can become fully integrated into the impact assessment suite and argue that the impact of HIA must not remain obscure.
Résumé
L'Organisation mondiale de la Santé encourage l'évaluation de l'impact sanitaire (EIS) depuis plus de 20 ans. Lors de la Conférence des Nations Unies de 2012 sur le développement durable (Rio+20), l'EIS a été discutée comme une méthode essentielle pour lier la santé à «l'économie verte» et aux stratégies du «cadre institutionnel» pour le développement durable. Dans les pays présentant un indice de développement humain élevé (IDH), l'EIS a été ajoutée à la suite de l'évaluation globale qui inclut généralement les impacts environnementaux et sociaux, mais qui est rarement nécessaire dans le cadre de l'évaluation de l'impact environnemental et social des grands projets de développement. Quand elles sont effectuées, les EIS axées sur les projets sont régies par une combinaison de normes de performances multilatérales du prêteur et du promoteur du projet, plutôt que par les exigences du pays d'accueil. Il n'est pas surprenant de constater que, dans les pays à faible IDH, l'EIS ne fait pas partie du programme et de la scène politique en l'absence d'un pilote externe du projet. Les principaux facteurs du changement mondial (comme la croissance démographique et l'urbanisation, la pression croissante sur les ressources naturelles et le changement climatique) affectent démesurément les pays à faible et à moyen IDH. Toutefois, dans ces pays, l'EIS est ostensiblement absente. Si la cape d'invisibilité de l'EIS doit être retirée, on doit prouver que l'EIS est utile et bénéfique, et que c'est donc une composante essentielle du programme du XXIe siècle en matière de développement durable. Nous analysons où et comment l'EIS peut être pleinement intégrée dans la suite de l'évaluation de l'impact et soutenons que l'impact de l'EIS ne doit pas rester dans l'ombre.
Resumen
La Organización Mundial de la Salud ha promovido la evaluación del impacto sanitario (EIS) a lo largo de más de 20 años. En la Conferencia de las Naciones Unidas sobre el Desarrollo Sostenible (Río+20) celebrada en el año 2012, se debatió sobre la EIS como método fundamental para vincular la salud con estrategias para promover una «economía ecológica» y un «marco institucional» para el desarrollo sostenible. En los países con un índice de desarrollo humano (IDH) elevado, la EIS se ha agregado a la evaluación global que normalmente incluye los impactos medioambientales y sociales, pero raramente se requiere como parte de la evaluación del impacto medioambiental y social de proyectos de desarrollo de grandes dimensiones. Cuando estos se llevan a cabo, las EIS impulsadas por proyectos se rigen más por una combinación de los estándares del defensor del proyecto y la función multilateral del prestamista que por los requerimientos del país anfitrión. No sorprende que, en países con un IDH bajo, la EIS no se incluya en los programas y en las estrategias debido a la ausencia de un conductor externo de los proyectos. Los principales factores del cambio global (por ejemplo, el crecimiento demográfico y la urbanización, la creciente presión sobre los recursos naturales y el cambio climático) afectan excesivamente a los países con IDH bajos y medios; sin embargo, en esos países la EIS brilla por su ausencia. Si se desea eliminar la capa de invisibilidad de la EIS, es necesario demostrar que esta última es útil y beneficiosa y, por tanto, un punto esencial de la agenda para el desarrollo sostenible del siglo XXI. Analizamos dónde y cómo podría integrarse plenamente la EIS dentro de las evaluaciones de impactos y opinamos que el impacto de la EIS no debe permanecer oculto.
ملخص
شجعت منظمة الصحة العالمية إجراء تقييم الأثر الصحي (HIA) على مدار ما يزيد عن 20 عاماً. وفي مؤتمر الأمم المتحدة للتنمية المستدامة لعام 2012 (ريو+ 20 )، تمت مناقشة تقييم الأثر الصحي كطريقة حاسمة لربط الصحة "بالاقتصاد الأخضر" واستراتيجيات "الإطار المؤسسي" للتنمية المستدامة. وفي البلدان ذات دليل التنمية البشرية (HDI) المرتفع، تم إضافة تقييم الأثر الصحي إلى نظام التقييم الشامل الذي يشتمل عادة على الآثار البيئية والاجتماعية المحتملة، ولكن نادراً ما يتم الاحتياج إليه كجزء من تقييم الأثر البيئي والاجتماعي لمشاريع التنمية الكبيرة. وعند تنفيذها، تخضع تقييمات الأثر الصحي الناجمة عن المشاريع لتوليفة من مؤيدي المشروعات ومعايير الأداء الخاصة بجهات الإقراض متعددة الأطراف بدلاً من متطلبات البلدان المضيفة. وليس من المدهش، افتقاد تقييم الأثر الصحي في البلدان ذات دليل التنمية البشرية المنخفض من البرنامج والساحة السياسية في غياب دافع خارجي للمشروع. وتؤثر دوافع التغيير العالمي الرئيسية (مثل نمو السكان والتوسع الحضري وزيادة الضغط على الموارد الطبيعية وتغير المناخ) بشكل زائد عن الحد على البلدان ذات دليل التنمية البشرية المنخفض والمتوسط؛ إلا أن هذه البلدان يغيب فيها تقييم الأثر الصحي على نحو واضح. و عند التخلص من ذريعة عدم رؤية تقييم الأثر الصحي، يجب إظهار فائدة تقييم الأثر الصحي وفعاليته، ومن ثم فهو مكون أساسي في جدول أعمال التنمية المستدامة في القرن الحادي والعشرين. ونحن نقوم بتحليل المواضع التي يمكن أن يصبح فيها تقييم الأثر الصحي متكاملاً بشكل تام في نظام تقييم الأثر وطريقة ذلك، ونبرهن على أن تأثير تقييم الأثر الصحي يجب ألا يظل غامضاً.
摘要
20 多年来,世界卫生组织一直在倡导健康影响评估(HIA)。2012 年联合国可持续发展大会(Rio+20)将HIA作为连接健康与可持续发展的“绿色经济”和“制度框架”战略的关键方法加以讨论。人类发展指数(HDI)高的国家已经将HIA加入整体一揽子评估中,这种一揽子评估通常包括潜在的环境和社会影响,但是大型开发项目的环境和社会影响评估很少要求纳入HIA。在执行评估时,由项目驱动的HIA受项目倡导者和多边贷方业绩标准共同支配,而不是主办国需求。在低HDI国家中,如果缺乏外部项目驱动者,计划和政策领域就会遗漏HIA,这种情况并不令人意外。全球变化的主要因素(如人口增长和城市化、日益增长的自然资源压力和气候变化)过度地影响中低水平HDI国家;然而,这些国家中,明显缺乏HIA。如果剥去HIA的隐身外衣,HIA的助益一定会显现出来,因此它是二十一世纪可持续发展日程的主要组成。我们分析在何处以及如何将HIA完全集成到一揽子影响评估中,并主张绝对不能让HIA的影响被掩盖下去。
Резюме
Всемирная организация здравоохранения занималась популяризацией оценки воздействия на здоровье (ОВЗ) на протяжении более 20 лет. В 2012 г. на Конференции Организации Объединенных Наций по устойчивому развитию («Рио +20») состоялось обсуждение ОВЗ как исключительно важного метода для установления связи здоровья с «зеленой экономикой» и «институциональными рамочными» стратегиями устойчивого развития. В странах с высоким индексом развития человеческого потенциала (ИРЧП) ОВЗ была добавлена в состав комплексной оценки, которая обычно включает в себя оценки потенциальных экологических и социальных последствий, но ОВЗ редко в обязательном порядке входит в оценку экологического и социального воздействия в рамках крупных проектов развития. При реализации подобных проектов решающее значение в оценках воздействия на здоровье для целей конкретного проекта имеет сочетание стандартов деятельности инициатора проекта и многосторонних кредиторов, а не требования принимающей страны. Не удивительно, что в странах с низким ИРЧП ОВЗ отсутствует в программах и на политической арене, если нет стимула в виде внешнего проекта. Основные движущие силы глобальных изменений (например, рост населения и урбанизация, более интенсивная эксплуатация природных ресурсов и изменение климата) сильно влияют и на страны с низким и средним ИРЧП, однако очевидно, что в таких странах ОВЗ не проводится. Если все-таки нужно привлечь внимание к ОВЗ, которого ей пока недостает, следует продемонстрировать, что ОВЗ является полезной и выгодной, и, следовательно, представляет собой важную составляющую устойчивого развития в XXI веке. Мы проводим анализ того, где и как ОВЗ может быть полностью интегрирована в комплексную оценку воздействия, и приводим доводы в пользу того, что эффект ОВЗ не должен оставаться в тени.
Introduction
At the first International Conference on Health Promotion, held in Ottawa in 1986, it was stated that “systematic assessment of the health impact of a rapidly changing environment – particularly in areas of technology, work, energy production and urbanization – is essential and must be followed by action to ensure positive benefit to the health of the public”.1 A quarter century later, this assertion is still true but health impact assessment (HIA) is seldom implemented, particularly in a developing country context. Nonetheless, the public and the private sector appreciate the value of evidence and health indicators for informed decision-making and health promotion, regardless of a given country’s human development index (HDI).2 Appropriately, the World Health Organization (WHO) has encouraged HIA as an important method for maximizing health promotion at the local, national and international levels.3 Lee et al., in the March 2007 issue of this journal, elaborated on the role of HIA in bridging the relationship between health and foreign policy by drawing the attention of decision-makers to relevant health issues and generating new evidence.4 Raising the profile of “health” is an important step towards holding governments, multilateral bodies and transnational corporations accountable for the potential health impacts of their policies and practices.5 More recently, WHO presented HIA as a key approach for linking health to “green economy” and “institutional framework” strategies designed to put health at the heart of the agenda of the 2012 United Nations Conference on Sustainable Development (Rio+20).
We have performed HIA in a host of settings, particularly for projects in low-HDI countries, and we have observed that a concerted effort is needed to fully link HIA to the sustainable development agenda of the 21st century.6 Population growth and urbanization, growing pressure on natural resources and global climate change are rapidly moving to centre stage and HIA is often conspicuously absent. Here, we summarize current HIA practice and outline the potential of HIA to become a critical player with the major drivers of global change.
Health impact assessment
WHO defines HIA as “a combination of procedures, methods, and tools by which a policy, programme, or project may be judged as to its potential effects on the health of a population, and the distribution of those effects within the population”.7 HIA is used to assess the likely effect of a policy, programme or project in a specific situation by drawing on the available evidence.2 HIA engages different stakeholders, such as project proponents and affected populations.8 It raises awareness among decision-makers that their actions can undermine health. Thus, HIA emphasizes the need for them to consider effects on health in all subsequent deliberations.9 Finally, HIA serves as a tool to highlight interdependencies between different types of impact assessment (environmental, social and human rights) and among key stakeholders, for the purpose of strengthening collaboration towards health promotion and development.3
Current practice
HIA has grown and diversified over the past two decades to the extent that a considerable spectrum of HIA practice now exists internationally.10 Several countries have established HIA practice as stand-alone processes (e.g. the United Kingdom of Great Britain and Northern Ireland), while others have integrated the assessment of health impacts into existing environmental and social assessment frameworks (e.g. Brazil).11,12 At the national level, legislative approaches that support (e.g. United States of America) or require (e.g. Thailand) HIA are in place.13 Other countries currently rely on voluntary processes with various degrees of government support and resources.14,15 International financial institutions (e.g. Equator Principles Financial Institutions [EPFIs], the World Bank Group and the Asian Development Bank) are critical actors.16 The Performance Standards of the International Finance Corporation (IFC, a member of the World Bank Group), which include a community health standard, are internationally recognized and guide the impact assessment performance for large development projects.17 As part of loan covenants, IFC and EPFIs incorporate standards on social and environmental performance and reporting. Table 1 provides an overview of voluntary and regulatory approaches to HIA, stratified by geographical level (i.e. national or international), that entail different degrees of accountability. However, HIA practice still varies considerably at the subnational level, as exemplified by Australia.18 Hence, the only constant feature is change and local idiosyncrasies are inevitable.
Table 1. Voluntary and regulatory approaches to health impact assessment (HIA) at the national, subnational and international levels.
| Level | Voluntary approaches | Regulatory approaches |
|---|---|---|
| National or subnational | Countries having policies that support HIA but do not require it: – many European countries – United States of America (through the NEPA) – increasing number of Asian countries (e.g. China and Mongolia) |
Different types of legislations and requirements at national or subnational level: – certain states of Australia (e.g. Tasmania and Victoria), Canada and New Zealand – some Asian countries (e.g. Lao People's Democratic Republic, the Philippines, Republic of Korea, Thailand and Viet Nam) |
| International | International institutions recommending HIA as an important approach for health promotion: – WHO – Regional development banks (e.g. ADB) – European Union – ICMM – IPIECA |
Requirement that human health be considered according to IFC performance standard 4: – loan agreement with IFC – loan agreement with EPFIs (77 adopting finance institutions as of August 2012) |
ADB, Asian Development Bank; EPFIs, Equator Principles Financial Institutions; HIA, health impact assessment; ICMM, International Council on Minerals and Metals; IFC, International Finance Corporation; IPIECA, International Petroleum Industry Environmental Conservation Association; NEPA, National Environmental Policy Act; WHO, World Health Organization.
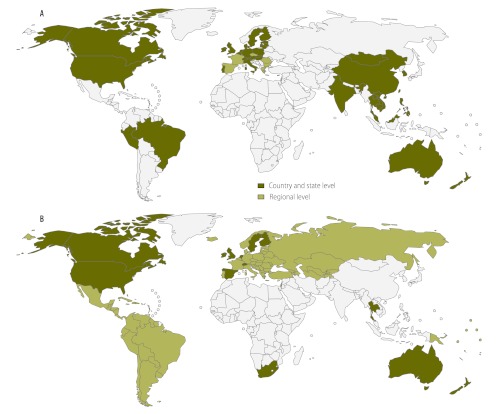
Although HIA is now common practice in most countries with a high HDI, this is not the case in low- and medium-HDI countries (Fig. 1).19 Moreover, in contrast to high-HDI countries where HIA is mostly undertaken by the public sector, low-HDI countries conduct HIA primarily on large development projects.13 This is because in places where no national HIA policy is in place, only best practice principles linked to financing projects and internal company standards apply.16 Hence, from a quantitative and qualitative perspective, there is a divide in HIA practice between high- and low-HDI countries. This has important ramifications affecting current and future global challenges, including protecting health.
Fig. 1.
Countries, states and regions that (A) are actively promoting health impact assessment (HIA) through a policy, regulation or other means of endorsement and (B) have produced guidelines on HIA
Fig. 1 (B) adapted from Hebert et al.19 and information obtained from WHO Regional Offices.
Global challenges
When discussing global challenges, it is important to consider the different health contexts that exist in high- and low-HDI countries. For example, the burden of disease per capita in low-income countries is approximately three times higher than in high-income countries.20 Moreover, high-HDI countries are mainly burdened by non-communicable diseases (NCDs), whereas in many low-HDI countries communicable diseases are still predominant, although patterns are changing rapidly.21 Indeed, in the developing world, a rapid upsurge in the burden of NCDs, including diabetes, hypertension and obesity, is occurring, particularly in urban areas. This is leading to a double burden of diseases, with high infectious disease rates in rural settings and rising NCD rates in urban areas.22 There is also a considerable divide between high- and low-HDI countries in how the three major drivers of global change, described in the following sections, can affect health.
Population growth and urbanization
In October 2011, the world’s population reached 7 billion. It will have exceeded 9 billion by 2050, according to predictions.23 This projected population rise – from 5.7 billion in 2011 to 8.0 billion in 2050 – will primarily occur in developing countries. Population growth is accompanied by an ever-growing fraction of urban dwellers. In 2009, for the first time in human history, more than half of the world’s population lived in urban settings, and by 2050 the world’s urban population is expected to reach 6.3 billion – or nearly twice what it was in 2011, at 3.6 billion.24 This urban growth will occur mainly in low- and medium-HDI regions. In Africa, the urban population is likely to triple. This exponential urban growth will have profound implications for health: (i) urbanization will put major pressure on access to safe drinking water, sewerage systems and solid waste management, and this, in turn, will increase the transmission of diseases acquired through contact with contaminated water, soil and waste; (ii) the urban environment commonly results in changes in human behaviour that affect the burden of NCDs and road traffic-related injuries; (iii) high population density increases exposure to tuberculosis, measles, influenza and sexually transmitted infections; (iv) when cities grow, vector ecology is changed, and this alters existing vector-related diseases or introduces new ones; (v) more people will be exposed to air and noise pollution; and (vi) socioeconomic disparities and health inequalities may become accentuated in urban centres and this will result in overt social and political conflicts.25–27
Growing pressure on natural resources
A growing world population, coupled with economic growth, will put additional strains on existing mineral and energy resources, with many of the remaining large deposits located in remote tropical areas. It has been estimated that due to construction activities, technology and increased wealth – particularly in low- and medium-HDI countries – the overall volume of metal flowing into use in 2050 will be five to ten times higher than today.28 Similarly, the world’s marketed energy consumption is estimated to increase by 53% from 2008 to 2035, and the total energy demand will increase by more than 80% in the Asian Pacific region, Latin America and sub-Saharan Africa.29 Although the global energy supply will continue to be filled by fossil fuels, renewable energy sources and green economy strategies are gaining traction.30
Moreover, geographical and climatic conditions in tropical regions are favourable for the production of hydroelectric and solar power, as well as fertile land for biofuel production. The development and management of these natural resources will be key to social and economic development in most low- and medium-HDI countries. However, large development projects, if not properly managed, can undermine the health of local populations by depleting ecosystems and the services that these provide to mankind.31,32 Impact mitigation strategies should thus form an integral part of project developments in tropical and subtropical zones.33 The Nam Theun 2 hydroelectric project in the Lao People's Democratic Republic is an important example of mitigation strategies implemented over time and with ongoing surveillance.34,35
Global climate change
Observational evidence from all continents and most oceans shows that many natural systems are being affected by regional and global climate change. This is likely to affect the health of millions of people, particularly in low-HDI countries.36 Documented and anticipated health effects include, among others: (i) increasing levels of malnutrition and related disorders; (ii) alteration in the distribution of diseases transmitted by insect vectors and intermediate host snails; (iii) increasing burden of diarrhoeal and respiratory diseases; (iv) increased frequency of cardiorespiratory diseases due to higher concentrations of critical pollutants such as ozone, and fine particulate matter (PM2.5); and (v) higher mortality rates due to floods, storms, heat waves, droughts and fires.37 One commonly anticipated impact of climate change is population displacement. Indeed, by 2050, between 200 million and 1 billion people may be displaced because of climate change.27,38 Bronen presents an illuminating case study of climate-induced relocation and mitigation in the Arctic (Alaska), a place where HIA is currently undergoing considerable development.39
Variation in these outcomes is evident by geographic region and socioeconomic status. Regions already experiencing the highest increase in diseases attributable to the rise in temperature over the past 30 years are inhabited by populations that bear the least responsibility for the greenhouse gas warming of the planet. This represents the largest health inequity of our time.40 A major challenge is to increase the effective capacity of most vulnerable countries to assess the potential impacts of global climate change in their specific contexts and to be able to translate the evidence into equitable public health programmes and policies. This requires comprehensive, yet flexible, transparent and integrated assessment methods that are able to: (i) systematically identify and quantify the many pathways through which climate change can affect health in different social and ecological contexts; (ii) cope with the uncertainties surrounding predictions on global warming; (iii) consider health equity, which is clearly part of the climate change challenge; and (iv) consider the full range of policy options for mitigating adverse health impacts as well as enhancing potential co-benefits from more upstream mitigation of greenhouse gas emissions.41–43
Tapping the potential
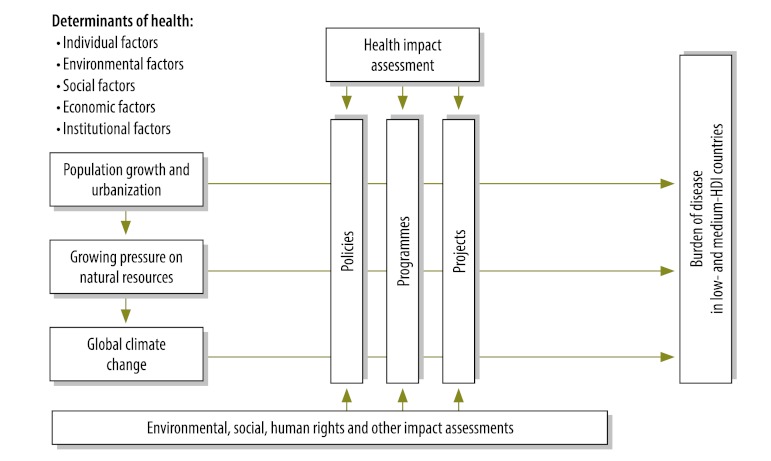
Low- and medium-HDI countries are particularly vulnerable to the major drivers of global change. Hence, existing policies and programmes should be modified and new ones developed in various sectors. As an integral part of the suite of impact assessments, HIA can contribute to raising awareness among decision-makers of the link between health and other factors so that they consider health effects in the planning of policies, programmes and projects (Fig. 2). This is supported by a broad set of examples of HIA in the context of urban planning, infrastructural development and policy development.44 In addition, for global climate change-related policy-making, the application of an HIA framework has been proposed.42 In practice, Spickett et al. employed HIA for addressing the potential health impacts of climate change in western Australia.45 They found that HIA, applied periodically, is an ideal tool for developing appropriate strategies for adapting to climate change. Such strategies can be used by the government for future decision-making. In western Africa, HIA, combined with vulnerability and adaptive capacity assessment methods, was conducted as part of an “EcoHealth” project for adaptation to climate change in riverine medium-sized towns.46 However, existing HIA practice falls short of what is required to meet the current and anticipated health challenges facing low- and medium-HDI countries. Yet, this leads to the question of how HIA practice can be promoted where it is most needed.
Fig. 2.
Health impact assessment as a decision-making tool for policies, programmes and projects designed to mitigate the adverse health effects from major drivers of global change
HDI, human development index.
A natural point of entry for HIA in the context of global challenges is during the planning process for climate-induced resettlements and the implementation of recommended mitigation strategies. In the example of Alaska mentioned above, HIA is only implicit, but many of the steps that would comprise an HIA were embedded in the comprehensive community planning process.39 Indeed, the embedding of HIA in the overall process of climate-induced resettlement is what puts the key health issues in front of the policy-makers who directly influence the implementation of plans.
Promoting health impact assessment
The following components were identified as cornerstones for the promotion and strengthening of HIA practice: (i) existing policy frameworks and procedures, including legislation and law; (ii) capacity-building mechanisms for HIA; (iii) institutional infrastructure; and (iv) intersectoral collaboration.15,47 With sustained efforts on these parameters, the Asian region has successfully promoted HIA practice over the past few years (Fig. 1).48 In the African region, however, all of these components are still largely non-existent at the national and regional levels. Consequently, the promotion of HIA practice is primarily dependent on voluntary corporate action and requirements for international financial institutions imposed by the EPFI and IFC.
Although these efforts are valuable contributions to the promotion of sustainable projects, they have major limitations. First, the performance standards put forth by the IFC and EPFIs only apply to those projects that depend on financing from these institutions. This is critical in a competitive environment such as the extractive industry, in which adherence to sustainable principles may impose an economic handicap.16 Second, all of these efforts are based on current best practices, which are not a substitute for legal requirements. The example of the European Union shows that HIA not being mandatory seriously hinders the ability to fully tap its potential for promoting public health.14,49 Third, the provision of performance standards and guidance on HIA alone is not sufficient for the execution of HIA on the ground. Human capacities, as well as specific tools that are adapted to the context of a given proposal, are still needed.8,50 Fourth, the current international standards in practice focus heavily on natural resource extraction and management, which appears reasonable in light of the strong global demand for hydroelectric power, water and other natural resources.28,29 However, in view of predictions regarding population development and climate change, it will be crucially important that HIA practice go beyond the hydroelectric power and extractive industry private sector and become common practice also in the public sector. Moreover, even if international enforcement mechanisms prove effective, there is a worrying imbalance, since the current human and technical capacity for conducting HIA in low- and medium-HDI countries is not enough to cope with the demand for HIA practice created by international institutions, let alone the demand in the public sector at the national and regional levels.
The mechanisms in place for the promotion of HIA in low-HDI countries have limitations, as we have seen, and their success is jeopardized by the current lack of trained health impact assessors. To further promote HIA practice in the developing world in general, and in the African region in particular, there is a need for capacity-building. WHO is uniquely positioned to take the lead in this process, ideally in close collaboration with the HIA community (e.g. practitioners and academics). Central to the HIA training activity is the need to develop programmes in schools of public health with a major component on human resource development. This offers an opportunity to fill what is currently an important educational and human resource gap.
The World Health Organization’s role
With the establishment by WHO’s Western Pacific Regional Office of a thematic working group for HIA, a body of more than 1000 HIA practitioners was formed across the Asian region.48 Such a leading institution is what is missing for the African Region to make a start in the development and promotion of HIA capacities. Hence, we propose that WHO initiates the establishment of a regional competence centre in HIA as a priority for the African Region. In a first step, awareness of, and interest in, HIA as an approach for health promotion should be fostered. This will trigger demand for HIA at the national and regional levels and thus create a dynamic for strengthening HIA practice. However, true interest is more often built on practical examples than on theoretical frameworks. To date, the promotion of HIA in the developing world is constrained by the small number of available references of best practice that can be used as benchmarks for future HIA.44 For instance, WHO’s web site has very few examples of HIA deriving from low- and medium-HDI countries. Hence, the available evidence base for the value and practicability of HIA in tropical regions is small. Experience gained in HIA practice in high-income countries is rarely directly applicable to a low- or middle-income country context. As a result, WHO’s primary mission, to create interest in HIA, is hindered by considerable weaknesses in the evidence on the benefits, pitfalls and practicability of HIA in low- and medium-HDI countries.
Research and practice
According to a growing body of HIA guidance, interdisciplinary, multi-method approaches are required for appraising the broad range of policies, programmes and projects that can affect health.19 However, independent of whether the guidance documents were developed specifically for industrialized countries or for more global application, they were almost uniquely developed by people from high-HDI countries. Consequently, they are, to a great extent, built on evidence and experience gained in such countries. In view of the differences in context between high- and low-HDI countries, which are unambiguously reflected by the burden of disease and major risk factors, this is critical.21 For example, an HIA methodology that is based on the social determinants of health model has its limitations in the context of HIA for large development projects in a tropical country.16 On the other hand, the social determinants of health as a guiding framework for HIA may outgrow the strengths it has in high-HDI countries when applied in the context of urbanization or policy planning in low- and medium-HDI countries.25
These examples highlight that the HIA community does not only have to scrutinize and amplify the methods at hand, but also become more clear about which methods make sense in what environment and for what purpose. However, ideally this should only be done on the ground and, importantly, in collaboration with local HIA practitioners. We therefore propose that the primary goal set by the HIA community be to advocate and expedite expertise in HIA that is integrated in governments, the private sector and academia in low- and medium-HDI countries. This requires the active promotion of partnership with local stakeholders by involving them in the entire HIA process. As recognized by WHO, the Rio+20 conference and resulting initiatives offer an opportunity to serve as a platform for turning this proposal into action. Collaboration and mutual learning will help strengthen the evidence base surrounding the value of HIA in low- and medium-HDI countries and also allow these countries to develop their own policy frameworks and procedures for HIA that are adapted to the structure and legislation of local ministries and to their environments and communities.
Conclusion
From a global perspective, HIA is generally still poorly recognized and practiced in most low- and middle-HDI countries. Recently, interest in HIA has increased in parts of the developing world, particularly in south-eastern Asia. Based on best practice principles, major extractive industry projects often have a strong impact assessment requirement. However, local interest and capacity for HIA in low- and middle-HDI countries are still weak. This is a serious constraint in light of the increasing demand for HIA in large development projects, notably stimulated by IFC and EPFIs’ performance standards, and for the institutionalization of HIA in the public sector at the national and regional levels. The latter will become of particular importance if HIA does indeed play a central role in the “green economy” and “institutional framework” sustainability agenda, as promulgated by WHO. Climate change-induced resettlement provides perhaps one of the most obvious contexts in which a direct and immediate link between HIA recommendations and policy implementation is essential.
HIA can no longer remain an invisible item on the international impact assessment stage and one that is rarely acted upon. The invisibility cloak must be removed so that health is seen and fully present in the unfolding 21st century sustainability agenda. HIA is a method that can be applied to a suite of issues, but this is not the same as recognizing that such issues must include a fully integrated health component. If the Rio+20 agenda is to genuinely benefit vulnerable populations, then “health” must be an equal participant and partner at the table.
Acknowledgements
We thank various colleagues from the WHO Regional Offices and elsewhere for their inputs on national and regional mechanism for the promotion and regulation of HIA. MSW is grateful to the Swiss Tropical and Public Health Institute for a post-doctoral fellowship.
Competing interests:
The authors have pursued numerous health impact assessments, including work for the private sector, government agencies, development banks, and multinational organizations, and have served on expert committees for the WHO and other international organizations.
References
- 1.The Ottawa Charter for health promotion Geneva: World Health Organization; 1986. [Google Scholar]
- 2.Mindell J, Biddulph J, Taylor L, Lock K, Boaz A, Joffe M, et al. Improving the use of evidence in health impact assessment. Bull World Health Organ. 2010;88:543–50. doi: 10.2471/BLT.09.068510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bos R. Health impact assessment and health promotion. Bull World Health Organ. 2006;84:914–5. doi: 10.2471/blt.06.030965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee K, Ingram A, Lock K, McInnes C. Bridging health and foreign policy: the role of health impact assessments. Bull World Health Organ. 2007;85:207–11. doi: 10.2471/BLT.06.037077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scott-Samuel A, O'Keefe E. Health impact assessment, human rights and global public policy: a critical appraisal. Bull World Health Organ. 2007;85:212–7. doi: 10.2471/BLT.06.037069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krieger GR, Singer BH, Winkler MS, Divall MJ, Tanner M, Utzinger J. Health impact assessment in developing countries. In: Kemm J, editor. Past achievement, current understanding and future progress in health impact assessment Oxford: Oxford University Press; 2012. pp. 265–76. [Google Scholar]
- 7.European Centre for Health Policy. Health impact assessment: main concepts and suggested approach: Gothenburg consensus paper. Copenhagen: WHO Regional Office for Europe; 1999. [Google Scholar]
- 8.Winkler MS, Krieger GR, Divall MJ, Singer BH, Utzinger J. Health impact assessment of industrial development projects: a spatio-temporal visualization. Geospat Health. 2012;6:299–301. doi: 10.4081/gh.2012.148. [DOI] [PubMed] [Google Scholar]
- 9.Kemm J, Parry J, Palmer S. Health impact assessment: concepts, theory, techniques, and applications Oxford: Oxford University Press; 2004. [Google Scholar]
- 10.Harris-Roxas B, Harris E. Differing forms, differing purposes: a typology of health impact assessment. Environ Impact Assess Rev. 2011;31:396–403. doi: 10.1016/j.eiar.2010.03.003. [DOI] [Google Scholar]
- 11.Vohra S. International perspective on health impact assessment in urban settings. N S W Public Health Bull. 2007;18:152–4. doi: 10.1071/NB07085. [DOI] [PubMed] [Google Scholar]
- 12.Wismar M, Blau J, Ernst K, Figueras J. The effectiveness of health impact assessment: scope and limitations of supporting decision-making in Europe Brussels: European Observatory on Health Systems and Policies; 2007. [Google Scholar]
- 13.Harris-Roxas B, Viliani F, Cave B, Divall MJ, Furu P, Harris P, et al. Health impact assessment: the state of the art. Impact Assess Project Appr. 2012;30:43–52. doi: 10.1080/14615517.2012.666035. [DOI] [Google Scholar]
- 14.Salay R, Lincoln P. Health impact assessment in the European Union. Lancet. 2008;372:860–1. doi: 10.1016/S0140-6736(08)61337-9. [DOI] [PubMed] [Google Scholar]
- 15.National Academy of Sciences. Improving health in the United States: the role of health impact assessment Committee on Health Impact Assessment, Board on Environmental Studies and Toxicology, Division on Earth and Life Studies, National Research Council, editors. Washington: The National Academies Press; 2011. [Google Scholar]
- 16.Krieger GR, Utzinger J, Winkler MS, Divall MJ, Phillips SD, Balge MZ, et al. Barbarians at the gate: storming the Gothenburg consensus. Lancet. 2010;375:2129–31. doi: 10.1016/S0140-6736(10)60591-0. [DOI] [PubMed] [Google Scholar]
- 17.Performance standards Washington: International Finance Corporation; 2012. Available from: http://www.ifc.org/performancestandards [accessed 26 January 2013].
- 18.Harris P, Spickett J. Health impact assessment in Australia: a review and directions for progress. Environ Impact Assess Rev. 2011;31:425–32. doi: 10.1016/j.eiar.2010.03.002. [DOI] [Google Scholar]
- 19.Hebert KA, Wendel AM, Kennedy SK, Dannenberg AL. Health impact assessment: a comparison of 45 local, national, and international guidelines. Environ Impact Assess Rev. 2012;34:74–82. doi: 10.1016/j.eiar.2012.01.003. [DOI] [Google Scholar]
- 20.The global burden of disease: 2004 update Geneva: World Health Organization; 2008. [Google Scholar]
- 21.Murray CJL, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2013;380:2197–223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 22.Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet. 2011;377:557–67. doi: 10.1016/S0140-6736(10)62037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World population prospects: the 2010 revisions New York: United Nations, Department of Economic and Social Affairs; 2011. [Google Scholar]
- 24.World urbanization prospects: the 2011 revisions New York: United Nations, Department of Economic and Social Affairs; 2012. [Google Scholar]
- 25.Marmot M, Friel S, Bell R, Houweling TAJ, Taylor S. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372:1661–9. doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- 26.Alirol E, Getaz L, Stoll B, Chappuis F, Loutan L. Urbanisation and infectious diseases in a globalised world. Lancet Infect Dis. 2011;11:131–41. doi: 10.1016/S1473-3099(10)70223-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Black R, Bennett SRG, Thomas SM, Beddington JR. Migration as adaptation. Nature. 2011;478:447–9. doi: 10.1038/478477a. [DOI] [PubMed] [Google Scholar]
- 28.Graedel TE, Cao J. Metal spectra as indicators of development. Proc Natl Acad Sci USA. 2010;107:20905–10. doi: 10.1073/pnas.1011019107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.International energy outlook 2011 Washington: United States Energy Information Administration; 2011. [Google Scholar]
- 30.Mathiesen BV, Lund H, Karlsson K. 100% Renewable energy systems, climate mitigation and economic growth. Appl Energ. 2011;88:488–501. doi: 10.1016/j.apenergy.2010.03.001. [DOI] [Google Scholar]
- 31.Utzinger J, Wyss K, Moto DD, Yemadji N, Tanner M, Singer BH. Assessing health impacts of the Chad–Cameroon petroleum development and pipeline project: challenges and a way forward. Environ Impact Assess Rev. 2005;25:63–93. doi: 10.1016/j.eiar.2004.04.002. [DOI] [Google Scholar]
- 32.Winkler MS, Divall MJ, Krieger GR, Schmidlin S, Magassouba ML, Knoblauch AM, et al. Assessing health impacts in complex eco-epidemiological settings in the humid tropics: modular baseline health surveys. Environ Impact Assess Rev. 2012;33:15–22. doi: 10.1016/j.eiar.2011.10.003. [DOI] [Google Scholar]
- 33.Singer BH, Castro MC. Bridges to sustainable tropical health. Proc Natl Acad Sci USA. 2007;104:16038–43. doi: 10.1073/pnas.0700900104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Krieger GR, Balge MZ, Chanthaphone S, Tanner M, Singer BH, Fewtrell L et al. Nam Theum 2 hydroelectric project, Lao PDR. In: Fewtrell L, Kay D, editors. Health impact assessment for sustainable water management London: IWA Publishing; 2008. pp. 199–232. [Google Scholar]
- 35.Guerrier G, Paul R, Sananikhom P, Kaul S, Luthi R, Katz J-P, et al. Strategic success for hydropower in Laos. Science. 2011;334:38. doi: 10.1126/science.334.6052.38-a. [DOI] [PubMed] [Google Scholar]
- 36.Intergovernmental Panel on Climate Change. Climate change 2007: impacts, adaptation and vulnerability. Contribution of working group II to the fourth assessment report of the Intergovernmental Panel on Climate Change Cambridge: Cambridge University Press; 2007. [Google Scholar]
- 37.Costello A, Abbas M, Allen A, Ball S, Bell S, Bellamy R, et al. Managing the health effects of climate change. Lancet. 2009;373:1693–733. doi: 10.1016/S0140-6736(09)60935-1. [DOI] [PubMed] [Google Scholar]
- 38.Myers SS, Bernstein A. The coming health crisis. Scientist. 2011;25:32–7. doi: 10.3410/B3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bronen R. Climate-induced community relocations: creating an adaptive governance framework based in human rights doctrine. NYU Rev Law Soc Change. 2011;35:357–407. [Google Scholar]
- 40.Friel S, Marmot M, McMichael AJ, Kjellstrom T, Vagero D. Global health equity and climate stabilisation: a common agenda. Lancet. 2008;372:1677–83. doi: 10.1016/S0140-6736(08)61692-X. [DOI] [PubMed] [Google Scholar]
- 41.McMichael C, Barnett J, McMichael AJ. An ill wind? Climate change, migration, and health. Environ Health Perspect. 2012;120:646–54. doi: 10.1289/ehp.1104375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Patz J, Campbell-Lendrum D, Gibbs H, Woodruff R. Health impact assessment of global climate change: expanding on comparative risk assessment approaches for policy making. Annu Rev Public Health. 2008;29:27–39. doi: 10.1146/annurev.publhealth.29.020907.090750. [DOI] [PubMed] [Google Scholar]
- 43.Wardekker JA, de Jong A, van Bree L, Turkenburg WC, van der Sluijs JP. Health risks of climate change: an assessment of uncertainties and its implications for adaptation policies. Environ Health. 2012;11:67. doi: 10.1186/1476-069X-11-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Erlanger TE, Krieger GR, Singer BH, Utzinger J. The 6/94 gap in health impact assessment. Environ Impact Assess Rev. 2008;28:349–58. doi: 10.1016/j.eiar.2007.07.003. [DOI] [Google Scholar]
- 45.Spickett JT, Brown HL, Katscherian D. Adaptation strategies for health impacts of climate change in western Australia: application of a health impact assessment framework. Environ Impact Assess Rev. 2011;31:297–300. doi: 10.1016/j.eiar.2010.07.001. [DOI] [Google Scholar]
- 46.Cissé G, Koné B, Bâ H, Mbaye I, Koba K, Utzinger J et al. Ecohealth and climate change: adaptation to flooding events in riverside secondary cities, West Africa. In: Otto-Zimmermann K, editor. Resilient cities: cities and adaptation to climate change – Proceedings of the Global Forum 2010 New York: Springer; 2011. pp. 55–67. [Google Scholar]
- 47.Caussy D, Kumar P, Sein UT. Health impact assessment needs in south-east Asian countries. Bull World Health Organ. 2003;81:439–43. [PMC free article] [PubMed] [Google Scholar]
- 48.Harris-Roxas B. Health impact assessment in the Asia Pacific. Environ Impact Assess Rev. 2011;31:393–5. doi: 10.1016/j.eiar.2010.10.001. [DOI] [Google Scholar]
- 49.Tarkowski S, Ricciardi W. Health impact assessment in Europe: current dilemmas and challenges. Eur J Public Health. 2012;22:612. doi: 10.1093/eurpub/cks120. [DOI] [PubMed] [Google Scholar]
- 50.Krieger GR, Bouchard MA, Marques de Sa I, Paris I, Balge Z, Williams D, et al. Enhancing impact: visualization of an integrated impact assessment strategy. Geospat Health. 2012;6:303–6. doi: 10.4081/gh.2012.149. [DOI] [PubMed] [Google Scholar]