Abstract
Humanitarian emergencies result in a breakdown of critical health-care services and often make vulnerable communities dependent on external agencies for care. In resource-constrained settings, this may occur against a backdrop of extreme poverty, malnutrition, insecurity, low literacy and poor infrastructure. Under these circumstances, providing food, water and shelter and limiting communicable disease outbreaks become primary concerns. Where effective and safe vaccines are available to mitigate the risk of disease outbreaks, their potential deployment is a key consideration in meeting emergency health needs. Ethical considerations are crucial when deciding on vaccine deployment. Allocation of vaccines in short supply, target groups, delivery strategies, surveillance and research during acute humanitarian emergencies all involve ethical considerations that often arise from the tension between individual and common good. The authors lay out the ethical issues that policy-makers need to bear in mind when considering the deployment of mass vaccination during humanitarian emergencies, including beneficence (duty of care and the rule of rescue), non-maleficence, autonomy and consent, and distributive and procedural justice.
Résumé
Les urgences humanitaires entraînent une rupture des services de soins de santé essentiels et elles rendent souvent les communautés vulnérables dépendantes des organismes externes pour leurs soins. Dans les milieux où les ressources sont comptées, cela peut se produire sur fond d'extrême pauvreté, de malnutrition, d’insécurité, de faible niveau d'alphabétisation et d’infrastructures insuffisantes. Dans ces circonstances, fournir nourriture, eau et abri, tout en limitant les épidémies de maladies transmissibles, devient une préoccupation centrale. Lorsqu'il existe des vaccins sûrs et efficaces pour limiter les risques d'épidémies, leur éventuel déploiement est un facteur clé pour satisfaire les besoins sanitaires d'urgence. Les considérations éthiques sont essentielles pour se prononcer sur le déploiement de la vaccination. La distribution de vaccins en quantités limitées, les groupes cibles, les stratégies de vaccination, la surveillance et la recherche lors de situations d'urgence humanitaire graves impliquent tous des considérations éthiques souvent nées de la tension entre le bien individuel et le bien commun. Les auteurs exposent les questions éthiques que les décideurs doivent garder à l'esprit lorsqu'ils envisagent le déploiement d’une vaccination de masse pendant les urgences humanitaires, notamment la bénéficience (devoir de diligence et devoir d’assistance), la non-maléficience, l’autonomie et le consentement, ainsi que la justice de répartition et l’équité procédurale.
Resumen
Las emergencias humanitarias causan el desplome de los servicios de atención de salud esenciales y, a menudo, provocan que la atención sanitaria de las comunidades vulnerables pase a depender de organismos externos. En entornos con recursos limitados esto puede darse en un contexto de pobreza extrema, desnutrición, inseguridad, bajos niveles de alfabetización e infraestructuras deficientes. Bajo estas circunstancias, suministrar alimentos, agua y refugio, así como limitar la aparición de brotes de enfermedades transmisibles representan las principales preocupaciones. Cuando se dispone de vacunas eficaces y seguras para reducir el riesgo de aparición de brotes de enfermedades, la distribución potencial de las mismas constituye un factor clave en las situaciones de emergencia sanitaria. Las consideraciones éticas son fundamentales a la hora de decidir sobre la distribución de las vacunas. La asignación de vacunas con suministro limitado, los grupos destinatarios de las mismas, las estrategias de entrega, así como la monitorización y los estudios durante las emergencias humanitarias graves implican consideraciones éticas que, a menudo, derivan de un enfrentamiento entre el beneficio individual y el bien común. Los autores exponen los problemas éticos que los responsables políticos deben tener en cuenta a la hora de considerar cómo distribuir la vacunación masiva durante las emergencias humanitarias, lo cual incluye principios como la beneficencia (el deber de atención y la regla del rescate), la no maleficencia, la autonomía y el consentimiento, así como la justicia distributiva y procesal.
ملخص
تؤدي حالات الطوارئ الإنسانية إلى تعطل خدمات الرعاية الصحية الحرجة، وغالباً ما تؤدي إلى اعتماد المجتمعات المستضعفة على الوكالات الخارجية للحصول على الرعاية. وقد يحدث هذا في البيئات محدودة الموارد في سياق الفقر المدقع وسوء التغذية وعدم استتباب الأمن وقلة الإلمام بالقراءة والكتابة وسوء البنية التحتية. وفي ظل هذه الظروف، يصبح توفير الغذاء والماء والمأوى والحد من فاشيات الأمراض السارية شواغل أساسية. وعندما تتوافر اللقاحات المأمونة والفعالة للتخفيف من مخاطر فاشيات الأمراض، يصبح النشر المحتمل لها من الاعتبارات الرئيسية في تلبية الاحتياجات الصحية الطارئة. كما تعد الاعتبارات الأخلاقية عاملاً حاسماً عند البت في نشر اللقاحات. وينطوي تخصيص اللقاحات بكمية غير كافية والفئات المستهدفة واستراتيجيات الإيتاء والترصد والبحث أثناء حالات الطوارئ الإنسانية الحادة على اعتبارات أخلاقية غالباً ما تنشأ عن التوتر بين المصلحة الفردية والمصلحة العامة. ويحدد المؤلفون المسائل الأخلاقية التي يتعين على صناع السياسة وضعها في الاعتبار عند التفكير في نشر حملات التطعيم الجماعية أثناء حالات الطوارئ الإنسانية، بما في ذلك عمل الخير (واجب الرعاية وقاعدة الإنقاذ) وعدم الإيذاء والاستقلال والموافقة والعدالة التوزيعية والإجرائية.
摘要
人道主义紧急事件引发关键的医疗保健服务崩溃?往往使弱势群体依赖于外部医疗机构。在资源有限的环境中?这种情况可能在极端贫困、营养不良、不安全、文化水平低和基础设施差的背景下发生。在这种情况下?提供食物、水和住所并限制传染病爆发成为首当其冲的问题。如果可以提供安全有效的疫苗来减少疾病爆发的风险?则其潜在的部署就是满足紧急医疗需求的重要考虑因素。决定部署疫苗时道德的考虑因素至关重要。在严重的人道主义紧急事件中分配供应短缺的疫苗、设定目标群体、制定战略、监测和研究都涉及道德方面的考虑?而这些问题往往源于个人和共同利益之间的紧张关系。作者阐述了在人道主义紧急事件中在考虑部署大规模疫苗接种时政策制定者需要牢记的道德问题?包括有利?谨慎责任和救援规则?、无害原则、自治和自愿以及分配与程序正义。
Резюме
Гуманитарные чрезвычайные ситуации приводят к прекращению оказания крайне важных медицинских услуг и часто обуславливают зависимость уязвимых сообществ от внешних организаций, занимающихся вопросами здравоохранения. В условиях ограниченности ресурсов это может происходить на фоне крайней нищеты, недоедания, отсутствия безопасности, низкого уровня грамотности и плохой инфраструктуры. В таких обстоятельствах самой актуальной проблемой становится предоставление продовольствия, воды, крова и ограничение вспышек болезней. При наличии эффективных и безопасных вакцин, снижающих риск вспышек заболеваний, их потенциальное применение является ключевым фактором в удовлетворении потребностей в неотложной медицинской помощи. Этические соображения имеют решающее значение при принятии решения о применении вакцины. Распределение дефицитных вакцин, выбор целевых групп, стратегия, наблюдение и исследования в критических гуманитарных чрезвычайных ситуациях — все это неразрывно связано с этическими соображениями, которые часто возникают из-за противоречий между интересами отдельного лица и общим благом. Авторы излагают этические аспекты, которые следует учитывать лицам, ответственным за принятие решений, при рассмотрении вопроса о применении массовой вакцинации в чрезвычайных гуманитарных ситуациях. К числу таких аспектов относятся милосердие (обязанность заботиться и правило спасения), принцип «не навреди», независимость и согласие, а также справедливость в распределении и процедурных вопросах.
Introduction
Acute humanitarian crises pose complex ethical dilemmas for policy-makers, particularly in settings with inadequate health-care services, which often become dependent on external agencies for urgently needed care.1 These ethical dilemmas are inherent in many spheres of the response activity, including measures to mitigate infectious disease transmission, which often cause outbreaks during humanitarian crises. In the initial emergency response, interventions to reduce communicable disease transmission, such as vaccination, should be deployed along with food, water and shelter, since communicable diseases, including some that are vaccine-preventable, can spread faster and be unusually severe in the crowded, unhygienic conditions that prevail during crises. Measles, with a case-fatality rate as high as 30% during a humanitarian crisis, is a fitting example.2
Several factors need to be considered before a vaccine is deployed: the potential burden of disease; vaccine-related risks (usually minimal); the desirability of prevention as opposed to treatment; the duration of the protection conferred; cost; herd immunity in addition to individual protection; and the logistical feasibility of a large-scale vaccination programme. Vaccination may be the only practical way to protect people against certain diseases, such as meningococcal meningitis and measles. Individuals who undergo medical or surgical treatment often need ongoing care; those who get vaccinated do not, yet they receive long-lasting benefits. However, the feasibility of a mass vaccination effort depends largely on available resources.
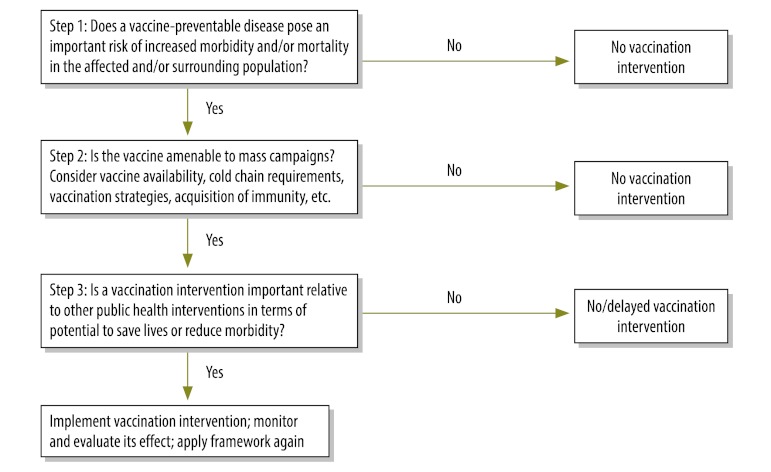
In a recent study on ethics in humanitarian health care, respondents pointed out the need for ethical guidance on issues such as vaccination during emergency situations.3 The World Health Organization (WHO) and several humanitarian nongovernmental organizations have acknowledged this need and, in an effort to address it, WHO’s Strategic Advisory Group of Experts (SAGE) on Immunization developed a framework for decision-makers on the deployment and effective use of vaccines that can save lives during emergencies.4,5 Under the framework, countries facing crises first assess the epidemiological risk posed by a potentially dangerous vaccine-preventable disease. They then explore the feasibility of a mass vaccination campaign in light of the properties of the necessary vaccine (Fig. 1).
Fig. 1.
Algorithm for making decisions surrounding vaccine deployment during acute humanitarian emergencies
The conflict between individual good and the common good is at the core of the ethical issues explored in this paper – issues pertaining to the allocation of a limited vaccine supply, the balance between benefits and harms, obtaining informed consent and research conduct. The key ethical principles that should prevail during public health emergencies are rooted in the more general ethical principles governing clinical medicine and public health. Acute humanitarian emergencies differ widely in nature, in the threats they pose, in the background conditions in which they occur, and in the type of agencies that must respond. Hence, this paper does not seek to provide specific, prescriptive guidance, but merely highlights the ethical issues that policy-makers need to consider when deciding to conduct mass vaccination during any emergency response.
Beneficence and human rights
The international community and national governments have a collective duty of care to ensure that effective, affordable measures for preventing unnecessary illness and death are available to those most in need. During humanitarian emergencies, the risk of communicable disease transmission is higher than usual. According to the duty of care based on the principle of beneficence, governments must make vaccines available against the most contagious diseases. In addition to the duty of care, institutions and individuals must abide by the rule of rescue, which is “the imperative […] to rescue identifiable individuals facing avoidable death”.6,7 This is influenced by the urgency of the situation, the consequences of doing nothing, the feasibility of preventing serious consequences and the sacrifice required of the responding individual or agency.8 Humanitarian emergencies occur often enough for timely access to an assured supply of vaccine to be necessary, since certain vaccine-preventable diseases have serious outcomes, including death.9,10 Global and local communities, including governments and nongovernmental organizations, are morally obligated to ensure this supply.
Some oppose vaccination and other measures that are not routinely offered in non-crisis settings. The underlying concern, based on the doctrines of developmental relief and sustainability, is that introducing such measures will result in aid dependency. However, the argument becomes invalid if vaccination during an acute humanitarian crisis can provide immediate protection against serious illness or death.11 A higher standard of care is needed during public health crises because of the immediate threat to life. It is ethically reasonable for the standard of preventive care to revert to pre-existing levels after the heightened threat has subsided. After an acute emergency, some medical interventions call for ongoing care or rehabilitation. Vaccination does not, yet it provides long-lasting benefits.
Humanitarian assistance has traditionally been seen as charity, in keeping with the principle of beneficence, but owing to the growing human rights focus, it has come to be viewed as an obligation. Those who are able to help are obligated to ensure that the rights of affected individuals and populations are respected and promoted.12 The Sphere Project’s Humanitarian Charter “defines the legal responsibilities of states and parties to guarantee the right to assistance and protection”.13 The charter draws on the Universal Declaration of Human Rights, international humanitarian law (the Geneva Conventions) and the Convention relating to the Status of Refugees to establish a legal framework for humanitarian action.14
From a human rights perspective, vaccination equitably promotes and protects public health. Article 25 of the Universal Declaration of Human Rights states that:
“Everyone has the right to a standard of living adequate for the health and well-being of himself and his family, including food, clothing, and medical care ... [and that] every individual and every organ of society …shall strive … by progressive measures, national and international, to secure [its] universal and effective recognition.”15
Irrespective of the principles underlying humanitarian assistance, vaccine donations can ensure timely access to vaccines during emergencies. Although WHO and the United Nations Children’s Fund (UNICEF) have agreed on five requirements for “good donations practice” – i.e. suitability, sustainability, informed key persons, supply and licensing – they acknowledge that in exceptional circumstances, including emergencies, these requirements can be overlooked.16
Non-maleficence
All decisions made during humanitarian crises involve seeking a balance between beneficence (doing good) and non-maleficence (avoiding or minimizing harm). Only vaccines that have proved effective and safe in routine use are likely to be considered for mass administration during the acute phase of a humanitarian crisis. Such vaccines not only protect people against specific diseases; when administered on a large scale, they confer additional benefit through herd immunity, which reduces disease transmission above specific vaccination coverage thresholds.
Vaccines are generally administered before people are exposed to the pathogen causing the targeted disease. Unnecessary vaccination entails opportunity costs and puts people at risk of side-effects. The risk of contagion must justify vaccination. Four variables determine risk magnitude: the nature of the illness and attendant local epidemiological and environmental characteristics; the probability of transmission; disease severity and disease duration.17 If a disaster occurs where vaccination coverage is already high or the risk of an outbreak is low, additional, emergency vaccination may be of minimal benefit. For example, following the earthquake in Sichuan Province in China in 2008, mass measles vaccination would have been inappropriate because a province-wide measles vaccination campaign with high coverage had just been completed.18
Vaccines produce benefits but can also cause individual or social harm. Side-effects are an example of individual harm. These range from mild, common reactions, such as inflammation and pain at the injection site, to more severe but extremely rare events. Established vaccines, which are normally used during humanitarian emergencies, have well-known side-effect profiles, but much less is known about adverse events that can occur in ill or malnourished people during a humanitarian emergency.19 Children in this category tend to be biologically more susceptible to vaccine-preventable diseases than others, and when their parents refuse to have them vaccinated, they may be causing them individual harm. On the other hand, vaccination is sometimes contraindicated or inappropriate. A child, for instance, can be too young to receive a certain vaccine.
Parents’ refusal to get vaccinated or to vaccinate their children can cause collective harm by incrementing the pool of unprotected, susceptible individuals in a community. With herd immunity compromised, devastating disease outbreaks can occur. In these settings, individuals are morally obligated to accept vaccination to prevent harm to others.20 Harm may result from errors of omission or commission. Failure to provide a vaccine that is indicated in a specific humanitarian emergency violates the principle of non-maleficence because it places vulnerable populations and individuals at risk of contracting a vaccine-preventable disease.
Distributive justice
Distributive justice requires the fair allocation of scarce basic resources, such as shelter, food, potable water and vaccines in short supply. A small supply of vaccine could be equitably distributed through a lottery, but prioritizing particularly susceptible groups and individuals, or those most likely to spread the disease, would not be possible. Different rules govern decision-making and priority-setting during acute crises. Resource distribution during a crisis is often suboptimal because those engaged in humanitarian assistance can only do the “best they can” in the context of imperfect information, exceptional circumstances and needs far outweighing the available resources.9
When resources, especially staff, are scarce, decision-makers often choose among interventions – implicitly or explicitly – on the basis of cost-effectiveness because they are seeking to maximize benefits. Vaccination is highly cost-effective and, in emergencies, it can mitigate the risk of serious infectious disease. Furthermore, large numbers of people can be vaccinated quickly. Other factors to consider are how urgent and intense is the need for vaccination; how much faster can vaccination be delivered than other interventions; and how groups at high risk or with high transmission rates can be targeted in situations where other interventions, such as safe water and sanitation, cannot be rapidly deployed.
All countries, regardless of their socioeconomic status or experience with humanitarian emergencies, need to decide how to allocate resources. All societies have a shared vulnerability to emergencies, although poor societies are more severely devastated because poverty undermines resilience. When allocating resources, a balance must be sought between utility – maximizing the common good and ensuring smooth economic and social functioning – and equality and fairness. This balance is essential to garner people’s trust in vaccination programmes during crises. In keeping with egalitarian considerations, resource allocation should not be discriminatory; everyone should have a fair chance of being vaccinated.21 Furthermore, resources should be allocated with the aim of achieving “the greatest good for the greatest number”. Utility can conflict with equality or fairness. You can, for example, save the most lives or avert the most DALYs (disability affected life years) by allocating vaccines to urban rather than rural areas because urban areas have greater population density,21 but doing so systematically would be inequitable. In conflict zones, threats to the physical safety of health workers often determine which populations they can and cannot vaccinate.
Efforts to maximize utility can conflict with the egalitarian goal of helping the neediest. When limited supplies are allocated to the most vulnerable, overall health utility is sometimes suboptimal (e.g. less aggregate well-being, fewer lives saved, and/or fewer DALYs averted). From the perspective of value pluralism, balancing utility and equality should be the goal, rather than prioritizing one or the other. When it comes to vaccination, utility is fortunately often greatest when the most socially disadvantaged groups are targeted.
The fair distribution of limited vaccine supplies was an important issue during preparations for the 2009 pandemic influenza. People in certain categories were prioritized: those at greatest risk of infection (e.g. school children and health-care workers); those most likely to become severely ill if infected (e.g. immunosuppressed individuals and chronic disease patients); those most likely to spread infection (e.g. children and emergency service providers).22 During humanitarian emergencies in which populations are displaced, neighbouring communities also require attention. In most circumstances, host communities and refugees should be given access to each other’s services.23 Refugee or displaced populations should not be treated as separate from the host community, and assistance programmes, including vaccination, should support everyone in the area as a whole.24 The guiding principle should be to provide equitable access to vaccination to equalize risk. From an inclusive perspective, there is efficiency in covering two communities with all the resources available. Fair and equitable approaches result in less hostility and rivalry between the host and the displaced communities.13
From the point of view of utility and equity, in many cases children should be prioritized because they are generally more vulnerable than older people to vaccine-preventable diseases. In addition, saving a child’s life will result in a larger reduction in disease burden because more years of healthy life are lost when a child dies.21 Parents and caregivers often prioritize children’s needs over their own. However, some communities may place greater value on the social roles of the elderly and of pregnant women and may prioritize their access to health care during emergencies.
From a utilitarian perspective, protecting frontline health workers against disease will indirectly benefit the health of the community. Under the principle of reciprocity, it is fair to prioritize the vaccination of health-care workers, who are often more exposed than others to the risk of contagion, since they are committed to caring for society. In addition, because health-care workers come into contact with susceptible individuals, they have a moral obligation to get vaccinated to avoid placing patients at risk of infection.25
Procedural justice
Procedural justice requires transparent decision-making with involvement of the communities affected by the decisions.26 To ensure procedural justice, it is very useful to have guidelines or a legal framework to follow. Guidelines are especially valuable in certain situations: when large numbers of people need to be treated or protected against disease; when delayed or suboptimal measures could lead to very poor outcomes; and when inadequate management could result in high mortality or a large-scale epidemic. Although guidelines do not have mandatory status, if they are evidence-based and contextually appropriate they should be considered normative practice and a benchmark for judging the actions of health officials and practitioners.
National legal systems should guide the implementation of vaccination programmes in individual nation states, but they seldom accommodate humanitarian emergencies. When national legislative frameworks are absent or dysfunctional, international human rights law dictates a duty of care to protect people needing assistance, and in such cases implementation should follow international health guidelines. WHO Member States can legitimately follow WHO vaccination guidelines, which were developed on the strength of the evidence and which take many factors into account, including the epidemiologic and clinical features of the target disease, vaccine characteristics, costs, health system infrastructure, social impact, legal and ethical considerations, and the local context.27,28
Efforts to improve accountability during humanitarian emergencies have resulted in the Sphere Project, the Humanitarian Accountability Partnership and the Active Learning Network for Accountability and Performance in Humanitarian Action.29 All three seek to involve beneficiaries in the planning and implementation of aid programmes, establish codes of conduct for responding agencies, promote technical standards, and encourage the use of performance indicators and impact assessments.
Observing appropriate rules of conduct during humanitarian crises is often difficult.10 In certain political contexts, health-care workers may find that following guidance from their governments or humanitarian organizations is in conflict with their commitment to promote individuals’ best interests. Affected populations are often disenfranchised and unable to defend their own interests. All factors considered before the introduction of a vaccination programme should be well documented and publicly available to donors, community leaders, local staff and governments. Channels should also be established for affected communities to express their concerns directly to responding agencies.
Consent
Obtaining valid consent from individuals before a medical intervention is an obligation under the principle of respect for the autonomy of persons. In non-emergency circumstances, the consent process needs to be thorough and takes time. During emergencies, it has to be modified. If time permits, information on the risks and benefits of vaccination should be communicated to target populations in sufficient depth to allow individuals to make informed decisions, while bearing in mind that many will lack a basic understanding of germ theory and immunology. During emergencies, vaccination often takes place while people are too desperate for food and other basic necessities to recognize its importance. Furthermore, in some developing countries people defer to decision-makers at the expense of individual autonomy.
The amount of information provided to the public needs to be weighed against the risk of delaying action. However, any questions raised by the community should be thoroughly addressed. For example, vaccinators should be prepared to answer common questions about the diseases targeted, the benefits of vaccination, potential side-effects, follow-up and alternative options. They should also know where to refer undecided individuals who have other questions, although this may not always be feasible. Visual aids and other media can be used to convey important information to the public in a time-efficient manner.
Vaccination should be voluntary unless it becomes critical to “prevent a concrete and serious harm”.30 The degree of risk to communities will determine to what extent individual rights may be restricted. Where the threat of widespread, serious infectious disease is imminent, individual liberties may be justifiably curtailed.31 The Siracusa Principles endorsed by the United Nations Economic and Social Council state that: “Public health may be invoked as a ground for limiting certain rights in order to allow a State to take measures dealing with a serious threat to the health of the population or individual members of the population. These measures must be specifically aimed at preventing disease or injury or providing care for the sick and injured”.32 It may thus be permissible for those in authority to restrict individual autonomy to prevent harm to others. Although this approach has been limited to immediate or direct threat under traditional public health law, it should arguably be extended to what is “reasonably foreseeable” based on epidemiology and historical occurrence.33 If the risk to health is extremely high, individuals should not be allowed to compromise group protection and communal rights.34–36 When personal liberty is restricted to protect public health, the measures applied must be effective, the least restrictive (i.e. least liberty-infringing), proportional to the risk, equitable and non-discriminatory, minimally burdensome and in line with due process. Those whose liberty is violated should, when appropriate, be compensated, particularly if they experience vaccine-associated side-effects.37,38 In addition, individual rights should be restricted only with utmost respect for the dignity of persons.
Children are at particularly high risk of contracting communicable diseases during humanitarian crises. In most emergencies, mortality in children under the age of 5 years is generally two to three times higher than crude mortality.39 Vaccinating children could reduce mortality in all age groups because epidemics often arise and spread among children.40 Parents’ refusal to have their children vaccinated should be respected if the risk of disease is low or the disease is mild. However, if the risk of harm to the child is high, parental authority may be overruled to protect the child’s best interests.20,41 In emergency settings a parent or guardian may not be available, and health-care workers should be empowered to rapidly decide whether to vaccinate a child if done in the child and community’s best interests.
Research
Opportunities for health and health service research abound during humanitarian crises.42,43 However, in resource-limited settings, medical care and service delivery must always take precedence over research.44 In disaster settings, research is often conducted by the same people who provide aid and thus “rightly takes second place to the provision of life-saving assistance”.45 If specific personnel were assigned exclusively to research, critical human resources would not be diverted away from care.45 Nonetheless, such personnel should only be allowed to conduct research after a local research ethics committee has determined that enough care personnel are available to meet demand.46 Regional or international ethics review boards should be created in places without appropriate local expertise. In countries without functioning research governance structures, researchers must rely on international ethics review boards.
Research must be distinguished from disease and programme surveillance.47 Surveillance is essential for assessing vaccination coverage, informing programme planning, evaluating vaccine effectiveness, and monitoring safety in the population as a whole and in certain subgroups.48 Surveillance also allows the rapid detection of cases that may signal programme failure requiring remediation. Since surveillance activities have an opportunity cost, the data collected must be analysed and used to direct public health action.49
Under the principle of justice, communities where research is conducted must stand to benefit. Research protocols should be relevant, methodologically sound and explicit about the benefits and potential harms to study participants. They should also clearly explain how the findings will be delivered to study participants if they are relocated after the humanitarian crisis.50 Research should not undermine the provision of health services and should be carried to completion.
Although most non-medical research conducted during disasters is observational, it is subject to ethics review to ensure that individual and social benefits outweigh any risks. The level of review should be proportional to the risk associated with a specific intervention. An expedited review is admissible if the risk to participants is low, whereas a full committee review is warranted when the research involves a higher risk. If the research is urgent and very important, it can proceed without ethics committee approval, but retrospective review should be sought as soon as possible. Whenever the nature of the research to be conducted during a humanitarian emergency can be anticipated, a full review of the generic protocols should be planned and discussed in advance with local research ethics committees. Provision should be made for counselling or debriefing should participants find the research interviews traumatic or distressing.51
Potential research participants may have impaired ability to make decisions or provide voluntary individual informed consent following an acute humanitarian emergency, especially in “vulnerable communities”, as defined by the Joint United Nations Programme on HIV/AIDS. Empirical research in developing countries has shown that obtaining informed consent from study participants is not easy, even under non-emergency circumstances. Acute humanitarian crises add a layer of complexity, and decisional capacity must be carefully assessed.52–56 In acute crises in which medical care is needed, patients often assume that a research intervention is known to be therapeutic or effective. During the consent process, study participants need to be made aware that they are consenting to research only, not to special or additional care.
Conclusion
Ethical considerations are vital to decision-making about the deployment of vaccines in acute humanitarian emergencies. Commitment to human rights and the rule of rescue place an onus on wealthy countries to ensure that life-saving vaccines are made available to the poorer countries during crises. Justice and ethics obligate those who are better off to assist those who are worse off and to allocate resources accordingly.57 National health authorities are morally obligated to do all that they reasonably can to implement evidence-based guidelines to avert preventable harm.58
The allocation of a limited supply of vaccine calls for a fine balance between utility and equality and fairness. Accountability demands that decision-making be explicit, documented and open to public review.
In emergencies, the informed consent process may be reasonably modified to avoid delaying protection for vulnerable communities. Autonomy is not absolute. In situations that threaten the health and well-being of others, authorities may be required to mandate vaccination and intervene on behalf of minors against parental wishes. Finally, emergency health-care workers should be trained in ethics to improve their decision-making skills during acute humanitarian emergencies.59
Acknowledgements
This review was prepared by WHO’s Strategic Advisory Group of Experts (SAGE). SAGE’s careful review and recommendations on the manuscript are gratefully acknowledged.
Competing interests:
None declared.
References
- 1.Levine C. The concept of vulnerability in disaster research. J Trauma Stress. 2004;17:395–402. doi: 10.1023/B:JOTS.0000048952.81894.f3. [DOI] [PubMed] [Google Scholar]
- 2.Shears P, Berry AM, Murphy R, Nabil MA. Epidemiological assessment of the health and nutrition of Ethiopian refugees in emergency camps in Sudan, 1985. BMJ. 1987;295:314–8. doi: 10.1136/bmj.295.6593.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Feudtner C, Marcuse EK. Ethics and immunization policy: promoting dialogue to sustain consensus. Pediatrics. 2001;107:1158–64. doi: 10.1542/peds.107.5.1158. [DOI] [PubMed] [Google Scholar]
- 4.Schwartz L, Hunt M, Sinding C, Elit L, Redwood-Campbell L, Adelson N, et al. Models for humanitarian health care ethics. Public Health Ethics. 2012;5:81–90. doi: 10.1093/phe/phs005. [DOI] [Google Scholar]
- 5.SAGE Working Group on Vaccination in Humanitarian Emergencies. SAGE working group on vaccination in humanitarian emergencies: a framework for decision-making. Geneva: World Health Organization; 2012. Available from: http://www.who.int/immunization/sage/meetings/2012/november/FinalFraft_FrmwrkDocument_SWGVHE_23OctFullWEBVERSION.pdf [accessed 24 January 2013].
- 6.Jonsen AR. Bentham in a box: technology assessment and health care allocation. Law Med Health Care. 1986;14:172–4. doi: 10.1111/j.1748-720x.1986.tb00974.x. [DOI] [PubMed] [Google Scholar]
- 7.Murphy L. Beneficence, law and liberty; the case of required rescue. Georgetown Law J. 2001;3:605–65. [Google Scholar]
- 8.Akabayashi A, Takimoto Y, Hayashi Y. Physician obligation to provide care during disasters: should physicians have been required to go to Fukushima? J Med Ethics. 2012;38:697–8. doi: 10.1136/medethics-2011-100216. [DOI] [PubMed] [Google Scholar]
- 9.Kenny C. Disaster risk reduction in developing countries: costs, benefits and institutions. Disasters. 2012;36:559–88. doi: 10.1111/j.1467-7717.2012.01275.x. [DOI] [PubMed] [Google Scholar]
- 10.Hurst SA, Mezger N, Mauron A. Allocating resources in humanitarian medicine. Public Health Ethics. 2009;2:89–99. doi: 10.1093/phe/phn042. [DOI] [Google Scholar]
- 11.Bradbury M. Normalising the crisis in Africa. Disasters. 1998;22:328–38. doi: 10.1111/1467-7717.00096. [DOI] [PubMed] [Google Scholar]
- 12.United Nations Economic, Scientific and Cultural Organization [Internet]. Universal Declaration on Bioethics and Human Rights. Paris: UNESCO; 2005. Available from: http://www.unesco.org/new/en/social-and-human-sciences/themes/bioethics/bioethics-and-human-rights [accessed 24 January 2013].
- 13.Sphere Project. The Sphere Project: humanitarian charter and minimum standards in humanitarian response Bourton on Dunsmore: Practical Action Publishing; 2011. Available from: http://practicalaction.org/sphere [accessed 24 January 2013].
- 14.United Nations High Commissioner for Refugees. Convention and protocol relating to the status of refugees Geneva: UNHCR; 1967. Available from: http://www.unhcr.org/3b66c2aa10.html [accessed 4 February 2013].
- 15.United Nations [Internet]. The Universal Declaration of Human Rights. New York: United Nations; 1948. Available from: www.un.org/en/documents/udhr/index.shtml [accessed 24 January 2013].
- 16.Vaccine donations: WHO–UNICEF joint statement. Geneva: World Health Organization & United Nations Children’s Fund; 2010 (WHO/IVB/10.09). Available from: http://whqlibdoc.who.int/hq/2010/WHO_IVB_10.09_eng.pdf [accessed 24 September 2012].
- 17.Rhodes RS, Telford GL, Hierholzer WJ, Barnes M. Bloodborne pathogen transmission from healthcare worker to patients. Legal issues and provider perspectives. Surg Clin North Am. 1995;75:1205–17. doi: 10.1016/s0039-6109(16)46792-7. [DOI] [PubMed] [Google Scholar]
- 18.Shu M, Liu Q, Wang J, Ao R, Yang C, Fang G, et al. Measles vaccine adverse events reported in the mass vaccination campaign of Sichuan province, China from 2007 to 2008. Vaccine. 2011;29:3507–10. doi: 10.1016/j.vaccine.2009.10.106. [DOI] [PubMed] [Google Scholar]
- 19.Savy M, Edmond K, Fine PEM, Hall A, Hennig BJ, Moore SE, et al. Landscape analysis of interactions between nutrition and vaccine responses in children. J Nutr. 2009;139:2154S–218S. doi: 10.3945/jn.109.105312. [DOI] [PubMed] [Google Scholar]
- 20.Dawson A. Vaccination ethics. In: Public health ethics Cambridge: Cambridge University Press; 2011. pp. 143–53. [Google Scholar]
- 21.Verweij M. Moral principles for allocating scarce medical resources in an influenza pandemic. J Bioeth Inq. 2009;6:159–69. doi: 10.1007/s11673-009-9161-6. [DOI] [Google Scholar]
- 22.Selgelid MJ. Pandethics. Public Health 2009;123:255-9. http://dx.doi.org/10.1016/j.puhe.2008.12.005 PMID:19223051 10.1016/j.puhe.2008.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.United Nations High Commissioner for Refugees. Guiding principles 2008–2012 Geneva: UNHCR; 2011. Available from: http://www.unhcr.org/4885959c2.htm [accessed 24 January 2013].
- 24.Hanquet G, editor. Médecins Sans Frontières. Refugee health: an approach to emergency situations MacMillan; 1997. Available from: http://www.refbooks.msf.org/MSF_Docs/En/Refugee_Health/RH.pdf [accessed 24 January 2013].
- 25.van Delden JJM, Ashcroft R, Dawson A, Marckmann G, Upshur R, Verweij MF. The ethics of mandatory vaccination against influenza for health care workers. Vaccine. 2008;26:5562–6. doi: 10.1016/j.vaccine.2008.08.002. [DOI] [PubMed] [Google Scholar]
- 26.Daniels N. Just health care Cambridge: Cambridge University Press; 1985. [Google Scholar]
- 27.Draft guidelines for WHO and SAGE development of evidence-based vaccine related recommendations. Geneva: World Health Organization; 2011. Available from: http://www.who.int/immunization/sage/1_Draft_Guidelines_Evidence_Review_GRADING_apr_2011.pdf [accessed 24 January 2013].
- 28.Duclos P, Durrheim D, Reingold A, Bhutta Z, Vannice K, Rees H. Developing evidence-based vaccine recommendations and GRADE. Vaccine. 2012;31:12–9. doi: 10.1016/j.vaccine.2012.02.041. [DOI] [PubMed] [Google Scholar]
- 29.Humanitarian Practice Network [Internet]. Humanitarian accountability. Humanitarian Exchange Magazine 2011;52. Available from: http://www.odihpn.org/humanitarian-exchange-magazine/issue-52/humanitarian-accountability [accessed 24 January 2013].
- 30.Verweij M, Dawson A. Ethical principles for collective immunisation programmes. Vaccine. 2004;22:3122–6. doi: 10.1016/j.vaccine.2004.01.062. [DOI] [PubMed] [Google Scholar]
- 31.Gostin LO. Influenza A(H1N1) and pandemic preparedness under the rule of international law. JAMA. 2009;301:2376–8. doi: 10.1001/jama.2009.849. [DOI] [PubMed] [Google Scholar]
- 32.United Nations Commission on Human Rights. The Siracusa principles on the limitation and derogation provisions in the International Covenant on Civil and Political Rights Geneva: UNCHR; 1984. Available from: http://www.unhcr.org/refworld/docid/4672bc122.html [accessed 24 January 2013].
- 33.Gostin LO. The resurgent tuberculosis epidemic in the era of AIDS: reflections on public health, law, and society. MD Law Rev. 1995;54:1–131. [PubMed] [Google Scholar]
- 34.Diekema D, Marcuse E. Ethical issues in the vaccination of children: primum non nocere today New York: Elsevier; 1998. [Google Scholar]
- 35.Harris J, Holm S. Is there a moral obligation not to infect others? BMJ. 1995;311:1215–7. doi: 10.1136/bmj.311.7014.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Simons KW. Negligence. Soc Philos Policy. 1999;16:52–93. doi: 10.1017/S0265052500002399. [DOI] [Google Scholar]
- 37.Isaacs D, Kilham H, Leask J, Tobin B. Ethical issues in immunisation. Vaccine. 2009;27:615–8. doi: 10.1016/j.vaccine.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 38.Selgelid MJ. A moderate pluralist approach to public health policy and ethics. Public Health Ethics. 2009;2:195–205. doi: 10.1093/phe/php018. [DOI] [Google Scholar]
- 39.Toole MJ, Waldman RJ. Prevention of excess mortality in refugee and displaced populations in developing countries. JAMA. 1990;263:3296–302. doi: 10.1001/jama.1990.03440240086021. [DOI] [PubMed] [Google Scholar]
- 40.Galvani AP, Medlock J, Chapman GB. The ethics of influenza vaccination. Science. 2006;313:758–60. doi: 10.1126/science.313.5788.758b. [DOI] [PubMed] [Google Scholar]
- 41.Finn A, Savulescu J. Is immunisation child protection? Lancet. 2011;378:465–8. doi: 10.1016/S0140-6736(11)60695-8. [DOI] [PubMed] [Google Scholar]
- 42.Collogan LK, Tuma F, Dolan-Sewell R, Borja S, Fleischman AR. Ethical issues pertaining to research in the aftermath of disaster. J Trauma Stress. 2004;17:363–72. doi: 10.1023/B:JOTS.0000048949.43570.6a. [DOI] [PubMed] [Google Scholar]
- 43.Kilpatrick DG. The ethics of disaster research: a special section. J Trauma Stress. 2004;17:361–2. doi: 10.1023/B:JOTS.0000048961.75301.74. [DOI] [PubMed] [Google Scholar]
- 44.World Medical Association [Internet]. WMA statement on medical ethics in the event of disasters. Ferney-Voltaire: WMA; 2006. Available from: http://www.wma.net/en/30publications/10policies/d7/index.html [accessed 24 September 2012].
- 45.Ford N, Mills EJ, Zachariah R, Upshur R. Ethics of conducting research in conflict settings. Confl Health. 2009;3:7. doi: 10.1186/1752-1505-3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Siriwardhana DC. Disaster research ethics – a luxury or a necessity for developing countries? Asian Tribune 13 February 2007. Available from: http://www.asiantribune.com/index.php?q=node/4524 [accessed 24 January 2013].
- 47.Research ethics in international epidemic response Geneva: World Health Organization; 2009. Available from: http://www.who.int/ethics/gip_research_ethics_.pdf [accessed 24 January 2012].
- 48.Fottrell E, Byass P. Identifying humanitarian crises in population surveillance field sites: simple procedures and ethical imperatives. Public Health. 2009;123:151–5. doi: 10.1016/j.puhe.2008.10.032. [DOI] [PubMed] [Google Scholar]
- 49.Carrel M. Demographic and health surveillance: longitudinal ethical considerations. Bull World Health Organ. 2008;86:612–6. doi: 10.2471/BLT.08.051037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.World Medical Association [Internet]. Declaration of Helsinki: ethical principles for medical research involving human subjects. Ferney-Voltaire: WMA; 1964. Available from: http://www.wma.net/en/20activities/10ethics/10helsinki/index.html [accessed 24 January 2013].
- 51.Wallis L, Smith W, editors. Disaster medicine Johannesburg: Juta; 2011. pp. 9–25. [Google Scholar]
- 52.Abdool Karim Q, Abdool Karim SS, Coovadia MH, Susser M. Informed consent for HIV testing in a South African hospital: is it truly informed and truly voluntary? Am J Public Health. 1998;88:637–40. doi: 10.2105/AJPH.88.4.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Joubert G, Steinberg H, van der Ryst E, Chikobvu P. Consent for Participation in the Bloemfontein Vitamin A Trial: How Informed and Voluntary? Am J Public Health. 2003;93:582–4. doi: 10.2105/AJPH.93.4.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Moodley K, Pather M, Myer L. Informed consent and participant perceptions of influenza vaccine trials in South Africa. J Med Ethics. 2005;31:727–32. doi: 10.1136/jme.2004.009910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Molyneux CS, Peshu N, Marsh K. Understanding of informed consent in a low-income setting: three case studies from the Kenyan Coast. Soc Sci Med. 2004;59:2547–59. doi: 10.1016/j.socscimed.2004.03.037. [DOI] [PubMed] [Google Scholar]
- 56.Frimpong-Mansoh A. Culture and voluntary informed consent in African health care systems. Dev World Bioeth. 2008;8:104–14. doi: 10.1111/j.1471-8847.2006.00181.x. [DOI] [PubMed] [Google Scholar]
- 57.Rawls J. A theory of justice Harvard: Harvard University Press; 1971. [Google Scholar]
- 58.Emerson CI, Singer PA. Is there an ethical obligation to complete polio eradication? Lancet. 2010;375:1340–1. doi: 10.1016/S0140-6736(10)60565-X. [DOI] [PubMed] [Google Scholar]
- 59.Hunt MR, Schwartz L, Elit L. Experience of ethics training and support for health care professionals in international aid work. Public Health Ethics. 2012;5:91–9. doi: 10.1093/phe/phr033. [DOI] [Google Scholar]