Abstract
Joint position sense (JPS), one method to assess proprioception, is the ability to replicate a target limb position. Feedback is commonly used to improve motor performance but it has not been demonstrated to improve JPS. The purpose of this study was to determine if feedback decreases error associated with knee JPS at three movement velocities. Healthy volunteers sat with their hip and knees flexed. The knee was passively extended at three velocities (0.5, 2, and 10°/s). Subjects were instructed to stop knee motion, via a thumb switch, at a 20° knee flexion target. Following movement, each subject received visual and proprioceptive feedback indicating final leg position relative to the target position. Movement velocities and times (4 s, 5 s, 6 s) were randomly presented so subjects could not predict the target position. Measures of JPS included constant error (CE), absolute error (AE), variable error (VE), and percent correct (%CORR). Significant decreases in CE, AE, and VE as well as an increase in %CORR were demonstrated. The majority of JPS improvement (85%) occurred by the tenth trial. Short-term improvements in JPS may be the result of temporary CNS adaptations via feedback that was provided to subjects. Long-term learning of JPS enhancement needs further investigation.
Keywords: Kinesthesia, Lower extremity, Motor learning, Sensorimotor, Somatosensory
Introduction
Proprioception has been described as afferent information typically arising from peripheral mechanoreceptors which contributes to joint position sense and joint stability, postural control and the conscious sensation of movement [13, 14]. Joint positions sense (JPS), a component of proprioception, represents the ability of subjects to actively or passively replicate a previously given limb position, in the absence of visual feedback. JPS is typically evaluated as the difference between terminal limb position and the given target position. Previous knee JPS tests used a wide range of methodologies including active or passive movement to replicate a target position, various subject positions (e.g., supine, side-lying, or prone), and various movement velocities (e.g., between 0.25 and 10.0°/s). Further complexity to understanding knee JPS arises from poor reliability from these types of tests [7]. Moreover, these different testing methodologies are applied to a number of patient populations such as those with ACL injuries, joint arthroplasty, and normal aging affects on JPS [3, 4, 18, 19]. Thus, finding methods to improve knee JPS testing may warrant increasing the clinical significance of this type of testing.
Researchers and clinicians understand the fundamental role of proprioception in sensorimotor integration and motor performance. There are a number of published studies that described improved motor performance due to improved proprioceptive training strategies [4, 6, 20, 23]. However, these studies incorporated training paradigms that potentially stimulated multiple sensorimotor systems, thereby limiting the direct association of training with proprioceptive enhancement. While proprioceptive enhancement is likely a factor in behavioral improvement these studies do not provide proof that the proprioceptive system was specifically trained, due the multifactorial and non-specific nature of the training paradigms. Proof of a purely proprioceptive training paradigm has been called for, but has not been as yet demonstrated in the literature [1].
Extrinsic feedback, such as “knowledge of results”, is critical for motor skill acquisition [15, 16]. Knowledge of results can be defined as information about the measured error between the terminal limb position and the given target position. Using extrinsic feedback to train solely proprioception has not been investigated. It is important to determine if the proprioceptive system can be trained by providing knowledge of results of final limb position relative to a target position, presented in order to enhance performance. However, to our knowledge, there has not been a published study that uses both knowledge of results type feedback in conjunction with passive movements in a JPS paradigm.
Developing more reliable methods of testing proprioception would enhance a clinician’s ability to identify and rehabilitate those that may be at risk of injury or rehabilitating from an existing injury. If in fact only passive movements are needed to train proprioception, novel ways of rehabilitation can be used to supplement traditional training paradigms. Clinicians can use passive movements and video game-like treatments to focus rehabilitation on the somatosensory system.
The purpose of this study was to determine if JPS can be improved using extrinsic feedback or “knowledge of results” by use of a passive training paradigm. The passive nature of this testing paradigm will enable us to isolate the afferent component of proprioception. Additionally, the use of multiple movement velocities may provide further insight on typical CNS responses under various movement conditions.
Methods
Subjects
Thirty healthy volunteers (27 ± 6.5 years; 15 males; 14 females; 171.0 ± 8.1 cm; 70.2 ± 16.4 kg) were brought into the Biomechanics Laboratory of the National Institutes of Health, where written informed consent was obtained and an explanation of the testing protocol was given following a brief medical screening. This research was conducted in accordance with all regulations specified by the internal review board of the National Institutes of Health (NIH), providing ethical approval for this study. Subjects were recruited from an existing database of volunteers of the Clinical Center at the NIH. Local volunteers typically peruse a NIH web-site to identify studies they may be interested in; some lab associates (n = 5) also participated in the study. While these subjects were typically young and healthy they were not athletes by definition of participating in high levels of competition.
Inclusion criteria were designated as healthy male and female subjects of age between 20 and 45 years. For this project, “healthy” was defined as having no existing neurological or physical pathology resulting in damage to muscle, nerve, ligament or cartilage in the left lower extremity. Additionally, the term healthy also referred to having no systemic disease that alters ability of the subject to participate in activities of his/her choice. Subjects were excluded if they had a recent (<3 months) history of lower extremity musculoskeletal injury, concussion or head trauma, current pain in the lower extremity, or impaired sensation in the lower extremity. The left lower extremity was tested on all subjects. Leg dominance was established by asking the subject which leg they preferred to use to kick a ball. Of the 30 subjects, we evaluated the non-dominant extremity on 25 subjects and the dominant extremity on the remaining five.
Apparatus and instrumentation
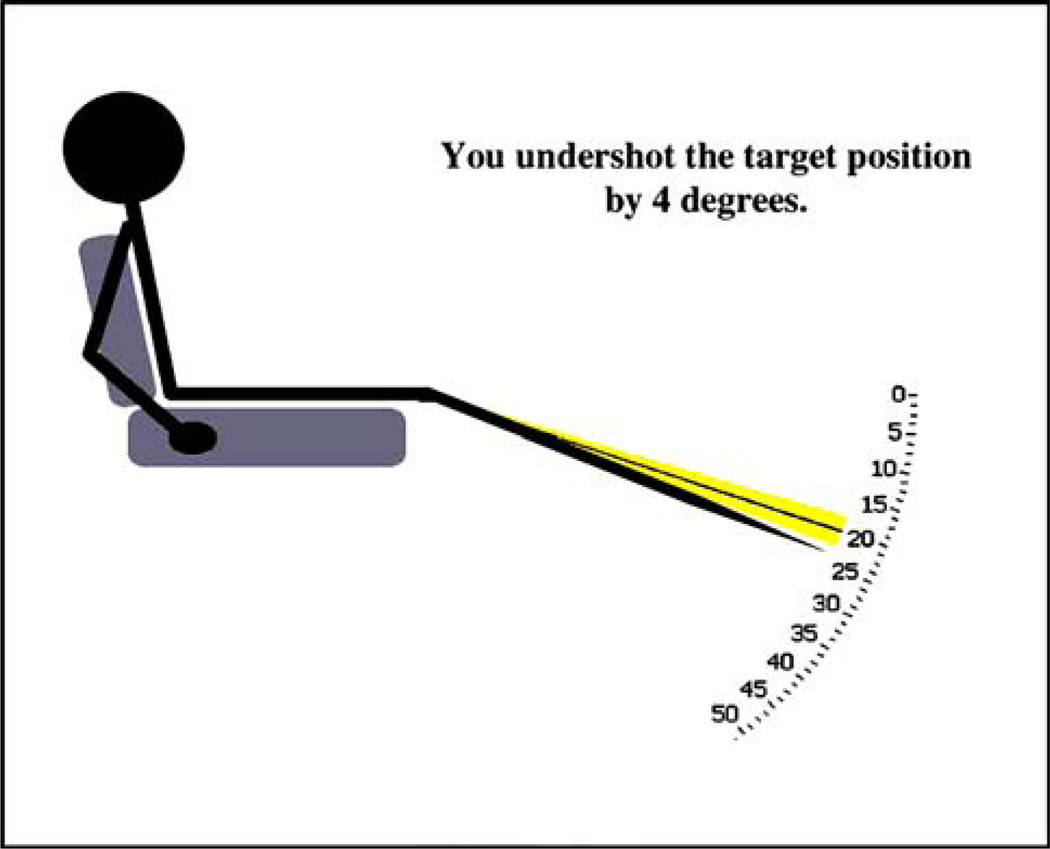
Each subject was seated on the chair of the Biodex 3 System (Biodex Medical Systems, Shirley, NY, USA). The subject’s hips were flexed to approximately 75° and the center of rotation of the knee and the dynamometer visually aligned. The subject’s left foot was placed in a custom-built foot/ankle apparatus designed to secure the foot at an angle of 90° to the shank. The foot was fixated at the calcaneus and a strap secured the forefoot (Fig. 1). The distal thigh and pelvis were also secured with straps. The dynamometer was controlled using LabView (National Instruments Corporation, Austin, TX, USA) and a custom-written software program. After each trial, visual feedback of final knee and leg position was provided to the subject through a video monitor located at eye level and at an arms-length away. Direct vision of the lower extremity workspace was occluded with a blanket. The feedback was generated from the angular position output of the dynamometer and was presented as a schematic figure of the subject seated on a chair (Fig. 2). The feedback provided spatial information for final leg position relative to the target position. A message on the video monitor was also included to describe the final placement of the leg relative to the target position (Fig. 2).
Fig. 1.
Apparatus used to move knee and method of foot fixation with ankle at 90°
Fig. 2.
Visual Feedback provided to subjects on video monitor
Feedback
A threshold, represented by shaded area on the feedback monitor (Fig. 2), of ±1.0° was used for knee rotational velocities of 0.5 and 2.0°/s, and ±2.0° for knee rotation at 10.0°/s. Selection of the threshold value (1–2°) was based on previous studies and takes into account increasing JPS errors at higher movement velocities [21]. Upon stopping movement of the knee and leg with the thumb-switch, the subject received the following message: “Within Threshold” if the final position was within the error threshold. If the final position was outside the error threshold, the subject received the following message: “You over/under shot the target by X degrees”, where X was the actual position error. The combination of textual and schematic information provided visual feedback of the subjects’ final leg position relative to the target position. To further reinforce the proporioceptive feedback and target position to the subject the dynamometer would passively rotate the knee and leg to the target position and would provide the following message: “This is the target position”. Messages on the video monitor were provided for approximately 5 s at the end of every trial.
Training paradigm
Procedure
Subjects were instructed that the purpose of this test was to replicate the target position as accurately as possible and that different movement times and speeds were going to be used, but ultimately it is the final position relative to the target position what is most important. The procedure consisted of two parts: an initial acclimation phase followed by a testing session. The acclimation phase established the target position and consisted of one trial at each velocity (e.g., 0.5, 2.0 and 10.0°/s) that would be used during the training session, as these movement velocities closely resemble testing conditions that have been used previously [2, 3, 7, 8, 17]. Throughout this phase, subjects could see the leg and final target position during movement on the video monitor. Twenty degrees of knee flexion (0° = full extension) was selected as the target joint position for all movements, which is also similar to previous knee JPS studies [7, 8, 17]. Each subject was instructed to stop the passive movement by depressing a thumb-switch when the knee and leg position was visually aligned with the target position. Upon completion of each trial the target position was reinforced via message on the video monitor: “Within threshold”. Each subject also received verbal reinforcement from the investigator of the target position.
Following the acclimation phase, each subject underwent a testing session of 45 trials (15 at each movement velocity) of passive knee extension. During testing, the video monitor went blank at the onset of passive movement. By removing the visual feedback during movement the subject was forced to rely solely on proprioceptive feedback to perceive where the knee and leg were in space. The subject was instructed to depress the thumb-switch when the knee was perceived to be at the target position. As soon as movement was stopped, final knee and leg position information from the potentiometer housed within the Biodex apparatus was displayed on the video monitor, providing feedback as described above, thereby ending the trial (Fig. 2). If the trial was outside of the threshold the leg was passively moved by the Biodex dynamometer to the target position and a message on the video monitor provided reinforcement of the target position. Following the presentation of visual and proprioceptive feedback, each subject’s leg was immediately moved to the starting position to begin the next trial. The nine movement conditions were randomly presented to each subject: Table 1 demonstrates the kinematics associated with each of the nine movement conditions. Variable movement times were used so that subjects could not predict when they were at or near the target.
Table 1.
Kinematic parameters describing starting knee angular position and total angular displacement toward target angle (20° of knee flexion) associated with nine movement conditions to passively move the knee
| Movement time (s) |
Knee rotational velocity | |||
|---|---|---|---|---|
| 0.5°/s | 2.0°/s | 10.0°/s | ||
| 4 s | Starting position (°) | 22° | 28° | 60° |
| Angular displacement (°) | 2° | 8° | 40° | |
| 5 s | Starting position (°) | 22.5° | 30° | 70° |
| Angular displacement (°) | 2.5° | 10° | 50° | |
| 6 s | Starting position (°) | 23° | 32° | 80° |
| Angular displacement (°) | 3° | 12° | 60° | |
Data reduction and statistical analysis
The final angular position of the dynamometer, representative of knee position, was captured and the following measures were calculated: constant error (CE), absolute error (AE) and variable error (VE) [5, 16]. These outcome measures were the dependent variables. Also captured was the percentage of correct trials (%CORR), or how often subjects were within the predetermined error threshold (Table 2). The %CORR data of previous trials were verbally provided to the subject every 4–6 trials in an effort to keep subjects motivated during the testing session.
Table 2.
Calculation of dependent variables from final knee position
|
where xi is the final knee joint position of the ith trial, T is the constant target position, and n is the number of trials over which the mean is calculated. | ||
|
where xi is the final knee joint position of the ith trial, T is the constant target position, and n is the number of trials over which the mean is calculated. | ||
|
where xi is the final knee joint position of the ith trial, X̄ is the mean of trials x1,…,xi, and n is the number of trials over which the mean is calculated. | ||
|
where n is the total number of observations and nk is the number of trials with AE falling outside of the threshold. |
Group (n = 30) means for the dependent variables were calculated across all 15 trials for each of the movement velocities to demonstrate how our subjects performed over time. Fifteen trials for each subject were collected at all three movement speeds and then grouped into the first, middle and last five trials; representing early, middle and late phases of the testing session.
In order to analyze CE, AE, and VE, separate, ANOVA with repeated measures were performed on two within-subject factors: testing session (3 levels: early, middle and late) and movement velocity (3 levels: 0.5, 2 and 10°/s). Evaluation of interactions and post-hoc analysis were performed with Bonferroni corrections to test for statistically significant differences.
Newell [11] introduced the analysis of motor performance using a mathematical power function to approximate the relationship between error versus training time. To further demonstrate the effect of the feedback that was provided on proprioception, log(trial number) − log(AE) regression equations were calculated for all subjects for at all three movement velocities (Excel, Microsoft, Inc., Redmond, WA, USA). From a mathematical perspective the slope of log(trial number) − log(AE) regression equations are equivalent to power function used in Newell’s [11] model. Only analysis of AE was used because the presence of negative values associated with CE does not allow the calculation of log variables, whereas VE provides information relative to precision rather than accuracy [16]. Group means of the log(trial number) − log(AE) regression slope coefficients were calculated for all three movement velocities. To determine if these slope coefficients were significantly negative (slope < 0), meaning decreasing AE, multiple Student t tests were used to compare slopes across all three movement velocities. Statistical significance was set atα = 0.05 for all statistical comparisons (SPSS v11.5, SPSS Inc, Chicago, IL, USA). Descriptive statistics were used to evaluate the %CORR across sequential trials.
Results
Mean performances from all three phases of the testing session are shown in Table 3. There was a significant interaction between the phase of the testing session and the movement velocity (F4,112 = 3.62, P = 0.008, 1-β = 0.95) for CE. Post-hoc interactions demonstrated significance between the early and middle (P = 0.012) phases and early and late (P < 0.001) phases at the slowest (0.5°/s) passive movement. At the 2.0°/s passive movement there was only a significant difference between the early and middle phases (P = 0.013) and at the fastest (10°/s) movement a significant difference was observed between the early and late phases (P = 0.002). There were also significant main effects for phase of the testing session (F2,56 = 64.9, P < 0.001) and the velocity of movement (F2,56 = 18.43, P < 0.001) on CE (Table 3).
Table 3.
Mean error scores (±SD) for early, middle and late phases of training final accuracy scores (CE, AE, VE) for the first (Early), middle (Middle) and last (Late) five trials across the 15 trials that were collected
| Error score | Movement velocity (°/s) |
Phase of test session | ||
|---|---|---|---|---|
| Early | Middle | Late | ||
| CE | 0.5 | −0.5 ± 0.5* | −0.3 ± 0.5 | −0.2 ± 0.4† |
| 2.0 | 0.2 ± 1.0* | 0.7 ± 1.0 | 0.7 ± 0.9 | |
| 10 | −2.0 ± 1.8* | −0.8 ± 2.1 | −0.7 ± 2.2† | |
| AE | 0.5 | 0.8 ± 0.2* | 0.6 ± 0.3 | 0.6 ± 0.2† |
| 2.0 | 1.3 ± 0.6 | 1.4 ± 0.6 | 1.3 ± 0.5 | |
| 10 | 3.6 ± 1.6* | 2.9 ± 1.1 | 3.2 ± 1.2 | |
| VE | 0.5 | 0.6 ± 0.4 | 0.5 ± 0.2 | 0.5 ± 0.2 |
| 2.0 | 1.3 ± 0.6* | 0.5 ± 0.2** | 1.1 ± 0.4 | |
| 10 | 3.5 ± 1.8* | 1.4 ± 0.5** | 3.1 ± 1.3 | |
Statistical significance between early and middle phase
Statistical Significance between middle and late stages
Statistical significance between early and late stages
There was a significant interaction between the phase of the testing session and the movement velocity (F4,112 = 4.05, P = 0.004;1-β = 0.89) for AE. Post-hoc comparisons of this interaction demonstrated significance between the early and late phases (P < 0.001) at the slowest passive movement (0.5°/s) and a significant difference between the early and middle phase (P = 0.008) during the fastest passive movement (10°/s). There were also significant main effects for phase of the testing session (F2,56 = 64.9, P < 0.001) and the velocity of movement (F2,56 = 18.43, P < 0.001) on AE (Table 3).
There was also a significant interaction between the phase of the testing session and the movement velocity (F4,112 = 17.3, P < 0.001; 1-β = 0.18) for VE. Post-hoc comparisons of this interaction demonstrate significance differences between the early and middle phases (P < 0.001) and middle and late phases (P = 0.001) at the 2.0°/s passive movement. Similarly, there were significance differences between the early and middle phases (P < 0.001) and middle and late phases (P = 0.001) at the 10°/s passive movement. There were also significant main effects for phase of testing session (F2,56 = 143.5, P < 0.001) and the velocity of movement (F2,56 = 36.6, P < 0.001) on VE (Table 3).
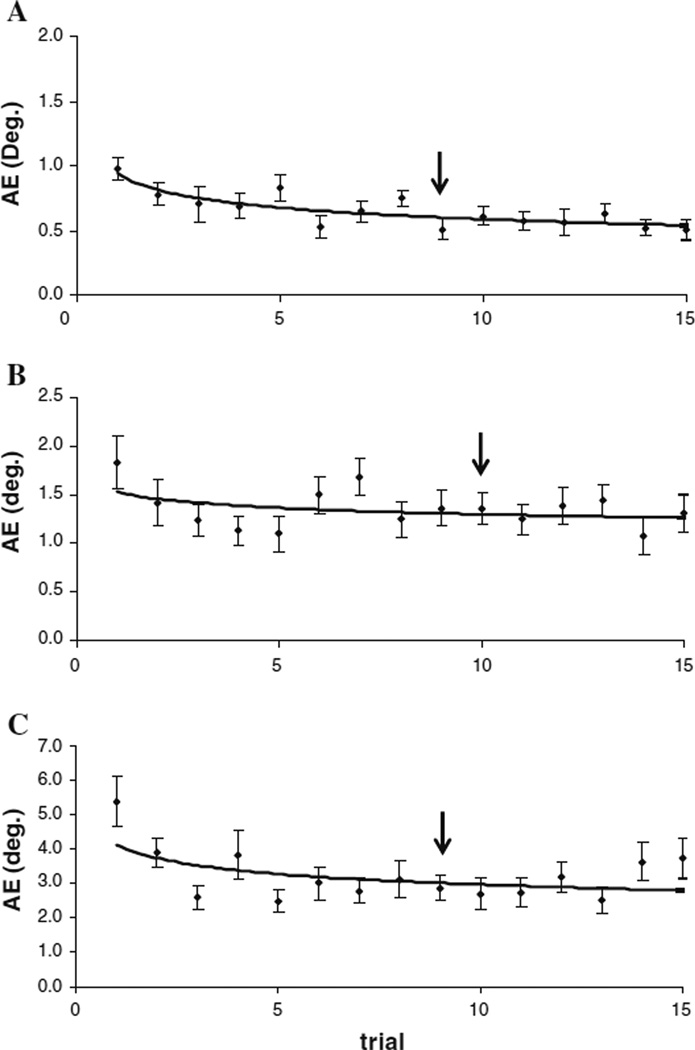
There was a significant negative slope in the log(trial number) − log(AE) regression equations at the 0.5°/s (slope = −0.23; P = 0.0005) and 10°/s (slope = −0.17; P = 0.009) movement velocities, but not for the 2°/s (slope = −0.04; P = 0.34) movement velocity. The AE decreased from 0.94° to 0.56° when the leg was rotated at 0.5°/s, decreased from 1.54° to 1.27° at 2.0°/s and decreased from 4.12° to 2.8° at 10°/s (Fig. 3).
Fig. 3.
Mean AE (±SE) for all three movement velocities a 0.5°/s, slope = −0.231 ± 0.059, P = 0.0005; b 2.0°/s, slope = −0.035 ± 0.063, P = 0.34, c 10.0°/s, slope = −0.172 ± 0.062, P = 0.009. Arrows (down arrow) indicate the trial at which 85% of overall improvement was achieved for each movement velocity. Please note the different scale for each graph
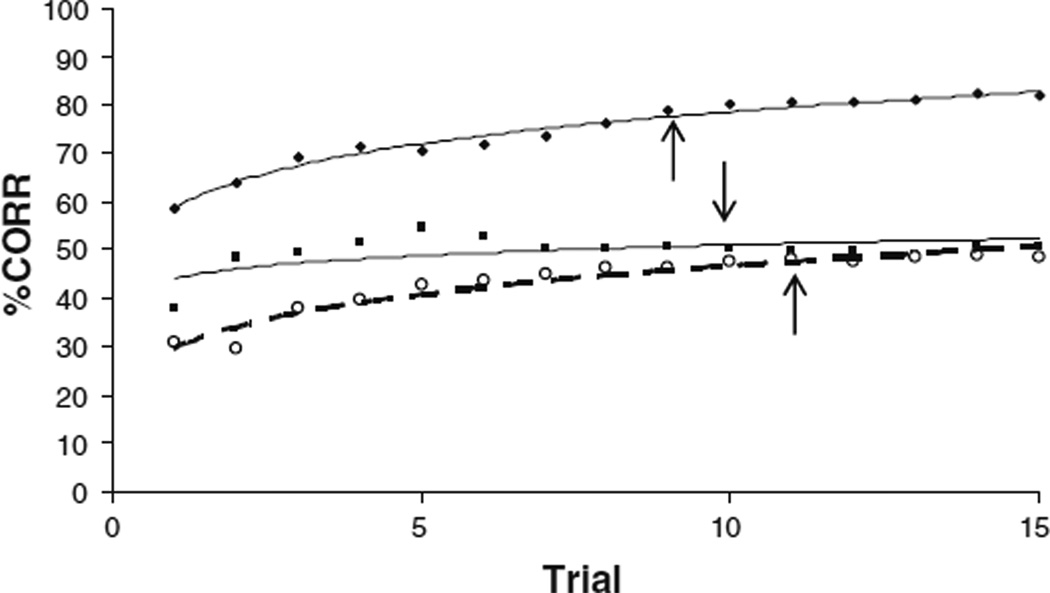
The %CORR also improved at for all three movement velocities: from 58.7 to 82.8% correct at 0.5°/s, from 44.1 to 52.3% correct at 2°/s and from 29.7 to 50.3% correct at 10°/s movement (Fig. 4).
Fig. 4.
Percent Correct for all three movement velocities. a 0.5°/s, (open circle with dashed line), b 2.0°/s, (filled square with dasshed line), c 10.0°/s, (filled circle with solid line) 85% of overall improvement occurred by the ninth trial for the 0.5 and 10°/s movement conditions and by the tenth trial for the 2.0°/s movement condition as indicated by the arrows (down arrow or up arrow)
Discussion
The purpose of this study was to determine if knee JPS could be enhanced using extrinsic feedback. Our passive method isolating only the sensory component of proprioception, may provide further opportunity to understand how the central nervous system may use this sensory feedback to motor planning [1]. Our main findings suggest that extrinsic feedback over the course of a single training session improved JPS across all movement velocities used here. Demonstrating improved knee JPS has, to the best of our knowledge, not been previously demonstrated in the literature. These data may suggest enhanced reliability associated with knee JPS.
At slow movement velocities (approx 0.5°/s) of the knee CE of −0.61 ± 0.6 has been reported when the knee was tested at 15° knee flexion target [21]. This is similar to the early phase (−0.5 ± 0.5) observed in this study. CE increases as movement velocity used to test knee JPS increases; 1.1° at 3°/s and 5.3° when tested at 10°/s [2, 3, 19]. This is also the trend that is demonstrated here as CE increased from −0.5 ± 0.5 to 2.0 ± 1.8. However, published results vary as others have reported CE as high as 13.8° for JPS when tested at 5°/s [7]. The results of our CE are within the range of published values but the variability associated CE of knee JPS makes it difficult to interpret.
While AE and VE are not reported as frequently as CE in the literature when evaluating knee JPS, Weiler and Awiszus [22] report AE of 2.9° ± 0.3°, at a 30° target position during slow movement velocities, which is larger than the 0.8 ± 0.2 AE observed in the early phase of our study. Differences in these results may be due to our study using a slightly slower movement velocity (0.6 vs. 0.5°/s), and the inclusion of feedback immediately following trials to improve performance. Additionally, Weiler and Awiszus [22] used a proximal pneumatic cuff that may have impeded circulation to the leg, which can affect mechanoreceptor sensitivity.
When JPS is evaluated in a group of ACL deficient subjects there is a reported increase in CE in both the involved and non-involved sides, which may suggest higher order CNS neuroplasticity in response to injury [8]. Providing feedback of performance, as was done in this study, may be a method of enhancing proprioceptive function, even if only temporary. Whether improvements observed in this study indicate a long-term adaptation or a temporary state is beyond the scope of this study, but future study of CNS mechanisms that account for this training effect is warranted.
Though the physiological response of the proprioceptive system to joint rotation was not directly measured some connections can be drawn between the improved performance observed in this study and the characteristics of peripheral receptors. The improved performance may be due to higher order CNS adaptations to the peripheral signals from Iα muscle spindles and joint receptors at the slow velocities and type II or dynamic muscle spindles at the fast movement velocities [9, 10]. However, it may be that subjects learned to activate the thumb switch earlier at the fastest movement velocity, thereby using the dynamic spindle feedback or simple reaction time, to predict final knee and leg position and ultimately improve their JPS scores. In essence subject became familiar with the testing paradigm, but the performance was not consistent across all movement velocities. Subjects demonstrated a consistent “undershooting” during both the fast and slow movement velocities; subjects consistently over shot the target during the 2.0 °/s movement velocity in this study (CE, in Table 3). Undershooting (-CE values) that occurred for both the 0.5 and 10°/s movement velocities may be due to relatively homogeneous feedback from the type II and Iα muscle spindles, respectively. However, feedback from both types of receptors may lead to more uncertainty resulting in overshooting for the 2.0°/s movement velocity. The receptor responses and associated CNS mechanisms behind over and undershooting are beyond the scope of the current study, but may be of interest for future investigation.
It has been suggested that a minimum of five to six trials are needed to demonstrate baseline knee JPS capability, but by providing feedback JPS may actually demonstrate better reliability [17]. The bulk of higher level neurophysiological changes associated with motor learning typically occur within the first ten trials [12, 16]. The preponderance of improvement (AE, %CORR) associated with JPS in our study, defined as 85% of observed progress, occurs by the tenth trial across all three movement velocities (Figs. 3, 4). It is unclear if the improvements observed in this study were short-lived or if there were true CNS adaptations leading to an altered state or learning. Future studies are necessary to determine the long-term effects of proprioceptive adaptations. Moreover, direct measures of CNS adaptations could confirm or refute any long-term training effects on proprioceptive abilities from paradigms similar to that used in this study. Studies of long-term adaptations of the proprioceptive system are warranted in order to further understand complex CNS alterations that may occur.
Currently, there is no standard for evaluating JPS at the knee, which has lead to a number of methodologies used to test knee joint proprioception. In this study we attempted to replicate common testing conditions (subject position, movement velocities and knee test angle) that have been used in previous studies. It is encouraging that the JPS values (CE, AE, and VE) of our subjects were in line with previous studies, suggesting validity of our methodology. However, it is not possible to directly compare the training effect on improved JPS performance to existing literature since this appears to be the first study of its kind. While this study demonstrated improved JPS over time and may suggest CNS adaptations or learning, the clinical or functional significance of this improvement remains in question. Additionally, it is not clear how improved JPS performance from a purely passive paradigm would translate to a motor performance. To further strengthen any claim of proprioceptive learning pre-testing measures with the absence of feedback and post feedback training measures should be obtained for future investigation. Highly competitive athletes may also demonstrate significantly different capabilities versus what was demonstrated in this study and warrants further investigation [2]. Our research also only tested a limited range of movement velocities (0.5–10°/s); it is unknown how proprioceptive performance and learning will be influenced as movement velocities that approach functional significance: movements greater than 100°/s. The fact that this study demonstrated enhanced proprioceptive performance with feedback as movement speed increased suggests that improvements can be obtained for faster movement velocities; however, this needs to be fully explored.
The only constant across all movement conditions was the target position. Randomization of the movement velocities and movement times was an attempt to minimize the influence of these on JPS outcomes. It was postulated that the interaction between variable movement times and velocities would minimally impact knee JPS in this study. Therefore, movement time was not included in the reported statistical analysis, but analysis our AE data (not reported here) separated into the three movement times confirmed this assumption; movement time did not influence JPS. Our initial base-line JPS measures arose from the first five trials (the “early” phase) which may indeed be different if feedback was not provided. While this may be true, our JPS scores from the initial trials are similar to previous published literature; it suggests similarity between our testing paradigm and other reported values.
The multiple outcomes used this study, such as the use of log(trial number) − log(AE) regression equations, %CORR and analyzing outcomes from three different phases (early, middle, and late), was to provide adequate scrutiny of observed trends across a testing session. The VE reported in this study demonstrated low power (1-β = 0.18) compared to CE and AE and serves as a warning against using a single metric of proprioceptive ability. Although, the best method to demonstrate learning has not been established, the methods used in our study offer supporting evidence toward improved JPS when feedback is provided to subjects.
Conclusions/clinical relevance
Our results indicate that using extrinsic feedback, such as “knowledge of results” improves knee joint proprioception or JPS, at least temporarily. The finding of improved JPS with extrinsic feedback may be the result of a long-term change to the CNS or more likely due to a temporary adaptation in which performance may return to an original state. While improvements reported in this study were small, they may prove significant with future testing associated with proprioceptive training. This study only examined the immediate effect of training and did not assess any long-term CNS adaptations. The results of this study suggest that by instituting a brief training session (e.g., 10 trials) in which subjects are provided with feedback of their performance, knee JPS reliability was improved. Thus, the immediate impact of this study may provide more reliable knee JPS testing. Long-term the applications from this type of testing may suggest that passive movements may be used to train the somatosensory system as an adjunct to traditional rehabilitation.
Contributor Information
Timothy J. Brindle, Email: Tbrindle@cc.nih.gov, Biomechanics Laboratory, National Institutes of Health, Building 10 CRC, Room 1-1469 10 Center Drive MCS 1604, Bethesda, MD 20892, USA.
J. C. Mizelle, School of Applied Physiology, Georgia Institute of Technology, Atlanta, GA 30332-0356, USA
Maria K. Lebiedowska, Biomechanics Laboratory, National Institutes of Health, Building 10 CRC, Room 1-1469 10 Center Drive MCS 1604, Bethesda, MD 20892, USA
Jeri L. Miller, Biomechanics Laboratory, National Institutes of Health, Building 10 CRC, Room 1-1469 10 Center Drive MCS 1604, Bethesda, MD 20892, USA
Steven J. Stanhope, College of Health Sciences, University of Delaware, Newark, DE 19716, USA
References
- 1.Ashton-Miller JA, Wojtys EM, Huston LJ, Fry-Welch D. Can proprioception really be improved by exercises? Knee Surg Sports Traumatol Arthrosc. 2001;9:128–136. doi: 10.1007/s001670100208. [DOI] [PubMed] [Google Scholar]
- 2.Barrack RL, Skinner HB, Brunet ME, Cook SD. Joint kinesthesia in the highly trained knee. J Sports Med Phys Fitness. 1984;24:18–20. [PubMed] [Google Scholar]
- 3.Barrack RL, Skinner HB, Brunet ME, Cook SD. Joint laxity and proprioception in the knee. Phys Sportsmed. 1983;11:130–135. doi: 10.1080/00913847.1983.11708565. [DOI] [PubMed] [Google Scholar]
- 4.Borsa PA, Lephart SM, Irrgang JJ, Safran MR, Fu FH. The effects of joint position and direction of joint motion on proprioceptive sensibility in anterior cruciate ligament-deficient athletes. Am J Sports Med. 1997;25:336–340. doi: 10.1177/036354659702500311. [DOI] [PubMed] [Google Scholar]
- 5.Brindle TJ, Nitz AJ, Uhl TL, Kifer E, Shapiro R. Measures of accuracy for active shoulder movements at 3 different speeds with kinesthetic and visual feedback. J Orthop Sports Phys Ther. 2004;34:468–478. doi: 10.2519/jospt.2004.34.8.468. [DOI] [PubMed] [Google Scholar]
- 6.Forkin DM, Koczur C, Battle R, Newton RA. Evaluation of kinesthetic deficits indicative of balance control in gymnasts with unilateral chronic ankle sprains. J Orthop Sports Phys Ther. 1996;23:245–250. doi: 10.2519/jospt.1996.23.4.245. [DOI] [PubMed] [Google Scholar]
- 7.Grob KR, Kuster MS, Higgins SA, Lloyd DG, Yata H. Lack of correlation between different measurements of proprioception in the knee. J Bone Joint Surg Br. 2002;84:614–618. doi: 10.1302/0301-620x.84b4.11241. [DOI] [PubMed] [Google Scholar]
- 8.Jensen TO, Fischer-Rasmussen T, Kjaer M, Magnusson SP. Proprioception in poor- and well-functioning anterior cruciate ligament deficient patients. J Rehabil Med. 2002;34:141–149. doi: 10.1080/165019702753714174. [DOI] [PubMed] [Google Scholar]
- 9.Johansson H, Sjolander P, Sojka P. A sensory role for the cruciate ligaments. Clin Orthop. 1991;268:161–178. [PubMed] [Google Scholar]
- 10.Lephart SM, Pincivero DM, Giraldo JL, Fu FH. The role of proprioception in the management and rehabilitation of athletic injuries. Am J Sports Med. 1997;25:130–137. doi: 10.1177/036354659702500126. [DOI] [PubMed] [Google Scholar]
- 11.Newell KM. Motor skill acquisition. Annu Rev Psychol. 1991;42:213–237. doi: 10.1146/annurev.ps.42.020191.001241. [DOI] [PubMed] [Google Scholar]
- 12.Paz R, Boraud T, Natan C, Bergman H, Vaadia E. Preparatory activity in motor cortex reflects learning of local visuomotor skills. Nat Neurosci. 2003;6:882–890. doi: 10.1038/nn1097. [DOI] [PubMed] [Google Scholar]
- 13.Reimann BL, Lephart SM. The sensorimotor system, Part I: The physiologic basis of functional joint stability. J Athletic Training. 2002;37:71–79. [PMC free article] [PubMed] [Google Scholar]
- 14.Reimann BL, Lephart SM. The sensorimotor system. Part II: The role of proprioception in motor control and functional joint stability. J Athletic Training. 2002;37:80–84. [PMC free article] [PubMed] [Google Scholar]
- 15.Salmoni AW, Schmidt RA, Walter CB. Knowledge of results and motor learning: a review and critical reappraisal. Psychol Bull. 1984;95:355–386. [PubMed] [Google Scholar]
- 16.Schmidt RA, Lee TD. Motor control and learning. Champaign: Human Kinetics; 1999. [Google Scholar]
- 17.Selfe J, Callaghan M, McHenry A, Richards J, Oldham J. An investigation into the effect of number of trials during proprioceptive testing in patients with patellofemoral pain syndrome. J Orthop Res. 2006;24:1218–1224. doi: 10.1002/jor.20127. [DOI] [PubMed] [Google Scholar]
- 18.Swanik CB, Lephart SM, Rubash HE. Proprioception, kinesthesia, and balance after total knee arthroplasty with cruciate-retaining and posterior stabilized prostheses. J Bone Joint Surg Am. 2004;86-A:328–334. doi: 10.2106/00004623-200402000-00016. [DOI] [PubMed] [Google Scholar]
- 19.Tsang WW, Hui-Chan CW. Effects of exercise on joint sense and balance in elderly men: Tai Chi versus golf. Med Sci Sports Exerc. 2004;36:658–667. doi: 10.1249/01.mss.0000122077.87090.2e. [DOI] [PubMed] [Google Scholar]
- 20.Verhagen E, van der Beek A, Twisk J, Bouter L, Bahr R, van Mechelen W. The effect of a proprioceptive balance board training program for the prevention of ankle sprains: a prospective controlled trial. Am J Sports Med. 2004;32:1385–1393. doi: 10.1177/0363546503262177. [DOI] [PubMed] [Google Scholar]
- 21.Weiler HT, Awiszus F. Characterisation of human knee-joint proprioception by means of a signal-detection theory. Exp Brain Res. 2001;138:110–117. doi: 10.1007/s002210100692. [DOI] [PubMed] [Google Scholar]
- 22.Weiler HT, Awiszus F. Influence of hysteresis on joint position sense in the human knee joint. Exp Brain Res. 2000;135:215–221. doi: 10.1007/s002210000512. [DOI] [PubMed] [Google Scholar]
- 23.Zatterstrom R, Friden T, Lindstrand A, Moritz U. The effect of physiotherapy on standing balance in chronic anterior cruciate ligament insufficiency. Am J Sports Med. 1994;22:531–536. doi: 10.1177/036354659402200416. [DOI] [PubMed] [Google Scholar]