Abstract
Context
Extensive observational evidence indicates youth in high-poverty neighborhoods exhibit poor mental health, although not all children may be affected similarly.
Objective
To use experimental evidence to assess whether gender and family health problems modify mental health effects of moving from high- to low-poverty neighborhoods.
Design, Setting, Participants
The Moving to Opportunity Study, a randomized controlled trial, enrolled volunteer low-income families in public housing in 5 U.S. cities from 1994–1997. We analyze 4–7 year outcomes among youth aged 12–19 (n=2829, 89% effective response rate).
Intervention
Families were randomized to control (remaining in public housing) or experimental (receiving government-funded rental subsidies to move into private apartments) groups. Intent-to-treat analyses included intervention interactions by gender and health vulnerability (defined as pre-randomization health/developmental limitations or disabilities among family members).
Outcome measures
Past-year psychological distress (K6), and Behavioral Problems Index (BPI). Supplemental analyses used past-year major depressive disorder (MDD).
Results
Male gender and family health vulnerability significantly adversely modified the intervention effect on K6 (gender: p=.02, health vulnerability: p=.002); male gender, but not health vulnerability, significantly adversely modified the intervention effect on BPI (gender: p=.01, health vulnerability: p=.17). Female adolescents without baseline health vulnerabilities were the only subgroup to benefit on any outcome (K6 (B= −0.21, 95% CI: (−0.34–−0.07), p=.003); MDD (Odds Ratio =0.42 (0.20–0.85) p=0.024). For male adolescents with health vulnerabilities, intervention was associated with worse K6 (B=.26, (0.09–0.44), p=.003) and BPI (B=.24 (0.09–0.40) p=.002). Neither females with health vulnerability, nor males without health vulnerability, experienced intervention benefits. Adherence-adjusted instrumental variable analysis found intervention effects twice as large. Patterns were similar for MDD but estimates were imprecise due to low prevalence.
Conclusions
Although some girls benefited, boys and adolescents from families with baseline health problems did not experience mental health benefits from housing mobility policies, and may need additional program supports.
Mental disorders and high levels of internalizing and externalizing symptoms among adolescents have negative health and social consequences throughout the life course1–4. Racial/ethnic minority families are disproportionately more likely to live in impoverished neighborhoods5, 6, and many research studies suggest adolescents residing in high-poverty communities experience elevated psychiatric morbidity7–9. However, prior neighborhood-mental health studies have been observational and thus effect estimates are potentially confounded9. Only one randomized trial that could evaluate effects of neighborhood context via housing mobility has been conducted: the Moving to Opportunity (MTO) trial. MTO randomly assigned families offers to move out of public housing using a Section 8 voucher which subsidizes rent in the private market, and these families moved to different neighborhood contexts. This experimental design is advantageous for evaluating the causal effects on mental health, related to moving out of public housing and changing neighborhood context.
Although housing policies are not usually considered part of national health services infrastructure, growing evidence documents that social and economic policies may influence health6, 10–14 by changing social determinants of health, for example, income, housing, or neighborhood context. Reducing mental health disparities will likely require multilevel approaches beyond only individual or family-level interventions; indeed, stress reduction accompanying a move to a low-poverty neighborhood may be of similar magnitude to that of pharmacologic treatment for mental disorder10.
Prior analyses of MTO documented puzzling evidence. Although neighborhood poverty was reduced in intervention group families compared to public-housing controls15, effects of these moves were not uniformly beneficial. Four to seven years after randomization, health effects for young children were not statistically significant16, while adult women in the MTO experimental group experienced better mental health and lower obesity; indeed, recently-released findings indicate this obesity advantage persisted 10–15 years post-randomization17. MTO benefited adolescent girls with respect to psychological distress, lifetime major depressive disorder (MDD), and health behaviors (e.g. smoking). Among adolescent boys however, effects for psychological distress and lifetime MDD outcomes were not statistically significant, and externalizing behaviors were unexpectedly increased by the intervention10, 11, 15, 18.
Because gender has shown such strong qualitative effect modification for other mental health outcomes in MTO, we hypothesized similar patterns for past-year MDD, which has not yet been examined in MTO. However no subsequent study has succeeded in explaining these opposite gender patterns or in extending findings to explain which children may benefit, and which may be harmed, by housing mobility. Indeed, previous evidence from psychosocial interventions suggests that frailer subgroups may not benefit from interventions to the same extent as healthier individuals, and in some circumstances may even be harmed19–21. We therefore hypothesized that family health-related vulnerability adversely modifies the effect of using rental subsidies to move out of public housing to lower-poverty neighborhoods. Intervention differences between more and less vulnerable groups may be due to either differential compliance rates (e.g. within MTO, if households with disabled family members were unable to find suitable private market rental units, even with voucher subsidies22, 23) or to differential effects among compliers (e.g. in vulnerable families, the benefit of moving may be offset by other chronic stressors24). Our manuscript therefore extends prior MTO findings by testing whether baseline health of families modifies the MTO intervention effect on adolescent mental health, in addition to improving operationalization of mental health.
DESIGN AND METHODS
Study Design
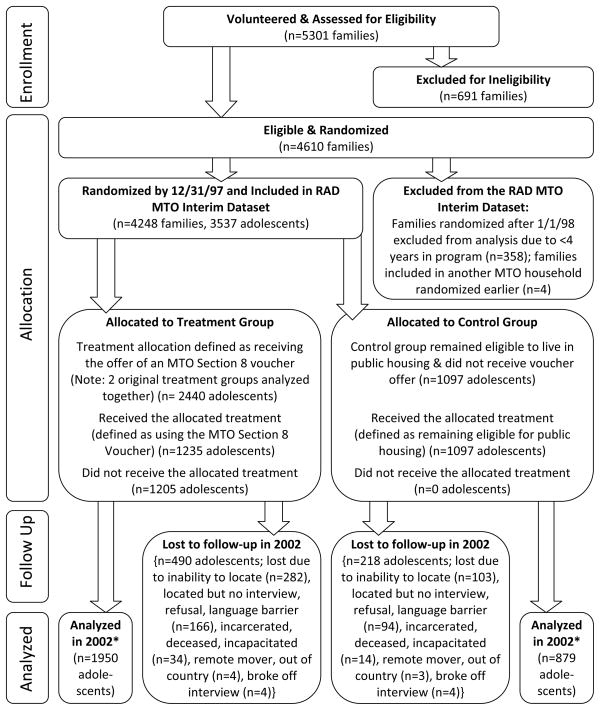
The Moving to Opportunity (MTO) for Fair Housing Demonstration Program was a randomized controlled trial (RCT) sponsored by the US Department of Housing & Urban Development (HUD)25, 26 in 5 US cities: Boston, Baltimore, Chicago, Los Angeles, New York. Eligible families had children under 18 years old and were recruited from public housing or project-based assisted housing in areas with high concentrations of poverty.26 Volunteer applicants were taken from MTO waiting lists, signed enrollment agreements and informed consents, completed the Baseline Participant Survey, and were evaluated for eligibility27 by local public housing authorities. Eligible families were randomly-assigned by computerized random-number generators to 1 of 3 intervention groups (Figure 1)15. MTO was not registered with CONSORT because it was not a medical intervention.
Figure 1. MTO Youth Enrollment, Intervention Allocation, and Attrition.
* 2002 Interim Survey yielded 89% effective response rate (RR) with a two-stage follow-up sampling strategy, calculated as: RR= MRR + SRR*(1-MRR), where MRR = response rate for main sample (respondents initially responding to 2002 survey interview request) and SRR= response rate for subsample (a 2nd attempt to find every 3 in 10 hard-to-reach families initially nonresponsive in 2002). 15(p.A-8).
Intervention Assignment
The “regular section 8” intervention group was offered housing vouchers that were redeemable to subsidize rent for a private market apartment. The “low-poverty neighborhood section 8” intervention group was offered housing vouchers that could only be used to subsidize rental housing located in low-poverty neighborhoods (<10% of the Census Tract lived in poverty). This group was also offered housing counseling services to aid relocation. Finally, an untreated control group received no further assistance from MTO, but could remain in public housing. Intervention group families could search for housing and rent a unit with their voucher for 90 days after randomization, or they lost their voucher (but could remain in public housing)27.
Evaluation surveys were conducted by Abt Associates at baseline and at the interim follow-up (4–7 years after baseline, Dec 2001-Sept 2002), among household heads and their children. Ninety-eight percent of interviews were in person via computer-assisted personal interviewing technology15, 27. Youth were interviewed predominantly in teen centers to improve privacy26. We focus on adolescents randomized 1994 through 1997 in the MTO Tier 1 Restricted Access Data (n=3537 aged 12–19 as of 5/31/01, aged 5–16 at randomization). Our analysis includes 2829 adolescents answering the interim survey. With a 2-stage follow up to locate participants, the interim survey had 89% effective response rate15 (Figure 1). Adults provided informed written consent before both surveys for themselves and their children15, 26, 27. The current analyses were approved by the Northeastern University Institutional Review Board.
Variables
Mental Health Outcomes (measured in 2002)
Past-month psychological distress was measured by survey using the Kessler K-6 scale (K6), a broad-gauged dimensional screening scale for mental illness28. K6 includes 5-item Likert answers (none, to all of the time during the past 30 days) for 6 items: so depressed nothing could cheer you up; nervous; restless or fidgety; hopeless; everything was an effort; worthless. We scored the K6 with two-parameter binary Item Response Theory (IRT) latent variable methods, recoding each item into a set of ordered dichotomies, and outputing a standardized factor score 28. For observations missing scale items (<3%) we calculated row-column imputed values. (Cronbach’s Alpha 0.80, mean (SD) = −0.0395 (1.123)). Given standardization, intervention effect sizes correspond approximately to the proportion of a SD-change in the outcome.
Behavior problems were measured by 11 self-reported survey items adapted from the Behavior Problems Index (BPI)29 primarily assessing externalizing behaviors. Responses for items such as “I lie or cheat” and “I have a hot temper” ranged from 0 (not true) to 2 (often true). Standardized BPI scores were estimated with two-parameter binary IRT models (alpha=0.80, mean (SD) = −.0250 (1.086)).
In supplemental analyses, we report outcomes for past-12 month and lifetime DSM-IV major depressive disorder (MDD). MDD was assessed by survey questions adapted from the National Comorbidity Survey Replication: Adolescent Supplement (NCS-A), implemented by trained lay interviewers. The lay-administered NCS-A displays good concordance with clinically-administered interviews such as the Schedule for Affective Disorders and Schizophrenia for School age Children,30 both of which seek to assess DSM diagnoses. The algorithm to derive MDD is described in Appendix e-text 1. Because of the low prevalence of 12-month MDD (.029) and lifetime MDD (.046), we report detailed results in online appendices e-Figures 1 and 2. We focus on past-year (vs. lifetime) MDD because within the context of a trial, the past-year measure captures MDD during a period that follows random assignment, preserving temporal order between exposure and outcome31. Moreover, results for past-year MDD have not been published within MTO.
Randomly-assigned treatment was modeled with one dichotomous variable: intervention vs. control group. Although the study contained 2 experimental intervention groups, intervention effects on mental health were statistically indistinguishable across experimental arms (vs. controls); therefore we combined the experimental groups to facilitate the presentation. However, Results retaining the original three intervention groups are presented in appendices e-Figures 3–5.
Intervention adherence for families in the experimental groups was defined as using the rental subsidy voucher to lease an apartment10, 15 (as opposed to random assignment, which provided an offer of a voucher). Many control and experimental families later moved away from public housing using other means besides the MTO voucher. Based on intent-to-treat (ITT) principles, these families are classified according to their original randomly-assigned exposure.
Modification of the effect of intervention on mental health was evaluated using pre-randomization covariates indicating gender (specified based on prior MTO results) and separately, family health-related vulnerability (specified a priori before our team had access to the data). Health vulnerability was operationalized with a family-level binary variable indicating any household member had a disability, or that a household child had any of four health or developmental problems: behavioral problems, learning problems, problems that made it difficult to get to school and/or to play active games, problems that required special medicine and/or equipment. We additionally hypothesized that violent crime victimization, and socioeconomic position modified the intervention effect, and these results are presented elsewhere. We stratified results here by site.
Covariates
We adjusted regression models for site and several pre-randomization covariates including demographic variables, and those significantly associated with the outcome, to increase precision32: adolescent age, black race (parent-reported in pre-specified categories; collected to monitor racial disparities in fair housing), gifted student, and whether the school asked to discuss the child’s schoolwork or behavior problems; and household head marital status, employment status, education, neighborhood stability, relationships with neighbors, presence of family or friends in neighborhood, and prior application to Section 8. The small proportion of missing baseline covariate data was imputed to site-specific means10. Results were statistically comparable in models with or without covariate adjustment..
Analytic Approach
Primary analyses were based on ITT principles33. We regressed mental health outcomes on the intervention arm indicator variable with covariate-adjusted linear (for K6 and BPI) or logistic (for MDD) regression. Approximately half (51%) of families randomized to receive rental subsidy vouchers did not adhere to the assigned intervention (to use the voucher to move) and remained in public housing, so the ITT effect estimate is likely attenuated, compared to the effect of using the voucher to move. When effect modification tests were statistically significant in ITT analyses, we also present adherence-adjusted effect estimates based on instrumental variable (IV) analysis, estimated with two-stage least squares regression. IV analysis is appropriate to correct for non-random adherence in RCTs because IV avoids biases associated with directly comparing compliers to non-compliers34, 35.
Using ITT regression analysis, we first evaluated the intervention effect averaged over all youth. Next, we assessed modification of the intervention effect on mental health by gender, using a gender-by-intervention interaction. We then assessed whether family health-related vulnerability modified the intervention effect by evaluating an intervention-by-vulnerability interaction. This allowed us to formally test the primary novel hypothesis that the intervention effect on mental health was modified by family vulnerability. To assess the robustness of our findings to omitted higher order interactions, a three-way interaction involving the intervention, gender, and baseline health-vulnerability variables was included but did not alter the results. For clarity, effect modification is displayed graphically (Figures 2–3) as average intervention effects on mental health (experimental minus control differences on the absolute scale) and corresponding 95% confidence intervals (CI), separately for each subgroup: girls from health-vulnerable families; girls not from vulnerable families; boys from vulnerable families; and boys not from vulnerable families. Negative values for intervention effect coefficients indicate beneficial intervention effects, while positive values indicate adverse effects. We exponentiated coefficients output from logistic regression into odds ratios (OR) and corresponding 95% CI’s; MDD was rare, so the OR estimates the risk ratio. We present the risk difference (RD) and its 95% CI for intervention vs. controls based on marginal predicted probabilities output from logistic models. To confirm that the overall pattern of intervention effect heterogeneity is not merely driven by lower adherence rates among vulnerable families,22, 23 we also estimated adherence-adjusted effects using IV analyses for distress and BPI.
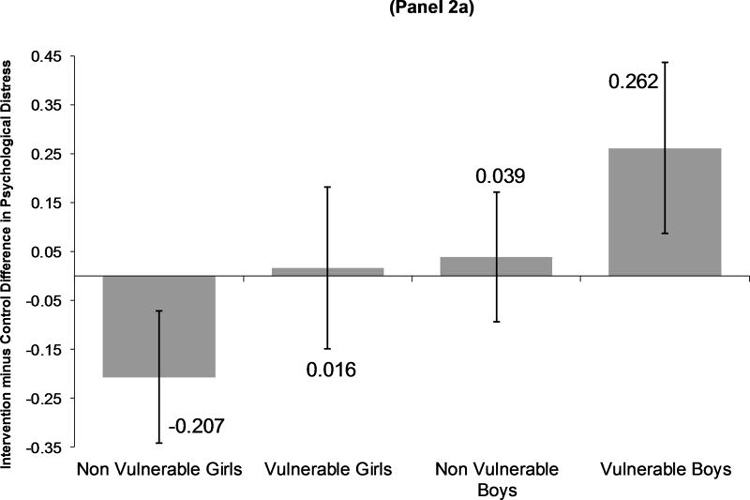
Figure 2. (Panel). MTO Intervention Effects on Mean Difference in Psychological Distress 4–7 Years After Baseline, Modified by Gender & Health Vulnerability.
Panel 2a presents the Linear Regression Intent to Treat (ITT) estimates. Panel 2b presents adherence-adjusted estimates of intervention effects from 2nd stage instrumental variable (IV) analysis. The primary hypothesis test tested whether the intervention-health vulnerability interaction coefficient was significantly different from zero. Intervention-health vulnerability interaction results for ITT: B(SE)=.223(.092), p=.02, CI(.042, .404), and for IV: B(SE)=.478(.192), p=.01, CI(.102, .854). Models adjusted for covariates listed in Table 2, plus intervention-baseline health vulnerability interaction. Subgroup sample size is n=875 for non-vulnerable girls, n=551 for vulnerable girls, n=761 for non-vulnerable boys, and n=642 for vulnerable boys.
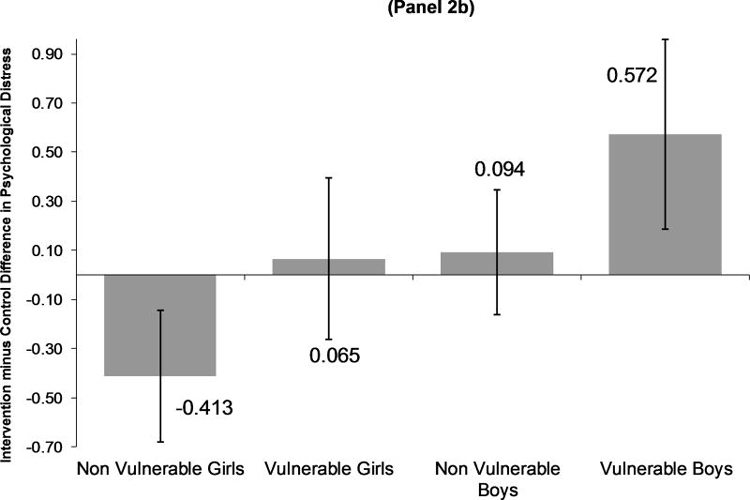
Figure 3. MTO Intervention Effects on Mean Difference in Behavior Problems 4–7 Years After Baseline, Modified by Gender & Health Vulnerability.
Panel 3a presents the Linear Regression Intent to Treat (ITT) estimates. Panel 3b presents adherence-adjusted estimates of intervention effects from 2nd stage instrumental variable (IV) analysis. The primary hypothesis test tested whether the intervention-health vulnerability interaction coefficient was significantly different from zero. Intervention-health vulnerability interaction results for ITT: B(SE)=.122(.090), p=.17, CI(−.054, .298), and for IV: B(SE)=.279(.183), p=.13, CI(−.079, .638). Models adjusted for covariates listed in Table 2, plus intervention-baseline health vulnerability interaction. Subgroup sample size is n=875 for non-vulnerable girls, n=551 for vulnerable girls, n=761 for non-vulnerable boys, and n=642 for vulnerable boys.
All analyses were weighted to account for time-changing random assignment ratios and nonresponse, and account for household clustering (using STATA’s clustered sandwich estimator) since up to two children per household were randomly sampled at interim follow-up10. We report robust standard errors with p-values from 2-sided tests. We used M-Plus 6.11 for IRT analyses and STATA 11.0 for all other analyses.
RESULTS
The MTO adolescents were 50% male, 63% African American, 30% Hispanic and 43% lived in families with baseline health vulnerabilities (Table 1). Youth lived in neighborhoods (tracts) that were 49.8% poor at baseline, while in 2002, mean neighborhood poverty was significantly lower for intervention youth vs. controls (mean neighborhood poverty: low-poverty-neighborhood group 31.4%, regular section 8 group 32.2%, controls 39.2%, F-test p<0.001).
Table 1.
Moving to Opportunity Youth, Baseline Variables, Overall and by Intervention Group.
| Construct | Variable | Overall | Intervention Group
|
||
|---|---|---|---|---|---|
| Low Poverty Neighborhood Section 8 | Geographically Unrestricted Section 8 | Controls | |||
| Total in Interim Survey in 2002 | N | 2829 | 1164 | 786 | 879 |
| Baseline mean poverty rate | Tract percent poverty rate at baseline (1990 values) | 49.8% | 49.6% | 49.5% | 50.5% |
| Family Characteristics | |||||
| Health | Household member had disability, health or developmental problem | 43.0% | 45.5% | 41.1% | 41.5% |
| Household member had a disability | 17.2% | 18.1% | 17.3% | 15.8% | |
| Site | Baltimore | 15.5% | 15.6% | 16.6% | 14.2% |
| Boston | 18.9% | 16.4% | 20.5% | 20.7% | |
| Chicago | 22.4% | 23.7% | 22.7% | 20.4% | |
| Los Angeles | 18.6% | 18.7% | 15.8% | 21.2% | |
| New York | 24.6% | 25.7% | 24.3% | 23.5% | |
| Household size | 2 people | 7.3% | 7.1% | 6.5% | 8.3% |
| 3 people | 22.3% | 22.6% | 21.4% | 22.9% | |
| 4 people | 25.4% | 26.6% | 25.7% | 23.4% | |
| 5 or more people | 45.0% | 43.7% | 46.4% | 45.4% | |
| Youth Characteristics | |||||
| Age (in years) | 9.94 | 9.98 | 9.95 | 9.88 | |
| Gender | Male | 49.9% | 48.0% | 51.5% | 51.0% |
| Female | 50.1% | 52.0% | 48.5% | 49.0% | |
| Race/ethnicity | African American | 62.8% | 63.5% | 62.7% | 62.1% |
| Hispanic ethnicity, any race | 30.0% | 30.1% | 30.5% | 29.5% | |
| White | 1.1% | 0.9% | 1.2% | 1.2% | |
| Other race | 2.2% | 2.3% | 2.4% | 1.9% | |
| Missing race | 3.8% | 3.2% | 3.2% | 5.3% | |
| Gifted | Special class for gifted students or did advanced work | 15.4% | 14.0% | 15.8% | 16.8% |
| Developmental Problems | Special school, class, or help for learning problem in past 2 years | 16.6% | 17.4% | 15.8% | 16.3% |
| Special school, class, or help for behavioral or emotional problems in past 2 years | 7.7% | 8.3% | 9.3% | 5.3% | |
| Problems that made it difficult to get to school and/or to play active games | 6.5% | 7.1% | 7.1% | 5.0% | |
| Problems that required special medicine and/or equipment | 9.1% | 9.1% | 11.3% | 7.0% | |
| School asked to talk about problems child having with schoolwork or behavior in past 2 years | 26.3% | 26.3% | 27.2% | 25.4% | |
| Household Head Characteristics | |||||
| Family Structure | Never married | 55.9% | 55.2% | 55.1% | 57.5% |
| Teen parent | 25.9% | 26.6% | 26.1% | 25.0% | |
| Socioeconomic Status | Employed | 25.8% | 28.3% | 23.1% | 25.3% |
| On AFDC (welfare) | 76.0% | 75.9% | 75.1% | 76.9% | |
| Education | Less than high school | 47.1% | 49.0% | 44.9% | 46.7% |
| High school diploma | 36.2% | 36.0% | 37.5% | 35.3% | |
| GED | 16.7% | 15.0% | 17.7% | 17.9% | |
| In School | 13.9% | 13.0% | 16.4% | 12.6% | |
| Neighborhood/Mobility Variables | Lived in neighborhood 5 or more years | 65.7% | 62.9% | 69.8% | 65.5% |
| No family living in neigh | 64.1% | 65.3% | 60.2% | 66.3% | |
| No friends living in neigh | 37.3% | 39.6% | 32.9% | 38.5% | |
| Had applied for section 8 voucher before | 44.3% | 46.0% | 40.3% | 45.8% | |
| Neighbor Relationships | Chats with neighbors at least once a week | 51.9% | 51.0% | 51.5% | 53.2% |
| Respondent very likely to tell neighbor if saw neighbor’s child getting into trouble | 56.7% | 57.1% | 56.5% | 56.4% | |
NOTE: All variables range between 0 & 1 except baseline age (5–16) and mean poverty rate. Analysis weighted for varying intervention random assignment ratios across time, and for attrition. Test of intervention group differences were Wald statistics outputted from logistic regression for dichotomous baseline characteristics and multinomial logistic regression for categorical characteristics. F-tests were used with linear regression for continuous variables. All tests were adjusted for clustering at the family level; the null hypothesis was that none of the 3 intervention group proportions or means differed. Intervention group proportions differed significantly at p<.05 for special school/class/help for behavioral/emotional problems.
ITT estimates of the marginal effect of the MTO intervention on psychological distress were not significant(B=0.012 (95% CI: −0.077, 0.102)), and on BPI were marginally harmful (B=0.075 (CI: −0.012, 0.162)). These average effects masked qualitative effect modification by gender (intervention-gender interaction for K6 B=0.265, CI: 0.097, 0.433, p=.002; for BPI B=0.210, CI:0.050, 0.371, p=.01). Randomization to the experimental intervention was significantly beneficial for girls’ distress (B= −0.121, CI: −0.241, −0.002, p=.05), significantly harmful for boys’ distress (B=0.143, CI: 0.018, 0.268, p=.03) and significantly harmful for boys’ BPI (B=0.179, CI:0.060, 0.298, p=.003). No statistical association was found relating the MTO intervention with girls’ BPI. (Table 2).
Table 2.
Moving to Opportunity Intervention Effects at Interim (4–7 Year) Follow Up on Mental Health among Adolescents, Effect Modification by Gender.
| Psychological Distress
|
Behavior Problems
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ITT a
|
Adherence-Adjusted b
|
ITT a
|
Adherence-Adjusted b
|
|||||||||||||
| Beta | SE | CI c | p | Beta | SE | CI c | p | Beta | SE | CI c | p | Beta | SE | CI c | p | |
| Regression Coefficients | ||||||||||||||||
| Intervention | −.121 | .061 | (−.241, −.002) | .05* | −.232 | .116 | (−.460, −.004) | .05* | −.031 | .060 | (−.148, .085) | .60 | −.061 | .113 | (−.283, .161) | .59 |
| Male | −.403 | .069 | (−.539, −.267) | <.001*** | −.400 | .068 | (−.534, −.266) | .000*** | −.079 | .067 | (−.211, .053) | .24 | −.077 | .067 | (−.207, .054) | .25 |
| Intervention*Male Interaction | .265 | .086 | (.097, .433) | .002** | .527 | .170 | (.193, .861) | .002** | .210 | .082 | (.050, .371) | .01** | .427 | .163 | (.107, .746) | .009** |
| Calculated Intervention Effects | ||||||||||||||||
| Girls | −.121 | .061 | (−.241, −.002) | .05* | −.232 | .116 | (−.460, −.004) | .05* | −.031 | .060 | (−.148, .085) | .60 | −.061 | .113 | (−.283, .161) | .59 |
| Boys | .143 | .064 | (.018, .268) | .03* | .295 | .130 | (.041, .549) | .02* | .179 | .061 | (.060, .298) | .003** | .366 | .124 | (.122, .609) | .003** |
ITT=Intent to Treat models run with linear regression adjusted for survey design.
Adherence Adjusted Estimates are estimated with Instrumental Variable Models adjusted for the survey design, 2nd stage estimates reported here.
CI=95% Confidence Interval for the mean
NOTES: Regression models adjusted for age, site, race (black, vs. Hispanic or non-hispanic white), household head marital status (single vs. not), currently working, education (GED, high school graduate, vs. less than high school), still in school, lived in neighborhood for 5 years or more, chats with neighbor at least once a week, no family in neighborhood, no friends in neighborhood, very likely to tell neighbor if he/she saw neighbor’s child getting into trouble, has applied for section 8 before, child is gifted, child had problems with schoolwork or behavior, plus male, intervention, and intervention*male interaction. Models adjusted for family-level clustering, output with robust standard errors, and weighted. IRT methods used to derive psychological distress and behavior problems. “Calculated intervention effects” calculated from the regression coefficients from the interaction model.
Family health-related vulnerability significantly adversely modified the effect of MTO intervention on psychological distress among both girls and boys in ITT models (intervention-vulnerability interaction B = 0.223, CI: 0.042, 0.404, p=.02; Figure 2a). The modest average beneficial effect of intervention for girls reflected large benefits among girls from families without health-related vulnerabilities (B= −0.207, CI: −0.342, −0.071, p=.003) and small and nonsignificant effects among girls from families with health-related vulnerabilities (B=0.016, CI: −0.149, 0.182). The overall harmful distress effect among boys reflected substantial harm among boys from health-vulnerable families (B=0.262, CI:0.087, 0.437, p=.003) and small and non significant effects among boys not from health-vulnerable families (B=0.039, CI: −0.094, 0.172).
Baseline health vulnerability generated similar ITT effect modification patterns of MTO on BPI as for K6, although the effect modification tests for BPI were not significant (interaction B=0.122, CI: −0.054, 0.298, p=.17; Figure 3a).
Adherence-adjusted IV results were similar to ITT results for both K6 and BPI, with a marked gradient across the 4 subgroups. IV estimates for K6 indicate significant benefits among girls from non-vulnerable families, harmful effects among boys from vulnerable families, and no significant effects for the other two groups. IV estimates for BPI indicate no significant effects among girls, and statistically significant adverse effects among boys, with larger adverse effects for boys from vulnerable families (Figure 2b, Figure 3b). IV effect estimates are about twice as large as ITT estimates.
For past-12 month MDD, patterns were similar but estimates were imprecise because of low prevalence in experimental (2.7%) and control (3.4%) groups. The non-significant average ITT effect (Odds Ratio=0.73; CI:0.43, 1.23) masked a beneficial intervention effect for girls’ MDD on both relative (OR=0.56, CI: 0.31, 1.01 p=.05) and absolute scales (RD= −0.024, CI: −0.051, 0.003, p=.09), and non significant adverse intervention effects for boys. Effect modification by gender for 12-month MDD was not significant (interaction OR=2.42, CI: 0.63, 9.35 p=.20). (Appendix e-Table 1).
Examining patterns by family health-related vulnerability, non-vulnerable girls were the only subgroup to benefit for past-year MDD (OR=0.42, CI 0.20, 0.85 p=.02; RD=−0.037, CI: −0.076, 0.001 p=.06)(Appendix e-Figure 1). The other three subgroups displayed no significant intervention effects. The health vulnerability-intervention interaction was in the harmful direction, but not significant (B=0.810, CI: −0.275, 1.89, p=0.14).
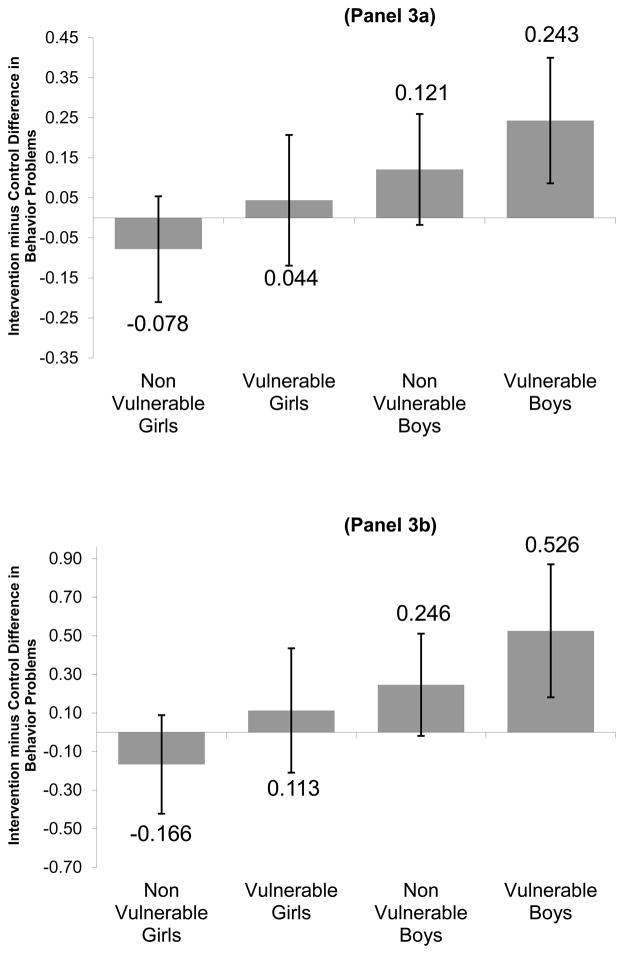
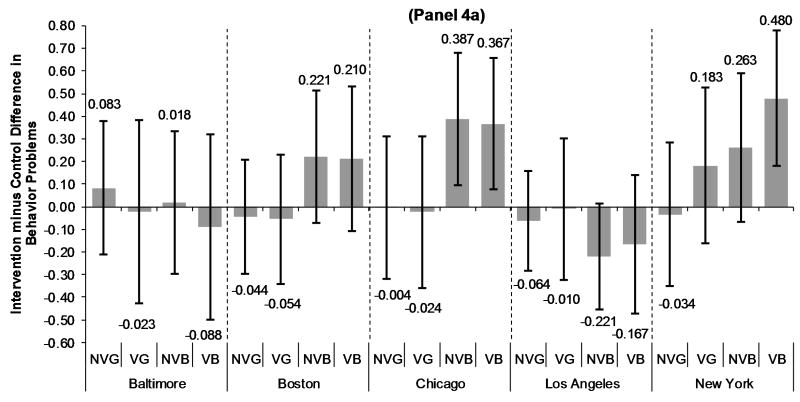
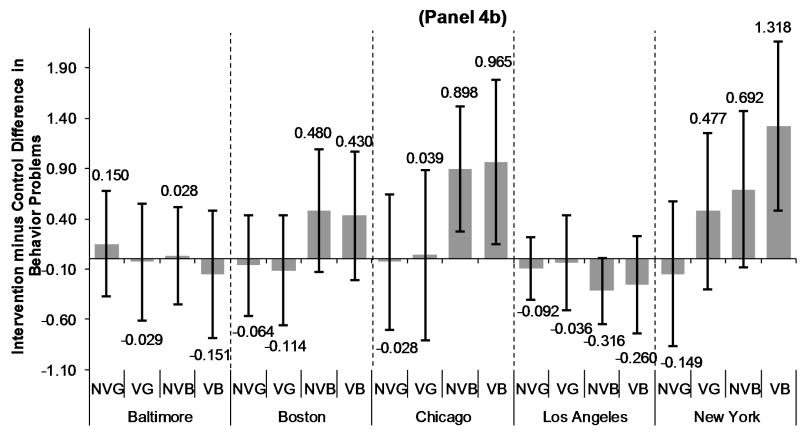
Although the pooled models for BPI show comparable patterns as for distress, BPI analyses stratified by site revealed considerable heterogeneity for boys (Figure 4), though confidence intervals are wide. New York seemed to drive the pooled BPI results; Chicago and Boston showed no differential adverse effect of vulnerability for boys; LA demonstrated strikingly-protective effects of the intervention on BPI that were marginally-significant for nonvulnerable boys. The patterns for distress were more consistent across sites (Appendix e-Figure 6).
Figure 4. MTO Intervention Effects on Mean Difference in Behavior Problems 4–7 Years After Baseline, Modified by Gender & Health Vulnerability, by Site.
Panel 4a presents the Linear Regression Intent to Treat (ITT) estimates by Site. Panel 4b presents adherence-adjusted estimates of intervention effects from 2nd stage instrumental variable (IV) analysis by Site. NVG=non-vulnerable girls, VG=vulnerable girls, NVB-non-vulnerable boys, and VB=vulnerable boys. The primary hypothesis test tested whether the intervention-health vulnerability interaction coefficient was significantly different from zero. Models adjusted for covariates listed in Table 2, plus intervention-baseline health vulnerability interaction. Subgroup sample size is: non-vulnerable girls n=145 for Baltimore, n=165 for Boston, n=193 for Chicago, n=193 for Los Angeles, and n=179 for New York; vulnerable girls n=79 for Baltimore, n=133 for Boston, n=113 for Chicago, n=56 for Los Angeles, and n=170 for New York; non-vulnerable boys n=136 for Baltimore, n=136 for Boston, n=161 for Chicago, n=191 for Los Angeles, and n=137 for New York; vulnerable boys n=88 for Baltimore, n=141 for Boston, n=134 for Chicago, n=90 for Los Angeles, and n=189 for New York.
COMMENT
We found heterogeneity in the mental health effects of moving to low poverty neighborhoods through the MTO program. Receipt of Section 8 housing vouchers had important mental health benefits for adolescent girls from families without health vulnerabilities. Unfortunately, the MTO program also apparently harmed the mental health of some adolescents, particularly boys from families with health vulnerabilities. The vulnerability hypothesis was supported-- the policy was more harmful or less beneficial for adolescents from more vulnerable families with health problems at baseline. The results for past-year MDD in the MTO study are presented for the first time here; although imprecise given the low MDD prevalence in this young population, the estimates from this diagnostic outcome suggest patterns similar to those of dimensional outcomes.
Results pooled across sites were similar using internalizing and externalizing measures, which is informative given gender differences in mental health manifestation and expression36, 37. However there was considerable variation across sites, particularly for boys’ BPI. Although site differences are not uncommon with social experiments (e.g. 38), we did not resolve what drove this heterogeneity. Relevant factors could include differential program implementation (e.g. variation in housing counseling services) or differential housing market conditions27.
Notably, the prior published results of the MTO experiment on Interim Survey psychological distress outcomes reported nonsignificant effects for boys 12–19.15 However, we find significant adverse intervention effects (p<.05) for this group. We believe the discrepancy is due to our improved operationalization of the K6 using IRT latent variable methods to reduce measurement error.33
Child development researchers posit different pathways through which neighborhood environment affects youth mental health39 based on ecologic theories emphasizing the influence of multiple contexts fostering youth development or psychopathology.40, 41 Hypothesized mechanisms include norms and social processes, relationships, and institutional resources. Living in disadvantaged contexts (i.e. poverty) may be associated with greater emotional distress for adolescents, due to the higher presence of stressors and fewer resources to buffer stress effects24, 42, 43. Developmental psychology and psychiatric epidemiology are increasingly incorporating social context, specifically factors at the neighborhood level, along with individual and family level explanations for youth mental health problems44. Focusing on context locates the sources of illness external to the child, implicating toxic environments that youth encounter, which often overwhelm the abilities of families to counteract the risk45.
The mental health benefit of social contexts may relate not only to social advantage of specific contexts, but also to the “fit” between individual and context 46. Such fit may differ by gender. For example, adolescent girls are more likely than boys to witness and experience community sexual violence47, 48; and sexual victimization and witnessing community violence are associated with depression48,47. Improved neighborhood safety from sexual violence may therefore contribute to the beneficial mental health intervention effects among girls. This is consistent with qualitative research among MTO participants showing that girls in high-poverty neighborhoods experienced pervasive sexual harassment and risk of sexual assault.49 This gendered dimension of safety may have been less relevant for boys, whereas the adjustment to new social networks in the new neighborhoods may have been more difficult for boys than for girls, for example due to the disruption of friendships or adult role models50. Other processes such as family structure, parental education, child’s education needs, or parental mental health may also be important moderators or mediators of the MTO intervention, based on prior evidence that these influence youth functioning44, 51. Although these explanations suggest directions for future work, we did not test them in this analysis, and therefore we do not know what accounts for these different intervention effects.
Certain child developmental stages may be sensitive periods52 during which exposure to certain neighborhood environments may imprint expression of later-life mental health, and these sensitive periods may differ by gender. Indeed, leading researchers have hypothesized that some experimental psychosocial interventions failed to improve health because the intervention was delivered after the relevant etiologic period53. Therefore future research should leverage MTO and other longitudinal studies to test life course theories to inform future housing interventions.
Establishing that neighborhoods causally affect adolescent mental health is challenging, because the vast majority of such studies use observational, cross-sectional designs. Therefore, prior research may be biased due to unmeasured confounding (by family characteristics such as socioeconomic status, or mobility-related residential selection), reverse causality, or violations of other causal inference assumptions.54, 55 Experimental designs alleviate some of the most serious threats to internal validity by balancing confounders across experimental groups at baseline and establishing temporal sequencing between exposure and outcome.56 MTO is the only study measuring mental health to date that randomly assigned individuals to receive different neighborhood contexts via offers to move with housing vouchers; this experimental design is strong for assessing whether moves from public to private housing may cause mental health, especially since MTO reduced exposure to neighborhood poverty.
Even then, experiments are not a panacea for understanding neighborhood effects.57–59 The MTO experiment resulted in a number of bundled “treatments” that changed for families, including not only the housing voucher, but also the move from public housing to private rental housing, the move from very poor to lower poverty neighborhoods, and housing unit quality improvement15. Analyses comparing the importance of these alternative mechanisms are potentially valuable for both theoretical understanding, and design of future interventions. Future housing experiments would benefit from conceptualizing how to separate these relevant processes analytically or through study design to inform the most important mediators of the (bundled) intervention effect.
Policy experts recommend two strategies to improve neighborhood environments for individuals: people-based interventions (like housing mobility vouchers) that help households acquire housing in better neighborhoods, and place-based interventions that improve conditions in disadvantaged neighborhoods.5, 6, 60 MTO used a people-based housing mobility intervention, modeled on Section 8 vouchers (now called Housing Choice Vouchers (HCV)); HCVs constitute the largest US federal affordable housing program61, accounting for approximately 40% of HUD’s recent annual budgets62. MTO did not focus on place-based improvement of disadvantaged neighborhoods, so we cannot infer that interventions such as neighborhood improvement initiatives would achieve similar effects as those in MTO. However, MTO is policy relevant given its mechanism of vouchers and therefore broadens the scope of potential interventions that may improve access to better neighborhoods.5
The demographic group apparently harmed by the MTO intervention -- low-income, predominantly racial/ethnic minority, adolescent boys -- is among the most vulnerable populations in the United States, with poor long-term health outcomes63. These findings therefore merit special attention to understand why these adolescents fared worse in the intervention group, whether this heterogeneity extends to other subgroups, and how clinical, social, or policy interventions can remediate this harm. Families receiving federal rental assistance are typically in extreme need, so reducing HCV housing support is not an appropriate response.
MTO was designed in the housing sector, without awareness that it would affect health, or that its effects would be modified by baseline health or gender. Our findings suggest that additional supportive services may be required to help vulnerable adolescents succeed in the context of residential moves, even when moving to seemingly better neighborhood environments. Children from health-vulnerable families may not be able to take advantage of the potential opportunities afforded by moves outside of public housing. These relationships between health and housing strongly suggest the need for more intersectoral collaboration, including for example, incorporating the type of resident supportive services required under the HOPE VI housing relocation program, including case management, and linkage to health care access or educational services, tailored to residents’ needs.64, 65 Housing mobility programs may also benefit from integrating services with medical-legal partnerships, which serve the needs of low-income households in health care settings by combining medical care with other unmet service needs (e.g. legal counseling, housing, and income support)66; such a multipronged approach is promising for addressing both prevention and treatment of mental health and housing problems. Moreover, future housing programs may benefit from measuring health and various forms of psychopathology or symptomatology, at baseline and follow-up, to identify and target health-vulnerable populations who may benefit from additional services.
Our results suggest factors shaping mental health may differ for different groups, since MTO’s mental health effects differed by gender and baseline health. Potential mental health benefits of residential moves may be counteracted by the difficulties faced by adolescents in families with health vulnerabilities. Existing health or developmental problems may be more important chronic stressors for causing mental illness than neighborhood environment. However in adolescents from families without these vulnerabilities, the relative importance of neighborhood context as a cause of mental illness may emerge67.
Limitations
The low prevalence of past year MDD limited power to test intervention effects on disorder, although patterns were similar to those for K6 and BPI. Assessing effects of context with dimensional measures of symptomatology are appropriate for population or community assessment if the effects of social context are nonspecific.68, 69
This study population comprised very-low income, minority adolescents living in extremely distressed, high-poverty neighborhoods. Our findings therefore may not be generalizable to other populations. However, this population is a high priority for targeting health care services and improvements in population health because over their life course they experience high morbidity in many domains64, 70.
Although the 51% intervention adherence in this study could attenuate the ITT effect estimates compared to the actual effect of moving, we used IV to model adherence-adjusted estimates. The IV results mirrored ITT results, but were twice as large, suggesting that differential take-up to use the Section 8 policy did not explain the effect modification patterns. IV interpretations rest on several assumptions, including that intervention assignment can only affect mental health indirectly, mediated by use of the voucher to move71. This assumption is more credible in randomized trials such as MTO than in quasi-experimental studies, but cannot be confirmed empirically. The Stable Unit Treatment Variable Assumption (SUTVA) is another assumption Which generally holds when programs (like MTO) are small scale relative to the community.71 With additional assumptions, IV effect estimates are generally interpreted as referring to specific subpopulations, for example, those who used a voucher to move71.
Compliance was defined by original investigators as using MTO Section 8 vouchers to move to private rental apartments. By design, control group members could not access MTO vouchers, so they could not take up the intervention.10 However, redefining take-up as moving away from public housing would reduce estimated adherence because some control group members moved without MTO vouchers.
CONCLUSION
This housing policy experiment benefited mental health of some adolescents, particularly girls in families without health vulnerabilities, but had either nonsignificant or harmful effects on mental health of adolescents from families with pre-existing health-related vulnerabilities, particularly boys. The questions raised in this analysis should be explored in the 10–15 year MTO follow-up. The implications of the findings may guide future housing policy, insofar as children from health-vulnerable families may require additional support or services during and after moves. These findings may, moreover, help improve understanding of the etiology of adolescent mental illness. Clinically, it is important to understand which adolescents are at special risk of poor mental health outcomes in the context of residential moves.
Supplementary Material
Acknowledgments
Funding & Sponsors: This work was supported by NIH grants 1R01MD006064-01 and 1R21HD066312-01 (Dr. Osypuk, PI). The NIH had no role in the analysis, preparation, or writing of this manuscript, or in the decision to submit the paper for publication. The US Department of Housing and Urban Development reviewed the manuscript to ensure respondent confidentiality was maintained in the presentation of results.
Abbreviations
- MDD
Major Depressive Disorder
- MTO
Moving to Opportunity
- CI
Confidence Interval
Footnotes
Presentation: Preliminary findings in this manuscript were presented at the 3rd North American Congress of Epidemiology Meeting, June 2011, and at the Population Association of America annual meeting, April 2011.
Author Contributions: Dr. Osypuk had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis, and had final responsibility for the decision to submit for publication. Dr. Osypuk conceived the hypotheses, obtained the data, conducted the majority of the data analysis, and wrote the majority of the manuscript. Dr. Glymour aided in writing the paper. Drs. Glymour and Tchetgen-Tchetgen advised on the statistical analysis and interpretation of findings, in addition to writing and editing considerable portions of the methods. Dr. Earls advised on the statistical analysis and interpretation of findings. Drs. Earls, Lincoln, and Acevedo-Garcia advised on the interpretation of findings and edited the paper. Dr. Schmidt assisted with data analysis and edited the paper. We thank Dr. Sandro Galea for helpful comments on a previous version of the manuscript.
Conflicts of Interest: The authors do not have any conflicts of interest to declare.
References
- 1.Kessler RC, Foster CL, Saunders WB, Stang PE. Social consequences of psychiatric disorders, I: educational attainment. Am J Psychiatry. 1995;152:1026–1032. doi: 10.1176/ajp.152.7.1026. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 3.Brodbeck J, Vilén U, Bachmann M, Znoj H, Alsaker F. Sexual risk behavior in emerging adults: gender-specific effects of hedonism, psychosocial distress, and sociocognitive variables in a 5-year longitudinal study. AIDS Educ Prev. 2010;22(2):148–159. doi: 10.1521/aeap.2010.22.2.148. [DOI] [PubMed] [Google Scholar]
- 4.Kaplan HB, Damphousse KR. Reciprocal relationships between life events and psychological distress. Stress Medicine. 1997;13(2):75–90. [Google Scholar]
- 5.Osypuk TL, Acevedo-Garcia D. Beyond individual neighborhoods: a geography of opportunity perspective for understanding racial/ethnic health disparities. Health Place. 2010;16(6):1113–1123. doi: 10.1016/j.healthplace.2010.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Acevedo-Garcia D, Osypuk TL, McArdle N, Williams D. Toward a policy-relevant analysis of geographic and racial/ethnic disparities in child health. Health Aff. 2008;27(2):321–333. doi: 10.1377/hlthaff.27.2.321. [DOI] [PubMed] [Google Scholar]
- 7.Leventhal T, Dupéré V, Gunn JB. Neighborhood influences on adolescent development. In: Lerner RM, Steinberg L, editors. Handbook of Adolescent Psychology, Volume 2, Contextual Influences on Adolescent Development. 3. Hoboken, NJ: Wiley; 2009. pp. 411–443. [Google Scholar]
- 8.Aneshensel C, Sucoff C. The neighborhood context of adolescent mental health. J Health Soc Behav. 1996;37:293–310. [PubMed] [Google Scholar]
- 9.Mair C, Diez Roux AV, Galea S. Are neighbourhood characteristics associated with depressive symptoms? A review of evidence. J Epidemiol Community Health. 2008;62(11):940–946. doi: 10.1136/jech.2007.066605. [DOI] [PubMed] [Google Scholar]
- 10.Kling JR, Liebman JB, Katz LF. Experimental analysis of neighborhood effects. Econometrica. 2007;75(1):83–119. [Google Scholar]
- 11.Leventhal T, Brooks-Gunn J. Moving to Opportunity: an experimental study of neighborhood effects on mental health. Am J Public Health. 2003;93(9):1576–1582. doi: 10.2105/ajph.93.9.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schoeni RF, House JS, Kaplan GA, Pollack H. Making Americans Healthier: Social and Economic Policy As Health Policy. New York: Russell Sage; 2008. [Google Scholar]
- 13.Herd P, Schoeni RF, House JS. Upstream solutions: does the supplemental security income program reduce disability in the elderly? Milbank Q. 2008;86(1):5–45. doi: 10.1111/j.1468-0009.2007.00512.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Strully KW, Rehkopf DH, Xuan Z. Effects of prenatal poverty on infant health: state earned income tax credits and birth weight. Am Sociol Rev. 2010;75(4):534–562. doi: 10.1177/0003122410374086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Orr L, Feins JD, Jacob R, Beecroft E, Sanbonmatsu L, Katz LF, Liebman JB, Kling JR. Moving to Opportunity for Fair Housing Demonstration Program: Interim Impacts Evaluation. Washington, DC: US Dept of HUD; 2003. [Google Scholar]
- 16.Fortson JG, Sanbonmatsu L. Child health and neighborhood conditions: results from a randomized housing voucher experiment. J Hum Resour. 2010;45(4):840–864. [Google Scholar]
- 17.Ludwig J, Sanbonmatsu L, Gennetian L, Adam E, Duncan GJ, Katz LF, Kessler RC, Kling JR, Lindau ST, Whitaker RC, McDade TW. Neighborhoods, obesity, and diabetes: a randomized social experiment. N Engl J Med. 2011;365(16):1509–1519. doi: 10.1056/NEJMsa1103216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Acevedo-Garcia D, Osypuk TL, Werbel RE, Meara ER, Cutler DM, Berkman LF. Does housing mobility policy improve health? Housing Policy Debate. 2004;15(1):49–98. [Google Scholar]
- 19.Ertel KA, Glymour MM, Glass TA, Berkman LF. Frailty modifies effectiveness of psychosocial intervention in recovery from stroke. Clin Rehabil. 2007;21(6):511–522. doi: 10.1177/0269215507078312. [DOI] [PubMed] [Google Scholar]
- 20.McCormick MC, Brooks-Gunn J, Buka SL, Goldman J, Yu J, Salganik M, Scott DT, Bennett FC, Kay LL, Bernbaum JC, Bauer CR, Martin C, Woods ER, Martin A, Casey PH. Early intervention in low birth weight premature infants: results at 18 years of age for the infant health and development program. Pediatrics. 2006;117(3):771–780. doi: 10.1542/peds.2005-1316. [DOI] [PubMed] [Google Scholar]
- 21.McCormick MC, McCarton C, Brooks-Gunn J, Belt P, Gross RT. The infant health and development program: interim summary. J Dev Behav Pediatr. 1998;19(5):359–370. doi: 10.1097/00004703-199810000-00009. [DOI] [PubMed] [Google Scholar]
- 22.Snell EK, Duncan GJ. Child characteristics and successful use of housing vouchers: estimates from the moving to opportunity demonstration. Housing Policy Debate. 2006;17(4):727–754. [Google Scholar]
- 23.Shroder M. Locational constraint, housing counseling, and successful lease-up in a randomized housing voucher experiment. Journal of Urban Economics. 2002;51:315–338. [Google Scholar]
- 24.Pearlin LI. The sociological study of stress. J Health Soc Behav. 1989;30(3):241–256. [PubMed] [Google Scholar]
- 25.US Department of Housing & Urban Development. First Biennial Report to Congress, Moving to Opportunity for Fair Housing Demonstration Program. Apr, 1996. Expanding Housing Choices For HUD-Assisted Families: Moving to Opportunity. [Google Scholar]
- 26.Feins JD, McInnis D. The Interim Impact Evaluation for the Moving to Opportunity Demonstration, C-OPC-21484. Cambridge, MA: Abt Associates Inc; 2001. [Google Scholar]
- 27.Goering J, Kraft J, Feins J, McInnis D, Holin MJ, Elhassan H. Moving to Opportunity for Fair Housing Demonstration Program: Current Status and Initial Findings. Washington, DC: US Department of Housing & Urban Development, Office of Policy Development and Research; 1999. [Google Scholar]
- 28.Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SL, Walters EE, Zaslavsky AM. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(06):959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- 29.Zill N. Behavior Problems Index Based on Parent-Report. Washington, DC: Child Trends; 1990. [Google Scholar]
- 30.Kessler R, Avenevoli S, Green JG, Gruber MJ, Guyer M, He Y, Jin R, Kaufman J, Sampson NA, Zaslavsky AM, Merikangas KR. National Comorbidity Survey Replication Adolescent Supplement (NCS-A): III. concordance of DSM-IV/CIDI diagnoses with clinical reassessments. J Am Acad Child Adolesc Psychiatry. 2009;48:386–399. doi: 10.1097/CHI.0b013e31819a1cbc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kramer M, Von Korff M, Kessler L. The lifetime prevalence of mental disorders: estimation, uses and limitations. Psychol Med. 1980;10:429–435. doi: 10.1017/s0033291700047310. [DOI] [PubMed] [Google Scholar]
- 32.Tsiatis AA, Davidian M, Zhang M, Lu X. Covariate adjustment for two-sample treatment comparisons in randomized clinical trials: a principled yet flexible approach. Statistics in Medicine. 2008;27:4658–4677. doi: 10.1002/sim.3113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kleinbaum DG, Sullivan KM, Barker ND. A Pocket Guide to Epidemiology. New York: Springer; 2007. [Google Scholar]
- 34.Newhouse JP, McClellan M. Econometrics in outcome research: the use of instrumental variables. Annu Rev Public Health. 1998;19:17–34. doi: 10.1146/annurev.publhealth.19.1.17. [DOI] [PubMed] [Google Scholar]
- 35.Angrist JD, Imbens GW, Rubin DB. Identification of causal effects using instrumental variables. Journal of the American Statistical Association. 1996;91(434):444–455. [Google Scholar]
- 36.Rosenfield S. Gender and mental health, do women have more psychopathology, men more, or both the same (and why)? In: Horwitz AV, Scheid TL, editors. A handbook for the study of mental health, social contexts, theories, and systems. Cambridge: Cambridge University Press; 1999. pp. 348–360. [Google Scholar]
- 37.Schwartz S, Meyer IH. Mental health disparities research: the impact of within and between group analyses on tests of social stress hypotheses. Soc Sci Med. 2010;70:1111–1118. doi: 10.1016/j.socscimed.2009.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hamilton G, Freedman S, Gennetian L, Michalopoulos C, Walter J, Adams-Ciardullo D, Gassman-Pines A, McGroder S, Zaslow M, Ahluwalia S, Brooks J, Small E, Ricchetti B. How Effective Are Different Welfare-to-Work Approaches? Five-Year Adult and Child Impacts for Eleven Programs. New York, NY: Manpower Demonstration Research Corporation and Child Trends; 2001. [Google Scholar]
- 39.Leventhal T, Brooks-Gunn J. The neighborhoods they live in: the effects of neighborhood residence on child and adolescent outcomes. Psychol Bull. 2000;126(2):309–337. doi: 10.1037/0033-2909.126.2.309. [DOI] [PubMed] [Google Scholar]
- 40.Bronfenbrenner U. Reality and research in the ecology of human development. Proc Am Philos Soc. 1975;119(6):439–469. [Google Scholar]
- 41.Boyce WT, Frank E, Jensen PS, Kessler RC, Nelson CA, Steinberg L. Social context in developmental psychopathology: recommendations for future research from the MacArthur Network on Psychopathology and Development. Dev Psychopathol. 1998;10:143–164. doi: 10.1017/s0954579498001552. [DOI] [PubMed] [Google Scholar]
- 42.Aneshensel CS. Social stress: theory and research. Annual Review of Sociology. 1992;18:15–38. [Google Scholar]
- 43.Brooks-Gunn J, Duncan GJ, Aber JL. Neighborhood Poverty: Context and Consequences for Children. I. New York: Russell Sage; 1997. [Google Scholar]
- 44.Merikangas KR, Nakamura EF, Kessler RC. Epidemiology of mental disorders in children and adolescents. Dialogues in Clin Neurosci. 2009;11(1):7–20. doi: 10.31887/DCNS.2009.11.1/krmerikangas. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Roosa MW, Jones S, Tein J-Y, Cree W. Prevention science and neighborhood influences on low-income children’s development: theoretical and methodological issues. Am J Community Psychol. 2003;31(1–2):55–72. doi: 10.1023/a:1023070519597. [DOI] [PubMed] [Google Scholar]
- 46.Veling W, Susser E, van Os J, Mackenbach JP, Selten J-P, Hoek HW. Ethnic density of neighborhoods and incidence of psychotic disorders among immigrants. Am J Psychiatry. 2008;165(1):66–73. doi: 10.1176/appi.ajp.2007.07030423. [DOI] [PubMed] [Google Scholar]
- 47.Foster J, Kuperminc GP, Price AW. Gender differences in posttraumatic stress and related symptoms among inner-city minority youth exposed to community violence. Journal of Youth and Adolescence. 2004;33(1):59–69. [Google Scholar]
- 48.Singer M, Anglin TM, Song L, Lunghofer L. Adolescents’ exposure to violence and associated symptoms and psychological trauma. JAMA. 1995;273(6):477–482. [PubMed] [Google Scholar]
- 49.Popkin SJ, Leventhal T, Weismann G. Girls in the ‘Hood: The Importance of Feeling Safe. Washington, DC: The Urban Institute; 2008. [Google Scholar]
- 50.Caldwell CH, Rafferty J, Reischl TM, De Loney EH, Brooks CL. Enhancing parenting skills among nonresident African American fathers as a strategy for preventing youth risky behaviors. Am J Community Psychol. 2010;45(1–2):17–35. doi: 10.1007/s10464-009-9290-4. [DOI] [PubMed] [Google Scholar]
- 51.Chapman MV. Neighborhood quality and somatic complaints among American youth. J Adolesc Health. 2005 Mar;36(3):244–252. doi: 10.1016/j.jadohealth.2004.02.029. [DOI] [PubMed] [Google Scholar]
- 52.Kuh D, Ben-Shlomo Y, Lynch J, Hallqvist J, Power C. Glossary: life course epidemiology. J Epidemiol Community Health. 2003;57(10):778–783. doi: 10.1136/jech.57.10.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Berkman LF. Social epidemiology: social determinants of health in the United States: are we losing ground? Annu Rev Public Health. 2009;30(1):27–41. doi: 10.1146/annurev.publhealth.031308.100310. [DOI] [PubMed] [Google Scholar]
- 54.Oakes JM. The (mis)estimation of neighborhood effects: causal inference for a practicable social epidemiology. Soc Sci Med. 2004;58(10):1929–1952. doi: 10.1016/j.socscimed.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 55.Sobel ME. What do randomized studies of housing mobility demonstrate? Causal inference in the face of interference. Journal of the American Statistical Association. 2006;101(476):1398–1407. [Google Scholar]
- 56.Pebley AR, Sastry N. Report CCPR-035-04. Los Angeles CA: UCLA; 2003. Neighborhoods, Poverty and Children’s Well-being: A Review. [Google Scholar]
- 57.Ludwig J, Liebman JB, Kling JR, Duncan GJ, Katz LF, Kessler RC, Sanbonmatsu L. What can we learn about neighborhood effects from the Moving to Opportunity experiment? A comment on Clampet-Lundquist and Massey. AJS. 2008;114(1):144–188. [Google Scholar]
- 58.Clampet-Lundquist S, Massey DS. Neighborhood effects on economic self-sufficiency: a reconsideration of the Moving to Opportunity experiment. AJS. 2008;114(1):107–143. [Google Scholar]
- 59.Sampson RJ. Moving to inequality: neighborhood effects and experiments meet social structure. AJS. 2008;114(1):189–231. doi: 10.1086/589843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Katz B. Neighborhoods of Choice and Connection: The Evolution of American Neighbourhood Policy and What it Means for the United Kingdom. York, UK: Joseph Rowntree Foundation; 2004. [Google Scholar]
- 61.Kruckenberg K Poverty & Race Research Action Council. Poverty & Race Research Action Council Policy Brief. Washington, DC: Poverty & Race Research Action Council; 2011. Two Simple Changes to Improve Health Outcomes in the Section 8 Voucher Program. http://www.prrac.org/pdf/HQS-SEMAPhealthpolicybriefApril2011.pdf. [Google Scholar]
- 62.National Low Income Housing Coalition. [Accessed Date 4/29/11];Federal budget & approps, HUD budget charts, FY11 and FY12 budget chart for selected HUD programs. 2011 Updated April 27, 2011. https://www2398.ssldomain.com/nlihc/template/page.cfm?id=28 http://www.nlihc.org/doc/FY11_12_Budget_Chart_HUD.pdf.
- 63.Arias E. United States Life Tables, 2006. Hyattsville, MD: National Center for Health Statistics; 2010. [PubMed] [Google Scholar]
- 64.Popkin SJ, Levy D, Harris LE, Comey J, Cunningham MK, Buron L. HOPE VI Panel Study: Baseline Report. Washington, DC: The Urban Institute; 2002. [Google Scholar]
- 65.Engdahl L. New Homes, New Neighborhoods, New Schools: A Progress Report on the Baltimore Housing Mobility Program. Baltimore, MD and Washington, DC: Baltimore Regional Housing Campaign, and Poverty & Race Research Action Council; 2009. [Google Scholar]
- 66.Cohen E, Fullerton DF, Retkin R, Weintraub D, Tames P, Brandfield J, Sandel M. Medical-legal partnership: collaborating with lawyers to identify and address health disparities. J Gen Intern Med. 2010;25(Suppl 2):136–139. doi: 10.1007/s11606-009-1239-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.VanderWeele TJ, Hernández-Diaz S. Is there a direct effect of pre-eclampsia on cerebral palsy not through preterm birth? Paediatr Perinat Epidemiol. 2011;25:111–115. doi: 10.1111/j.1365-3016.2010.01175.x. [DOI] [PubMed] [Google Scholar]
- 68.Aneshensel CS. Research in mental health: social etiology versus social consequences. J Health Soc Behav. 2005;46:221–228. doi: 10.1177/002214650504600301. [DOI] [PubMed] [Google Scholar]
- 69.McMahon SD, Grant KE, Compas BE, Thurm AE, Ey S. Stress and psychopathology in children and adolescents: is there evidence of specificity? J Child Psychol Psychiatry. 2003;44(1):107–133. doi: 10.1111/1469-7610.00105. [DOI] [PubMed] [Google Scholar]
- 70.Manjarrez CA, Popkin SJ, Guernsey E. Poor Health: Adding Insult to Injury for HOPE VI Families. Washington, DC: The Urban Institute; 2007. [Google Scholar]
- 71.Gennetian LA, Bos JM, Morris PA. Using Instrumental Variables Analysis to Learn More from Social Policy Experiments. New York, NY: Manpower Demonstration Research Corporation; 2002. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.