Abstract
Throughout the 1990s, many villagers in rural China were infected with HIV through commercial plasma/blood donation. These former plasma/blood donors (FPDs) experienced many HIV-related stressors. This study tested a cognitive appraisal model of stress and coping in a sample of HIV-positive adult FPDs. Participants (N = 207) from multiple villages completed a battery of questionnaires assessing HIV-related stress, HIV symptoms, cognitive appraisal, coping behaviors, and psychological distress. Participants reported high levels of HIV-related stress, depression, and anxiety. In a structural equation model, greater HIV-related stress, HIV symptoms, and threat appraisal were directly associated with psychological distress. HIV-related stress was also indirectly associated with psychological distress through threat appraisal. In a second model, coping was found to mediate the relationship between challenge appraisal and psychological distress. Results support the utility of cognitive appraisal theory. Stress management interventions targeting HIV-positive FPDs in China are indicated.
Keywords: HIV/AIDS, cognitive appraisal, coping, psychological distress, China
China has experienced a unique epidemic of HIV transmission through commercial plasma/blood collection (Mastro and Yip, 2006). In the 1990s, thousands of commercial collection stations were established where individuals were paid to donate plasma or blood (Cohen, 2004). This practice was particularly common in rural regions of several provinces, including Henan, Shanxi, Anhui, and Shandong. One survey in Shanxi Province found that 30% of villagers reported a history of plasma/blood donation (Qian et al., 2006). Many of the collection centers pooled and centrifuged the blood, retained the plasma, and reinfused donors with red blood cells from the pool. This process was highly efficient, allowing individuals to sell their plasma more frequently. Unfortunately, it also placed donors at high risk for blood borne infections, including HIV. Authorities recognized the problem in 1995, and new laws eventually prevented this practice from continuing. By then, however, many former plasma/blood donors (FPDs) were already infected with HIV.
Studies of FPDs in rural China have found HIV prevalence rates ranging from 1.3% to 15% (Ji et al., 2006; Qian et al., 2006; Wu et al., 2001; Wu et al., 2006). In 2005, Chinese officials estimated that 55,000 FPDs were living with HIV/AIDS, though many more had already died from AIDS-related causes (Ministry of Health, 2006). At this point, most FPDs have been infected for over 10 years and account for the majority of the known AIDS patients in China (Wang, 2007).
Persons living with HIV/AIDS may experience a multitude of stressors, including intrusive physical symptoms, complex medical treatments, relationship difficulties, cognitive impairments, and discrimination/stigma (Bogart et al., 2000; Kalichman and Catz, 2000; Pakenham et al., 1996). HIV-infected FPDs in China may face additional stressors. Most live in extreme poverty in rural villages, and financial stress typically motivated plasma/blood donation in the first place. Following HIV diagnosis, many villagers were discriminated from working or were simply unable to work due to declining health, leading to even more dire circumstances (Ji et al., 2007). HIV stigma continues to be a serious problem in China, especially in rural villages where knowledge of HIV/AIDS is limited (Ji et al., 2007). This stigma can strain prior relationships, causing isolation and loneliness. Furthermore, because blood donation was a widespread practice in these villages, many friends and relatives were also infected with HIV. As a result, AIDS bereavement is a common experience, and social support may be further limited.
Psychological distress, particularly depression and anxiety symptoms, has been consistently found to predict HIV symptoms, disease progression, and mortality (Ickovics et al., 2001; Ironson et al., 2005; Leserman et al., 1999; Mayne et al., 1996). This finding led to increased awareness of the importance of treating psychological distress in HIV patients. To date, there has been limited research examining psychological distress among HIV-positive individuals in China. One study found that the rate of major depressive disorder was much higher in HIV-positive compared to HIV-negative participants (79% versus 4%, respectively), with most first episodes occurring after HIV diagnosis and persisting over time (Jin et al., 2006). Given the multiple stressors faced by HIV-positive FPDs living in rural China, further research examining depression and anxiety in this unique population is indicated.
Richard Lazarus' influential theory of stress and coping suggests that cognitive appraisal and coping behavior are critical mediators in the relationship between stress and adaptation (Lazarus, 1966, 1991; Lazarus and Folkman, 1984). Cognitive appraisal is the process through which a person evaluates if a particular stressor is relevant and, if so, whether it is primarily threatening (possibly causing harm or loss) or challenging (offering potential for mastery or benefit). This primary appraisal influences how the person might behave to cope with the stressor. Prior studies have found that cognitive appraisal is a significant predictor of coping behavior (e.g., Folkman et al., 1986). Coping, in turn, determines how the person adapts to the stressful event using cognitive and behavioral efforts.
In U.S. samples, the relationship between coping behavior and psychological distress in HIV-positive persons has been extensively studied. In general, avoidant coping is associated with greater distress (Blaney et al., 2004; Fleishman and Fogel, 1994; Simoni et al., 2000), while problem-focused coping is associated with less distress (Fleishman and Fogel, 1994; Pakenham and Rinaldis, 2001). Very little research exists on coping with HIV/AIDS in China. In one sample of adults newly diagnosed with HIV in Hong Kong, anxiety was associated with less positive thinking and more problem solving, avoidance, and realistic acceptance, while depression was associated with less positive thinking and more denial (Chan et al., 2006). Further research is needed to better understand the relationship between coping and psychological distress among HIV-positive persons in China, including rural regions.
Prior studies conducted in Western countries also support the relationship between cognitive appraisal and psychological distress in HIV-positive persons. In a sample of gay/bisexual men, threat appraisal, but not challenge appraisal, was positively correlated with depression symptoms and global distress; however, the mediating role of threat appraisal was not tested (Pakenham and Rinaldis, 2001). In a sample of women, HIV-related stress was indirectly associated with psychological distress through cognitive appraisal in a structural equation model (Moneyham et al., 1997). Specifically, women who experienced more HIV-related stress also reported more intrusive thoughts and perceived stigma related to HIV, which in turn predicted greater distress. Finally, in a study of men and women, threat appraisal mediated the negative relationship between self-esteem and mood disturbance (Anderson, 1995). That is, individuals with higher self-esteem perceived HIV as less threatening, which in turn was associated with less psychological distress. Thus, Lazarus' stress and coping theory may provide a useful framework in which to examine the relationship between HIV-related stress and psychological distress.
The purpose of the current study was to report the severity of HIV-related stress and the level of depression and anxiety symptoms in a sample of HIV-positive FPDs in rural China, and to test a cognitive appraisal model of stress and coping using structural equation modeling. We hypothesized that cognitive appraisal would mediate the relationship between HIV-related stress and psychological distress, with threat appraisal predicting greater distress and challenge appraisal predicting less distress. We further hypothesized that coping behavior would mediate the relationship between cognitive appraisal and psychological distress. Specifically, we expected that challenge appraisal would be associated with more action-oriented coping (problem solving and support seeking), which in turn would predict less distress, and that threat appraisal would be associated with more emotion-focused coping (avoidance, wishful thinking, and self-blaming), which in turn would predict greater distress.
METHODS
Participants and Procedures
Participants were recruited from 20 villages from one county in Henan Province in January 2003. Chinese villages serve as organizational units for rural, farming communities. They have defined boundaries and one designated village head. These villages range in population from one hundred to a few thousand, though they are typically small enough that villagers know each other well. Prior to 1995, commercial blood/plasma donation was a common practice in these villages. After the problem of contaminated blood was discovered, the Chinese government implemented an active HIV testing initiative and offered free health care to HIV-positive villagers, including antiretroviral therapy (Zhang et al., 2005). Among many other governmental duties, the village head is responsible for coordinating HIV-related services.
Eligibility criteria for the current study were HIV infection, history of paid blood/plasma donation, and 18 to 60 years of age. After obtaining permission from the County Health Bureau, research staff met with each of the 20 village heads individually to describe the study. The village head, being aware of villagers' HIV status, inquired about individuals' potential interest in the study. After receiving permission to do so, research staff approached villagers in their homes; village heads were not present for consenting or assessment procedures. After providing verbal informed consent, participants completed a battery of questionnaires. The questionnaires were anonymous; they contained no names or identifying information. For 34 illiterate participants, the battery was administered as an interview by trained research staff. The questionnaires took 45–80 minutes to complete. Participants were paid 10 Yuan (approximately US$1.25) as compensation.
The goal was to recruit a convenience sample of 250 participants from 20 villages. Though systematic records were not kept, some individuals who were targeted for recruitment were not enrolled because they were either not home, too busy to participate, or uninterested in the study. Of 260 eligible individuals who provided informed consent, 220 (85%) returned usable questionnaires. An additional 13 cases were dropped because of missing data on key variables, leaving a final sample of 207.
Measures
The assessment battery was comprised of well-validated instruments commonly used in HIV/AIDS research. Most of these instruments have been translated into Mandarin Chinese, with acceptable reliability and validity, and are publicly available for use in Chinese samples. However, some measures had to be translated for this study, as noted below. In these cases, we used the back translation method, with minor modifications by the corresponding author to ensure comprehension by villagers.
Psychological distress
The Chinese version of the Beck Depression Inventory (BDI) was used to assess depression (Beck et al, 1991; Zheng et al., 1988). Participants rated the severity of 21 symptoms during the past week on a scale ranging from 0 (absent) to 3 (severe). The standard cutoffs for the BDI are: 0–9 minimal, 10–18 mild, 19–29 moderate, and 30–63 severe. Because vegetative symptoms of depression (e.g., fatigue, change in appetite, sleep disturbance) may overlap with HIV symptoms, only the cognitive-affective subscale was included in the structural equation models (14 items; α = .83). The Chinese version of the Zung Self-rating Anxiety Scale (SAS) was used to assess anxiety (Zhang, 1993; Zung, 1971). Participants reported how frequently they experienced each of 20 symptoms during the past week on a scale ranging from 1 (none of the time) to 4 (most of the time). The standard cutoffs for the SAS are: 20–44 normal, 45–59 mild-moderate, 60–74 marked-severe, and 75–80 extreme. Again, because vegetative symptoms of anxiety (e.g., dizzy spells, weakness, indigestion) may overlap with HIV symptoms, only cognitive-affective items were included in the models (12 items; α = .73).
HIV-related stress
The 23-item HIV/AIDS Stress Scale was used to assess the stressfulness of everyday HIV-related problems (Pakenham and Rinaldis, 2002). Participants indicated how troublesome each problem was in the past month on a scale ranging from 0 (not at all) to 4 (extremely). There are three subscales: social stress (10 items, α = .73; e.g., relationship difficulties, disclosure concerns, discrimination/stigma), instrumental stress (6 items, α = .55; e.g., financial difficulties, treatment-related problems, lack of access to healthcare services), and existential/emotional stress (7 items, α = .70; e.g., grief/bereavement, difficulty accepting HIV/AIDS status, concerns about death). Mean scores were calculated for each subscale. This instrument was translated into Chinese for this study.
HIV symptoms
The Chinese Version of the Sign and Symptom Checklist for Persons with HIV was used to assess HIV symptoms (Holzemer et al., 1999; Tsai et al., 2003). For each of 26 items, participants reported their intensity on that day on a scale ranging from 0 (not detected) to 3 (severe). There are five subscales: fever (4 items, α = .63; e.g., fever, day sweats), weakness (6 items, α = .74; e.g., fatigue, muscle ache, thirst); gastrointestinal/nausea (7 items, α = .75; e.g., diarrhea, vomiting, bloating), shortness of breath (3 items, α = .63; e.g., wheezing, shortness of breath at rest), and confusion/distress (6 items, α = .72; e.g., difficulty concentrating, depression, fear). Mean scores were calculated for each subscale. The weakness and confusion/distress subscales were not included in the structural equation models to eliminate redundancy with the psychological distress measures. Participants also self-reported their most recent CD4 cell count.
Cognitive appraisal
Primary cognitive appraisal was assessed using the method developed by Folkman and colleagues (1986). Participants indicated the extent to which their main HIV-related stressor had the potential to harm their physical well-being and their emotional well-being (2 threat items; 1 = no harm, 7 = extremely harmful), and the potential for personal growth and personal challenge (2 challenge items; 1 = nil potential, 7 = high potential). This instrument was translated into Chinese for this study.
Ways of coping
The Ways of Coping (WOC) questionnaire was used to assess coping related to HIV/AIDS disease (Folkman and Lazarus, 1988). This questionnaire has been translated into Chinese and used successfully in Chinese samples (Chan, 1994). For the current study, we used the brief version of the WOC (Vitaliano et al., 1985), which we translated into Chinese. Participants rated the degree to which they used each of 41 coping strategies on a scale ranging from 0 (not at all characteristic of me) to 4 (very characteristic of me) to manage their HIV/AIDS “in general”. There are five subscales: problem solving (15 items, α = .77; e.g., tried harder to make things work, came up with a couple of different solutions, took things one step at a time), support seeking (6 items, α = .51; e.g., accepted sympathy from others, talked to someone to find out more about the situation), wishful thinking (8 items, α = .55; e.g., had fantasies about how things might turn out, hoped for a miracle), avoidance (9 items, α = .43; e.g., went on as if nothing happened, kept my feelings to myself), and self blame (3 items, α = .43; e.g., blamed yourself, criticized or lectured yourself). Mean scores were calculated for each subscale. The problem-solving and support seeking subscales are considered action-oriented strategies, while the wishful thinking, avoidance, and self blame subscales are considered emotion-focused strategies (Vitaliano et al., 1985).
Data analysis
The sample was described using frequencies and means. Structural equation modeling (SEM) was used to test the relationship between HIV-related stress, cognitive appraisal, coping behaviors, and psychological distress. The theoretical model was tested in two steps. The first model examined the relationship between HIV-related stress, cognitive appraisal (threat and challenge), and psychological distress, controlling for HIV symptoms. The second model tested the hypothesis that coping behavior mediated the relationship between cognitive appraisal and psychological distress. In both models, indicator loadings on the latent factors ranged from .50 to .95 (all p < .01). Age and gender were added as covariates. For each model, four things were assessed: (1) overall fit of the model, (2) significance of individual structural paths, (3) amount of variability (R2) of the latent variables accounted for by the observed variables, and (4) direct and indirect effects.
For the overall fit, the closeness of the hypothetical model to the empirical data was evaluated through goodness-of-fit indices, specifically chi-square (χ2), root mean square error of approximation (RMSEA), comparative fit index (CFI), and non-normed fit index (NNFI). A χ2 value of no more than twice the degrees of freedom in the model is generally indicative of a plausible, well-fitting model (Bollen, 1989; Jaccard and Wan, 1996). However, because the χ2 value is influenced by sample size and even good fitting models may have significant values, it is recommended that multiple fit indices be used to assess model fit. The RMSEA assesses absolute fit but penalizes for less parsimonious models. It is a badness-of-fit index, with values less than 0.06 being desirable (Hu and Bentler, 1999). The CFI and NNFI compare the absolute fit with an independence model that assumes no relationships among variables, and values greater than .95 indicate good fit (Hu and Bentler, 1999).
Mediation was tested by computing the direct and indirect relationships between the predictors and the dependent variable using bootstrap methodology (Shrout and Bolger, 2002). This approach computes an estimate of the indirect effects and 95% confidence intervals. Compared to the causal steps approach to testing mediation (e.g., Baron and Kenny, 1986), bootstrap methodology directly tests the indirect effect, is more statistically powerful, and does not rely on distributional assumptions. Finally, the significance of the indirect effects were tested using Sobel tests (Preacher and Hayes, 2004).
RESULTS
Sample description
The sample included 207 HIV-positive FPDs. They ranged in age from 27 to 59 years (M = 39.6, SD = 7.0). Approximately half (54%) were female, and all were ethnically Han. The educational level was 11% illiterate, 56% primary school, 32% junior high school, and 1% senior high school. Participants donated plasma and/or blood between 1989 and 1996. The number of years since HIV diagnosis ranged from 1 to 10 years (M = 2.9, SD = 1.6). Participants were likely infected 6 to 14 years before, but widespread HIV testing did not occur in the villages until early 2000. Among the subset of participants who reported their most recent CD4 cell count (58%), it ranged from 16 to 730 (M = 305.9, SD = 171.7) and was negatively correlated with HIV symptoms (r = −.28, p < .01).
Table I summarizes the descriptive statistics for measured variables included in the analyses. Participants reported extremely high levels of depression and anxiety. The mean BDI score was 27.25 (SD = 11.31), with 47% reporting moderate and 36% severe depression. The mean SAS score was 46.02 (SD = 9.34), with 52% reporting mild-moderate and 8% reporting marked-severe anxiety. Compared to men, women reported higher levels of anxiety (47.75 ± 9.14 vs. 44.11 ± 9.14; t(204) = 2.85, p < .01) but not depression (28.21 ± 10.55 vs. 25.87 ± 11.93; t(204) = 1.50, ns).
Table I.
Descriptive statistics for measured variables
| Possible range | Min | Max | Mean | SD | |
|---|---|---|---|---|---|
| Psychological distress | |||||
| Depression | 0–63 | 0 | 58 | 27.25 | 11.31 |
| Anxiety | 20–80 | 20 | 71 | 46.02 | 9.34 |
| HIV-related stress | |||||
| Social | 0–4 | 0.40 | 3.90 | 2.03 | 0.65 |
| Instrumental | 0–4 | 0.33 | 4.00 | 2.05 | 0.71 |
| Emotional/existential | 0–4 | 0.57 | 4.00 | 2.19 | 0.72 |
| HIV symptoms | |||||
| Fever | 0–3 | 0.00 | 3.00 | 1.25 | 0.66 |
| Shortness of breath | 0–3 | 0.00 | 3.00 | 1.32 | 0.73 |
| Weakness | 0–3 | 0.17 | 3.00 | 1.62 | 0.59 |
| Gastrointestinal/nausea | 0–3 | 0.00 | 3.00 | 1.15 | 0.59 |
| Confusion/distress | 0–3 | 0.00 | 3.00 | 1.47 | 0.59 |
| Threat appraisal | |||||
| Physical well-being | 1–7 | 1 | 7 | 5.67 | 1.54 |
| Emotional well-being | 1–7 | 1 | 7 | 4.90 | 1.78 |
| Challenge appraisal | |||||
| Personal growth | 1–7 | 1 | 7 | 4.12 | 2.18 |
| Personal challenge | 1–7 | 1 | 7 | 4.26 | 2.03 |
| Coping behavior | |||||
| Problem solving | 0–4 | 0.53 | 3.80 | 2.35 | 0.54 |
| Support seeking | 0–4 | 0.33 | 4.00 | 2.31 | 0.62 |
| Avoidance | 0–4 | 0.67 | 3.67 | 1.99 | 0.55 |
| Wishful thinking | 0–4 | 0.25 | 3.75 | 2.17 | 0.63 |
| Self blaming | 0–4 | 0.00 | 4.00 | 1.82 | 0.91 |
Most participants endorsed (score ≥ 1) many of the HIV-related stressors. The most common stressors were dealing with declining health (97%), financial problems (97%), and relationship problems (96%). The least common stressors were substance abuse (52%), suicidal ideation/attempts (72%), and legal problems (74%). Overall, the HIV-related stressors were moderately troublesome to participants (M = 2.13, SD = 0.59), with similar levels of stress across the three subscales (social, instrumental, and emotional/existential). While participants utilized all types of coping strategies, they were more likely to utilize action-oriented strategies (problem solving and support seeking) than emotion-focused strategies (avoidance, wishful thinking, and self blaming) (2.33 ± 0.49 vs. 1.99 ± 0.50, respectively; t(206) = 9.44, p < .01). Table II shows the correlations among the five coping subscales and the two psychological distress measures. Contrary to our hypothesis, the problem solving, support seeking, wishful thinking, and avoidance subscales were significantly and positively correlated with one another. Consequently, these subscales loaded onto a single coping latent construct in the SEM model. The self blame subscale was poorly correlated with the other subscales and was therefore not included in SEM model. As expected, the depression and anxiety measures were significantly and positively correlated with one another.
Table II.
Correlation matrix for coping subscales and psychological distress measures
| Problem solving | Support seeking | Avoidance | Wishful thinking | Self blaming | Depression | Anxiety | |
|---|---|---|---|---|---|---|---|
| Problem solving | -- | ||||||
| Support seeking | .42** | -- | |||||
| Avoidance | .49** | .26** | -- | ||||
| Wishful thinking | .49** | .37** | .42** | -- | |||
| Self blaming | .09 | .17* | .19** | .21** | |||
| Depression | −.19* | .02 | −.13 | −.02 | .14* | ||
| Anxiety | −.04 | .06 | −.11 | .10 | .17* | .46** | -- |
p < .05
p < .01
SEM models
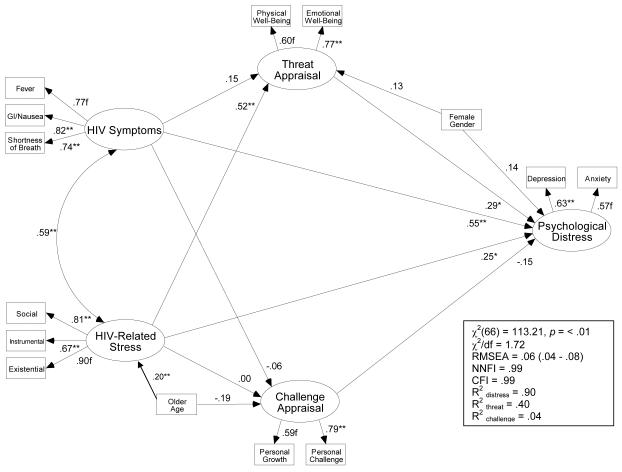
The first model tested the relationship between HIV-related stress, cognitive appraisal (threat and challenge), and psychological distress (Figure 1). The structural model had excellent fit to the data (χ2(66) = 113.21, p < .01; χ2/df = 1.72; RMSEA = .06 (.04 − .08); NNFI = .99; CFI = .99). HIV-related stress (β = .25; p < .05), HIV symptoms (β = .55; p < .01), and threat appraisal (β = .29; p < .05) were associated with greater psychological distress. Challenge appraisal was associated with less psychological distress, but this relationship was not significant (β = −.15; p < .10). HIV-related stress was indirectly associated with psychological distress (β = .15 (.01 − .43), p < .05) but HIV symptoms was not (β = .05 (−.04 − .21), ns). A Sobel test confirmed that HIV-related stress was indirectly associated with psychological distress through threat appraisal (Z = 2.00, p < .05) but not through challenge appraisal (Z = −0.04, ns). These results suggest that, after controlling for HIV symptoms, individuals who experienced greater HIV-related stress perceived greater threat to their well-being, which in turn was associated with greater psychological distress.
Figure 1.
Structural equation model predicting cognitive appraisal and psychological distress in HIV-positive former blood/plasma donors. Standardized path coefficients are presented. Residual error variances were calculated but omitted from the figure. A superscript of f denotes a fixed path. *p < .05, **p < .01.
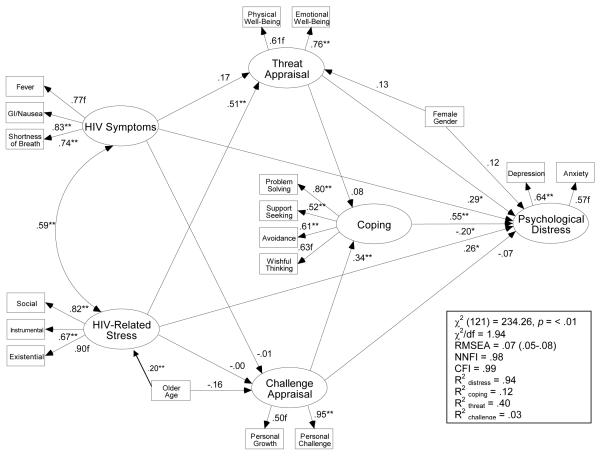
The second model tested whether coping behavior mediated the relationship between cognitive appraisal and psychological distress (Figure 2). The structural model fit the data well (χ2(121) = 234.26, p < .01; χ2/df = 1.94; RMSEA = .07 (.05 − .08); NNFI = .98; CFI = .99). HIV-related stress (β = .26, p < .05), HIV symptoms (β = .55, p < .01), threat appraisal (β = .29, p < .05), and coping behavior (β = −.20, p < .05) were directly associated with psychological distress. Challenge appraisal was not directly associated with psychological distress (β = −.07, p > .05), but it was indirectly associated with psychological distress through its effect on coping behavior (β = −.07 (−.20 – −.01), p < .05). A Sobel test confirmed that challenge appraisal was indirectly associated with psychological distress through coping (Z = −2.02, p < .05). There was no indirect effect of threat appraisal on psychological distress (β = −.02 (−.12 − .02), ns). These results suggest that individuals who perceived HIV-related stressors as an opportunity for personal growth and challenge engaged in more coping behaviors, which in turn was associated with less psychological distress. In contrast, threat appraisal was unrelated to coping but was directly associated with greater psychological distress.
Figure 2.
Structural equation model predicting cognitive appraisal, coping behavior, and psychological distress in HIV-positive former blood/plasma donors. Standardized path coefficients are presented. Residual error variances were calculated but omitted from the figure. A superscript of f denotes a fixed path. *p < .05, **p < .01.
DISCUSSION
Consistent with cognitive appraisal theory, we found that threat and challenge appraisals played important, albeit different, roles in the relationship between HIV-related stress and mental health among HIV-positive FPDs in rural China. While most participants reported many HIV-related stressors, those who experienced more severe stress viewed HIV/AIDS as a greater threat to their well-being. To a certain extent, this may be a valid appraisal, insofar as HIV/AIDS does impact physical and emotional health, particularly in regions with high rates of HIV infection and limited resources. However, excessive threat appraisal may interfere with adaptation, leading to greater psychological distress. For example, realistic acceptance has been found to predict decreased survival time in HIV-positive persons (Reed et al., 1994). On the other hand, participants who viewed HIV/AIDS as less threatening, even after controlling for HIV symptoms and HIV-related stress, experienced lower psychological distress. However, coping did not mediate the relationship between threat appraisal and psychological distress. In contrast, challenge appraisal was associated with lower psychological distress, and coping behavior mediated this relationship. Participants who viewed HIV-related stressors as an opportunity for personal growth and challenge engaged in more coping behaviors, which in turn predicted lower psychological distress. Challenge appraisal may motivate adaptive behavior, thereby buffering the negative effects of HIV-related stress on mental health. Previous studies have also found that positive cognitions, including benefit finding and optimism, are associated with better mental health in HIV-positive persons (Bower et al., 1998; Littlewood et al., 2008; Taylor et al., 1992).
Contrary to our original hypothesis, in this sample of HIV-positive FPDs in rural China, both action-oriented and emotion-focused coping strategies were associated with lower psychological distress. Participants utilized action-oriented strategies more frequently than emotion-focused strategies, but both types of coping behaviors had a positive impact on mental health. This is in contrast to U.S. studies, which typically find that avoidance is associated with increased psychological distress in HIV-positive persons (Blaney et al., 2004; Fleishman and Fogel, 1994; Simoni et al., 2000). Two studies conducted in Hong Kong also found that HIV-positive outpatients utilized multiple strategies to cope with HIV/AIDS, and that internal (i.e., avoidance, fatalism, and self reliance) and emotion-focused (i.e., avoidance, denial) coping strategies were associated with greater psychological distress (Chan et al., 2006; Molassiotis et al., 2001).
There are a number of possible explanations for the observed relationships between coping and psychological distress in the current study. First, the HIV-positive FPDs lived in rural regions of China and differed from prior samples in terms of available resources for treating and managing HIV infection. Many of the participants had lived with HIV/AIDS for years before learning of their disease and receiving treatment. This sample was also unique in terms of the types and severity of HIV-related stressors. For example, the widespread prevalence of HIV infection in these rural communities strained available social supports, and financial stress and poor access to healthcare limited practical options for managing HIV/AIDS. According to Lazarus and Folkman's (1984) theory of stress and coping, the optimal coping response depends on the situation: if a stressor is changeable, action-orientated strategies predominate; if it is not changeable, emotion-focused strategies predominate. The desperate situation facing many HIV-positive FPDs may have required mobilization of multiple coping behaviors, and the use of emotion-focused strategies, including maintaining hope and use of distraction, seems to have been somewhat effective. However, avoidant coping has been found to predict poorer health status and faster HIV disease progression (Ironson et al., 2005; Leserman et al., 2000; Mulder et al., 1999). Further research might assess the impact of avoidant coping on physical health outcomes in HIV-positive persons living in rural and resource poor areas of the world.
Alternatively, the high levels of psychological distress reported in this cohort of HIV-positive FPDs may have suppressed all types of coping strategies. When individuals perceive an absence of control over the outcome of a situation, they may develop “learned helplessness”, which impacts behavioral adaptation (Seligman, 1975). In persons living with HIV, perceived lack of control has been associated with less self-care activities, greater psychological distress, and poorer health status (Folkman et al., 1993; Ironson et al., 2005; Pakenham and Rinaldis, 2001; Reynolds et al., 2007). Contrary to this theory, however, participants in this study utilized coping behaviors at a frequency comparable to other HIV-positive samples (Pakenham and Rinaldis, 2001).
Nevertheless, the remarkably high levels of psychological distress reported in this sample is concerning. Emerging evidence suggests that the risk of depression following HIV diagnosis in China may be high. A small study conducted primarily in Beijing found that HIV-positive participants had significantly greater depression symptoms compared to HIV-negative participants (Jin et al., 2006). The level of depression symptoms was even higher in our sample of HIV-positive FPDs, with 83% of participants reporting moderate to severe depression. Additionally, 60% of participants reported moderate to severe anxiety. The high levels of psychological distress may in part be explained by the greater number and severity of HIV-related stressors experienced by HIV-positive adults in rural China. For example, social stigmatization of HIV/AIDS may subject villagers to more severe consequences (e.g., job loss, isolation). Furthermore, there continues to be a widespread belief in China that HIV/AIDS is a terminal illness, and many villagers have poor access to healthcare. Indeed, participants reported higher levels of stress compared to an Australian sample of gay and bisexual men using the same HIV/AIDS Stress Scale (Pakenham and Rinaldis, 2002). As in prior studies conducted globally (Blaney et al., 2004; Chan et al., 2006; Folkman et al., 1993; Murphy et al., 2000; Pakenham and Rinaldis, 2001; Remien et al., 2006), HIV-related stress was strongly and independently associated with psychological distress.
The results of this study suggest that cognitive appraisal theory may provide a useful foundation for designing mental health interventions for HIV-positive FPDs in China. Interventions might begin by assessing individuals' appraisal of HIV-related stressors. Threat-based appraisals, even if accurate, can have deleterious effects on health outcomes. Cognitive-behavioral techniques may be helpful for altering these thought patterns (Beck, 1995). On the other hand, eliciting challenge-based appraisals may lead to an increased sense of situational control and motivate adaptive behaviors. In addition, interventions might help individuals indentify and apply appropriate coping behaviors to specific stressors, within the context of cultural norms and available resources. As discussed above, both action-oriented and emotion-focused strategies may be appropriate in rural China. Stress management and coping interventions based on these principles have been effective in reducing distress and improving psychological functioning in HIV-positive persons in Western countries (Brown and Vanable, 2008; Scott-Sheldon et al., 2008; Sikkema et al., 2006; Sikkema et al., 2007). However, given the high rates of psychological distress among this sample of HIV-positive FPDs, these stress management programs may not be sufficient. Dissemination of empirically-supported treatments for psychological disorders, including both traditional Chinese and Western approaches, into rural China might be necessary to adequately treat HIV-positive villagers presenting with severe depression and/or anxiety.
Interpretations from this study must be made in the context of several limitations. First, due to the cross-sectional design, causality could not be determined. For example, it is possible that depression may impact perceptions of stress and threat, or more likely that the effects are bidirectional. Prospective designs are needed to investigate causal relationships among stress, appraisal, coping, and mental health. Future studies might also include biological measures to assess the relationship between cognitive appraisal and coping behavior on disease progression. Second, some of the measures were translated into Chinese for this study, without supporting psychometric evidence. Further research is needed to develop reliable and valid measures of HIV-related stress and cognitive appraisal and to determine the ability of coping measures to distinguish between action-oriented and emotion-focused coping in Chinese samples. Because coping measures can be unstable across different samples and stressors (van Heck and de Ridder, 2001), some studies factor analyze scale items to better reflect the particular situation (e.g., (Simoni et al., 2000; Tarakeshwar et al., 2005). However, due to sample size restrictions, a factor analysis would not have been appropriate in the current study. Finally, although efforts were made to target a diverse sample by recruiting from 20 villages, results of this convenience sample may not be representative of all HIV-positive FPDs in rural China (e.g., individuals who were unaware of their HIV infection, or those who were unable or unwilling to participate in the study). Results may also not generalize to HIV-positive adults who are infected through other transmission routes, are less socioeconomically disadvantaged, and/or live in other regions of the world.
In conclusion, we found that HIV-positive FPDs in rural China experienced multiple HIV-related stressors and high levels of psychological distress. Beginning in 2002, the Chinese government launched the China Comprehensive AIDS Response program to expand access to HIV/AIDS treatment and care services throughout the most heavily affected provinces (Zhang et al., 2005), though challenges remain in the implementation of national HIV/AIDS programs (Yin and Wu, 2007). Furthermore, the mental health needs of many HIV-positive villagers may not be sufficiently addressed. Results of the current study support the utility of cognitive appraisal theory in understanding the relationship between HIV-related stress and mental health. Psychological interventions that target maladaptive cognitive processes and motivate adaptive coping behavior, in addition to empirically supported treatments for psychological disorders, may help improve quality of life among the many HIV-positive FPDs living the rural China.
AKNOWLEDMENTS
This study was supported by funding from China's 15 Year Science and Technology Plan (2001-BA705801), the Chinese Ministry of Health Science and Technology Agency (WA2002-01-01), and the United States National Institutes of Health (T32-DA015036).
REFERENCES
- Anderson SEH. Personality, appraisal, and adaptational outcomes in HIV seropositive men and women. Research in Nursing and Health. 1995;18:303–312. doi: 10.1002/nur.4770180404. [DOI] [PubMed] [Google Scholar]
- Baron R, Kenny D. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical consideration. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. Psychological Corporation; San Antonio, TX: 1991. [Google Scholar]
- Beck JS. Cognitive Therapy: Basics and Beyond. Guilford Press; New York: 1995. [Google Scholar]
- Blaney N, Fernandez M, Ethier K, Wilson T, Walter E, Koenig L. Psychosocial and behavioral correlates of depression among HIV-infected pregnant women. AIDS Patient Care and STDs. 2004;18:405–415. doi: 10.1089/1087291041518201. [DOI] [PubMed] [Google Scholar]
- Bogart LM, Catz SL, Kelly JA, Gray-Bernhardt ML, Hartman BR, Otto-Salaj LL, et al. Psychosocial issues in the era of new AIDS treatments from the perspective of persons living with HIV. Journal of Health Psychology. 2000;5:500–516. doi: 10.1177/135910530000500408. [DOI] [PubMed] [Google Scholar]
- Bollen KA. Structural Equations with Latent Variables. Wiley; New York: 1989. [Google Scholar]
- Bower JE, Kemeny ME, Taylor SE, Fahey JL. Cognitive processing, discovery of meaning, CD4 decline, and AIDS-related mortality among bereaved HIV-seropositive men. Journal of Consulting and Clinical Psychology. 1998;66:979–986. doi: 10.1037//0022-006x.66.6.979. [DOI] [PubMed] [Google Scholar]
- Brown JL, Vanable PA. Cognitive-behavioral stress management interventions for persons living with HIV: a review and critique of the literature. Annals of Behavioral Medicine. 2008;35:26–40. doi: 10.1007/s12160-007-9010-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan DW. The Chinese Ways of Coping Questionnaire: assessing coping in secondary school teachers and students in Hong Kong. Psychological Assessment. 1994;6:1040–3590. [Google Scholar]
- Chan I, Au A, Li P, Chung R, Lee MP, Yu P. Illness-related factors, stress, and coping strategies in relation to psychological distress in HIV-infected persons in Hong Kong. AIDS Care. 2006;18:977–982. doi: 10.1080/09540120500490093. [DOI] [PubMed] [Google Scholar]
- Cohen J. HIV/AIDS in China. An unsafe practice turned blood donors into victims. Science. 2004;304:1438–1439. doi: 10.1126/science.304.5676.1438. [DOI] [PubMed] [Google Scholar]
- Fleishman JA, Fogel B. Coping and depressive symptoms among people with AIDS. Health Psychology. 1994;13:156–169. doi: 10.1037//0278-6133.13.2.156. [DOI] [PubMed] [Google Scholar]
- Folkman S, Chesney M, Pollack L, Coates T. Stress, control, coping, and depressive mood in human immunodeficiency virus-positive and -negative gay men in San Francisco. Journal of Nervous and Mental Disease. 1993;181:409–416. doi: 10.1097/00005053-199307000-00002. [DOI] [PubMed] [Google Scholar]
- Folkman S, Lazarus RS. Manual for the Ways of Coping Questionnaire: Research Edition. Consulting Psychological Press; Palo Alto, CA: 1988. [Google Scholar]
- Folkman S, Lazarus RS, Dunkel-Schetter C, DeLongis A, Gruen RJ. Dynamics of a stressful encounter: cognitive appraisal, coping, and encounter outcomes. Journal of Personality and Social Psychology. 1986;50:992–1003. doi: 10.1037//0022-3514.50.5.992. [DOI] [PubMed] [Google Scholar]
- Holzemer WL, Henry SB, Nokes KM, Corless IB, Brown MA, Powell-Cope GM, et al. Validation of the Sign and Symptom Checklist for Persons with HIV disease (SSC-HIV) Journal of Advanced Nursing. 1999;30:1041–1049. doi: 10.1046/j.1365-2648.1999.01204.x. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criterion for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Ickovics JR, Hamburger ME, Vlahov D, Schoenbaum EE, Schuman P, Boland RJ, et al. Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women: longitudinal analysis from the HIV epidemiology research study. JAMA. 2001;285:1466–1474. doi: 10.1001/jama.285.11.1466. [DOI] [PubMed] [Google Scholar]
- Ironson G, O'Cleirigh C, Fletcher MA, Laurenceau JP, Balbin E, Klimas N, et al. Psychosocial factors predict CD4 and viral load change in men and women with human immunodeficiency virus in the era of highly active antiretroviral treatment. Psychosomatic Medicine. 2005;67:1013–1021. doi: 10.1097/01.psy.0000188569.58998.c8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaccard J, Wan CK. LISREL Approaches to Interaction Effects in Multiple Regression. Sage; Thousand Oaks, CA: 1996. [Google Scholar]
- Ji G, Detels R, Wu Z, Yin Y. Correlates of HIV infection among former blood/plasma donors in rural China. AIDS. 2006;20:585–591. doi: 10.1097/01.aids.0000210613.45212.c4. [DOI] [PubMed] [Google Scholar]
- Ji G, Li L, Lin C, Sun S. The impact of HIV/AIDS on families and children--a study in China. AIDS. 2007;21:S157–161. doi: 10.1097/01.aids.0000304712.87164.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin H, Hampton Atkinson J, Yu X, Heaton RK, Shi C, Marcotte TP, et al. Depression and suicidality in HIV/AIDS in China. Journal of Affective Disorders. 2006;94:269–275. doi: 10.1016/j.jad.2006.04.013. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Catz SL. Stressors in HIV infection. In: Nott K, Vedhara K, editors. Psychosocial and Biomedical Interactions in HIV Infection. Harwood Academic; Amsterdam: 2000. pp. 31–60. [Google Scholar]
- Lazarus RS. Psychological Stress and Coping Process. McGraw-Hill; New York: 1966. [Google Scholar]
- Lazarus RS. Emotion and Adaptation. Oxford University Press; Oxford: 1991. [Google Scholar]
- Lazarus RS, Folkman S. Stress, Appraisal, and Coping. Springer Publishing Company; New York: 1984. [Google Scholar]
- Leserman J, Jackson ED, Petitto JM, Golden RN, Silva SG, Perkins DO, Cai J, Folds JD, Evans DL. Progression to AIDS: the effects of stress, depressive symptoms, and social support. Psychosomatic Medicine. 1999;61:397–406. doi: 10.1097/00006842-199905000-00021. [DOI] [PubMed] [Google Scholar]
- Leserman J, Petito JM, Golden RN, Gaynes BN, Gu H, Perkins DO, Silva SG, Folds JD, Evans DL. Impact of stressful life events, depression, social support, coping, and cortisol on progression to AIDS. American Journal of Psychiatry. 2000;157:1221–1228. doi: 10.1176/appi.ajp.157.8.1221. [DOI] [PubMed] [Google Scholar]
- Littlewood RA, Vanable PA, Carey MP, Blair DC. The association of benefit finding to psychosocial and health behavior adaptation among HIV+ men and women. Journal of Behavioral Medicine. 2008;31:145–155. doi: 10.1007/s10865-007-9142-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mastro TD, Yip R. The legacy of unhygienic plasma collection in China. AIDS. 2006;20:1451–1452. doi: 10.1097/01.aids.0000233580.56844.c1. [DOI] [PubMed] [Google Scholar]
- Mayne TJ, Vittinghoff E, Chesney MA, Barrett DC, Coates TJ. Depressive affect and survival among gay and bisexual men infected with HIV. Archives of Internal Medicine. 1996;156:2233–2238. [PubMed] [Google Scholar]
- Ministry of Health, People's Republic of China . Update on the HIV/AIDS Epidemic and Response in China. National Center for AIDS/STD Prevention and Control; Beijing: 2006. [Google Scholar]
- Molassiotis A, Callaghan P, Twinn SF, Lam SW. Correlates of quality of life in symptomatic HIV patients living in Hong Kong. AIDS Care. 2001;13:319–334. doi: 10.1080/09540120120043973. [DOI] [PubMed] [Google Scholar]
- Moneyham L, Seals B, Sowell R, Hennessy M, Demi A, Brake S. The impact of HIV on emotional distress of infected women: cognitive appraisal and coping as mediators. Scholarly Inquiry for Nursing Practice. 1997;11:125–145. [PubMed] [Google Scholar]
- Mulder CL, de Vroome EM, van Griensven GJ, Antoni MH, Sandfort TG. Avoidance as a predictor of the biological course of HIV infection over a 7-year period in gay men. Health Psychology. 1999;18:107–113. doi: 10.1037//0278-6133.18.2.107. [DOI] [PubMed] [Google Scholar]
- Murphy DA, Moscicki AB, Vermund SH, Muenz LR. Psychological distress among HIV+ adolescents in the REACH study: effects of life stress, social support, and coping. The Adolescent Medicine HIV/AIDS Research Network. Journal of Adolescent Health. 2000;27:391–398. doi: 10.1016/s1054-139x(00)00158-0. [DOI] [PubMed] [Google Scholar]
- Pakenham KI, Dadds MR, Terry DJ. Adaptive demands along the HIV disease continuum. Social Science and Medicine. 1996;42:245–256. doi: 10.1016/0277-9536(95)00099-2. [DOI] [PubMed] [Google Scholar]
- Pakenham KI, Rinaldis M. The role of illness, resources, appraisal, and coping strategies in adjustment to HIV/AIDS: the direct and buffering effects. Journal of Behavioral Medicine. 2001;24:259–279. doi: 10.1023/a:1010718823753. [DOI] [PubMed] [Google Scholar]
- Pakenham KI, Rinaldis M. Development of the HIV/AIDS Stress Scale. Psychology and Health. 2002;17:203–219. [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavioral Research Methods, Instruments, and Computers. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Qian HZ, Vermund SH, Kaslow RA, Coffey CS, Chamot E, Yang Z, Qiao X, Zhang Y, Shi X, Shao Y, Wang N. Co-infection with HIV and hepatitis C virus in former plasma/blood donors: challenge for patient care in rural China. AIDS. 2006;20:1429–1435. doi: 10.1097/01.aids.0000233577.33973.fa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed GM, Kemeny ME, Taylor SE, Wang HY, Visscher BR. Realistic acceptance as a predictor of decreased survival time in gay men with AIDS. Health Psychology. 1994;13:299–307. doi: 10.1037//0278-6133.13.4.299. [DOI] [PubMed] [Google Scholar]
- Remien RH, Exner T, Kertzner RM, Ehrhardt AA, Rotheram-Borus MJ, Johnson MO, Weinhardt LS, Kittle LE, Goldstein RB, Pinto RM, Morin SF, Chesney MA, Lightfoot M, Gore-Felton C, Dodge B, Kelly JA. Depressive symptomatology among HIV-positive women in the era of HAART: a stress and coping model. American Journal of Community Psychology. 2006;38:275–285. doi: 10.1007/s10464-006-9083-y. [DOI] [PubMed] [Google Scholar]
- Reynolds NR, Sanzero Eller L, Nicholas PK, Corless IB, Kirksey K, Hamilton MJ, Kemppainen JK, Bunch E, Dole P, Wantland D, Sefcik E, Nokes KM, Coleman CL, Rivero M, Canaval GE, Tsai YF, Holzemer WL. HIV illness representation as a predictor of self-care management and health outcomes: a multi-site, cross-cultural study. AIDS and Behavior. doi: 10.1007/s10461-007-9297-5. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott-Sheldon LA, Kalichman SC, Carey MP, Fielder RL. Stress management interventions for HIV+ adults: a meta-analysis of randomized controlled trials, 1989 to 2006. Health Psychology. 2008;27:129–139. doi: 10.1037/0278-6133.27.2.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligman MEP. Helplessness: On Depression, Development, and Death. W. H. Freeman; San Francisco: 1975. [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychological Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- Sikkema KJ, Hansen NB, Ghebremichael M, Kochman A, Tarakeshwar N, Meade CS, Zhang H. A randomized controlled trial of a coping group intervention for adults with HIV who are AIDS bereaved: longitudinal effects on grief. Health Psychology. 2006;25:563–570. doi: 10.1037/0278-6133.25.5.563. [DOI] [PubMed] [Google Scholar]
- Sikkema KJ, Hansen NB, Kochman A, Tarakeshwar N, Neufeld S, Meade CS, Fox AM. Outcomes from a group intervention for coping with HIV/AIDS and childhood sexual abuse: reductions in traumatic stress. AIDS and Behavior. 2007;11:49–90. doi: 10.1007/s10461-006-9149-8. [DOI] [PubMed] [Google Scholar]
- Simoni JM, Demas P, Mason H, Drossman J, Davis M. HIV disclosure among women of African descent: associations with coping, social support, and psychological adaptation. AIDS and Behavior. 2000;4:147–158. [Google Scholar]
- Tarakeshwar N, Hansen NB, Kochman A, Sikkema KJ. Gender, ethnicity and spiritual coping among bereaved HIV-positive individuals. Mental Health, Religion and Culture. 2005;8:109–125. [Google Scholar]
- Taylor SE, Kemeny ME, Aspinwall LG, Schneider SG, Rodriguez R, Herbert M. Optimism, coping, psychological distress, and high-risk sexual behavior among men at risk for acquired immunodeficiency syndrome (AIDS) Journal of Personality and Social Psychology. 1992;63:460–473. doi: 10.1037//0022-3514.63.3.460. [DOI] [PubMed] [Google Scholar]
- Tsai YF, Hsiung PC, Holzemer WL. Validation of a Chinese version of the sign and symptom checklist for persons with HIV diseases. Journal of Pain and Symptom Management. 2003;25:363–368. doi: 10.1016/s0885-3924(02)00687-5. [DOI] [PubMed] [Google Scholar]
- van Heck G, de Ridder D. Assessment of coping with loss: Dimensions and measurement. In: Stroebe MS, Hansson RO, Stroebe W, Schut H, editors. Handbook of bereavement research: Consequences, coping and care. American Psychological Association; Washington, DC: 2001. [Google Scholar]
- Vitaliano PP, Russo J, Carr JE, Maiuro RD, Becker J. The ways of coping checklist: revision and psychometric properties. Multivariate Behavioral Research. 1985;20:3–26. doi: 10.1207/s15327906mbr2001_1. [DOI] [PubMed] [Google Scholar]
- Wang L. Overview of the HIV/AIDS epidemic, scientific research and government responses in China. AIDS. 2007;21:S3–7. doi: 10.1097/01.aids.0000304690.24390.c2. [DOI] [PubMed] [Google Scholar]
- Wu Z, Rou K, Detels R. Prevalence of HIV infection among former commercial plasma donors in rural eastern China. Health Policy and Planning. 2001;16:41–46. doi: 10.1093/heapol/16.1.41. [DOI] [PubMed] [Google Scholar]
- Wu Z, Sun X, Sullivan SG, Detels R. Public health: HIV testing in China. Science. 2006;312:1475–1476. doi: 10.1126/science.1120682. [DOI] [PubMed] [Google Scholar]
- Yin W-Y, Wu Z-Y. Challenges and opportunities: the expanded government-led HIV/AIDS programs in China. Virologica Sinica. 2007;22:493–500. [Google Scholar]
- Zhang FJ, Pan J, Yu L, Wen Y, Zhao Y. Current progress of China's free ART program. Cell Research. 2005;15:877–882. doi: 10.1038/sj.cr.7290362. [DOI] [PubMed] [Google Scholar]
- Zhang MY. Ranking Scales for Mental Health. Science and Technology Press; Changsha, Hunan: 1993. [Google Scholar]
- Zheng YP, Wei LA, Goa LG, Zhang GC, Wong CG. Applicability of the Chinese Beck Depression Inventory. Comprehensive Psychiatry. 1988;29:484–489. doi: 10.1016/0010-440x(88)90063-6. [DOI] [PubMed] [Google Scholar]
- Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12:371–379. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]