Abstract
Background
Orthostatic tremor (OT) is a high-frequency tremor (13–18 Hz) present in the legs when standing. Underlying disease is found in one-third of OT patients.
Case report
We describe an 86-year-old man with progressive shaking of the legs while standing, which disappears immediately after sitting down or while walking. Polymyography confirmed a tremor of the legs (10–11 Hz) while standing. Magnetic resonance imaging (MRI) and neurologic examination showed no underlying disease.
Discussion
Primary OT can appear at a lower frequency of 10–11 Hz.
Keywords: Orthostatic, tremor
Introduction
Orthostatic tremor (OT) is a rare condition defined as a high-frequency tremor (13–18 Hz) in the legs when standing.1 Patients with OT usually report instability while standing, which decreases and eventually disappears through walking or sitting. OT is generally considered to be an idiopathic disorder. However, in about one-third of cases, the tremor is related to Parkinson's disease, cerebellar or brainstem pathology, or restless legs syndrome.2 The pathophysiology is unknown. However, a central oscillator located in the pons or cerebellum is thought to be involved.3
We describe the first case of an OT of primary origin with a frequency lower than 13–18 Hz.
Case report
An 86-year-old man presented with progressive shaking of the legs that had started 6 months earlier. The tremor forced him to sit down after several minutes, but it was absent while sitting or walking. In addition, the patient had noticed a mild shaking of his hands and head over the past year. His previous medical history included a transient ischemic attack and carpal tunnel release. The tremor was not affected by alcohol consumption.
On examination, a tremor was palpable in both legs on standing and could be auscultated by a stethoscope in the left leg. A mild, irregular, low-amplitude, postural tremor of the hands was also observed. This tremor was barely visible and scored only one point on The Essential Tremor Rating Assessment Scale (TETRAS).4 The described no-no shaking tremor of the head was not detected by the clinician or video registration. No signs of parkinsonism or cerebellar dysfunction were found.
At follow-up, head and hand tremors were no longer perceived by the patient and could not be determined on examination. However, the oscillation of the legs persisted.
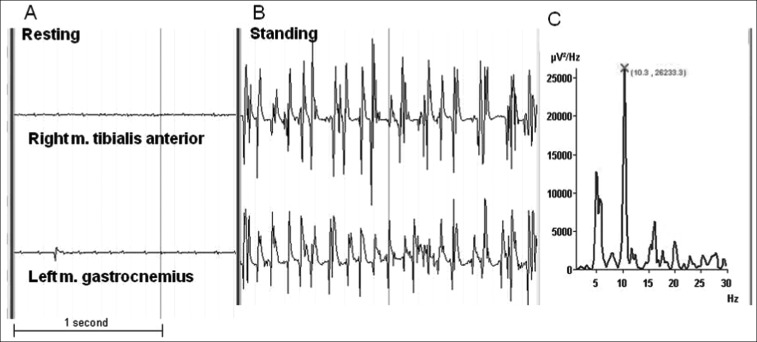
Polymyography with surface electrodes on the right tibialis anterior, left rectus femoris, and left gastrocnemius muscles, demonstrated a tremor of the legs in an upright position with a frequency of 10–11 Hz (Figure 1). The tremor was immediately present on standing, had a constant frequency during standing, and disappeared after sitting down. A synchronous tremor was registered in all three muscles, but it was not present while the patient was seated or when the muscles were actively contracted without standing in an upright position. Video registration during polymyography revealed a very fine, jerky tremor of the hands. However, this tremor was not detectable by polymyography.
Figure 1. Polymyography Of The Right Tibialis Anterior And Left Gastrocnemius Muscles.
Measurements during resting (A) and standing (B). Frequency analysis with fast Fourier transformation (C) during standing showed a peak frequency of 10.3 Hz.
Brain imaging was performed with a 1.5-Tesla magnetic resonance (MR) scanner and T1, T2, fluid-attenuated inversion recovery (FLAIR), contrast-enhanced T1, and diffusion weighted (DWI) MR imaging were performed. The scan showed global atrophy in accordance with the patient's age. There were no indications of a tumor or (recent) ischemia in the cerebellum or the brainstem.
Discussion
The clinical symptoms of unsteadiness and shaking legs while standing in the present case are consistent with a diagnosis of OT. However, the frequency was lower than the previously described 13–18 Hz.
OT characterized by low frequencies is called slow OT. Williams et al. recently described a patient with cerebellar atrophy and OT with a frequency of 9 Hz, and Baker et al. reported a patient with multiple sclerosis and OT of 4 Hz.5,6 One case report has been published regarding a patient with slow OT without underlying disease, but the description of this case was so minimal that a secondary origin of the tremor could not be excluded.7 Slow OT was defined in these articles as the characteristic symptom of OT with electromyography (EMG) bursts with frequencies less than 12 Hz. Our case fits this description. However, in comparison to previously described patients, no underlying disease was found on neurological examination or MRI.
Essential tremor (ET) is a symmetric postural and kinetic tremor that most commonly affects the hands, with a frequency of 4–12 Hz.8 In this case, tremor frequency, age at onset, and the occurrence of a mild postural tremor of the hands and attendant head tremor are consistent with ET. However, the presentation of a tremor in the legs exclusively during standing is not characteristic of ET. In addition, the tremors in the arms and head could not be demonstrated objectively and had disappeared at follow-up. The tremor of the arms is therefore more likely to be an enhanced physiologic tremor. Furthermore, the combination of OT and postural tremor of the arms was described in more than half of the patients with primary OT.2 Nevertheless, a diagnosis of ET could not be entirely excluded.
An orthostatic myoclonus may also manifest as unsteadiness on standing.9,10 On polymyography, this myoclonus is registered exclusively during standing and disappears after sitting or while walking. Results are therefore comparable to those of OT. However, EMG bursts in orthostatic myoclonus are irregular, non-rhythmic, have a frequency of 9–15 Hz, and are not synchronic for different muscles in both legs. In this case, there was a constant tremor registered during standing, and it was synchronous in all measured muscles; therefore an orthostatic myoclonus is unlikely.
The polymyography performed in this case had a few limitations. Firstly, it was identified during regular patient care, which means that not all antagonists and homologous leg muscles were examined. However, the pattern of immediate tremor appearance on standing and disappearance after being seated and the synchronic bursts of activity in the examined muscles fit very well with a diagnosis OT. Secondly, the peak frequency was not as dominant as in other OT cases, but there was certainly a clear peak between 10 and 11 Hz. Finally, there was no polymyography registration while walking. Collectively, our polymyography findings are a clear match with a slow OT.
In conclusion, OT of primary origin is not necessarily a high-frequency tremor; it can also occur in a lower frequency of 10–11 Hz.
Footnotes
Funding: None.
Financial disclosures: None.
Conflict of Interests: The authors report no conflicts of interest.
References
- 1.Heilman KM. Orthostatic tremor. Arch Neurol. 1984;41:880–881. doi: 10.1001/archneur.1984.04050190086020. [DOI] [PubMed] [Google Scholar]
- 2.Gerschlager W, Münchau A, Katzenschlager R. Natural history and syndromic associations of orthostatic tremor: a review of 41 patients. Mov Disord. 2004;19:788–795. doi: 10.1002/mds.20132. [DOI] [PubMed] [Google Scholar]
- 3.Piboolnurak P, Yu QP, Pullman SL. Clinical and neurophysiologic spectrum of orthostatic tremor: case series of 26 subjects. Mov Disord. 2005;20:1455–1461. doi: 10.1002/mds.20588. [DOI] [PubMed] [Google Scholar]
- 4.Elble R, Comella C, Fahn S, et al. Reliability of a new scale for essential tremor. Mov Disord. 2012;27:1567–1569. doi: 10.1002/mds.25162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Williams ER, Jones RE, Baker SN, Baker MR. Slow orthostatic tremor can persist when walking backward. Mov Disord. 2010;25:795–797. doi: 10.1002/mds.23024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baker M, Fisher K, Lai M, Duddy M, Baker S. Slow orthostatic tremor in multiple sclerosis. Mov Disord. 2009;24:1550–1553. doi: 10.1002/mds.22630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Uncini A, Onofrj M, Basciani M, Cutarella R, Gambi D. Orthostatic tremor: report of two cases and an electrophysiological study. Acta Neurol Scand. 1989;79:119–122. doi: 10.1111/j.1600-0404.1989.tb03722.x. [DOI] [PubMed] [Google Scholar]
- 8.Thanvi B, Lo N, Robinson T. Essential tremor-the most common movement disorder in older people. Age Ageing. 2006;35:344–349. doi: 10.1093/ageing/afj072. [DOI] [PubMed] [Google Scholar]
- 9.Leu-Semenescu S, Roze E, Vidailhet M, et al. Myoclonus or tremor in orthostatism: an under-recognized cause of unsteadiness in Parkinson's disease. Mov Disord. 2007;22:2063–2069. doi: 10.1002/mds.21651. [DOI] [PubMed] [Google Scholar]
- 10.Glass GA, Ahlskog JE, Matsumoto JY. Orthostatic myoclonus: a contributor to gait decline in selected elderly. Neurology. 2007;68:1826–1830. doi: 10.1212/01.wnl.0000260225.46732.af. [DOI] [PubMed] [Google Scholar]