Abstract
This study examined human immunodeficiency virus (HIV) as a traumatic stressor, intrusive and deliberate cognitive processing, psychological distress, and posttraumatic growth. One-hundred twelve participants completed interviews on posttraumatic stress disorder (PTSD) Criterion A, Rumination Scale-Revised, Impact of Event Scale, and the Posttraumatic Growth Inventory; relationships were modeled using path analysis. Model 1 attempted to replicate prior empirical research, Model 2 attempted to empirically replicate part of the posttraumatic growth theoretical model, and Model 3 attempted to empirically replicate an integrated model of posttraumatic growth and traumatic stress theories. Model 3 had good fit with study data. Results suggest shared and separate pathways from traumatic stressor to psychological distress and posttraumatic growth, with pathways mediated by cognitive processing. Implications of findings are discussed.
Receiving a diagnosis of human immunodeficiency virus (HIV) can be a highly stressful event. The American Psychiatric Association included a diagnosis of a life-threatening illness as a potentially traumatic stressor that may lead to the development of posttraumatic stress disorder (PTSD) in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV, American Psychiatric Association [APA], 1994). Thus, researchers have begun to examine the potentially traumatic nature of receiving a diagnosis of HIV and living with the disease (Martin & Kagee, 2008).
Further, research has shown that many individuals report experiencing some form of psychological growth or transformation, namely posttraumatic growth, in the aftermath of potentially traumatic events (Tedeschi & Calhoun, 2004). Psychological distress and PTSD are distinct from posttraumatic growth. While PTSD is a negative psychological outcome resulting from a disruption in the recovery process (Resick, 2001), posttraumatic growth represents a positive psychological outcome resulting from struggling with and working through a traumatic event (Tedeschi & Calhoun, 2004). Although PTSD and posttraumatic growth are discrete outcomes of exposure to traumatic events, they may have shared predictors. Additionally, the presence of posttraumatic growth does not indicate the absence of psychological distress. In fact, Tedeschi and Calhoun (2004) suggest psychological distress may be necessary for the initiation of posttraumatic growth, and research has shown positive relationships between posttraumatic growth and traumatic stress symptoms (e.g., Morris, Shakespeare-Finch, Rieck, & Newbery, 2005).
According to Tedeschi and Calhoun (2004) several important components are involved in the development of posttraumatic growth, including personal characteristics, social support, impact of the event, and cognitive processing. They further suggest that cognitive processing is central to the development of posttraumatic growth. Therefore, the current study tested the direct and indirect impact of both experiencing a potentially traumatic event and engaging in cognitive processing on psychological distress and posttraumatic growth. This approach builds upon previous posttraumatic growth research by synthesizing and empirically evaluating the posttraumatic growth model with cognitive models of trauma.
Posttraumatic growth theory suggests that potentially traumatic events must be seismic in nature (i.e., cause disruption of core beliefs or assumptions about the self and the world and create a state of cognitive confusion) to initiate cognitive processing (Tedeschi & Calhoun, 2004). However, this has rarely been examined. Instead, it has been assumed a priori that potentially traumatic stressors were experienced as seismic, which may or may not have been true. Nonetheless, the characteristics and perception of the stressor are important to initiating and maintaining engagement in cognitive processing and indirectly related to the development of posttraumatic growth (Tedeschi & Calhoun, 2004). Similarly, cognitive models of trauma emphasize the importance of the impact of the stressor in the later development of pathology (Creamer, Burgess, & Pattison, 1992). Therefore, a better understanding of the impact of the potentially traumatic event may help clarify the complex cognitive processing in its aftermath.
Criterion A for PTSD diagnosis in the DSM-IV (APA, 1994, pp. 424) is one means of determining if a potentially traumatic stressor is perceived as traumatic. In fact, some studies examining posttraumatic growth have used this criterion as a measure of the perception of an event as a traumatic stressor (Cordova, Cunningham, Carlson, & Andrykowski, 2001; Cordova et al., 2007). Results indicate a significant positive relationship between meeting PTSD Criterion A and posttraumatic growth in individuals identifying cancer as the traumatic stressor.
Further, Tedeschi and Calhoun (2004) propose cognitive processing, a type of recurrent thinking, as a necessary step in the process of posttraumatic growth. This involves intrusive cognitive processing, such as negative and unwanted ruminative thoughts (Ehlers & Clark, 2000), as well as more deliberate cognitive processing (Calhoun & Tedeschi, 2006) including meaning making (Davis, 2000). It is important to note that cognitive processing as referred to here is qualitatively different from depressive rumination. Cognitive processing among trauma survivors is often about the traumatic event and its consequences (Ehlers & Clark, 2000), whereas the ruminations of those with depressed moods are generally not linked to life events, but are focused on depressive symptoms and their consequences (Nolen-Hoeksema, 1991). Further, deliberate cognitive processing is characterized as purposeful, an idea adapted from Martin and Tesser’s (1996) conceptualization of cognitive processing, which includes making sense (e.g., making sense of the trauma or loss, coming up with an acceptable explanation) and problem solving. Calhoun and Tedeschi (2006) suggest that though intrusive and deliberate cognitive processing generally co-occur, the cognitive processing that occurs in the immediate aftermath of a traumatic event is primarily intrusive whereas more deliberate cognitive processing is present later in the development of posttraumatic growth.
Across a number of studies, a positive relationship has been identified between cognitive processing and posttraumatic growth (Linley & Joseph, 2004). However, the amount, timing, and type of cognitive processing require further exploration. Some researchers have found that those who engage in deliberate cognitive processing soon after the event have higher levels of posttraumatic growth than those who do not. For example, Taku, Calhoun, Cann, & Tedeschi (2008) examined the timing of intrusive and deliberate cognitive processing in bereaved Japanese college students and found those who engaged in deliberate cognitive processing soon after their loss had greater levels of posttraumatic growth, whereas those who were experiencing current intrusive cognitive processing had greater levels of psychological distress.
In summary, traumatic stress and posttraumatic growth are separate outcomes of exposure to traumatic events; however, based on the research discussed above, they may have shared predictors. Specifically, the perception of a potentially traumatic event as life threatening and disruptive to current assumptions (i.e., seismic) is necessary in the development of PTSD (Creamer et al., 1992) as well as for the initiation of posttraumatic growth (Tedeschi & Calhoun, 2004). Additionally, although there is a positive relationship between cognitive processing and psychological growth (Linley & Joseph, 2004; Taku et al., 2008), there is also a positive relationship between cognitive processing and psychological distress (Taku et al., 2008). It is not clear if the type and timing of cognitive processing involved in posttraumatic growth is distinctly different from the type and timing of cognitive processing involved in the development of traumatic stress or PTSD. Therefore, further research is necessary to disentangle these complex relationships.
The current study used path analysis to examine the unique and shared pathways to psychological distress and/or posttraumatic growth by testing models based on prior posttraumatic growth research findings and by integrating posttraumatic growth and cognitive trauma theories into a comprehensive framework. Three models were examined using data obtained from a sample of individuals receiving care for HIV or acquired immune deficiency syndrome (AIDS). Model 1 is based on previous research by Taku and colleagues (2008), and hypothesized that intrusive cognitive processing is (a) expected immediately after receiving an HIV diagnosis, (b) is not indicative of later psychological distress or posttraumatic growth, and (c) is indirectly related to psychological distress through current intrusive cognitive processing. Further, Model 1 hypothesized that deliberate cognitive processing immediately following an HIV diagnosis is directly related to posttraumatic growth, whereas current deliberate cognitive processing is directly related to current intrusive cognitive processing and thus indirectly related to psychological distress. Finally, Model 1 hypothesized a positive direct relationship between psychological distress and posttraumatic growth.
Model 2 is based on components of Calhoun and Tedeschi’s (2006) theory of posttraumatic growth. Model 2 adds a variable indicating the seismic nature of the traumatic event (here measured with PTSD Criterion A), but does not include past deliberate or current intrusive cognitive processing due to the assumption that the cognitive processing immediately following a seismic event is primarily intrusive and the cognitive processing that occurs later is primarily deliberate. Model 2 hypothesized two indirect paths from PTSD Criterion A to posttraumatic growth through cognitive processing and psychological distress and that cognitive processing will mediate the relationship between PTSD Criterion A and posttraumatic growth.
Model 3 is an integrated model that includes all of the constructs in the previous models. This model synthesizes cognitive trauma theories (Creamer et al., 1992; Ehlers & Clark, 2000) and posttraumatic growth theory (Calhoun & Tedeschi, 2006). Model 3 hypothesized that experiencing one’s diagnosis as a traumatic stressor is (a) directly related to both types of past cognitive processing, (b) indirectly related to posttraumatic growth through past intrusive and current deliberate cognitive processing, and (c) indirectly related to psychological distress through past and current intrusive cognitive processing. Model 3 further hypothesized positive direct relationships between (a) past intrusive cognitive processing and past deliberate cognitive processing, (b) current intrusive cognitive processing and current deliberate cognitive processing, (c) past deliberate cognitive processing and current deliberate cognitive processing, and (d) psychological distress and posttraumatic growth.
METHOD
Participants
Over a 6-month recruitment period, 146 patients receiving care in an HIV/AIDS clinic at an urban medical center in Chicago, Illinois were approached by research assistants while waiting for appointments. Of these, 114 (78%) were eligible and agreed to participate in the study. Patients were eligible if they were (a) at least 18 years of age, (b) HIV-positive for at least a year, and (c) receiving care at the clinic. Twenty-eight declined participation and 4 were ineligible (diagnosed within the past year). No participants withdrew from the study. Two participants did not complete one of the study measures, thus their data were excluded from these analyses. The final sample included 112 participants.
Once patients agreed to participate, they were escorted to a private room and provided further study information, including risks and benefits of participation, after which informed consent to participate was obtained. Research assistants verbally administered a demographics questionnaire and conducted a semistructured interview based on DSM-IV PTSD criteria. To eliminate possible literacy problems, participants were offered the opportunity to complete self-report questionnaires independently or have them read aloud. Participants were compensated with $15 store gift cards. The study was approved by the institutional review boards of the medical center and the second author’s institution. Further, a Certificate of Confidentiality was obtained from the National Institute of Health.
Measures
Self-report demographics included gender, age, marital/relationship status, ethnicity, sexual orientation, education, income, and employment status.
A brief structured clinical interview was used to assess HIV as a traumatic stressor using Criterion A for PTSD based on the DSM-IV (APA, 1994). Participants were requested to recall the date they were diagnosed with HIV. If they were unable to recall the date, the research assistant probed further with questions regarding age at diagnosis, season of the year when diagnosed, etc. Participants were then asked to respond to two yes/no questions based on DSM-IV PTSD criteria: (1) “Did you perceive this experience as a threat to your life or a threat to your physical well-being?” and (2) “Did your response involve intensive fear, helplessness, or horror?” (Cordova et al., 2001). The use of Criterion A has been deemed a “feasible definition of trauma” that can “serve a wide range of clinical and research needs” (Weathers & Keane, 2007). Criterion A for PTSD was coded as a dichotomous variable; endorsement of both criteria indicated that HIV diagnosis was perceived as a traumatic stressor.
The Rumination Scale-Revised (A. Cann, personal communication, January 25, 2007) was used to measure cognitive processing. It is a 12-item self-report questionnaire containing two subscales (deliberate and intrusive cognitive processing) based on the original 7-item Rumination Scale (Calhoun, Cann, Tedeschi, & McMillan, 2000) and Martin and Tesser’s (1996) rumination conceptualization. Each item was administered twice with items anchored at two time periods: during the first 3 months after learning one’s HIV diagnosis, and over the past 3 months. This procedure yielded four subscale scores, including (a) past intrusive cognitive processing (e.g., “Soon after learning about my diagnosis of HIV I thought about it when I did not mean to”), (b) past deliberate cognitive processing (e.g., “Soon after learning about my diagnosis of HIV I reminded myself of some benefits that came from adjusting to the diagnosis”), (c) current intrusive cognitive processing, and (d) current deliberate cognitive processing. Each subscale contained six items scored on a 4-point scale ranging from 0 = not at all to 3 = often, with items from each subscale summed to yield four independent scores. Subscales had adequate internal consistency for the current study (Cronbach’s alpha), ranging from .67 to .91.
The Posttraumatic Growth Inventory (Tedeschi & Calhoun, 1996) was used to measure posttraumatic growth. This 21-item self-report measure assesses positive outcomes following a negative event, with items rated on a 6-point Likert Scale ranging from 0 (not at all) to 5 (a very great degree). The Posttraumatic Growth Inventory demonstrated good internal consistency, with current study Cronbach’s alpha = .96.
The Impact of Event Scale (IES; Horowitz, Wilner, & Alvarez, 1979) was used to measure psychological distress related to receiving a diagnosis of HIV. This measure contains 15 items assessing commonly reported intrusion and avoidance symptoms of traumatic stress. Items are rated on a 4-point scale from 0 (not at all), 1 (rarely), 3 (sometimes), to 5 (often) based on how frequently each symptom has been experienced within the past week. Higher scores indicate greater distress, with scores 36 and over representing significant distress (Witteveen, Bramsen, Hovens, & van der Ploeg, 2005). Previous research found good split-half reliability (.87) and one-week test-retest reliability (.87) for the total score (Horowitz et al., 1979), and a current study Cronbach’s alpha of .91.
Data Analysis
Version 16.0 of SPSS was used for descriptive analyses and AMOS 17.0 was used to evaluate the path models. A missing data analysis conducted on the final sample of 112 participants suggested data were missing at random; therefore regression imputation replaced missing data.
RESULTS
There were no response differences for participants who completed self-report questionnaires independently versus those who had self-report questions read aloud. Participants were on average 44.9 years old (SD = 8.9), 73% male, 57% heterosexual, 88% African American, and 70% unemployed/disabled. Descriptive statistics for all study variables are presented in Table 1.
Table 1.
Descriptive Statistics for Variables in the Models (N = 112)
| Variables | N | % | M | SD | Range |
|---|---|---|---|---|---|
| PTSD Criterion A | |||||
| Perceived threat to life | 46 | 41 | |||
| Response was fear, helplessness, horror | 66 | 59 | |||
| HIV diagnosis as traumatic stressor | 37 | 33 | |||
| Revised Rumination Scale | |||||
| Past intrusive cognitive processing | 10.18 | 5.34 | 0–18 | ||
| Past deliberate cognitive processing | 10.67 | 4.15 | 0–18 | ||
| Current intrusive cognitive processing | 6.19 | 5.02 | 0–18 | ||
| Current deliberate cognitive processing | 8.28 | 4.48 | 0–18 | ||
| Impact of Event Scale (psychological distress) | 25.32 | 18.19 | 0–66 | ||
| Posttraumatic Growth Inventory | 61.14 | 28.51 | 0–105 |
Note: PTSD = posttraumatic stress disorder.
On average, participants had been living with HIV for 10.9 (SD = 5.7) years (range 1 to 23 years). Time since HIV diagnosis was not significantly related to any variables in the study and was therefore not included in the models. Overall, 33% of the participants experienced their HIV diagnosis as a traumatic stressor. Further, the mean on the Posttraumatic Growth Inventory in the current study was 61.14 (SD = 28.51) and is comparable to previous research examining posttraumatic growth in other medically ill populations, including breast cancer survivors (mean Posttraumatic Growth Inventory = 57.8; SD = 24.4) (Cordova et al., 2007) and bone marrow transplant patients (mean Posttraumatic Growth Inventory = 64.67; SD = 21.30; Widows, Jacobsen, Booth-Jones, & Fields, 2005).
Path Analysis
Table 2 presents the correlation matrix for all variables included in the study. Collinearity analyses indicated multicollinearity was not a serious concern (Tabachnick & Fidell, 2007).
Table 2.
Correlation Matrix of all Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1. PTSD Criterion A | – | |||||||
| 2. Past intrusive cognitive processing | .46** | – | ||||||
| 3. Past deliberate cognitive processing | .22* | .61** | – | |||||
| 4. Current intrusive cognitive processing | .27** | .58** | .41** | – | ||||
| 5. Current deliberate cognitive processing | .28** | .51** | .55** | .79** | – | |||
| 6. Psychological distress | .22* | .61** | .52** | .72** | .62** | – | ||
| 7. Posttraumatic growth | .02 | .31** | .23* | .21* | .33** | .22* | – | |
| 8. Years since HIV + diagnosis | .10 | −.02 | −.06 | −.10 | −.11 | −.14 | −.02 | – |
Note: PTSD = posttraumatic stress disorder.
p < .05.
p < .01.
Preliminary analyses were conducted to assess assumptions of normality. Analyses of the Revised Rumination scales and the Impact of Event Scale measure revealed small to moderate positive skewness and small to large kurtosis. The Posttraumatic Growth Inventory did not violate normality assumptions. Due to normality violations and small sample size, we used appropriate estimation methods and fit indices to test the hypothesized path models. Specifically, we used the bootstrap-corrected asymptotically distribution-free estimation method (Yuan & Bentler, 1994). To assess the fit of the models, a number of measures of model fit were utilized. First, the comparative fit index (CFI) and the root mean square error of approximation (RMSEA) were used as the comparative fit indices. Second, the goodness-of-fit (GFI) and the adjusted fit index (AGFI) were used as indices of the proportion of observed covariance explained by the model. A nonsignificant χ2 value indicates that the hypothesized model does not differ from the covariance structure of the data. Values for CFI, GFI, and AGFI above .95 and RMSEA values of .06 or less are indicative of a good model fit (Hu & Bentler, 1999). Finally, we examined the significance of indirect effects through bootstrapping and obtained bias-corrected confidence intervals.
Model 1
This model examined the current data’s fit with a previously tested model (Taku et al., 2008) and included direct paths from (a) past deliberate cognitive processing to posttraumatic growth, (b) current intrusive cognitive processing to psychological distress, and (c) psychological distress to posttraumatic growth. Model 1 also hypothesized that the path from (a) past intrusive cognitive processing to psychological distress is mediated by current intrusive cognitive processing, and (b) current deliberate cognitive processing to psychological distress is mediated by current intrusive cognitive processing.
Figure 1 presents the tested paths for Model 1. The path co-efficients that are significant in this model are current deliberate to current intrusive (p < .001), past intrusive to current intrusive (p < .001), and current intrusive to psychological distress (p < .001). The path coefficients from psychological distress to post-traumatic growth and from past deliberate to posttraumatic growth are nonsignificant. Overall, the hypothesized model was a poor fit with the study data, χ2 (7) = 37.25, p < .001 (RMSEA = .20, 90% CI = .14–.26, CFI = .82, GFI = .93, and AGFI = .80). Modification indices did not suggest the inclusion of other paths that would significantly improve the fit of the model. For Model 1, only past deliberate cognitive processing was directly related to posttraumatic growth; current intrusive cognitive processing was directly related to psychological distress. Both past intrusive and current deliberate cognitive processing were indirectly related to psychological distress.
Figure 1.
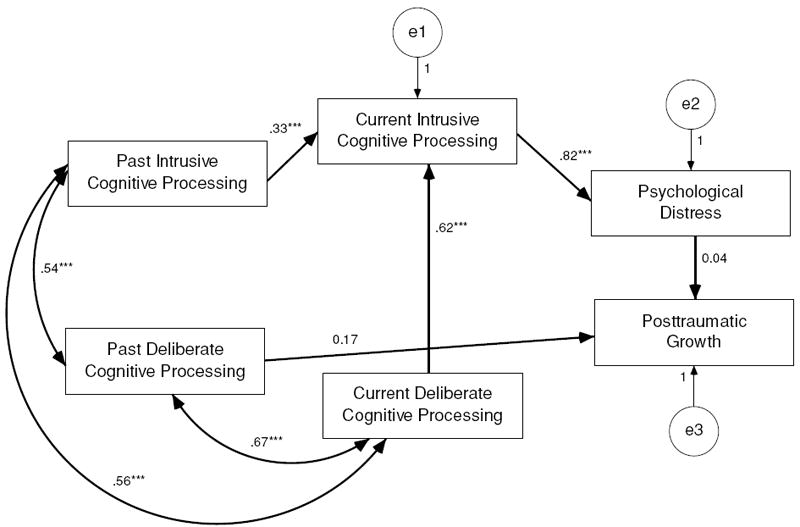
Path analysis examining Model 1, based on previous research findings (Taku et al., 2008), hypothesizing a direct path from past deliberate cognitive processing and indirect paths through current cognitive processing and psychological distress to posttraumatic growth. Curved double-arrow lines represent hypothesized covariances, straight single-arrow lines represent hypothesized paths, *** p < .001. Variance in outcomes explained by the model: psychological distress R2 = .66, posttraumatic growth R2 = .00.
Model 2
This model was designed to examine the fit of the current study data with components of Calhoun and Tedeschi’s (2006) posttraumatic growth model. The variable PTSD Criterion A was added to the model as a means of measuring a seismic event. Further, past deliberate and current intrusive cognitive processing were removed from the model. Model 2 hypothesized (a) the path from PTSD Criterion A to posttraumatic growth is mediated by psychological distress, and (b) mediated by past intrusive cognitive processing and current deliberate cognitive processing. Model 2 also included direct paths from (a) PTSD Criterion A to past intrusive cognitive processing, (b) past intrusive cognitive processing to current deliberate cognitive processing, and (c) current deliberate cognitive processing to posttraumatic growth.
Figure 2 presents the final version of Model 2 taking into account modification indices. Prior to the inclusion of modification indices (e1 to e2, e1 to e3, e2 to e4) the model did not achieve good fit. In the final model, the hypothesized paths from current deliberate cognitive processing to posttraumatic growth and from psychological distress to posttraumatic growth were nonsignificant. Overall, the hypothesized model was a good fit with the study data, χ2 < 1 (RMSEA = .00, 90% CI = .00–.14), CFI = 1.00, GFI = .99, and AGFI = .99).
Figure 2.
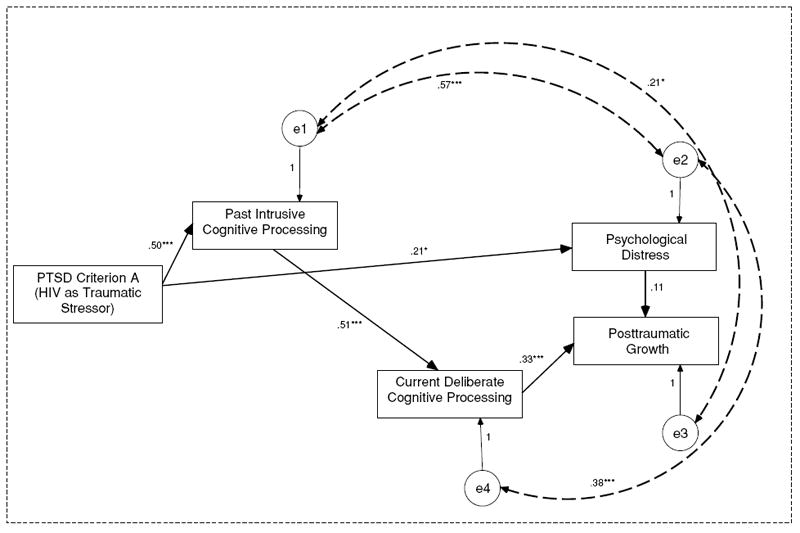
Path analysis examining Model 2, based on part of Calhoun and Tedeschi’s (2006) model, hypothesizing indirect paths from traumatic stressors through past intrusive and current deliberate cognitive processing and psychological distress to posttraumatic growth. Dashed curved double-arrow lines represent covariances added based on modification indices, straight single-arrow lines represent hypothesized paths,* p < .05, ** p < .01, *** p < .001. Variance in predictors and outcomes explained by the model: past intrusive cognitive processing R2 = .25, current deliberate cognitive processing R2 = .26, psychological distress R2 = .07, posttraumatic growth R2 = .01.
Model 3
This model integrates cognitive models of trauma (Creamer et al., 1992; Ehlers & Clark, 2000) and posttraumatic growth theories (Calhoun & Tedeschi, 2006) and hypothesized that psychological distress and posttraumatic growth have both shared and separate pathways. Specifically, Model 3 included (a) direct paths from PTSD Criterion A to past intrusive and past deliberate cognitive processing, (b) indirect paths from PTSD Criterion A through past intrusive to past deliberate cognitive processing to current deliberate cognitive processing to posttraumatic growth, (c) indirect paths from PTSD Criterion A through past intrusive cognitive processing to current deliberate cognitive processing to posttraumatic growth, (d) indirect paths from PTSD Criterion A through past deliberate cognitive processing to current deliberate cognitive processing to posttraumatic growth, (e) indirect paths from PTSD Criterion A through past and current intrusive cognitive processing to psychological distress, and (e) a direct path from psychological distress to posttraumatic growth.
Figure 3 presents the final version of Model 3 taking into account modification indices, which suggested adding a direct path from past intrusive cognitive processing to posttraumatic growth and adding a direct path from past deliberate cognitive processing to psychological distress. Further, the hypothesized direct path from past intrusive cognitive processing to current deliberate cognitive processing was removed. In the final model, the direct path from PTSD Criterion A to past intrusive cognitive processing was significant (p < .001); however, the path from PTSD Criterion A to past deliberate cognitive processing was nonsignificant. The indirect path from PTSD Criterion A to posttraumatic growth was significant: standardized indirect effects = .16 (95% CI = .02–.29), p < .05. The indirect path from PTSD Criterion A to psychological distress was significant: standardized indirect effects = .29 (95% CI = .15–.39), p < .01. The direct path from psychological distress to posttraumatic growth was nonsignificant. Overall, the hypothesized model was a good fit with the study data, χ2 (9) = 11.35, p = .25 (RMSEA = .05, 90% CI = .00–.12; CFI = .99, GFI = .99, and AGFI = .95).
Figure 3.
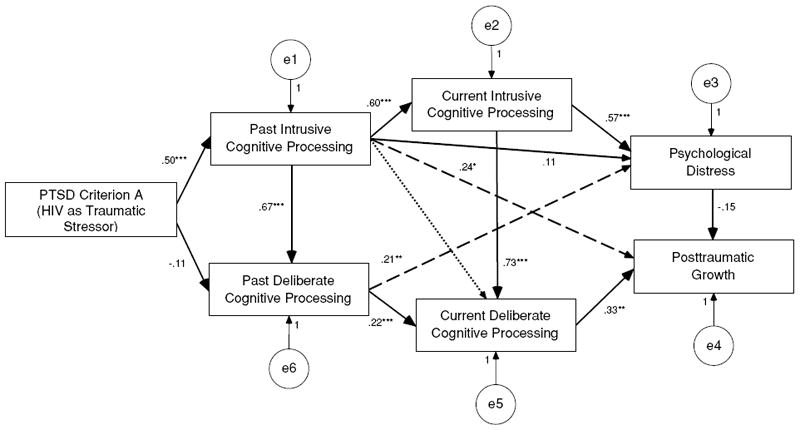
Path analysis examining an integrated model of posttraumatic growth, synthesizing cognitive trauma theories and post-traumatic growth theory (Model 3), hypothesizing direct paths from past intrusive and current deliberate cognitive processing, and multiple indirect paths from the traumatic stressor through past and current cognitive processing, and psychological distress to post-traumatic growth. Straight lines represent hypothesized paths that remained in the final model, long dashed lines represent paths added to the final model based on modification indices, and short dashed lines represent hypothesized paths removed from the final model, * p < .05, ** p < .01, ** p < .001. Variance in predictors and outcomes explained by the model: past intrusive cognitive processing R2 = .24, past deliberate cognitive processing R2 = .39, current intrusive cognitive processing R2 = .35, current deliberate cognitive processing R2 = .70, psychological distress R2 = .62, posttraumatic growth R2 = .18.
Figures 1, 2, and 3 demonstrate the likenesses and differences among the three proposed models and include the standardized parameter estimates. Although both Models 2 and 3 achieved good fit with study data, only Model 3 accounted for large portions of variance in outcome variables, including 60% of the variance in psychological distress and 17% of the variance in posttraumatic growth.
DISCUSSION
This study examined three posttraumatic growth models of the possible shared and separate pathways from PTSD Criterion A and cognitive processing to psychological distress and posttraumatic growth in a sample of individuals in care for HIV. Our findings are consistent with Calhoun and Tedeschi’s (2006) posttraumatic growth model indicating an indirect relationship between PTSD Criterion A and posttraumatic growth through multiple cognitive processing paths. Additionally, consistent with cognitive trauma models, there was a significant indirect relationship between PTSD Criterion A and psychological distress through past and current intrusive cognitive processing. These findings contribute to the fields of posttraumatic growth and trauma research in several ways.
First, the current study is one of few studies to examine the impact of a potentially traumatic stressor on both psychological distress and posttraumatic growth, and the only study we are aware of to examine these variables while concurrently examining cognitive processing. Theories of posttraumatic growth and cognitive theories of trauma emphasize that the impact of a traumatic stressor is crucial in the development of both posttraumatic growth and PTSD. Further, it is well established that perceptions of the traumatic stressor have an effect on both immediate and long-term responses (Ehlers & Clark, 2000). However, within the field of posttraumatic growth research, this perception has rarely been examined.
Second, this study provided evidence for both shared and separate pathways to psychological distress and posttraumatic growth. Model 3 indicates that past intrusive cognitive processing was more likely in participants who perceived their HIV diagnosis as a traumatic stressor. Further, past intrusive cognitive processing was also directly and indirectly related to current cognitive processing, psychological distress, and posttraumatic growth. This is consistent with trauma theories that suggest intrusive cognitive processing is common immediately following a traumatic event and may lead to continued intrusive cognitive processing and/or other types of cognitive processing (Ehlers & Clark, 2000). The current study suggests a better understanding of the timing of different types of cognitive processing would improve prediction of likely outcomes. Specifically, past intrusive cognitive processing was directly related to posttraumatic growth, whereas past deliberate cognitive processing was directly related to psychological distress. However, when examined more recently, these relationships were reversed. Further, although intrusive cognitive processing is generally perceived as disruptive and unwanted, it can comprise both positive and negative intrusive ruminative thoughts (Rachman, 1981) that may be necessary in the immediate aftermath of a trauma as part of the process of posttraumatic growth. Finally, in the immediate aftermath of a traumatic experience, the deliberate engagement in meaning making may be premature and may not lead to the successful development of meaning, thus contributing to later psychological distress.
Third, this study provides further evidence for the co-occurrence of distress and posttraumatic growth. Although a controversial discussion in the field of posttraumatic growth, our findings support the conclusion that these are distinct and separate constructs and the presence of one does not preclude the presence of the other. Findings indicated a small positive relationship between psychological distress and posttraumatic growth (r = 0.22, p < .05). Moreover, participants in the current study were experiencing significant levels of distress as evidenced by the mean score on the IES of 25.3 (SD = 18.2), with 45% of the participants scoring in the moderate to severe distress range.
Findings should be understood within the limitations of the study. First, the retrospective recall of emotional responses and cognitive processing related to a highly distressing event is a major limitation. Recall may have been influenced by other unknown factors present during the acute aftermath of receiving an HIV diagnosis and/or may have been influenced by participants’ current mood. Further, participants engaging in retrospective recall may not have been able to identify the subtle nuances in cognitive processing, consequently limiting interpretation of results. Second, although the constructs examined are temporally based, the study design is cross-sectional. Thus, causal relationships cannot be identified. Prospective longitudinal studies are needed to reliably identify the temporal relationship between variables. Third, the sample size is small for the type of analysis utilized. Although significant findings are considered reliable, the study was under-powered and may have been unable to identify small but significant relationships between variables. Additionally, there may have been insufficient power to reject the null hypothesis when considering model fit (i.e., nonsignificant chi-square value). Therefore, our use of multiple fit indices was imperative to support goodness of fit. Fourth, the Rumination Scale-Revised (A. Cann, personal communication, January 25, 2007) has not been widely used. However, data from the current study have been provided to the measure authors for validation purposes. Fifth, at the time of data collection for this study, a measure to assess whether an event was perceived as seismic was not available. Therefore, a conservative measure, namely PTSD Criterion A, was applied. Since the completion of this data collection, the Core Beliefs Inventory (Cann et al., 2010) has been developed as a means of examining the seismic nature of a traumatic event. Sixth, approximately a third of the participants met PTSD Criterion A. These findings likely reflect an important factor in the HIV epidemic: With the availability of highly active antiretroviral therapy, HIV is no longer considered a progressive, fatal disease; rather it is now considered a chronic, life-threatening disease. With treatment, one can continue to live a healthy life for many years. Finally—both a strength and a limitation—the majority of the study sample was African American and represent an underserved and low socioeconomic status population. Therefore, these findings may not be generalizable to the general population, and have limited generalizability to nonurban or predominately Caucasian HIV populations.
In conclusion, this study is timely in that it is the first study we are aware of to examine both a potentially traumatic stressor and cognitive processing as they relate to psychological distress and posttraumatic growth. Our findings highlight the importance of timing related to cognitive processing, and begin to tease apart the shared and separate pathways to trauma outcomes. Additionally, this study examined these constructs in a sample of individuals in care for HIV/AIDS, a population that to date has not been adequately represented in the trauma and posttraumatic growth literature. Due to some of the unique factors related to having a diagnosis of HIV, future research examining posttraumatic growth in this population should examine the relationship between posttraumatic growth and HIV-related stigma. Further, prospective longitudinal research is needed to examine the temporal relationship between cognitive processing and posttraumatic growth. Finally, our findings demonstrate the importance of evaluating the traumatic impact of receiving an HIV diagnosis, understanding the cognitive processing that occurs immediately after receiving a diagnosis of HIV, and addressing intrusive cognitive processing that continues to occur long after the initial diagnosis.
Acknowledgments
This research was partly funded by a dissertation grant awarded to the first author from the Institute of Psychology at Illinois Institute of Technology and was supported by grants T32-MH020031, P30 MH62294 (Center for Interdisciplinary Research on AIDS), and K23-MH076671 from the National Institute of Mental Health. The authors gratefully acknowledge our community collaborations with the HIV Care Program formally located within Michael Reese Hospital in Chicago, IL, especially Arthur Moswin and Norma Rolfsen, as well as the research assistance of Lisa Bauer, Melissa Mattson, Kristin Neil, and Sarah Thilges.
Contributor Information
Vienna R. Nightingale, Epidemiology and Public Health, Yale University School of Medicine
Tamara G. Sher, Institute of Psychology, Illinois Institute of Technology
Nathan B. Hansen, Department of Psychiatry, Yale University School of Medicine
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Calhoun LG, Cann A, Tedeschi RG, McMillan J. A correlational test of the relationship between posttraumatic growth, religion, and cognitive processing. Journal of Traumatic Stress. 2000;13:521–527. doi: 10.1023/A:1007745627077. [DOI] [PubMed] [Google Scholar]
- Calhoun LG, Tedeschi RG. The foundations of posttraumatic growth: An expanded framework. In: Calhoun LG, Tedeschi RG, editors. Handbook of posttraumatic growth. Mahwah, NJ: Erlbaum; 2006. pp. 3–23. [Google Scholar]
- Cann A, Calhoun LG, Tedeschi RG, Kilmer RP, Gil-Rivas V, Vishnevsky T, et al. The Core Beliefs Inventory: A brief measure of disruption in the assumptive world. Anxiety, Stress, & Coping. 2010;23:1477–2205. doi: 10.1080/10615800802573013. [DOI] [PubMed] [Google Scholar]
- Cordova MJ, Cunningham LLC, Carlson CR, Andrykowski MA. Posttraumatic growth following breast cancer: A controlled comparison study. Health Psychology. 2001;20:176–185. [PubMed] [Google Scholar]
- Cordova MJ, Giese-Davis J, Golant M, Kronenwetter C, Chang V, Spiegel D. Breast cancer as trauma: Posttraumatic stress and posttraumatic growth. Journal of Clinical Psychology in Medical Settings. 2007;14:308–319. [Google Scholar]
- Creamer M, Burgess P, Pattison P. Reaction to trauma: A cognitive processing model. Journal of Abnormal Psychology. 1992;101:452–459. doi: 10.1037//0021-843x.101.3.452. [DOI] [PubMed] [Google Scholar]
- Davis CG. The tormented and the transformed: Understanding responses to loss and trauma. In: Neimeyer RA, editor. Meaning reconstruction and the experience of loss. Washington, DC: American Psychological Association; 2000. pp. 137–155. [Google Scholar]
- Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy. 2000;38:319–345. doi: 10.1016/s0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: A measure of subjective stress. Psychosomatic Medicine. 1979;41:209–217. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Linley PA, Joseph S. Positive change following trauma and adversity: A review. Journal of Traumatic Stress. 2004;17:11–21. doi: 10.1023/B:JOTS.0000014671.27856.7e. [DOI] [PubMed] [Google Scholar]
- Martin L, Kagee A. Lifetime and HIV-related PTSD among persons recently diagnosed with HIV. AIDS and Behavior. doi: 10.1007/s10461-008-9498-6. in press. [DOI] [PubMed] [Google Scholar]
- Martin LL, Tesser A. Clarifying our thoughts. In: Wyer RS, editor. Ruminative thought: Advances in social cognition. Vol. 9. Mahwah, NJ: Erlbaum; 1996. pp. 189–209. [Google Scholar]
- Morris BA, Shakespeare-Finch J, Rieck M, Newbery J. Multidimensional nature of posttraumatic growth in an Australian population. Journal of Traumatic Stress. 2005;18:575–585. doi: 10.1002/jts.20067. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Responses to depression and their effects on the duration of depressive episodes. Journal of Abnormal Psychology. 1991;100:569–582. doi: 10.1037//0021-843x.100.4.569. [DOI] [PubMed] [Google Scholar]
- Rachman S. Emotional processing. Behavior Research and Therapy. 1981;18:51–60. doi: 10.1016/0005-7967(80)90069-8. [DOI] [PubMed] [Google Scholar]
- Resick PA. Stress and trauma. New York: Psychology Press; 2001. [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 5. Boston: Allyn and Bacon; 2007. [Google Scholar]
- Taku K, Calhoun LG, Cann A, Tedeschi RG. The role of rumination in the coexistence of distress and posttraumatic growth among bereaved Japanese university students. Death Studies. 2008;32:428–444. doi: 10.1080/07481180801974745. [DOI] [PubMed] [Google Scholar]
- Tedeschi RG, Calhoun LG. The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress. 1996;9:455–471. doi: 10.1007/BF02103658. [DOI] [PubMed] [Google Scholar]
- Tedeschi RG, Calhoun LG. Posttraumatic growth: Conceptual foundations and empirical evidence. Psychological Inquiry. 2004;15:1–18. [Google Scholar]
- Weathers FW, Keane TM. The Criterion A problem revisited: Controversies and challenges in defining and measuring psychological trauma. Journal of Traumatic Stress. 2007;20:107–121. doi: 10.1002/jts.20210. [DOI] [PubMed] [Google Scholar]
- Widows MR, Jacobsen PB, Booth-Jones M, Fields KK. Predictors of posttraumatic growth following bone marrow transplantation for cancer. Health Psychology. 2005;24:266–273. doi: 10.1037/0278-6133.24.3.266. [DOI] [PubMed] [Google Scholar]
- Witteveen AB, Bramsen I, Hovens JE, van der Ploeg HM. Utility of the Impact of Event Scale in screening for posttraumatic stress. Psychological Reports. 2005;97:297–308. doi: 10.2466/pr0.97.1.297-308. [DOI] [PubMed] [Google Scholar]
- Yuan KH, Bentler PM. Bootstrap-corrected ADF test statistics in covariance structure analysis. British Journal of Mathematical and Statistical Psychology. 1994;47:63–84. doi: 10.1111/j.2044-8317.1994.tb01025.x. [DOI] [PubMed] [Google Scholar]


