Abstract
BACKGROUND:
Patients with lung cancer often experience a reduction in exercise tolerance, muscle weakness and decreased quality of life. Although the effectiveness of pulmonary rehabilitation programs is well recognized in other forms of cancers and in many pulmonary diseases, few researchers have studied its impact in patients with lung cancer, particularly in those awaiting lung resection surgery (LRS).
OBJECTIVES:
To investigate the feasibility of a short, home-based exercise training program (HBETP) with patients under investigation for non-small cell lung cancer and potential candidates for LRS, and to determine the effectiveness of this program on exercise tolerance, skeletal muscle strength and quality of life.
METHODS:
Sixteen patients with lung cancer awaiting LRS participated in a four-week HBETP including moderate aerobic activities (walking and cycling) and muscle training performed three times weekly. Before and after the intervention, a cardiopulmonary exercise test, a 6 min walk test and the assessment of muscle strength and quality of life were performed.
RESULTS:
Thirteen patients completed the four-week HBETP and all the patients completed >75% of the prescribed exercise sessions. The duration of the cycle endurance test (264±79 s versus 421±241 s; P<0.05) and the 6 min walk test distance (540±98 m versus 568±101 m; P<0.05) were significantly improved. Moreover, the strength of the deltoid, triceps and hamstrings were significantly improved (Δ post-pre training 1.82±2.83 kg, 1.32±1.75 kg and 3.41±3.7 kg; P<0.05, respectively).
CONCLUSION:
In patients with lung cancer awaiting LRS, HBETP was feasible and improved exercise tolerance and muscle strength. This may be clinically relevant because poor exercise capacity and muscle weakness are predictors of postoperative complications.
Keywords: Exercise, Exercise tolerance, Home-based pulmonary rehabilitation, Lung cancer, Muscle strength, Quality of life, Training
Abstract
HISTORIQUE :
Les patients atteints d’un cancer du poumon sont souvent moins tolérants à l’exercice et présentent souvent une faiblesse musculaire et une diminution de leur qualité de vie. Même si l’efficacité des programmes de réadaptation pulmonaire est reconnue pour d’autres formes de cancers et de nombreuses maladies pulmonaires, peu de chercheurs en ont étudié les répercussions en cas de cancer du poumon, notamment chez les personnes en attente d’une résection pulmonaire (RP).
OBJECTIFS :
Examiner la faisabilité d’un court programme d’exercices à domicile (CPED) chez des patients en cours d’examens diagnostiques d’un cancer pulmonaire non à petites cellules qui étaient des candidats potentiels à une RP, et déterminer l’efficacité de ces programmes sur la tolérance à l’exercice, la force musculaire squelettique et la qualité de vie.
MÉTHODOLOGIE :
Seize patients atteints d’un cancer du poumon en attente d’une RP ont participé à un CPED de quatre semaines comportant des activités aérobiques modérées (marche et vélo) et un entraînement musculaire à une fréquence de trois fois par semaine. Avant et après l’intervention, les patients ont subi une épreuve d’effort cardiorespiratoire, une épreuve d’effort de 6 minutes et une évaluation de la force musculaire et de la qualité de vie.
RÉSULTATS :
Treize patients ont effectué le CPED de quatre semaines et tous les patients ont effectué au moins 75 % des séances d’exercices prescrites. La durée du cycle de leur épreuve d’endurance (264±79 s par rapport à 421±241 s; P<0,05) et la distance de leur épreuve d’effort de 6 minutes (540±98 m par rapport à 568±101 m; P<0,05) s’amélioraient considérablement, de même que la force de leurs deltoïdes, de leurs triceps et de leurs ischiojambiers (Δ après-avant l’entraînement 1,82±2,83 kg, 1,32±1,75 kg et 3,41±3,7 kg; P<0,05, respectivement).
CONCLUSION :
Chez les patients atteints d’un cancer du poumon en attente d’une RP, le CPED était faisable et améliorait la tolérance à l’exercice et la force musculaire. Ce peut être pertinent sur le plan clinique, car une capacité à l’exercice médiocre et une faiblesse musculaire sont des prédicteurs de complications postopératoires.
With 1.6 million new cases diagnosed each year and 1.3 million deaths, lung cancer is the leading cause of cancer-related deaths worldwide and represents a pressing health issue that generates significant personal and social costs (1).
Patients with lung cancer often experience greater fatiguability, a reduction in exercise tolerance, muscle weakness and compromised quality of life (QoL) as a direct consequence of their disease or as an indirect consequence of their cancer therapy (2–4). For individuals with localized non-small cell lung cancer (NSCLC), lung resection surgery (LRS) offers the best chance of cure. Although survival rates are improved following the surgery, morbidity and mortality rates resulting from postoperative cardiopulmonary complications remain considerable. Moreover, because of the link between low exercise capacity and cardiopulmonary complications following LRS (5–7), exercise tolerance is an important element in the decision-making process regarding the feasibility of lung cancer resection, especially in patients with low aerobic capacity.
Although the effectiveness of exercise-based rehabilitation programs are well recognized to improve exercise capacity, muscle strength and QoL for patients with various pulmonary disorders (8,9), the role of this intervention in an oncology setting is less well defined. However, there is emerging literature suggesting that exercise-based rehabilitation may improve oxygen uptake, physical fitness, muscle function and QoL in cancer patients (10,11). In lung cancer patients, exercise-based rehabilitation has received increased attention (12–15), with some promising studies demonstrating that it is possible to improve exercise performance and symptoms without increasing the risk of promoting cancer progression (12,13,16).
Consequently, the implementation of a preoperative exercise-based rehabilitation program focused on improving exercise capacity and muscle function could have significant positive outcomes in patients with lung cancer, notably by reducing postoperative mortality and morbidity (7). In this regard, it seems clinically relevant to use the preoperative waiting period to increase the exercise tolerance of patients with lung cancer. However, implementation of exercise-based rehabilitation in a supervised setting would be difficult, due to a lack of accessibility of resources and also because the preoperative period itself is a very stressful and busy time for the patients, a context that may impact on their willingness to participate in such a program (16,17).
The effectiveness and safety of a home-based exercise training intervention has already been demonstrated in patients with severe emphysema awaiting lung volume reduction surgery (18). Those results were recently confirmed in a randomized multicentre clinical trial on home-based pulmonary rehabilitation in chronic obstructive pulmonary disease (COPD) that was conducted in 10 participating centres across Canada (19). However, its implementation and efficacy in patients with lung cancer needs to be addressed.
Therefore, we aimed to prospectively examine the feasibility of a short (four week), home-based exercise training program (HBETP) with patients under investigation for NSCLC and potential candidates for LRS, and to determine the effectiveness of this program on exercise capacity, muscle strength and QoL.
METHODS
Study design
The present analysis was a nonrandomized interventional study conducted at the Institut universitaire de cardiologie et de pneumologie de Québec (IUCPQ) (Sainte-Foy, Quebec). The research protocol was approved by the institutional ethics committee. All of the participants provided written informed consent before study enrollment.
Potentially eligible patients (men or women, between 45 and 80 years of age, under investigation for NSCLC) were recruited from the Clinique spécialisée en pneumologie of IUCPQ. Exclusion criteria were as follows: oxygen-pulsed saturation (SpO2) <80% during the cardiopulmonary exercise test; contraindications to exercise testing (per American Thoracic Society [ATS]/American College of Chest Physicians Exercise Testing Guidelines [20]); a history of significant cardiovascular disease, hypertension, diabetes or musculoskeletal concerns that might limit the ability of these subjects to perform active exercises; and severe psychiatric illness compromising adherence to training rehabilitation.
A complete assessment of pulmonary function, exercise capacity, muscle strength and QoL was performed before and after completion of the four-week HBETP. The full assessment was performed in one day and all tests were administered in the same order pre- and post-HBETP. Care was taken to allow a 2 h rest period between incremental and constant cycling tests, and a 20 min rest period between the two 6-min walk tests (6MWTs).
Assessments
Anthropometric and pulmonary measurements:
Weight and height were measured to determine body mass index. Standard pulmonary function tests including spirometry, lung volumes and carbon monoxide diffusion capacity, were performed for all subjects according to previously described guidelines (21) and compared with predicted reference values (22,23).
Exercise capacity:
Exercise capacity was assessed using the following exercise tests:
Incremental cycling exercise test:
Peak exercise capacity and oxygen consumption were determined during incremental cycle ergometry with 12-lead electrocardiogram monitoring (Cardiosoft, Corina, USA) as originally described by Jones et al (3) and following the ATS guidelines (20). Briefly, the tests were performed on an electronically braked cycle ergometer (Quinton Corival 400; A–H Robins, USA) with breath-by-breath expired gas analysis (Sensor Medics, Vmax Legacy, USA) to monitor ventilation, oxygen consumption (V̇O2), carbon dioxide output and respiratory exchange ratio. After 3 min of rest, participants began unloaded cycling for 1 min. Each subsequent minute, workload was increased by 10 W to 20 W until a symptom limitation was achieved. During exercise, heart rate (ECG Cardiosoft, Corina, USA) and SpO2 (OSM2 Hexoximeter, Radiometer, Denmark) were monitored continuously, whereas blood pressure was measured every 2 min (Quinton 410, A–H Robins Cie, USA). Dyspnea and leg fatigue were evaluated every 2 min using a modified Borg scale for perceived exertion (24).
Constant workrate cycle exercise:
The constant workrate cycle exercise test was monitored similarly to the maximal exercise test. After 1 min of unloaded cycling, patients were asked to pedal to exhaustion at 80% of the peak workload determined during the incremental test. Heart rate, dyspnea Borg score and oxygen saturation were monitored. The endurance time was defined as the duration of the test excluding the 1 min warm-up period.
6MWT:
According to the ATS guidelines (25), the 6MWT was conducted in an enclosed corridor on a flat, 30 m long course between two cones. Patients were instructed to cover the longest distance possible in 6 min with or without pause. During the test, only standardized encouragement was given to the patient (25). The test was performed twice and the greater distance was recorded.
Muscle strength:
Quadriceps strength of the dominant leg was assessed by measuring maximum voluntary contraction. Subjects were seated in a recumbent chair (N-K 330 Exercise Table; N-K Products, USA) with 90° knee flexion and the ankle attached to a strain gauge (Hewlett-Packard, USA). Maximum voluntary contraction of the dominant biceps, triceps, deltoid and hamstring were measured using a hand-held dynamometer (Microfet, Hoggan Inc, USA) using the method described and validated by Andrews et al (26). Finally, maximal prehension strength was assessed using a hydraulic dynamometer (Jamar, Lafayette Instrumet Company, USA). Muscle strength assessment was performed during the rest period between cycling tests. Reported values for maximum voluntary contraction of all muscles are the mean of the two strongest contractions and strength is reported in kilograms.
QoL:
QoL was assessed using three standard questionnaires described and validated for patients with lung cancer. The 36-item Short-Form Health Survey (SF-36) was selected as a generic questionnaire to assess QoL for its ease of administration and because it has comparative normative values (27). A French-Canadian version of the SF-36 is currently available and was previously validated (27). Cancer-related QoL was assessed using the self-reported European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC QLQ-30) including the lung cancer-specific questionnaire QLQ-LC13 (28,29). This questionnaire was developed and validated for cancer patients. It includes 30 items divided into functional, symptom and health-related subscales. Finally, the French Canadian version of the Hospital Anxiety and Depression Scale (HADS) was used to identify patients with anxiety disorders or depression (30). It has 14 questions divided into an anxiety subscale (HADS-A) and a depression subscale (HADS-D). Questionaires were systematically completed at the beginning of the evaluation day.
HEBTP
Following the initial assessment, participants began a four-week exercise-training program. This was a self-monitored and minimally supervised home-exercise program. Exercise training modalities and intensity were adapted to patient’s individual condition. It included aerobic and strength exercises three to five times per week for four weeks. Aerobic training was performed on a loaned portable ergocycle on which resistance could be manually adjusted. The target intensity corresponded to 60% to 80% of the peak workload achieved during the incremental cycling exercise test, aiming for a cumulative time of 30 min. Patients were also instructed to reduce the intensity of training in case of a dyspnea Borg score≥ 6. Free weights (1 kg to 2 kg) and gravity-resisted exercises were used to train the muscle groups of the upper limbs (biceps curl, wall push-up, lateral shoulder raise), lower limbs (wall squat, hips raise) and abdominal wall (sit up). Ten repetitions of each movement were initially performed. The number of repetitions was progressively increased, as tolerated, until two sets of 15 repetitions were achieved. Home training periods, training intensity and adverse events were noted in a diary. Individual teaching with practice and feedback were performed by a kinesiologist before the program to ensure complete understanding from participants. Furthermore, weekly telephone follow-ups were conducted to ensure patient adherence, to adjust the exercise prescription and to follow potential adverse events. This strategy was previously used successfully in clinical trials involving patients with COPD (19) and patients with emphysema in preparation for lung volume reduction surgery (18).
Feasibility outcomes
To assess the feasibility of the HBETP, recruitment rate, completion rate, adherence, adverse events, subjective perception of obstacles, and benefits and acceptability were collected and analyzed. Recruitment rate was defined as the ratio of the recruited patients to those who were eligible. Completion rate was defined as the proportion of participants who completed all of the intervention from the moment of the initial assessment. Adherence was calculated from the ratio of the number of completed exercise sessions over the number of prescribed sessions (12). In pulmonary rehabilitation programs involving COPD patients, the reported adherence rates vary between 74% and 83% (31–33). Therefore, a similar adherence rate was anticipated in the present population. It was determined a priori that patients who attended nine training sessions during the four-week period (75%) would be classified as meeting the adherence requirement. In addition, adverse events were systematically tracked during the weekly telephone call.
Finally, a motivational survey developed by the authors was used to describe the subjective perception of obstacles and benefits, and the acceptability of the program. The survey also provided an overview of which situations may increase or decrease the motivation of the patient to perform physical activities and asked questions about perception of physical fitness. Questions such as the following were asked: “Overall, how would you rate your current physical condition?”; “How were you motivated to engage in the HBETP? ”; “To what extent do you think your participation in this HBETP was good for you?” All questions were answered on a scale from 1 to 7. A high score generally indicates a positive association, except for the obstacles scales in which a higher score indicates more perceived obstacles.
Statistical analysis
Baseline subject characteristics, including demographics, pulmonary function, muscle strength and score on all exercise and functional tests, were reported using descriptive data (mean ± SD). Isotime was defined as the highest equivalent duration reached pre- and post-HBETP for the cycle endurance test. Pre- and post-training comparisons were made using a paired t test; P<0.05 was considered to be statistically significant. The data were analyzed using SAS version 9.2 (Service Pack 4, SAS Institute Inc, USA).
RESULTS
Feasibility outcomes
A flow chart of the study is presented in Figure 1. From May 2009 to November 2010, 72 patients were initially identified as potentially eligible. After detailed review of medical history, 52 patients were excluded because they were ineligible (n=32) and 20 patients declined to participate. The main reasons for nonconsent were lack of time (n=6); not specified (n=6); lack of interest about engaging in a research project (n=5); or high level of anxiety (n=3).
Figure 1).
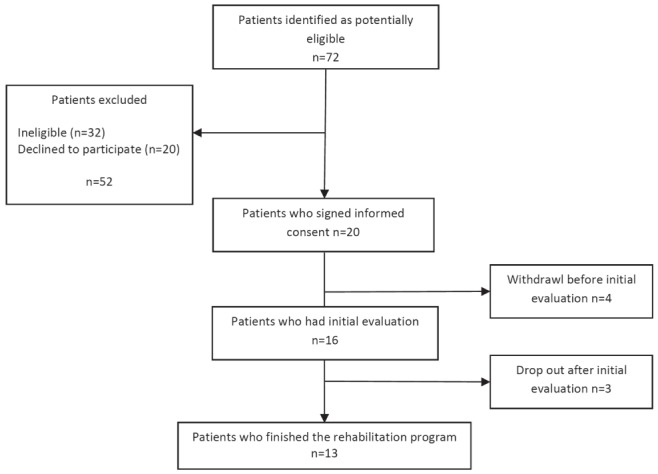
Flow diagram of the study
Finally, 20 patients consented to participate over the 40 who were truly eligible, yielding a recruitment rate of 50%. Among those who consented, 16 completed the baseline evaluation. Four patients were excluded before the baseline evaluation due to scheduled surgery within one week of consent (n=3) or clinical deterioration (n=1). Three patients failed to complete the rehabilitation program due to clinical deterioration (n=2) or psychological distress (n=1). Thus, 13 patients completed all the HBRTP, yielding a completion rate of 81%. They performed a mean of 15±5 aerobic exercise sessions and a mean of 10±4 muscle strengthening sessions of the 12 prescribed. All of the participants reached the adherence goal of 75% (nine sessions) with a mean adherence of 125% and 83% for the aerobic and strength prescriptions, respectively. Finally, no adverse events were reported by patients during telephone follow-up.
Participant characteristics
The baseline characteristics for the 13 patients who completed the four-week HBETP are presented in Table 1. Patients who completed the HBETP had a relatively preserved exercise capacity with a mean percentage of predicted peak V̇O2 of 107%. Some patients had one or more of the following comorbidities: COPD (n=5), arterial hypertension (n=5), dyslipidemia (n=3), type 2 diabetes (n=2) and anxiety (n=2). No significant difference for physiological or psychological characteristics were observed between patients who completed the program and those who did not.
TABLE 1.
Subject characteristics (n=13)
| Variable | Patients |
|---|---|
| Age, years | 59±9 |
| Sex, male/female, n/n | 5/8 |
| Body mass index, kg/m2 | 27±7 |
| Smoking status, n | |
| Current | 6 |
| Former | 4 |
| Never smoker | 3 |
| V̇O2 peak, mL/kg/min | 22±78 |
| V̇O2 peak, % predicted | 107±23 |
| Pulmonary function | |
| FEV1, L | 2.18±0.87 |
| FEV1, % predicted | 79±21 |
| Forced expiratory capacity, L | 3.33±1.04 |
| FVC, % predicted | 97±19 |
| FEV1/FVC, % | 64±9 |
| Total lung capacity, L | 5.88±1.28 |
| Total lung capacity, % predicted | 102±13 |
| Residual volume, L | 2.45±0.82 |
| Residual volume, % predicted | 117±36 |
| DLco, mL/min/mmHg | 18.02±7.61 |
| DLco, % predicted | 80±24 |
| Diagnosis, n | |
| Adenocarcinoma | 9 |
| Squamous carcinoma | 1 |
| Typical carcinoid tumor | 1 |
| Round pneumonia | 1 |
| Langerhans cell histiocytosis | 1 |
| Cancer stage, n | |
| I | 5 |
| II | 4 |
| III | 0 |
| IV | 2 |
| Treatment during rehabilitation, n | |
| Awaiting surgery | 10 |
| Chemotherapy | 1 |
| Palliative chemotherapy | 1 |
| Palliative radiotherapy + chemotherapy | 1 |
Data presented as mean ± SD unless otherwise indicated. DLco Diffusion capacity of carbon monoxide; FEV1 Forced expiratory volume in 1 s; FVC Forced vital capacity; V̇O2 Oxygen uptake
Physiological effects of training
Physiological data before and after completion of the HBETP are presented in Table 2. Compared with pre-HBETP, the post-HBETP peak V̇O2, peak workload and pulmonary function were not significantly different. Constant workrate cycle exercise duration significantly improved by 60% (157±195 s), with seven patients increasing their endurance time by more than 100 s (Figure 2, panels A and B). The 6MWT distance improved by 28±29 m (540±98 prerehabilitation versus 568±101 postrehabilitation; P<0.05), with seven patients increasing their 6MWT distance by more than 26 m (Figure 2, panels C and D). Compared with pre-HBETP, isotime V̇O2, carbon dioxide output, ventilation and respiratory exchange ratio were reduced after the HBETP (Figure 3).
TABLE 2.
Physiological response at peak incremental exercise and at the end of constant workrate exercise before and after the four-week home-based exercise training program
| Variable |
Rehabilitation
|
P | |
|---|---|---|---|
| Pre | Post | ||
| Incremental cycling exercise | |||
| V̇O2peak, mL/kg/min | 21.6±7.8 | 23.3±7.5 | NS |
| V̇O2peak, % predicted | 107±23 | 103±25 | NS |
| V̇O2peak, L/min | 1.63±0.64 | 1.75±0.71 | NS |
| Peak heart rate, beats/min | 144±26 | 149±24 | NS |
| Peak workrate, W | 110±53 | 118±50 | NS |
| V̇Epeak, L/min | 66.1±27.4 | 68.0±20.3 | NS |
| RRpeak, breath/min | 39±11 | 42±11 | NS |
| RERpeak | 1.22±0.11 | 1.23±0.10 | NS |
| SpO2peak, % | 95±5 | 96±4 | NS |
| Constant workrate cycling exercise | |||
| Duration, s | 264±79 | 421±241 | <0.05 |
| Workrate, W | 88±42 | 88±42 | NS |
| V̇O2, mL/kg/min | 21.4±7.3 | 21.6±7.2 | NS |
| Heart rate, beats/min | 144±26 | 146±29 | NS |
| V̇E, L/min | 60.9±23.8 | 61.7±25.2 | NS |
| RR, breaths/min | 38±11 | 41±11 | NS |
| RER | 1.18±0.07 | 1.08±0.10 | <0.05 |
| SpO2, % | 95±3 | 97±3 | NS |
| Dyspnea Borg score | 7±2 | 7±2 | NS |
| Leg fatigue Borg score | 7±2 | 7±2 | NS |
Data presented as mean ± SD unless otherwise indicated. NS Not statistically significant; RER Respiratory exchange ratio; RR Respiratory rate; SpO2 Pulse oxygen saturation; V̇E Ventilation; V̇O2 Oxygen uptake
Figure 2).
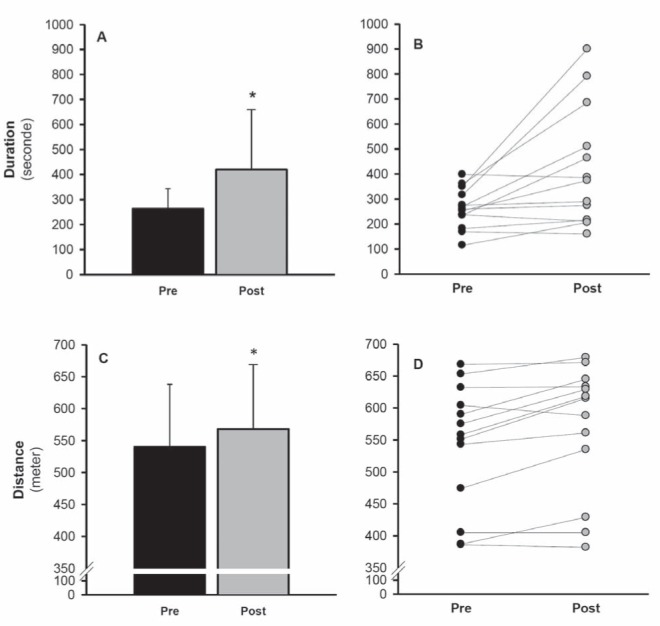
Group mean ± SD (panels A and C) and individuals values (panels B and D) for the endurance time during the constant workrate cycling exercise (panels A and B) and for the 6 min walk distance (panels C and D) at the pre- (closed bars) and post- (open bars) rehabilitation assessment. *P<0.05
Figure 3).
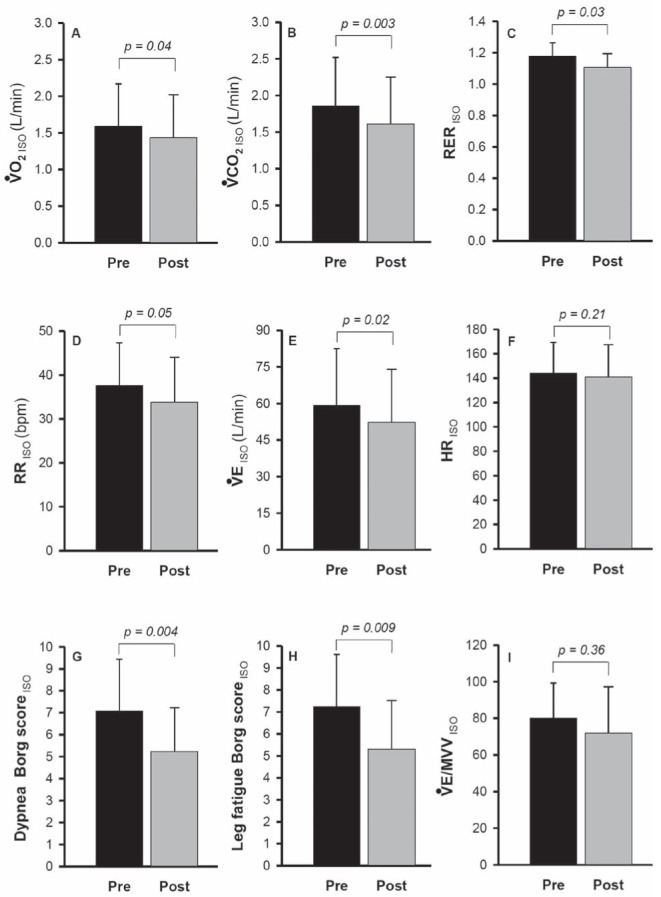
Group mean ± SD isotime values during the constant workate cycling exercise test for peak oxygen consumption (V̇O2, panel A); carbon dioxide output (V̇CO2, panel B); respiratory exchange ratio (RER, panel C), respiratory rate (RR, panel D), ventilation (V̇E, panel E), heart rate (HR, panel F), dyspnea Borg score (panel G), fatigue Borg score (panel H) and V̇E /maximum voluntary ventilation (MVV) ratio (panel I), pre- rehabilitation (pre, closed bars) and postrehabilitation (post, open bars)
Strength of the deltoid, triceps and hamstring muscles increased significantly with training by 1.82±2.83 kg, 1.32±1.75 kg and 3.41±3.7 kg, respectively (P<0.05). This corresponded to a strength improvement of 18±31%, 14±25% and 27±40%, respectively (P<0.05). In contrast, changes in hand grip, biceps and quadriceps strength with training were not statistically significant.
Motivational survey
After the HBETP, perceived physical fitness improved significantly (3.38±1.26 pre-HBETP versus 4.69±0.95 post-HBETP; P<0.05). The most commonly perceived benefits reported by the patients were: helped to start performing physical activities (n=6); improved dyspnea (n=5); improved strength (n=3); and having more energy (n=3). The most important obstacle was the lack of time to perform the program and the difficulties in integrating it into an already busy schedule of several medical appointments. Nevertheless, patients believed that the intervention was relevant for individuals with lung cancer, that they were willing to encourage a friend with cancer to engage in such a program and that they were globally very satisfied with their participation (mean 5.85, 6.08 and 6.07 on the 0 to 7 scale, respectively).
QoL
The impact of the HBETP on health-related QoL is presented in Table 3. With the exception of an improvement in the depression scale of the HADS, there were no significant changes for any measure of QoL after the intervention.
TABLE 3.
Quality of life before and after the four-week home-based exercise training program
|
Rehabilitation
|
P | ||
|---|---|---|---|
| Pre | Post | ||
| SF-36 domains | |||
| Physical functioning | 61.5±23.1 | 63.9±23.0 | NS |
| Role physical | 67.3±26.4 | 63.6±24.6 | NS |
| Bodily pain | 69.2±29.0 | 69.6±17.7 | NS |
| General health | 59.7±19.8 | 59.3±21.9 | NS |
| Vitality | 57.2±21.2 | 61.5±16.1 | NS |
| Social functioning | 68.3±26.8 | 76.0±26.7 | NS |
| Role emotional | 69.9±26.2 | 69.2±21.4 | NS |
| Mental health | 67.3±21.7 | 68.9±14.7 | NS |
| QLQ-C30 subscale | |||
| Global health status/QoL | 51.3±18.0 | 54.0±18.2 | NS |
| Physical functioning | 73.3±31.3 | 73.3±30.6 | NS |
| Role functioning | 69.4±32.4 | 73.6±30.5 | NS |
| Emotional functioning | 62.5±22.1 | 65.2±28.0 | NS |
| Cognitive functioning | 66.6±32.6 | 79.1±25.8 | NS |
| Social functioning | 88.9±16.4 | 83.3±21.3 | NS |
| Fatigue | 21.3±15.3 | 26.8±16.0 | NS |
| Nausea and vomiting | 6.9±13.2 | 2.8±6.5 | NS |
| Pain | 11.1±16.4 | 11.1±14.8 | NS |
| Dyspnea | 30.5±30.0 | 30.5±22.3 | NS |
| Insomnia | 22.2±29.6 | 19.4±22.3 | NS |
| Appetite loss | 13.9±22.3 | 8.3±20.7 | NS |
| Constipation | 5.6±13.0 | 11.1±16.4 | NS |
| Diarrhea | 8.3±15.1 | 2.8±9.6 | NS |
| Financial difficulties | 0±0 | 2.8±9.6 | NS |
| QLQ-LC13 subscale | |||
| Dyspnea | 28.7±20.9 | 23.1±14.6 | NS |
| Coughing | 41.6±20.9 | 25.0±20.7 | NS |
| Haemoptysis | 5.6±25.1 | 2.8±9.6 | NS |
| Sore mouth | 2.8±9.6 | 0±0 | NS |
| Dysphagia | 11.1±16.4 | 2.8±9.6 | NS |
| Peripheral neuropathy | 8.3±20.7 | 11.1±21.7 | NS |
| Alopecia | 11.1±21.7 | 11.1±21.7 | NS |
| Pain in chest | 5.6±13.0 | 8.33±20.7 | NS |
| Pain in arm or shoulder | 13.9±26.4 | 16.7±22.5 | NS |
| Pain in other parts | 16.7±22.5 | 11.1±16.4 | NS |
| HADS | |||
| Anxiety | 8.8±4.2 | 7.4±3.5 | NS |
| Depression | 5.4±3.6 | 3.9±2.3 | <0.05 |
Data presented as mean ± SD. HADS Hospital Anxiety and Depression Scale; NS Not statistically significant; QLQ-C30 European Organization for Research and Treatment of Cancer Quality of Life Questionnaire; QLQ-LC13 Lung Cancer-Specific Questionnaire; QoL Quality of life; SF-36 Short-Form 36 Health Survey
DISCUSSION
To our knowledge, the present investigation was the first to examine the feasibility and potential benefit of a short (four weeks) HBETP with patients under investigation for NSCLC and potential candidates for LRS. The main finding of the present study was that a short, moderate intensity, HBETP was feasible, safe and well tolerated in this context. In addition, participation in such a program produced physiological effects, including improved cycling endurance, walk distance and muscle strength.
Although the recruitment rate was low, the completion rate and adherence to the program were acceptable. In other studies, completion rates for exercise intervention programs varied widely. For example, Temel and al (16) reported a completion rate of 44% in patients with advanced NSCLC. There are several possible explanations for the high completion rate in our study. First, most of our patients were young and had early stage lung cancer and, furthermore, as suggested by Temel and al (16), an HBETP may be more feasible in this population. Moreover, modalities and intensities of training were adapted to the patients’ individual condition and a weekly phone follow-up was conducted to reinforce the importance of the exercises, to detect problems and to adjust the exercise prescription, if necessary. In addition to to this close follow-up, a potential selection bias associated with referral patterns by the nurses, pulmonologists and surgeons may have influenced the results by selecting people who were initially more motivated to perform physical activities. On the other hand, none of the participating patients were regularly physically active before the intervention.
Another important finding was that the HBETP had beneficial effects on exercise capacity and muscle strength. The absence of improved peak exercise capacity in such a short training program is not unexpected because this parameter does not change markedly with exercise training (34). We found a statistically and clinically significant improvement in the endurance time to constant workrate cycling exercise and in the 6MWT distance. The 157 s increase in the endurance time to constant workrate exercise exceeded the 100 s that is generally considered to represent a clinically significant outcome for this variable (35). Similarly, the gain in the 6MWT distance was superior to the minimal important difference for this variable (36). The possibility to improve muscle strength before the surgery is of clinical interest. Bolliger et al (37) recently reported the frequent occurrence of muscle weakness in lung cancer patients and confirmed that after lobectomy, much of the limitation in exercise capacity may be explained by peripheral muscle function.
While exercise led to a substantial improvement of physiological parameters, no statistically significant or clinically meaningful changes in QoL were observed, apart from a reduction in depression score, which was statically and clinically reduced postrehabilitation. This improvement may be clinically relevant because in cancer patients, depression is associated with increased mortality, poorer adherence to treatment and increased length of hospitalization after thoracic surgery for malignancy (38,39). Also, for the SF-36, compared with normative data (40), physical functioning, general health and social functioning were all significantly lower in our patients. However, following the program, social functioning was no longer different from normative data but role limitations due to physical problems, role limitations due to emotional problems and mental health became different, suggesting that the preoperative period itself may have had an impact on QoL. On a positive note, it is possible that without exercise training, patients may have experienced a worse decline of their QoL; however, in the absence of a control group, it is difficult to draw a definitive conclusion. Nevertheless, these findings are consistent with the conflicting results in the literature and with the other studies that did not find any change in QoL following exercise training in patients with lung cancer (41–43). Other studies specially designed to address this relevant question need to be conducted. In addition, it could be hypothesized that the absence of any educational or group-based sessions in the present study may have impacted the capacity of the intervention to improve QoL. Other studies specifically designed to address this relevant question need to be conducted.
Although we found that HBETP was feasible in patients under investigation for NSCLC, we acknowledge that only 50% of the potentially eligible candidates agreed to participate in the present study. The main reasons for this relatively low recruitment rate included a high level of anxiety, lack of interest and lack of time. Nonparticipation in this type of intervention could be explained by a variety of barriers such as psychological distress (anxiety, depression) or physical symptoms (pain, fatigue). The challenge of facing a cancer diagnosis may have, by itself, impacted the patients’ willingness to participate in our study (16).
Some methodological aspects of our study warrant consideration. First, due to the short period of time between the final diagnosis of lung cancer and surgery, we decided a priori to include patients immediately when they began their investigation for lung cancer. Despite this recruitment strategy, only one patient did not ultimately have lung cancer. Thus, we are confident that the data from our study can be generalized to a large proportion of patients with lung cancer awaiting LRS. The tight schedule of the patients during the preoperative period led to another challenging limitation: the requirement of a one-day assessment period. In a perfect setting, the evaluation would be performed during two different visits. However, in the present study, this design was not possible because of the short period of time allowed. However, to minimize bias, all tests were administered in the same order in pre- and post-HBETP and a 2 h rest period between incremental and constant cycle exercise tests and 20 min between the two 6MWT was allowed.
Additionally, the small number of patients who agreed to participate reduced the statistical power of the study. One message to gain from this is that rehabilitative interventions are challenging to implement in clinical practice.
From this perspective, it could be hypothesized that due to implementation difficulties of rehabilitation on a large scale, this modality should be primarily considered for compromised patients who are seldom candidates for surgery because of their marginal cardiovascular capacity and because of the postoperative cardiopulmonary complications related to it. Indeed, based on physiological results achieved in our study and the available literature, it is reasonable to believe that it is possible to sufficiently improve the aerobic capacity of some of these patients to place them above the threshold where the risk of complications are acceptable to consider surgery. In addition, a recent study by Bozcuk and Martin (44) found that delaying treatment until 48 days after diagnosis did not appear to have any effect on survival. Thus, it may be beneficial to use an extended preoperative period to improve cardiovascular fitness of some patients with the aim of reducing postoperative complications. However, the present study was not designed nor did it have the statistical power to determine whether exercise training could lower postoperative surgical complications. Also, from a clinical perspective, it may have been interesting to perform a formal economic analysis of HBETP. However, based on the COPD literature (19), we had no reason to believe that there were major differences in related costs between home-based and in-patient intervention.
The absence of a control group was another potential limitation with regard to interpretation of the results. We elected not to include a control group given that one of our main goals was to demonstrate the feasibility of the intervention. At this stage, we did not want to compromise and slow the progression of the study by trying to include a control group. A cross-over study design would have been impossible given the imperative surgery schedule. Only a few studies evaluating the impact of exercise training in postoperative lung cancer patients have included a control group, confirming the challenges associated with this methodological design (42,45).
CONCLUSION
In motivated patients under investigation for lung cancer and awaiting LRS, an HBETP is a feasible therapeutic modality. Patients showed good adherence and were able to achieve the objectives of participation. In addition, our study found that a four-week HBETP produces physiological effects such as improved cycling exercise endurance, 6MWT distance and muscle strength. Such improvements may be clinically relevant because exercise intolerance and muscle weakness are predictors of cardiopulmonary complications of thoracic surgical procedures.
Acknowledgments
The authors acknowledge the help of Dr Rosaire Vaillancourt, Dr Massimo Conti, Dr Jocelyn Grégoire, Marie-Josée Breton, Dominique Léveillée and all the personnel at the Clinique Spécialisée en pneumologie de l’IUCPQ, in accomplishing this study and are grateful to Eric Nadreau and Cynthia Brouillard for their technical support during the exercise testing. The authors also thank Serge Simard for statistical assistance and Debbie Deslauriers for her helpful linguistic revision. The authors also thank the anonymous reviewers for their excellent suggestions.
Footnotes
FINANCIAL SUPPORT: V Coats is a recipient of a research training award from the Canadian Institute of Heath Research. This work was supported by the Canadian Lung Association.
AUTHOR CONTRIBUTIONS: All authors were substantially involved in design, acquisition, analysis and interpretation of the study. All authors contributed to the intellectual content of the manuscript and were consulted for final approval of the submitted version. Accordingly, the authors did not omit to include any other author who would fulfill these authorship requirements.
REFERENCES
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. (Erratum in: CA Cancer J Clin 2011;61:134). [DOI] [PubMed] [Google Scholar]
- 2.Morris GS, Gallagher GH, Baxter MF, et al. Pulmonary rehabilitation improves functional status in oncology patients. Arch Phys Med Rehabil. 2009;90:837–41. doi: 10.1016/j.apmr.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 3.Jones LW, Eves ND, Peterson BL, et al. Safety and feasibility of aerobic training on cardiopulmonary function and quality of life in postsurgical nonsmall cell lung cancer patients: A pilot study. Cancer. 2008;113:3430–9. doi: 10.1002/cncr.23967. [DOI] [PubMed] [Google Scholar]
- 4.Brunelli A, Socci L, Refai M, Salati M, Xiumø F, Sabbatini A. Quality of life before and after major lung resection for lung cancer: A prospective follow-up analysis. Ann Thorac Surg. 2007;84:410–6. doi: 10.1016/j.athoracsur.2007.04.019. [DOI] [PubMed] [Google Scholar]
- 5.Bolliger CT, Jordan P, Soler M, et al. Exercise capacity as a predictor of postoperative complications in lung resection candidates. Am J Respir Crit Care Med. 1995;151:1472–80. doi: 10.1164/ajrccm.151.5.7735602. [DOI] [PubMed] [Google Scholar]
- 6.Brutsche MH, Spiliopoulos A, Bolliger CT, Licker M, Frey JG, Tschopp JM. Exercise capacity and extent of resection as predictors of surgical risk in lung cancer. Eur Respir J. 2000;15:828–32. doi: 10.1034/j.1399-3003.2000.15e03.x. [DOI] [PubMed] [Google Scholar]
- 7.Benzo RP. Pulmonary rehabilitation in lung cancer: A scientific opportunity. J Cardiopulm Rehabil Prev. 2007;27:61–4. doi: 10.1097/01.HCR.0000265030.02521.f1. [DOI] [PubMed] [Google Scholar]
- 8.Ries AL, Bauldoff GS, Carlin BW, et al. Pulmonary Rehabilitation: Joint ACCP/AACVPR Evidence-Based Clinical Practice Guidelines. Chest. 2007;131:4S–42S. doi: 10.1378/chest.06-2418. [DOI] [PubMed] [Google Scholar]
- 9.Lacasse Y, Goldstein R, Lasserson TJ, Martin S. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2006;18(4):CD003793. doi: 10.1002/14651858.CD003793.pub2. [DOI] [PubMed] [Google Scholar]
- 10.Dimeo F, Fetscher S, Lange W, Mertelsmann R, Keul J. Effects of aerobic exercise on the physical performance and incidence of treatment-related complications after high-dose chemotherapy. Blood. 1997;90:3390–4. [PubMed] [Google Scholar]
- 11.Galvao DA, Newton RU. Review of exercise intervention studies in cancer patients. J Clin Oncol. 2005;23:899–909. doi: 10.1200/JCO.2005.06.085. [DOI] [PubMed] [Google Scholar]
- 12.Cesario A, Ferri L, Galetta D, et al. Pre-operative pulmonary rehabilitation and surgery for lung cancer. Lung Cancer. 2007;57:118–9. doi: 10.1016/j.lungcan.2007.03.022. [DOI] [PubMed] [Google Scholar]
- 13.Bobbio A, Chetta A, Ampollini L, et al. Preoperative pulmonary rehabilitation in patients undergoing lung resection for non-small cell lung cancer. Eur J Cardiothorac Surg. 2008;33:95–8. doi: 10.1016/j.ejcts.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 14.Jones LW, Eves ND, Peterson BL, et al. Safety and feasibility of aerobic training on cardiopulmonary function and quality of life in postsurgical nonsmall cell lung cancer patients: A pilot study. Cancer. 2008;113:3430–9. doi: 10.1002/cncr.23967. [DOI] [PubMed] [Google Scholar]
- 15.Spruit MA, Janssen PP, Willemsen SC, Hochstenbag MM, Wouters EF. Exercise capacity before and after an 8-week multidisciplinary inpatient rehabilitation program in lung cancer patients: A pilot study. Lung Cancer. 2006;52:257–60. doi: 10.1016/j.lungcan.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 16.Temel JS, Greer JA, Goldberg S, et al. A structured exercise program for patients with advanced non-small cell lung cancer. J Thorac Oncol. 2009;4:595–601. doi: 10.1097/JTO.0b013e31819d18e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brooks D, Sottana R, Bell B, et al. Characterization of pulmonary rehabilitation programs in Canada in 2005. Can Respir J. 2007;14:87–92. doi: 10.1155/2007/951498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Debigare R, Maltais F, Whittom F, Deslauriers J, Leblanc P. Feasibility and efficacy of home exercise training before lung volume reduction. J Cardiopulm Rehabil. 1999;19:235–41. doi: 10.1097/00008483-199907000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Maltais F, Bourbeau J, Shapiro S, et al. Effects of home-based pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: A randomized trial. Ann Intern Med. 2008;149:869–78. doi: 10.7326/0003-4819-149-12-200812160-00006. [DOI] [PubMed] [Google Scholar]
- 20.ATS/ACCP Statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med. 2003;167:211–277. doi: 10.1164/rccm.167.2.211. [DOI] [PubMed] [Google Scholar]
- 21.Standardization of spirometry – 1987 update. Official statement of American Thoracic Society. Respir Care. 1987;32:1039–60. [PubMed] [Google Scholar]
- 22.Knudson RJ, Slatin RC, Lebowitz MD, Burrows B. The maximal expiratory flow-volume curve. Normal standards, variability, and effects of age. Am Rev Respir Dis. 1976;113:587–600. doi: 10.1164/arrd.1976.113.5.587. [DOI] [PubMed] [Google Scholar]
- 23.Goldman HI, Becklake MR. Respiratory function tests; normal values at median altitudes and the prediction of normal results. Am Rev Tuberc. 1959;79:457–67. doi: 10.1164/artpd.1959.79.4.457. [DOI] [PubMed] [Google Scholar]
- 24.Borg G. Simple rating methods for estimation of perceived exertion. Wenner-Gren Center International Symposium Series. 1976;28:39–47. [Google Scholar]
- 25.ATS Statement: Guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–7. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 26.Andrews AW, Thomas MW, Bohannon RW. Normative values for isometric muscle force measurements obtained with hand-held dynamometers. Physical Ther. 1996;76:248–59. doi: 10.1093/ptj/76.3.248. [DOI] [PubMed] [Google Scholar]
- 27.McHorney CA, Ware JE, Jr, Raczek AE. The MOS 36-item Short-Form Health survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–63. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–76. doi: 10.1093/jnci/85.5.365. [DOI] [PubMed] [Google Scholar]
- 29.Bergman B, Aaronson NK, Ahmedzai S, Kaasa S, Sullivan M. The EORTC QLQ-LC13: A modular supplement to the EORTC Core Quality of Life Questionnaire (QLQ-C30) for use in lung cancer clinical trials. EORTC Study Group on Quality of Life. Eur J Cancer. 1994;30A:635–42. doi: 10.1016/0959-8049(94)90535-5. (Abst) [DOI] [PubMed] [Google Scholar]
- 30.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 31.Troosters T, Gosselink R, Decramer M. Short- and long-term effects of outpatient rehabilitation in patients with chronic obstructive pulmonary disease: A randomized trial. Am J Med. 2000;109:207–12. doi: 10.1016/s0002-9343(00)00472-1. [DOI] [PubMed] [Google Scholar]
- 32.Normandin EA, McCusker C, Connors M, Vale F, Gerardi D, ZuWallack RL. An evaluation of two approaches to exercise conditioning in pulmonary rehabilitation. Chest. 2002;121:1085–91. doi: 10.1378/chest.121.4.1085. [DOI] [PubMed] [Google Scholar]
- 33.Maltais F, Bourbeau J, Shapiro S, et al. Effects of home-based pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: A randomized trial. Ann Intern Med. 2008;149:869–78. doi: 10.7326/0003-4819-149-12-200812160-00006. [DOI] [PubMed] [Google Scholar]
- 34.Nici L, Donner C, Wouters E, et al. American Thoracic Society/European Respiratory Society statement on pulmonary rehabilitation. Am J Respir Crit Care Med. 2006;173:1390–413. doi: 10.1164/rccm.200508-1211ST. [DOI] [PubMed] [Google Scholar]
- 35.Laviolette L, Bourbeau J, Bernard S, et al. Assessing the impact of pulmonary rehabilitation on functional status in COPD. Thorax. 2008;63:115–21. doi: 10.1136/thx.2006.076844. [DOI] [PubMed] [Google Scholar]
- 36.Puhan MA, Chandra D, Mosenifar Z, et al. The minimal important difference of exercise tests in severe COPD. Eur Respir J. 2011;37:784–90. doi: 10.1183/09031936.00063810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bolliger CT, Jordan P, Soler M, et al. Pulmonary function and exercise capacity after lung resection. Eur Respir J. 1996;9:415–21. doi: 10.1183/09031936.96.09030415. [DOI] [PubMed] [Google Scholar]
- 38.Kitagawa R, Yasui-Furukori N, Tsushima T, Kaneko S, Fukuda I. Depression increases the length of hospitalization for patients undergoing thoracic surgery: A preliminary study. Psychosomatics. 2011;52:428–32. doi: 10.1016/j.psym.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 39.Pirl WF, Temel JS, Billings A, et al. Depression after diagnosis of advanced non-small cell lung cancer and survival: A pilot study. Psychosomatics. 2008;49:218–24. doi: 10.1176/appi.psy.49.3.218. [DOI] [PubMed] [Google Scholar]
- 40.Hopman WM, Towheed T, Anastassiades T, et al. Canadian normative data for the SF-36 health survey. Canadian Multicentre Osteoporosis Study Research Group. CMAJ. 2000;163:265–71. [PMC free article] [PubMed] [Google Scholar]
- 41.Peddle CJ, Jones LW, Eves ND, et al. Effects of presurgical exercise training on quality of life in patients undergoing lung resection for suspected malignancy: A pilot study. Cancer Nurs. 2009;32:158–65. doi: 10.1097/NCC.0b013e3181982ca1. [DOI] [PubMed] [Google Scholar]
- 42.Arbane G, Tropman D, Jackson D, Garrod R. Evaluation of an early exercise intervention after thoracotomy for non-small cell lung cancer (NSCLC), effects on quality of life, muscle strength and exercise tolerance: Randomised controlled trial. Lung Cancer. 2011;71:229–234. doi: 10.1016/j.lungcan.2010.04.025. [DOI] [PubMed] [Google Scholar]
- 43.Jones LW, Peddle CJ, Eves ND, et al. Effects of presurgical exercise training on cardiorespiratory fitness among patients undergoing thoracic surgery for malignant lung lesions. Cancer. 2007;110:590–8. doi: 10.1002/cncr.22830. [DOI] [PubMed] [Google Scholar]
- 44.Bozcuk H, Martin C. Does treatment delay affect survival in non-small cell lung cancer? A retrospective analysis from a single UK centre. Lung Cancer. 2001;34:243–52. doi: 10.1016/s0169-5002(01)00247-1. [DOI] [PubMed] [Google Scholar]
- 45.Cesario A, Ferri L, Galetta D, et al. Post-operative respiratory rehabilitation after lung resection for non-small cell lung cancer. Lung Cancer. 2007;57:175–80. doi: 10.1016/j.lungcan.2007.02.017. [DOI] [PubMed] [Google Scholar]


