Abstract
Background
Susceptibility to and severity of ankylosing spondylitis (AS) are largely genetically determined. PPARGC1B, RUNX3 and TBKBP1 have recently been found to be associated with AS in patients of western European descent. Our purpose is to examine the influence of PPARGC1B, RUNX3 and TBKBP1 polymorphisms on the susceptibility to and the severity of ankylosing spondylitis in Chinese ethnic majority Han population.
Methods
Blood samples are drawn from 396 AS patients and 404 unrelated healthy controls. All the patients and the controls are Han Chinese and the patients are HLA-B27 positive. The AS patients are classified based on the severity of the disease. Twelve tag single nucleotide polymorphisms (tagSNPs) in PPARGC1B, RUNX3 and TBKBP1 are selected and genotyped. Frequencies of different genotypes and alleles are analyzed among the different severity AS patients and the controls.
Results
After Bonferroni correction, the rs7379457 SNP in PPARGC1B shows significant difference when comparing all AS patients to controls (p = 0.005). This SNP also shows significant difference when comparing normal AS patients to controls (p = 0.002). The rs1395621 SNP in RUNX3 shows significant difference when comparing severe AS patients to controls (p = 0.007). The rs9438876 SNP in RUNX3 shows significant difference when comparing normal AS patients to controls (p = 0.007). The rs8070463 SNP in TBKBP1 shows significant difference in genotype distribution when comparing severe AS patients to controls (p = 0.003).
Conclusions
The rs7379457 SNP in PPARGC1B is related to susceptibility to AS in Chinese Han population. The rs7379457 SNP in PPARGC1B, the rs1395621 and rs9438876 SNPs in RUNX3, and the rs8070463 SNP in TBKBP1 are related to the severity of AS in Chinese Han population.
Introduction
Ankylosing spondylitis (AS) is a chronic inflammatory disorder characterized by inflammation in the spine and sacroiliac joints causing initial bone and joint erosion and subsequent ankylosis [1]. Most patients develop first symptoms of AS younger than 30 years of age [2]. Significant radiographic progression occurs in the first 10 years of disease, and more recent studies have shown that structural damage at initial presentation is the best predictor of further damage [3]–[5].
AS patients’ disease severity is largely genetically determined [6]. We aim to identify patients with susceptibility to AS before the appearance of significant deformities and disabilities, so we can intervene earlier. In genome-wide association studies (GWAS), rs11959820 in PPARGC1B, rs11249215 in RUNX3, and rs8070463 in TBKBP1 are related to AS susceptibility in patients of western European descent [7]–[9]. These findings must be replicated and refined in different populations. Interpreting GWAS results at a gene-specific level is an important step towards understanding the molecular processes that lead to the disease [10].
We hypothesize that the PPARGC1B, RUNX3, and TBKBP1 are related to AS in the Chinese ethnic majority Han population. Additionally, some single nucleotide polymorphisms (SNPs) of these genes may predict the severity of AS.
Methods
Study Population
In this work, 396 AS patients are recruited, along with 404 unrelated healthy controls who are age and sex-matched. All patients and controls are Han Chinese. All AS patients are HLA-B27 positive. All AS patients are treated by non-steroidal anti-inflammatory drug routinely; no other treatments are used for patients. Among the AS patients, there are 354 males (89.4%) and 42 females (10.6%); the average age is 29.6 years (range 16 to 60 years) (Table 1). Among the controls, there are 364 males (90.1%) and 40 females (9.9%); the average age is 30.0 years (range 16 to 60 years). Neither sex nor age distributions show significant differences between AS and control patients (p = 0.742, 0.518 respectively). The average duration since AS diagnosis is 11.5 years (range 8 to 18 years). The diagnosis of AS has been made by experienced rheumatologists; all diagnoses satisfy the modified New York criteria [11]. Subjects with inflammatory bowel disease, psoriasis, rheumatoid arthritis, or other autoimmune diseases are excluded from both the AS and the control groups.
Table 1. Demographic data of AS patients and controls.
| Sex | Cases (396) | Controls (404) | p-value | |
| male | 354 (89.4%) | 364 (90.1%) | 0.742 | |
| female | 42(10.6%) | 40 (9.9%) | ||
| Age | 29.6±8.5 | 30.0±9.4 | 0.518 | |
| Duration of diagnosis | 11.5±2.1 | N/A | ||
| BASFI | 3.97±1.49 | N/A | ||
| BASDAI | 3.95±1.05 | N/A | ||
| mSASSS | 12.6±13.4 | N/A |
There is no significant difference in age and sex-distribution between AS patients and controls. Numerical values presented as mean±standard deviation. BASFI : Bath ankylosing spondylitis function index. BASDAI: Bath ankylosing spondylitis disease activity index. mSASSS: modified Stokes ankylosing spondylitis Spine Score.
Basic Data Acquisition
The Bath AS function index (BASFI) and Bath AS disease activity index (BASDAI) are administered to the patients using questionnaires; these indices are the most widely used tools for the assessment of AS functional status and disease activity [12] [13]. The modified Stokes AS Spine Score (mSASSS) is a validated scoring system for quantification of chronic spinal changes [14]. Standard anteroposterior and lateral radiographs of the cervical and lumbar spine are obtained for each subject, and the lateral view is used to derive a mSASSS score for each patient [15] [16]. Three of the authors separately assigned the mSASSS scores, and the average is used.
Severity Classification
There is a lack of consensus on how to classify AS severity [17]. In this work, we define severe subtype of AS as the disease form in those patients who require surgery within first ten years of diagnosis. The indications of surgery include inability to stand upright, inability to look straight ahead, and compression of the viscera due to kyphosis that manifests as pain [18]. Patients with the normal type of AS exhibit inflammation of sacroiliac joints, but their spine and other joints are relatively spared; these patients require only medical treatment. By this definition, 82 AS patients have the severe subtype, and 314 AS patients have the normal subtype. Clinical features comparing severe AS and normal AS are shown in Table 2.
Table 2. Clinical features comparing severe AS and normal AS.
| Sex | severe AS (82) | normal AS (314) | p value | |
| male | 76(92.7%) | 276(87.9%) | 0.220 | |
| female | 6(7.3%) | 38(12.1%) | ||
| Age | 31.5±9.2 | 29.0±8.3 | 0.097 | |
| Duration of diagnosis | 11.2±3.0 | 11.6±1.8 | 0.290 | |
| BASFI | 6.03±2.06 | 3.43±0.55 | <0.001 | |
| BASDAI | 5.49±1.10 | 3.55±0.55 | <0.001 | |
| mSASSS | 37.1±13.3 | 6.21±1.06 | <0.001 |
There is no difference between severe AS patients and normal patients in age and sex distribution; however, the BASFI, BASDAI and mSASSS are higher in severe AS patients.
SNPs Selection
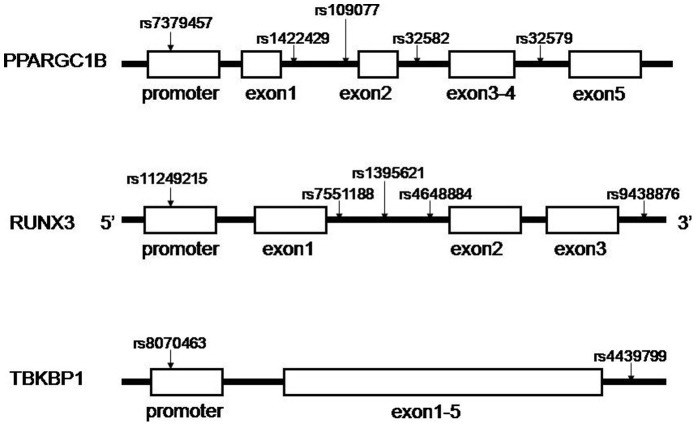
The SNPs in this study include five in PPARGC1B, five in RUNX3 and two in TBKBP1. These three genes localize to chromosome 5, 1, and 17, respectively. The selected SNPs serve as multi-marker tagging algorithm with criteria of r2 more than 0.8 and for all SNPs with minor allele frequency more than 5% from the Han Chinese in Beijing population in the HapMap database. Haploview 4.2 software (Broad Institute, Cambridge, Massachusetts, USA) is used to select the tagSNPs. Figure 1 shows the positions of each tagSNP. The rs7379457 SNP is located in the promoter of PPARGC1B. The rs11249215 SNP is located in the promoter of RUNX3. The rs8070463 SNP is located in the promoter of TBKBP1. Other SNPs are located in the introns. Most SNPs in TBKBP1 are in high linkage disequilibrium (LD), hence only two tagSNPs are selected.
Figure 1. Positions of each selected tagSNP on the genes.
The SNP rs7379457 is in the promoter of PPARGC1B. The SNP rs11249215 is in the promoter of RUNX3. The SNP rs8070463 is in the promoter of TBKBP1. Other SNPs are all in introns.
DNA Extraction and Genotyping Analysis
DNA is isolated from 2 ml whole blood samples using AxyPrep Blood Genomic DNA Miniprep kit (Axygen Biosciences, Union City, CA, USA). Detection of the SNPs is performed by MassARRAY system (Sequenom, San Diego, CA, USA). The chip-based matrix-assisted laser desorption ionization time-of-flight (MALDI-TOF) mass spectrometry technology is used in this procedure [19]. Most of the SNPs are successfully genotyped. The rs109077 SNP is 98.5% genotyped in case group and 97.5% in control group. The rs4648884 SNP is 98.5% genotyped in case group. The rs9438876 is 90.9% genotyped in case group and 95.5% in control group. In the other SNPs, more than 99.5% is genotyped in both case and control groups.
Statistical Analysis
The Hardy-Weinberg equilibrium is tested for all 12 tagSNPs. The Pearson’s chi-squared test and independent-samples t-test are used to compare the differences in age and sex between cases and controls. Comparisons of the distributions of the genotype, allele and haplotype frequencies are performed using the Pearson’s chi-squared test. Especially, in the rs7379457 SNP the TT genotype is rare. Therefore, we use Fisher’s exact test. Binary logistic regression analysis is used to adjust for age and sex. After Bonferroni correction, p-value less than 0.01 is considered significant. The last genotype of each SNP is the major genotype and the last allele is the major allele. The relative risks associated with the major genotypes or major alleles are estimated as an odds ratio (OR) with a 95% confidence interval (CI). The p-values of genotypes indicated in the result tables are used to estimate the significance of the distribution of genotype between cases and controls. All three genotypes of each SNP are compared, P-value for individual genotypes are shown only if significant at 0.05 level (Table 3, details are shown in Table S1, Table S2 and Table S3). We compared the severe AS group to the entirety of the control group and then normal AS group to the entirety control group. Pearson’s chi-squared test is used to compare the constructed haplotypes. The SNPs which show significant differences between AS patients and controls are considered to be related to susceptibility to AS. The SNPs which show significant differences between severe AS patients and controls but no differences between normal AS patients and controls are considered related to severity of AS. Moreover, SNPs show significant differences between normal AS patients and controls but no differences between severe AS patients and controls are considered related to severity of AS. Statistical analyses are carried out with SPSS v.17.0 software package (IBM, Armonk, New York, USA).
Table 3. Positive SNPs in PPARGC1B RUNX3 and TBKBP1 which are related to susceptibility to AS or severity of AS comparing all AS patients, severe AS patients and normal AS patients to the controls.
| SNP | All AS subjects cases/controls | Severe AS subjects cases/controls | Normal AS subjects cases/controls | ||||||||
| frequencies | OR(95% CI)c | p | frequencies | OR(95% CI) | p | frequencies | OR(95% CI) | p | |||
| PPARGC1B | rs7379457 | Alla | N/A | N/A | N/A | ||||||
| Genotype | TT | 8/0 | 1.024(1.007∼1.041) | 0.005 * | 0/0 | N/A | N/A | 8/0 | 1.029(1.009∼1.050) | 0.002 * | |
| CT | 50/72 | 0.671(0.453∼0.993) | 0.046# | 18/72 | 1.292(0.714∼2.339) | 32/72 | 0.538(0.344∼0.841) | 0.006 * | |||
| CC | 336/330 | 1b | 64/330 | 1 | 272/330 | 1 | |||||
| Allele | T | 66/72 | 0.929(0.655∼1.318) | 18/72 | 1.253(0.726∼2.164) | 48/72 | 0.847(0.579∼1.240) | ||||
| C | 722/732 | 1 | 146/732 | 1 | 576/732 | 1 | |||||
| RUNX3 | rs1395621 | All | 0.041# | 0.008 * | 0.147 | ||||||
| Genotype | AA | 58/66 | 0.730(0.477∼1.117) | 6/66 | 0.408(0.178∼0.934) | 0.007 * | 52/66 | 0.834(0.534∼1.303) | |||
| AG | 189/220 | 0.689(0.504∼0.943) | 0.015# | 39/220 | 0.538(0.321∼0.903) | 0.025# | 150/220 | 0.736(0.527∼1.028) | |||
| GG | 149/118 | 1 | 37/118 | 1 | 112/118 | 1 | |||||
| Allele | A | 305/352 | 0.811(0.665∼0.991) | 0.040# | 51/352 | 0.585(0.408∼0.837) | 0.003 * | 254/352 | 0.880(0.712∼1.087) | ||
| G | 487/456 | 1 | 113/456 | 1 | 374/456 | 1 | |||||
| rs9438876 | All | 0.022# | 0.716 | 0.004 * | |||||||
| Genotype | GG | 43/30 | 1.347(0.807∼2.251) | 4/30 | 0.556(0.180∼1.713) | 39/30 | 1.590(0.937∼2.699) | ||||
| AG | 129/172 | 0.743(0.547∼1.008) | 0.047# | 32/172 | 0.905(0.538∼1.523) | 97/172 | 0.701(0.504∼0.974) | 0.028# | |||
| AA | 188/184 | 1 | 0.038# | 38/184 | 1 | 150/184 | 1 | 0.007 * | |||
| Allele | G | 215/232 | 0.991(0.794∼1.237) | 40/232 | 0.862(0.581∼1.278) | 175/232 | 1.026(0.811∼1.298) | ||||
| A | 505/540 | 1 | 108/540 | 1 | 397/540 | 1 | |||||
| TBKBP1 | rs8070463 | All | 0.187 | 0.014# | 0.415 | ||||||
| Genotype | CC | 72/94 | 0.788(0.531∼1.170) | 8/94 | 0.400(0.186∼0.861) | 0.003 * | 64/94 | 0.928(0.611∼1.411) | |||
| CT | 198/184 | 1.084(0.786∼1.494) | 40/184 | 0.815(0.483∼1.376) | 158/184 | 1.170(0.828∼1.654) | |||||
| TT | 124/124 | 1 | 34/124 | 1 | 90/124 | 1 | |||||
| Allele | C | 342/372 | 0.890(0.731∼1.085) | 56/372 | 0.602(0.424∼0.856) | 0.004 * | 286/372 | 0.983(0.797∼1.212) | |||
| T | 446/432 | 1 | 108/432 | 1 | 338/432 | 1 | |||||
“All” means the p value that we compare all the three genotype using 3×2 chi squared method. P-value for individual genotypes are shown only if significant at 0.05 level.
The last lines of genotypes or alleles are the major genotypes or the major alleles. The other genotypes or alleles are compared to them. The relative risk associated with major genotypes and major alleles is estimated as an odds ratio (OR) with a 95% confidence interval (CI).
OR (95% CI) are adjusted by age and sex using multiple regression analysis.
indicates p-value is less than 0.05 but cannot pass Bonferroni correction which shows marginal significant difference.
Ethics Statement
The blood samples of both AS patients and controls used in this study are part of samples taken for diagnostic tests. During the collection and use of DNA samples, clinical data guidelines, regulations of the local Ethics Committee and the Helsinki Declaration in 1975 are followed. Written informed consents were obtained from all the patients and subjects (or their parents in the case of two patients less than 18 years old). The study procedure is approved by our Institutional Review Board.
Results
Clinical Features
The BASFI, BASDAI and mSASSS for the AS patients are recorded in Table 1. Among the 396 AS patients, the mean BASFI is 3.97±1.49 (mean±standard deviation). The mean BASDAI is 3.95±1.05. The mean mSASSS is 12.6±13.4. When comparing the severe AS and the normal AS patient groups, there is no significant difference in sex, age, and disease duration (p-value = 0.220, 0.097, 0.290 respectively; Table 2). The BASFI is higher in severe AS group (6.03±2.06) than normal AS group (3.43±0.55) (p-value<0.001), reflecting poorer function of patients in the severe AS group. The BASDAI is similarly higher in the severe AS group (5.49±1.10) than normal AS group (3.55±0.55) (p-value<0.001), reflecting higher disease activity. The pattern holds for mSASSS (37.1±13.3 versus 6.21±1.06, p-value<0.001), signifying more radiographic changes in the severe AS patients.
Genotype and Allele
We genotyped 12 SNPs, the detailed results are summarized in Table S1, Table S2, and Table S3. The genotype frequencies of these 12 tagSNPs are in Hardy-Weinberg equilibrium in all groups. Four of the 12 SNPs show significant difference in disease diagnosis and severity (Table 3). The genotype frequencies of these 12 tagSNPs are in Hardy-Weinberg equilibrium in all groups. After Bonferroni correction, the rs7379457 SNP in PPARGC1B shows significant difference when comparing all AS patients to controls, with TT genotype higher in AS than in controls (p = 0.005). This SNP also shows significant difference when comparing normal AS patients to controls, with TT genotype higher in normal AS than in controls (p = 0.002) and CC genotype higher in normal AS than in controls (p = 0.006). The rs1395621 SNP in RUNX3 shows significant difference when comparing severe AS patients to controls, with AA genotype lower in severe AS patients than in controls (p = 0.007) and A allele is lower in severe AS patients than in controls (p = 0.003). The rs9438876 SNP in this gene shows significant difference when comparing normal AS patients to controls, with GG genotype lower in normal AS patients than in controls (p = 0.007). The rs8070463 SNP in TBKBP1 shows significant difference in genotype distribution when comparing severe AS patients to controls, with CC genotype lower in severe AS patients than in controls (p = 0.003). This SNP also shows significant difference in C allele distribution when comparing severe AS patients to controls, with C allele lower in severe AS patients than in controls (p = 0.004).
Haplotype
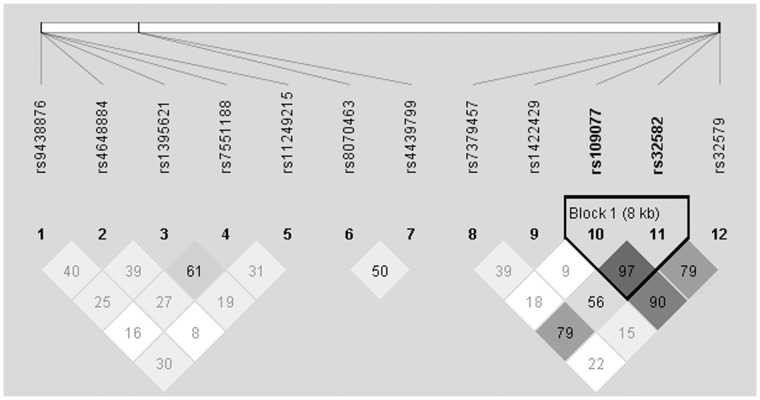
LD maps of the 12 tagSNPs of PPARGC1B, TBKBP1 and RUNX3 comparing all AS patients, severe AS patients, and normal AS patients to controls subjects are shown in Figure 2, Figure S1 and Figure S2, respectively. These figures have only a little difference, only Figure 2 is shown in the text comparing all AS patients to controls. Figure S1 and Figure S2 are shown in the supporting information comparing severe patients and normal patients to controls separately. Most of the SNPs are not in high linkage disequilibrium, with exception of one block in RUNX3. Analyses of constructed haplotypes for this block comparing all AS patients, severe AS patients, and normal AS patients to controls subjects are shown in Table 4. None of them is associated with the susceptibility to AS or severity of AS.
Figure 2. Linkage disequilibrium (LD) map comparing All AS patients and controls.
Darker color indicates higher linkage disequilibrium (LD), lighter color indicates less LD. Numbers in the squares indicate correlation coefficient (R2) value. The left part of the picture contains 5 SNPs (from rs9438876 to rs11249215). They are from RUNX3. The middle part of the picture contains 2 SNPs (rs8070463 and rs4439799). They are from TBKBP1. The right part of the picture contains 4 SNPs (from rs7379457 to rs32579). They are from PPARGC1B. Haplotypes are constructed from the darker blocks (high linkage disequilibrium). They are TG, GT and GG.
Table 4. Haplotype analysis in block 1.
| rs109077 | rs32582 | Case Ratio | Control Ratio | Chi Square | p value | |
| All AS patients vs. controls | T | G | 529∶263 | 536∶272 | 0.037 | 0.847 |
| G | T | 136∶656 | 141∶667 | 0.022 | 0.883 | |
| G | G | 123∶669 | 130∶678 | 0.094 | 0.759 | |
| Severe AS patients vs. controls | T | G | 114∶50 | 537∶271 | 0.574 | 0.449 |
| G | T | 28∶136 | 142∶666 | 0.024 | 0.878 | |
| G | G | 22∶142 | 130∶678 | 0.739 | 0.390 | |
| Normal AS patients vs. controls | T | G | 415∶213 | 536∶272 | 0.010 | 0.920 |
| G | T | 108∶520 | 141∶667 | 0.016 | 0.900 | |
| G | G | 101∶527 | 130∶678 | 1.04E-5 | 0.997 |
Haplotypes are constructed. Case ratio means in the case group, the frequency of this kind of haplotype vs. other kinds of haplotype; control ratio means in the control group, the frequency of this kind of haplotype vs. other kinds of haplotype. None of the constructed haplotype has significant difference between cases and controls.
Discussion
The pathogenesis of AS remains poorly understood. However, genetic factors play a significant role [20]. Changes in the spine involve syndesmophytes forming bony ankylosis of adjacent vertebrae or ankylosis of small vertebral joints. Some classification systems exist based on clinical and radiographic criteria [21] [22]. Most of our patients present with mild symptoms and do well with chronic medical treatments; however, some patients have more severe manifestations that require surgery within the first ten years of diagnosis. We use this criterion to define severe and normal AS disease subtypes. We aim to find genetic markers for susceptibility to AS in general, as well as to the severe form of AS. This would provide powerful tools to clinicians and researchers to confirm the diagnosis of AS and predict for the development of severe form of AS. The ability to classify AS based on allelic differences would also have significant new therapies implications [23].
The human PPARGC1B gene (peroxisome proliferator-activated receptor-gamma coactivator 1 beta), encoding PGC-1β, localizes to chromosome 5q32, a region that shows linkage to type 2 diabetes [24]. Wirtenberger and colleagues found PGC-1β to be associated with familial breast cancer [25]. The mechanism that PPARGC1B relates to these diseases is still being investigated. Numerous publications indicate PPARGC1B plays a critical role in regulating multiple aspects of energy metabolism including mitochondrial biogenesis, thermogenesis, gluconeogenesis, and fatty acid β-oxidation [26]–[30]. Oxidative phosphorylation (OXPHOS) dysfunction plays a critical pathogenic role in several human diseases [31]. Sarika found that PGC-1β over-expression can lead to a marked improvement in OXPHOS defects caused by mutations in mitochondrial DNA (mtDNA) or nuclear DNA (nDNA) [32]. Kiyo-aki found PGC-1β accelerated osteoclastic bone resorption through the coordination of mitochondrial biogenesis and the cell-differentiation program [33]. Our data shows that rs7379457 SNP which localizes to the promoter of PPARGC1B is related to the susceptibility to AS and severity of AS. As a result, the functions of osteoclasts are inhibited due to decreased oxidative phosphorylation. With the imbalance between osteoblasts and osteoclasts, ossification predominates and thus leads to osteophyte formation and even ankylosis.
The RUNX3 gene (Runt-related transcription factor 3) encodes for RUNX3, and it localizes to chromosome 1p36.11. RUNX3 is a downstream target of the transforming growth factor-β (TGF-β) pathway, which is considered a tumor suppressor pathway, as components are frequently altered in cancers, especially those of the gastrointestinal tract [34]. RUNX3 is inactivated in gastric cancer by hemizygous deletion, promoter hypermethylation, histone modification, and protein mislocalization, suggesting a tumor-suppressive role of RUNX3 in this malignancy [35]–[37]. Since the discovery of the potential role of RUNX3 in the initiation and the progression of gastric cancer, RUNX3 has been found to be involved in the development of a variety of cancers, including colon, liver, lung and breast cancer [38]–[41]. RUNX3 knockout mice spontaneously develop inflammatory bowel disease characterized by leukocyte infiltration, mucosal hyperplasia, formation of lymphoid clusters, and increased production of IgA. RUNX3 belongs to the runt domain family of transcription factors, which are key regulators of lineage-specific gene expression and more recently are found to be linked to human autoimmunity [42]. When RUNX3 is suppressed in human T cells, either through gene inactivation or with small interference RNA, Foxp3 expression is reduced, which in turn disrupts the recognition of regulatory T cells. As with other autoimmune diseases, AS patients exhibit an imbalance of CCR4+CCR6+ helper T cells and regulatory T cells [43] [44]. RUNX3 is highly expressed in dendritic cells (DC), where it functions as a component of the transforming growth factor (TGF-β) signaling cascade [45]. It is obvious that RUNX3 is not only a tumor suppressor but also plays an important role in autoimmune diseases and inflammations. In our data, the rs1395621 and rs9438876 SNP show significant relationship to severity of AS. We conclude the RUNX3 can influence the AS severity due to its effect on the inflammatory process.
TBKBP1 (tumor necrosis factor family member-associated NF-κB activator binding kinase 1 binding protein) is an adaptor protein that binds to TBK1, also known as sintbad. The precise function of TBKBP1 in the process of TBK1 activation has not been defined fully, but there is evidence that the adaptor proteins link the kinases to the upstream signaling pathways, possibly by its interaction with TRAF3 [46]. Ken performed bone-marrow transfer experiments which revealed that TBK1-mediated signaling in hematopoietic cells is critical for the induction of antigen specific B and CD4+ T cells, whereas in non-hematopoietic cells TBK1 is required for CD8+ T-cell induction. These data suggest that TBK1 is a key signaling molecule for DNA-vaccine-induced immunogenicity, in addition to being part of the classic NF-κB inflammatory pathway [47]. Acute or chronic inflammation is an important feature of AS, with degree of inflammation correlated to severity of disease [48]. Appropriately, our data shows that rs8070463 SNP of TBKBP1 is related to the severity of AS.
In conclusion, PPARGC1B is associated with the susceptibility to AS; PPARGC1B, RUNX3 and TBKBP1 are associated with the severity of AS in the Chinese Han population. These findings support the GWAS results that these three genes are related to AS. Our findings can provide context for better understanding of the genetic and molecular pathogenesis of AS. The specific SNPs in these genes can be used to guide genetic analysis and counseling, medical and surgical treatment options, and ultimate prognosis. Further studies are needed to elucidate the molecular roles these genes play in AS.
Supporting Information
Linkage disequilibrium map comparing severe AS patients and controls. The distribution and position of SNPs are the same as Figure 2. Haplotypes are constructed from the darker blocks (high linkage disequilibrium). They are TG, GT and GG.
(TIF)
Linkage disequilibrium map comparing normal AS patients and controls. The distribution and position of SNPs are the same as Figure 2. Haplotypes are constructed from the darker blocks (high linkage disequilibrium). They are TG, GT and GG.
(TIF)
Genotype and allele frequencies of PPARGC1B SNPs among all AS patients, severe AS patients, normal AS patients versus controls. SNPs in PPARGC1B are compared between all AS patients, severe AS patients, and normal AS patients versus the control subjects. P-value for each SNP is shown, and p-value for individual genotypes are shown only if significant at 0.05 level. # indicates p-value is less than 0.05 but cannot pass Bonferroni correction which shows marginal significant difference. *indicates p-value is less than 0.01 which shows significant difference after Bonferroni correction. OR and 95% CI are adjusted by age and sex. The rs7379457 SNP shows significant difference when comparing all AS patients to controls, TT genotype carrier frequency is higher than controls (p = 0.005*). This SNP also shows significant difference in comparing normal AS patients to controls, TT genotype carrier frequency is higher than controls (p = 0.002*); CC genotype carrier frequency is lower than controls (p = 0.006*).
(DOCX)
Genotype and allele frequencies of RUNX3 SNPs among all AS patients, severe AS patients, normal AS patients versus controls. SNPs in RUNX3 are compared between all AS patients, severe AS patients, and normal AS patients versus the control subjects. # indicates p-value is less than 0.05 but cannot pass Bonferroni correction which shows marginal significant difference. *indicates p-value is less than 0.01 which shows significant difference after Bonferroni correction. After Bonferroni correction, the rs1395621 SNP shows significant difference when comparing severe AS patients to controls, AA genotype carrier frequency is lower than controls (p = 0.007*) and A allele carrier frequency is lower than controls (p = 0.003*). The rs9438876 SNP shows significant difference when comparing normal AS patients to controls, the AA genotype is lower than controls (p = 0.007*).
(DOCX)
Genotype and allele frequencies of TBKBP1 SNPs among all AS patients, severe AS patients, normal AS patients versus controls. SNPs in TBKBP1 are compared between all AS patients, severe AS patients, and normal AS patients versus the control subjects. # indicates p-value is less than 0.05 but cannot pass Bonferroni correction which shows marginal significant difference. *indicates p-value shows significant difference after Bonferroni correction. After Bonferroni correction the rs8070463 SNP shows significant difference in genotype distribution when comparing severe AS patients to controls, CC genotype carrier frequency is lower than controls (p = 0.003*). This SNP also shows significant difference in C allele distribution when comparing severe AS patients to controls, C allele carrier frequency is lower than controls (p = 0.004*). The rs8070463 SNP is related to the severity of AS.
(DOCX)
Acknowledgments
The authors wish to thank all the patients and families that participated in this study, and all clinical doctors helped us in Chinese PLA general hospital.
Funding Statement
Nature science founding of Beijing supports this research. The number is 7102146. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Brown MA, Wordsworth BP, Reveille JD (2002) Genetics of ankylosing spondylitis. Clin Exp Rheumatol 20: S43–9. [PubMed] [Google Scholar]
- 2. Braun J, Sieper J (2007) Ankylosing spondylitis. Lancet 369: 1379–90. [DOI] [PubMed] [Google Scholar]
- 3. Carette S, Graham D, Little H, Rubenstein J, Rosen P (1983) The natural disease course of ankylosing spondylitis. Arthritis Rheum 26: 186–90. [DOI] [PubMed] [Google Scholar]
- 4. Gran JT, Skomsvoll JF (1997) The outcome of ankylosing spondylitis: a study of 100 patients. Br J Rheumatol 36: 766–71. [DOI] [PubMed] [Google Scholar]
- 5.Wanders A, Landewé R, Spoorenberg A, de Vlam K, Mielants H, et al.. (2004) Scoring of radiographic progression in randomised clinical trials in ankylosing spondylitis: a preference for paired reading order. Ann Rheum Dis. Dec;63(12): 1601–4. Epub Aug 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hamersma J, Cardon LR, Bradbury L, Brophy S, van der Horst-Bruinsma I, et al.. (2001) Is disease severity in ankylosing spondylitis genetically determined? [DOI] [PubMed] [Google Scholar]
- 7. The Australo-Anglo-American Spondyloarthritis Consortium (TASC) & the Wellcome Trust Case Control Consortium (WTCCC) (2007) Association scan of 14,500 nsSNPs in four common diseases identifies variants involved in autoimmunity. Nat Genet. 39(11): 1329–1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.The Australo-Anglo-American Spondyloarthritis Consortium (TASC) & the Wellcome Trust Case Control Consortium (WTCCC) (2011) Interaction between ERAP1 and HLA-B27 in ankylosing spondylitis implicates peptide handling in the mechanism for HLA-B27 in disease susceptibility. Nature Genetics volume 43 number 8 August. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sirota M, Schaub MA, Batzoglou S, Robinson WH, Butte AJ (2009) Autoimmune Disease Classification by Inverse Association with SNP Alleles PLoS Genet. Dec 5(12): e1000792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lehne B, Lewis CM, Schlitt T (2011) From SNPs to genes: disease association at the gene level. PLoS ONE June, Volume 6, Issue 6, e20133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. van der Linden S, Valkenburg HA, Cats A (1984) Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum. 27: 361–368. [DOI] [PubMed] [Google Scholar]
- 12. Calin A, Garrett S, Whitelock H, Kennedy LG, O’Hea J, Mallorie P, et al. (1994) A new approach to defining functional ability in ankylosing spondylitis: the development of Bath ankylosing spondylitis disease functional index (BASFI). J Rheumatol 21: 2281–2285. [PubMed] [Google Scholar]
- 13. Garrett S, Jenkinson TR, Whitelock HC, Kennedy LG, Gaisford P, et al. (1994) A new approach to defining disease status in AS: the Bath ankylosing spondylitis disease activity index (BASDAI). J Rheumatol 21: 2286–2291. [PubMed] [Google Scholar]
- 14. Baraliakos X, Listing J, von der Recke A, Braun J (2009) The natural course of radiographic progression in ankylosing spondylitis–evidence for major individual variations in a large proportion of patients. J Rheumatol 36: 997–1002. [DOI] [PubMed] [Google Scholar]
- 15. Creemers MC, Franssen MJ, van’t Hof MA, Gribnau FW, van de Putte LB, et al. (2005) Assessment of outcome in ankylosing spondylitis: an extended radiographic scoring system. Ann Rheum Dis 64: 127–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sieper J, Rudwaleit M, Baraliakos X, Brandt J, Braun J, et al.. (2009) The Assessment of SpondyloArthritis international Society (ASAS) handbook: a guide to assess spondyloarthritis. Ann Rheum Dis 68(Suppl II): 1–44. [DOI] [PubMed] [Google Scholar]
- 17. Amor B, Santos RS, Nahal R, Listrat V, Dougados M (1994) Predictive factors for the longterm outcome of spondyloarthropathies. J Rheumatol 21: 1883–87. [PubMed] [Google Scholar]
- 18. Kiaer T, Gehrchen M (2010) Transpedicular closed wedge osteotomy in ankylosing spondylitis: results of surgical treatment and prospective outcome analysis. Eur Spine J 19: 57–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tost J, Gut IG (2005) Genotyping single nucleotide polymorphisms by MALDI mass spectrometry in clinical applications. Clinical Biochemistry 38: 335–350. [DOI] [PubMed] [Google Scholar]
- 20. Reveille JD, Ball EJ, Khan MA (2001) HLA-B27 and genetic predisposing factors in spondyloarthropathies. Curr.Opin. Rheumatol. 13: 265–272. [DOI] [PubMed] [Google Scholar]
- 21.Taylor AL, Balakrishnan C, Calin A (1998) Reference centile charts for measures of disease activity, functional imparirment, and metrology in ankylosing spongdylitis. Arthritis & Rheumatism Vol 41. No 6. June. 1119–1125. [DOI] [PubMed] [Google Scholar]
- 22. Braun J, van der Heijde D, Dougados M, Emery P, Khan MA, et al. (2002) Staging of patients with ankylosing spondylitis: a preliminary proposal. Ann Rheum Dis Dec 61 Suppl 3iii9–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sirota M, Schaub MA, Batzoglou S, Robinson WH, Butte AJ (2009) Autoimmune disease classification by Inverse association with SNP alleles. PLoS genetics December, Volume 5, Issue 12, e1000792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Vionnet N, Hani EH, Dupont S, Gallina S, Francke S, et al. (2000) Genome wide search for type 2 diabetes-susceptibility genes in French whites: evidence for a novel susceptibility locus for early-onset diabetes on chromosome 3q27-qter and independent replication of a type 2-diabetes locus on chromosome 1q21-q24. Am J Hum Genet 67: 1470–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wirtenberger M, Tchatchou S, Hemminki K, Schmutzhard J, Sutter C, et al. (2006) Associations of genetic variants in the estrogen receptor coactivators PPARGC1A, PPARGC1B and EP300 with familial breast cancer. Carcinogenesis 27: 2201–2208. [DOI] [PubMed] [Google Scholar]
- 26. Puigserver P, Wu Z, Park CW, Graves R, Wright M, et al. (1998) A cold-inducible coactivator of nuclear receptors linked to adaptive thermogenesis, Cell. 92: 829–839. [DOI] [PubMed] [Google Scholar]
- 27. Lehman JJ, Barger PM, Kovacs A, Saffitz JE, Medeiros DM, et al. (2000) Peroxisome proliferator-activated receptor coactivator-1 promotes cardiac mitochondrial biogenesis, J. Clin. Invest. 106: 847–856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Yoon JC, Puigserver P, Chen G, Donovan J, Wu Z, et al. (2001) Spiegelman, Control of hepatic gluconeogenesis through the transcriptional coactivator PGC-1, Nature. 413: 131–138. [DOI] [PubMed] [Google Scholar]
- 29. Herzig S, Long F, Jhala US, Hedrick S, Quinn R, et al. (2001) CREB regulates hepatic gluconeogenesis through the coactivator PGC-1, Nature. 413: 179–183. [DOI] [PubMed] [Google Scholar]
- 30. Vega RB, Huss JM, Kelly DP (2000) The coactivator PGC-1 cooperates with peroxisome proliferator-activated receptor a in transcriptional control of nuclear genes encoding mitochondrial fatty acid oxidation enzymes, Mol. Cell. Biol. 20: 1868–1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Dimauro S, Schon EA (2008) Mitochondrial disorders in the nervous system. Annu. Rev. Neurosci. 31: 91–123. [DOI] [PubMed] [Google Scholar]
- 32. Srivastava S, Diaz F, Iommarini L, Aure K, Lombes A, et al. (2009) PGC-1 1alpha/beta induced expression partially compensates for respiratory chain defects in cells from patients with mitochondrial disorders. Human Molecular Genetics, Vol. 18 10: 1805–1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ishii KA, Fumoto T, Iwai K, Takeshita S, Ito M, et al.. (2009) Coordination of PGC-1beta and iron uptake in mitochondrial biogenesis and osteoclast activation. Nat Med. Mar;15(3): 259–66. Epub 2009 Mar 1. [DOI] [PubMed] [Google Scholar]
- 34. Derynck R, Akhurst RJ, Balmain A (2001) TGF-beta signaling in tumor suppression and cancer progression. Nat Genet 29: 117–29. [DOI] [PubMed] [Google Scholar]
- 35. Li QL, Ito K, Sakakura C (2002) Causal relationship between the loss of RUNX3 expression and gastric cancer. Cell 109: 113–24. [DOI] [PubMed] [Google Scholar]
- 36. Li QL, Ito K, Sakakura C, Fukamachi H, Inoue K, et al. (2005) RUNX3, a novel tumor suppressor, is frequently inactivated in gastric cancer by protein mislocalization. Cancer Res 65: 7743–50. [DOI] [PubMed] [Google Scholar]
- 37. Fujii S, Ito K, Ito Y, Ochiai A (2008) Enhancer of zeste homologue 2 (EZH2) down-regulates RUNX3 by increasing histone H3 methylation. J Biol Chem 283: 17324–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Subramaniam MM, Chan JY, Yeoh KG, Quek T, Ito K, et al. (2009) Molecular pathology of RUNX3 in human carcinogenesis. Biochim Biophys Acta 1796: 315–331. [DOI] [PubMed] [Google Scholar]
- 39. Goel A, Arnold CN, Tassone P, Chang DK, Niedzwiecki D, et al. (2004) Epigenetic inactivation of RUNX3 in microsatellite unstable sporadic colon cancers. Int J Cancer 112: 754–9. [DOI] [PubMed] [Google Scholar]
- 40. Li QL, Kim HR, Kim WJ, Choi JK, Lee YH, et al. (2004) Transcriptional silencing of the RUNX3 gene by CpG hypermethylation is associated with lung cancer. Biochem Biophys Res Commun 314: 223–8. [DOI] [PubMed] [Google Scholar]
- 41. Lau QC, Raja E, Salto-Tellez M, Liu Q, Ito K, et al. (2006) RUNX3 is frequently inactivated by dual mechanisms of protein mislocalization and promoter hypermethylation in breast cancer. Cancer Res 66: 6512–20. [DOI] [PubMed] [Google Scholar]
- 42. Alarcón-Riquelme ME (2004) Role of RUNX in autoimmune diseases linking rheumatoid arthritis, psoriasis and lupus. Arthritis Res. Ther. 6: 169–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Klunker S, Chong MM, Mantel PY, Palomares O, Bassin C, et al. (2009) Transcription factors RUNX1 and RUNX3 in the induction and suppressive function of Foxp3+ inducible regulatory T cells. J Exp Med 206(12): 2701–2715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Wu Y, Ren M, Yang R, Liang X, Ma Y, et al. (2011) Reduced immunomodulation potential of bone marrow-derived mesenchymal stem cells induced CCR4+CCR6+Th/Treg cell subset imbalance in ankylosing spondylitis. Arthritis Res Ther 13(1): R29. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 45. Fainaru O, Woolf E, Lotem J, Yarmus M, Brenner O, et al. (2004) Runx3 regulates mouse TGF-beta-mediated dendritic cell function and its absence results in airway inflammation. EMBO J. 23: 969–979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Unterholzner L, Sumner RP, Baran M, Ren H, Mansur DS, et al.. (2011) Vaccinia Virus Protein C6 Is a Virulence Factor that Binds TBK-1 Adaptor Proteins and Inhibits Activation of IRF3 and IRF7 PLoS pathogens Sep;7(9): e1002247. Epub 2011 Sep 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ishii KJ, Kawagoe T, Koyama S, Matsui K, Kumar H, et al. (2008) TANK-binding kinase-1 delineates innate and adaptive immune responses to DNA vaccines. Nature. Feb 7 451(7179): 725–9. [DOI] [PubMed] [Google Scholar]
- 48. Reveille JD, Ball EJ, Khan MA (2001) HLA-B27 and genetic predisposing factors in spondyloarthropathies. Curr.Opin. Rheumatol. 13: 265–272. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Linkage disequilibrium map comparing severe AS patients and controls. The distribution and position of SNPs are the same as Figure 2. Haplotypes are constructed from the darker blocks (high linkage disequilibrium). They are TG, GT and GG.
(TIF)
Linkage disequilibrium map comparing normal AS patients and controls. The distribution and position of SNPs are the same as Figure 2. Haplotypes are constructed from the darker blocks (high linkage disequilibrium). They are TG, GT and GG.
(TIF)
Genotype and allele frequencies of PPARGC1B SNPs among all AS patients, severe AS patients, normal AS patients versus controls. SNPs in PPARGC1B are compared between all AS patients, severe AS patients, and normal AS patients versus the control subjects. P-value for each SNP is shown, and p-value for individual genotypes are shown only if significant at 0.05 level. # indicates p-value is less than 0.05 but cannot pass Bonferroni correction which shows marginal significant difference. *indicates p-value is less than 0.01 which shows significant difference after Bonferroni correction. OR and 95% CI are adjusted by age and sex. The rs7379457 SNP shows significant difference when comparing all AS patients to controls, TT genotype carrier frequency is higher than controls (p = 0.005*). This SNP also shows significant difference in comparing normal AS patients to controls, TT genotype carrier frequency is higher than controls (p = 0.002*); CC genotype carrier frequency is lower than controls (p = 0.006*).
(DOCX)
Genotype and allele frequencies of RUNX3 SNPs among all AS patients, severe AS patients, normal AS patients versus controls. SNPs in RUNX3 are compared between all AS patients, severe AS patients, and normal AS patients versus the control subjects. # indicates p-value is less than 0.05 but cannot pass Bonferroni correction which shows marginal significant difference. *indicates p-value is less than 0.01 which shows significant difference after Bonferroni correction. After Bonferroni correction, the rs1395621 SNP shows significant difference when comparing severe AS patients to controls, AA genotype carrier frequency is lower than controls (p = 0.007*) and A allele carrier frequency is lower than controls (p = 0.003*). The rs9438876 SNP shows significant difference when comparing normal AS patients to controls, the AA genotype is lower than controls (p = 0.007*).
(DOCX)
Genotype and allele frequencies of TBKBP1 SNPs among all AS patients, severe AS patients, normal AS patients versus controls. SNPs in TBKBP1 are compared between all AS patients, severe AS patients, and normal AS patients versus the control subjects. # indicates p-value is less than 0.05 but cannot pass Bonferroni correction which shows marginal significant difference. *indicates p-value shows significant difference after Bonferroni correction. After Bonferroni correction the rs8070463 SNP shows significant difference in genotype distribution when comparing severe AS patients to controls, CC genotype carrier frequency is lower than controls (p = 0.003*). This SNP also shows significant difference in C allele distribution when comparing severe AS patients to controls, C allele carrier frequency is lower than controls (p = 0.004*). The rs8070463 SNP is related to the severity of AS.
(DOCX)