Abstract
Purpose
The proper indication for laparoendoscopic single-site surgery (LESS) in urology is still under debate, especially for malignant diseases. We compared the perioperative outcomes between LESS and conventional laparoscopy (CL) for upper urinary tract malignancies.
Materials and Methods
We reviewed the records of 75 patients who underwent radical nephrectomy, nephroureterectomy with bladder cuff excision, or partial nephrectomy with the LESS or CL approach between December 2008 and December 2010. We compared characteristics and perioperative outcomes between patients who underwent LESS or CL. All operations were performed by three surgeons using the transperitoneal approach.
Results
For all three surgery types, no differences in patient characteristics, estimated blood losses, transfusion rates, or durations of hospital stay were found between the two groups. No complications were found between the two groups in those who underwent nephroureterectomy with bladder cuff excision; however, significantly more complications were found in the LESS group than in the CL group in those who underwent radical nephrectomy or partial nephrectomy. Most of the complications with LESS radical nephrectomy occurred in the early introduction period of the technique.
Conclusions
No significant differences in perioperative outcomes were found between the LESS and CL groups in those who underwent radical nephrectomy or nephroureterectomy with bladder cuff excision. Therefore, the use of LESS in these cases is expected to expand as surgeons gain more experience with this technique and as other technical advances in laparoscopic instruments occur. However, partial nephrectomy with LESS should be performed restrictively considering the current level of surgical skill.
Keywords: Laparoscopy, Nephrectomy, Renal cell carcinoma, Ureteral neoplasms
INTRODUCTION
During the last 10 years, the transition from conventional laparoscopy (CL) to laparoendoscopic single-site surgery (LESS) as a step toward scar-free surgery may represent a paradigm shift in reconstructive and extirpative surgeries in many surgical fields. To overcome the several limitations of CL (e.g., bleeding, hernias, internal organ damage, and undesirable cosmetic effects) that can occur at working ports with CL approaches, LESS for minimally invasive surgery has been the focus of numerous investigations. Consequently, the use of LESS in urology has increased substantially with the refinement of laparoscopic instruments [1-6].
However, although many studies have already demonstrated the safety and feasibility of LESS for almost all types of urological surgeries [1,6-11], and some comparative studies have suggested that LESS is comparable with CL, the clinical advantage of LESS over CL in urology is still under debate, especially for malignant diseases [12,13]. Thus, the current study was designed to compare the perioperative outcomes between LESS and CL for upper urinary tract malignancies.
MATERIALS AND METHODS
1. Patient selection
Since we started performing LESS in December 2008 (simple nephrectomy), we have enrolled 75 consecutive patients who underwent radical nephrectomy, nephroureterectomy with bladder cuff resection, or partial nephrectomy for upper urinary tract malignancies with the LESS or CL approach between December 2008 and December 2010. All surgeries were performed by three laparoscopic surgeons with sufficient prior experience with CL. For patients who did not have general contraindications for CL, the surgical approach was chosen by the patient after a thorough discussion of the merits and drawbacks of both LESS and CL. Preoperatively, all patients granted informed consent, and our institution's institutional review board approved this study. The types of surgeries performed and characteristics of the patients are summarized in Table 1.
TABLE 1.
Patient characteristics
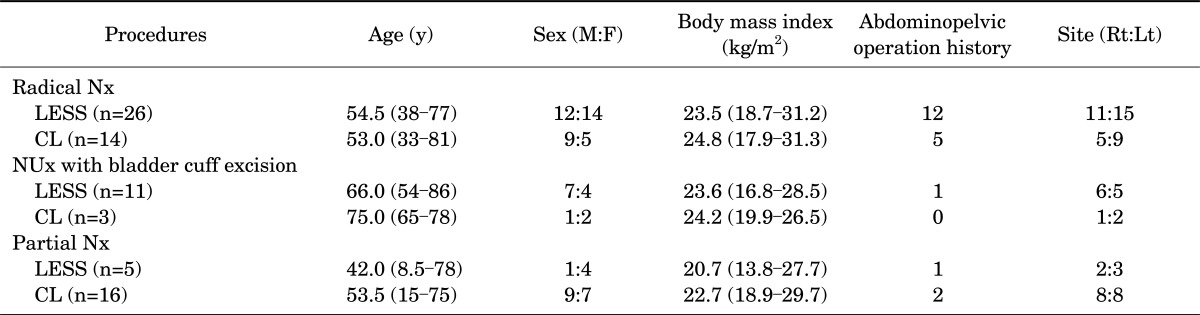
Values are presented as median (range).
Rt, right; Lt, left; Nx, nephrectomy; LESS, laparoendoscopic single-site surgery; CL, conventional laparoscopy; NUx, nephroureterectomy.
2. Surgical technique
1) LESS technique
All LESS cases were performed transperitoneally by using homemade port placement through the umbilicus. A detailed description of homemade port placement and laparoscopic instrumentation was described previously [7,14,15]. For the nephroureterectomy cases, the ureter was dissected to the level of the bladder after the nephrectomy was completed. The bladder cuff was dissected circumferentially around the ureteric orifice, and then we performed laparoscopic stapling of the distal ureter and bladder cuff using a pure extravesical approach without an additional incision. An additional trocar was selectively used for proper exposure or traction. The umbilical incision was extended until the specimen in the laparoscopic retrieval bag could be extracted intact without resistance. After hemostasis was confirmed, we selectively placed the drainage tube through the umbilical incision site.
2) CL technique
All CL cases were performed transperitoneally by using a 12-mm trocar at the umbilicus for the laparoscope. Depending on the type of surgery and the surgeon's preference, an additional two, three, or occasionally four trocars (5-mm or 12-mm) were used. As with LESS, the specimen was extracted through the extended umbilicus and we selectively placed the drainage tube.
3. Postoperative management and outcomes
In both groups, routine postoperative care for standard laparoscopic surgeries was provided. In all patients, the postoperative visual analog scale (VAS) pain score was determined by the nursing staff on a 10-point scale until the second postoperative day, and most patients received continuous intravenous patient-controlled analgesia with fentanyl 0.2 mcg/kg/h for 48 hours and intravenous tramadol (50 mg/A), which was administered as a bolus if the VAS pain score was 5 or greater. All patients were discharged at their own discretion after assessment of their general condition.
The demographics, operation time (OPT), estimated blood loss (EBL), transfusion rate, length of hospital stay (LHS), incision length, VAS pain score, perioperative complications, and final pathological results of all patients were recorded. The LESS and CL groups were compared by using Fisher's exact test and the Mann-Whitney U test for categorical and continuous variables, respectively. We used repeated-measures analysis of variance to compare the serial changes in VAS score during the first two postoperative days, only for the adult patients with intravenous patient-controlled analgesia. Statistical analysis was performed by using IBM SPSS ver. 18.0 (IBM Co., Armonk, NY, USA), and two-sided p-values <0.05 were considered statistically significant.
RESULTS
For all three types of surgery, there were no significant differences in median age, sex, body mass index, abdominopelvic operation history, or site of operation between the two groups (radical nephrectomy: p=0.52, p=0.33, p=0.55, p=0.74 and p=0.75; nephroureterectomy with bladder cuff excision: p=0.35, p=0.54, p=0.94, p=1.00, and p=1.00; partial nephrectomy: p=0.51, p=0.31, p=1.00, p=0.43, and p=1.00 respectively) (Table 1).
The pathologic results of three surgeries are summarized in Table 2. For radical nephrectomy, T stage was widely distributed from pT1 to pT3. The same result was found for nephroureterectomy with bladder cuff excision. However, partial nephrectomy was performed in patients whose pathologic result was pT1. Regardless of surgery type, only one case of a positive surgical margin was found in a patient who underwent partial nephrectomy by CL. In nephroureterectomy with bladder cuff excision cases, no positive bladder cuff excision margins were found in either the LESS or the CL group (Fig. 1).
TABLE 2.
Pathologic results of surgeries for upper urinary tract malignancies
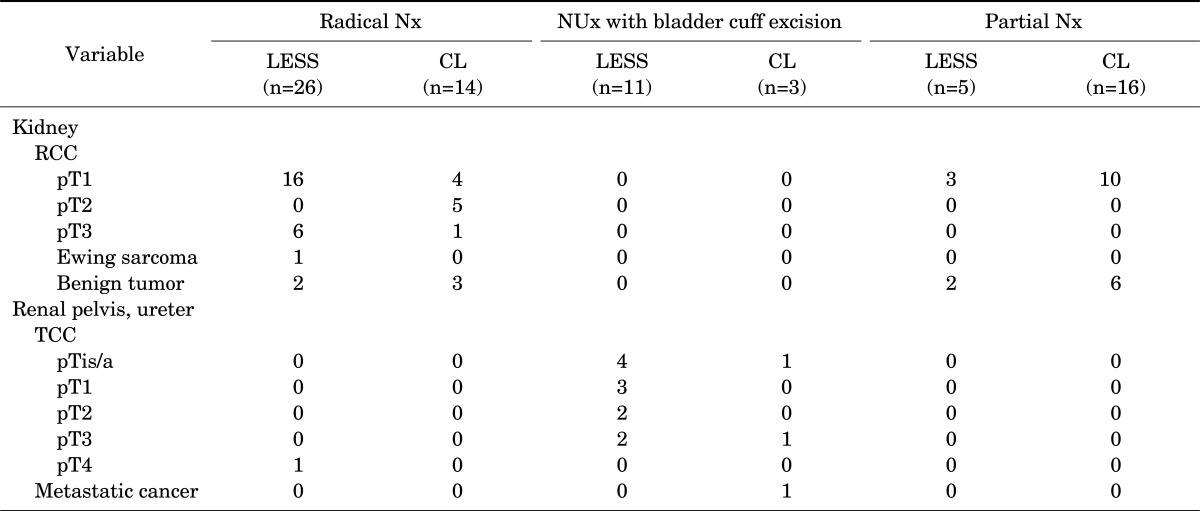
Nx, nephrectomy; NUx, nephroureterectomy; LESS, laparoendoscopic single-site surgery; CL, conventional laparoscopy; RCC, renal cell carcinoma; TCC, transitional cell carcinoma.
FIG. 1.

Gross pathologic image of laparoendoscopic single-site surgery nephroureterectomy with bladder cuff excision. Final pathologic result: high-grade transitional cell carcinoma, pT3, located at the right lower ureter with a negative bladder cuff excision margin.
In total, there were no grade IV, V Clavien-Dindo classifications in any of the laparoscopic surgeries and no port-related morbidity in any CL cases [16]. Moreover, no instances of emergency care or readmission after discharge occurred, regardless of surgery type.
In the radical nephrectomy cases, no significant differences in OPT, EBL, transfusion rate, LHS, or VAS pain score were found between the two groups (p=0.62, p=0.71, p=0.22, p=0.23, and p=0.08, respectively), but the complication rate was greater in the LESS group than in the CL group. These complications occurred in some (<10) of the earlier cases, but were eliminated after the surgeons became more experienced (Table 3).
TABLE 3.
Perioperative outcomes of CL and LESS for upper urinary tract malignancies
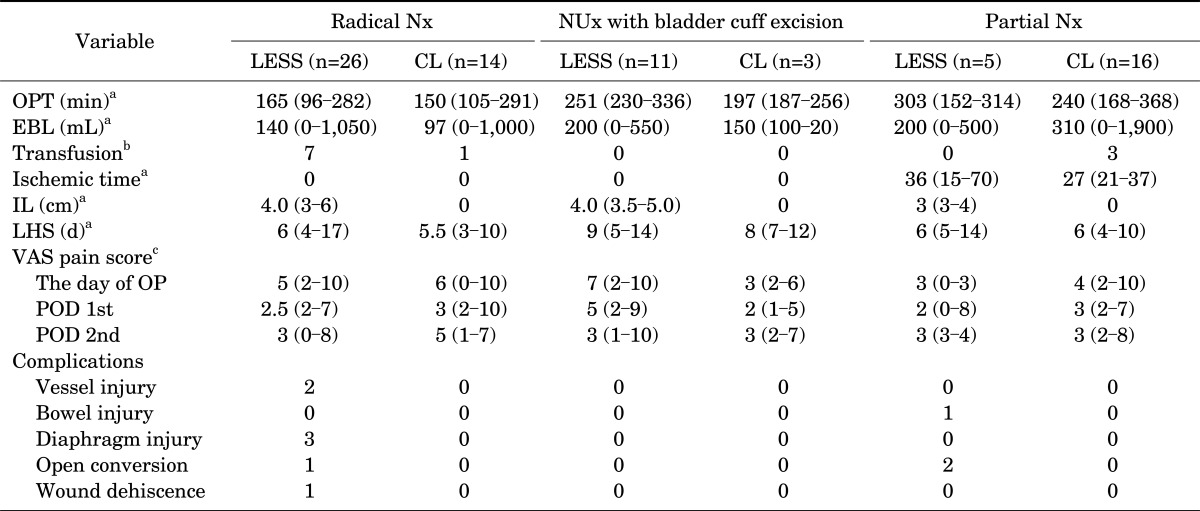
Values are presented as median (range).
CL, conventional laparoscopy; LESS, laparoendoscopic single-site surgery; Nx, nephrectomy; NUx, nephroureterectomy; OPT, operation time; EBL, estimated blood loss; IL, incision length; LHS, length of hospital stay; VAS, visual analog scale; OP, operation; POD, postoperative day.
a:Mann-Whitney test, b:Fisher's exact test, c:repeated measures analysis of variance.
In the nephroureterectomy with bladder cuff excision cases, no significant differences in OPT, EBL, LHS, or VAS pain score were found between the two groups (p=0.10, p=0.64, p=0.81, and p=0.25, respectively). Moreover, no transfusions were needed and no complications occurred in either group (Table 3).
In the partial nephrectomy cases, no significant differences in OPT, EBL, ischemic time, LHS, or VAS pain score were found between the two groups (p=0.27, p=0.13, p=0.581, p=0.93, and p=0.19, respectively), but the complication rate was greater in the LESS group than in the CL group. Furthermore, transfusions occurred in three cases in the CL group (Table 3).
DISCUSSION
For the past several years, LESS has been used in various types of urologic surgeries, and many studies of the safety and feasibility of LESS have been conducted. However, few comparative studies between LESS and other surgical modalities have been conducted, especially for the malignant diseases [2,6,14].
Several comparative studies of radical nephrectomy have shown no differences in mean OPT, LHS, complications rates, or the use of analgesics between CL and LESS patients [10,17,18]. Moreover, Park et al. [9] reported that radical nephrectomy with LESS is as safe and effective as radical nephrectomy and is associated with less postoperative pain and shorter hospital stays. In our study, although no significant differences in OPT, EBL, transfusion rates, VAS pain score, or LHS were found between the LESS and CL groups for all three surgery types, more complications occurred in the LESS radical nephrectomy group than in the CL radical nephrectomy group. However, because most of the complications with LESS radical nephrectomy occurred in the early introductory period of the procedure, we expect that the complication rates with LESS and CL will cease to be significantly different as surgeons gain more experience.
In the case of partial nephrectomy, more complications occurred with LESS (3/5) than with CL (0/16) in our study. Other studies of partial nephrectomy with LESS showed various complication rates. Irwin et al reported complications in 37.5% (3/8) of cases of partial nephrectomy with LESS [19]. Desai et al. [2] reported 1 complication among 6 patients who underwent partial nephrectomy with LESS. Only five patients at our institution have undergone partial nephrectomy with LESS; therefore, we expect that the incidence of complications will decrease as our surgeons gain more experience. However, given the current level of experience with the LESS techniques, we suggest that partial nephrectomy with LESS be performed restrictively.
Some studies of nephroureterectomy with bladder cuff excision with LESS have shown it to be safe and feasible [20,21]. However, few studies have compared LESS with CL. In our studies, no statistically significant differences in perioperative outcomes were found between nephroureterectomy with LESS and nephroureterectomy with CL, even though the VAS pain scores were higher in the LESS group than in the CL group until the second postoperative day. These higher VAS pain scores in the LESS group may have been related to longer OPTs in the LESS group, especially because of difficulties with bladder cuff excision and bladder repair. However, as surgeons gain more experience, these difficulties will be overcome. If surgery can be conducted and completed through a single, small incision while remaining true to oncological principles and without serious complications (as occurred in our nephroureterectomy cases with LESS), especially for extirpative cases, patients will undoubtedly benefit. Therefore, we suggest that nephroureterectomy with bladder cuff excision with LESS may be used for malignant cases, for which the benefits of LESS could be maximized despite the small number of patients in our study.
There is no doubt that LESS is more technically challenging than CL. Thus, it may not share the broad applicability of CL for complex procedures, although this may change as the technique matures and with robotic innovations in LESS. Therefore, notwithstanding the major limitations of the current study, including the retrospective design and small number of patients, we suggest that LESS should be used selectively and mainly for radical nephrectomy and nephroureterectomy with bladder cuff excision, We also believe that LESS is a very attractive surgical technique, and the benefits of LESS could be maximized in cases requiring extirpative procedures.
A prospective randomized control trial remains the ideal way to assess new surgical innovations; however, it is difficult to use such an approach in actual patients in a clinical setting, as in robot-assisted laparoscopic prostatectomy versus open prostatectomy. Therefore, a practical, well-designed multicenter observational study including more urologic surgeries would provide the necessary guidance to assess the proper role for LESS.
CONCLUSIONS
Perioperative outcomes for radical nephrectomy and nephroureterectomy with bladder cuff excision with LESS were not statistically different from those with the CL approach. Therefore, the use of LESS in these cases is expected to expand as surgeons gain more experience with this technique and as further technical advances in laparoscopic instruments occur. However, partial nephrectomy with LESS should be performed restrictively considering the current level of surgical skills.
Footnotes
The authors have nothing to disclose.
References
- 1.Canes D, Desai MM, Aron M, Haber GP, Goel RK, Stein RJ, et al. Transumbilical single-port surgery: evolution and current status. Eur Urol. 2008;54:1020–1029. doi: 10.1016/j.eururo.2008.07.009. [DOI] [PubMed] [Google Scholar]
- 2.Desai MM, Berger AK, Brandina R, Aron M, Irwin BH, Canes D, et al. Laparoendoscopic single-site surgery: initial hundred patients. Urology. 2009;74:805–812. doi: 10.1016/j.urology.2009.02.083. [DOI] [PubMed] [Google Scholar]
- 3.Irwin BH, Rao PP, Stein RJ, Desai MM. Laparoendoscopic single site surgery in urology. Urol Clin North Am. 2009;36:223–235. doi: 10.1016/j.ucl.2009.02.011. [DOI] [PubMed] [Google Scholar]
- 4.Kommu SS, Kaouk JH, Rane A. Laparo-endoscopic single-site surgery: preliminary advances in renal surgery. BJU Int. 2009;103:1034–1037. doi: 10.1111/j.1464-410X.2008.08282.x. [DOI] [PubMed] [Google Scholar]
- 5.Liatsikos E, Kallidonis P, Kyriazis I, Al-Aown A, Stolzenburg JU. Urologic laparoendoscopic single-site surgery. Nat Rev Urol. 2009;6:654–659. doi: 10.1038/nrurol.2009.217. [DOI] [PubMed] [Google Scholar]
- 6.Stolzenburg JU, Kallidonis P, Hellawell G, Do M, Haefner T, Dietel A, et al. Technique of laparoscopic-endoscopic single-site surgery radical nephrectomy. Eur Urol. 2009;56:644–650. doi: 10.1016/j.eururo.2009.06.022. [DOI] [PubMed] [Google Scholar]
- 7.Ham WS, Im YJ, Jung HJ, Hong CH, Han WK, Han SW. Initial experience with laparoendoscopic single-site nephrectomy and nephroureterectomy in children. Urology. 2011;77:1204–1208. doi: 10.1016/j.urology.2010.07.535. [DOI] [PubMed] [Google Scholar]
- 8.Jeong BC, Park YH, Han DH, Kim HH. Laparoendoscopic single-site and conventional laparoscopic adrenalectomy: a matched case-control study. J Endourol. 2009;23:1957–1960. doi: 10.1089/end.2009.0404. [DOI] [PubMed] [Google Scholar]
- 9.Park YH, Park JH, Jeong CW, Kim HH. Comparison of laparoendoscopic single-site radical nephrectomy with conventional laparoscopic radical nephrectomy for localized renal-cell carcinoma. J Endourol. 2010;24:997–1003. doi: 10.1089/end.2009.0554. [DOI] [PubMed] [Google Scholar]
- 10.Raman JD, Bagrodia A, Cadeddu JA. Single-incision, umbilical laparoscopic versus conventional laparoscopic nephrectomy: a comparison of perioperative outcomes and short-term measures of convalescence. Eur Urol. 2009;55:1198–1204. doi: 10.1016/j.eururo.2008.08.019. [DOI] [PubMed] [Google Scholar]
- 11.Tugcu V, Ilbey YO, Mutlu B, Tasci AI. Laparoendoscopic single-site surgery versus standard laparoscopic simple nephrectomy: a prospective randomized study. J Endourol. 2010;24:1315–1320. doi: 10.1089/end.2010.0048. [DOI] [PubMed] [Google Scholar]
- 12.Autorino R, Cadeddu JA, Desai MM, Gettman M, Gill IS, Kavoussi LR, et al. Laparoendoscopic single-site and natural orifice transluminal endoscopic surgery in urology: a critical analysis of the literature. Eur Urol. 2011;59:26–45. doi: 10.1016/j.eururo.2010.08.030. [DOI] [PubMed] [Google Scholar]
- 13.Rassweiler JJ. Is LESS/NOTES really more? Eur Urol. 2011;59:46–48. doi: 10.1016/j.eururo.2010.08.040. [DOI] [PubMed] [Google Scholar]
- 14.Han WK, Park YH, Jeon HG, Jeong W, Rha KH, Choi H, et al. The feasibility of laparoendoscopic single-site nephrectomy: initial experience using home-made single-port device. Urology. 2010;76:862–865. doi: 10.1016/j.urology.2009.10.038. [DOI] [PubMed] [Google Scholar]
- 15.Jeon HG, Jeong W, Oh CK, Lorenzo EI, Ham WS, Rha KH, et al. Initial experience with 50 laparoendoscopic single site surgeries using a homemade, single port device at a single center. J Urol. 2010;183:1866–1871. doi: 10.1016/j.juro.2010.01.023. [DOI] [PubMed] [Google Scholar]
- 16.Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–196. doi: 10.1097/SLA.0b013e3181b13ca2. [DOI] [PubMed] [Google Scholar]
- 17.Raybourn JH, 3rd, Rane A, Sundaram CP. Laparoendoscopic single-site surgery for nephrectomy as a feasible alternative to traditional laparoscopy. Urology. 2010;75:100–103. doi: 10.1016/j.urology.2009.05.028. [DOI] [PubMed] [Google Scholar]
- 18.Seo IY, Lee JW, Rim JS. Laparoendoscopic single-site radical nephrectomy: a comparison with conventional laparoscopy. J Endourol. 2011;25:465–469. doi: 10.1089/end.2010.0465. [DOI] [PubMed] [Google Scholar]
- 19.Irwin BH, Cadeddu JA, Tracy CR, Kim FJ, Molina WR, Rane A, et al. Complications and conversions of upper tract urological laparoendoscopic single-site surgery (LESS): multicentre experience: results from the NOTES Working Group. BJU Int. 2011;107:1284–1289. doi: 10.1111/j.1464-410X.2010.09663.x. [DOI] [PubMed] [Google Scholar]
- 20.Lee JY, Kim SJ, Moon HS, Kim YT, Lee TY, Park SY. Initial experience of laparoendoscopic single-site nephroureterectomy with bladder cuff excision for upper urinary tract urothelial carcinoma performed by a single surgeon. J Endourol. 2011;25:1763–1768. doi: 10.1089/end.2010.0729. [DOI] [PubMed] [Google Scholar]
- 21.Park YH, Park SY, Kim HH. Laparoendoscopic single-site nephroureterectomy with bladder cuff excision for upper urinary tract transitional-cell carcinoma: technical details based on oncologic principles. J Endourol. 2010;24:563–566. doi: 10.1089/end.2009.0502. [DOI] [PubMed] [Google Scholar]


