Abstract
Exercise is recommended by public health agencies for weight management; however, the role of exercise is generally considered secondary to energy restriction. Few studies exist that have verified completion of exercise, measured the energy expenditure of exercise, and prescribed exercise with equivalent energy expenditure across individuals and genders.
Objective
The objective of this study was to evaluate aerobic exercise, without energy restriction, on weight loss in sedentary overweight and obese men and women.
Design and Methods
This investigation was a randomized, controlled, efficacy trial in 141 overweight and obese participants (body mass index, 31.0 ± 4.6 kg/m2; age 22.6 ± 3.9 years). Participants were randomized (2:2:1 ratio) to exercise at either 400 kcal/session or 600 kcal/session or to a non-exercise control. Exercise was supervised, 5 days/week, for 10 months. All participants were instructed to maintain usual ad libitum diets. Due to the efficacy design, completion of ≥ 90% of exercise sessions was an a priori definition of per protocol, and these participants were included in the analysis.
Results
Weight loss from baseline to 10 months for the 400 and 600 kcal/session groups was 3.9 ± 4.9kg (4.3%) and 5.2 ± 5.6kg (5.7%), respectively compared to weight gain for controls of 0.5 ± 3.5kg (0.5%) (p<0.05). Differences for weight loss from baseline to 10 months between the exercise groups and differences between men and women within groups were not statistically significant.
Conclusions
Supervised exercise, with equivalent energy expenditure, results in clinically significant weight loss with no significant difference between men and women.
Introduction
The prevalence of overweight (BMI ≥ 25.0) and obesity (BMI ≥ 30.0) among US adults is ~68% and 34%, respectively.1 Overweight and obesity contribute to heart disease, hypertension, diabetes, and some cancers as well as psychosocial and economic difficulties.2-5 Exercise is recommended for weight management by virtually every public health organization6-10; however, the role of exercise is generally considered secondary to energy restriction for the treatment of obesity.11-13 The secondary role for exercise may be due to the absence of studies that verify the completion of exercise, measure the energy expenditure of exercise (EEEx), and prescribe the exercise to have equivalent EEEx across individuals and genders. Measurement of EEEx and verification of exercise completion are essential components of any study to adequately evaluate the impact of exercise on weight loss.
The Midwest Exercise Trial-2 (MET-2) was an adequately powered, properly designed, 10 month efficacy trial to evaluate the role of supervised exercise without energy restriction on weight loss in a sample of overweight and obese young adult men and women to address the following aims:
Does exercise without energy restriction result in clinically significant weight change across groups from baseline to 10 months?
Do men and women have equivalent changes in weight in response to exercise completed at equivalent levels of EEEx?
Methods and Procedures
Design
A detailed description of the rationale and design for MET-2 has been published.14 One hundred forty one overweight or obese individuals, age 18-30 years, with a BMI between 25-40 kg/m2 were randomized to an exercise intervention (EEEx = 400 or 600 kcal/session) or non-exercise control condition. Exercise sessions were completed 5 days/week for 10 months, were supervised, and EEEx was assessed monthly by indirect calorimetry. All participants were instructed to maintain their baseline diet and physical activity patterns over the 10 month study. Participants who did not complete ≥90% of scheduled exercise sessions at the assigned level of EEEx and all outcome assessments, were dismissed from the study. Ninety two participants (46 men/46 women) were compliant with the study protocol and are included in the analysis presented herein. The primary outcomes were body weight and body composition. Secondary outcomes of maximal aerobic capacity, energy and macronutrient intake, and daily physical activity are presented briefly and detailed procedures have been published.14 With the exception of EEEx all assessments were identical for the exercise and control groups. All participants provided written informed consent prior to participating and were compensated at a rate of $7.87/hour for an average total of 254 hours for participation in physical activity and testing throughout the study. Approval for this study was obtained from the Human Subjects Committee at the University of Kansas-Lawrence.
Participant inclusion/exclusion
Participants were men and women (BMI 25-40 kg/m2, age 18 to 30 years) who were able to exercise and willing to be randomized. Participants were excluded for the following reasons: A history of chronic disease (i.e., diabetes, heart disease, etc.), elevated blood pressure (>140/90), lipids (cholesterol >6.72 mmol/L; triglycerides >5.65 mmol/L), fasting glucose (>7.8 mmol/L), use of tobacco products, medications affecting physical performance (e.g., beta blockers), or metabolism (e.g., thyroid, steroids), inability to perform laboratory tests or moderate-to-vigorous exercise, and planned physical activity greater than 500 kcal/week.15
Randomization and blinding
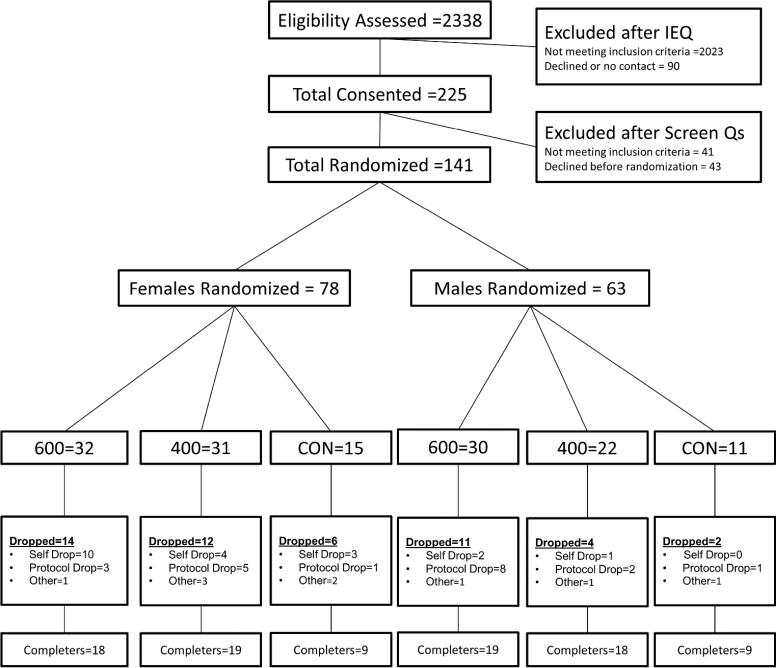
Participants were stratified by gender and randomized by an independent statistician under the supervision of the project statistician (MSM) in a 2:2:1 ratio to 400 and 600 kcal/session and control, respectively (Figure 1). Blinding of participants to group assignment was not possible. Investigators and research assistants were blinded at the level of outcome assessments, data entry and data analysis.
Figure 1.
MET-2 CONSORT Diagram
Exercise Intervention
We evaluated two levels of EEEx at 400 and 600 kcal/session, 5 days/week. These levels of EEEx are consistent with recommendations from The American College of Sports Medicine Position Stand “Appropriate Physical Activity Intervention Strategies for Weight Loss and Prevention of Weight Regain for Adults”.11 Exercise was primarily walking/jogging on motor-driven treadmills; however, to provide variety and decrease overuse injuries, alternate activities were allowed for 20% of the exercise sessions. Exercise progressed from 150 kcal/session at intervention onset to the target EEEx of 400 or 600 kcal/session at the end of month 4 and remained at target for the final 6 months of the study (Table 1).
Table 1. Ten month exercise progression by group kcal/session and exercise intensity.
Baseline characteristics for completers by group and gender (N = 92)
| Month | 400 kcal |
600 kcal |
% heart rate maximum (days/week) |
|---|---|---|---|
| kcal/session | kcal/session | ||
| 1 | 150-175 | 150-250 | 70% (5) |
| 2 | 200-225 | 275-375 | 70% (4) / 80% (1) |
| 3 | 250-325 | 400-500 | 70% (3) / 80% (2) |
| 4 | 350-400 | 525-600 | 70% (0-2) / 80% (3-5) |
| 5-10 | 400 | 600 | 70% (0-1) / 80% (4-5) |
Note. Ten month exercise progression by group and exercise intensity (days/week). For example, in month 2 there were five days of exercise with four exercise sessions completed at 70% and 1 exercise session completed at 80% of heart rate maximum.
Energy expenditure of exercise (EEEx)
Detailed information regarding prescription of exercise has been reported elsewhere.14 Briefly, participants were provided with the duration of exercise sessions required to achieve the prescribed level of EEEx. The duration was provided by results from indirect calorimetry (ParvoMedics TrueOne2400, ParvoMedics Inc., Sandy, UT) whereby the EEEx was measured at 70% and 80% of maximal heart rate. The resulting kcal/min was used to calculate the minutes necessary to achieve the desired EEEx and this procedure was conducted at baseline and repeated monthly with adjustments to the treadmill speed, grade and duration as necessary. For example: EEEx = 9.2 kcal/minute, prescribed exercise = 400 kcal/session, exercise duration = 400/9.2 = 44 minutes/session.
Exercise compliance and supervision
Exercise was supervised by trained research staff and the duration and intensity of all exercise sessions were verified by a heart rate monitor (RS 400; Polar Electro Inc, Woodbury, NY). Compliance was considered as successfully completing ≥ 90% of exercise sessions. Participants who were non compliant during any 3 month interval (months 0-3, 3-6, and 6-9) or during the final month of the study (month 10) were dismissed.
Assessments
Outcome assessments for analyses were completed at baseline and 10 months by trained research assistants. The details of these procedures have been published elsewhere.14
Weight and body composition
Weight was measured between 7 and 10 a.m. using a scale accurate to ±0.1 kg (PS6600, Befour Inc., Saukville, WI). Participants were weighed prior to breakfast and wore a standardized hospital gown. Dual energy x-ray absorptiometry (DXA) was used to determine fat-free mass, fat mass, and percent body fat (Lunar DPX-IQ). Women completed pregnancy testing prior to each DXA test.
Aerobic capacity
Maximal aerobic capacity was assessed on a motor-driven treadmill using a modified Balke protocol.16 The test was considered valid if participants meet three of four criteria: 1) heart rate ±10 beats·min-1 of the age-predicted maximal heart rate, 2) rating of perceived exertion greater than 17, 3) respiratory exchange ratio greater than 1.10, and 4) oxygen consumption plateau.
Energy intake/macronutrient composition
Energy intake and macronutrient composition was assessed over a 7-day period, 4 times over the course of the study during ad libitum eating in The University of Kansas cafeteria. Digital photographs were obtained before and after consumption and the type and amount of foods and beverages consumed were quantified by trained research staff.17,18 Food consumed outside the cafeteria was assessed with multiple pass 24-hour recall procedures. Food and beverage consumption were entered into Nutrition Data System for Research (University of Minnesota, Minneapolis, MN v. 2006) for determination of total energy and macronutrient content.
Physical activity
Daily physical activity outside the exercise program was documented using a portable accelerometer (ActiGraph Model GT1M; Actigraph, LLC, Pensacola, FL). Participants wore the ActiGraph on a belt over the non-dominant hip for 7 consecutive days at baseline, 3, 6 and 10 months. Data were analyzed for daily physical activity using a custom software program.
Sample size
Sample size was determined to provide adequate statistical power for the analysis of aims 1 and 2. Aim 1 compared weight change (10-months baseline) across the three groups. From our previous work,19 we expected participants randomized to the control arm to gain weight (~5%), the 400 kcal/session group to remain weight stable, and participants in the 600 kcal/session group to lose weight (~5%). In our previous studies the 5% gain and 5% loss were equivalent to an average change of approximately 0.5 standard deviations. Given these assumptions, and a conservative rate of attrition of 33%, 136 participants were needed to be randomized to the 400 kcal/session and 600 kcal/session groups and a control group in a 2:2:1 ratio to insure a total sample of 90. A sample of 90 completers provided 88% power to detect the hypothesized difference across the groups using a one-way analysis of variance with a type I error rate of 5%. Aim 2 determined if the change in weight (10-months baseline) was equivalent between males and females for both the 400 and 600 kcal/session groups, respectively. Equivalence was defined as a ratio of the average weight change in males versus females between 0.85 and 1.15. Previous data from MET-1indicated that the coefficient of variation (standard deviation/mean) is 0.10 for change in weight at 10 months.19 Given these assumptions, 18 males and 18 females were necessary to determine if the ratio of the means was equivalent with 95% power assuming a type I error rate of 0.025. Each statistical test was conducted at two levels of exercise, therefore we used a type I error rate of 0.025 for each test.
Statistical Analyses
Baseline demographic and outcome variables were summarized by means and standard deviations. Based upon the design, we first examined if weight loss, BMI, fat mass, body fat percentage, and fat-free mass were equivalent between men and women in the 400 and 600 kcal/session groups. These variables were found not equivalent thus gender, which was a stratification variable, was examined as a potential factor related to the primary and all secondary outcomes using a two factor analysis of variance with treatment and gender as main effects and the interaction effect between gender and treatment. The test for interaction was completed first, and if not significant, tests for main effects were performed. All interaction and main effects were tested at the 0.05 level of significance. Since there were three treatment groups, if a treatment main effect was seen for an outcome, pairwise comparison using Tukey's HSD adjustment was used to determine which treatment groups differed from one another. This investigation was an efficacy study; therefore, all analyses were only conducted on subjects who were compliant and completed the 10 month intervention. No form of imputation was necessary or performed for the analysis presented in this manuscript. All analyses were performed in SAS Software v9.2.
Results
Participants
One hundred forty one individuals were initially randomized to exercise or control and 92 individuals (65.2%) complied with the study protocol and completed all outcome assessments (Figure 1). The baseline characteristics of the 92 completers are shown in Table 2. There were no significant differences in baseline characteristics between the 3 study groups or between participants initially randomized (n =141) and completers (n = 92) with the exception of maximal aerobic capacity.
Table 2. Baseline characteristics for completers by group and gender (N = 92).
Ten month exercise progression by group kcal/session and exercise intensity
| Control |
400 kcal |
600 kcal |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Total (n=18) | Female (n=9) | Male (n=9) | Total (n=37) | Female (n=19) | Male (n=18) | Total (n=37) | Female (n=18) | Male (n=19) | |
| Age (yrs) | 22.6 (3.0) | 21.8 (2.6) | 23.3 (3.4) | 23.(3.0) | 22.6 (2.9) | 23.5 (3.2) | 23.0 (3.5) | 22.6 (3.2) | 23.3 (3.7) |
| Height (cm) | 170.5 (9.7) | 164.9 (6.3) | 177.8 (8.1) | 169.7 (10.0) | 165.1 (6.4) | 176.5 (8.1) | 172.4 (10.1) | 167.1 (5.5) | 178.4 (7.2) |
| Weight (kg) | 87.4 (14.6) | 78.7 (12.6) | 96.2 (11.1) | 91.4 (20.7) | 83.3 (18.9) | 99.9 (19.4) | 92.0 (16.1) | 81.3 (13.0) | 102.1 (11.7) |
| Body Composition | |||||||||
| BMI (kg·m2) | 29.7 (3.8) | 28.9 (3.4) | 30.6 (4.2) | 31.2 (5.6) | 30.4 (5.6) | 32.0 (5.5) | 30.6 (3.9) | 29.1 (3.8) | 32.1 (3.5) |
| Fat mass (kg) | 34.1 (7.7) | 34.1 (7.8) | 34.1 (7.9) | 34.6 (11.2) | 34.8 (11.1) | 34.5 (11.6) | 35.3 (8.4) | 34.1 (9.4) | 36.4 (7.5) |
| Fat-free mass (kg) | 49.2 (9.7) | 40.9 (4.6) | 57.5 (4.9) | 52.3 (11.9) | 44.2 (7.5) | 60.8 (9.4) | 52.6 (11.1) | 43.2 (5.2) | 61.4 (7.1) |
| Body fat (%) | 41.0 (6.1) | 45.1 (4.6) | 36.9 (4.4) | 39.6 (7.5) | 43.6 (5.8) | 35.4 (6.8) | 40.2 (6.2) | 43.5 (5.7) | 37.0 (5.0) |
| Fitness | |||||||||
| VO2 (ml·kg-1·min-1) | 32.3 (5.0) | 30.2 (3.3) | 34.3 (5.8) | 33.4 (6.5) | 29.8 (4.1) | 37.1 (6.5) | 34.1 (5.7) | 31.6 (3.8) | 36.4 (6.4) |
| VO2 (L·min-1) | 2.8 (0.6) | 2.4 (0.2) | 3.2 (0.4) | 3.0 (0.7) | 2.5 (0.4) | 3.6 (0.5) | 3.1 (0.8) | 2.5 (0.3) | 3.7 (0.7) |
| Energy Intake | |||||||||
| kcal per day | 2836.0 (641.7) | 2397.7 (408.3) | 3274.2 (525.7) | 2887.2 (670.2) | 2492.1 (389.4) | 3304.1 (657.4) | 2948.4 (687.3) | 2654.0 (466.5) | 3227.3 (755.2) |
Note. There were no significant differences between the exercise and control groups or for males or females between groups (all p > 0.05).
Exercise compliance
Attendance at exercise sessions did not differ by exercise group (400 kcal/session = 91.9 ± 2.9%, 600 kcal/session = 91.3 ± 3.0 %) or by gender (men = 91.4 ± 3.0%, women = 91.7 ± 2.6%). The average target heart rate for the exercise groups for months 4-10 was 150.6 ± 11.6 beats·min-1 while the actual exercise heart rate averaged 150.8 ± 11.7 beats·min-1. The average EEEx from month 4-10 for the 400 and 600 kcal/session groups was 402 ± 6 and 604 ± 7 kcal/session, respectively. EEEx did not differ between men and women assigned to either of the exercise groups. Women required 48 ± 7 min/session and 63 ± 9 min/session to complete the 400 kcal and 600 kcal prescriptions, respectively. Men required 31 ± 6 min/session and 42 ± 8 min/session to achieve the 400 and 600 kcal prescriptions, respectively.
Body weight/composition
Weight change over the 10 month intervention in both the 400 (-3.9 ± 4.9; 4.3%) and 600 (-5.2 ± 5.6 kg; 5.7%) kcal/session groups was significantly different than control [(0.5 ± 3.5 kg; 0.5%); Table 3]; however, weight change between exercise groups did not differ significantly. There were no significant differences for weight change between men and women in either the 400 (men: -3.8 ± 5.8 kg; 3.7%; women = -4.1 ± 4.2 kg; 4.9%) or 600 kcal/session groups (men: -5.9 ± 6.7 kg; 5.9%; women = -4.4 ± 2.1 kg; 5.4%). Although not significantly different, weight loss for men in the 600 kcal/session group was 2.1 kg greater than for the 400 kcal/session group. Weight loss in women in the 600 kcal/session group was only 0.3 kg greater than the 400 kcal/session group.
Table 3. Change in weight, BMI, body composition and aerobic capacity by group and gender.
Change in weight, BMI, body composition and aerobic capacity by group and gender.
| Variable | Baseline | 10 Month | Change | Group Difference |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (95% CI) | p-value | |
| Weight (kg) | 0.0008ab | |||
| Control | 87.4 (14.6) | 88.0 (15.8) | 0.5 (-1.2, 2.3) | |
| Male | 96.2 (11.1) | 96.7 (12.5) | 0.6 (-1.3, 2.5) | |
| Female | 78.7 (12.6) | 79.2 (14.1) | 0.5 (-3.0, 3.9) | |
| 400 kcal | 91.4 (20.7) | 87.4 (20.2) | -3.9 (-5.6, -2.3) | |
| Male | 99.9 (19.4) | 96.1 (19.0) | -3.8 (-6.6, -0.9) | |
| Female | 83.3 (18.9) | 79.2 (18.1) | -4.1 (-6.1, -2.0) | |
| 600 kcal | 92.0 (16.1) | 86.8 (16.6) | -5.2 (-7.0, -3.3 ) | |
| Male | 102.0 (11.7) | 96.2 (14.2) | -5.9 (-9.1, -2.7) | |
| Female | 81.3 (13.0) | 76.9 (12.8) | -4.4 (-6.5, -2.3) | |
| BMI (kgm2) | 0.0007ab | |||
| Control | 29.7 (3.8) | 29.9 (4.4) | 0.2 (-0.5, 0.8) | |
| Male | 30.6 (4.2) | 30.7 (4.4) | 0.2 (-0.4, 0.8) | |
| Female | 28.9 (3.4) | 29.1 (4.4) | 0.2 (-1.1, 1.5) | |
| 400 kcal | 31.2 (5.6) | 29.8 (5.5) | -1.4 (-1.9, -0.8) | |
| Male | 32.0 (5.5) | 30.8 (5.5) | -1.2 (-2.1, -0.3) | |
| Female | 30.4 (5.6) | 28.9 (5.4) | -1.5 (-2.2, -0.8) | |
| 600 kcal | 30.6 (3.9) | 28.9 (4.2) | -1.7 (-2.3, -1.1) | |
| Male | 32.1 (3.5) | 30.2 (4.3) | -1.9 (-2.9, -0.9) | |
| Female | 29.1 (3.8) | 27.5 (3.7) | -1.6 (-2.3, -0.8) | |
| Body fat (%) | 0.0064b | |||
| Control | 41.0 (6.1) | 40.4 (7.2) | -0.6 (-1.7, 0.6) | |
| Male | 36.9 (4.4) | 35.8 (5.6) | -1.1 (-2.6, 0.5) | |
| Female | 45.1 (4.6) | 45.0 (5.5) | -0.1 (-2.1, 2.0) | |
| 400 kcal | 39.6 (7.5) | 36.6 (8.3) | -2.9 (-4.3, -1.6) | |
| Male | 35.4 (6.8) | 32.8 (7.5) | -2.7 (-4.9, -0.4) | |
| Female | 43.6 (5.8) | 40.5 (7.3) | -3.2 (-4.9, -1.6) | |
| 600 kcal | 40.2 (6.2) | 35.9 (7.6) | -4.3 (-5.8, -2.8) | |
| Male | 37.0 (5.0) | 32.5 (6.8) | -4.5 (-6.9, -2.2) | |
| Female | 43.5 (5.7) | 39.4 (6.8) | -4.1 (-6.1, -2.1) | |
| Fat mass (kg) | 0.001b | |||
| Control | 34.1 (7.7) | 34.2 (9.1) | 0.2 (-1.4, 1.7) | |
| Male | 34.1 (7.9) | 34.0 (9.5) | -0.1 (-2.6, 2.4) | |
| Female | 34.1 (7.8) | 34.5 (9.2) | 0.4 (-2.1, 2.9.) | |
| 400 kcal | 34.6 (11.2) | 31.3 (11.6) | -3.5 (-5.1, -1.8) | |
| Male | 34.5 (11.6) | 31.0 (11.4) | -3.6 (-6.2, -0.9) | |
| Female | 34.8 (11.1) | 31.7 (12.2) | -3.4 (-5.7, -1.1) | |
| 600 kcal | 35.3 (8.4) | 30.1 (9.7) | -5.2 (-6.9, -3.4) | |
| Male | 36.4 (7.5) | 30.5 (10.1) | -5.9 (-8.8, -3.0) | |
| Female | 34.1 (9.4) | 29.7 (9.6) | -4.4 (-6.6, -2.3) | |
| Fat free mass (kg) | 0.0733 | |||
| Control | 52.1 (10.1) | 53.3 (11.5) | 1.2 (0.2, 2.1) | |
| Male | 60.7 (5.0) | 62.8 (6.2) | 2.1 (0.8, 3.3) | |
| Female | 43.5 (5.1) | 43.7 (6.3) | 0.3 (-1.2, 1.7) | |
| 400 kcal | 55.7 (12.5) | 55.7 (12.1) | 0.0 (-0.6, 0.7) | |
| Male | 64.4 (9.9) | 64.4 (9.2) | 0.0 (-1.0, 1.0) | |
| Female | 46.9 (8.0) | 47.0 (7.7) | 0.1 (-0.7, 0.9) | |
| 600 kcal | 55.8 (11.5) | 56.4 (11.2) | 0.6 (0.1, 1.1) | |
| Male | 65.0 (7.3) | 65.4 (7.4) | 0.4 (-0.4, 1.2) | |
| Female | 46.1 (5.3) | 46.9 (4.8) | 0.8 (0.2, 1.5) | |
| VO2 (ml·kg-1·min-1) | <0.0001ab | |||
| Control | 32.3 (5.0) | 31.4 (5.3) | -0.9 (-1.9, 0.1) | |
| Male | 34.3 (5.8) | 33.0 (6.4) | -1.3 (-3.2, 0.5) | |
| Female | 30.2 (3.3) | 29.8 (3.7) | -0.4 (-1.6, 0.7) | |
| 400 kcal | 33.4 (6.5) | 39.4 (7.9) | 5.9 (4.6, 7.2) | |
| Male | 37.1 (6.5) | 42.9 (8.0) | 5.8 (4.2, 7.3) | |
| Female | 29.8 (4.1) | 35.9 (6.2) | 6.1 (3.8, 8.3) | |
| 600 kcal | 34.1 (5.7) | 40.8 (7.2) | 6.7 (5.3, 8.1) | |
| Male | 36.4 (6.4) | 44.2 (7.6) | 7.8 (5.4, 10.2) | |
| Female | 31.6 (3.8) | 37.2 (4.7) | 5.6 (4.2, 7.1) | |
| VO2 (L·min-1) | <0.0001ab | |||
| Control | 2.8 (0.6) | 2.7 (0.5) | -0.1 (-0.1, 0.0 ) | |
| Male | 3.2 (0.4) | 3.1 (0.4) | -0.1 (-0.2, 0.0) | |
| Female | 2.4 (0.2) | 2.3 (0.3) | -0.0 (-0.1, 0.1) | |
| 400 kcal | 3.0 (0.7) | 3.4 (0.8) | 0.3 (0.2, 0.4) | |
| Male | 3.6 (0.5) | 4.0 (0.5) | 0.4 (0.3, 0.5) | |
| Female | 2.5 (0.4) | 2.7 (0.5) | 0.2 (0.0, 0.5) | |
| 600 kcal | 3.1 (0.8) | 3.5 (0.9) | 0.4 (0.3, 0.5) | |
| Male | 3.7 (0.7) | 4.2 (0.7) | 0.6 (0.4, 0.7) | |
| Female | 2.5 (0.3) | 2.8 (0.3) | 0.3 (0.2, 0.4) |
Note.
Indicates 400 kcal/session group differs from control group.
Indicates 600 kcal/session group differs from control group. 400 kcal/session and 600 kcal/session were not different (all p > 0.05). No gender effect or group-gender interaction (all p > 0.05).
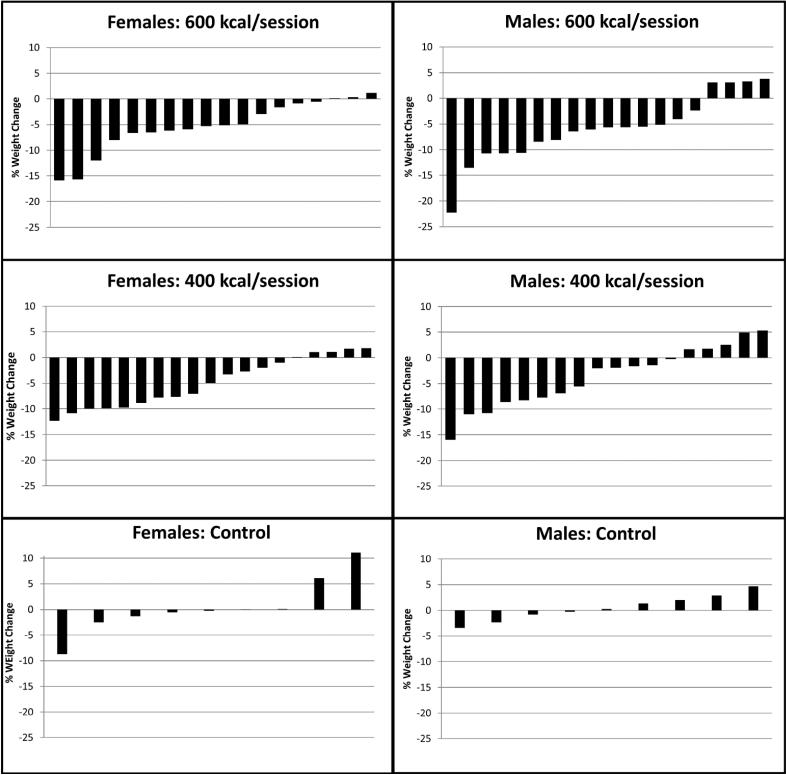
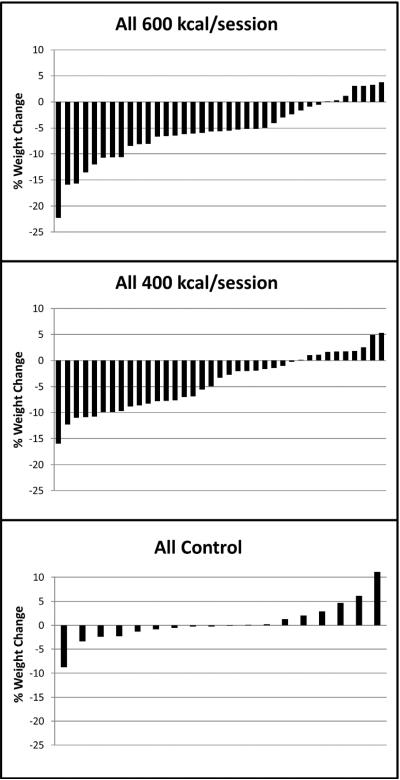
Figure 2 presents individual data for percent weight change by group. In the 600 kcal/session group 62.2% of participants achieved weight loss ≥ 5% of baseline weight compared with 45.9% in the 400 kcal/session group. In the 600 kcal/session group 55.6% of women and 68.4% of men achieved ≥ 5% of baseline weight loss compared with 47.4% of women and 44.5% of men in the 400 kcal/session group (Figure 3). Forty four percent of participants in the control group gained weight compared to 27% in the 400 and 19% in the 600 kcal/session groups.
Figure 2.
Individual weight change percent by group and gender
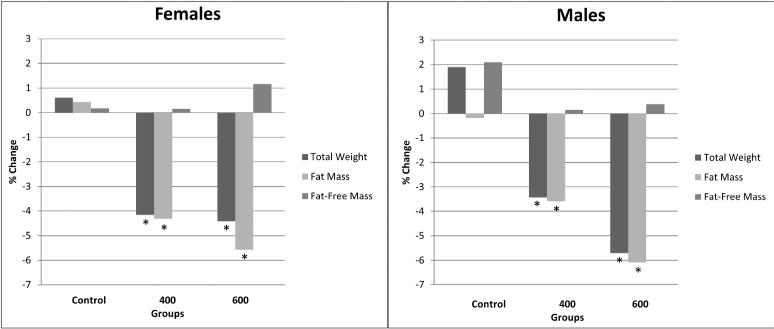
Figure 3.
Body composition change percent by group and gender. * Indicates significantly different from control group.
At 10 months, the mean change in fat mass was significantly different from baseline in both the 400 kcal/session (-3.5 ± 4.8 kg,) and 600 kcal/session groups (-5.2 ± 5.2 kg), but not in controls (+0.2 ± 3.2 kg). The reduction in fat mass in the 400 and 600 kcal/session groups was significantly different from control but it was not significantly different between exercise groups. There were no significant differences for change in fat mass between men and women in either the 400 (men: -3.6 ± 5.3 kg, women: -3.4 ± 4.6 kg) or 600 (men: -5.9 ± 6.0 kg, women: -4.4 ± 4.3 kg) kcal/session groups.
Significant changes in percent body fat over 10 months were observed in both the 400 (-2.9 ± 3.9 %) and 600 (-4.4 ± 4.4 %) kcal/session groups. Percent fat was unchanged in the control group (-0.6 ± 2.4 %). The change in percent fat was significantly greater in the 600 kcal/session group compared with the control group but did not differ between the 400 kcal/session and control groups or between the 400 and 600 kcal/session groups. The reductions in body weight observed in both exercise groups were a result of decreased fat mass and preservation or increase in fat-free mass (Figure 4). At 10 months, there were significant differences between the control group and both the 400 and 600 kcal/session groups for total weight and fat mass. The reduction in total weight and fat mass in the 400 and 600 kcal/session groups was not significantly different between exercise groups by gender.
Figure 4.
Individual weight change percent by group
Aerobic capacity
Maximal oxygen consumption (ml·kg-1·min-1) increased 18.3 ± 13.2% and 20.2 ±13.5% for the 400 and 600 kcal/session groups, respectively and these changes were significantly different compared to the control group that declined -2.8 ± 5.6%. The change in maximal oxygen consumption was not significantly different between the exercise groups and was not significantly different between men and women for the 400 and 600 kcal/session groups and control group.
Energy intake/Physical Activity
There were no significant between group differences for energy intake (kcal/day) over the 10 month intervention. Daily physical activity in the control group did not change over the 10 month intervention. During the intervention, daily physical activity in both exercise groups was significantly greater than control; however, there were no significant differences between exercise groups.
Discussion
This study was designed and adequately powered to determine differences for weight change from baseline to 10 months between control and 2 levels of verified EEEx during an ad libitum diet. Exercise with EEEx of 400 or 600 kcal/session provided clinically meaningful weight loss (average 5%).11 When exercise is supervised and EEEx is of a sufficient magnitude, weight loss from exercise alone surpasses that observed in many very intense behavioral weight loss interventions using energy restriction20,21 and provides weight loss similar to the most successful interventions such as the Diabetes Prevention Program 22-24 without using energy restriction or intensive behavioral counseling. Moreover, weight loss with exercise, during ad libitum diet, was entirely due to loss in fat mass (100%). These results are comparable to previous exercise studies where fat mass decreased and lean mass remained unchanged or increased.19,25,26 In contrast, studies that use energy restriction and exercise for weight loss often observe reductions in lean mass that typically accounts for 22% to 30% of weight loss.27,28
Our results are in general agreement with the limited number of studies in individuals where exercise was verified, prescribed exercise by level of EEEx, and delivered in a dose sufficient to induce weight loss. For example, Ross et al.29 reported a mean weight loss of 8% in 16 obese middle age men (~45 yrs.) who completed 700 kcal/day (70% peak VO2) treadmill exercise over 12 weeks. Ross et al.30 have shown similar results in a sample of 17 obese post-menopausal women (~43 yrs) where a 14 week 500 kcal/day (80% maximal heart rate) aerobic exercise program resulted in a mean weigh loss of 6.8%. King et al.31 reported a mean weight loss of 4.1% in a sample of overweight and obese middle-aged age (~30 yrs.) men (n = 10) and women (n = 25) who participated in a 12 week supervised exercise program with EEEx of 500 kcal/session, 5 days/week.
The literature on exercise level and weight loss is limited and results are mixed.32 For example, Jakicic et al.33 reported nearly identical and clinically non significant weight loss in a sample of predominantly women (~ 90%) who were randomly assigned to 18 months of non-supervised aerobic exercise at 150 (-0.9%) or 300 minutes/week (-1.1%). Similar results were reported by Church et al.34 from a 6 month trial of supervised exercise (3-4 days/week, 50% VO2 peak) at 4 kcal/kg/week (72 min), 8 kcal/kg/week (136 min) or 12 kcal·kg-1·wk-1 (194 min). Weight loss in all the exercise groups was minimal and did not increase significantly with increased levels of exercise (4 kcal·kg-1·xwk-1 = -1.7%, 8 kcal·kg-1·wk-1 = -2.5%, 12 kcal·kg-1·wk-1 = -1.8%). These results are in contrast to those reported by both Slentz et al.35 and Irwin et al.36. For example, Slentz et al.35 completed a supervised exercise trial that compared weight loss between groups randomly assigned to either low (14 kcal·kg-1·wk-1) or high (23 kcal·kg-1·wk-1) volume exercise at 65-85% peak VO2 (3.5 days/week) over 8 months in middle aged to older (45-65 yrs) sedentary overweight men and women. Weight loss in the high volume group (-4.1%) was significantly greater than that observed in the low volume group (-1.3%). We ight loss data was not reported by gender, therefore it is not possible to determine if there was an effect of gender on the dose-response association.
No significant gender differences for weight loss at equivalent levels of EEEx were observed in the current study. This is in contrast to the results from our previous exercise trial (MET-1) where exercise was prescribed by frequency, intensity and duration which resulted in higher levels of EEEx and weight loss for men compared to women as a function of differences in body weight.19 Taken together, the results from MET-1 and the current study (MET-2) demonstrate the importance of prescribing exercise by level of EEEx when addressing questions relative to the impact of exercise on gender responses for body weight and composition. We are aware of only one additional report on gender differences for weight loss in response to exercise without energy restriction. After completing a 12 month program of aerobic exercise, Stefanick et al.37) reported similar and non-significant weight loss for both men (-0.6 kg, 0.7%) and women (-0.4 kg, 0.6%). However, the exercise program employed by Stefanick et al.37 was only partially supervised, prescribed by distance walked/jogged (10 miles/week), and compliance with the exercise protocol inadequately documented; thus, the results should be interpreted cautiously.
A high level of individual variability in weight change was observed in both the 400 and 600 kcal/session within the groups (Figure 2) even though the level of EEEx was tightly controlled. Inherent inter-individual genetic differences in the weight response to exercise would be expected. However, the high degree of inter-individual variability in weight change suggests compensation in components of energy balance. Further work is warranted to identify the sources of compensation in both behavioral (i.e., energy intake, physical activity) and physiologic parameters (i.e., resting metabolic rate, appetite hormones) which might be potentially be modified to improve the efficacy of the use of exercise for targeted weight management interventions.
Strengths of the current investigation include supervised exercise prescribed by level of EEEx rather than frequency, intensity, and duration, and delivery of EEEx with a high level of precision (± 1% of target). The design of the study clearly illustrates the influence of the method of exercise prescription on outcomes of weight. To our knowledge, this is the only study to have a priori designed tests examining the equivalence of weight loss between men and women for varying exercise regimens. Limitations of this study may include the rate of attrition (34.8%). However, we emphasize that MET-2 was an efficacy study designed to answer questions relative to the effect of exercise when completed as intended, and not designed to answer questions if exercise is completed as intended (i.e., effectiveness). Efficacy studies generally have higher attrition compared to effectiveness trials. We projected an overall attrition of 33% in our power calculations and the actual rate was 34.8%. The current study design included strict protocol requirements for compliance. In addition to participant attrition, we also dismissed individuals that fell below the compliance criteria. The attrition rate is not unlike other weight loss studies found in the literature. For example, the attrition rate in a 16 week clinic-based weight loss program in 866 individuals was 31%.38 Another weight loss program in nearly 1800 people across 23 medical centers observed an attrition rate of 52% at 12 months.39 Additionally, due to the inclusion criteria (age, BMI) caution should be used for projecting these results to other populations. Lastly, the magnitude of weight loss may not generalize to studies that use intent to treat designs where compliance is not a criteria for inclusion in analysis and weight loss is generally lower compared to the current study.20,23,24
Summary
EEEx at 400 or 600 kcal/session resulted in a significant reduction in weight compared to controls. The average weight loss of 5% was due to reductions in fat mass and these reductions are known to provide improvements in chronic disease risk factors. Prescription of exercise using EEEx rather than frequency, intensity and duration resulted in similar weight loss for men and women in both exercise groups. Absence of a significant increase in weight loss between the 400 and 600 kcal/session groups suggests compensation in components of energy balance and warrants additional investigation that could lead to targeted interventions. When weight and gender are variables of interest, we recommend that exercise be prescribed using EEEx.
Acknowledgments
This study was supported by the National Institutes of Health (NIH) grant R01-DK049181.
Footnotes
Disclosure: The authors have no conflict of interest to declare.
References
- 1.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999 2008. JAMA. 2010;303(3):235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 2.U.S.Department of Health and Human Services P . Healthy People 2000: National health promotion and disease prevention objectives. DHHS Publication No. (PHS) 91-50212. U.S. Government Printing Office, Public Health Service; Washington, D.C.: 1990. [Google Scholar]
- 3.Gortmaker SL, Must A, Perrin JM, Sobol AM, Dietz WH. Social an economic consequences of overweight in adolescence and young adulthood. N Engl J Med. 1993;329(14):1008–1012. doi: 10.1056/NEJM199309303291406. [DOI] [PubMed] [Google Scholar]
- 4.Mokdad AH, Ford ES, Bowman BA, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289:76–79. doi: 10.1001/jama.289.1.76. [DOI] [PubMed] [Google Scholar]
- 5.Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. JAMA. 1999;282(16):1523–1529. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- 6.Shephard RJ, Lankenau B, Pratt M, et al. Physical Activity Policy Development: a synopsis of the WHO/CDC Consultation, September 29 through October 2, 2002, Atlanta, Georgia. Public Health Rep. 2004;119(3):346–351. doi: 10.1016/j.phr.2004.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pate RR, Pratt M, Blair SN, et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273(5):402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control Healthy people 2000 review 1997. Healthy People 2000. 1997:1–223. [Google Scholar]
- 9.U.S.Department of Health and Human Services Physical activity and health: a report of the surgeon general. U.S.Department of Health and Human Services. 1996 [Google Scholar]
- 10.U.S. Department of Health and Human Services Public Health Service. Office of Disease Prevention and Health Promotion [December 2011];Healthy People 2010. Available at http://www.healthypeople.gov/2010/.
- 11.Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK. American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;41(2):459–471. doi: 10.1249/MSS.0b013e3181949333. [DOI] [PubMed] [Google Scholar]
- 12.Katzel LI, Bleecker ER, Colman EG, Rogus EM, Sorkin JD, Goldberg AP. Effects of weight loss vs aerobic exercise training on risk factors for coronary disease in healthy, obese, middle-aged and older men. A randomized controlled trial. JAMA. 1995;274(24):1915–1921. doi: 10.1001/jama.1995.03530240025035. [DOI] [PubMed] [Google Scholar]
- 13.Janssen I, Katzmarzyk PT, Ross R. Body mass index, waist circumference, and health risk: evidence in support of current National Institutes of Health guidelines. Arch Intern Med. 2002;162(18):2074–2079. doi: 10.1001/archinte.162.18.2074. [DOI] [PubMed] [Google Scholar]
- 14.Donnelly JE, Washburn RA, Smith BK, et al. A randomized, controlled, supervised, exercise trial in young overweight men and women: The Midwest Exercise Trial II (MET2). Contemp Clin Trials. 2012 doi: 10.1016/j.cct.2012.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Taylor H, Jacobs D, Schucker B, Knudsen J, Leon A, Debacker G. A questionnaire for the assessment of leisure time physical activities. J Chronic Dis. 1978;31:741–755. doi: 10.1016/0021-9681(78)90058-9. [DOI] [PubMed] [Google Scholar]
- 16.American College of Sports Medicine Guidelines for exercise testing and prescription. 6 ed. Lippincott Williams & Wilkins; Philadelphia: 2000. [Google Scholar]
- 17.Grunwald GK, Sullivan DK, Hise M, et al. Number of days, number of subjects, and sources of variation in longitudinal intervention or crossover feeding trials with multiple days of measurement. Br J Nutr. 2003;90(6):1087–1095. doi: 10.1079/bjn2003989. [DOI] [PubMed] [Google Scholar]
- 18.Hise ME, Sullivan DK, Jacobsen DJ, Johnson SL, Donnelly JE. Validation of energy intake measurements determined from observer-recorded food records and recall methods compared with the doubly labeled water method in overweight and obese individuals. Am J Clin Nutr. 2002;75:263–267. doi: 10.1093/ajcn/75.2.263. [DOI] [PubMed] [Google Scholar]
- 19.Donnelly JE, Hill JO, Jacobsen DJ, et al. Effects of a 16-month randomized controlled exercise trial on body weight and composition in young, overweight men and women: the Midwest Exercise Trial. Arch Intern Med. 2003;163(11):1343–1350. doi: 10.1001/archinte.163.11.1343. [DOI] [PubMed] [Google Scholar]
- 20.Ross R, Lam M, Blair SN, et al. Trial of prevention and reduction of obesity through active living in clinical settings: a randomized controlled trial. Arch Intern Med. 2012;172(5):414–424. doi: 10.1001/archinternmed.2011.1972. [DOI] [PubMed] [Google Scholar]
- 21.Bennett GG, Warner ET, Glasgow RE, et al. Obesity Treatment for Socioeconomically Disadvantaged Patients in Primary Care Practice. Arch Intern Med. 2012 doi: 10.1001/archinternmed.2012.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Knowler WC, Barrett Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Appel LJ, Clark JM, Yeh HC, et al. Comparative effectiveness of weight-loss interventions in clinical practice. N Engl J Med. 2011;365(21):1959–1968. doi: 10.1056/NEJMoa1108660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wadden TA, Volger S, Sarwer DB, et al. A two-year randomized trial of obesity treatment in primary care practice. N Engl J Med. 2011;365(21):1969–1979. doi: 10.1056/NEJMoa1109220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wood PD, Stefanick ML, Dreon DM, et al. Changes in plasma lipids and lipoproteins in overweight men during weight loss through dieting as compared with exercise. N.Engl.J.Med. 1988;319(18):1173–1179. doi: 10.1056/NEJM198811033191801. [DOI] [PubMed] [Google Scholar]
- 26.Lee S, Kuk JL, Davidson LE, et al. Exercise without weight loss is an effective strategy for obesity reduction in obese individuals with and without Type 2 diabetes. J Appl Physiol. 2005;99(3):1220–1225. doi: 10.1152/japplphysiol.00053.2005. [DOI] [PubMed] [Google Scholar]
- 27.Metzner CE, Folberth-Vogele A, Bitterlich N, et al. Effect of a conventional energy-restricted modified diet with or without meal replacement on weight loss and cardiometabolic risk profile in overweight women. Nutr Metab (Lond) 2011;8(1):64. doi: 10.1186/1743-7075-8-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nicklas BJ, Wang X, You T, et al. Effect of exercise intensity on abdominal fat loss during calorie restriction in overweight and obese postmenopausal women: a randomized, controlled trial. Am J Clin Nutr. 2009;89(4):1043–1052. doi: 10.3945/ajcn.2008.26938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ross R, Dagnone D, Jones PJ, et al. Reduction in obesity and related comorbid conditions after diet-induced weight loss or exercise-induced weight loss in men. A randomized, controlled trial. Ann Intern Med. 2000;133(2):92–103. doi: 10.7326/0003-4819-133-2-200007180-00008. [DOI] [PubMed] [Google Scholar]
- 30.Ross R, Janssen I, Dawson J, et al. Exercise-induced reduction in obesity and insulin resistance in women: a randomized controlled trial. Obes Res. 2004;12(5):789–798. doi: 10.1038/oby.2004.95. [DOI] [PubMed] [Google Scholar]
- 31.King NA, Hopkins M, Caudwell P, Stubbs RJ, Blundell JE. Individual variability following 12 weeks of supervised exercise: identification and characterization of compensation for exercise-induced weight loss. Int J Obes (Lond) 2008;32(1):177–184. doi: 10.1038/sj.ijo.0803712. [DOI] [PubMed] [Google Scholar]
- 32.Ross R, Janssen I. Physical activity, total and regional obesity: dose-response considerations. Med Sci Sports Exerc. 2001;33(6 Suppl):S521–527. doi: 10.1097/00005768-200106001-00023. discussion S528-529. [DOI] [PubMed] [Google Scholar]
- 33.Jakicic JM, Otto AD, Lang W, et al. The Effect of Physical Activity on 18-Month Weight Change in Overweight Adults. Obesity (Silver Spring) 2011 doi: 10.1038/oby.2010.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Church TS, Martin CK, Thompson AM, Earnest CP, Mikus CR, Blair SN. Changes in weight, waist circumference and compensatory responses with different doses of exercise among sedentary, overweight postmenopausal women. PLoS One. 2009;4(2):e4515. doi: 10.1371/journal.pone.0004515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Slentz CA, Duscha BD, Johnson JL, et al. Effects of the amount of exercise on body weight, body composition, and measures of central obesity - STRRIDE - A randomized controlled study. Archives of Internal Medicine. 2004;164(1):31–39. doi: 10.1001/archinte.164.1.31. [DOI] [PubMed] [Google Scholar]
- 36.Irwin ML, Yasui Y, Ulrich CM, et al. Effect of exercise on total and intra-abdominal body fat in postmenopausal women: a randomized controlled trial. JAMA. 2003;289(3):323–330. doi: 10.1001/jama.289.3.323. [DOI] [PubMed] [Google Scholar]
- 37.Stefanick ML, Mackey S, Sheehan M, Ellsworth N, Haskell WL, Wood PD. Effects of diet and exercise in men and postmenopausal women with low levels of HDL cholesterol and high levels of LDL cholesterol. N Engl J Med. 1998;339(1):12–20. doi: 10.1056/NEJM199807023390103. [DOI] [PubMed] [Google Scholar]
- 38.Honas JJ, Early JL, Frederckson DD, O'Brian MS. Predictors of attrition in a large clinic-based weight-loss program. Obesity Research. 2003;11(7):888–894. doi: 10.1038/oby.2003.122. [DOI] [PubMed] [Google Scholar]
- 39.Dalle Grave R, Calugi S, Molinari E, et al. Weight loss expectations in obese patients and treatment attrition: an observational multicenter study. Obes Res. 2005;13(11):1961–1969. doi: 10.1038/oby.2005.241. [DOI] [PubMed] [Google Scholar]