Abstract
Purpose
Global sagittal alignment is considered as an important aspect in the management of spinal disorders, but the evidence establishing its clinical impact in lumbosacral spondylolisthesis is still poor. This study evaluated the impact of global sagittal alignment on the health-related quality of life (HRQOL) of patients with spondylolisthesis.
Methods
A retrospective study of 149 consecutive unoperated children and adolescents presenting with lumbosacral spondylolisthesis (117 low-grade and 32 high-grade) was performed. Two global sagittal alignment parameters were measured on standing lateral radiographs: spinal tilt (ST) and C7 plumbline deviation (C7P deviation). All patients completed the SRS-22 questionnaire to assess HRQOL. Pearson’s correlations were calculated between parameters of global sagittal alignment and HRQOL. Multiple regression analyses were also undertaken to account for slip percentage and lumbosacral kyphosis (LSK).
Results
Both global sagittal alignment parameters were correlated with the SRS-22 total score. When analyzed separately, the correlation was absent in patients with a low-grade slip but remained significant for patients with a high-grade slip (r = 0.35 for ST; r = −0.35 for C7P deviation). The relation was strengthened in high-grade spondylolisthesis when considering only patients with a C7P in front of the posterior corner of upper sacral endplate (r = 0.48 for ST; r = –0.48 for C7P deviation) and was also positive for the SRS-22 pain and appearance domains. For these last patients, the relationship with global sagittal alignment remained significant in the multiple regression analysis. HRQOL was particularly worse for high-grade patients with a C7P in front of the hip axis.
Conclusions
In high-grade spondylolisthesis, an increasing positive sagittal alignment was related to a poorer SRS-22 total score, especially when the C7P is in front of the hip axis. Global sagittal alignment should particularly be assessed in patients with high-grade spondylolisthesis.
Keywords: Quality of life, Sagittal alignment, Spine, Spondylolisthesis
Introduction
Although lumbosacral spondylolisthesis involves a local deformity at the lumbosacral junction, it can have a meaningful impact on the sagittal alignment of the entire spine. The global sagittal alignment, a measure of the overall alignment of the spine from a single parameter, is considered by many clinicians of prime importance in the evaluation and surgical planning of patients with spondylolisthesis, but the evidence supporting its clinical impact remains limited [1].
Studies from Glassman et al. [2, 3] and Mac-Thiong et al. [4] have reported significant correlations between global sagittal alignment and health related quality of life (HRQOL) in adult patients with spinal deformity. Berven et al. [5] addressed this relationship specifically for adult spondylolisthesis and found that global sagittal alignment was the only individual radiographic parameter with a moderate correlation with health status.
Some authors have compared the sagittal alignment of the spine between normal subjects and patients with spondylolisthesis, and have attempted to provide better understanding of the global sagittal alignment for these patients. Jackson et al. [6] and Rajnics et al. [7] have not found any difference in global sagittal alignment between spondylolisthetic and normal adults. Mac-Thiong et al. [8] have later described abnormal global sagittal alignment in high-grade spondylolisthesis, suggesting that evaluation of this parameter is particularly important for these patients. However, these studies did not relate parameters of global sagittal alignment to HRQOL.
Also, the classification of lumbosacral spondylolisthesis proposed by the Spinal Deformity Study Group (SDSG) introduced global sagittal alignment, measured by the position of the C7 plumbline with respect to the femoral heads, as one of three important characteristics that should be assessed in high-grade spondylolisthesis [9]. However, evidence-based data supporting that global alignment has a clinical impact on the HRQOL of young patients with lumbosacral spondylolisthesis are still poor.
The hypothesis of this study is that global sagittal alignment is related to HRQOL for children and adolescents with lumbosacral spondylolisthesis. The purpose of this study is to determine if global sagittal alignment is relevant in the clinical evaluation of lumbosacral spondylolisthesis. Accordingly, the relationship between parameters of global sagittal alignment and HRQOL has been assessed in a cohort of 149 children and adolescents with unoperated lumbosacral spondylolisthesis.
Materials and methods
The medical and radiographic files of 149 consecutive children and adolescents evaluated for isthmic lumbosacral spondylolisthesis at a single pediatric institution were retrospectively studied. Although some patients (n = 32) underwent spine surgery, all data included in the study were taken prior to surgery for these patients. There were 93 females and 56 males, aged 13.5 ± 7.0 years.
Of the 149 patients included in the study, 117 had low-grade spondylolisthesis and 32 patients had high-grade spondylolisthesis. Low-grade spondylolisthesis refers to a slip percentage smaller than 50 %, while high-grade spondylolisthesis refers to a slip percentage of 50 % or greater. The mean percentage of slip was 17 ± 10 % (range 0.2–49 %) for low-grade patients, and 79 ± 16 % (range 51–100 %) for high-grade patients. Each patient completed the SRS-22 questionnaire.
All radiographs were taken using the same radiograph setting, with subjects standing in a comfortable position with hips and knees fully extended. The elbows were fully flexed with the fists resting on the clavicles [10]. Radiographs were evaluated using the custom software IdeFx (LIO, CHUM Notre-Dame, Montréal, Canada). All measurements were done by the same observer.
On standing lateral radiographs of the spine and pelvis, the following anatomical landmarks are identified with the use of the software for all subjects: center of C7 vertebral body, four corners (antero-superior, postero-superior, antero-inferior, and postero-inferior) of L5 and S1, and contours of both femoral heads. Based on the position of these anatomical landmarks, the software calculated the following parameters of global sagittal alignment:
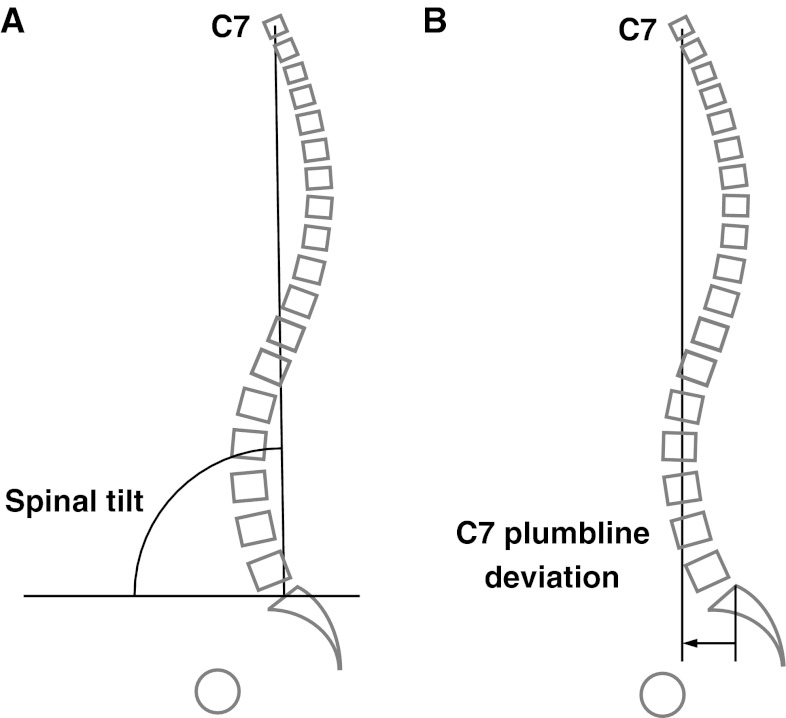
Spinal tilt (ST) [11]: angle subtended by the horizontal line and the line from the center of C7 vertebral body to the center of upper sacral endplate (Fig. 1a). ST is smaller than 90° when the center of C7 vertebral body is in front of the center of upper sacral endplate, and greater than 90° when behind it.
C7 plumbline deviation (C7P deviation): horizontal distance between C7P (vertical line originating from the middle of the C7 vertebral body) and the posterior corner of upper sacral endplate (Fig. 1b). C7P deviation is positive when C7P falls in front of the posterior corner of upper sacral endplate, and negative when behind it.
Fig. 1.
a Measurement of spinal tilt. b Measurement of the C7 plumbline deviation
Using various additional landmarks, the following pelvic and regional sagittal parameters were measured to detail the pelvic morphology and regional sagittal alignment of all patients:
Thoracic kyphosis (TK): the angle between the upper endplate of T1 and the lower endplate of T12.
Lumbar lordosis (LL): the angle between the upper sacral endplate and the upper endplate of L1.
Pelvic incidence (PI): the angle between a line joining the center of the upper endplate of S1 to the axis of the femoral heads and a line perpendicular to the upper endplate of S1.
Sacral slope (SS): the angle between the upper sacral endplate and the horizontal line.
Pelvic tilt (PT): the angle between the vertical line and the line joining the middle of the sacral endplate and the axis of the femoral heads. It is positive when the hip axis lies in front of the middle of the sacral endplate.
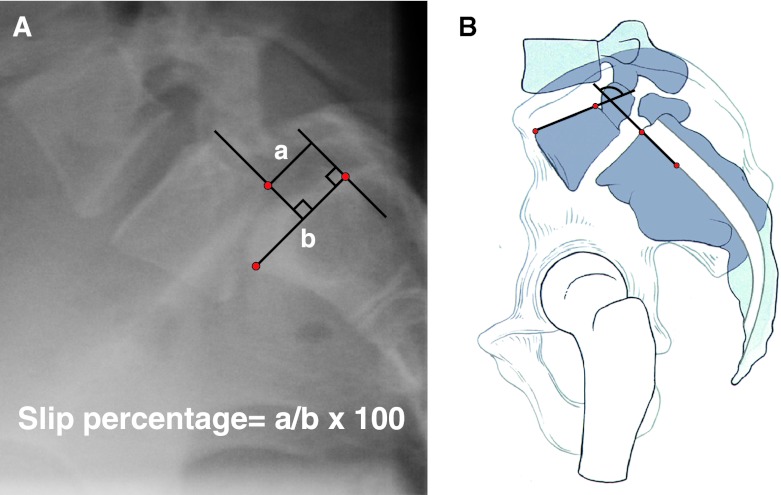
In addition to descriptive statistics, SRS-22 total score and individual domains, ST and C7P deviation, as well as pelvic parameters and regional sagittal curves were compared between low- and high-grade subjects using bilateral Student’s t tests. Pearson correlation coefficients were calculated between each parameter of global sagittal alignment and the SRS-22 domains and total score for all patients, and after subgrouping patients based on slip percentage (low-grade vs. high-grade). The same correlation analysis was repeated only with the 29 high-grade patients with a C7P in front of the posterior corner of the upper sacral endplate (positive alignment subgroup). Correlations were also calculated between global sagittal alignment (ST and C7P deviation) and local lumbosacral deformity (slip percentage and LSK) for high-grade patients only. Slip percentage and LSK were measured following the techniques described in Fig. 2.
Fig. 2.
Measurement of slip percentage (a) and lumbosacral kyphosis (b)
For the positive alignment subgroup, multiple linear regression analyses were performed with the SRS-22 total score and the pain domain score as dependent variables, and the C7P deviation, slip percentage, and LSK as independent variables. The same analysis was repeated with ST, slip percentage, and LSK as independent variables.
The positive alignment subgroup was further divided based on the position of the C7P relative to the hip axis (HA, center of the line connecting the center of each femoral head). Mann–Whitney U tests were performed to assess the difference in SRS-22 total and individual domain scores, slip percentage, LSK, and pelvic and regional sagittal parameters between the 11 high-grade patients with a C7P falling in front of HA and the 18 high-grade patients with a C7P falling behind the HA.
Statistical analysis was performed with SPSS Statistics 18 (SPSS Inc., Chicago, IL, USA) using a level of significance of 0.05.
Results
Means and standard deviations for calculated parameters of global sagittal alignment, SRS-22 domains and total score, pelvic parameters, and regional sagittal curves are presented in Table 1 for all patients and after grouping patients based on slip percentage (low-grade vs. high-grade). Compared to low-grade subjects, high-grade subjects had a significantly lower SRS-22 total score (p < 10−3), pain (p < 10−4), appearance (p < 10−3), and activity domains (p < 10−4). The mental health domain was similar between low-grade and high-grade subjects. Patients with high-grade spondylolisthesis had a significantly smaller ST (p < 10−6) and larger C7P deviation (p < 10−5), showing a tendency for a more forward position of C7P in these patients. High-grade patients also showed significantly smaller TK (p < 10−5), LL (p < 10−4) as well as increased PI (p < 10−5) and PT (p < 10−6). SS was not different between high-grade and low-grade spondylolisthesis.
Table 1.
Mean ± standard deviations for SRS-22 scores and parameters of global sagittal alignment
| Parameters | All patients | Subgrouping by slip percentage | ||
|---|---|---|---|---|
| Low-grade (n = 117) | High-grade (n = 32) | p | ||
| SRS-22 total score | 3.84 ± 0.54 | 3.92 ± 0.52 | 3.52 ± 0.48 | <10−3* |
| Pain domain | 3.76 ± 0.86 | 3.92 ± 0.81 | 3.21 ± 0.83 | <10−4* |
| Appearance domain | 3.79 ± 0.64 | 3.89 ± 0.60 | 3.42 ± 0.66 | <10−3* |
| Activity domain | 4.02 ± 0.65 | 4.14 ± 0.60 | 3.59 ± 0.65 | <10−4* |
| Mental health domain | 3.95 ± 0.71 | 3.96 ± 0.72 | 3.91 ± 0.68 | 0.714 |
| ST (°) | 88.6 ± 4.4 | 89.5 ± 3.5 | 85.2 ± 5.6 | <10−6* |
| C7P (mm) | 22.1 ± 35.3 | 15.2 ± 28.3 | 50.5 ± 42.4 | <10−5* |
| Thoracic kyphosis (°) | 36.4 ± 12.0 | 38.8 ± 10.5 | 27.7 ± 13.1 | <10−5* |
| Lumbar lordosis (°) | 60.9 ± 14.8 | 63.6 ± 13.1 | 51.1 ± 16.6 | <10−4* |
| Pelvic incidence (°) | 63.6 ± 13.7 | 61.0 ± 12.9 | 73.0 ± 12.8 | <10−5* |
| Pelvic tilt (°) | 10.9 ± 14.5 | 6.4 ± 12.3 | 27.4 ± 9.0 | <10−6* |
| Sacral slope (°) | 49.2 ± 10.9 | 50.0 ± 10.8 | 46.2 ± 10.8 | 0.078 |
ST spinal tilt, C7P C7 plumbline deviation
* Level of significance: p < 0.05
Values in ST ranged from 79° to 102° in low-grade patients, and the range in ST was shifted forward for patients with high-grade slippage (68°−96°). The range in C7P deviation is also shifted forward in high-grade subjects (–15.2−203.2 mm) compared to low-grade subjects (–73.6−94.1 mm). As for the SRS-22 total score, it ranged from 2.50 to 4.90 for low-grade subjects and from 2.40 to 4.40 for high-grade subjects.
The correlation analysis showed a small but statistically significant correlation between global sagittal alignment parameters and SRS-22 total score (ST: p = 0.01, C7P: p = 0.02) for all patients (Table 2). This correlation remained significant when considering the individual scores for the appearance (ST: r = 0.27, p = 0.001; C7P: –0.28, p = 0.001) and activity (ST: r = 0.226, p = 0.006; C7P: r = –0.209, p = 0.011) domains, but not the pain and mental health domains. For low-grade patients only, these correlations did not reach statistical significance.
Table 2.
Correlation study between parameters of global sagittal alignment and SRS-22 total score
| Parameters | All patients | Low-grade | High-grade | |||||
|---|---|---|---|---|---|---|---|---|
| All (n = 32) | Positive sagittal alignment subgroup (n = 29) | |||||||
| r | p value | r | p value | r | p value | r | p value | |
| ST (°) | 0.21 | 0.01* | 0.001 | 0.99 | 0.35 | 0.047* | 0.48 | 0.008* |
| C7P (mm) | –0.19 | 0.02* | 0.024 | 0.80 | –0.35 | 0.050 | −0.48 | 0.008* |
Positive sagittal alignment subgroup: C7P falling in front of the posterior corner of upper sacral endplate
ST spinal tilt, C7P C7 plumbline deviation
* Level of significance: p < 0.05
For high-grade patients, ST (r = 0.35; p = 0.047) was significantly related to SRS-22 total score, while the relationship between SRS-22 total score and C7P deviation almost reached statistical significance (r = –0.35; p = 0.050). When considering the individual domain scores, only the appearance domain correlated significantly with the global sagittal alignment parameters (ST: r = 0.52, p = 0.002; C7P: r = –0.48, p = 0.005) (Table 3). When high-grade patients from the positive alignment subgroup were considered separately, the correlations were strengthened between SRS-22 total score and both ST (r = 0.48; p = 0.008) and C7P deviation (r = –0.48; p = 0.008). In this subgroup, the global sagittal alignment parameters were also correlated to the pain (ST: p = 0.37, p = 0.047; C7P: r = –0.45, p = 0.013) and appearance (ST: r = 0.62, p = 0.0003; C7P: r = –0.58, p = 0.001) individual domain scores (Table 3). In addition for high-grade patients, correlation analysis showed that neither ST nor C7P deviation was significantly related to LSK or slip percentage in high-grade patients (Table 4).
Table 3.
Correlations between parameters of global sagittal alignment and the different domains and total score of the SRS-22 questionnaire in high-grade spondylolisthesis and in the positive sagittal alignment subgroup
| All high-grade (n = 32) | Positive sagittal alignment subgroup (n = 29) | |||||||
|---|---|---|---|---|---|---|---|---|
| ST | C7P | ST | C7P | |||||
| r | p value | r | p value | r | p value | r | p value | |
| Pain | 0.23 | 0.215 | –0.29 | 0.109 | 0.371 | 0.047* | –0.454 | 0.013* |
| Appearance | 0.52 | 0.002* | –0.48 | 0.005* | 0.621 | 0.0003* | –0.577 | 0.001* |
| Activity | 0.32 | 0.069 | –0.34 | 0.058 | 0.337 | 0.074 | –0.355 | 0.059 |
| Mental health | 0.07 | 0.707 | –0.05 | 0.777 | 0.093 | 0.631 | –0.082 | 0.672 |
| Total | 0.35 | 0.047* | –0.35 | 0.050 | 0.481 | 0.008* | –0.482 | 0.008* |
Positive sagittal alignment subgroup: C7P falling in front of the posterior corner of upper sacral endplate
ST Spinal Tilt, C7P C7 plumbline deviation
* Level of significance: p < 0.05
Table 4.
Correlations between parameters of global sagittal alignment, slip percentage and LSK in high-grade spondylolisthesis
| Slip percentage | LSK | |||
|---|---|---|---|---|
| r | p value | r | p value | |
| C7P (mm) | 0.23 | 0.21 | –0.27 | 0.14 |
| ST (°) | –0.19 | 0.29 | 0.26 | 0.16 |
LSK lumbosacral kyphosis; C7P C7 plumbline; ST spinal tilt
* Level of significance: p < 0.05
In the positive alignment subgroup, multiple regression analysis showed that the C7P deviation (p = 0.005) and slip percentage (p = 0.008) were independently related to the SRS-22 score, while LSK was not statistically significant (p = 0.26). The overall correlation coefficient with the SRS-22 total score was r = 0.65. Similar results were obtained when the C7P deviation was replaced by ST in the regression analysis, with an overall correlation coefficient of r = 0.66 (p = 0.004 for ST; p = 0.006 for slip percentage; p = 0.23 for LSK). The regression analysis showed similar results with the SRS-22 pain domain as the dependent variable. In a model with C7P, slip percentage, and LSK as independent variables, only C7P was significant (p = 0.012) with an overall correlation coefficient of r = 0.54. After replacing C7P with ST in the model, the overall correlation coefficient was r = 0.49 and the global sagittal parameter was still the only significant variable (p = 0.031).
Mann–Whitney U test showed that high-grade patients with a C7P in front of the HA had a significantly lower SRS-22 total score (p = 0.024) as well as pain (p = 0.016) and appearance (p = 0.0005) domains than those with a C7P behind the HA (Table 5). Patients with a C7P in front of the HA also had a significantly lower LL (p = 0.009). The other regional sagittal curves and pelvic parameters, including slip percentage and LSK, were similar. Age distribution was not significantly different between both groups (p = 0.06).
Table 5.
Comparison of SRS-22 total score, slip percentage, and LSK in high-grade subjects with positive sagittal alignment based on the position of C7P relative to HA
| Parameters | C7P behind HA (n = 18) | C7P in front of HA (n = 11) | p |
|---|---|---|---|
| Slip percentage (%) | 77.64 ± 17.2 | 79.89 ± 15.3 | 0.620 |
| LSK (°) | 74.21 ± 14.8 | 73.04 ± 20.2 | 0.653 |
| SRS-22 total score | 3.69 ± 0.43 | 3.22 ± 0.38 | 0.024* |
| Pain domain | 3.51 ± 0.84 | 2.8 ± 0.63 | 0.016* |
| Appearance domain | 3.70 ± 5.79 | 2.93 ± 0.40 | 0.0005* |
| Activity domain | 3.67 ± 0.51 | 3.38 ± 0.76 | 0.256 |
| Mental health domain | 4.03 ± 0.68 | 3.67 ± 0.65 | 0.134 |
| Thoracic kyphosis (°) | 29.9 ± 11.6 | 21.7 ± 14.7 | 0.188 |
| Lumbar lordosis (°) | 56.5 ± 14.9 | 39.9 ± 16.3 | 0.009* |
| Pelvic incidence (°) | 75.7 ± 13.8 | 72.5 ± 10.0 | 0.465 |
| Pelvic tilt (°) | 27.7 ± 6.7 | 29.9 ± 10.5 | 0.74 |
| Sacral slope (°) | 48.4 ± 13.6 | 42.5 ± 5.1 | 0.084 |
Positive sagittal alignment: C7P in front of the posterior corner of the upper sacral endplate
LSK lumbosacral kyphosis; HA hip axis
* Level of significance: p < 0.05
Discussion
This study is the first that attempts to assess the clinical relevance of evaluating global sagittal alignment with respect to HRQOL in pediatric lumbosacral spondylolisthesis. Overall, the study showed a significant relation between global sagittal alignment and HRQOL for children and adolescents with lumbosacral spondylolisthesis. These results are in agreement with those previously reported by Berven et al. [5] for adult spondylolisthesis, as well as those observed by Glassman et al. [2, 3] and Mac-Thiong et al. [4] in adult spinal deformity.
Patients with a high-grade slip were found to have a significantly higher SRS-22 score compared to patients with a low-grade slip, with an absolute difference of 0.4 in the total score, 0.71 in the pain domain, 0.47 in the appearance domain, 0.58 for the activity domain, and 0.05 for the mental health domain. To assess the clinical significance of these differences, we compared them to the minimum clinically important difference (MCID)—the threshold above which a change in a score is considered clinically meaningful—for the SRS-22 questionnaire [12]. The MCID were of 0.6 for the pain domain, 0.5 for the appearance domain, 0.8 for the activity domain, 0.4 for the mental health domain, and varied between 0.4 and 0.6 for the total score. Thus, the differences between patients with low-grade and high-grade slips in the SRS-22 pain domain and total score reported in our study are comparable to the reported MCID, and therefore are probably significant clinically. However, the interpretation is limited by the fact that these values were measured based on a population of patients operated for idiopathic scoliosis, which differ from our population of unoperated spondylolisthetic patients. The comparison between patients with high-grade and low-grade spondylolisthesis also revealed differences in the regional sagittal curves and pelvic parameters in accordance with previous findings [8].
The present study suggests a smaller impact of global sagittal alignment in low-grade spondylolisthesis since it was not related to the SRS-22 total score or its individual domains. Accordingly in the SDSG classification of lumbosacral spondylolisthesis [9], global sagittal alignment is not taken into account for low-grade slips. Global sagittal alignment is less likely to have an impact on HRQOL in low-grade spondylolisthesis possibly due to the following reasons: (1) the great majority of patients with low-grade slips have normal C7P deviation and ST, (2) the great majority of patients with low-grade slips have a normal HRQOL, and (3) global sagittal alignment is less variable in low-grade than high-grade spondylolisthesis. Furthermore, low-grade patients tend to have an overall sagittal spinal alignment similar to that of asymptomatic subjects, as previously described by Mac-Thiong et al. [8], so its impact on HRQOL is likely to be negligible in low-grade spondylolisthesis.
For high-grade patients, it is possible that the lumbosacral deformity is so severe in some cases that compensation mechanisms from remaining spinal segments, pelvis and/or hips become ineffective and fail to maintain an acceptable global sagittal alignment. Evaluating global sagittal alignment was indeed particularly relevant for high-grade patients in this study, where a moderate correlation was found between parameters of global sagittal alignment and SRS-22 total score. This correlation associated increasing forward global sagittal alignment with lower SRS-22 scores. The relationship between HRQOL and global sagittal alignment was further reinforced in high-grade patients with a C7P in front of the posterior corner of the upper sacral endplate (Table 2). In this positive sagittal alignment subgroup, a large correlation was found between parameters of global sagittal alignment and SRS-22 total score, as well as the pain and appearance domains. The correlation with the pain domain is particularly relevant, as back pain is the major complaint of patients with spondylolisthesis. This finding suggests that in high-grade spondylolisthesis, clinicians need to be particularly concerned with global sagittal alignment when C7P is in front of the posterior corner of the upper sacral endplate as for these patients an increase in positive sagittal alignment is associated with increased pain and a generally lower HRQOL.
The SDSG classification of lumbosacral spondylolisthesis [9] uses the position of the C7P relative to the femoral heads as an important aspect to consider when treating patients with high-grade spondylolisthesis. However, this decision has never been evaluated in previous studies. The current study supports this concept since among high-grade patients with positive sagittal alignment, those with a C7P in front of the HA have a lower SRS-22 total score, pain and appearance domains than those with a C7P behind the HA, without significant difference in slip percentage or LSK between the two subgroups.
As the slip percentage and LSK progress and result in an increasingly positive sagittal alignment, the spine and pelvis seem to compensate though three main mechanisms: (1) increased LL (2) decreased TK, and (3) retroversion of the pelvis (or verticalization of sacrum). All these modifications are aimed at bringing back the C7 vertebrae behind the femoral heads to restore a normal global sagittal alignment. Failure of these compensatory mechanisms in patients with spondylolisthesis results in an abnormally positive sagittal alignment. In our study, we found that patients with a C7P in front of HA have a significantly lower LL compared to those with a C7P behind HA. Therefore, patients who have a C7P in front of HA failed to increase their LL sufficiently, resulting in a more positive sagittal alignment. As these patients reach their limit in terms of LL, they probably try to compensate their positive sagittal alignment relying on the two other mechanisms, as shown by the trend towards a lower TK and increased pelvic retroversion (higher PT and lower SS) in the patients with a C7P in front of HA. Our study does not allow us to understand why some patients were able to increase their LL sufficiently and limit the forward displacement of their C7P while others were unable to reach that level of compensation. This difference is probably due to individual variability in the skeletal and muscular components involved.
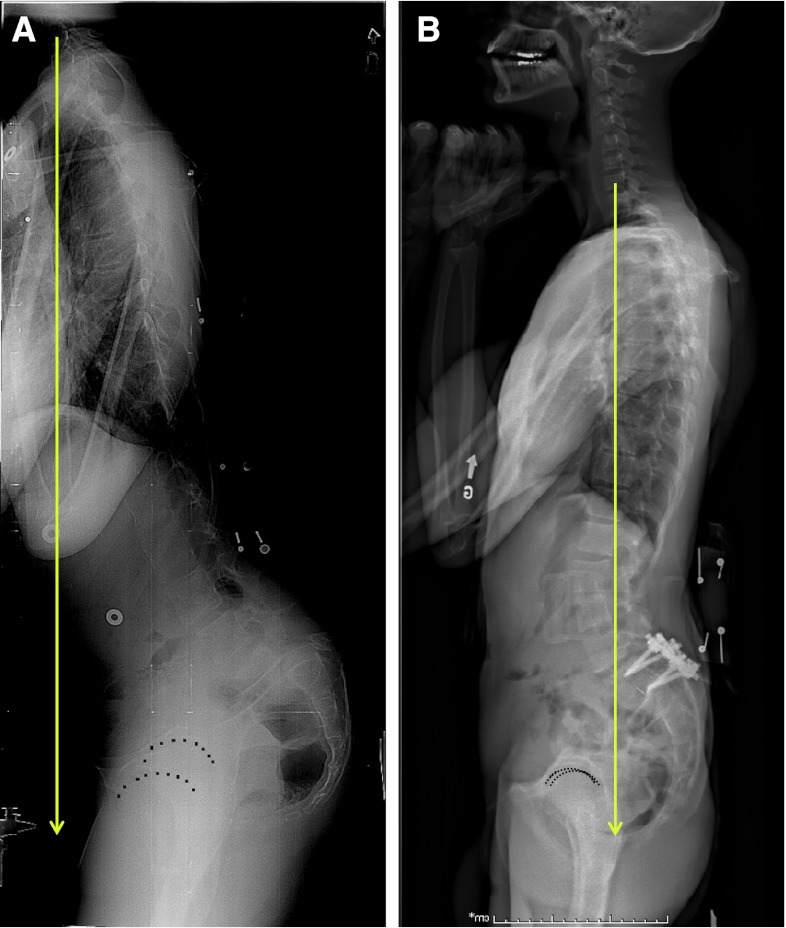
Our results show that restoration of a normal global sagittal alignment for patients with a C7P in front of the HA by formal reduction of the spondylolisthesis during surgery is appealing, in an attempt to improve the HRQOL. Indeed, a normal sagittal global alignment is generally restored after surgical reduction of slip and particularly LSK in patients with high-grade spondylolisthesis presenting with a C7P in front of the hip axis preoperatively (Fig. 3).
Fig. 3.
Restoration of a normal global sagittal alignment after surgical reduction of the spondylolisthesis in a 15-year-old patient. a Preoperative radiograph with C7 plumbline in front of hip axis. b Postoperative radiograph 4 years after surgery with C7 plumbline behind hip axis
Slip percentage [13] and LSK [14] have both been shown to have a clinical impact on HRQOL in lumbosacral spondylolisthesis. These parameters were considered as possible co-variables affecting the correlation between global sagittal alignment and HRQOL. However, C7P deviation and ST were not individually related to slip percentage or LSK in high-grade lumbosacral spondylolisthesis, suggesting that global sagittal alignment is independent from slip percentage and LSK in this group. Also, in the positive alignment subgroup, the relationship between global sagittal alignment parameters and both the SRS-22 pain domain and total score persisted even after accounting for slip percentage and LSK in multiple linear regression analyses. These findings suggest that global sagittal alignment is an independent factor affecting the HRQOL in high-grade spondylolisthesis, particularly for patients with a C7P in front of the posterior corner of the upper sacral endplate.
Doming of the sacrum is a key feature in spondylolisthesis and could potentially influence pelvic and global sagittal alignment measurements on lateral radiographs. However, a previous study by Vialle et al. [15] has demonstrated that when a computer-assisted technique is used, measurement of pelvic incidence in high-grade spondylolisthesis is associated with excellent reliability with intraclass correlation coefficients ranging from 0.986 to 0.992. As for the measurement of global spinal alignment, doming of the sacrum could potentially have influenced the measurement of ST that uses the upper sacral endplate as a landmark, but is not likely to have influence the measurement of C7 plumbline deviation. On the other hand, because it is an angular parameter, ST is less sensitive to variations in radiological protocols and magnification, allowing easier comparison between studies. It also has the advantage of taking into account the spinal height of each subject. Nevertheless, C7P deviation and ST were similar in their relationship with HRQOL and were both independent of LSK and slip percentage. Whether the use of other parameters of global sagittal alignment or HRQOL questionnaires would result in additional findings should be addressed in the future. In this study, we used the SRS-22 questionnaire to measure the HRQOL. While this questionnaire was originally designed for patients with adolescent idiopathic scoliosis, a previous study showed that the SRS-22 total score can discriminate between healthy controls and spondylolisthesis patients, and therefore indirectly reflects the influence of clinical symptoms on their quality of life [16]. We also included in our analyses the individual domain scores of the SRS-22 for a more accurate evaluation of HRQOL.
In addition, the limited number of patients with high-grade spondylolisthesis is a recognized limitation of this study, and further investigation is needed to better define the impact of global sagittal alignment in the management of high-grade spondylolisthesis. In particular, the relationship between global sagittal alignment and HRQOL after surgery should be addressed. Also, reduction of high-grade spondylolisthesis is associated with a higher risk of iatrogenic neurologic injury, most commonly L5 radiculopathy [17], but also with a risk of adjacent disease above the fused segment. These potentially serious complications must be weighed against the potential benefit of reducing the spondylolisthesis, although restoring a proper sagittal alignment must remain a main goal of the surgical treatment.
Conclusion
In conclusion, this study showed that the influence of global sagittal alignment on HRQOL is negligible in low-grade spondylolisthesis. For high-grade patients with a C7P in front of the posterior corner of the upper sacral endplate, and especially for those with a C7P in front of the femoral heads, an increasing positive global sagittal alignment is related to increased pain and a poorer HRQOL, independently of slip percentage and LSK. These findings support the need to take global sagittal alignment into account when evaluating and treating patients with high-grade spondylolisthesis. This study also supports the restoration of an adequate global sagittal alignment through formal reduction of the spondylolisthesis in the surgical management of high-grade patients, in an attempt to improve the HRQOL. Further investigation is however necessary to establish the exact clinical impact of global sagittal alignment on the HRQOL of high-grade patients, with a particular emphasis on the impact of surgery.
Acknowledgments
Conflict of interest
This study has been funded by the Fonds de Recherche Québec - Santé (FRQS) and by the Ressources humaines et développement des compétences Canada (RHDCC).
References
- 1.Angevine PD, McCormick PC. The importance of sagittal balance: how good is the evidence? J Neurosurg Spine. 2007;6:101–103. doi: 10.3171/spi.2007.6.2.101. [DOI] [PubMed] [Google Scholar]
- 2.Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine. 2005;30:2024–2029. doi: 10.1097/01.brs.0000179086.30449.96. [DOI] [PubMed] [Google Scholar]
- 3.Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine. 2005;30:682–688. doi: 10.1097/01.brs.0000155425.04536.f7. [DOI] [PubMed] [Google Scholar]
- 4.Mac-Thiong JM, Transfeldt EE, Mehbod AA, Perra JH, Denis F, Garvey TA, Lonstein JE, Wu C, Dorman CW, Winter RB. Can c7 plumbline and gravity line predict health related quality of life in adult scoliosis? Spine. 2009;34:E519–E527. doi: 10.1097/BRS.0b013e3181a9c7ad. [DOI] [PubMed] [Google Scholar]
- 5.Berven S LH, Deriven V, O’Brien MF, Roussouly P (2007) Spondylolisthesis and lumbopelvic parameters: defining the relationship between radiographic measurements and health-related quality of life (HRQL). Presented at the 42nd International Meeting of the Scoliosis Research Society, Edinburgh, 5–8 September 2007
- 6.Jackson RP, Phipps T, Hales C, Surber J. Pelvic lordosis and alignment in spondylolisthesis. Spine. 2003;28:151–160. doi: 10.1097/00007632-200301150-00011. [DOI] [PubMed] [Google Scholar]
- 7.Rajnics P, Templier A, Skalli W, Lavaste F, Illes T. The association of sagittal spinal and pelvic parameters in asymptomatic persons and patients with isthmic spondylolisthesis. J Spinal Disord Techniques. 2002;15:24–30. doi: 10.1097/00024720-200202000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Mac-Thiong JM, Wang Z, de Guise JA, Labelle H. Postural model of sagittal spino-pelvic alignment and its relevance for lumbosacral developmental spondylolisthesis. Spine. 2008;33:2316–2325. doi: 10.1097/BRS.0b013e318186b236. [DOI] [PubMed] [Google Scholar]
- 9.Labelle H, Mac-Thiong JM, Roussouly P. Spino-pelvic sagittal balance of spondylolisthesis: a review and classification. Eur Spine J. 2011;20(Suppl 5):641–646. doi: 10.1007/s00586-011-1932-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Horton WC, Brown CW, Bridwell KH, Glassman SD, Suk SI, Cha CW. Is there an optimal patient stance for obtaining a lateral 36″ radiograph? A critical comparison of three techniques. Spine. 2005;30:427–433. doi: 10.1097/01.brs.0000153698.94091.f8. [DOI] [PubMed] [Google Scholar]
- 11.Roussouly P, Gollogly S, Noseda O, Berthonnaud E, Dimnet J. The vertical projection of the sum of the ground reactive forces of a standing patient is not the same as the C7 plumb line: a radiographic study of the sagittal alignment of 153 asymptomatic volunteers. Spine. 2006;31:E320–E325. doi: 10.1097/01.brs.0000218263.58642.ff. [DOI] [PubMed] [Google Scholar]
- 12.Bago J, Perez-Grueso FJ, Les E, Hernandez P, Pellise F. Minimal important differences of the SRS-22 Patient Questionnaire following surgical treatment of idiopathic scoliosis. Eur Spine J. 2009;18:1898–1904. doi: 10.1007/s00586-009-1066-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Labelle H RP, Mac-Thiong J-M, et al. 2010 Relationship between HRQL measures and spino-pelvic alignment in adolescent spondylolisthesis compared to a control population. Presented at the Scoliosis Research Society 45th annual meeting and combined course, Kyoto, 21–24 September 2010
- 14.Tanguay F, Labelle H, Wang Z, Joncas J, de Guise JA, Mac-Thiong JM. Clinical significance of lumbosacral kyphosis in adolescent spondylolisthesis. Spine. 2012;37:304–308. doi: 10.1097/BRS.0b013e31821cc558. [DOI] [PubMed] [Google Scholar]
- 15.Vialle R, Ilharreborde B, Dauzac C, Guigui P. Intra and inter-observer reliability of determining degree of pelvic incidence in high-grade spondylolisthesis using a computer assisted method. Eur Spine J. 2006;15:1449–1453. doi: 10.1007/s00586-006-0096-x. [DOI] [PubMed] [Google Scholar]
- 16.Parent S, Joncas J, Roy-Beaudry M, Beausejour M, Grimard G, Forcier M, Labelle H, (2008) The SRS Outcome Questionnaire can discriminate between patients with spondylolisthesis and normal healthy adolescents. 15th International meeting on advanced spine techniques, Hong Kong, 8–11 July 2008
- 17.Cheung EV, Herman MJ, Cavalier R, Pizzutillo PD. Spondylolysis and spondylolisthesis in children and adolescents: II. Surg Manag JAAOS. 2006;14:488–498. doi: 10.5435/00124635-200608000-00006. [DOI] [PubMed] [Google Scholar]