Abstract
Purpose
Fusion of the sacroiliac joints (SIJ) has been a treatment option for patients with severe pelvic girdle pain (PGP). The primary aims were to evaluate the long-term outcomes in patients who underwent SIJ fusion and to compare 1-year outcomes with long-term outcomes. The secondary aim was to compare patients who underwent SIJ fusion with a comparable group who did not.
Methods
This study includes fifty patients that underwent SIJ fusion between 1977 and 1998. Function (the Oswestry disability index; ODI), pain intensity (visual analogue scale; VAS) and health-related quality of life (SF-36) were determined according to a patient-reported questionnaire. The questionnaire scores were compared with previously recorded 1-year outcomes and with questionnaire scores from a group of 28 patients who did not undergo SIJ fusion.
Results
The patients who underwent SIJ fusion reported a mean ODI of 33 (95 % CI 24–42) and a mean VAS score of 54 (95 % CI 46–63) 23 years (range 19–34) after surgery. Regarding quality of life, the patients reported reduced physical function, but mental health was not affected in the same manner. The patients with successful 1-year outcomes (48 %) retained significantly improved function and reduced pain levels compared with the subgroup of patients with unsuccessful 1-year outcomes (28 %). The patients who underwent surgery did not differ from the non-surgery group in any outcome at the long-term follow-up.
Conclusions
Patients treated with SIJ fusion had moderate disability and pain 23 years after surgery, and the 1-year outcomes were sustained 23 years after surgery. Although many fused patients reported good outcome, this group did not differ from the comparable non-surgical group.
Keywords: Sacroiliac joint, Pelvic girdle pain, Long-term follow-up, Fusion, Arthrodesis
Introduction
The sacroiliac joint (SIJ) is a source of pain for 13–30 % of patients with lower back pain [17] and can become painful following inflammatory diseases, metabolic disorders, post-traumatic arthritis, malalignment and infections [2]. The origin and diagnosis of pelvic girdle pain (PGP) are controversial when radiological findings are absent and objective diagnostic tests lack proper evidence. The cause of PGP is unclear, but it may be a biomechanical disorder in which SIJ hypermobility causes pain [5]. The theory of abnormal joint mobility is one reason some orthopaedic surgeons have fused pelvic joints to reduce PGP [7]. There is, however, no evidence of a correlation between sacroiliac instability and symptoms [14, 15, 19], whereas a correlation between asymmetrical movement in the SIJ and symptom intensity has been described [4].
Conservative treatment is the first choice for patients with PGP and has proven efficient [13]. Despite appropriate conservative treatments, some patients remain severely disabled by persistent pain; therefore, pelvic joint fusion has been performed on those patients. Pelvic joint fusions have been reported in a number of studies, but there has been no consistency in the inclusion criteria used [1, 3, 10, 16, 18]. The results of pelvic joint fusions are mostly reported in small case series, with the exception of one report that included 58 patients [16]. The reported short-term results have been mainly positive [1, 3, 16, 18], but poor results have also been reported [10]. To our knowledge, the longest follow-up reported in the literature is 5.8 years [3].
The main aims of this study were to evaluate long-term functioning, pain and health-related quality of life in patients who had previously undergone pelvic joint fusion surgery and to compare the 1-year outcomes with the long-term results. The secondary aim was to compare patients with PGP, who underwent surgery with a comparable group of patients who did not undergo surgery.
Materials and methods
Design and subjects
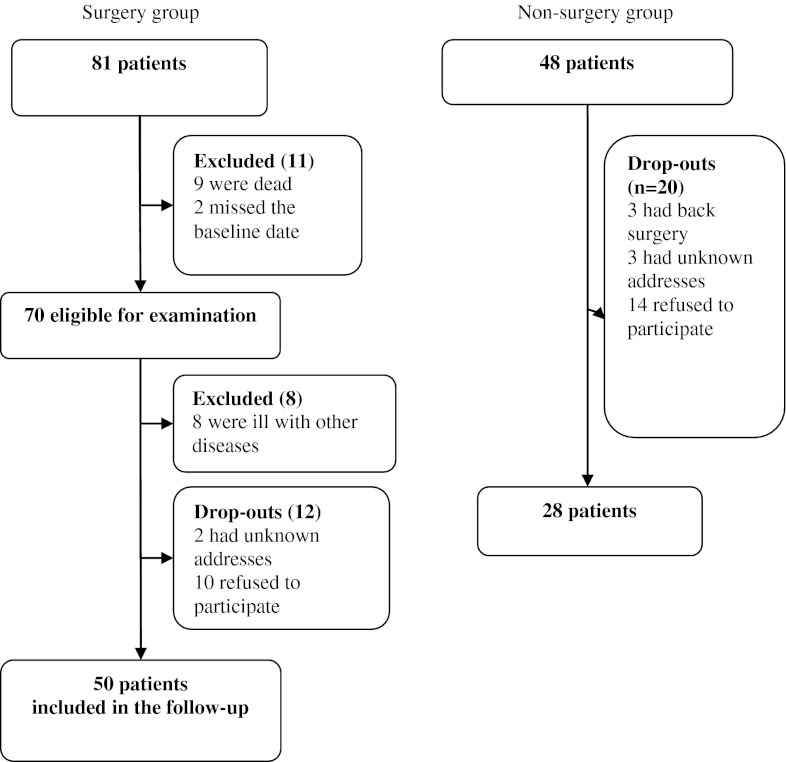
This cross-sectional study included patients with SIJ pain that had been operated at the Hagavik Orthopaedic Hospital between 1977 and 1998 (Fig. 1). During 2009 the patients received a questionnaire including self-report of pain and function. The material consists of data from 50 subjects 1 year after SIJ fusion and long-term follow-up. The regional committee of ethics approved the study (project number: 1.2006.1574).
Fig. 1.
Flow chart of the study population
Indications for surgery
The patients were selected and operated on primarily by one of the authors (E.Sudmann). The criteria for surgery were based on patient history and radiological and clinical examinations. Inclusion criteria were pain in the SIJ > 1 year after pregnancy or after trauma, pain with an idiopathic origin, severe disability and resistance to conservative treatment. The clinical tests performed included tenderness at the superior and inferior posterior iliac spines, active and passive straight leg raise, Patrick Fabere’s test, passive hip rotation, forcible inward rotation and extension of the hip joint. Further tests included normal neurological and gynaecological examinations, normal spinal X-rays, symphysis movement of less than 3 mm on plain radiographs during a one-leg stance, normal radiculography, negative rheumatology tests, and negative blood tests. Before the surgery only 5 (10 %) patients had the ability to work and 23 (46 %) had to use some kind of walking aids.
Surgical technique and post-operative management
The patients were operated on using a dorsal approach, with either a trans-iliac fusion or an intra/extra-articular fusion between the ilium and the sacrum. When the trans-iliac fusion was performed, an iliac window was constructed to access the joint [12]. The joint surface was cleared of cartilage and decorticated. The cortical iliac window was used as a graft and was usually hammered into the sacrum to promote intra-articular bone formation and conduction. Additional cancellous bone was impacted around the cortical graft. In a dorsal intra/extra-articular fusion, iliac crest autografts were added after joint removal and bone decortications [18]. The pubic symphysis was fused in four patients using an open technique with an iliac crest block bone autograft and plating. In some patients a Hoffman frame was tried to achieve post-operative fixation, but in most cases the patients were confined to bedrest, usually for 6 weeks.
One-year outcomes and the classification of subgroups
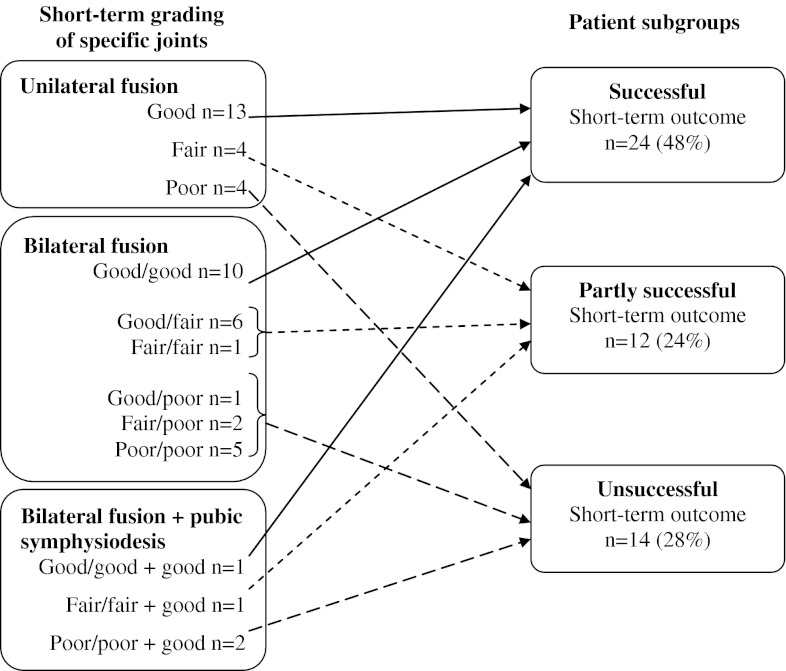
The patients were examined with CT after 1 year, and the clinical outcome was graded according to the following criteria: a joint with negative SIJ tests and no or minor pain that did not interfere with the patients’ work was graded “good”. A joint with obvious improvement in comparison to the pre-operative status and little pain, but pain that interfered with work (professional or at home) was graded “fair”. A joint was graded “poor” if there was no relief from pain or if the joint deteriorated after surgery. In cases of bilateral surgery, each of the patient’s joints could receive a different grade. According to the grading of the joints 1 year after surgery, the patients were allocated to three different subgroups (Fig. 2). Twenty-four patients (48 %) had all joints classified as “good” and were assigned to the subgroup “successful”. Fourteen patients (28 %) had at least one joint classified as “poor” and were assigned to the subgroup “unsuccessful”. Twelve patients (24 %) had their worse joint scored as “fair” and represented the subgroup “partly successful”. These three subgroups became the baseline for comparing the long-term effects. The patients’ 1-year outcomes were consecutively and systematically registered in a DOS Advanced relational database.
Fig. 2.
Each joint was graded after 1 year as good, fair or poor. For comparison purposes, three different subgroups were created based on this 1-year grading
Outcome measures
All patients from the database were contacted and asked to complete and return a questionnaire. The questionnaire included validated measures for function (the Oswestry disability index) [6], pain intensity at worst, morning and evening was measured by 100 mm visual analogue scale (VAS; 0=no pain, 100=worst possible pain) and health-related quality of life (SF-36) [20]. The Oswestry disability index (ODI) is a 10-item questionnaire that assesses patient function (0 indicates the best, 100 indicates the worst). A 10-point difference represents a significant clinical change [6, 8]. The SF-36 questionnaire contains 36 items representing 8 subscales: physical functioning, role physical, bodily pain, general health, vitality, social functioning, role emotional and mental health. Additionally, if the patients experienced any effect from the operation, they graded the effect as excellent, good, some or minor.
Non-surgery group
On the basis of their experiences with surgery failures, surgeons became increasingly reluctant to perform SIJ fusion. As a result, surgery was declined for a number of patients in the 1990s. These 28 patients constitute the non-surgery group. According to the patient charts 5 (17 %) patients had the ability to work at the time they were diagnosed and 17 (61 %) had to use some sort of walking aid. There were no differences in working ability (p = 0.32) and the use of walking aids (p = 0.21) between the surgical group and the non-surgical group at the time they were diagnosed. Beside these parameters, no other measurements of physical function or pain were available at that time.
Statistical analyses
The means were adjusted for BMI, age and time of follow-up (least square mean) and are presented with a 95 % confidence interval. The differences in the mean ODI, VAS and SF-36 scores between the three subgroups and between the patients who underwent surgery and those who did not were tested using analysis of covariance, adjusting for BMI, age and time of follow-up. Pair wise comparisons were performed using t tests with Bonferroni’s adjustment. The correlations between the 1-year outcome and ODI/VAS were expressed by Spearman’s ρ. A p value of 0.05 was regarded as significant. Statistical analyses were performed using SPSS Version 18.
Results
Demographics and patient characteristics
Eighty-one consecutive patients were selected for this study. Nine of the 81 patients were dead at inclusion, and two patients were excluded because of insufficient baseline data. Of the remaining 70 patients, 50 (71 %) responded to the questionnaire. Among the 20 non-responders, 8 did not answer because of serious illness, 10 refused to participate and 2 had an unknown address (Fig. 1). The patient demographics at the long-term follow-up are presented in Table 1. The non-responders and the excluded patients did not differ from the included patients with regards to age, follow-up or short-term outcomes.
Table 1.
Characteristics of the participants in the long-term follow-up study
| Surgery group (n = 50) | Non-surgery group (n = 28) | p value | |
|---|---|---|---|
| Age (years) | 58 (56–61) | 52 (49–55) | 0.003 |
| Follow-up (years) | 23 (22–24) | 17 (16–18) | <0.001 |
| Education (years) | 12 (11–13) | 13 (12–15) | 0.08 |
| Male/female | 3/47 | 0/28 | |
| Body mass index (BMI) | 27 (26–28) | 25 (24–27) | 0.16 |
| Duration of SIJ pain (years) | 5 (range 1–21) | ||
| Aetiology | |||
| Pregnancy | 60 % | 68 % | 0.8* |
| Trauma | 16 % | 14 % | |
| Idiopathic | 24 % | 18 % | |
| Disability pension received at long-term follow-up | |||
| 0 % | 30 % | 28 % | 0.9* |
| 50–99 % | 16 % | 18 % | |
| 100 % | 54 % | 54 % | |
| Pain medication use at long-term follow-up | |||
| None | 28 % | 11 % | 0.3* |
| Seldom | 10 % | 18 % | |
| 1–6 days/week | 16 % | 21 % | |
| Daily | 46 % | 50 % | |
The means are presented with a 95 % confidence interval. Comparisons were performed with a two-sample t test
* Chi-squared test
Of the 50 patients, 21 patients had a unilateral SIJ fusion, 25 patients had a bilateral fusion and 4 patients received fusion of both the SIJ and the pubic symphysis. In total, 83 joints were surgically fused; only 7 joints had an inferior result that required a second operation, including 4 with a CT-verified pseudarthrosis. In total, there were eight joints (10 %) with a CT-verified pseudarthrosis. The patients with pseudarthrosis had a 29 % greater risk of a poor result compared with those with a solid fusion (8 %). Pseudarthrosis caused a 3.6-fold increased risk of chronic painful joints compared with a fused joint (p = 0.009). There were few complications: one patient developed icterus of unknown aetiology, one developed a pulmonary embolism and one contracted a pin tract infection after the use of a Hoffman frame. In addition, unrelated to the fusion surgery, one patient required surgery because of immediate post-operative acute appendicitis, and one required surgery for a small bowel obstruction.
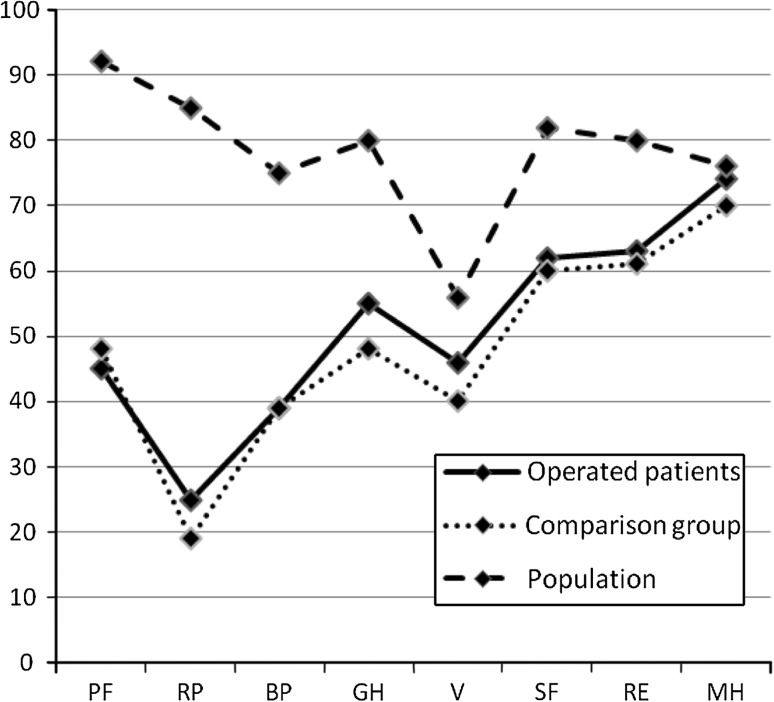
Long-term follow-up
The patients who underwent surgery had a mean ODI score of 33 (95 % CI 24–42; Table 2). Twenty-eight percent of the patients scored less than 20 on the ODI; 69 % had a score below 40. The patients had a mean evening VAS score of 54 (95 % CI 46–63; Table 2). Twenty percent of the patients had a VAS score under 20, and 53 % had a VAS score higher than 60. In the morning, 40 % of the patients had a VAS score below 40, and 30 % had a score higher than 60. The SF-36 score indicated that the patients had impaired physical health, as represented by the four subscales for physical functioning, role physical, bodily pain and general health (Fig. 3). Patient mental health was not affected in a similar manner, but the patients presented lower scores than a representative sample from the general Norwegian population [9] (Fig. 3).
Table 2.
Scores for ODI (0 indicates no disability, 100 indicates a high degree of disability), visual analogue scale (VAS) (0 indicates no pain, 100 indicates the worst pain) and SF-36 (0–100; 100 indicates the best health-related quality of life)
| Scores in the three subgroups with different short-term outcomes | |||||
|---|---|---|---|---|---|
| Patients with SIJ fusion (n=50) |
Successful (n=24) |
Partly successful (n=12) |
Unsuccessful (n=14) |
Non-surgery group (n=28) |
|
| Adjusted means (95 % CI) | |||||
| Oswestry disability index (ODI) |
33 (24–42) |
27 (20–34) |
37 (26–47) |
43 (34–53) |
37 (31–43) |
| Morning VAS score |
44 (31–57) |
38 (27–49) |
41 (24–57) |
62 (48–76) |
50 (41–59) |
| Evening VAS score |
54 (46–63) |
42 (31–53) |
60 (44–77) |
71 (56–85) |
60 (46–74) |
| SF-36 | |||||
| Physical functioning |
45 (36–54) |
56 (45–68) |
47 (30–63) |
32 (17–48) |
48 (34–62) |
| Role physical |
25 (12–37) |
27 (9–44) |
31 (5–56) |
18 (−6–41) |
19 (1–39) |
| Bodily pain |
39 (32–47) |
46 (36–55) |
42 (28–56) |
28 (15–41) |
39 (28–51) |
| General health |
55 (48–63) |
55 (46–64) |
53 (40–66) |
55 (43–67) |
48 (37–59) |
| Vitality |
46 (40–53) |
49 (41–57) |
51 (40–62) |
42 (31–52) |
36 (26–45) |
| Social functioning |
62 (54–71) |
65 (56–75) |
69 (56–83) |
53 (41–66) |
59 (47–72) |
| Role emotional |
63 (49–76) |
61 (44–79) |
66 (41–92) |
60 (37–83) |
61 (49–76) |
| Mental health |
73 (67–79) |
72 (64–80) |
76 (64–87) |
76 (66–87) |
71 (62–80) |
Means are presented as least-square means, as they were adjusted for BMI, age and time at follow-up, and are presented with a 95 % confidence interval
Fig. 3.
The SF-36 questionnaire includes 8 subscales (0 is worst, 100 is best). PF physical functioning, RP role physical, BP bodily pain, GH general health, V vitality, SF social functioning, RE role emotional and MH mental health. The patients who underwent surgery, the non-surgery comparison group and normative scores from the general Norwegian population are presented
The three subgroups of patients did not differ significantly in terms of age, follow-up, BMI or level of education (Table 3). The subgroup with a “successful” 1-year result (48 %) reported significantly lower scores on the ODI and VAS compared with the subgroup with an “unsuccessful” 1-year result (28 %; Table 2). The observed 16-point (95 % CI 1–32) difference in mean ODI was regarded as both clinically and statistically significant (p = 0.034; Table 2). The difference in VAS score was 24 (95 % CI 2–47) in the morning (p = 0.029) and 28 (95 % CI 6–51) in the evening (p = 0.011). There was a positive correlation between the 1-year outcome and three different long-term outcomes; VAS in the morning (ρ = 0.34, p = 0.0016), VAS in the evening (ρ = 0.42, p = 0.013) and ODI (ρ = 0.43, p = 0.002). For the SF-36 subscales, there were no significant differences between the subgroups, except for the physical functioning subscale, on which the subgroup with a “successful” short-term result had a 24-point higher score than the “unsuccessful” group (p = 0.040).
Table 3.
Demographic data and follow-up time for the patients who underwent SIJ fusion surgery
| Successful | Partly successful | Unsuccessful | |
|---|---|---|---|
| Number of patients | 24 | 12 | 14 |
| Age (years) | 60 (57–63) | 58 (52–64) | 55 (50–60) |
| Follow-up (years) | 24 (22–23) | 22 (20–23) | 23 (21–25) |
| Body mass index | 27 (25–29) | 29 (25–33) | 26 (24–28) |
| Education (years) | 13 (12–15) | 11 (10–13) | 11 (10–12) |
The three subgroups were defined by the patient’s worse joint, based on the 1-year outcomes
The means are presented with a 95 % confidence interval
At follow-up, 65 % of the patients reported that the surgery had a positive effect, and 74 % of these reported a good or excellent result. Eighteen percent of patients reported no effect, and the remaining patients were uncertain. Among the patients with a “successful” 1-year outcome, 80 % reported experiencing a good or excellent effect. Despite these results, 54 % of the patients who underwent surgery received a 100 % disability pension, and 46 % used some sort of pain medication daily (Table 1).
There were no significant differences in ODI (p = 0.54), morning VAS (p = 0.54), evening VAS scores (p = 0.50) or SF-36 scores between the group that underwent surgery and the non-surgery group at the long term-follow-up (Table 2). The non-surgery comparison group was in average 6 years younger (p = 0.003) and had a 6-year shorter follow-up time (p < 0.001) than the patients who underwent surgery. Aside from these differences, there were no significant differences between these two groups in terms of BMI, aetiology or education level (Table 1).
Discussion
The patients who underwent pelvic joint fusion reported having a moderate disability, with moderate to severe pain 23 years after surgery. They had impaired physical function, but their mental health was not reduced in a similar manner. The 1-year outcomes appeared to predict long-term outcomes with regard to pain and disability. The patients who underwent surgery did not differ from a non-matched comparison group of PGP patients who did not undergo surgery.
There are several strengths and limitations to this study. Its strengths include the long follow-up time and high response rate. To our knowledge, no other studies in the literature have a 23-year follow-up. Fifty out of 70 eligible patients were included, and the drop-outs did not differ significantly from the included patients. Moreover, most patients were selected and operated on by one surgeon, and the 1-year outcomes were consecutively and systematically registered. Another strength is the use of multiple clinical tests for inclusion [17] and validated questionnaires for the follow-up. However, a limitation is the subgroup classification; the sub-grouping may not be optimal, even though the joints were classified according to specific criteria. The non-surgery group differed from the surgery group with regard to age and time of follow-up, but was similar concerning working ability and the need for walking aids. Because pre-operative data on pain and disability are lacking we do not know whether the operated and the non-operated group were comparable. Because there are no RCTs or other studies with a control group found in the literature, the use of this comparison group might be justified.
The primary aim of this study was to evaluate long-term patient outcomes after SIJ fusion. The patients reported being moderately disabled, with 70 % of their scores below the limit of severe disability [6]. One-third of the patients reported no or minimal disability, with ODI scores below 20. Half of the patients had chronic pain and used pain medication daily. Their reported pain intensity was quite high and was worse in the evening. As many as 70 % of the patients received some sort of disability pension. Despite these moderate results, 65 % of the patients reported that surgery had a positive effect, mostly good or excellent. It is known that patients tend to report a high grade of satisfaction, even when the clinical outcome is moderate [11]. Because few studies have examined the long-term outcomes after surgery, comparison with other studies is difficult. The longest follow-up study that we found was 5.8 years [3]. That study reported a positive effect of surgery in terms of satisfaction and health-related quality of life, with SF-36 scores that were similar to those reported in our study.
Few studies used more than one post-operative measurement [10, 16]. Consequently, the long-term outcomes after SIJ fusion are difficult to predict. Interestingly, we found that the 1-year outcomes predicted the long-term outcomes, even 23 years after surgery. The subgroup of patients with successful 1-year outcomes reported significantly reduced disability and pain levels when compared with the subgroup with an unsuccessful outcome. van Zwienen et al. [16] reported that surgery had a positive effect on functional outcomes after 1 year, with further improvement after 2 years. Most of the patients in our study reported to be relieved (48 %) or almost relieved (24 %) from pain at the 1-year point, but 28 % were not; this outcome distribution was relatively constant. The 1-year outcomes of our study were similar to those of other studies [1, 16, 18] reporting a positive effect from surgery; however, a fraction of our patients reported that the surgery had no effect. The effect of SIJ fusion for patients with PGP, has however to be examined in future studies with proper designs.
Pelvic joint fusion is a controversial surgical procedure. The scientific evidence supporting the use of this surgery is weak, as only case series are available [17]. In our study, the patients who underwent surgery showed no differences in the outcome measurements when compared with the non-surgery patients. As surgery appears to have provided positive and long-lasting results in some patients, future research should address the question of who will benefit from this surgery. However, a poor understanding of the pathogenesis and aetiology of PGP persists, and there is no consensus on which clinical and radiological tests should be used to select patients for surgery. It is hoped that improved insights into the pathogenesis of PGP and improved diagnostic tools will allow the correct patients to be selected for surgery, resulting in improved outcomes.
Conclusions
Patients with chronic PGP who underwent SIJ fusion reported being moderately disabled, with moderate or severe pain intensity 23 years after surgery, and the 1-year outcomes were sustained 23 years after surgery. Two-thirds of the patients experienced a positive long-term effect from the fusion surgery, and 20 % reported no effect from the surgery. Although some patients report to have a successful long-term outcome, the group of patients who underwent SIJ fusion did not differ from the group of patients that were not operated, in regard of physical function, pain and HRQoL. These two groups of patients were not matched at baseline, hence further studies are needed to address the efficacy of surgery for patients with PGP.
Acknowledgments
We gratefully acknowledge the assistance of Ingar Holme for his help with statistics, Kaja Sætre (study coordinator) and Terje Sande with the DOS patient database. This study was supported by grants from the Norwegian Foundation for Health and Rehabilitation and Sophies Minde Ortopedi AS.
Conflict of interest
None.
References
- 1.Al-Khayer A, Hegarty J, Hahn D, Grevitt MP. Percutaneous sacroiliac joint arthrodesis: a novel technique. J Spinal Disord Tech. 2008;21:359–363. doi: 10.1097/BSD.0b013e318145ab96. [DOI] [PubMed] [Google Scholar]
- 2.Bellamy N, Park W, Rooney PJ. What do we know about the sacroiliac joint? Semin Arthritis Rheum. 1983;12:282–313. doi: 10.1016/0049-0172(83)90011-2. [DOI] [PubMed] [Google Scholar]
- 3.Buchowski JM, Kebaish KM, Sinkov V, Cohen DB, Sieber AN, Kostuik JP. Functional and radiographic outcome of sacroiliac arthrodesis for the disorders of the sacroiliac joint. Spine J. 2005;5:520–528. doi: 10.1016/j.spinee.2005.02.022. [DOI] [PubMed] [Google Scholar]
- 4.Damen L, Buyruk HM, Guler-Uysal F, Lotgering FK, Snijders CJ, Stam HJ. Pelvic pain during pregnancy is associated with asymmetric laxity of the sacroiliac joints. Acta Obstet Gynecol Scand. 2001;80:1019–1024. doi: 10.1034/j.1600-0412.2001.801109.x. [DOI] [PubMed] [Google Scholar]
- 5.Dreyfuss P, Michaelsen M, Pauza K, McLarty J, Bogduk N. The value of medical history and physical examination in diagnosing sacroiliac joint pain. Spine (Phila Pa 1976) 1996;21:2594–2602. doi: 10.1097/00007632-199611150-00009. [DOI] [PubMed] [Google Scholar]
- 6.Fairbank JC, Pynsent PB. The oswestry disability index. Spine (Phila Pa 1976) 2000;25:2940–2952. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 7.Hagen R. Pelvic girdle relaxation from an orthopaedic point of view. Acta Orthop Scand. 1974;45:550–563. doi: 10.3109/17453677408989178. [DOI] [PubMed] [Google Scholar]
- 8.Hagg O, Fritzell P, Nordwall A. The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J. 2003;12:12–20. doi: 10.1007/s00586-002-0464-0. [DOI] [PubMed] [Google Scholar]
- 9.Loge JH, Kaasa S. Short form 36 (SF-36) health survey: normative data from the general Norwegian population. Scand J Soc Med. 1998;26:250–258. [PubMed] [Google Scholar]
- 10.Schutz U, Grob D. Poor outcome following bilateral sacroiliac joint fusion for degenerative sacroiliac joint syndrome. Acta Orthop Belg. 2006;72:296–308. [PubMed] [Google Scholar]
- 11.Sitzia J. How valid and reliable are patient satisfaction data? An analysis of 195 studies. Int J Qual Health Care. 1999;11:319–328. doi: 10.1093/intqhc/11.4.319. [DOI] [PubMed] [Google Scholar]
- 12.Smith-Peterson MN. Arthrodesis of the sacroiliac joint. A new method of approch. J Bone Joint Surg. 1921;3:400–405. [Google Scholar]
- 13.Stuge B, Laerum E, Kirkesola G, Vollestad N. The efficacy of a treatment program focusing on specific stabilizing exercises for pelvic girdle pain after pregnancy: a randomized controlled trial. Spine (Phila Pa 1976) 2004;29:351–359. doi: 10.1097/01.BRS.0000090827.16926.1D. [DOI] [PubMed] [Google Scholar]
- 14.Sturesson B, Selvik G, Uden A. Movements of the sacroiliac joints. A roentgen stereophotogrammetric analysis. Spine. 1989;14:162–165. doi: 10.1097/00007632-198902000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Sturesson B, Uden A, Vleeming A. A radiostereometric analysis of the movements of the sacroiliac joints in the reciprocal straddle position. Spine (Phila Pa 1976) 2000;25:214–217. doi: 10.1097/00007632-200001150-00012. [DOI] [PubMed] [Google Scholar]
- 16.van Zwienen CMA, van den Bosch EW, Snijders CJ, van Vugt AB. Triple Pelvic Ring Fixation in Patients With Severe Pregnancy-Related Low Back and Pain. Spine. 2004;29:478–484. doi: 10.1097/01.BRS.0000092367.25951.4A. [DOI] [PubMed] [Google Scholar]
- 17.Vleeming A, Albert HB, Ostgaard HC, Sturesson B, Stuge B. European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur Spine J. 2008;17:794–819. doi: 10.1007/s00586-008-0602-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Waisbrod H, Krainick JU, Gerbershagen HU. Sacroiliac joint arthrodesis for chronic lower back pain. Arch Orthop Trauma Surg. 1987;106:238–240. doi: 10.1007/BF00450461. [DOI] [PubMed] [Google Scholar]
- 19.Walheim GG. Stabilization of the pelvis with the Hoffmann frame. An aid in diagnosing pelvic instability. Acta Orthop Scand. 1984;55:319–324. doi: 10.3109/17453678408992365. [DOI] [PubMed] [Google Scholar]
- 20.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]