Abstract
Introduction
Intraobserver and interobserver reliabilities of the several different methods to measure lumbar lordosis have been reported. However, it has not been studied sofar in patients with ankylosing spondylitis (AS).
Materials and methods
We evaluated the inter and intraobserver reliabilities of six specific measures of global lumbar lordosis in patients with AS. Ninety-one consecutive patients with AS who met the most recently modified New York criteria were enrolled and underwent anteroposterior and lateral radiographs of whole spine. The radiographs were divided into non-ankylosis (no bony bridge in the lumbar spine), incomplete ankylosis (lumbar spines were partially connected by bony bridge) and complete ankylosis groups to evaluate the reliability of the Cobb L1–S1, Cobb L1–L5, centroid, posterior tangent L1–S1, posterior tangent L1–L5, and TRALL methods.
Results
The radiographs were composed of 39 non-ankylosis, 27 incomplete ankylosis and 25 complete ankylosis. Intra- and inter-class correlation coefficients (ICCs) of all six methods were generally high. The ICCs were all ≥0.77 (excellent) for the six radiographic methods in the combined group. However, a comparison of the ICCs, 95 % confidence intervals and mean absolute difference (MAD) between groups with varying degrees of ankylosis showed that the reliability of the lordosis measurements decreased in proportion to the severity of ankylosis. The Cobb L1–S1, Cobb L1–L5 and posterior tangent L1–S1 method demonstrated higher ICCs for both inter and intraobserver comparisons and the other methods showed lower ICCs in all groups. The intraobserver MAD was similar in the Cobb L1–S1 and Cobb L1–L5 (2.7°–4.3°), but the other methods showed higher intraobserver MAD. Interobserver MAD of Cobb L1–L5 only showed low in all group.
Conclusion
These results are the first to provide a reliability analysis of different global lumbar lordosis measurement methods in AS. The findings in this study demonstrated that the Cobb L1–L5 method is reliable for measuring the global lumbar lordosis in AS.
Keywords: Ankylosing spondylitis, Lumbar lordosis, Radiographic measure
Introduction
The relationship of lumbar lordosis and low back disorders has received considerable attention. Clinical observations have suggested that maintenance of the normal lumbar lordotic curve is associated with the prevention of spinal disorders [4, 13]. Therefore, appropriate measurement of the lumbar curvature is important for clinical decisions. Several methods had been developed to measure the lumbar lordosis [1–5, 9, 16, 17]. The interobserver and intraobserver reliabilities of several different types of lumbar lordosis analysis have been reported [3, 11, 13, 17]. These include the Cobb, centroid, TRALL, and posterior tangent methods. Harrison et al. [8] compared these four measurement methods in lumbar lordosis and demonstrated high reliability of all methods. Hong et al. [10] compared these four measurement methods of lumbar lordosis in adult scoliosis and demonstrated that the Cobb L1–L5 and the posterior tangent L1–L5 methods were reliable. Chen et al. [3] compared the reliability of the Cobb and centroid methods and reported higher reliability in centroid method. However, there are no reports of lumbar lordosis measurement in ankylosing spondylitis (AS).
Recognition of the importance of reliability analysis for spine disease has led to several studies and radiological analysis of AS before and after surgery has been demonstrated in several studies. However, to date, the reliability of the lordosis angle measurements in AS has not been reported. Global lumbar lordosis is an important value for AS, the role of which in deformity progression, symptoms, and outcomes needs to be determined.
The AS is a chronic and inflammatory rheumatic disease characterized by inflammatory back pain due to sacroiliitis and spondylitis, the formation of syndesmophytes leading to ankylosis [19]. AS is thought to be the most common and most typical form of spondyloarthropathy. The arthritic changes and osteoporosis in the vertebral body could affect a precise measurement of lumbar lordosis. Therefore, determining the appropriate methods for measuring the lumbar lordosis is important for clinical decisions in AS. The aim of this study was to test the inter and intraobserver reliabilities of six specific measures of global lumbar lordosis in patients with AS, and to suggest a better method in measures of lumbar lordosis.
Patients and methods
Ninety-one consecutive patients were enrolled. The AS patients were recruited from the patients those were attending the outpatient clinic. Demographic characteristic and disease characteristics were obtained. There were 17 women and 74 men. The average age was 44.3 ± 13.5 years.
All patients with AS met the most recently modified New York criteria [18] and were eligible to participate in the trial if they were in medical treatment for at least 1 year. Exclusion criteria were age >60 years and the presence of concomitant neurological and psychiatric disease. Patients with attested orthopaedic diseases at spine (fracture, spinal disc herniation, spinal surgery, etc.) and lower extremities (such as prosthesis, etc.) were also excluded.
The participants underwent anteroposterior and lateral radiographs of whole spine. Radiographs were taken by one technician at a 72-in. standard distance using a standard technique and same X-ray machine in the standing position. The distance between the radiographic tube and the film was 120 cm. All anteroposterior and lateral radiographs included both hip joints and C7 vertebra. According to the ankylosis status of the curve in the radiographs, the radiographs were divided into three groups: non-ankylosis (no bony bridge in the lumbar spine), incomplete ankylosis (lumbar spines were partially connected by bony bridge) and complete ankylosis. The radiographs were composed of 39 non-ankylosis, 27 incomplete ankylosis and 25 complete ankylosis.
A delayed and repeated measurement design was used to evaluate the reliability of the three examiners. All radiographs were measured twice by each of three examiners with 2-week delay between the first and the second measurement. All measurements were carried out using a computer-based digital radiogram on a picture achieving computer system (PACS Expertise, Marosis, South Korea), which allowed easy and accurate determinations. A total of 546 measurements were taken for each of the six different radiographic methods. The six methods included the Cobb L1–S1, Cobb L1–L5, centroid, posterior tangent L1–S1, posterior tangent L1–L5, and TRALL methods.
Cobb L1–S1 method and L1–L5 method
These methods are widely used to measure spine alignment. The angle between the superior endplate of L1 and the superior endplate of S1, and the angle between the superior endplate of L1 and the inferior endplate of L5 are measured.
Centroid method (Fig. 1)
Fig. 1.
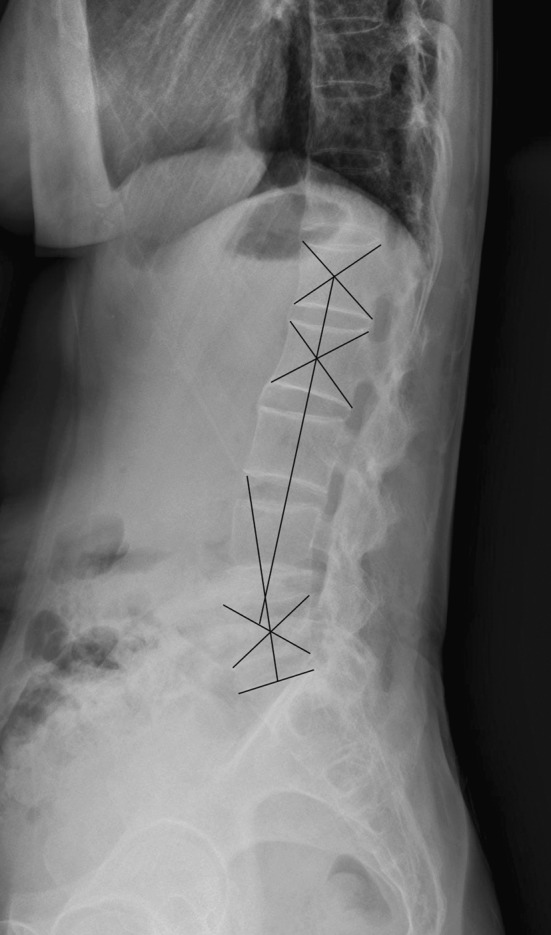
Centroid method
The intersections of four vertebral body corners are connected diagonally as vertebral centroids (L1, L2, L5). The intersection of the perpendicular lines drawn from the proximal and distal line made the lumbar lordosis. The proximal line connects the L1 and L2 centroid, and the distal line the L5 and bisected sacral point.
Posterior tangent L1–S1 method and L1–L5 method (Fig. 2)
Fig. 2.
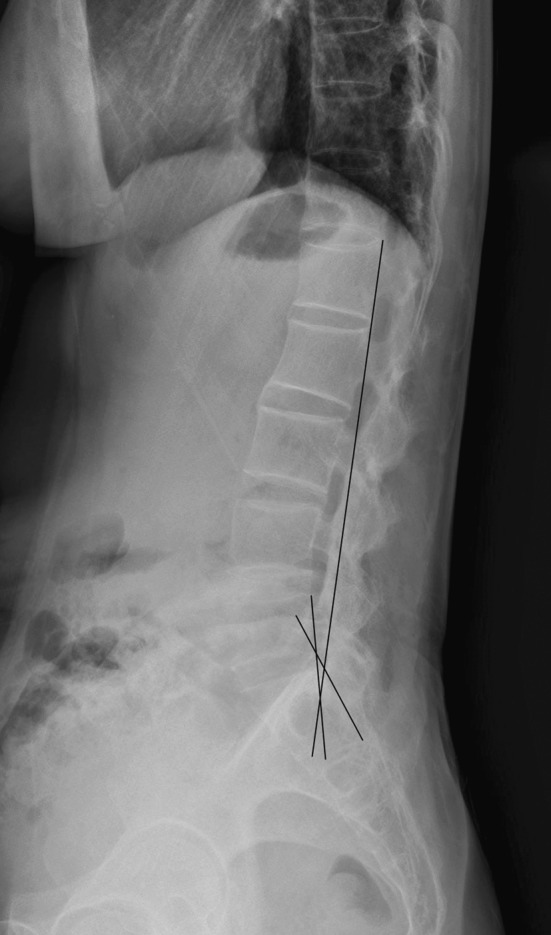
Posteior tangent L1–S1 method and L1–L5 method
The posterior tangent method uses the superior-posterior and inferior-posterior body corners.
TRALL method (Fig. 3)
Fig. 3.
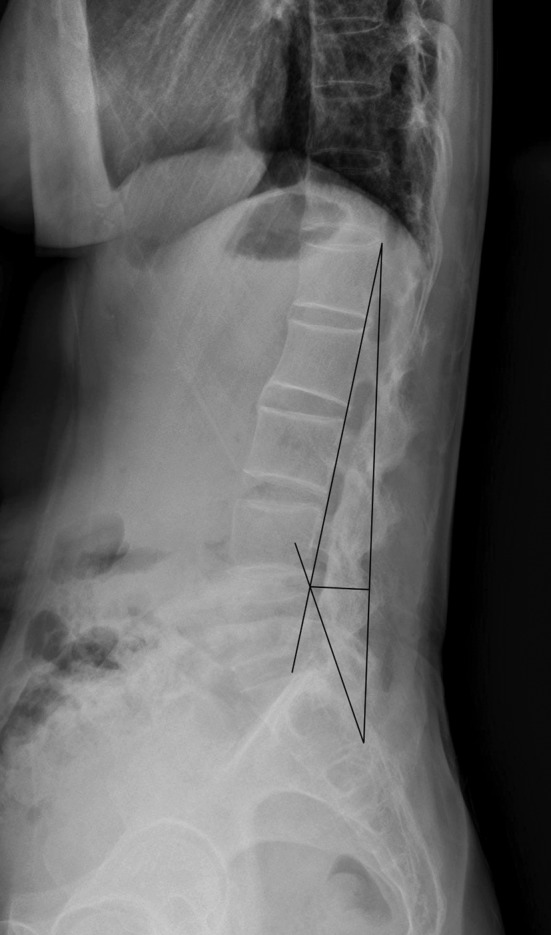
TRALL method
TRALL uses an apex at the greatest depth of lordosis. This greatest depth (to the posterior longitudinal ligament) is from a line connecting the inferior-posterior of S1 to the superior-posterior body corner of L1.
Statistical analysis was performed with SPSS 13 software for Windows (SPSS, Chicago, IL, USA) and MedCal software (Belgium). Data were expressed as mean ± SD.
Mean, SDs, interclass and intraclass correlation coefficients (ICCs), 95 % confidence intervals (CIs) were calculated. ICCs were considered by Shrout and Fleiss’s [6, 14] classifications (poor, <0.4; fair to good, 0.4–0.75; excellent, >0.75). The mean absolute differences (MADs) of observers’ measurements were determined to provide an error analysis. Using three-way analysis of variance (ANOVA), all statistical calculations for reliability results were performed with the assumptions that measurement is crossed with the examiner and patient, and that the examiner is a random factor rather than a fixed factor.
Results
Table 1 lists the overall mean and SD of the outcome measures covering the two readings of 91 radiographs by the three examiners. The ICCs, 95 % CI and MAD are provided for the two Cobb methods and centroid method, two posterior tangent methods and TRALL method. Table 2 provides the data for each group of the radiographs, which was classified by the degree of the curve ankylosis. In general, ICCs of all six methods were high. The ICCs were all ≥0.77 (excellent) for the six radiographic methods in the combined group (Table 1). However, a comparison of the ICCs and 95 % CI between groups with varying degrees of ankylosis showed that the reliability of the lordosis measurements decreased in proportion to the severity of ankylosis (Table 2). The six methods consistently demonstrated higher ICCs for both inter and intraobserver comparisons in non-ankylosis group, and five methods except TRALL method showed higher ICCs for both comparisons in incomplete group. However, in complete ankylosis group, The Cobb L1–S1, Cobb L1–L5 and posterior tangent L1–S1 methods demonstrated higher ICCs for both inter and intraobserver comparisons and the other methods showed lower ICCs.
Table 1.
Mean, standard deviations and ICC values of each measurement method
| Methods | Mean ± SD | Intraobserver reliability | Interobserver reliability | ||||
|---|---|---|---|---|---|---|---|
| ICC | 95 % CI | MAD | ICC | 95 % CI | MAD | ||
| C L1–S1 | 33.1 ± 11.3 | 0.96 | 0.94–0.97 | 3.3 | 0.95 | 0.92–0.96 | 4.4 |
| C L1–L5 | 23.1 ± 11.7 | 0.97 | 0.95–0.98 | 2.9 | 0.96 | 0.95–0.98 | 3.4 |
| Centroid | 25.3 ± 11.2 | 0.90 | 0.85–0.93 | 5.1 | 0.86 | 0.79–0.91 | 7.1 |
| P L1–S1 | 43.0 ± 11.1 | 0.90 | 0.85–0.93 | 5.4 | 0.93 | 0.89–0.95 | 5.7 |
| P L1–L5 | 18.7 ± 11.3 | 0.85 | 0.77–0.90 | 5.6 | 0.90 | 0.85–0.94 | 5.6 |
| TRALL | 29.3 ± 8.1 | 0.77 | 0.66–0.84 | 5.3 | 0.83 | 0.75–0.89 | 6.4 |
Table 2.
Mean, SD and ICC values of each measurement method for each group divided by the severity of ankylosis
| Methods | Mean ± SD | Intraobserver reliability | Interobserver reliability | ||||
|---|---|---|---|---|---|---|---|
| ICC | 95 % CI | MAD | ICC | 95 % CI | MAD | ||
| Non-ankylosis | |||||||
| C L1–S1 | 37.2 ± 10.5 | 0.97 | 0.95–0.98 | 2.8 | 0.97 | 0.94–0.98 | 3.2 |
| C L1–L5 | 26.5 ± 13.5 | 0.99 | 0.97–0.99 | 2.7 | 0.99 | 0.98–0.99 | 2.5 |
| Centroid | 29.0 ± 13.4 | 0.96 | 0.93–0.98 | 4.0 | 0.88 | 0.78–0.94 | 5.7 |
| P L1–S1 | 43.6 ± 9.9 | 0.92 | 0.86–0.96 | 4.8 | 0.94 | 0.90–0.97 | 4.4 |
| P L1–L5 | 22.9 ± 13.2 | 0.90 | 0.82–0.94 | 5.1 | 0.95 | 0.91–0.98 | 4.6 |
| TRALL | 29.2 ± 8.2 | 0.88 | 0.79–0.94 | 3.9 | 0.90 | 0.82–0.95 | 5.3 |
| Incomplete ankylosis | |||||||
| C L1–S1 | 30.8 ± 10.9 | 0.97 | 0.94–0.99 | 3.2 | 0.96 | 0.91–0.98 | 4.5 |
| C L1–L5 | 20.4 ± 8.9 | 0.95 | 0.90–0.98 | 2.8 | 0.98 | 0.95–0.99 | 3.7 |
| Centroid | 23.8 ± 9.7 | 0.84 | 0.67–0.93 | 5.4 | 0.91 | 0.82–0.96 | 5.8 |
| P L1–S1 | 43.0 ± 10.2 | 0.86 | 0.71–0.93 | 6.8 | 0.93 | 0.84–0.97 | 6.9 |
| P L1–L5 | 16.2 ± 9.7 | 0.83 | 0.65–0.92 | 5.4 | 0.88 | 0.76–0.95 | 5.6 |
| TRALL | 31.3 ± 7.7 | 0.57 | 0.10–0.80 | 6.7 | 0.75 | 0.46–0.89 | 7.4 |
| Complete ankylosis | |||||||
| C L1–S1 | 27.9 ± 9.2 | 0.87 | 0.63–0.92 | 4.3 | 0.85 | 0.66–0.93 | 5.4 |
| C L1–L5 | 20.3 ± 8.8 | 0.93 | 0.84–0.97 | 3.5 | 0.91 | 0.79–0.93 | 3.9 |
| Centroid | 26.0 ± 11.6 | 0.68 | 0.29–0.85 | 6.7 | 0.64 | 0.20–0.85 | 10.7 |
| P L1–S1 | 39.9 ± 10.7 | 0.89 | 0.76–0.95 | 4.8 | 0.90 | 0.78–0.96 | 6.4 |
| P L1–L5 | 15.5 ± 9.9 | 0.57 | 0.06–0.81 | 6.7 | 0.61 | 0.14–0.84 | 7.2 |
| TRALL | 30.0 ± 9.7 | 0.75 | 0.44–088 | 6.0 | 0.79 | 0.54–0.92 | 7.3 |
For the aspect of error analysis, in combined group, intraobserver MAD in the Cobb L1–S1 and Cobb L1–L5 and interobserver MAD in the Cobb L1–L5 were similar (2.9–3.4), but the other methods showed higher intra and interobserver MAD. A comparison of the MAD between the groups with varying degrees of ankylosis showed that the reliability of the lordosis measurements decreased in proportion to the severity of ankylosis. The intraobserver MAD was similar in the Cobb L1–S1 and Cobb L1–L5 (2.7°–4.3°), but the other methods showed higher intraobserver MAD. Interobserver MAD of measurement methods in all groups showed decreased reliability of measurement except for Cobb L1–L5 method.
Discussion
The inter and interobserver reliability of several different measurement methods of lumbar lordosis in normal population have been reported [3, 11, 13, 17]. Harrison et al. [8] compared the Cobb, centroid, posterior tangent, and TRALL methods for an analysis of segmental and global lumbar lordosis in a normal population. They reported that the inter and intraobserver reliabilities of measuring all segmental and global angles were high (ICCs > 0.83). Chen et al. [3] compared the Cobb and centroid methods in measurement of global lordosis, and reported interobserver reliability of 0.903, 0.826, and 0.784 for the centroid, Cobb L1–L5 and Cobb L1–S1, respectively. They concluded that the centroid method is more reliable for measuring lumbar lordosis than the Cobb method. However, reliability might be different under specific conditions such as AS. Hong et al. [10] compared Cobb, centroid, posterior tangent, and TRALL methods in measurement of global lordosis in adult scoliosis. They reported that the Cobb L1–L5 and the posterior tangent L1–L5 methods were reliable method for measuring the global lumbar lordosis in adult scoliosis. In this study, it was assumed that ICCs of the lumbar lordosis measurement method might be different in AS radiographs. Measurement of lumbar lordosis is important in treatment of AS. AS patients show lumbar hypolordosis and lumbar hypolordosis is related to the spinopelvic orientation, which can rotate the pelvis and change the gross sagittal alignment of spine. Kim et al. [12] and Suk et al. [15] reported that restoration of a more normal sagittal balance is the critical goal for any reconstructive spine surgery in AS. They mentioned that increased thoracic kyphosis and decreased global lumbar lordosis can break a sagittal balance in AS. The global lordosis angle can be an important value in AS, and accurate measurements of the lordosis angle are needed to examine AS patients. However, measurements of the lumbar lordosis in AS are difficult due to spondylitis and the formation of syndesmophytes in the vertebral body and endplate. In addition, osteopenic changes of spine often blur the vertebral silhouette. Therefore, the reliability of the lumbar lordosis measurement in AS may be different from that in the normal population. In this study, we analyze the reliability of the global lordosis measurement method to suggest a better method in AS patients. Segmental lumbar lordosis measurement is also clinically important in the AS surgery. However, it was very difficult drawing a multiple line in a small deformed segment; global lumbar lordosis is more valuable than segmental lordosis in AS patient, because AS is a systemic disease which often involves whole spine. Therefore, we could not compare the reliability of segmental lordosis measurement methods in AS patients and excluded segmental lordosis measurement in this study.
In this study, the ICCs of the combined 91 radiographs were all high (ICCs ≥ 0.77) in all groups. However, in each of the ankylosis groups, the intra and interobserver reliability decreased in proportion to the severity of the curve. The Cobb L1–L5, Cobb L1–S1 and posterior tangent L1–S1 showed consistently high ICCs in the ankylosis group (≥0.78). On the other hand, only the Cobb L1–L5 method demonstrated lower MAD for comparisons in all groups (≤3.9).
Between similar reliability of two methods, MAD has been useful for determining the most reliable method. Harrison et al. [8] said that high ICCs and low MAD means high reliability of the methods, and proposed that MAD should be provided for an error analysis in the reliability studies. Similarly, Chen et al. [3] reported that comparing the Cobb and centroid methods for lumbar lordosis in normal population, lower MAD of measurements in centroid method. They conclude that centroid method is better than Cobb method with high ICCs and low MAD.
In this study, only Cobb L1–L5 method showed higher reliability. The Cobb method is the technique that is most commonly used by clinicians, because it provides a simple and quick measurement of lumbar lordosis. Previous studies reported that the Cobb method is sensitive to contour changes, such as wedge, biconcave and brush, which resulted from osteoporosis [7, 13]. For above reasons, several authors have included other radiographic measurement methods on the lateral radiographs, such as posterior vertebral body tangents and centroid methods. However, it might be different in AS patients, as there is no report of AS. Although, regardless of the degenerative change, the posterior vertebral body margin of L1 and L5 is quite visible in normal population, it is difficult to accurately draw the posterior body margin because of spondylitis and formation of the syndesmophytes in AS patients. In the present study, the intra and interobserver reliability for the global L1–L5 Cobb angle was high with ICCs ≥0.91 in all groups, and Cobb L1–L5 method showed better reliability than Cobb L1–S1 and posterior tangent method. This result is in line with the S1 vertebra which is often affected by degenerative changes and its contour usually invisible in arthritic patients [13]. However, reliable methods including L5–S1 joint are also important. Cobb L1–S1, posterior tangent L1–S1, centroid and TRALL methods include the S1 vertebra, which often affects the degenerative changes. In this study, these four methods showed lower ICCs than Cobb L1–L5 method in all groups. However, Cobb L1–S1 and posterior tangent L1–S1 showed high ICCs (≥0.85). MAD of L1–S1 method was lower than that of posterior tangent L1–S1 method.
This results are the first to provide a reliability analysis of different global lumbar lordosis measurement methods in AS. The findings in this study demonstrated that the Cobb L1–L5 method is reliable for measuring the global lumbar lordosis in AS. In addition, the Cobb L1–S1 method is more reliable than other methods including the L5–S1 joint in assessment of lumbar lordosis.
Conflict of interest
None.
References
- 1.Adams MA, Hutton WC. The effect of posture on the lumbar spine. J Bone Joint Surg [Br] 1985;67:625–629. doi: 10.1302/0301-620X.67B4.4030863. [DOI] [PubMed] [Google Scholar]
- 2.Bernhardt M, Bridwell KH. Segmental analysis of the sagittal plane alignment of the normal thoracic and lumbar spines and thoracolumbar junction. Spine. 1989;14:717–721. doi: 10.1097/00007632-198907000-00012. [DOI] [PubMed] [Google Scholar]
- 3.Chen YL. Vertebral centroid measurement of lumbar lordosis compared with the Cobb technique. Spine. 1999;24:1786–1790. doi: 10.1097/00007632-199909010-00007. [DOI] [PubMed] [Google Scholar]
- 4.Chernukha KV, Daffner RH, Reigel DH. Lumbar lordosis measurement: a new method versus Cobb technique. Spine. 1998;23:74–79. doi: 10.1097/00007632-199801010-00016. [DOI] [PubMed] [Google Scholar]
- 5.Cobb J. Outline for the study of scoliosis. Instructional course lectures. Ann Arbor: American Academy of Orthopaedic Surgeons; 1948. pp. 261–275. [Google Scholar]
- 6.Dunn G. Design and analysis of reliability studies. Stat Methods Med Res. 1992;1:123–157. doi: 10.1177/096228029200100202. [DOI] [PubMed] [Google Scholar]
- 7.Genant HK, Li J, Wu CY, Shepherd JA. Vertebral fractures in osteoporosis: a new method for clinical assessment. J Clin Densitom. 2000;3:281–290. doi: 10.1385/JCD:3:3:281. [DOI] [PubMed] [Google Scholar]
- 8.Harrison DE, Harrison DD, Cailliet R, Janik TJ, Holland B. Radiographic analysis of lumbar lordosis: centroid, Cobb, TRALL, and Harrison posterior tangent methods. Spine. 2001;26:E235–E242. doi: 10.1097/00007632-200106010-00003. [DOI] [PubMed] [Google Scholar]
- 9.Hedman TP, Fernie GR. Mechanical response of the lumbar spine to seated postural loads. Spine. 1997;22:734–743. doi: 10.1097/00007632-199704010-00004. [DOI] [PubMed] [Google Scholar]
- 10.Hong JY, Suh SW, Modi HN, Hur CY, Song HR, Park JH. Reliability analysis for radiographic measures of lumbar lordosis in adult scoliosis: a case-control study comparing six methods. Eur Spine J. 2010;19:1551–1557. doi: 10.1007/s00586-010-1422-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jackson RP, Kanemura T, Kawakami N, Hales C. Lumbopelvic lordosis and pelvic balance on repeated standing lateral radiographs of adult volunteers and untreated patients with constant low back pain. Spine. 2000;25:575–586. doi: 10.1097/00007632-200003010-00008. [DOI] [PubMed] [Google Scholar]
- 12.Kim KT, Lee SH, Suk KS, Lee JH, Im YJ. Spinal pseudarthrosis in advanced ankylosing spondylitis with sagittal plane deformity: clinical characteristics and outcome analysis. Spine. 2007;32:1641–1647. doi: 10.1097/BRS.0b013e318074c3ce. [DOI] [PubMed] [Google Scholar]
- 13.Polly DW, Kilkelly FX, McHale KA, Asplund LM, Mulligan M, Chang AS. Measurement of lumbar lordosis: evaluation of intraobserver, interobserver, and technique variability. Spine. 1996;21:1530–1536. doi: 10.1097/00007632-199607010-00008. [DOI] [PubMed] [Google Scholar]
- 14.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi: 10.1037/0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 15.Suk KS, Kim KT, Lee SH, Kim JM. Significance of chin-brow vertical angle in correction of kyphotic deformity of ankylosing spondylitis patients. Spine. 2003;28:2001–2005. doi: 10.1097/01.BRS.0000083239.06023.78. [DOI] [PubMed] [Google Scholar]
- 16.Troyanovich SJ, Cailliet R, Janik TJ, Harrison DD, Harrison DE. Radiographic mensuration characteristics of the sagittal lumbar spine from a normal population with a method to synthesize prior studies of lordosis. J Spinal Disord. 1997;10:380–386. doi: 10.1097/00002517-199710000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Troyanovich SJ, Harrison DE, Harrison DD, Holland B, Janik TJ. Further analysis of the reliability of the posterior tangent lateral lumbar radiographic mensuration procedure: concurrent validity of computer-aided X-ray digitization. J Manip Physiol Ther. 1998;21:460–467. [PubMed] [Google Scholar]
- 18.van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis: a proposal for modification of the New York criteria. Arthr Rheum. 1984;27:361–368. doi: 10.1002/art.1780270401. [DOI] [PubMed] [Google Scholar]
- 19.Zochling J, van der Heijde D, Burgos-Vargas R, Collantes E, Davis JC, Dijkmans B, Jr, Dougados M, Geher P, Inman RD, Khan MA, Kvien TK, Leirisalo-Repo M, Olivieri I, Pavelka K, Sieper J, Stucki G, Sturrock RD, van der Linden S, Vendling D, Bohm H, van Royen BJ, Braun J. ASAS/EULAR recommendations for the management of ankylosing spondylitis. Ann Rheum Dis. 2006;65:442–452. doi: 10.1136/ard.2005.041137. [DOI] [PMC free article] [PubMed] [Google Scholar]


