Abstract
Background
Bloodstream infections (BSI) occur in up to 350 000 inpatient admissions each year in the US, with BSI rates among patients receiving parenteral nutrition (PN) varying from 1.3% to 39%. BSI-attributable costs were estimated to approximate $US12000 per episode in 2000. While previous studies have compared the cost of different PN preparation methods, this analysis evaluates both the direct costs of PN and the treatment costs for BSI associated with different PN delivery methods to determine whether compounded or manufactured pre-mixed PN has lower overall costs.
Objective
The purpose of this study was to compare costs in the US associated with compounded PN versus pre-mixed multi-chamber bag (MCB) PN based on underlying infection risk.
Methods
Using claims information from the Premier Perspective™ database, multivariate logistic regression was used to estimate the risk of infection. A total of 44 358 hospitalized patients aged ≥18 years who received PN between 1 January 2005 and 31 December 2007 were included in the analyses. A total of 3256 patients received MCB PN and 41 102 received compounded PN. The PN-associated costs and length of stay were analysed using multivariate ordinary least squares regression models constructed to measure the impact of infectious events on total hospital costs after controlling for baseline and clinical patient characteristics.
Results
There were 7.3 additional hospital days attributable to BSI. After adjustment for baseline variables, the probability of developing a BSI was 30% higher in patients receiving compounded PN than in those receiving MCB PN (16.1% vs 11.3%; odds ratio= 1.56; 95% CI 1.37, 1.79; p<0.0001), demonstrating 2172 potentially avoidable infections. The observed daily mean PN acquisition cost for patients receiving MCB PN was $US164 (including all additives and fees) compared with $US239 for patients receiving compounded PN (all differences p < 0.001). With a mean cost attributable to BSI of $US16 141, the total per-patient savings (including avoided BSI and PN costs) was $US1545.
Conclusion
In this analysis of real-world PN use, MCB PN is associated with lower costs than compounded PN with regards to both PN acquisition and potential avoidance of BSI. Our base case indicates that $US1545 per PN patient may be saved; even if as few as 50% of PN patients are candidates for standardized pre-mix formulations, a potential savings of $US773 per patient may be realized.
Key points for decision makers
Parenteral nutrition (supplied through an intravenous catheter directly into a vein in the arm or chest) is used when oral or tube feeding is not possible in hospitalized patients who are at risk of malnutrition, but increases the risk of bloodstream infection
Bloodstream infection associated with parenteral nutrition added 7.3 days and $US16141 to the average US hospital stay
Bloodstream infection rates were 30% higher with parenteral nutrition compounded manually or through a compounding device than with parenteral nutrition manufactured in a pre-mix formulation
The use of pre-mix rather than compounded parenteral nutrition offers potential savings of up to $US1545 per patient, or between $US48 million and $US96 million in annual savings to the US healthcare system
Background
The prevalence of hospital malnutrition has been reported to range from 23% to 60% of all hospital admissions.[1–6] While some of these individuals are malnourished upon admission, many become depleted during hospital stay.[7] Surgery, trauma, critical illness and infection are just some of the conditions associated with increased nutrient requirements and the risk for developing in-hospital malnutrition.[8]
Bloodstream infection (BSI) occurs in up to 350 000 inpatient admissions each year in the US,[9] and is considered one of the four major infection types that together account for 78% of all hospital-associated infections.[10] Moreover, with an attributable mortality of 15%, BSI represents one of the eight leading causes of in-hospital death in the US,[9] depending on population characteristics and illness severity. In addition to the human toll consequential to infection, BSI-attributable costs approximated $US12000 per episode in 2000.[11]
The adverse impact of malnutrition can be minimized with early supplemental feeding.[12] Parenteral nutrition (PN) is used when enteral nutrition (EN) fails or is contraindicated. Yet PN is not without additional cost or risk of adverse events, and BSI rates among PN patients have been reported to vary widely (from 1.3% to 39%[13,14] depending on the patient population).
In the US, hospitals compound sterile intravenous admixtures, including PN, under the guidance of the US Pharmacopeia Chapter 797 (USP).[15] Comprehensive and costly procedures for controlling the environment, training pharmacy staff, handling the infusate and validating the process are included in the published USP standards as a means to minimize contamination.[16] Despite these recommendations, intravenous compounding practices range from the poorly controlled addition of drugs to an intravenous bag at the bedside, to fully controlled compounding centres.[17]
Contamination rates during PN compounding are estimated to range from 4.4% to 6.7%.[18,19] Pre-mixed and ready-to-use products, for which sterility is guaranteed by the manufacturing process, require fewer additives and thereby minimize the potential for touch contamination during PN preparation and administration.[20–22] According to publications by the USP[15] and the American Society of Health System Pharmacists,[23] compounded formulations are generally considered medium risk for patient exposure to microbial and physical contaminants, while manufactured pre-mix is considered low risk, provided any additions to the bag are sterile. In fact, the US Joint Commission[24] recommends the use of pre-mixed products whenever possible.
The decision around PN choice can be complex, and there are no specific guidelines advising the appropriate circumstances under which premixed, standardized or custom PN should be used for various patient populations.[25,26] The greatest potential disadvantage to pre-mixed standardized PN appears to be the limited range of formulae available, particularly in some countries. In addition, some populations, including critically ill or fluid-restricted patients, or those with organ dysfunction, may be more appropriately served with custom PN.[20]
Several studies have compared the cost of different PN compounding methods,[27–29] but there have been no investigations of costs associated with differential infection rates for various methods of PN preparation. The purpose of this study was to compare per-patient costs associated with compounded PN versus pre-mixed multi-chamber bag (MCB) PN based on underlying infection risk. Since the method of PN preparation has been demonstrated to have a significant impact on infection rates,[30] it is expected that costs will be lower for patients receiving PN delivered via MCB than via compounded PN. However, the extent of potential savings due to both the reduced risk of BSI and the preparation cost of PN is unknown.
Methods
Data Source
We evaluated PN costs using claims data from a nationally representative group of US hospitals managed by Premier Healthcare Alliance, which covers more than 400 hospitals in the US. The Premier Perspective™ database includes patients’ complete billing and coding history at the level of the individual patient. While typical claims databases rely on charges only reimbursable by insurance for their economic analysis, Premier Perspective™ has the advantage of having available the transaction-level cost data for each admission, including procedures and diagnostic, therapeutic, laboratory and pharmacy services (including PN and additives). The only costs not included are physician or other provider charges that are typically billed separately, either to a payer or directly to the patient. All cost data were inflation-adjusted to $US, year 2009 values.
Study Population
All hospital inpatients aged ≥18 years who received any PN formulation between 1 January 2005 and 31 December 2007 were included. Any patient who was admitted with infection, hepatic dysfunction, acute cholecystitis, phlebitis or thrombophlebitis was excluded from the analyses. In addition, we excluded all patients with renal failure or cirrhosis, since the costs associated with their primary condition would skew our economic analysis. Analysis of patients with the above conditions, both with and without renal failure or cirrhosis, will be reported elsewhere.[30,31] The initial database contained over 11 million inpatients, of which 73 048 patients received at least one charge for PN. After excluding all patients aged <18 years, and those admitted with any of the previously mentioned diagnoses, a total of 44 358 patients from 194 hospitals were included in the final analyses.
Patients were classified as receiving PN via either pre-mixed MCB (manufactured PN in a dualchamber bag with dextrose and amino acids, which may have included additions of minerals, vitamins, electrolytes or lipids; n=3256) or compounded admixture (either hospital compounded or outsourced; n=41 102).
Outcomes
The primary objective of this study was to calculate the cost associated with different methods of delivering PN to patients. Economic outcomes included hospital length of stay (LOS), use of ICU and ICU LOS, and total hospital costs. BSI, assumed to be a primary cost driver in this analysis, was defined as any ICD-9 codes of 038.x (septicaemia), 995.91 (sepsis), 995.92 (severe sepsis) and 790.7 (bacteraemia). Outcomes were compared across the two treatment groups for all patients in the analytic dataset.[31]
Analysis
Treatment Group Differences
Baseline demographics, co-morbidities and hospitalization characteristics were reported descriptively for each treatment group using means (with SDs) and medians (with ranges) for continuous variables, and by raw counts (with percentages) for categorical measures. Differences were reported using chi-squares for categorical measures and t-tests for continuous variables. Incidence rates for BSI were reported by treatment group.
All Patient Refined DRG (APR-DRG) classifications are generally used to estimate severity of illness and risk of mortality. Since all variables used to calculate APR-DRG were available to us, we included them individually in model estimates. We did report proportions of APR-DRG severity in the PN population for descriptive purposes.
Risk of Bloodstream Infection (BSI)
Multivariate logistic regression was used to create a model to estimate the risk of BSI for patients receiving MCB versus compounded PN. The model adjusted for baseline differences, risk factors and potential confounders available in the database, including hospital variables (size, geographical region, teaching status and urban/rural location); patient demographics (age, sex, ethnicity, payer); patient co-morbidities; and other indicators of acuity defined by ICD-9 codes (nutritional deficiency, intestinal malabsorption, acute pancreatitis, peritonitis, gastrointestinal fistula, Crohn’s disease, cancer, diabetes mellitus, tuberculosis, emergency or urgent admission, surgical status, prior surgery or prior PN); and length of PN treatment. Details on model development and validation will be published in Mercaldi et al.[31]
The initial model contained all independent variables listed above. Variable-selection procedures were aimed at identifying a reduced set of independent variables that provided the best fit for the model. The final model was determined using backward elimination variable selection, with a significance level of 0.10 of the Wald chisquared statistic to specify the co-variates that would remain in each step. Model fit was assessed using the C-statistic, which corresponds to the area under a receiver operating characteristic (ROC) curve. The ROC curve indicates the probability that randomly selected patients with the event have a higher predicted probability of the event than randomly selected patients without the event. Risk of BSI was reported as adjusted probability of the event, and an odds ratio (OR) with 95% confidence levels. Further details on data integrity safeguards, the calculation of infection risk and sensitivity analyses, including propensity score modelling, will be published else where.[30]
Length of Stay (LOS), BSI-Attributable Total and Daily Parenteral Nutrition Costs
Baseline patient characteristics, including markers of severity, could affect our estimation of cost benefits. PN-associated costs and LOS were estimated using multivariate ordinary least squares regression models constructed to measure the impact of infection events on total hospital costs after controlling for baseline and clinical patient characteristics. As both cost and hospital stay data generally do not follow a Normal distribution and are often right-skewed, these variables were transformed to their natural logs. Adjusted mean log-costs and log-LOS were then retransformed using Duan’s smearing estimate.[32] Statistical comparisons across groups were conducted using t-tests of adjusted least squares mean log-cost and log-LOS. The incremental difference in adjusted mean hospital costs and LOS between patients with and without an infection event was assumed to be the total hospital costs and LOS attributable to having an infection. This analysis yielded estimates for costs and LOS that were attributable to BSI. A similar analysis yielded an adjusted difference in daily PN costs between the two groups, controlling for baseline and clinical patient characteristics.[31] PN costs for both MCB and compounded PN included nutrient additives and pharmacy labour as per the Premier Perspective™ database. Since PN costs were evaluated separately from BSI-attributable costs, contributions of each to total savings could be identified.
Avoidable BSI
If either method of PN preparation was associated with fewer BSIs than the other method, the number of potentially avoidable infections could be calculated from ORs. However, if the OR calculation was the product of logistic regression and BSI incidence rates were greater than 10%, both risk and avoidable infections (as calculated from risk), could be overestimated.[33] To avoid this, we performed a correction to our adjusted ORs to more accurately represent relative risk.[33] To estimate potentially avoidable BSIs for the group with the higher rate of events, we calculated the difference between the number of observed and expected events (equation 1):

where the number of expected events was calculated by multiplying actual events by relative risk.
Calculation of Total Per-Patient Savings
While there were significant differences in overall costs for the two groups, the intent of our analysis was to identify the primary cost drivers. Consequently, primary savings originated from differences in daily PN cost, plus savings due to avoidable BSIs. To calculate savings per patient due to differences in PN cost, we multiplied the difference in daily PN cost by the mean number of PN days for the total population (equation 2):
where the difference in daily PN cost is the observed difference adjusted for baseline characteristics.
To calculate per-patient savings due to avoidable BSI, avoidable BSI was multiplied by the attributable costs for BSI, and divided by the number of patients with the opportunity to avoid BSI (equation 3):
where the n of patients in the higher BSI rate group represents the number of patients with the opportunity to avoid BSI.
To calculate the total per-patient cost savings, we added per-patient PN savings to avoidable BSI savings.
Sensitivity Analyses
In the first sensitivity analyses, logistic regression was repeated using both ICD-9 codes andthe administration of any intravenous antibiotic following the initiation of PN to identify BSIs. This served as an accuracy check of the ICD-9 codes used to identify BSIs. Second, minimum and maximum per-patient savings were calculated via a series of one-way sensitivity analyses using 95% confidence intervals for daily PN and avoidable BSI. All three upper and all three lower limits were then added to achieve an extreme sensitivity (absolute minimum and maximum) for total potential per-patient savings.
As previously discussed, not all patients are appropriate candidates for standardized pre-mix PN formulae. The calculations in equations 1 and 2 assume that 100% of patients would be equally appropriate for PN prepared by either method, but this is not likely to be the case. Additional sensitivities on total per-patient savings were calculated, assuming 50%, 65%, 80% and 95% levels of appropriateness for pre-mixed MCB PN.
Results
Baseline and Clinical Characteristics
Tables I and II compare the descriptive hospital, patient and treatment variables for the two groups. MCB PN was commonly used in urban hospitals (62.4%), non-teaching hospitals (81.9%), and those with fewer than 500 beds (96.7%), while compounded PN was also commonly used in urban hospitals (92.5%) and non-teaching hospitals (54.0%), but in larger hospitals with 250–999 beds (88.8%). The proportion of hospitals using MCB or compounded PN were significantly (p<0.01) different with regard to all hospital characteristics, with the exception of hospital size ≥1000 beds (table I).
Table I.
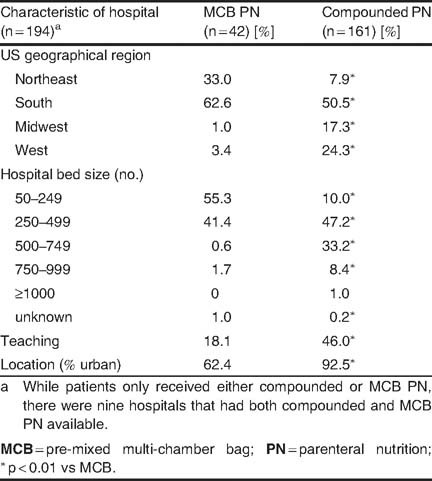
Descriptive variables at baseline: hospitals
Table II.
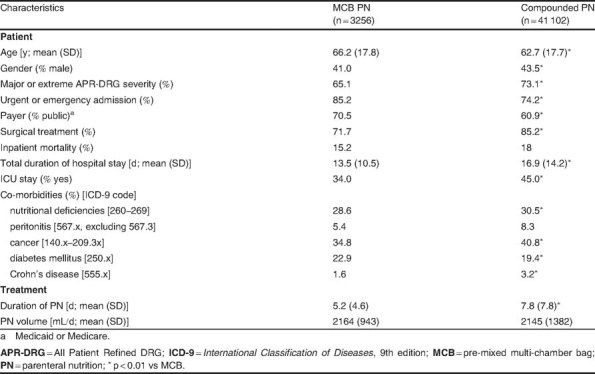
Descriptive variables at baseline: patients and treatment
Patients who received PN via MCB were slightly older (aged 66.2 vs 62.7 years), more likely to have had an urgent or emergency admission (85.2% vs 74.2%), and more likely to be on Medicaid or Medicare (70.5% vs 60.9%), yet less likely to have an ICU stay (34.0% vs 45.0%) than those receiving compounded PN; all differences p<0.01 (table II). Patients in both groups were equally likely to die in hospital (15.2% vs 18%). Patients receiving compounded PN were more likely to have an APR-DRG severity rating of ‘major’ or ‘severe’ (73.1% vs 65.1%), and to be admitted with nutritional deficiencies (30.5% vs 26.8%), peritonitis (8.3% vs 5.4%), cancer (40.8% vs 34.8%) or Crohn’s disease (3.2% vs 1.6%), and were less likely to have diabetes mellitus (19.2% vs 22.9%) than those receiving MCB PN; all differences p<0.01. With regards to PN treatment (table II), patients in the compounded PN group received PN for longer than those in the MCB group (7.8 vs 5.2 days; p<0.01).
BSI Rates, LOS and Costs
Figure 1 depicts the observed and adjusted BSI rates for the two groups. There were 6788 BSIs observed in the compounded PN group and 363 in the MCB PN group. The compounded PN group demonstrated a 33% increase in observed BSI rates over the MCB PN group (16.5% vs 11.1%; OR=1.72; 95% CI 1.59, 1.85; p<0.0001), while the adjusted rates are associated with a 30% higher probability of BSI in the compounded PN group (16.1% vs 11.3%; OR=1.56; 95% CI 1.37, 1.79; p<0.0001). Further details on infection rates and sensitivity modelling will be published in Turpin et al.[30]
Fig. 1.
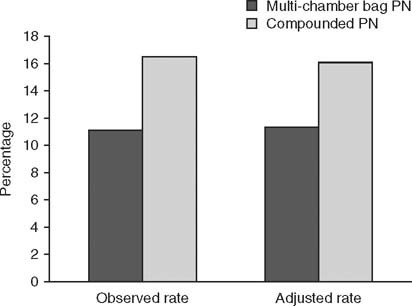
Bloodstream infection rates in the pre-mixed multi-chamber bag and compounded parenteral nutrition (PN) groups. Odds ratio for observed rate = 1.72; 95% CI1.59,1.85; p < 0.0001. Odds ratio for adjusted rate = 1.56; 95% CI 1.37, 1.79; p<0.0001.
The observed differences in total LOS were 13.5 days for the MCB PN group and 16.9 days for the compounded PN group. The additional hospital days attributable to BSI were 7.3 days. The MCB PN group had an observed daily mean PN cost of $US164 (including all additives) for a mean total PN cost of $US845; the compounded PN group had a mean daily PN cost of $US239 (including all additives), with a mean total PN cost of $US1681 (all differences p<0.001). The adjusted difference between groups (accounting for baseline characteristics and clinical variables) in PN daily cost was $US91.
Potentially Avoidable BSI
To estimate relative risk, a corrected OR was calculated, as recommended by Zhang and Yu.[33] Relative risk estimates indicate that 2172 of the 6788 BSIs experienced by the compounded PN group may have been avoided by using MCB PN (if 100% were appropriate for pre-mixed MCB PN) [equation 4]:
 |
4 |
where 6788 is the number of compounded PN patients, and 0.68 is the adjusted OR for BSI.
In a sensitivity analysis, the number of potentially avoidable BSI is reduced by changing the number of patients who were potential candidates for MCB PN from 2172 (100% appropriate) to 2063 (95% appropriate), 1738 (80% appropriate), 1412 (65% appropriate) and 1086 (50% appropriate).
Per-Patient Savings and Sensitivity Analysis
After adjusting for baseline characteristics, the total per-patient PN cost for the MCB PN group was $US91 less per day than for the compounded PN group. To extrapolate the analysis to the entire US population receiving PN, the mean number of PN days for all patients in this analysis was used (7.6 days). Per-patient PN savings were estimated by multiplying the difference in daily PN costs by the mean number of PN days for the total population (equation 5):
where $US91 is the adjusted difference in PN cost per day, and 7.6 is the mean PN days.
Estimated savings per patient due to avoidable BSI is obtained by multiplying the number of potentially avoidable BSI by the costs attributable to BSI, and dividing by the number of patients with the opportunity to avoid BSI (equation 6):
 |
6 |
where 2172 is number of potentially avoidable BSI, $US16141 is the cost attributable to BSI, and 41102 is the number of compounded PN patients.
Total potential per-patient savings were estimated by adding the savings in PN to the savings due to avoidable BSI (equation 7):
 |
7 |
where $US692 is per-patient PN savings, and $US853 is the avoidable BSI savings.
Figure 2 illustrates total cost savings per patient, and the results of the sensitivity analysis. The base case indicates that $US1545 per PN patient can be saved (PN costs and BSI cost avoidance) if all PN patients are appropriate candidates to receive PN via MCB. If as few as 50% of PN patients are able to use the standardized formulations provided in MCBs, savings are reduced to $US773 per PN patient. The extreme sensitivity analysis at the 95% confidence limits included either the lowest or the highest values for avoidable BSI, BSI-attributable costs and adjusted daily PN savings. The confidence intervals illustrated in figure 2 demonstrate that, even at its most extreme case, using the 95% lower limit and a 50% appropriateness level, use of MCBs still potentially yields a $US568 savings per PN patient.
Fig. 2.
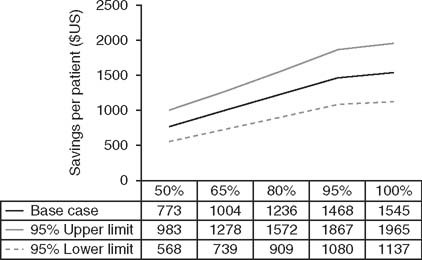
Savings per patient by appropriateness for pre-mixed multichamber bag (MCB) parenteral nutrition (PN). Extreme sensitivity analysis (absolute lower and upper limits) achieved by adding sensitivities of daily PN savings, bloodstream infection (BSI)-attributable costs and avoidable BSI. Appropriateness for standardized PN via MCB based on potential needs of each patient population.
Discussion
The present analysis suggests that there are important differences in PN costs when compounded or purchased as a pre-mixed MCB. Savings resulting from lower direct costs (for purchasing PN components) and cost avoidance (through potentially fewer BSIs) were considered in this cost analysis. Results from the sensitivity analysis indicate that, under even the most extreme sensitivities, use of pre-mixed MCB PN may lead to significant cost savings.
While the intestinal tract is functional, it is preferable to utilize the oral or enteral routes to provide nutrition. EN supports the integrity of the gut and is associated with a lower infection risk than PN. According to US guidelines, when a patient is unable to use EN and there is no evidence of protein-calorie malnutrition, PN is not recommended until after the first 7 days of hospitalization.[34] A key rationale for this relatively conservative approach to PN therapy centres around infectious morbidity. Until now, data to distinguish between the method of PN preparation and its potential impact on BSI have not been available, although closed-intravenous systems (fully collapsible containers that do not use an external vent to empty the solution, with self-sealing injection ports), have consistently demonstrated significantly lower incidences of central venous catheter-associated bacteraemia than open systems.[35–38] The analysis presented here may provide a greater understanding of the factors that influence infection in PN patients.
According to the Healthcare Cost and Utilization Project, there were 220194 adults in the US who received PN in 2007.[39,40] When applying the inclusion and exclusion criteria of this study (39.3% of patients were excluded for reasons previously articulated), the proportion of patients receiving PN via MCB (92.7% in the current study), and the BSI rates from our analyses (adjusted rates 16.1 % for compounded PN vs 11.3% for MCB PN), 19947 of the remaining 73 048 could expect to experience a BSI. Of those 19947 BSI, 5947 would have been potentially avoidable by using MCBs (if all PN patients were candidates for MCB).
The number of potentially avoidable BSIs is reduced when fewer patients are appropriate candidates for MCB PN: 5650 (with 95% appropriate), 4758 (80% appropriate), 3866 (65% appropriate), 2974 (50% appropriate). The large number of potentially avoidable BSI in the US each year, with attributable costs of $US16 141 per BSI, could potentially save the US healthcare system from $US48 million (with 50% of patients appropriate candidates for MCB PN) to $US96 million (100% appropriate) each year. Significantly greater savings could be realized if the higher BSI rates found among patients with cirrhosis or renal failure[30,31] were included in these estimates.
One of the most influential factors in cost is LOS, and, unsurprisingly, BSI resulted in substantially increased LOS. Further studies have shown that, after controlling for severity of illness, patients who received early and sufficient nutrition had significantly shorter LOS,[41–43] with malnourished patients in one study experiencing increased LOS of 3.3 days (7.7 ±7 days vs 11±9 days; p<0.0001).[44] Thus, both early clinical nutrition and prevention of BSI are important factors in limiting LOS and, therefore, costs.[45]
Typical of any retrospective analysis, further study with adequate controls is necessary before any definitive direction can be taken. This is a particularly sensitive issue with regards to the investment in pharmacy clean-rooms and specially trained personnel that many hospitals have either undertaken or chosen to outsource to improve the safety of their parenteral preparations. Despite these investments, 95.4% of US hospitals purchase pre-mixed large-volume parenteral products, which may include pre-mixed PN.[17] Use of standardized PN formulae, when compounded in-hospital, are attributed to a 55.8% reduction in wasted PN bags and a 36.9% decrease in cost (labour, materials and inventory), with PN preparation times cut by 66.1% and acquisition costs of PN reduced by 54.5%.[46] Nonetheless, the analysis presented here may provide further ideas for quality improvement and other initiatives to hospitals.
One of the greatest strengths of conducting claims database research is the ability to examine the real-world use of PN on a large scale. However, this retrospective observational study design does introduce some limitations. For one, the inability to randomize exposure limits our capacity to determine a causal relationship between PN type and infection rates. Analyses of these data[30] using a matched propensity score model created balanced groups of patients receiving MCB and compounded PN (including measures of severity). Significant differences in adjusted BSI rates were found between the groups (MCB PN 18.8%; compounded PN 24.5%; OR 1.49; p<0.001). While these data do not enhance our ability to identify causality, they do provide additional validity to our analysis.
Second, the potential confounders that we could explore could only include variables measured in the database and, therefore, we cannot guarantee that we have completely accounted for all sources of variance. Most notably, data on the type and duration of central access device use were not reliably available. As such, we could not calculate intravenous catheter days and were unable to report BSI per catheter day as commonly used by organizations such as the US Centers for Disease Control and Prevention and the Joint Commission.[10,24] The medical literature has reported BSI rates with PN in the range of 7.2–39%, providing an appropriate context for our findings.[13,47] Although central catheters are an infection risk, we were able to include many of the variables in our analysis that are correlated with central line use (e.g. diagnosis, co-morbidities, surgical status, number of hospital PN days).
Finally, although our sensitivity analysis confirmed that ICD-9 codes were likely adequate in identifying BSI, we did not conduct a review of individual patient records in order to validate these findings. Nonetheless, the large population in our analysis provides us with the unique opportunity to explore these associations with adequate power and guide further study into this relationship.
Despite the limitations imposed by retrospective database analyses, these types of studies are used by the US FDA to detect and explore safety signals for marketed drugs. [48] One of the best-known examples was the identification of increased coronary symptoms associated with cyclo-oxygenase (COX)-2 selective NSAIDs in the early 2000s. Epidemiological studies of large retrospective databases led to further study, and eventually the withdrawal of valdecoxib (Bextra®) and refocoxib (Vioxx®) from the US market.[48,49]
Conclusions
This analysis represents real-world PN use in the largest adult hospitalized patient population to date. The group receiving compounded PN had more severe illness, a higher observed BSI rate and a longer LOS than the group that received MCB PN. Once illness severity and other baseline variables were accounted for, the adjusted probability of BSI remained significantly lower for the MCB than the compounded PN group. The savings associated with lower PN costs and BSI cost avoidance may provide an opportunity to reduce healthcare spending when PN is delivered via MCB.
The retrospective nature of these data limits us to identifying potential associations, and not causality, between type of PN preparation and BSI. Nonetheless, these findings may contribute to an open discussion in the nutrition community regarding potential risks associated with various PN products. The analysis presented here demonstrates a clear need for randomized trials to further explore this critical issue.
Footnotes
International Classification of Diseases, 9th edition (ICD-9) codes for exclusions are as follows: hypoglycaemia 251.2; hyperglycaemia 249, 790.29; hepatic dysfunction 570, 572.2; acute cholecystitis 575; phlebitis, thrombophlebitis or pulmonary embolism 451.82, 451.83, 451.84, 415.1x; cirrhosis or chronic liver disease 571.x–573.x; renal failure 584.x, 585.x.
Using the corrected OR yields a conservative estimate of potentially avoidable BSI. When using a non-corrected OR, the estimate for potentially avoidable BSI is 2482.
References
- 1.Correia M.I., Waitzberg D.L. The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr. 2003;22(3):235–9. doi: 10.1016/S0261-5614(02)00215-7. [DOI] [PubMed] [Google Scholar]
- 2.Joosten K.F., Hulst J.M. Prevalence of malnutrition in pediatric hospital patients. Curr Opin Pediatr. 2008;20(5):590–6. doi: 10.1097/MOP.0b013e32830c6ede. [DOI] [PubMed] [Google Scholar]
- 3.Meijers J.M., Schols J.M., van Bokhorst-de van der Schueren M.A., et al. Br J Nutr. 2009. Malnutrition prevalence in the Netherlands: results of the annual Dutch national prevalence measurement of care problems. [DOI] [PubMed] [Google Scholar]
- 4.Pirlich M., Schütz T., Norman K., et al. The German hospital malnutrition study. Clin Nutr. 2006;25(4):563–72. doi: 10.1016/j.clnu.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 5.Shum N.C., Hui W.W., Chu F.C., et al. Prevalence of malnutrition and risk factors in geriatric patients of a convalescent and rehabilitation hospital. Hong Kong Med J. 2005;11(4):234–42. [PubMed] [Google Scholar]
- 6.Waitzberg D.L., Caiaffa W.T., Correia M.I. Hospital malnutrition: the Brazilian national survey (IBRANUTRI): a study of 4000 patients. Nutrition. 2001;17(7-8):573–80. doi: 10.1016/S0899-9007(01)00573-1. [DOI] [PubMed] [Google Scholar]
- 7.Beghetto M.G., Koglin G., de Mello E.D. Influence of the assessment method on the prevalence of hospital malnutrition: a comparison between two periods. Nutr Hosp. 2010;25(5):774–80. [PubMed] [Google Scholar]
- 8.Norman K., Pichard C., Lochs H., et al. Prognostic impact of disease-related malnutrition. Clin Nutr. 2008;27(1):5–15. doi: 10.1016/j.clnu.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 9.Wenzel R.P., Edmond M.B. The impact of hospital-acquired bloodstream infections. Emerg Infect Dis. 2001;7(2):174–7. doi: 10.3201/eid0702.010203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Klevens R.M., Edwards J.R., Richards C.L., et al. Estimating health care-associated infections and deaths in US hospitals, 2002. Public Health Rep. 2007;122(2):160–6. doi: 10.1177/003335490712200205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Warren D.K., Quadir W.W., Hollenbeak C.S., et al. Attributable cost of catheter-associated bloodstream infections among intensive care patients in a nonteaching hospital. Crit Care Med. 2006;34(8):2084–9. doi: 10.1097/01.CCM.0000227648.15804.2D. [DOI] [PubMed] [Google Scholar]
- 12.Btaiche I.F., Chan L.N., Pleva M., et al. Critical illness, gastrointestinal complications, and medication therapy during enteral feeding in critically ill adult patients. Nutr Clin Pract. 2010;25(1):32–49. doi: 10.1177/0884533609357565. [DOI] [PubMed] [Google Scholar]
- 13.Dissanaike S., Shelton M., Warner K., et al. The risk for bloodstream infections is associated with increased parenteral caloric intake in patients receiving parenteral nutrition. Crit Care. 2007;11(5):R114. doi: 10.1186/cc6167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Opilla M. Epidemiology of bloodstream infection associated with parenteral nutrition. Am J Infect Control. 2008;36(10):S173.e5–8. doi: 10.1016/j.ajic.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 15.Chapter 797. In: The United States Pharmacopeial Convention. USP 31/NF 26. Rockville (MD): The United States Pharmacopeial Convention, 2008
- 16.Kastango E.S. The cost of quality in pharmacy. J Pharm Technol. 2003;19(1):49–52. [PubMed] [Google Scholar]
- 17.Pedersen C.A., Schneider P.J., Scheckelhoff D.J. ASHP national survey of pharmacy practice in hospital settings: dispensing and administration — 2008. Am J Health-Syst Pharm. 2009;66(10):926–46. doi: 10.2146/ajhp080715. [DOI] [PubMed] [Google Scholar]
- 18.Trissel L.A., Gentempo J.A., Anderson R.W., et al. Using a medium-fill simulation to evaluate the microbial contamination rate for USP medium-risk-level compounding. Am J Health-Syst Pharm. 2005;62(3):285–8. doi: 10.1093/ajhp/62.3.285. [DOI] [PubMed] [Google Scholar]
- 19.Hansen E.W., Nielsen P.L. Intrinsic and extrinsic microbial contamination of home total parenteral nutrition manufactured in eva-infusion bags (the i.v. bag) J Clin Pharm Ther. 1987;12(5):325–31. doi: 10.1111/j.1365-2710.1987.tb00544.x. [DOI] [PubMed] [Google Scholar]
- 20.Miller S.J. Commercial premixed parenteral nutrition: is it right for your institution? Nutr Clin Pract. 2009;24(4):459–69. doi: 10.1177/0884533609339067. [DOI] [PubMed] [Google Scholar]
- 21.Pichard C., Mühlebach S., Maisonneuve N., et al. Prospective survey of parenteral nutrition in Switzerland: a three-year nation-wide survey. Clin Nutr. 2001;20(4):345–50. doi: 10.1054/clnu.2001.0428. [DOI] [PubMed] [Google Scholar]
- 22.Planas M., Puiggrós C., Sänchez J.R., et al. Use of ready-to-use (RTU) products in home-based parenteral nutrition. Nutr Hosp. 2006;21(1):64–70. [PubMed] [Google Scholar]
- 23.ASHP technical assistance bulletin on quality assurance for pharmacy-prepared sterile products Am J Hosp Pharm. 1993;50(11):2386–98. [PubMed] [Google Scholar]
- 24.Bing C.M. Joint Commission Resources, Inc. A guide to JCAHO’s medication management standards. Oakbrook Terrace (IL): Joint Commission Resources Inc.; 2004. Compliance with the Joint Commission medication management standards; pp. 11–29. [Google Scholar]
- 25.Kochevar M., Guenter P., Holcombe B., et al. ASPEN statement on parenteral nutrition standardization. JPEN J Parenter Enteral Nutr. 2007;31(5):441–8. doi: 10.1177/0148607107031005441. [DOI] [PubMed] [Google Scholar]
- 26.Gates D.M., Smolarek R.T., Stevenson J.G. Outsourcing the preparation of parenteral nutrient solutions. Am J Health-Syst Pharm. 1996;53(18):2176–8. doi: 10.1093/ajhp/53.18.2176. [DOI] [PubMed] [Google Scholar]
- 27.Dickson L.B., Somani S.M., Herrmann G., et al. Automated compounder for adding ingredients to parenteral nutrient base solutions. Am J Hosp Pharm. 1993;50(4):678–82. [PubMed] [Google Scholar]
- 28.Ryan D.M., Daniels C.E., Somani S.M. Personnel costs and preparation time in a centralized intravenous admixture program. Am J Hosp Pharm. 1986;43(5):1222–5. [PubMed] [Google Scholar]
- 29.Petros W.P., Shank W.A., Jr A standardized parenteral nutrition solution: prescribing, use, processing, and material cost implications. Hosp Pharm. 1986;21(7):648–9. [PubMed] [Google Scholar]
- 30.Turpin R, Canada T, Rosenthal V, et al. Bloodstream infections associated with parenteral nutrition preparation methods in the United States: a retrospective, large database analysis. JPEN J Parenter Enteral Nutr. In press [DOI] [PubMed]
- 31.Mercaldi C.J., Reynolds M.W., Turpin R.S. JPEN J Parenter Enteral Nutr. Epub. 2011. Methods to identify and compare parenteral nutrition administered from hospital compounded and premixed multi-chamber bags in a retrospective hospital claims database. [DOI] [PubMed] [Google Scholar]
- 32.Duan N. Smearing estimate: a nonparametric retransformation method. J Amer Statist Assoc. 1983;78:605–10. doi: 10.1080/01621459.1983.10478017. [DOI] [Google Scholar]
- 33.Zhang J., Yu K.F. What’s the relative risk? A method of correcting the odds ratios in cohort studies of common outcomes. JAMA. 1998;280(19):1690–1. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 34.McClave S.A., Martindale R.G., Vanek V.W., et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) JPEN J Parenter Enteral Nutr. 2009;33(3):277–316. doi: 10.1177/0148607109335234. [DOI] [PubMed] [Google Scholar]
- 35.Franzetti F., Borghi B., Raimondi F., et al. Impact on rates and time to first central vascular-associated bloodstream infection when switching from open to closed intravenous infusion containers in a hospital setting. Epidemiol Infect. 2009;137(7):1041–8. doi: 10.1017/S095026880800174X. [DOI] [PubMed] [Google Scholar]
- 36.Rangel-Frausto M.S., Higuera-Ramirez F., Martinez-Soto J., et al. Should we use closed or open infusion containers for prevention of bloodstream infections? Ann Clin Microbiol Antimicrob. 2010;9:6. doi: 10.1186/1476-0711-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rosenthal V., Maki D.G. Prospective study of the impact of open and closed infusion systems on rates of central venous catheter-associated bacteremia. Am J Infect Control. 2004;32(3):135–41. doi: 10.1016/j.ajic.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 38.Vilins M., Blecher S., Silva M.A., et al. Rate and time to develop first central line-associated bloodstream infections when comparing open and closed infusion containers in a Brazilian hospital. Braz J Infect Dis. 2009;13(5):335–40. doi: 10.1590/S1413-86702009000500004. [DOI] [PubMed] [Google Scholar]
- 39.Healthcare Cost and Utilization Project (HCUP) Rockville (MD): Agency for Healthcare Research and Quality; 2007. State Inpatient Databases (SID) [PubMed] [Google Scholar]
- 40.Databases and related tools from the Healthcare Cost and Utilization Project (HCUP): fact sheet [AHRQ publication no. 09-PFS003] Rockville (MD): AHRQ; 2009. [Google Scholar]
- 41.Neumayer L.A., Smout R.J., Horn H.G., et al. Early and sufficient feeding reduces length of stay and charges in surgical patients. J Surg Res. 2001;95(1):73–7. doi: 10.1006/jsre.2000.6047. [DOI] [PubMed] [Google Scholar]
- 42.Kyle U.G., Genton L., Pichard C. Hospital length of stay and nutritional status. Curr Opin Clin Nutr Metab Care. 2005;8(4):397–402. doi: 10.1097/01.mco.0000172579.94513.db. [DOI] [PubMed] [Google Scholar]
- 43.Genton L., Mühlebach S., Dupertuis Y.M., et al. Ergonomic and economic aspects of total parenteral nutrition. Curr Opin Clin Nutr Metab Care. 2006;9(2):149–54. doi: 10.1097/01.mco.0000214574.82686.ac. [DOI] [PubMed] [Google Scholar]
- 44.Ockenga J., Freudenreich M., Zakonsky R., et al. Nutritional assessment and management in hospitalised patients: implication for DRG-based reimbursement and health care quality. Clin Nutr. 2005;24(6):913–9. doi: 10.1016/j.clnu.2005.05.019. [DOI] [PubMed] [Google Scholar]
- 45.Donabedian H. Nutritional therapy and infectious diseases: a two-edged sword. Nutr J. 2006;5:21. doi: 10.1186/1475-2891-5-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Maswoswe J.J., Newcomer D.R., Quandt C.M. Achieving parenteral nutrition cost savings through prescribing guidelines and formulary restrictions. Am J Hosp Pharm. 1987;44(6):1376–81. [PubMed] [Google Scholar]
- 47.Holton D., Paton S., Conly J., et al. Central venous catheter-associated bloodstream infections occurring in Canadian intensive care units: a six-month cohort study. Can J Infect Dis Med Microbiol. 2006;17:169–76. doi: 10.1155/2006/781735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Weaver J., Willy M., Avigan M. Informatic tools and approaches in postmarketing pharmacovigilance used by FDA. AAPS J. 2008;10(1):35–41. doi: 10.1208/s12248-007-9004-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Velentgas P., West W., Cannuscio C.C., et al. Cardiovascular risk of selective cyclooxygenase-2 inhibitors and other non-aspirin non-steroidal anti-inflammatory medications. Pharmacoepidemiol Drug Saf. 2006;15:641–52. doi: 10.1002/pds.1192. [DOI] [PubMed] [Google Scholar]


