Abstract
Background
A long-standing debate concerns whether dysfunctional cognitive processes and content play a causal role in the etiology of depression or more simply represent correlates of the disorder. There has been insufficient appreciation in this debate of specific predictions afforded by cognitive theory in relation to major life stress and changes in cognition over time. In this paper we present a novel perspective for investigating the etiological relevance of cognitive factors in depression. We hypothesize that individuals who experienced a severe life event prior to the onset of major depression will exhibit greater changes in dysfunctional attitudes over the course of the episode than will individuals without a severe life event.
Method
Fifty-three participants diagnosed with major depression were assessed longitudinally, approximately 1 year apart, with state-of-the-art measures of life stress and dysfunctional attitudes.
Results
Depressed individuals with a severe life event prior to episode onset exhibited greater changes in cognitive biases over time than did depressed individuals without a prior severe event. These results were especially pronounced for individuals who no longer met diagnostic criteria for major depression at the second assessment.
Conclusions
Specific patterns of change in cognitive biases over the course of depression as a function of major life stress support the etiological relevance of cognition in major depression.
INTRODUCTION
Cognitive theories of depression propose that, at least for particular subtypes of major depression, biases or distortions in the processing of emotional information are associated with the onset, maintenance and remission of the disorder (Beck, 1987; Abramson et al. 1989; Blatt & Zuroff, 1992; Ingram et al. 1998; Gotlib & Neubauer, 2000; Sher et al. 2005). A wealth of empirical research has demonstrated that during a depressive episode, many aspects of cognition are altered. Furthermore, when a depressive episode remits, cognitive biases tend to normalize (Gotlib & Cane, 1987; Dohr et al. 1989; Ingram et al. 1998), although not all studies evidence this pattern (see Just et al. 2000). Overall, changes in cognitive processing as the depressive episode begins and ends are considered to be core causal elements in the cognitive model.
The centrality of cognition in the onset and course of depression, however, is not clear based on such information alone. Depression affects functioning across a range of social, psychological, cognitive and biological processes, and distorted cognitions or altered information processing may be simply another characteristic or ‘symptom’ of depression, as are disruptions of sleep and mood (Teasdale, 1983; Coyne, 1992). More generally, a long-standing challenge has been for research to distinguish causal factors from factors that are only correlates or consequences of the disorder (Monroe & Steiner, 1986; Barnett & Gotlib, 1988a; Kramer et al. 1997). Indeed, some critics contend that much of the existing literature on cognitive factors in depression reflects associations that are essentially irrelevant for etiology (Coyne, 1992). Consequently, other approaches are required to clarify how cognitive dysfunction is, or is not, involved with the etiology of depression.
One approach to clarify the etiological significance of cognition in depression is to develop more precise tests of cognitive theory for this disorder. For example, cognitive models posit that vulnerability to depression is associated with schemas that remain latent until activated by a stressful life event (Beck, 1967, 1976; Ingram & Ritter, 2000). Once the schemas are activated, biased information processing and increased negative cognitive content contribute to depressive affect, which in turn further reinforces the operation of these negative cognitive factors (Ingram et al. 1998). Moreover, when the depression begins to abate, distorted cognitive functioning subsides and approximates pre-morbid levels. Overall, cognitive theory predicts that major life stress initially activates schema-driven biased information processing, thereby increasing negative cognitive content and, furthermore, that these stress-activated cognitive processes eventually normalize with recovery.
Because major depression is a disorder with heterogeneous causes and distinct subtypes (Abramson et al. 1989; Gotlib & Hammen, 2002), life stress (and its implications for cognitive functioning) is most probably is a central feature for a subset of depressed individuals. In this vein, it is noteworthy that one of the most consistent findings in depression research is that severe life events often, but not always, precede the onset of a major depressive episode (Mazure, 1998; Monroe & Hadjiyannakis, 2002; Hammen, 2005). Thus, information about severe or major life events occurring prior to onset could provide an important focus for understanding individual differences in changes in cognitive biases over time for depression.
When considered in the context of cognitive theories of depression, these ideas and data on major life stress present an innovative hypothesis. Because life stress activates negative cognitive schemas, depressed persons who experience major stress prior to onset should exhibit distinctive patterns of change in cognitive processing and content over the course of their depressive episode. Specifically, depressed people with major stress should show over time a more pronounced decrease in distorted thinking and processes, reflecting the initial activation of depressive cognition and the subsequent normalization with recovery. By contrast, depressed people without major life events prior to onset should show less dramatic changes in cognitive functioning over the course of their depressive episode. Generally stated, depressed persons who have and who have not experienced a prior major life event should be characterized by different slopes for change in biased cognition from the acute phase of the disorder over time and with recovery.
These predictions have important implications for the role of cognitive factors in the etiology of depression. Specifically, a unique association between major events and cognitive changes over time would help to rule out the concern that cognitive changes are due to the confounding of cognition with depression. Findings of a specific pattern of change in cognitive biases for the stress group alone cannot be dismissed as merely an artifact of depression abating, or as another symptom of depression decreasing as the episode subsides. If biased cognition simply ebbed and flowed with changes in the severity of depressive symptoms, a particular pattern of changes would not be associated with major life stress. Rather, the initial elevation followed by a decrease in cognitive bias would be evident for all depressed individuals, regardless of whether they experienced prior major life stress. Furthermore, findings of specific changes in cognition associated with major life stress would support the inference that cognitive factors are of causal relevance, albeit indirectly. That is, cognitive changes that are distinctively related to major life stress are consistent with theory, even though they do not directly test the initial activation component. Overall, a unique association of cognitive changes with antecedent major stress : (1) is precisely what would be predicted from cognitive theories of depression; (2) would help to counter the argument that such changes are merely a function of changes in depression status; and (3) would provide a conceptually consistent etiological explanation of changes in cognitive functioning over time.
Although the theoretical importance of the interaction of major life events with changes in cognitive bias has not been discussed previously, indirect empirical support is found in a number of studies. For example, investigators have reported that the interaction of life events with cognitive vulnerability predicts subsequent changes in depression. Some of these studies used ‘remission’ designs, in which high stress and high cognitive dysfunction in depressed samples prior to onset predicts lower levels of depression over time or with treatment (e.g. Simons et al. 1995). Other studies utilized ‘developmental’ designs, in which high stress and high cognitive dysfunction in initially non-depressed samples predict subsequent increases in depressive symptoms over time (e.g. Hankin et al. 2004). Although the results of these lines of research have not been entirely consistent (cf. Barnett & Gotlib, 1988b, 1990; see Scher et al. 2005, for a recent review), overall the data suggest the importance of stress–cognition interactions for the development, course and remission of depression. The crucial piece of information that is missing, however, is data on the specific pattern of changes in cognitive functioning over time in relation to major life stress.
The present study was designed to provide a prospective test of these specific predictions regarding life stress and changes in biased cognition for depressed individuals over time. The general hypothesis is that persons with major depression who experienced a severe life event within 12 weeks prior to onset would demonstrate a distinctive pattern of greater change in cognitive biases from the acute phase of the active episode over time as the episode ends. By contrast, depressed persons who had not experienced a major life event prior to onset would be expected to exhibit a pattern of less change in cognitive biases over the course of the disorder.
We used two analytical strategies to test this general hypothesis. First, for the full sample of 53 individuals in the acute phase of major depression, we assessed life stress and cognitive functioning during the acute phase (Time 1), and conducted a follow-up assessment of cognitive functioning approximately a year later. This interval between assessments provided sufficient time for the changes in cognition and depression to occur. Second, it is likely that changes in cognitive functioning in relation to life stress are most evident for participants who experience clinical improvement. Based on this line of reasoning, we conducted a second set of analyses on 37 participants who evidenced clinical improvement by the time of the second assessment. Although this latter approach possesses less statistical power, the enhanced sensitivity of the design increases the likelihood of detecting differential changes in cognitive bias with recovery from depression. Overall, these two approaches converge on the general question of whether biased cognition in depression is uniquely related to prior major life stress and, if so, they provide a novel and informative examination of the meaning of such changes.
METHOD
Participants and procedures
Participants were 53 adults (38 females, 15 males) between the ages of 18 and 58 (mean = 34.25, s.d.=10.08) diagnosed with major depressive disorder (MDD). Participants were a subset of individuals from a larger investigation (see Gotlib et al. 2004a, b; Monroe et al. 2007), with inclusion in the present study requiring participants with a recent onset of depression and two clinical and cognitive assessments separated by approximately 1 year. Sixty per cent of participants were single (32% married or living with a partner; 8% divorced or widowed) and 64% were Caucasian (28% Asian; 4% African American; 4% Latino/Hispanic). Participants tended to be well educated (28% had a graduate or professional degree; 57% had completed 4 years of college ; 15% had some college) and to have diverse incomes (15% less than US$10 000, 17% between US$10 000 and US$25 000, 23% between US$25 000 and US$50 000, 19% between US$50 000 and US$75 000, and 19% over US$100 000; four subjects did not provide income information). Participants were recruited through advertisements and flyers, and through referrals from two out-patient psychiatry clinics at Stanford University.
All participants were screened by telephone to recruit individuals with a high likelihood of meeting DSM-IV criteria for current MDD with a relatively recent onset of the disorder (98% of the present sample had an onset within the previous 2 years). Individuals who passed this initial telephone screen were invited to the Department of Psychology at Stanford University, where they were administered a structured diagnostic interview and completed self-report questionnaires. Individuals who met criteria for study inclusion (see below) were asked to return approximately 1 week later to complete additional measures. Participants then were invited for a third session in which the life stress interview was administered. All participants provided written informed consent and were paid $25 per hour.
All individuals were administered the Structured Clinical Interview for DSM-IV (SCID; First et al. 1995) and met criteria for current MDD according to DSM-IV (APA, 1994). Individuals were excluded if they had current co-morbid panic disorder or social phobia; a lifetime history of mania, hypomania, or primary psychotic symptoms; a recent history (past 6 months) of alcohol or psychoactive substance abuse or dependence; or a history of brain injury or mental retardation. Interviewers were advanced psychology graduate students and post-baccalaureate research assistants. To assess inter-rater reliability, an independent rater who was unaware of group membership evaluated randomly selected audiotapes of SCIDs. These interviews were drawn from individuals for the overall parent project, and included people who met criteria for depression, social phobia, and panic disorder, and those who did not meet diagnostic criteria. In all 15 cases, diagnoses of depression, social phobia and non-psychiatric control matched the diagnosis made by the original interviewer, κ = 1.00. Although this represents excellent reliability, the interviewers used the ‘skip out’ strategy of the SCID, which may have reduced the opportunities for the independent raters to disagree with the diagnoses (Gotlib et al. 2004a, b). Participants were recontacted approximately 1 year after the initial assessment (mean = 337.46 days) and their clinical status was re-evaluated to determine if they still met DSM-IV criteria for MDD (n=16), or no longer met criteria for MDD (n = 37).
Measures
Life stress assessment
The Life Events and Difficulties Schedule (LEDS; Brown & Harris, 1978) was used to assess and operationalize life stress. The LEDS system uses a semi-structured interview that systematically covers life domains and provides the respondent with numerous probes and opportunities to stimulate recall of past experiences. This information is subsequently presented to a panel of raters trained in the LEDS procedures to define life events and rate dimensions of life stress (Brown & Harris, 1978). Relevant information pertaining to stressors is presented first, with raters permitted to ask clarifying questions. Subsequently, each rater provides ratings of the major stress dimensions (see below). All discrepancies are then resolved through group discussion and consensus ratings.
Previous research with the LEDS has established severe acute events as important for predicting the onset of depression (Brown & Harris, 1989; Mazure, 1998; Monroe & Hadjiyannakis, 2002). This is an explicitly defined category of events that is based on a high degree of contextual threat, unpleasantness, and a high likelihood of prolonged consequences. Within the LEDS rating system, all events are rated based on extensive information about the circumstances surrounding the event and on the particular individual’s biographic circumstances (i.e. ‘contextual’ ratings ; see Brown & Harris, 1978; Brown, 1989). In accord with prior research using LEDS procedures (Brown & Harris, 1989; Monroe & Hadjiyannakis, 2002), a 12-week period prior to the onset of the depressive episode was used to define the presence or absence of a severe event.
After interviewers completed the LEDS assessment at Stanford, they presented the detailed life stress information by teleconferencing to trained raters at the University of Oregon (Eugene). For these operations, the LEDS manuals provide extensive examples to assist with standardization (e.g. the 520-page manual contains thousands of case vignettes for defining events and assigning contextual threat ratings). All ratings were performed after discussion and consensus agreement, and were carried out blind to relevant information (e.g. timing of depression onset, participant emotional response to event, cognitive bias). On average, interviews and rating sessions each required approximately 2 hours to complete.
The LEDS has established psychometric validity and is widely regarded as a state-of-the-art instrument for measuring life stress (Brown, 1989; Hammen, 2005). Reliability for the present project for pair-wise comparisons of 2–4 raters ranged from 0.72 to 0.79 (mean = 0.76; Cohen’s κ, corrected for differences in the number of raters per event; Uebersax, 1982).
Dysfunctional cognitions
The Dysfunctional Attitude Scale (DAS) is a 40-item self-report questionnaire designed to measure the presence of excessive and rigid maladaptive beliefs that are hypothesized to render an individual vulnerable to depression (Beck, 1967, 1976). The DAS has good internal consistency (coefficient α=0.95 for Time 1 and Time 2 the present study) and a test–retest correlation of 0.84 over an 8-week period (Weissman, 1979; see also Fava et al. 1994; Furlong & Oei, 2002).
Analyses
The primary analyses were two two-way repeated-measures analyses of variance (ANOVA) conducted on DAS scores, with presence or absence of severe life events in the 12 weeks preceding onset as the between-subjects factor, and Time 1/Time 2 as the within-subject factor. In the first ANOVA, all 53 participants were included (eight of these participants had experienced a severe event in the 12 weeks prior to onset). In the second ANOVA, the analyses were restricted to the participants who were no longer depressed (n = 37) at the second assessment (six of these participants had experienced a severe event in the 12 weeks prior to onset).1,†
RESULTS
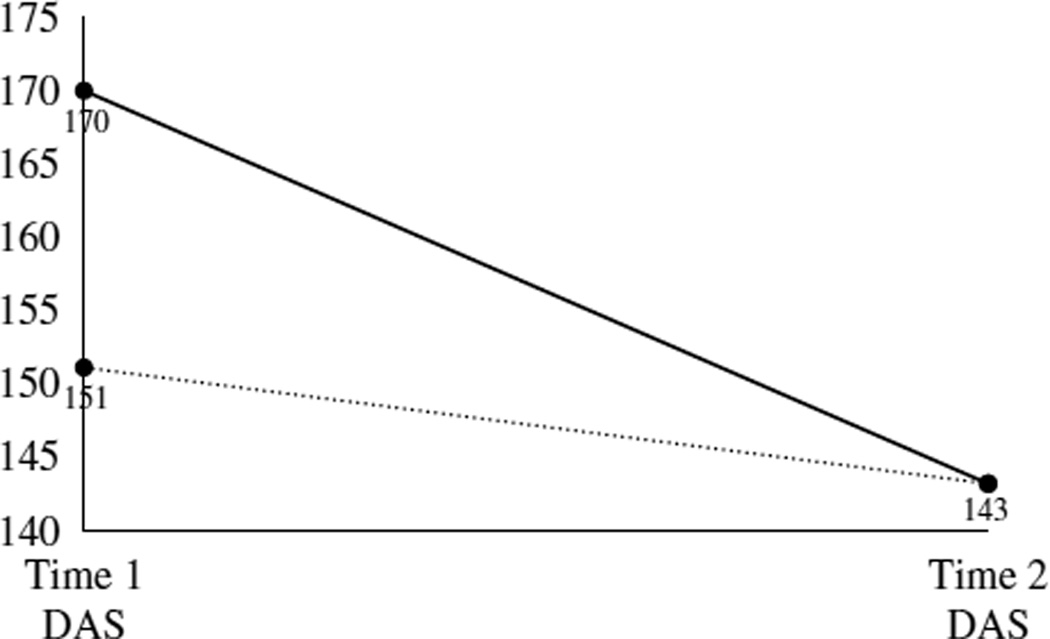
For the full sample, the first repeated-measures ANOVA conducted on DAS scores yielded the expected main effect for time [F(1, 51) = 17.11, p<0.001; η2partial = 0.25] ; DAS scores at Time 1 (mean = 153.94, s.d. = 38.15) were significantly higher than were scores at Time 2 (mean = 143.40, s.d.=36.89). The main effect for life events (i.e. DAS scores collapsed over time) was not significant [F(1, 51) = 0.46, p≥0.50; η2partial = 0.01]. Most important, and consistent with the study hypotheses, there was a significant interaction between life stress and changes in DAS scores from Time 1 to Time 2 [F(1, 51) = 5.26, p<0.03; η2partial = 0.09]. This interaction is presented graphically in Fig. 1. Probing this interaction revealed that participants with a severe event prior to the onset of depression exhibited a significantly greater change in cognitive bias from Time 1 to Time 2 than did participants without a severe event [mean = 26.75, s.d. = 35.46 v. mean = 7.67, s.d. = 18.58; t(51) = 2.29, p<0.03].2
Fig. 1.
Change in cognitive biases over the course of depression as a function of major life stress within 12 weeks prior to episode onset.  , Severe event;
, Severe event;  , No severe event. DAS, Dysfunctional Attitudes Scale.
, No severe event. DAS, Dysfunctional Attitudes Scale.
Stronger effects were found when the sample was restricted to participants who exhibited clinical improvement over the two assessments. Specifically, as expected, main effect for time on cognitive functioning was significant [F(1, 53) = 27.16, p<0.001; η2partial = 0.44]. DAS scores at Time 1 (mean = 154.32, s.d. = 40.33) were significantly higher than scores at Time 2 (mean = 141.35, s.d. = 38.17). Again, there was no main effect for stress [F(1, 35) = 1.85, p>0.15; η2partial = 0.05]. Finally, the interaction of stress with time was highly significant in predicting changes in DAS scores [F(1, 35) = 12.07, p≤0.001; η2partial = 0.26]. Parallel analyses to those described above revealed that, compared to the non-severe event group, participants with a severe event had a much larger and highly significant decrease in cognitive bias between Time 1 and Time 2 [mean = 39.33, s.d. = 26.20 v. mean = 7.87, s.d. = 19.15; t(35) = 3.47, p≤0.001].3
DISCUSSION
There has been considerable debate about the meaning of changes in cognitive functioning as an individual recovers from a depressive episode. One plausible and parsimonious argument is that cognitive biases are simply symptoms of depression. By contrast, cognitive conceptualizations of depression suggest specific, theoretically driven alternations in cognitive biases over the course of a depressive episode. What has been needed is an empirical means of distinguishing between these two competing accounts of the nature of the relationship between cognitive biases and depression over time. We introduce life stress as a pivotal theoretical consideration for probing the meaning of changes in cognitive bias over the course of a depressive episode, and present data congruent with these expanded predictions afforded by cognitive theory.
Cognitive theories of depression assume a role for life stress in activating dysfunctional thinking (Scher et al. 2005). As we have pointed out, this formulation dovetails with the extensive literature on the prevalence of major life events prior to the onset of depression, the latter indicating that many, but not all, people who become depressed do so following a severe life event (Mazure, 1998; Hammen, 2005). If changes in cognitive bias are uniquely linked to the presence of major life events prior to the onset of depression, then such findings counter the concern that the cognitive factors are simply symptoms of the disorder, and argue for the relevance of an interactive role of stress and cognition in triggering a depressive episode. The present results are consistent with this position and demonstrate that antecedent major life events predict a distinctive pattern of cognitive change over the course of a depressive episode.
Using the full sample of participants (assuming that depressed people tend to recover over time), we examined the role of major events in predicting different patterns of change in dysfunctional thinking. As hypothesized, individuals with major life events prior to onset experienced larger decreases in dysfunctional thinking over time than did individuals who did not experience such stressors. Furthermore, examining a subset of depressed people who no longer met diagnostic criteria for major depression at the second assessment, these findings were reinforced and strengthened. Each of these two approaches indicates differential decreases in cognitive biases over time as a function of the presence or absence of prior major life events. These differential patterns of change are difficult to explain by – and thereby directly challenge – the position that cognitive variations merely reflect changes in the symptoms of depression. Thus, these results provide a fresh avenue of information that adds to the emerging literature indicating that cognitive processes and content are not solely confounded with depression.
It is also interesting that the distinctive pattern of change in dysfunctional attitudes from the acute phase of the disorder to the follow-up assessment matched the specific pattern predicted from the cognitive diathesis-stress perspective we extrapolated. Although we did not have information on cognitive biases prior to onset of depression to fully test the activation component of the model, we did measure dysfunctional attitudes and beliefs during the acute phase of the disorder. Furthermore, the LEDS methodology assessed life stress during the same time period, and has demonstrated high reliability and capability for assuring the timing of life events in relation to depression onset (Brown & Harris, 1978, 1989). Thus, the design is prospective, in that these two pieces of information together forecasted the subsequent distinctive patterns of change in cognition. Because this pattern is precisely what would be expected from a causal model based on cognitive theories of depression, the present results lend further, albeit indirect, support for a causal role of cognitive factors in depression. Nonetheless, as noted, we did not have a ‘complete’ prospective picture (i.e. measures of cognitive processes or content prior to the onset of the depressive episode were not available). The full temporal ordering and unfolding of cognitive changes over time as a function of stress can only be inferred from these data. A next step in this line of research is to assess individuals at multiple time points, beginning prior to the occurrence of both life events and the onset of depression. With such an approach, the temporal sequence involving stress and cognitive activation could be delineated more precisely.
Two aspects of the present study are noteworthy and merit further discussion. First, given the overall propensity for cognitive biases to abate as the depressive episode subsides, it is all the more remarkable that the presence or absence of major stress forecasted a distinctive pattern of change over time. That is, against the general backdrop of decreases in dysfunctional thinking as depression remits, finding larger decreases for people with severe major events is especially important. The second point worth noting involves the comparatively stronger effects obtained for individuals who experienced formal improvement in clinical status over the two assessments. We would expect that chronic forms of depression would not be informative with respect to changes in cognitive biases over repeated measurement occasions (as long as they remained clinically depressed). That is, the inclusion of individuals with chronic depression would be likely to reduce the sensitivity of the study design to detect differences in cognitive changes between individuals with and without stress. This interpretation is in keeping with the stronger effects for changes in cognitive bias by stress group for participants who had at least partially remitted from their depressive episode. Because of the relatively small number of fully remitted depressed individuals, we were not able to evaluate this issue in greater detail. We predict, however, that future studies examining samples of fully remitted individuals will show even stronger differential changes in dysfunctional thinking as a function of major life stress.
Given the intensive assessment requirements for measuring life stress and following participants over time, the sample size was limited. Although this does not detract from the importance of the positive findings for the predicted results, it does suggest that with greater power, differences between the stress groups would be more pronounced (e.g. see notes 2 and 3). Larger samples would also permit more fine-grained analyses of related tenets of cognitive theory (e.g. matching of specific types of events and types of cognitive vulnerability) and stress theory (e.g. capability of less severe stressors to activate cognitive biases) to be conducted. Nevertheless, it is important to emphasize that the approach we have adopted provides a novel empirical inroad to investigating a historically challenging issue, and that the findings are consistent with these theoretical principles.
ACKNOWLEDGMENTS
This work was sponsored in part by National Institute of Mental Health Research Grants MH60802 (S.M.M.) and MH59259 (I.H.G.). We thank Lauren Anas, Erica Aronson, Kathryn Dingman and Danielle Keenan-Miller for help with conducting life stress interviews, and Faith Brozovich for assisting with data management. For participating in stress ratings, we thank Keely Muscatell, Julien Guillaumot, Corrie Doyle and Tiffany Thornton.
Footnotes
The notes appear on p. 869.
Preliminary analyses examined associations between major demographic and clinical variables with stress and cognitive bias. Few significant associations emerged, and the primary analyses were rerun controlling for these possible confounding associations. The results of these latter analyses in all instances were substantively the same as those for the reported analyses.
The primary hypothesis was that major stress predicts a greater degree of change in cognitive bias over time. This is addressed most directly as reported above by comparing change in DAS scores from Time 1 to Time 2 for the participants with and without severe events. Post hoc analyses of both the between and within contrasts for the stress/no-stress groups over the two time points, however, are also of interest. (Despite clear a priori directional predictions, we maintain conservative two-tailed tests of statistical significance.) For the full study sample (n = 53), participants with a severe event compared to those without a severe event had non-significantly higher DAS scores at Time 1 [mean = 170.00, s.d. = 49.75 v. mean = 151.09, s.d. = 35.65; t(51) = 1.30, p≥0.20] and, as expected, did not evidence any trend toward differences at follow-up on the DAS (Time 2) [mean = 143.25, s.d. = 37.09 v. mean = 143.42, s.d. = 37.28; t(51)=−0.12, p>0.90]. Moreover, participants with a severe event had a large but statistically marginal decline from Time 1 to Time 2 on the DAS [mean = 170.00, s.d.=49.75 v. mean = 143.25, S.D. = 37.09; paired t(7) = 2.13, p≤0.07]. Although participants without a severe event had less of an absolute decrease in DAS score from Time 1 to Time 2, these changes attained statistical significance [mean = 151.09, s.d. = 35.65 v. mean = 143.42, s.d. = 37.28; paired t(44)=2.77, p<0.01], probably because of the larger number of subjects and greater statistical power.
For the restricted sample of participants evidencing clinical change over the course of the study (n = 37), post hoc analyses for the interaction parallel to those conducted in note 2 indicated that participants with a severe event, compared to those without a severe event, had significantly higher DAS scores at Time 1 [mean = 186.33, s.d. = 46.70 v. mean = 148.13, s.d. = 36.66; t(35) = 2.24, p<0.04] and, as expected, did not evidence any trend toward differences at follow-up on the DAS (Time 2) [mean = 147.00, s.d. = 40.11 v. mean = 140.26, s.d. = 38.37; t(35) = 0.39, p>0.65]. Moreover, participants with a severe event had a large and statistically significant decline from Time 1 to Time 2 on the DAS [mean = 186.33, s.d. = 46.70 v. mean = 147.00, s.d. = 40.11; paired t[5] = 3.68, p<0.02]. Participants without a severe event again had less of an absolute decrease in DAS score from Time 1 to Time 2, which also remained statistically significant [mean = 148.13, s.d. = 36.66 v. mean = 140.26, s.d. = 38.37; paired t(30)=2.29, p<0.03].
Portions of the results reported in this article were presented at the 18th Annual Meeting of the Society for Research in Psychopathology in Toronto, Ontario, Canada.
DECLARATION OF INTEREST
None.
REFERENCES
- Abramson LY, Metalsky GI, Alloy LB. Hopelessness depression: a theory-based subtype of depression. Psychological Review. 1989;96:358–372. [Google Scholar]
- APA. Diagnostic and Statistical Manual of Mental Disorders. 4th edn. Washington, DC: American Psychiatric Press; 1994. [Google Scholar]
- Barnett PA, Gotlib IH. Psychosocial functioning and depression: distinguishing among antecedents, concomitants, and consequences. Psychological Bulletin. 1988a;104:97–126. doi: 10.1037/0033-2909.104.1.97. [DOI] [PubMed] [Google Scholar]
- Barnett PA, Gotlib IH. Dysfunctional attitudes and psychosocial stress : the differential prediction of future psychological symptomatology. Motivation and Emotion. 1988b;12:251–270. [Google Scholar]
- Barnett PA, Gotlib IH. Cognitive vulnerability to depressive symptoms among men and women. Cognitive Therapy and Research. 1990;14:47–61. [Google Scholar]
- Beck AT. Depression: Clinical, Experimental, and Theoretical Aspects. Philadelphia: University of Pennsylvania Press; 1967. [Google Scholar]
- Beck AT. Cognitive Therapy and the Emotional Disorders. Oxford: International Universities Press; 1976. [Google Scholar]
- Beck AT. Cognitive model of depression. Journal of Psychotherapy. 1987;1:2–27. [Google Scholar]
- Blatt SJ, Zuroff DC. Interpersonal relatedness and selfdefinition: two prototypes for depression. Clinical Psychology Review. 1992;12:527–562. [Google Scholar]
- Brown GW. Life events and measurement. In: Brown GW, Harris TO, editors. Life Events and Illness. London: Guilford Press; 1989. pp. 3–45. [Google Scholar]
- Brown GW, Harris TO. Social Origins of Depression : A Study of Psychiatric Disorder in Women. New York: The Free Press; 1978. [Google Scholar]
- Brown GW, Harris TO. Depression. In: Brown GW, Harris TO, editors. Life Events and Illness. London: Guilford Press; 1989. pp. 49–93. [Google Scholar]
- Coyne JC. Cognition in depression : a paradigm in crisis. Psychological Inquiry. 1992;3:232–234. [Google Scholar]
- Dohr KB, Rush AJ, Bernstein IH. Cognitive biases and depression. Journal of Abnormal Psychology. 1989;98:263–267. doi: 10.1037//0021-843x.98.3.263. [DOI] [PubMed] [Google Scholar]
- Fava M, Bless E, Otto MW, Pava JA, Rosenbaum JF. Dysfunctional attitudes in major depression: changes with pharmacotherapy. Journal of Nervous and Mental Disease. 1994;182:45–49. [PubMed] [Google Scholar]
- Furlong M, Oie TPS. Changes to automatic thoughts and dysfunctional attitudes in group CBT for depression. Behavioral and Cognitive Psychotherapy. 2002;30:351–360. [Google Scholar]
- First MB, Spitzer MB, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders – Patient Edition (SCID-I/P, Version 2.0) New York: Biometrics Research Department, New York State Psychiatric Institute; 1995. [Google Scholar]
- Gotlib IH, Cane CA. Construct accessibility and clinical depression: a longitudinal investigation. Journal of Abnormal Psychology. 1987;96:199–204. doi: 10.1037//0021-843x.96.3.199. [DOI] [PubMed] [Google Scholar]
- Gotlib IH, Hammen CL, editors. Handbook of Depression. New York: Guilford Press; 2002. Introduction. [Google Scholar]
- Gotlib IH, Kasch KL, Traill S, Joormann J, Arnow BA, Johnson SL. Coherence and specificity of informationprocessing biases in depression and social phobia. Journal of Abnormal Psychology. 2004a;113:386–398. doi: 10.1037/0021-843X.113.3.386. [DOI] [PubMed] [Google Scholar]
- Gotlib IH, Krasnoperova E, Yue DN, Joormann J. Attentional biases for negative interpersonal stimuli in clinical depression. Journal of Abnormal Psychology. 2004b;113:127–135. doi: 10.1037/0021-843X.113.1.121. [DOI] [PubMed] [Google Scholar]
- Gotlib IH, Neubauer DL. Information-processing approaches to the study of cognitive biases in depression. In: Johnson SL, Hayes AM, Field TM, Schneiderman N, McCabe S, editors. Stress, Coping, and Depression. Hillsdale, NJ: Erlbaum; 2000. pp. 117–143. [Google Scholar]
- Hammen C. Stress and depression. Annual Review of Clinical Psychology. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY, Miller N, Haeffel GJ. Cognitive vulnerability-stress theories of depression: examining affective specificity in the prediction of depression versus anxiety in three prospective studies. Cognitive Therapy and Research. 2004;28:309–345. [Google Scholar]
- Ingram RE, Miranda J, Segal ZV. Cognitive Vulnerability to Depression. New York: Guilford Press; 1998. [Google Scholar]
- Ingram RE, Ritter J. Vulnerability to depression: cognitive reactivity and parental bonding in hi-risk individuals. Journal of Abnormal Psychology. 2000;109:588–596. doi: 10.1037//0021-843x.109.4.588. [DOI] [PubMed] [Google Scholar]
- Just N, Abramson LY, Alloy LB. Remitted depression studies as tests of the cognitive vulnerability hypotheses of depression onset: a critique and conceptual analysis. Clinical Psychology Review. 2000;21:63–83. doi: 10.1016/s0272-7358(99)00035-5. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Kazdin AE, Offord DR, Kessler RC. Coming to terms with the terms of risk. Archives of General Psychiatry. 1997;54:337–343. doi: 10.1001/archpsyc.1997.01830160065009. [DOI] [PubMed] [Google Scholar]
- Mazure CM. Life stressors as risk factors in depression. Clinical Psychology: Science and Practice. 1998;5:291–313. [Google Scholar]
- Monroe SM, Hadjiyannakis K. The social environment and depression: focusing on severe life stress. In: Gotlib IH, Hammen CL, editors. Handbook of Depression. New York: Guilford Press; 2002. pp. 314–340. [Google Scholar]
- Monroe SM, Slavich GM, Torres LD, Gotlib IH. Major life events and major chronic difficulties are differentially associated with history of major depression. Journal of Abnormal Psychology. 2007;116:116–124. doi: 10.1037/0021-843X.116.1.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe SM, Steiner SC. Social support and psychopathology: interrelations with preexisting disorder, stress, and personality. Journal of Abnormal Psychology. 1986;95:29–39. doi: 10.1037//0021-843x.95.1.29. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Torres L, Guillaumot J, Harkness KL, Roberts JE, Frank E, Kupfer D. Life stress and the long-term treatment course of recurrent depression: III. Non-severe life events predict recurrence for medicated patients over 3 years. Journal of Consulting and Clinical Psychology. 2006;74:112–120. doi: 10.1037/0022-006X.74.1.112. [DOI] [PubMed] [Google Scholar]
- Scher CD, Ingram RE, Segal ZV. Cognitive reactivity and vulnerability : empirical evaluation of construct activation and cognitive diatheses in unipolar depression. Clinical Psychology Review. 2005;25:487–510. doi: 10.1016/j.cpr.2005.01.005. [DOI] [PubMed] [Google Scholar]
- Simons AD, Gordon JS, Monroe SM, Thase ME. Toward an integration of psychologic, social, and biologic factors in depression: effects on outcome and course of cognitive therapy. Journal of Consulting and Clinical Psychology. 1995;63:369–377. doi: 10.1037//0022-006x.63.3.369. [DOI] [PubMed] [Google Scholar]
- Teasdale JD. Negative thinking in depression: cause, effect, or reciprocal relationship? Advances in Behavior Therapy and Research. 1983;5:3–25. [Google Scholar]
- Uebersax JS. A generalized kappa coefficient. Educational and Psychological Measurement. 1982;42:181–183. [Google Scholar]
- Weissman A. The Dysfunctional Attitude Scale: a validation study. Dissertation Abstracts International. 1979;40:1389–1390. [Google Scholar]